User login
The search for the hidden depressant
History: Initial symptoms
Ms. G, 17, has battled attention-deficit/hyperactivity disorder (ADHD) since age 6, and within the past 2 years was also diagnosed as having schizoaffective disorder, bipolar type. An outpatient child psychiatrist and a therapist have helped keep her symptoms in control through much of her life.
During one recent visit to her psychiatrist, however, she complained of decreased energy, increased crying spells, broken sleep, and a depressed mood. She reported that these symptoms began approximately 2 months before the visit, and neither she nor her parents could identify a clear-cut cause.
Throughout her life she has complied with her drug regimens. For 2 years she has been taking divalproex sodium, 500 mg twice daily to manage her manic and depressive episodes, dextroamphetamine sulfate, 30 mg in the morning for her ADHD; risperidone, 2 mg at bedtime for her psychotic symptoms; and mestranol, 60 mcg/d, plus norethindrone, 1 mg/d, for contraception. A recent valproic acid reading of 62 μg/ml is consistent with levels over the last 2 years.
During previous psychotic episodes, Ms. G often became delusional and paranoid with command-type hallucinations. She destroyed her room during her most recent episode.
Ms. G’s adoptive mother accompanied her during this visit. She is concerned for her daughter, especially with the start of school about 1 month away.
Which would you address first: the depression or the psychosis? Would you change Ms. G’s medication and if so, how?
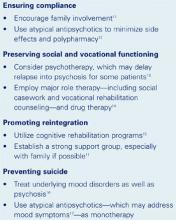
Figure 1 DEPRESSION IN SCHIZOPHRENIA: IMPROVING OUTCOMES
Drs. Yu’s and Maguire’s observations
Complaints of depression in a patient with schizoaffective disorder are especially concerning because multiple domains could be affected (Figure 1). For patients with schizophrenia, the 60% lifetime incidence of major depressive disorder substantially exceeds the 8 to 26% risk in the general population. Ms. G’s comorbid depression also may predispose her to an increased rate of relapse into schizoaffective psychosis, poor treatment response, and a longer duration of psychotic illness that could require hospitalization.1
Although Ms. G’s divalproex level was therapeutic (between 50 and 100 μg/ml), some data indicate that valproic acid may be less effective in schizoaffective disorder than in bipolar I disorder. Still, treatment of schizoaffective disorder often follows antimanic and antidepressant protocols.2
Treatment: An agent is added
The outpatient psychiatrist adds fluoxetine, 20 mg each morning, to address Ms. G’s depressive symptoms. She reports no improvement after 1 month, and her fluoxetine is increased to 30 mg/d.
Three weeks later, Ms. G’s parents bring her to the psychiatrist for an emergency visit. She reports suicidal ideation over the previous month. Rolling up both sleeves, she reveals several superficial cuts on her forearms and wrists that she inflicted after breaking up with her boyfriend.
Her mother, appearing anxious and overwhelmed, reports that her daughter pushed her because she had refused to give Ms. G her calling card. She had told her mother that she wanted to call a boy in Utah that she had met over the Internet.
Ms. G’s speech is noticeably pressured and she is extremely distractible. Her mother notes that her daughter is sleeping only 2 to 3 hours a night, yet exhibits no decrease in energy. Still depressed, her affect is markedly labile, crying at one moment when discussing her suicidality, then railing at her mother when she tries to explain Ms. G’s aggressiveness. When the psychiatrist recommends hospitalization to stabilize her symptoms, she vehemently demands to be let out so that she can run in front of a moving car. The police are called, and she is restrained and brought into the hospital.
What caused Ms. G’s sudden decline? How would you address it?
Drs. Yu’s and Maguire’s observations
Although antidepressants can effectively treat depression in schizoaffective disorder, many of these medications can trigger a manic episode,3 which can include mania, mixed mania with depression, or rapid cycling every few days or hours. In Ms. G’s case, an increase in serotonin due to the fluoxetine may have caused her mania.
We would stop the fluoxetine and see if her manic symptoms resolve. Fluoxetine’s long half-life (4 to 16 days) cuts down the odds of a serotonin-discontinuation syndrome, making immediate discontinuation feasible.
Still, the cause of Ms. G’s depressive symptoms remains unknown. At this stage, observation in the adolescent inpatient ward holds our best hope of reaching a definitive diagnosis.
Treatment: A diagnostic clue surfaces
Blood tests on admission (including a negative drug screen for narcotics or other depressogenic substances) are normal, and her valproic acid level is 61 μg/ml. Her divalproex is increased to 500 mg in the morning and 750 mg at bedtime, and she is tapered off fluoxetine. Her symptoms gradually improve with the change in the medications and her attendance in milieu and group therapy on the ward. A second valproic acid reading on day three of hospitalization is 67 μg/ml.
That day, a nurse informs the inpatient child/adolescent psychiatrist that Ms. G has requested extra hospital gowns. Ms. G later reveals that for about 4 months she has been producing a milky discharge from both breasts, and that the flow has been increasing in frequency and quantity. She adds that she has not menstruated for almost 5 months and complains of breast tenderness.
What do Ms. G’s latest symptoms suggest? How will your response to these symptoms affect treatment?
Drs. Yu’s and Maguire’s observations
Complaints of menstrual irregularities, breast tenderness, and galactorrhea should arouse suspicions of hyperprolactinemia. Because tumors that raise prolactin levels are rare, medications are the most likely culprit in Ms. G’s case. Dopamine blockade within the tuberoinfundibular tract is the mechanism of action behind prolactin elevation.4
Prolactin levels in patients with schizophrenia are generally normal (1 to 25 mg/L) prior to treatment,5 but have been known to increase with use of typical antipsychotics. The atypical antipsychotic risperidone has been associated with dose-related increases in plasma prolactin concentration, although Kleinberg et al found no correlation between risperidone-induced plasma prolactin concentrations and adverse events.6
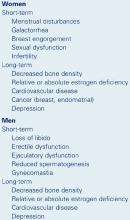
Figure 2 POSSIBLE ADVERSE EFFECTS OF HYPERPROLACTINEMIA8
Prolactin-sparing atypical antipsychotics such as olanzapine, quetiapine, ziprasidone, and aripiprazole may cause a transient prolactin increase in the first few weeks of use. These levels tend to remain within the normal range before decreasing to baseline levels or lower.7,8
Prolactin elevation in women may lead to an estrogen deficiency, causing changes in mood and cognition and psychopathology9 that can manifest as increased depression, anxiety, and hostility.10 Hyperprolactinemia can also cause depression in men, though the mechanism of action is unknown.
Prolactin elevation can lead to numerous other health disturbances (Figure 2). When screening women who are taking antipsychotics, ask about menstrual irregularities, sexual dysfunction, breast tenderness, and galactorrhea. Ask male patients about a loss of libido, erectile dysfunction, ejaculatory dysfunction, and gynecomastia.
When hyperprolactinemia becomes apparent, we suggest discontinuing the offending drug and, if necessary:
- switching to a prolactin-sparing atypical antipsychotic
- or trying another agent, such as bromocriptine or pergolide, if switching to another antipsychotic is infeasible.10,11
Baseline prolactin levels should be measured before starting any prolactin-elevating antipsychotic. Because prolactin levels may not correlate with severity of clinical symptoms, the net change in these levels may be a better indicator.4 If prolactin levels exceed 100 mg/L, consider an MRI with fine cuts though the sellae to check for a primary adenoma.4
Conclusion: A cause is found
An MRI of Ms. G’s head is normal, but her serum prolactin level is 125 μg/L. Her risperidone is tapered off, and olanzapine, 10 mg at bedtime, is started with her mother’s consent. Two days later, her prolactin level drops to 85 μg/L. Notable improvement is reported on day seven of hospitalization; she is sleeping and eating well with no suicidal or homicidal ideations and notes no psychotic symptoms. She is discharged that day.
Two weeks later, Ms. G’s improvement continues. Lab tests reveal normal prolactin levels. Over the next few months, she remains stable, attends school, and takes her medications with no adverse effects.
Related resources
- Maguire GA. Prolactin elevation with antipsychotic medications: mechanisms of action and clinical consequences. J Clin Psychiatry 2002; 63(suppl 4):56-62. Available at: www.psychiatrist.com/supplenet/v63s04/v63s0408.pdf. Accessed March 11, 2003.
Drug brand names
- Aripiprazole • Abilify
- Dextroamphetamine sulfate • Dexadrine
- Divalproex sodium • Depakote
- Fluoxetine • Prozac
- Mestranol • Necon 1/50
- Norethindrone • Activella
- Pergolide • Permax
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Ziprasidone • Geodon
Disclosure
Dr. Yu receives research/grant support from, is a consultant to, and/or is a speaker for Cephalon Inc., Eli Lilly and Co., Novartis Pharmaceuticals Corp., and Pfizer Inc.
Dr. Maguire receives research/grant support from, is a consultant to, and/or is a speaker for Eli Lilly and Co., Pfizer Inc., Forest Laboratories, and GlaxoSmithKline.
1. Bartels SJ, Drake RE. Depressive symptoms in schizophrenia: comprehensive differential diagnosis. Compr Psychiatry 1988;29(5):467-83.
2. Sadock BJ, Sadock VA. Kaplan and Sadock’s comprehensive textbook of psychiatry (7th ed). Philadelphia Lippincott Williams & Wilkins, 2000.
3. Stahl SM. Essential psychopharmacology: neuroscientific basis and practical application (2nd ed). Cambridge, UK: Cambridge University Press, 2000:chap 5.
4. Maguire GA. Prolactin elevation with antipsychotic medications: mechanisms of action and clinical consequences. J Clin Psychiatry 2002;63(suppl 4):56-62.
5. Kuruvilla A, Srikrishna G, Peedicayil J, et al. A study on serum prolactin levels in schizophrenia: correlation with positive and negative symptoms. Int Clin Psychopharmacol 1993;8:177-9.
6. Kleinberg DL, Davis JM, De Coster R, et al. Prolactin levels and adverse events in patients treated with risperidone. J Clin Psychopharmacol 1999;19:57-61.
7. Petty RG. Prolactin and antipsychotic medications: mechanisms of actions. Schizophr Res 1999;35(suppl):S67-S73.
8. Tran PV, Hamilton SH, Kuntz AJ, et al. Double-blind comparison of olanzapine versus risperidone in the treatment of schizophrenia and other psychotic disorders. J Clin Psychopharmacology 1997;17:407-18.
9. Panay N, Studd JW. The psychotherapeutic effects of estrogens. Gynecol Endocrinol 1998;12:353-65.
10. Kellner R, Buckman MT, Fava M, et al. Prolactin, aggression and hostility: a discussion of recent studies. Psychiatry Dev 1984;2:131-8.
11. Pharoah FM, Mari JJ, Streiner D. Family intervention for schizophrenia. Cochrane Database Syst Rev 2000;(2):CD000088.-
12. Weiden PJ, Aquila R, Emanuel M, Zygmunt A. Long-term considerations after switching antipsychotics. J Clin Psychiatry 1998;59(suppl 19):36-49.
13. Goldberg SC, Schooler NR, Hogarty GE, et al. Prediction of relapse in schizophrenic outpatients treated by drug and sociotherapy. Arch Gen Psychiatry 1977;34:171-84.
14. Hogarty GE, Ulrich RF. The limitations of antipsychotic medication on schizophrenia relapse and adjustment and the contributions of psychosocial treatment. J Psychiatr Res 1998;32:243-50.
15. Bellack AS, Gold JM, Buchanan RW. Cognitive rehabilitation for schizophrenia: problems, prospects, and strategies. Schizophr Bull 1999;25:257-75.
16. Siris SG. Assessment and treatment of secondary depression in schizophrenia. Psychiatr Ann 1994;24:463-7.
17. Keck PE, Jr, Strakowski SM, McElroy SL. The efficacy of atypical antipsychotics in the treatment of depressive symptoms, hostility and suicidality in patients with schizophrenia. J Clin Psychiatry 2000;61(suppl 3):4-9.
18. Mattox JH, Buckman MT, Bernstein J, et al. Dopamine agonists for reducing depression associated with hyperprolactinemia. J Reprod Med 1986;31:694-8.
History: Initial symptoms
Ms. G, 17, has battled attention-deficit/hyperactivity disorder (ADHD) since age 6, and within the past 2 years was also diagnosed as having schizoaffective disorder, bipolar type. An outpatient child psychiatrist and a therapist have helped keep her symptoms in control through much of her life.
During one recent visit to her psychiatrist, however, she complained of decreased energy, increased crying spells, broken sleep, and a depressed mood. She reported that these symptoms began approximately 2 months before the visit, and neither she nor her parents could identify a clear-cut cause.
Throughout her life she has complied with her drug regimens. For 2 years she has been taking divalproex sodium, 500 mg twice daily to manage her manic and depressive episodes, dextroamphetamine sulfate, 30 mg in the morning for her ADHD; risperidone, 2 mg at bedtime for her psychotic symptoms; and mestranol, 60 mcg/d, plus norethindrone, 1 mg/d, for contraception. A recent valproic acid reading of 62 μg/ml is consistent with levels over the last 2 years.
During previous psychotic episodes, Ms. G often became delusional and paranoid with command-type hallucinations. She destroyed her room during her most recent episode.
Ms. G’s adoptive mother accompanied her during this visit. She is concerned for her daughter, especially with the start of school about 1 month away.
Which would you address first: the depression or the psychosis? Would you change Ms. G’s medication and if so, how?
Figure 1 DEPRESSION IN SCHIZOPHRENIA: IMPROVING OUTCOMES
Drs. Yu’s and Maguire’s observations
Complaints of depression in a patient with schizoaffective disorder are especially concerning because multiple domains could be affected (Figure 1). For patients with schizophrenia, the 60% lifetime incidence of major depressive disorder substantially exceeds the 8 to 26% risk in the general population. Ms. G’s comorbid depression also may predispose her to an increased rate of relapse into schizoaffective psychosis, poor treatment response, and a longer duration of psychotic illness that could require hospitalization.1
Although Ms. G’s divalproex level was therapeutic (between 50 and 100 μg/ml), some data indicate that valproic acid may be less effective in schizoaffective disorder than in bipolar I disorder. Still, treatment of schizoaffective disorder often follows antimanic and antidepressant protocols.2
Treatment: An agent is added
The outpatient psychiatrist adds fluoxetine, 20 mg each morning, to address Ms. G’s depressive symptoms. She reports no improvement after 1 month, and her fluoxetine is increased to 30 mg/d.
Three weeks later, Ms. G’s parents bring her to the psychiatrist for an emergency visit. She reports suicidal ideation over the previous month. Rolling up both sleeves, she reveals several superficial cuts on her forearms and wrists that she inflicted after breaking up with her boyfriend.
Her mother, appearing anxious and overwhelmed, reports that her daughter pushed her because she had refused to give Ms. G her calling card. She had told her mother that she wanted to call a boy in Utah that she had met over the Internet.
Ms. G’s speech is noticeably pressured and she is extremely distractible. Her mother notes that her daughter is sleeping only 2 to 3 hours a night, yet exhibits no decrease in energy. Still depressed, her affect is markedly labile, crying at one moment when discussing her suicidality, then railing at her mother when she tries to explain Ms. G’s aggressiveness. When the psychiatrist recommends hospitalization to stabilize her symptoms, she vehemently demands to be let out so that she can run in front of a moving car. The police are called, and she is restrained and brought into the hospital.
What caused Ms. G’s sudden decline? How would you address it?
Drs. Yu’s and Maguire’s observations
Although antidepressants can effectively treat depression in schizoaffective disorder, many of these medications can trigger a manic episode,3 which can include mania, mixed mania with depression, or rapid cycling every few days or hours. In Ms. G’s case, an increase in serotonin due to the fluoxetine may have caused her mania.
We would stop the fluoxetine and see if her manic symptoms resolve. Fluoxetine’s long half-life (4 to 16 days) cuts down the odds of a serotonin-discontinuation syndrome, making immediate discontinuation feasible.
Still, the cause of Ms. G’s depressive symptoms remains unknown. At this stage, observation in the adolescent inpatient ward holds our best hope of reaching a definitive diagnosis.
Treatment: A diagnostic clue surfaces
Blood tests on admission (including a negative drug screen for narcotics or other depressogenic substances) are normal, and her valproic acid level is 61 μg/ml. Her divalproex is increased to 500 mg in the morning and 750 mg at bedtime, and she is tapered off fluoxetine. Her symptoms gradually improve with the change in the medications and her attendance in milieu and group therapy on the ward. A second valproic acid reading on day three of hospitalization is 67 μg/ml.
That day, a nurse informs the inpatient child/adolescent psychiatrist that Ms. G has requested extra hospital gowns. Ms. G later reveals that for about 4 months she has been producing a milky discharge from both breasts, and that the flow has been increasing in frequency and quantity. She adds that she has not menstruated for almost 5 months and complains of breast tenderness.
What do Ms. G’s latest symptoms suggest? How will your response to these symptoms affect treatment?
Drs. Yu’s and Maguire’s observations
Complaints of menstrual irregularities, breast tenderness, and galactorrhea should arouse suspicions of hyperprolactinemia. Because tumors that raise prolactin levels are rare, medications are the most likely culprit in Ms. G’s case. Dopamine blockade within the tuberoinfundibular tract is the mechanism of action behind prolactin elevation.4
Prolactin levels in patients with schizophrenia are generally normal (1 to 25 mg/L) prior to treatment,5 but have been known to increase with use of typical antipsychotics. The atypical antipsychotic risperidone has been associated with dose-related increases in plasma prolactin concentration, although Kleinberg et al found no correlation between risperidone-induced plasma prolactin concentrations and adverse events.6
Figure 2 POSSIBLE ADVERSE EFFECTS OF HYPERPROLACTINEMIA8
Prolactin-sparing atypical antipsychotics such as olanzapine, quetiapine, ziprasidone, and aripiprazole may cause a transient prolactin increase in the first few weeks of use. These levels tend to remain within the normal range before decreasing to baseline levels or lower.7,8
Prolactin elevation in women may lead to an estrogen deficiency, causing changes in mood and cognition and psychopathology9 that can manifest as increased depression, anxiety, and hostility.10 Hyperprolactinemia can also cause depression in men, though the mechanism of action is unknown.
Prolactin elevation can lead to numerous other health disturbances (Figure 2). When screening women who are taking antipsychotics, ask about menstrual irregularities, sexual dysfunction, breast tenderness, and galactorrhea. Ask male patients about a loss of libido, erectile dysfunction, ejaculatory dysfunction, and gynecomastia.
When hyperprolactinemia becomes apparent, we suggest discontinuing the offending drug and, if necessary:
- switching to a prolactin-sparing atypical antipsychotic
- or trying another agent, such as bromocriptine or pergolide, if switching to another antipsychotic is infeasible.10,11
Baseline prolactin levels should be measured before starting any prolactin-elevating antipsychotic. Because prolactin levels may not correlate with severity of clinical symptoms, the net change in these levels may be a better indicator.4 If prolactin levels exceed 100 mg/L, consider an MRI with fine cuts though the sellae to check for a primary adenoma.4
Conclusion: A cause is found
An MRI of Ms. G’s head is normal, but her serum prolactin level is 125 μg/L. Her risperidone is tapered off, and olanzapine, 10 mg at bedtime, is started with her mother’s consent. Two days later, her prolactin level drops to 85 μg/L. Notable improvement is reported on day seven of hospitalization; she is sleeping and eating well with no suicidal or homicidal ideations and notes no psychotic symptoms. She is discharged that day.
Two weeks later, Ms. G’s improvement continues. Lab tests reveal normal prolactin levels. Over the next few months, she remains stable, attends school, and takes her medications with no adverse effects.
Related resources
- Maguire GA. Prolactin elevation with antipsychotic medications: mechanisms of action and clinical consequences. J Clin Psychiatry 2002; 63(suppl 4):56-62. Available at: www.psychiatrist.com/supplenet/v63s04/v63s0408.pdf. Accessed March 11, 2003.
Drug brand names
- Aripiprazole • Abilify
- Dextroamphetamine sulfate • Dexadrine
- Divalproex sodium • Depakote
- Fluoxetine • Prozac
- Mestranol • Necon 1/50
- Norethindrone • Activella
- Pergolide • Permax
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Ziprasidone • Geodon
Disclosure
Dr. Yu receives research/grant support from, is a consultant to, and/or is a speaker for Cephalon Inc., Eli Lilly and Co., Novartis Pharmaceuticals Corp., and Pfizer Inc.
Dr. Maguire receives research/grant support from, is a consultant to, and/or is a speaker for Eli Lilly and Co., Pfizer Inc., Forest Laboratories, and GlaxoSmithKline.
History: Initial symptoms
Ms. G, 17, has battled attention-deficit/hyperactivity disorder (ADHD) since age 6, and within the past 2 years was also diagnosed as having schizoaffective disorder, bipolar type. An outpatient child psychiatrist and a therapist have helped keep her symptoms in control through much of her life.
During one recent visit to her psychiatrist, however, she complained of decreased energy, increased crying spells, broken sleep, and a depressed mood. She reported that these symptoms began approximately 2 months before the visit, and neither she nor her parents could identify a clear-cut cause.
Throughout her life she has complied with her drug regimens. For 2 years she has been taking divalproex sodium, 500 mg twice daily to manage her manic and depressive episodes, dextroamphetamine sulfate, 30 mg in the morning for her ADHD; risperidone, 2 mg at bedtime for her psychotic symptoms; and mestranol, 60 mcg/d, plus norethindrone, 1 mg/d, for contraception. A recent valproic acid reading of 62 μg/ml is consistent with levels over the last 2 years.
During previous psychotic episodes, Ms. G often became delusional and paranoid with command-type hallucinations. She destroyed her room during her most recent episode.
Ms. G’s adoptive mother accompanied her during this visit. She is concerned for her daughter, especially with the start of school about 1 month away.
Which would you address first: the depression or the psychosis? Would you change Ms. G’s medication and if so, how?
Figure 1 DEPRESSION IN SCHIZOPHRENIA: IMPROVING OUTCOMES
Drs. Yu’s and Maguire’s observations
Complaints of depression in a patient with schizoaffective disorder are especially concerning because multiple domains could be affected (Figure 1). For patients with schizophrenia, the 60% lifetime incidence of major depressive disorder substantially exceeds the 8 to 26% risk in the general population. Ms. G’s comorbid depression also may predispose her to an increased rate of relapse into schizoaffective psychosis, poor treatment response, and a longer duration of psychotic illness that could require hospitalization.1
Although Ms. G’s divalproex level was therapeutic (between 50 and 100 μg/ml), some data indicate that valproic acid may be less effective in schizoaffective disorder than in bipolar I disorder. Still, treatment of schizoaffective disorder often follows antimanic and antidepressant protocols.2
Treatment: An agent is added
The outpatient psychiatrist adds fluoxetine, 20 mg each morning, to address Ms. G’s depressive symptoms. She reports no improvement after 1 month, and her fluoxetine is increased to 30 mg/d.
Three weeks later, Ms. G’s parents bring her to the psychiatrist for an emergency visit. She reports suicidal ideation over the previous month. Rolling up both sleeves, she reveals several superficial cuts on her forearms and wrists that she inflicted after breaking up with her boyfriend.
Her mother, appearing anxious and overwhelmed, reports that her daughter pushed her because she had refused to give Ms. G her calling card. She had told her mother that she wanted to call a boy in Utah that she had met over the Internet.
Ms. G’s speech is noticeably pressured and she is extremely distractible. Her mother notes that her daughter is sleeping only 2 to 3 hours a night, yet exhibits no decrease in energy. Still depressed, her affect is markedly labile, crying at one moment when discussing her suicidality, then railing at her mother when she tries to explain Ms. G’s aggressiveness. When the psychiatrist recommends hospitalization to stabilize her symptoms, she vehemently demands to be let out so that she can run in front of a moving car. The police are called, and she is restrained and brought into the hospital.
What caused Ms. G’s sudden decline? How would you address it?
Drs. Yu’s and Maguire’s observations
Although antidepressants can effectively treat depression in schizoaffective disorder, many of these medications can trigger a manic episode,3 which can include mania, mixed mania with depression, or rapid cycling every few days or hours. In Ms. G’s case, an increase in serotonin due to the fluoxetine may have caused her mania.
We would stop the fluoxetine and see if her manic symptoms resolve. Fluoxetine’s long half-life (4 to 16 days) cuts down the odds of a serotonin-discontinuation syndrome, making immediate discontinuation feasible.
Still, the cause of Ms. G’s depressive symptoms remains unknown. At this stage, observation in the adolescent inpatient ward holds our best hope of reaching a definitive diagnosis.
Treatment: A diagnostic clue surfaces
Blood tests on admission (including a negative drug screen for narcotics or other depressogenic substances) are normal, and her valproic acid level is 61 μg/ml. Her divalproex is increased to 500 mg in the morning and 750 mg at bedtime, and she is tapered off fluoxetine. Her symptoms gradually improve with the change in the medications and her attendance in milieu and group therapy on the ward. A second valproic acid reading on day three of hospitalization is 67 μg/ml.
That day, a nurse informs the inpatient child/adolescent psychiatrist that Ms. G has requested extra hospital gowns. Ms. G later reveals that for about 4 months she has been producing a milky discharge from both breasts, and that the flow has been increasing in frequency and quantity. She adds that she has not menstruated for almost 5 months and complains of breast tenderness.
What do Ms. G’s latest symptoms suggest? How will your response to these symptoms affect treatment?
Drs. Yu’s and Maguire’s observations
Complaints of menstrual irregularities, breast tenderness, and galactorrhea should arouse suspicions of hyperprolactinemia. Because tumors that raise prolactin levels are rare, medications are the most likely culprit in Ms. G’s case. Dopamine blockade within the tuberoinfundibular tract is the mechanism of action behind prolactin elevation.4
Prolactin levels in patients with schizophrenia are generally normal (1 to 25 mg/L) prior to treatment,5 but have been known to increase with use of typical antipsychotics. The atypical antipsychotic risperidone has been associated with dose-related increases in plasma prolactin concentration, although Kleinberg et al found no correlation between risperidone-induced plasma prolactin concentrations and adverse events.6
Figure 2 POSSIBLE ADVERSE EFFECTS OF HYPERPROLACTINEMIA8
Prolactin-sparing atypical antipsychotics such as olanzapine, quetiapine, ziprasidone, and aripiprazole may cause a transient prolactin increase in the first few weeks of use. These levels tend to remain within the normal range before decreasing to baseline levels or lower.7,8
Prolactin elevation in women may lead to an estrogen deficiency, causing changes in mood and cognition and psychopathology9 that can manifest as increased depression, anxiety, and hostility.10 Hyperprolactinemia can also cause depression in men, though the mechanism of action is unknown.
Prolactin elevation can lead to numerous other health disturbances (Figure 2). When screening women who are taking antipsychotics, ask about menstrual irregularities, sexual dysfunction, breast tenderness, and galactorrhea. Ask male patients about a loss of libido, erectile dysfunction, ejaculatory dysfunction, and gynecomastia.
When hyperprolactinemia becomes apparent, we suggest discontinuing the offending drug and, if necessary:
- switching to a prolactin-sparing atypical antipsychotic
- or trying another agent, such as bromocriptine or pergolide, if switching to another antipsychotic is infeasible.10,11
Baseline prolactin levels should be measured before starting any prolactin-elevating antipsychotic. Because prolactin levels may not correlate with severity of clinical symptoms, the net change in these levels may be a better indicator.4 If prolactin levels exceed 100 mg/L, consider an MRI with fine cuts though the sellae to check for a primary adenoma.4
Conclusion: A cause is found
An MRI of Ms. G’s head is normal, but her serum prolactin level is 125 μg/L. Her risperidone is tapered off, and olanzapine, 10 mg at bedtime, is started with her mother’s consent. Two days later, her prolactin level drops to 85 μg/L. Notable improvement is reported on day seven of hospitalization; she is sleeping and eating well with no suicidal or homicidal ideations and notes no psychotic symptoms. She is discharged that day.
Two weeks later, Ms. G’s improvement continues. Lab tests reveal normal prolactin levels. Over the next few months, she remains stable, attends school, and takes her medications with no adverse effects.
Related resources
- Maguire GA. Prolactin elevation with antipsychotic medications: mechanisms of action and clinical consequences. J Clin Psychiatry 2002; 63(suppl 4):56-62. Available at: www.psychiatrist.com/supplenet/v63s04/v63s0408.pdf. Accessed March 11, 2003.
Drug brand names
- Aripiprazole • Abilify
- Dextroamphetamine sulfate • Dexadrine
- Divalproex sodium • Depakote
- Fluoxetine • Prozac
- Mestranol • Necon 1/50
- Norethindrone • Activella
- Pergolide • Permax
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Ziprasidone • Geodon
Disclosure
Dr. Yu receives research/grant support from, is a consultant to, and/or is a speaker for Cephalon Inc., Eli Lilly and Co., Novartis Pharmaceuticals Corp., and Pfizer Inc.
Dr. Maguire receives research/grant support from, is a consultant to, and/or is a speaker for Eli Lilly and Co., Pfizer Inc., Forest Laboratories, and GlaxoSmithKline.
1. Bartels SJ, Drake RE. Depressive symptoms in schizophrenia: comprehensive differential diagnosis. Compr Psychiatry 1988;29(5):467-83.
2. Sadock BJ, Sadock VA. Kaplan and Sadock’s comprehensive textbook of psychiatry (7th ed). Philadelphia Lippincott Williams & Wilkins, 2000.
3. Stahl SM. Essential psychopharmacology: neuroscientific basis and practical application (2nd ed). Cambridge, UK: Cambridge University Press, 2000:chap 5.
4. Maguire GA. Prolactin elevation with antipsychotic medications: mechanisms of action and clinical consequences. J Clin Psychiatry 2002;63(suppl 4):56-62.
5. Kuruvilla A, Srikrishna G, Peedicayil J, et al. A study on serum prolactin levels in schizophrenia: correlation with positive and negative symptoms. Int Clin Psychopharmacol 1993;8:177-9.
6. Kleinberg DL, Davis JM, De Coster R, et al. Prolactin levels and adverse events in patients treated with risperidone. J Clin Psychopharmacol 1999;19:57-61.
7. Petty RG. Prolactin and antipsychotic medications: mechanisms of actions. Schizophr Res 1999;35(suppl):S67-S73.
8. Tran PV, Hamilton SH, Kuntz AJ, et al. Double-blind comparison of olanzapine versus risperidone in the treatment of schizophrenia and other psychotic disorders. J Clin Psychopharmacology 1997;17:407-18.
9. Panay N, Studd JW. The psychotherapeutic effects of estrogens. Gynecol Endocrinol 1998;12:353-65.
10. Kellner R, Buckman MT, Fava M, et al. Prolactin, aggression and hostility: a discussion of recent studies. Psychiatry Dev 1984;2:131-8.
11. Pharoah FM, Mari JJ, Streiner D. Family intervention for schizophrenia. Cochrane Database Syst Rev 2000;(2):CD000088.-
12. Weiden PJ, Aquila R, Emanuel M, Zygmunt A. Long-term considerations after switching antipsychotics. J Clin Psychiatry 1998;59(suppl 19):36-49.
13. Goldberg SC, Schooler NR, Hogarty GE, et al. Prediction of relapse in schizophrenic outpatients treated by drug and sociotherapy. Arch Gen Psychiatry 1977;34:171-84.
14. Hogarty GE, Ulrich RF. The limitations of antipsychotic medication on schizophrenia relapse and adjustment and the contributions of psychosocial treatment. J Psychiatr Res 1998;32:243-50.
15. Bellack AS, Gold JM, Buchanan RW. Cognitive rehabilitation for schizophrenia: problems, prospects, and strategies. Schizophr Bull 1999;25:257-75.
16. Siris SG. Assessment and treatment of secondary depression in schizophrenia. Psychiatr Ann 1994;24:463-7.
17. Keck PE, Jr, Strakowski SM, McElroy SL. The efficacy of atypical antipsychotics in the treatment of depressive symptoms, hostility and suicidality in patients with schizophrenia. J Clin Psychiatry 2000;61(suppl 3):4-9.
18. Mattox JH, Buckman MT, Bernstein J, et al. Dopamine agonists for reducing depression associated with hyperprolactinemia. J Reprod Med 1986;31:694-8.
1. Bartels SJ, Drake RE. Depressive symptoms in schizophrenia: comprehensive differential diagnosis. Compr Psychiatry 1988;29(5):467-83.
2. Sadock BJ, Sadock VA. Kaplan and Sadock’s comprehensive textbook of psychiatry (7th ed). Philadelphia Lippincott Williams & Wilkins, 2000.
3. Stahl SM. Essential psychopharmacology: neuroscientific basis and practical application (2nd ed). Cambridge, UK: Cambridge University Press, 2000:chap 5.
4. Maguire GA. Prolactin elevation with antipsychotic medications: mechanisms of action and clinical consequences. J Clin Psychiatry 2002;63(suppl 4):56-62.
5. Kuruvilla A, Srikrishna G, Peedicayil J, et al. A study on serum prolactin levels in schizophrenia: correlation with positive and negative symptoms. Int Clin Psychopharmacol 1993;8:177-9.
6. Kleinberg DL, Davis JM, De Coster R, et al. Prolactin levels and adverse events in patients treated with risperidone. J Clin Psychopharmacol 1999;19:57-61.
7. Petty RG. Prolactin and antipsychotic medications: mechanisms of actions. Schizophr Res 1999;35(suppl):S67-S73.
8. Tran PV, Hamilton SH, Kuntz AJ, et al. Double-blind comparison of olanzapine versus risperidone in the treatment of schizophrenia and other psychotic disorders. J Clin Psychopharmacology 1997;17:407-18.
9. Panay N, Studd JW. The psychotherapeutic effects of estrogens. Gynecol Endocrinol 1998;12:353-65.
10. Kellner R, Buckman MT, Fava M, et al. Prolactin, aggression and hostility: a discussion of recent studies. Psychiatry Dev 1984;2:131-8.
11. Pharoah FM, Mari JJ, Streiner D. Family intervention for schizophrenia. Cochrane Database Syst Rev 2000;(2):CD000088.-
12. Weiden PJ, Aquila R, Emanuel M, Zygmunt A. Long-term considerations after switching antipsychotics. J Clin Psychiatry 1998;59(suppl 19):36-49.
13. Goldberg SC, Schooler NR, Hogarty GE, et al. Prediction of relapse in schizophrenic outpatients treated by drug and sociotherapy. Arch Gen Psychiatry 1977;34:171-84.
14. Hogarty GE, Ulrich RF. The limitations of antipsychotic medication on schizophrenia relapse and adjustment and the contributions of psychosocial treatment. J Psychiatr Res 1998;32:243-50.
15. Bellack AS, Gold JM, Buchanan RW. Cognitive rehabilitation for schizophrenia: problems, prospects, and strategies. Schizophr Bull 1999;25:257-75.
16. Siris SG. Assessment and treatment of secondary depression in schizophrenia. Psychiatr Ann 1994;24:463-7.
17. Keck PE, Jr, Strakowski SM, McElroy SL. The efficacy of atypical antipsychotics in the treatment of depressive symptoms, hostility and suicidality in patients with schizophrenia. J Clin Psychiatry 2000;61(suppl 3):4-9.
18. Mattox JH, Buckman MT, Bernstein J, et al. Dopamine agonists for reducing depression associated with hyperprolactinemia. J Reprod Med 1986;31:694-8.
New therapies can help patients who stŭťtər
Despite its prevalence, stuttering has not received as much attention as other psychiatric disorders from patients or psychiatrists—with good reason. Until recently, little was known about the neurophysiology of stuttering, and treatment was generally ineffective especially in adults (Box 1). Despite their own personal struggles with the disorder, patients have questioned the need for psychiatric treatment.
That has now changed. We know now that stuttering is likely a disorder of brain chemistry. Studies suggests that olanzapine, a novel dopamine antagonist, is a useful, well-tolerated medication for the treatment of stuttering. As a result, psychiatrists are now equipped to play an important role in its management.
Furthermore, we can give patients the therapeutic opportunity to discuss what often has been a lifetime of frustration with stuttering. We can enable them to understand the course and treatment of this disorder and encourage them to take advantage of the opportunities to lessen the symptoms of stuttering and, ultimately, improve their quality of life.
How stuttering develops
Stuttering is a speech disorder characterized by frequent prolongations, repetitions, or blocks of spoken sounds and/or syllables. A common disorder affecting 1% of adults and 4% of children, stuttering is classified in DSM-IV as an Axis I disorder (Box 2).1
Stuttering has occurred throughout history, with descriptions from the ancient Egyptians and Greeks. For centuries, theories on its etiology involved abnormalities in the tongue or larynx, and the treatments addressed such ideology. Even today, some stuttering treatments involve such archaic methods as cauterizing or cutting the tongue. Treatments focused on the tongue or larynx have not demonstrated consistent efficacy.
The pioneering work of Orton21 and Travis22 signaled a significant change in the understanding of stuttering. They postulated that stuttering may arise from abnormal cerebral activity, signaling a significant change in the theories of the etiology of stuttering. Unfortunately, stuttering treatments did not reflect this new understanding until fairly recently.
Psychoanalytic theorists believed that stuttering arose from the individual’s attempt to fulfill some type of unconscious neurotic need, usually resulting from disturbed early parent-child interaction.23 Psychoanalytic therapy was largely ineffective, however.
Most stuttering treatment practiced today involves speech therapy utilizing cognitive and behavioral methods. Such methods are often limited in their efficacy, especially in adults.24 Some forms of therapy involving speech motor training have been shown effective in young children while the brain is still in development.25 The pharmacologic treatment of stuttering is not widespread today, but new and recent research identifying certain cerebral abnormalities is providing clues for pharmacologic interventions.
Stuttering usually begins in childhood and is likely a developmental disorder. Rare cases of acquired stuttering begin in adulthood but are related to secondary causes such as medications, brain trauma, or stroke.3 Some 80% to 90% of developmental stuttering begins by age 6; onset after age 9 is likely to have some psychogenic or neurogenic basis.4 In approximately 60% of the children who stutter, the symptoms will remit by age 16. Children who stutter require early intervention, given the importance of communication in a child’s development.5
Stuttering shares many similarities with Tourette syndrome. Both begin in childhood, follow a waxing or waning course, have a 4:1 male-to-female ratio, are made worse by anxiety, involve abnormalities in the basal ganglia, and respond to dopamine antagonist therapy.6 Persons who stutter often exhibit tic motions, similar to those seen in Tourette syndrome, which are associated with the struggles to produce speech. Genetic studies have shown possible high additive genetic effects; pair-wise concordance for stuttering was significantly higher in identical twins (63%) than it was in fraternal same-sex twins (19%).7,8 Researchers are investigating potential molecular genetic markers for stuttering.
Functional brain imaging studies suggest that stuttering is associated with abnormal cerebral activation primarily involving abnormally low metabolism of the cortical speech areas and the striatum. The defects in stuttering occur primarily in the timing and initiation of spontaneous speech, with such tasks as singing and reading in chorus being spared. A clue to understanding stuttering lies with these “induced fluency” tasks.
Functional positron emission tomography studies utilizing18 F-deoxyglucose showed that stuttering is associated with abnormally low metabolism of speech cortical areas (Wernicke’s and Broca’s) and low metabolism of the basal ganglia, notably the striatum. During the induced fluency, Wernicke’s and Broca’s areas normalize but the striatum remains abnormally low.
Riley postulates two “loops” of speech, an inner or medial system and an outer or lateral system.9 The lateral system is preserved in stuttering and can be activated through singing, rhythmic speech, etc., but the inner loop, as mediated by the striatum and influenced by dopamine, remains impaired. Once a person who stutters initiates speech, he or she often avoids taking a breath as the whole system must again be jump-started. The low striatal metabolism may be the common-state phenomenon underlying this timing.
- Disturbance in normal fluency and time patterning of speech (inappropriate for the individual’s age), characterized by frequent occurrences of one or more of the following:
- Sound and syllable repetitions
- Sound prolongations
- Interjections
- Broken words (e.g., pauses within a word)
- Audible or silent blocking (filled or unfilled pauses in speech)
- Circumlocutions (word substitutions to avoid problematic words)
- Words produced with an excess of physical tension
- Monosyllabic whole-word repetitions (e.g., “I-I-I-I see him”)
- Sound and syllable repetitions
- The disturbance in fluency interferes with academic or occupational achievement or with social communications
- If a speech-motor or sensory deficit is present, the speech difficulties are in excess of those usually associated with these problems.
Coding note: If a speech-motor or sensory deficit or a neurological condition is present, code the condition on Axis III.
The dopamine hypothesis of stuttering
Stuttering is likely related to abnormal elevations of cerebral dopamine activity. Stimulant medications, which increase dopamine activity, have been shown to increase stuttering symptoms.10 As will be reviewed later, dopamine antagonist medications have been shown to improve the symptoms of stuttering. Also, the striatal hypometabolism in stuttering seen in PET imaging may be a result of a hyperdopaminergic state.
To investigate this dopamine hypothesis of stuttering, Wu et al measured presynaptic dopamine levels in individuals who stutter.11 These were found to have 50% to 200% higher levels of dopamine activity than did the controls. Dopamine is inhibitory to striatal metabolism, providing an explanation for the striatal hypometabolism seen in stuttering. Also, risperidone was found to increase striatal metabolism in those whose stuttering improved on this medication.12
Evaluating the patient
One should begin with a comprehensive psychiatric history. Because many patients began stuttering in childhood and have had difficulty dealing with their disorder, other psychiatric disorders such as social phobia may be present. Moreover, other medical etiologies (e.g., stroke) may cause a speech disorder that resembles stuttering.
Stuttering involves abnormalities in fluency as well as tic motions and cognitive avoidances. Inquiries should be made as to the patient’s fluency of speech during work, during introductions, speaking in front of an audience, with family, etc.; the level of stuttering can vary depending on the particular environment.
Stuttering fluency can be rated through an objective scale known as the Riley SSI-3.13 This scale measures the duration of each stuttering event, the percentage of syllables stuttered versus syllables spoken, the severity of associated tic motions, and a global score of the aforementioned components. Because most psychiatrists cannot routinely perform this scale to assess the patient’s progress, it is best to partner with a speech-language pathologist who can also assist the patient through speech therapy.
Nonetheless, you may assess the progress of treatment by relying on your own “ear,” the patient’s own assessment, and the input of a significant other or family member.
In addition to considering DSM-IV criteria, comprehensive treatment should address all aspects of this disorder, including not only the fluency enhancement but improvement in social avoidances and cognitive restructuring. Be aware that stuttering waxes and wanes over time. You should expect to see some “dips” in efficacy during the course of therapy. A longitudinal assessment over several months is needed to determine if the stuttering treatment is efficacious.
What we’ve learned about drug therapy
Many medications have been tried to treat stuttering but few have shown efficacy in well-controlled trials. Most pharmacologic studies did not include a placebo control or employ objective measures of stuttering severity, nor did they provide multiple baseline and treatment measures.
The critical new knowledge is this: Medications that lower dopamine activity have shown replicated efficacy in improving stuttering. The benzodiazepines have been shown to reduce anxiety short-term but have not been shown to improve fluency in stuttering. Limited studies of serotonergic antidepressants suggest a possible role in reducing the social anxiety of stuttering but have not been shown in well-controlled trials to improve stuttering fluency directly.
Multiple studies of haloperidol in the 1970s showed that this medication improved fluency in individuals who stutter. Long-term compliance with this medication, however, was poor given its dysphoric side effects, sexual dysfunction, extrapyramidal concerns, and risks of tardive dyskinesia. Limited research with calcium-channel-blocking medications (e.g., verapamil, nimodipine) showed limited efficacy in stuttering.14,15 Calcium-channel blockers, however, may exert a mild antidopamine effect.
Further supporting dopamine hyperactivity in the pathology of stuttering, Stager et al compared pimozide (n = 6), a selective dopamine (D2) antagonist, paroxetine (n = 5), a highly selective serotonin reuptake inhibitor, and placebo (n = 6). The researchers found a positive clinical response in those on pimozide compared with those taking placebo, whereas the paroxetine group exhibited no clinical response.16 Although small, such a study supports the hypothesis that dopamine may be a principal transmitter involved in stuttering pathology, and serotonin may play a minor role, if any.
Risperidone, a newer-generation dopamine antagonist with a side-effect profile more favorable than haloperidol, has been shown in a well-controlled, double-blind, placebo-controlled study to improve stuttering symptoms (0.5 mg to 2 mg/d). Although generally well tolerated, long-term compliance was hindered by prolactin-related side effects such as sexual dysfunction, galactorrhea, amenorrhea, and dysphoria.17 Dysphoria with risperidone has also recently been reported to occur with its use in Tourette disorder.18
Olanzapine is a novel psychotropic medication that possesses dopamine-blocking qualities but is not associated as much with prolactin-related side effects or dysphoria. A preliminary open-label study suggests that it too improves the symptoms of stuttering.19
A multicenter study of olanzapine in the treatment of adult developmental stuttering involved 23 adults in a 3-month, double-blind, placebo-controlled trial preceded by a 1-month baseline rating period. At the end of the double-blind phase, subjects were followed for 1 year. Olanzapine (2.5 mg titrated to 5 mg/d) was shown to exert a statistically significant improvement over placebo in multiple objective measures of stuttering severity. The medication was well tolerated without prolactin-associated side effects. Concerns of appetite increase and weight gain with olanzapine were minimized through simple education. The average weight gain was 4 lb in the treatment group, compared with 1 lb in the placebo group. Compliance was also high. All subjects elected to enter the open-label phase of the protocol.
In many patients in the study, stuttering symptoms have continued to improve over 6 months to 1 year or even longer, suggesting that an adequate treatment trial should be measured not in days or even weeks, but possibly months. Also, some individuals in the open-label phase have shown even further efficacy with dose escalation to 7.5 mg to 10 mg/d or higher of olanzapine.20
It is likely, however, that pharmacologic treatment will not be the total answer. In the studies cited earlier, the novel dopamine antagonists led to significant—yet only partial—reductions in stuttering symptoms. The future of optimal stuttering treatment will likely involve the active collaboration between a speech language pathologist and a psychiatrist, using speech therapy to enhance the positive benefits of the medication.
Related resources
- National Stuttering Association http://www.nsastutter.org
- University of California-Irvine Medical Center: Facts About Stuttering. http://www.ucihealth.com/News/UCI%20Health/stutter2.htm
- Hulstijn W, Peters HFM, Van Lieshout PHHM, eds. Speech Production: Motor Control, Brain Research and Fluency Disorders. International Congress Series 1146. Amsterdam, Netherlands: Excerpta Medica, 1997.
- Haloperidol • Haldol
- Nimodipine • Nimotop
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Pimozide • Orap
- Risperidone • Risperdal
Drs. Maguire and Franklin report that they receive grant/research support from, serve as consultants to, and are on the speaker’s bureau of Eli Lilly &Co.
Dr. Maguire also reports that he receives grant/research support from Johnson & Johnson, and serves on the speaker’s bureau of Pfizer Inc. and GlaxoSmithKline.
Dr. Yu reports that he serves on the speaker’s bureau of Cephalon Inc.
Drs. Riley and Ortiz report no financial relationship with any company whose products are mentioned in this article.
1. American Psychiatric Association. DSM-IV-R. Washington, DC: American Psychiatric Association, 2000.
2. Maguire GA, Riley GD, Franklin DL, Wu JC, et al. The dopamine hypothesis of stuttering and its treatment implications. Intern J Neuropsychopharmacology 2000;3(1):
3. Ludlow CL, Dooman AG. Genetic aspects of idiopathic speech and language disorders. Otolaryngol Clin N Am 1992;25(5):979-94.
4. Manning WH. Clinical decision making in fluency disorders. 2nd ed. San Diego, Calif: Singular, 2001;107-8.
5. Riley G, Ingham J. Acoustic duration changes associated with two types of treatment for children who stutter. J Speech Language Hearing 2000;43:965-78.
6. Wu JC, Maguire GA, et al. A positron emission tomography [18F] deoxyglucose study of developmental stuttering. Neuroreport 1995;6:501-5.
7. Felsenfeld S, Kirk KM, Zhu G, et al. A study of the genetic and environmental etiology of stuttering in a selected twin sample. Behav Gen 2000;30(5):359-66.
8. Howie PM. Concordance for stuttering in monozygotic and dizygotic twin pairs. J Speech Hearing Research 1981;24(3):317-21.
9. Riley GD, Wu JC, Maguire GA. Pet scan evidence of parallel cerebral systems related to treatment effects. In Hulstijn W, Peters HFM, Van Lieshout PHHM (eds.), Speech Production: Motor Control, Brain Research and Fluency Disorders. Amsterdam: Excerpta Medica, 1997.
10. Burd, Kerbeshian J. Stuttering and stimulants [letter]. J Clin Psychopharmacology 1991;11(1):72-3.
11. Wu JC, Maguire G, Riley G, et al. Increased dopamine activity associated with stuttering. Neuroreport 1997;8(3):767-70.
12. Maguire GA. The Dopamine Hypothesis of Stuttering and its Treatment Implications. Presented at Collegium Internationale Neuro-Psychopharmacologicum. Brussels, Belgium, July 2000.
13. Riley G. Stuttering Severity Instrument. 3rd ed. Austin, Tex: ProEd, 1994.
14. Brady JP, McAllister TW, Price TR. Verapamil in stuttering [letter]. Biol Psychiatry 1990;27(6):680-1.
15. Maguire G, Riley G, Hahn R, Plon L. Nimodipine in the treatment of stuttering. ASHA Journal 1994;36:51.-
16. Stager S, Calis K, Grothe D, et al. A double-blind trial of pimozide and paroxetine for stuttering. In: Hulstijn W, Peters HRM, van Lieshout PHHM, eds. Speech Production: Motor Control, Brain Research and Fluency Disorders. International Congress Series 1146. Amsterdam: Excerpta Medica, 1997;379-82.
17. Maguire GA, Riley GD, Franklin DL, Gottshalk LA. Risperidone for the Treatment of Stuttering. J Clin Psychopharmacology 2000-20:479-82.
18. Margolese HC, Annabel L, Dion Y. Depression and dysphoria in adult and adolescent patients with Tourette syndrome treated with risperidone. Presented at the American College of Neuropsychopharmacology, Waikoloa, Hawaii Dec. 10, 2001.
19. Lavid N, Franklin DL, Maguire GA. Management of Child and Adolescent Stuttering with Olanzapine: Three Case Reports. Ann Clin Psychiatry 1999;11(4):233-36.
20. Maguire GA, et al. Olanzapine in the Treatment of Adult Developmental Stuttering. Presented at the American College of Neuropsychopharmacology, Waikoloa, Hawaii Dec. 10, 2001.
21. Orton ST. Studies in stuttering. Arch Neurology Psychiatry 1927;18:671-2.
22. Travis LE. Speech Pathology. New York: Appleton-Century-Crofts, 1931.
23. Sadock BJ, Sadock VA. Kaplan and Sadock’s Comprehensive Textbook of Psychiatry. 7th ed. Baltimore, Md: Lippincott Williams & Wilkins, 2000.
24. Manning WH. Clinical Decision Making in Fluency Disorders. 2nd ed. San Diego, Calif: Singular Publishing, 2001;311-14.
25. Riley G, Ingham J. Acoustic duration changes associated with two types of treatment for children who stutter. J Speech Language Hearing 2000;43:965-78.
Despite its prevalence, stuttering has not received as much attention as other psychiatric disorders from patients or psychiatrists—with good reason. Until recently, little was known about the neurophysiology of stuttering, and treatment was generally ineffective especially in adults (Box 1). Despite their own personal struggles with the disorder, patients have questioned the need for psychiatric treatment.
That has now changed. We know now that stuttering is likely a disorder of brain chemistry. Studies suggests that olanzapine, a novel dopamine antagonist, is a useful, well-tolerated medication for the treatment of stuttering. As a result, psychiatrists are now equipped to play an important role in its management.
Furthermore, we can give patients the therapeutic opportunity to discuss what often has been a lifetime of frustration with stuttering. We can enable them to understand the course and treatment of this disorder and encourage them to take advantage of the opportunities to lessen the symptoms of stuttering and, ultimately, improve their quality of life.
How stuttering develops
Stuttering is a speech disorder characterized by frequent prolongations, repetitions, or blocks of spoken sounds and/or syllables. A common disorder affecting 1% of adults and 4% of children, stuttering is classified in DSM-IV as an Axis I disorder (Box 2).1
Stuttering has occurred throughout history, with descriptions from the ancient Egyptians and Greeks. For centuries, theories on its etiology involved abnormalities in the tongue or larynx, and the treatments addressed such ideology. Even today, some stuttering treatments involve such archaic methods as cauterizing or cutting the tongue. Treatments focused on the tongue or larynx have not demonstrated consistent efficacy.
The pioneering work of Orton21 and Travis22 signaled a significant change in the understanding of stuttering. They postulated that stuttering may arise from abnormal cerebral activity, signaling a significant change in the theories of the etiology of stuttering. Unfortunately, stuttering treatments did not reflect this new understanding until fairly recently.
Psychoanalytic theorists believed that stuttering arose from the individual’s attempt to fulfill some type of unconscious neurotic need, usually resulting from disturbed early parent-child interaction.23 Psychoanalytic therapy was largely ineffective, however.
Most stuttering treatment practiced today involves speech therapy utilizing cognitive and behavioral methods. Such methods are often limited in their efficacy, especially in adults.24 Some forms of therapy involving speech motor training have been shown effective in young children while the brain is still in development.25 The pharmacologic treatment of stuttering is not widespread today, but new and recent research identifying certain cerebral abnormalities is providing clues for pharmacologic interventions.
Stuttering usually begins in childhood and is likely a developmental disorder. Rare cases of acquired stuttering begin in adulthood but are related to secondary causes such as medications, brain trauma, or stroke.3 Some 80% to 90% of developmental stuttering begins by age 6; onset after age 9 is likely to have some psychogenic or neurogenic basis.4 In approximately 60% of the children who stutter, the symptoms will remit by age 16. Children who stutter require early intervention, given the importance of communication in a child’s development.5
Stuttering shares many similarities with Tourette syndrome. Both begin in childhood, follow a waxing or waning course, have a 4:1 male-to-female ratio, are made worse by anxiety, involve abnormalities in the basal ganglia, and respond to dopamine antagonist therapy.6 Persons who stutter often exhibit tic motions, similar to those seen in Tourette syndrome, which are associated with the struggles to produce speech. Genetic studies have shown possible high additive genetic effects; pair-wise concordance for stuttering was significantly higher in identical twins (63%) than it was in fraternal same-sex twins (19%).7,8 Researchers are investigating potential molecular genetic markers for stuttering.
Functional brain imaging studies suggest that stuttering is associated with abnormal cerebral activation primarily involving abnormally low metabolism of the cortical speech areas and the striatum. The defects in stuttering occur primarily in the timing and initiation of spontaneous speech, with such tasks as singing and reading in chorus being spared. A clue to understanding stuttering lies with these “induced fluency” tasks.
Functional positron emission tomography studies utilizing18 F-deoxyglucose showed that stuttering is associated with abnormally low metabolism of speech cortical areas (Wernicke’s and Broca’s) and low metabolism of the basal ganglia, notably the striatum. During the induced fluency, Wernicke’s and Broca’s areas normalize but the striatum remains abnormally low.
Riley postulates two “loops” of speech, an inner or medial system and an outer or lateral system.9 The lateral system is preserved in stuttering and can be activated through singing, rhythmic speech, etc., but the inner loop, as mediated by the striatum and influenced by dopamine, remains impaired. Once a person who stutters initiates speech, he or she often avoids taking a breath as the whole system must again be jump-started. The low striatal metabolism may be the common-state phenomenon underlying this timing.
- Disturbance in normal fluency and time patterning of speech (inappropriate for the individual’s age), characterized by frequent occurrences of one or more of the following:
- Sound and syllable repetitions
- Sound prolongations
- Interjections
- Broken words (e.g., pauses within a word)
- Audible or silent blocking (filled or unfilled pauses in speech)
- Circumlocutions (word substitutions to avoid problematic words)
- Words produced with an excess of physical tension
- Monosyllabic whole-word repetitions (e.g., “I-I-I-I see him”)
- Sound and syllable repetitions
- The disturbance in fluency interferes with academic or occupational achievement or with social communications
- If a speech-motor or sensory deficit is present, the speech difficulties are in excess of those usually associated with these problems.
Coding note: If a speech-motor or sensory deficit or a neurological condition is present, code the condition on Axis III.
The dopamine hypothesis of stuttering
Stuttering is likely related to abnormal elevations of cerebral dopamine activity. Stimulant medications, which increase dopamine activity, have been shown to increase stuttering symptoms.10 As will be reviewed later, dopamine antagonist medications have been shown to improve the symptoms of stuttering. Also, the striatal hypometabolism in stuttering seen in PET imaging may be a result of a hyperdopaminergic state.
To investigate this dopamine hypothesis of stuttering, Wu et al measured presynaptic dopamine levels in individuals who stutter.11 These were found to have 50% to 200% higher levels of dopamine activity than did the controls. Dopamine is inhibitory to striatal metabolism, providing an explanation for the striatal hypometabolism seen in stuttering. Also, risperidone was found to increase striatal metabolism in those whose stuttering improved on this medication.12
Evaluating the patient
One should begin with a comprehensive psychiatric history. Because many patients began stuttering in childhood and have had difficulty dealing with their disorder, other psychiatric disorders such as social phobia may be present. Moreover, other medical etiologies (e.g., stroke) may cause a speech disorder that resembles stuttering.
Stuttering involves abnormalities in fluency as well as tic motions and cognitive avoidances. Inquiries should be made as to the patient’s fluency of speech during work, during introductions, speaking in front of an audience, with family, etc.; the level of stuttering can vary depending on the particular environment.
Stuttering fluency can be rated through an objective scale known as the Riley SSI-3.13 This scale measures the duration of each stuttering event, the percentage of syllables stuttered versus syllables spoken, the severity of associated tic motions, and a global score of the aforementioned components. Because most psychiatrists cannot routinely perform this scale to assess the patient’s progress, it is best to partner with a speech-language pathologist who can also assist the patient through speech therapy.
Nonetheless, you may assess the progress of treatment by relying on your own “ear,” the patient’s own assessment, and the input of a significant other or family member.
In addition to considering DSM-IV criteria, comprehensive treatment should address all aspects of this disorder, including not only the fluency enhancement but improvement in social avoidances and cognitive restructuring. Be aware that stuttering waxes and wanes over time. You should expect to see some “dips” in efficacy during the course of therapy. A longitudinal assessment over several months is needed to determine if the stuttering treatment is efficacious.
What we’ve learned about drug therapy
Many medications have been tried to treat stuttering but few have shown efficacy in well-controlled trials. Most pharmacologic studies did not include a placebo control or employ objective measures of stuttering severity, nor did they provide multiple baseline and treatment measures.
The critical new knowledge is this: Medications that lower dopamine activity have shown replicated efficacy in improving stuttering. The benzodiazepines have been shown to reduce anxiety short-term but have not been shown to improve fluency in stuttering. Limited studies of serotonergic antidepressants suggest a possible role in reducing the social anxiety of stuttering but have not been shown in well-controlled trials to improve stuttering fluency directly.
Multiple studies of haloperidol in the 1970s showed that this medication improved fluency in individuals who stutter. Long-term compliance with this medication, however, was poor given its dysphoric side effects, sexual dysfunction, extrapyramidal concerns, and risks of tardive dyskinesia. Limited research with calcium-channel-blocking medications (e.g., verapamil, nimodipine) showed limited efficacy in stuttering.14,15 Calcium-channel blockers, however, may exert a mild antidopamine effect.
Further supporting dopamine hyperactivity in the pathology of stuttering, Stager et al compared pimozide (n = 6), a selective dopamine (D2) antagonist, paroxetine (n = 5), a highly selective serotonin reuptake inhibitor, and placebo (n = 6). The researchers found a positive clinical response in those on pimozide compared with those taking placebo, whereas the paroxetine group exhibited no clinical response.16 Although small, such a study supports the hypothesis that dopamine may be a principal transmitter involved in stuttering pathology, and serotonin may play a minor role, if any.
Risperidone, a newer-generation dopamine antagonist with a side-effect profile more favorable than haloperidol, has been shown in a well-controlled, double-blind, placebo-controlled study to improve stuttering symptoms (0.5 mg to 2 mg/d). Although generally well tolerated, long-term compliance was hindered by prolactin-related side effects such as sexual dysfunction, galactorrhea, amenorrhea, and dysphoria.17 Dysphoria with risperidone has also recently been reported to occur with its use in Tourette disorder.18
Olanzapine is a novel psychotropic medication that possesses dopamine-blocking qualities but is not associated as much with prolactin-related side effects or dysphoria. A preliminary open-label study suggests that it too improves the symptoms of stuttering.19
A multicenter study of olanzapine in the treatment of adult developmental stuttering involved 23 adults in a 3-month, double-blind, placebo-controlled trial preceded by a 1-month baseline rating period. At the end of the double-blind phase, subjects were followed for 1 year. Olanzapine (2.5 mg titrated to 5 mg/d) was shown to exert a statistically significant improvement over placebo in multiple objective measures of stuttering severity. The medication was well tolerated without prolactin-associated side effects. Concerns of appetite increase and weight gain with olanzapine were minimized through simple education. The average weight gain was 4 lb in the treatment group, compared with 1 lb in the placebo group. Compliance was also high. All subjects elected to enter the open-label phase of the protocol.
In many patients in the study, stuttering symptoms have continued to improve over 6 months to 1 year or even longer, suggesting that an adequate treatment trial should be measured not in days or even weeks, but possibly months. Also, some individuals in the open-label phase have shown even further efficacy with dose escalation to 7.5 mg to 10 mg/d or higher of olanzapine.20
It is likely, however, that pharmacologic treatment will not be the total answer. In the studies cited earlier, the novel dopamine antagonists led to significant—yet only partial—reductions in stuttering symptoms. The future of optimal stuttering treatment will likely involve the active collaboration between a speech language pathologist and a psychiatrist, using speech therapy to enhance the positive benefits of the medication.
Related resources
- National Stuttering Association http://www.nsastutter.org
- University of California-Irvine Medical Center: Facts About Stuttering. http://www.ucihealth.com/News/UCI%20Health/stutter2.htm
- Hulstijn W, Peters HFM, Van Lieshout PHHM, eds. Speech Production: Motor Control, Brain Research and Fluency Disorders. International Congress Series 1146. Amsterdam, Netherlands: Excerpta Medica, 1997.
- Haloperidol • Haldol
- Nimodipine • Nimotop
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Pimozide • Orap
- Risperidone • Risperdal
Drs. Maguire and Franklin report that they receive grant/research support from, serve as consultants to, and are on the speaker’s bureau of Eli Lilly &Co.
Dr. Maguire also reports that he receives grant/research support from Johnson & Johnson, and serves on the speaker’s bureau of Pfizer Inc. and GlaxoSmithKline.
Dr. Yu reports that he serves on the speaker’s bureau of Cephalon Inc.
Drs. Riley and Ortiz report no financial relationship with any company whose products are mentioned in this article.
Despite its prevalence, stuttering has not received as much attention as other psychiatric disorders from patients or psychiatrists—with good reason. Until recently, little was known about the neurophysiology of stuttering, and treatment was generally ineffective especially in adults (Box 1). Despite their own personal struggles with the disorder, patients have questioned the need for psychiatric treatment.
That has now changed. We know now that stuttering is likely a disorder of brain chemistry. Studies suggests that olanzapine, a novel dopamine antagonist, is a useful, well-tolerated medication for the treatment of stuttering. As a result, psychiatrists are now equipped to play an important role in its management.
Furthermore, we can give patients the therapeutic opportunity to discuss what often has been a lifetime of frustration with stuttering. We can enable them to understand the course and treatment of this disorder and encourage them to take advantage of the opportunities to lessen the symptoms of stuttering and, ultimately, improve their quality of life.
How stuttering develops
Stuttering is a speech disorder characterized by frequent prolongations, repetitions, or blocks of spoken sounds and/or syllables. A common disorder affecting 1% of adults and 4% of children, stuttering is classified in DSM-IV as an Axis I disorder (Box 2).1
Stuttering has occurred throughout history, with descriptions from the ancient Egyptians and Greeks. For centuries, theories on its etiology involved abnormalities in the tongue or larynx, and the treatments addressed such ideology. Even today, some stuttering treatments involve such archaic methods as cauterizing or cutting the tongue. Treatments focused on the tongue or larynx have not demonstrated consistent efficacy.
The pioneering work of Orton21 and Travis22 signaled a significant change in the understanding of stuttering. They postulated that stuttering may arise from abnormal cerebral activity, signaling a significant change in the theories of the etiology of stuttering. Unfortunately, stuttering treatments did not reflect this new understanding until fairly recently.
Psychoanalytic theorists believed that stuttering arose from the individual’s attempt to fulfill some type of unconscious neurotic need, usually resulting from disturbed early parent-child interaction.23 Psychoanalytic therapy was largely ineffective, however.
Most stuttering treatment practiced today involves speech therapy utilizing cognitive and behavioral methods. Such methods are often limited in their efficacy, especially in adults.24 Some forms of therapy involving speech motor training have been shown effective in young children while the brain is still in development.25 The pharmacologic treatment of stuttering is not widespread today, but new and recent research identifying certain cerebral abnormalities is providing clues for pharmacologic interventions.
Stuttering usually begins in childhood and is likely a developmental disorder. Rare cases of acquired stuttering begin in adulthood but are related to secondary causes such as medications, brain trauma, or stroke.3 Some 80% to 90% of developmental stuttering begins by age 6; onset after age 9 is likely to have some psychogenic or neurogenic basis.4 In approximately 60% of the children who stutter, the symptoms will remit by age 16. Children who stutter require early intervention, given the importance of communication in a child’s development.5
Stuttering shares many similarities with Tourette syndrome. Both begin in childhood, follow a waxing or waning course, have a 4:1 male-to-female ratio, are made worse by anxiety, involve abnormalities in the basal ganglia, and respond to dopamine antagonist therapy.6 Persons who stutter often exhibit tic motions, similar to those seen in Tourette syndrome, which are associated with the struggles to produce speech. Genetic studies have shown possible high additive genetic effects; pair-wise concordance for stuttering was significantly higher in identical twins (63%) than it was in fraternal same-sex twins (19%).7,8 Researchers are investigating potential molecular genetic markers for stuttering.
Functional brain imaging studies suggest that stuttering is associated with abnormal cerebral activation primarily involving abnormally low metabolism of the cortical speech areas and the striatum. The defects in stuttering occur primarily in the timing and initiation of spontaneous speech, with such tasks as singing and reading in chorus being spared. A clue to understanding stuttering lies with these “induced fluency” tasks.
Functional positron emission tomography studies utilizing18 F-deoxyglucose showed that stuttering is associated with abnormally low metabolism of speech cortical areas (Wernicke’s and Broca’s) and low metabolism of the basal ganglia, notably the striatum. During the induced fluency, Wernicke’s and Broca’s areas normalize but the striatum remains abnormally low.
Riley postulates two “loops” of speech, an inner or medial system and an outer or lateral system.9 The lateral system is preserved in stuttering and can be activated through singing, rhythmic speech, etc., but the inner loop, as mediated by the striatum and influenced by dopamine, remains impaired. Once a person who stutters initiates speech, he or she often avoids taking a breath as the whole system must again be jump-started. The low striatal metabolism may be the common-state phenomenon underlying this timing.
- Disturbance in normal fluency and time patterning of speech (inappropriate for the individual’s age), characterized by frequent occurrences of one or more of the following:
- Sound and syllable repetitions
- Sound prolongations
- Interjections
- Broken words (e.g., pauses within a word)
- Audible or silent blocking (filled or unfilled pauses in speech)
- Circumlocutions (word substitutions to avoid problematic words)
- Words produced with an excess of physical tension
- Monosyllabic whole-word repetitions (e.g., “I-I-I-I see him”)
- Sound and syllable repetitions
- The disturbance in fluency interferes with academic or occupational achievement or with social communications
- If a speech-motor or sensory deficit is present, the speech difficulties are in excess of those usually associated with these problems.
Coding note: If a speech-motor or sensory deficit or a neurological condition is present, code the condition on Axis III.
The dopamine hypothesis of stuttering
Stuttering is likely related to abnormal elevations of cerebral dopamine activity. Stimulant medications, which increase dopamine activity, have been shown to increase stuttering symptoms.10 As will be reviewed later, dopamine antagonist medications have been shown to improve the symptoms of stuttering. Also, the striatal hypometabolism in stuttering seen in PET imaging may be a result of a hyperdopaminergic state.
To investigate this dopamine hypothesis of stuttering, Wu et al measured presynaptic dopamine levels in individuals who stutter.11 These were found to have 50% to 200% higher levels of dopamine activity than did the controls. Dopamine is inhibitory to striatal metabolism, providing an explanation for the striatal hypometabolism seen in stuttering. Also, risperidone was found to increase striatal metabolism in those whose stuttering improved on this medication.12
Evaluating the patient
One should begin with a comprehensive psychiatric history. Because many patients began stuttering in childhood and have had difficulty dealing with their disorder, other psychiatric disorders such as social phobia may be present. Moreover, other medical etiologies (e.g., stroke) may cause a speech disorder that resembles stuttering.
Stuttering involves abnormalities in fluency as well as tic motions and cognitive avoidances. Inquiries should be made as to the patient’s fluency of speech during work, during introductions, speaking in front of an audience, with family, etc.; the level of stuttering can vary depending on the particular environment.
Stuttering fluency can be rated through an objective scale known as the Riley SSI-3.13 This scale measures the duration of each stuttering event, the percentage of syllables stuttered versus syllables spoken, the severity of associated tic motions, and a global score of the aforementioned components. Because most psychiatrists cannot routinely perform this scale to assess the patient’s progress, it is best to partner with a speech-language pathologist who can also assist the patient through speech therapy.
Nonetheless, you may assess the progress of treatment by relying on your own “ear,” the patient’s own assessment, and the input of a significant other or family member.
In addition to considering DSM-IV criteria, comprehensive treatment should address all aspects of this disorder, including not only the fluency enhancement but improvement in social avoidances and cognitive restructuring. Be aware that stuttering waxes and wanes over time. You should expect to see some “dips” in efficacy during the course of therapy. A longitudinal assessment over several months is needed to determine if the stuttering treatment is efficacious.
What we’ve learned about drug therapy
Many medications have been tried to treat stuttering but few have shown efficacy in well-controlled trials. Most pharmacologic studies did not include a placebo control or employ objective measures of stuttering severity, nor did they provide multiple baseline and treatment measures.
The critical new knowledge is this: Medications that lower dopamine activity have shown replicated efficacy in improving stuttering. The benzodiazepines have been shown to reduce anxiety short-term but have not been shown to improve fluency in stuttering. Limited studies of serotonergic antidepressants suggest a possible role in reducing the social anxiety of stuttering but have not been shown in well-controlled trials to improve stuttering fluency directly.
Multiple studies of haloperidol in the 1970s showed that this medication improved fluency in individuals who stutter. Long-term compliance with this medication, however, was poor given its dysphoric side effects, sexual dysfunction, extrapyramidal concerns, and risks of tardive dyskinesia. Limited research with calcium-channel-blocking medications (e.g., verapamil, nimodipine) showed limited efficacy in stuttering.14,15 Calcium-channel blockers, however, may exert a mild antidopamine effect.
Further supporting dopamine hyperactivity in the pathology of stuttering, Stager et al compared pimozide (n = 6), a selective dopamine (D2) antagonist, paroxetine (n = 5), a highly selective serotonin reuptake inhibitor, and placebo (n = 6). The researchers found a positive clinical response in those on pimozide compared with those taking placebo, whereas the paroxetine group exhibited no clinical response.16 Although small, such a study supports the hypothesis that dopamine may be a principal transmitter involved in stuttering pathology, and serotonin may play a minor role, if any.
Risperidone, a newer-generation dopamine antagonist with a side-effect profile more favorable than haloperidol, has been shown in a well-controlled, double-blind, placebo-controlled study to improve stuttering symptoms (0.5 mg to 2 mg/d). Although generally well tolerated, long-term compliance was hindered by prolactin-related side effects such as sexual dysfunction, galactorrhea, amenorrhea, and dysphoria.17 Dysphoria with risperidone has also recently been reported to occur with its use in Tourette disorder.18
Olanzapine is a novel psychotropic medication that possesses dopamine-blocking qualities but is not associated as much with prolactin-related side effects or dysphoria. A preliminary open-label study suggests that it too improves the symptoms of stuttering.19
A multicenter study of olanzapine in the treatment of adult developmental stuttering involved 23 adults in a 3-month, double-blind, placebo-controlled trial preceded by a 1-month baseline rating period. At the end of the double-blind phase, subjects were followed for 1 year. Olanzapine (2.5 mg titrated to 5 mg/d) was shown to exert a statistically significant improvement over placebo in multiple objective measures of stuttering severity. The medication was well tolerated without prolactin-associated side effects. Concerns of appetite increase and weight gain with olanzapine were minimized through simple education. The average weight gain was 4 lb in the treatment group, compared with 1 lb in the placebo group. Compliance was also high. All subjects elected to enter the open-label phase of the protocol.
In many patients in the study, stuttering symptoms have continued to improve over 6 months to 1 year or even longer, suggesting that an adequate treatment trial should be measured not in days or even weeks, but possibly months. Also, some individuals in the open-label phase have shown even further efficacy with dose escalation to 7.5 mg to 10 mg/d or higher of olanzapine.20
It is likely, however, that pharmacologic treatment will not be the total answer. In the studies cited earlier, the novel dopamine antagonists led to significant—yet only partial—reductions in stuttering symptoms. The future of optimal stuttering treatment will likely involve the active collaboration between a speech language pathologist and a psychiatrist, using speech therapy to enhance the positive benefits of the medication.
Related resources
- National Stuttering Association http://www.nsastutter.org
- University of California-Irvine Medical Center: Facts About Stuttering. http://www.ucihealth.com/News/UCI%20Health/stutter2.htm
- Hulstijn W, Peters HFM, Van Lieshout PHHM, eds. Speech Production: Motor Control, Brain Research and Fluency Disorders. International Congress Series 1146. Amsterdam, Netherlands: Excerpta Medica, 1997.
- Haloperidol • Haldol
- Nimodipine • Nimotop
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Pimozide • Orap
- Risperidone • Risperdal
Drs. Maguire and Franklin report that they receive grant/research support from, serve as consultants to, and are on the speaker’s bureau of Eli Lilly &Co.
Dr. Maguire also reports that he receives grant/research support from Johnson & Johnson, and serves on the speaker’s bureau of Pfizer Inc. and GlaxoSmithKline.
Dr. Yu reports that he serves on the speaker’s bureau of Cephalon Inc.
Drs. Riley and Ortiz report no financial relationship with any company whose products are mentioned in this article.
1. American Psychiatric Association. DSM-IV-R. Washington, DC: American Psychiatric Association, 2000.
2. Maguire GA, Riley GD, Franklin DL, Wu JC, et al. The dopamine hypothesis of stuttering and its treatment implications. Intern J Neuropsychopharmacology 2000;3(1):
3. Ludlow CL, Dooman AG. Genetic aspects of idiopathic speech and language disorders. Otolaryngol Clin N Am 1992;25(5):979-94.
4. Manning WH. Clinical decision making in fluency disorders. 2nd ed. San Diego, Calif: Singular, 2001;107-8.
5. Riley G, Ingham J. Acoustic duration changes associated with two types of treatment for children who stutter. J Speech Language Hearing 2000;43:965-78.
6. Wu JC, Maguire GA, et al. A positron emission tomography [18F] deoxyglucose study of developmental stuttering. Neuroreport 1995;6:501-5.
7. Felsenfeld S, Kirk KM, Zhu G, et al. A study of the genetic and environmental etiology of stuttering in a selected twin sample. Behav Gen 2000;30(5):359-66.
8. Howie PM. Concordance for stuttering in monozygotic and dizygotic twin pairs. J Speech Hearing Research 1981;24(3):317-21.
9. Riley GD, Wu JC, Maguire GA. Pet scan evidence of parallel cerebral systems related to treatment effects. In Hulstijn W, Peters HFM, Van Lieshout PHHM (eds.), Speech Production: Motor Control, Brain Research and Fluency Disorders. Amsterdam: Excerpta Medica, 1997.
10. Burd, Kerbeshian J. Stuttering and stimulants [letter]. J Clin Psychopharmacology 1991;11(1):72-3.
11. Wu JC, Maguire G, Riley G, et al. Increased dopamine activity associated with stuttering. Neuroreport 1997;8(3):767-70.
12. Maguire GA. The Dopamine Hypothesis of Stuttering and its Treatment Implications. Presented at Collegium Internationale Neuro-Psychopharmacologicum. Brussels, Belgium, July 2000.
13. Riley G. Stuttering Severity Instrument. 3rd ed. Austin, Tex: ProEd, 1994.
14. Brady JP, McAllister TW, Price TR. Verapamil in stuttering [letter]. Biol Psychiatry 1990;27(6):680-1.
15. Maguire G, Riley G, Hahn R, Plon L. Nimodipine in the treatment of stuttering. ASHA Journal 1994;36:51.-
16. Stager S, Calis K, Grothe D, et al. A double-blind trial of pimozide and paroxetine for stuttering. In: Hulstijn W, Peters HRM, van Lieshout PHHM, eds. Speech Production: Motor Control, Brain Research and Fluency Disorders. International Congress Series 1146. Amsterdam: Excerpta Medica, 1997;379-82.
17. Maguire GA, Riley GD, Franklin DL, Gottshalk LA. Risperidone for the Treatment of Stuttering. J Clin Psychopharmacology 2000-20:479-82.
18. Margolese HC, Annabel L, Dion Y. Depression and dysphoria in adult and adolescent patients with Tourette syndrome treated with risperidone. Presented at the American College of Neuropsychopharmacology, Waikoloa, Hawaii Dec. 10, 2001.
19. Lavid N, Franklin DL, Maguire GA. Management of Child and Adolescent Stuttering with Olanzapine: Three Case Reports. Ann Clin Psychiatry 1999;11(4):233-36.
20. Maguire GA, et al. Olanzapine in the Treatment of Adult Developmental Stuttering. Presented at the American College of Neuropsychopharmacology, Waikoloa, Hawaii Dec. 10, 2001.
21. Orton ST. Studies in stuttering. Arch Neurology Psychiatry 1927;18:671-2.
22. Travis LE. Speech Pathology. New York: Appleton-Century-Crofts, 1931.
23. Sadock BJ, Sadock VA. Kaplan and Sadock’s Comprehensive Textbook of Psychiatry. 7th ed. Baltimore, Md: Lippincott Williams & Wilkins, 2000.
24. Manning WH. Clinical Decision Making in Fluency Disorders. 2nd ed. San Diego, Calif: Singular Publishing, 2001;311-14.
25. Riley G, Ingham J. Acoustic duration changes associated with two types of treatment for children who stutter. J Speech Language Hearing 2000;43:965-78.
1. American Psychiatric Association. DSM-IV-R. Washington, DC: American Psychiatric Association, 2000.
2. Maguire GA, Riley GD, Franklin DL, Wu JC, et al. The dopamine hypothesis of stuttering and its treatment implications. Intern J Neuropsychopharmacology 2000;3(1):
3. Ludlow CL, Dooman AG. Genetic aspects of idiopathic speech and language disorders. Otolaryngol Clin N Am 1992;25(5):979-94.
4. Manning WH. Clinical decision making in fluency disorders. 2nd ed. San Diego, Calif: Singular, 2001;107-8.
5. Riley G, Ingham J. Acoustic duration changes associated with two types of treatment for children who stutter. J Speech Language Hearing 2000;43:965-78.
6. Wu JC, Maguire GA, et al. A positron emission tomography [18F] deoxyglucose study of developmental stuttering. Neuroreport 1995;6:501-5.
7. Felsenfeld S, Kirk KM, Zhu G, et al. A study of the genetic and environmental etiology of stuttering in a selected twin sample. Behav Gen 2000;30(5):359-66.
8. Howie PM. Concordance for stuttering in monozygotic and dizygotic twin pairs. J Speech Hearing Research 1981;24(3):317-21.
9. Riley GD, Wu JC, Maguire GA. Pet scan evidence of parallel cerebral systems related to treatment effects. In Hulstijn W, Peters HFM, Van Lieshout PHHM (eds.), Speech Production: Motor Control, Brain Research and Fluency Disorders. Amsterdam: Excerpta Medica, 1997.
10. Burd, Kerbeshian J. Stuttering and stimulants [letter]. J Clin Psychopharmacology 1991;11(1):72-3.
11. Wu JC, Maguire G, Riley G, et al. Increased dopamine activity associated with stuttering. Neuroreport 1997;8(3):767-70.
12. Maguire GA. The Dopamine Hypothesis of Stuttering and its Treatment Implications. Presented at Collegium Internationale Neuro-Psychopharmacologicum. Brussels, Belgium, July 2000.
13. Riley G. Stuttering Severity Instrument. 3rd ed. Austin, Tex: ProEd, 1994.
14. Brady JP, McAllister TW, Price TR. Verapamil in stuttering [letter]. Biol Psychiatry 1990;27(6):680-1.
15. Maguire G, Riley G, Hahn R, Plon L. Nimodipine in the treatment of stuttering. ASHA Journal 1994;36:51.-
16. Stager S, Calis K, Grothe D, et al. A double-blind trial of pimozide and paroxetine for stuttering. In: Hulstijn W, Peters HRM, van Lieshout PHHM, eds. Speech Production: Motor Control, Brain Research and Fluency Disorders. International Congress Series 1146. Amsterdam: Excerpta Medica, 1997;379-82.
17. Maguire GA, Riley GD, Franklin DL, Gottshalk LA. Risperidone for the Treatment of Stuttering. J Clin Psychopharmacology 2000-20:479-82.
18. Margolese HC, Annabel L, Dion Y. Depression and dysphoria in adult and adolescent patients with Tourette syndrome treated with risperidone. Presented at the American College of Neuropsychopharmacology, Waikoloa, Hawaii Dec. 10, 2001.
19. Lavid N, Franklin DL, Maguire GA. Management of Child and Adolescent Stuttering with Olanzapine: Three Case Reports. Ann Clin Psychiatry 1999;11(4):233-36.
20. Maguire GA, et al. Olanzapine in the Treatment of Adult Developmental Stuttering. Presented at the American College of Neuropsychopharmacology, Waikoloa, Hawaii Dec. 10, 2001.
21. Orton ST. Studies in stuttering. Arch Neurology Psychiatry 1927;18:671-2.
22. Travis LE. Speech Pathology. New York: Appleton-Century-Crofts, 1931.
23. Sadock BJ, Sadock VA. Kaplan and Sadock’s Comprehensive Textbook of Psychiatry. 7th ed. Baltimore, Md: Lippincott Williams & Wilkins, 2000.
24. Manning WH. Clinical Decision Making in Fluency Disorders. 2nd ed. San Diego, Calif: Singular Publishing, 2001;311-14.
25. Riley G, Ingham J. Acoustic duration changes associated with two types of treatment for children who stutter. J Speech Language Hearing 2000;43:965-78.