User login
Management of the low-grade abnormal Pap smear: What are women’s preferences?
- Any of several approaches may be used in managing women who have low-grade Pap smear abnormalities.
- Women’s preferences for a particular management approach to an abnormal Pap smear vary widely.
- Asking patients specific questions about their desire to avoid procedures and tolerance for uncertainty may help to clarify preferences.
The management of women who have low-grade cytologic abnormalities—including atypical squamous cells (ASC) and low-grade squamous intraepithelial lesions (LSIL)—is controversial.1-4 Without strong evidence favoring a single approach, some clinicians recommend immediate colposcopy to obtain a definitive diagnosis and to exclude the presence of a high-grade lesion, while others recommend observation with serial Pap smears, given the tendency for many low-grade lesions to regress spontaneously.5,6 Immediate colposcopy has the advantage of giving a patient a relatively rapid assessment of the nature and extent of her cervical dysplasia; however, the procedure is uncomfortable, and overall management may not be affected. Observation with serial Pap smears may avoid an invasive procedure, but it may also cause anxiety as time passes without a definitive diagnosis.
Eliciting and understanding patient preferences is an important part of clinical decision making. The clinician provides the best available information on the probability of clinical outcomes and the implications of each for the patient’s health. But only the patient knows what these outcomes mean to her well-being (also called “utility”).
Given the clinical disagreement over how to proceed with abnormal ASC and LSIL Pap smear results, the decision should be influenced by a patient’s preference, informed by knowledge of outcomes and costs of alternative approaches. It is unclear which approach women prefer, and whether women’s preferences for specific protocols are associated with sociodemographic characteristics. To understand better how women weigh these trade-offs, we evaluated the preferences of a diverse group of women for contrasting management approaches to the evaluation of a hypothetical low-grade abnormal Pap smear result.
Methods
Study population
Study participants were recruited from the waiting rooms of 5 family planning clinics in Northern California’s Central Valley. Women were eligible for the study if they were 18 years of age or older, or, if minors, they were emancipated and could thus provide informed consent. Potential subjects were excluded if they spoke neither English nor Spanish or if they had never had a Pap smear. The study protocol and informed consent procedures were reviewed and approved by the University of California, Davis, Human Subjects Committee.
Instruments and outcome measures
Interviews were conducted in English or Spanish. Information regarding demographic characteristics, level of education, past experiences with abnormal Pap smears and cervical cancer, and self-rated religiosity was collected with a self-administered questionnaire. The primary outcome measures were utilities (quantified preferences for specific health states) for 6 different scenarios. These were assessed by the standard gamble (SG) method, described in more detail below.7
Possible utility scores range from 0 to 1. A score of 0 represents immediate death; a score of 1 represents full (or ideal) health for the rest of one’s life. Because the scenarios under consideration in this study did not involve any meaningful level of risk of death, we expected utility scores for the scenarios to cluster toward the upper end of the scale. As a result, a measurement instrument based on an “immediate death” versus “full health” scale would be unable to discriminate between different scenarios. To avoid this problem, a scale was used in which the lower end point was a non-death state unambiguously less preferred than each of the scenarios under consideration.8 We used “invasive cervical cancer requiring hysterectomy” as the lower end point (utility of 0) contrasted with “full health with all normal Pap smears” (utility of 1) to generate the original score (SG Dys). In a separate standard gamble, subjects rated invasive cervical cancer versus immediate death (SG Ca), so that all utilities could be converted to the standard scale, using the formula: (1 – SG Ca) (SG Dys) + SG Ca.
The 6 scenarios rated in the study are shown in Table 1. The scenarios represent 3 sets of progressively more invasive interventions for a low-grade abnormal Pap smear: (1) resolution, representing spontaneous regression with treatment not required; (2) a low-grade abnormality requiring treatment with cryotherapy; (3) a more severe abnormality requiring a cervical cone biopsy. Following either spontaneous resolution or treatment, all scenarios assumed the abnormality was resolved. For each of the 3 results, a management strategy based on observation with serial Pap smears was applied in 1 instance, and a strategy of early colposcopy was applied in the other instance, resulting in 6 different pathways to the ultimate outcome; a normal Pap smear. The time frame for these scenarios was 18–36 months.
Trained interviewers used a standardized approach to elicit preferences from each subject. Subjects were read a description of all the procedures involved in the scenarios. Descriptions were accompanied by cards summarizing each procedure in pictures and words, and included information about the possibility of progression and spontaneous regression of the Pap smear abnormality. Subjects were encouraged to ask questions at any point during the interview. Procedure descriptions are available from the authors on request.
TABLE 1
Clinical scenarios classified by management approach and required treatment*
| Spontaneous resolution | Cryotherapy | Cone biopsy | |
|---|---|---|---|
| Observation | Pap smear: low-grade abnormal | Pap smear: low-grade abnormal | Pap smear: low-grade abnormal |
| ↓ | ↓ | ↓ | |
| Pap smear: normal | Pap smear: low-grade abnormal | Pap smear: normal | |
| ↓ | ↓ | ↓ | |
| 2 Pap smears every 6 months: normal | Pap smear: low-grade abnormal | Pap smear: normal | |
| ↓ | ↓ | ||
| Pap smear: low-grade abnormal | Pap smear: normal | ||
| ↓ | ↓ | ||
| Colposcopy and biopsy at 1 month | Colposcopy and biopsy at 1 month | ||
| ↓ | ↓ | ||
| Biopsy: low-grade abnormal | Biopsy: abnormal with ? ECC | ||
| ↓ | ↓ | ||
| Cryotherapy at 1 month | Cone biopsy at 1 month: moderately abnoramal cells | ||
| ↓ | ↓ | ||
| 3 Pap smears every 6 months: normal | Cure with cone biopsy | ||
| ↓ | |||
| 3 Pap smears every 6 months: normal | |||
| Early colposcopy | Pap smear: low-grade abnormal | Pap smear: low-grade abnormal | Pap smear: low-grade abnormal |
| ↓ | ↓ | ↓ | |
| Colposcopy and biopsy at 1 month | Colposcopy and biopsy at 1 month | Colposcopy and biopsy at 1 month | |
| ↓ | ↓ | ↓ | |
| Biopsy: normal | Biopsy: abnormal with ? ECC | Biopsy: abnormal with ? ECC | |
| ↓ | ↓ | ↓ | |
| Second colposcopy and biopsy | Cone biopsy at 1 month | Cone biopsy at 1 month | |
| ↓ | ↓ | ↓ | |
| Biopsy: normal | Biopsy: moderately abnormal | Biopsy: moderately abnormal | |
| ↓ | ↓ | ↓ | |
| 2 Pap smears every 6 months: normal | Cure with cone biopsy | Cure with cone biopsy | |
| ↓ | ↓ | ↓ | |
| Pap smear: low-grade abnormal | Colposcopy: normal | Colposcopy: normal | |
| ↓ | ↓ | ↓ | |
| Colposcopy and biopsy at 1 month | 2 Pap smears every 6 months: normal | 2 Pap smears every 6 months: normal | |
| ↓ | |||
| Biopsy: low-grade abnormal | |||
| ↓ | |||
| Colposcopy: normal | |||
| ↓ | |||
| 2 Pap smears every 6 months: normal | |||
| *Intervals are 6 months unless specified otherwise. ECC, endocervical curettage. | |||
Standard gamble
Subjects were asked their preference between the certainty of the scenario under consideration and an uncertain prospect of either having cervical cancer treated by hysterectomy or full health. A probability wheel was used as visual aid.9 The probability of cervical cancer was altered until the subject was indifferent between the certain scenario and the uncertain prospect. Once all 6 scenarios had been scored, each subject was asked about her preference between the certainty of cervical cancer treated by hysterectomy and the uncertain prospect of immediate death or full health, using the same method.
At the end of the interview, both the subject and the interviewer completed evaluation forms including ratings of how well the subject understood the standard gamble rating exercises. Subject confusion was also defined a priori as those placing a higher utility on scenario 3 (observation for a long period followed by cone biopsy), which represented the longest period of uncertainty followed by the most invasive procedure, than on scenario 1 (a single mildly abnormal Pap smear evaluated by observation which then resolved spontaneously), which represented the absence of any invasive procedure.
Statistical analysis
Descriptive statistics were generated for ratings of each scenario for the entire group and with the confused subjects removed. Confused subjects included those who reported they found the interview “very confusing,” those who were recorded by the interviewer as finding the interview “very confusing,” and those whose rankings met the criteria for subject confusion, as described above. Means, standard deviations, medians, and percentiles were calculated for each scenario. The mean differences in adjusted standard gamble ratings between paired scenarios was evaluated using a t distribution. Multiple regression analyses were used to explore how much between-subject variation in the standard gamble scores was explained by the variables listed above.
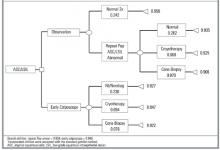
A simple decision tree (Figure 1) was constructed to contrast preferences for an observational approach vs early colposcopy. Outcome probabilities were derived from meta-analyses of the medical literature,5 from observational data obtained at the same Northern California family planning clinics,10 and, for cone biopsy outcomes, from expert opinion obtained using a modified Delphi process.11 Utilities were assigned to the decision tree based on the standard gamble results. Women having 2 consecutive low-grade abnormal Pap results followed by a normal Pap result were assigned the same utility value as that for women with a single abnormal result. Analysis of the tree, including 1-way and 2-way sensitivity analysis of key variables, was conducted with Data 3.5.
Results
One hundred seventy interviews were completed. Characteristics of the interview subjects are shown in Table 2. A total of 22 subjects were designated “confused.” Analyses including the confused subjects did not alter the pattern of results, but the range in responses was larger. All analyses are presented here with confused subjects removed (n = 148).
Median ratings with 25th–75th percentiles for the paired scenarios rated by the standard gamble are shown as box plots in Figure 2. Mean adjusted scores, standard deviations, and mean differences in scores between paired scenarios are shown in Table 3. Notable findings include the following. (1) For each scenario, the range of responses by either rating method was very large. (2) Mean differences in utilities for observation vs early colposcopy were small. (3) For the paired scenarios in which the outcome was spontaneous resolution, observation was preferred (P = .01); in the paired scenarios in which the outcome was cryotherapy, early colposcopy was preferred (P = .02). (4) In the multiple regression analyses for each scenario, age, education, ethnicity, religiosity, and having known someone with cervical cancer together explained only a small amount of the variability between subjects (range for R2, .09–.22).
The decision model with baseline probabilities is shown in Figure 1. The model was simplified to exclude the outcome of cervical cancer, which is a very rare outcome for women with ASC or LSIL cervical smears who have adequate follow-up.5 In the baseline analysis, the overall utility of early colposcopy was slightly favored over the overall utility of the observation approach (utility of observation = 0.932; utility of early colposcopy = 0.940).
Sensitivity analysis examines the effect of varying elements of the model on the outcome. In sensitivity analyses of probabilities, the early colposcopy branch was favored, but the differences were small. The maximum difference in utilities between branches was 0.012 in these sensitivity analyses. In 1-way sensitivity analysis of branch utilities, threshold utility values to favor the observation branch were 0.986 for spontaneous resolution after observation and 0.898 for early colposcopy. Threshold values for cryotherapy were 0.938 for observation and 0.938 for early colposcopy.
TABLE 2
Characteristics of study subjects (n = 170)
| Characteristics | n (%) |
|---|---|
| Mean age (range), y | 26 (14–53) |
| Education | |
| Less than high school | 58 (34%) |
| High school | 77 (45%) |
| Some college | 35 (20%) |
| Ethnicity | |
| African American | 21 (12%) |
| Caucasian | 84 (49%) |
| Latina | 46 (27%) |
| Other | 21 (12%) |
| Interview language, Spanish | 15 (9%) |
| Prior colposcopy | 23 (14%) |
| Moderately or very religious | 64 (38%) |
| Knows someone with cervical cancer | 43 (25%) |
TABLE 3
Adjusted standard gamble values and paired differences* (n=148)
| Management Strategy | ||||
|---|---|---|---|---|
| Short-term outcome | Observation Mean (SD) | Early colposcopy Mean (SD) | Difference | P value (2 sided) |
| Spontaneous resolution | .96 ±..13) | .93±.20) | .03 ±..15) | .01 |
| Cryotherapy | .93 ±..17) | .95 ±..14) | -.02 ±.11) | .02 |
| Cone biopsy | .91 ±..21) | .92 ±..16) | -.02 ±..17) | .23 |
| *Adjusted to scale so that immediate death had a utility of 0 and “full health with all normal Pap smears” had a utility of 1. | ||||
FIGURE 1Decision model comparing observation with early colposcopy *
FIGURE 2Distribution of individual utilities as assessed by the standard gamble*
Discussion
We found wide variation in women’s preferences for management approaches to a low-grade abnormal Pap smear result. The range of responses was very large and the variation between individuals rating the same scenario was substantially greater than the variation in mean ratings between different scenarios. Measured subject characteristics explained only a small proportion of the observed variation, indicating that other unmeasured factors contributed substantially to the variation. Although 25% of subjects stated they knew someone with cervical cancer, this high percentage seems improbable and more likely reflects knowledge of someone who had an abnormal Pap smear.
The decision model displayed a small preference for immediate colposcopy. This may be related to preference for quicker resolution of the concern about cancer, although it involves more procedures. Small changes in utilities for spontaneous resolution and cryotherapy influenced the model to prefer observation. For cryotherapy, these utility values were within 1 standard deviation of the mean.
Our finding of a wide variation in preferences is supported by other patient preference studies,12-14 including 2 on this subject. Ferris et al assessed triage preferences for the evaluation and management ASC and LSIL.13 They used a questionnaire with a sample of 968 women who presented for care at obstetrics and gynecology and family practice clinics. They found that more women preferred repeat Pap smear when the index smear was ASC, and more women preferred colposcopy when the index smear was LSIL. Among a group of 136 Canadian women with atypia or LSIL referred for colposcopy, Meana et al found that 64% preferred early colposcopy, while 17% preferred observation and 17% had no strong preference.14
The factors contributing to patient preferences are complex. Differences in preferences may be influenced by knowledge and understanding of the disease and possible interventions, risk aversion, access to services, socioeconomics, cultural background, and other factors. While 1 patient may be most interested in establishing a definitive diagnosis and undergoing treatment as soon as possible, another may place priority on avoiding invasive or uncomfortable procedures. How differences in patient preferences influence clinical choices is highlighted by the work of Kuppermann et al.15 These investigators found that utilities for outcomes of prenatal diagnostic testing predicted subsequent testing behavior.
Our findings are limited by our use of a convenience sample of women attending family planning clinics. They may not be representative of women’s preferences in general, or even those of women attending family planning clinics. Outcomes in our study were specified during the preference assessment process; in real decision making, the outcome is always unknown at the time the decision is made. We did not include HPV typing as an option in our clinical scenarios. While HPV typing may have a role for triage of ASC,6,16 it appears not to be useful in management of LSIL.17
Cost-effectiveness analysis would offer important information about which management approach might be favored in the context of resource allocation. For decision making by individual patients and doctors, however, decision analysis is often more relevant. In this case, the “preferred” decision is very sensitive to patient utilities, emphasizing the need for clear physician-patient communication.
Strengths of our study include the diversity of the subjects, the formal process for preference assessment, and the paired scenarios, which allow assessment of preferences for a single management decision, in which 2 separate paths lead to an equivalent ultimate outcome. Our findings are consistent with previous work showing that the sequence of events leading to an outcome will influence utilities for the outcome.18
Application to clinical practice
How might our findings be translated into clinical practice? In clinical situations where different approaches to management are unlikely to result in substantial outcome differences (a “toss-up”), patient preferences are a key aspect of the decision-making process.19 For women with lowgrade Pap abnormalities, several diagnostic options are available and no single option is strongly supported by evidence to offer better outcomes. Our study indicates that no single option is preferred by most women. Under these conditions, engaging the patient in the decision-making process may produce better health outcomes.20 Clinicians should anticipate highly varied preferences, and will need to adopt a flexible approach. Not all patients will want to be actively involved in the decision process, but the desire for information is nearly universal. Flexible use of the questions in Table 4 may help patients to define their preferences and will likely improve their satisfaction and adherence to the treatment plan.
TABLE 4
Questions for patients with an abnormal Pap smear
| What is your understanding of what it means for you to have an abnormal Pap smear showing _____________? |
| There are different options for the next step. Would you like to be involved in deciding which option is preferred for your case? |
| What questions do you have about these options? |
| How important is it to you to have a definite answer as soon as possible? |
| How do you feel about undergoing colposcopy? |
| Would you prefer to have a follow-up Pap smear in ____ months, which might avoid a colposcopy, or would you prefer to have a colposcopy sooner? |
· Acknowledgments ·
The authors thank the staff of Planned Parenthood Mar Monte East for their assistance with subject recruitment and interviews.
1. Woolf SH. Screening for cervical cancer. In: Goldbloom RB, Lawrence RS, eds. Preventing disease: beyond the rhetoric. New York: Spring-Verlag, 1990:319–23.
2. Kurman RJ, Henson DE, Herbst AL, Noller KL, Schiffman MH. Interim guidelines for management of abnormal cervical cytology. The 1992 National Cancer Institute Workshop. JAMA 1994;271:1866-69.
3. Miller AB, Anderson G, Brisson J, Laidlaw J, Le Pitre N, Malcolmson P, et al. Report of a national workshop on screening for cancer of the cervix. Can Med Assoc J 1991;145:1301-25.
4. American College of Obstetricians and Gynecologists. Cervical cytology: evaluation and management of abnormalities. ACOG technical bulletin no. 183. Washington, DC: American College of Obstetricians and Gynecologists, 1993.
5. Melnikow J, Nuovo J, Willan AR, Chan BK, Howell LP. Natural history of cervical squamous intraepithelial lesions: A meta-analysis. Obstet Gynecol 1998;92:727-34.
6. Wright TC, Cox TJ, Massad LS, Twiggs LB, Wilkonson EJ. Consensus guidelines for the management of women with cervical cytological abnormalities. JAMA 2002;287:2120-29.
7. Drummond MF, O’Brien BJ, Stoddart GL, Torrance GW, eds. Methods for the economic evaluation of health care programs. 2nd edition. New York: Oxford University Press, 1997.
8. Torrance G. Measurement of health state utilities for economic appraisal: A review. J Health Econ., 1986;5:1-30.
9. Furlong W, Feeny D, Torrance GW, Barr R, Horsman J. Guide to design and development of health state utility instrumentation. Centre for Health Economics and Policy Development. Working Paper Series # 90-9. Hamilton, McMaster University, 1990.
10. Melnikow J, Nuovo J, Paliescheskey M, Stewart GK, Howell L, Green B. Detection of high grade cervical dysplasia: Impact of age and Bethesda system-related follow-up criteria. Diagnostic Cytopathol 1997;17:321-25.
11. Fink A, Kosecoff J, Chassin M, Brook RH. Consensus methods: Characteristics and guidelines for use. Am J Pub Health 1984;74:979-83.
12. Nease RF, Kneeland T, O’Connor GT, Sumner W, Lumpkins C, Shaw L, et al. Variation in patient utilities for outcomes of the management of chronic stable angina. JAMA 1995;273:1185-90.
13. Ferris DG, Kriegel D, Cole L, Litaker M, Woodward L. Women’s triage and management p for cervical cytologic reports demonstrating atypical squamous cells of undetermined significance and low grade squamous intraepithelial lesions. Arch Fam Med 1997;6:348-53.
14. Meana M, Steward DE, Lickrish GM, Murphy J, Rosen B. Patient preference for the management of midly abnormal Papanicolaou smears. J Women’s Health and Gender Based Medicine 1999;8:941-7.
15. Kuppermann M, Nease RF, Learman LA, Gates E, Posner SF, Washington AE. How do women value Down syndrome-affected birth and miscarriage? The thirty-five-year-old question. Decis Making 1998;18:468.-
16. Solomon D, Schiffman M, Tarone R. Comparison of three management strategies for patients with atypical squamous cells of undetermined significance: baseline results from a randomized trial. J Natl Cancer Inst 2001;93(4):252-3.
17. The atypical squamous cells of undetermined significance/low grade squamous intraepithelial lesions triage study (ALTS) group. Human papillomavirus testing for triage of women with cytologic evidence of low-grade squamous intra-epithelial lesions: baseline data from a randomized trial. J Natl Cancer Inst,. 2000;92:397-402.
18. Kuppermann M, Shiboski S, Feeny D, Elkin E, Washington AE. Can preference scores for discrete states be used to derive preference scores for an entire path of events? An application to prenatal diagnosis. Med Decis Making 1997;17:42-55.
19. Kassirer JP, Pauker SG. The toss up. N Engl J Med 1981;305:1457-9.
20. Kaplan SH, Greenfield S, Ware JE, Jr. Assessing the effects of physician patient interactions on the outcomes of care. Med Care 1989;27 (Suppl 3):S110-27.
- Any of several approaches may be used in managing women who have low-grade Pap smear abnormalities.
- Women’s preferences for a particular management approach to an abnormal Pap smear vary widely.
- Asking patients specific questions about their desire to avoid procedures and tolerance for uncertainty may help to clarify preferences.
The management of women who have low-grade cytologic abnormalities—including atypical squamous cells (ASC) and low-grade squamous intraepithelial lesions (LSIL)—is controversial.1-4 Without strong evidence favoring a single approach, some clinicians recommend immediate colposcopy to obtain a definitive diagnosis and to exclude the presence of a high-grade lesion, while others recommend observation with serial Pap smears, given the tendency for many low-grade lesions to regress spontaneously.5,6 Immediate colposcopy has the advantage of giving a patient a relatively rapid assessment of the nature and extent of her cervical dysplasia; however, the procedure is uncomfortable, and overall management may not be affected. Observation with serial Pap smears may avoid an invasive procedure, but it may also cause anxiety as time passes without a definitive diagnosis.
Eliciting and understanding patient preferences is an important part of clinical decision making. The clinician provides the best available information on the probability of clinical outcomes and the implications of each for the patient’s health. But only the patient knows what these outcomes mean to her well-being (also called “utility”).
Given the clinical disagreement over how to proceed with abnormal ASC and LSIL Pap smear results, the decision should be influenced by a patient’s preference, informed by knowledge of outcomes and costs of alternative approaches. It is unclear which approach women prefer, and whether women’s preferences for specific protocols are associated with sociodemographic characteristics. To understand better how women weigh these trade-offs, we evaluated the preferences of a diverse group of women for contrasting management approaches to the evaluation of a hypothetical low-grade abnormal Pap smear result.
Methods
Study population
Study participants were recruited from the waiting rooms of 5 family planning clinics in Northern California’s Central Valley. Women were eligible for the study if they were 18 years of age or older, or, if minors, they were emancipated and could thus provide informed consent. Potential subjects were excluded if they spoke neither English nor Spanish or if they had never had a Pap smear. The study protocol and informed consent procedures were reviewed and approved by the University of California, Davis, Human Subjects Committee.
Instruments and outcome measures
Interviews were conducted in English or Spanish. Information regarding demographic characteristics, level of education, past experiences with abnormal Pap smears and cervical cancer, and self-rated religiosity was collected with a self-administered questionnaire. The primary outcome measures were utilities (quantified preferences for specific health states) for 6 different scenarios. These were assessed by the standard gamble (SG) method, described in more detail below.7
Possible utility scores range from 0 to 1. A score of 0 represents immediate death; a score of 1 represents full (or ideal) health for the rest of one’s life. Because the scenarios under consideration in this study did not involve any meaningful level of risk of death, we expected utility scores for the scenarios to cluster toward the upper end of the scale. As a result, a measurement instrument based on an “immediate death” versus “full health” scale would be unable to discriminate between different scenarios. To avoid this problem, a scale was used in which the lower end point was a non-death state unambiguously less preferred than each of the scenarios under consideration.8 We used “invasive cervical cancer requiring hysterectomy” as the lower end point (utility of 0) contrasted with “full health with all normal Pap smears” (utility of 1) to generate the original score (SG Dys). In a separate standard gamble, subjects rated invasive cervical cancer versus immediate death (SG Ca), so that all utilities could be converted to the standard scale, using the formula: (1 – SG Ca) (SG Dys) + SG Ca.
The 6 scenarios rated in the study are shown in Table 1. The scenarios represent 3 sets of progressively more invasive interventions for a low-grade abnormal Pap smear: (1) resolution, representing spontaneous regression with treatment not required; (2) a low-grade abnormality requiring treatment with cryotherapy; (3) a more severe abnormality requiring a cervical cone biopsy. Following either spontaneous resolution or treatment, all scenarios assumed the abnormality was resolved. For each of the 3 results, a management strategy based on observation with serial Pap smears was applied in 1 instance, and a strategy of early colposcopy was applied in the other instance, resulting in 6 different pathways to the ultimate outcome; a normal Pap smear. The time frame for these scenarios was 18–36 months.
Trained interviewers used a standardized approach to elicit preferences from each subject. Subjects were read a description of all the procedures involved in the scenarios. Descriptions were accompanied by cards summarizing each procedure in pictures and words, and included information about the possibility of progression and spontaneous regression of the Pap smear abnormality. Subjects were encouraged to ask questions at any point during the interview. Procedure descriptions are available from the authors on request.
TABLE 1
Clinical scenarios classified by management approach and required treatment*
| Spontaneous resolution | Cryotherapy | Cone biopsy | |
|---|---|---|---|
| Observation | Pap smear: low-grade abnormal | Pap smear: low-grade abnormal | Pap smear: low-grade abnormal |
| ↓ | ↓ | ↓ | |
| Pap smear: normal | Pap smear: low-grade abnormal | Pap smear: normal | |
| ↓ | ↓ | ↓ | |
| 2 Pap smears every 6 months: normal | Pap smear: low-grade abnormal | Pap smear: normal | |
| ↓ | ↓ | ||
| Pap smear: low-grade abnormal | Pap smear: normal | ||
| ↓ | ↓ | ||
| Colposcopy and biopsy at 1 month | Colposcopy and biopsy at 1 month | ||
| ↓ | ↓ | ||
| Biopsy: low-grade abnormal | Biopsy: abnormal with ? ECC | ||
| ↓ | ↓ | ||
| Cryotherapy at 1 month | Cone biopsy at 1 month: moderately abnoramal cells | ||
| ↓ | ↓ | ||
| 3 Pap smears every 6 months: normal | Cure with cone biopsy | ||
| ↓ | |||
| 3 Pap smears every 6 months: normal | |||
| Early colposcopy | Pap smear: low-grade abnormal | Pap smear: low-grade abnormal | Pap smear: low-grade abnormal |
| ↓ | ↓ | ↓ | |
| Colposcopy and biopsy at 1 month | Colposcopy and biopsy at 1 month | Colposcopy and biopsy at 1 month | |
| ↓ | ↓ | ↓ | |
| Biopsy: normal | Biopsy: abnormal with ? ECC | Biopsy: abnormal with ? ECC | |
| ↓ | ↓ | ↓ | |
| Second colposcopy and biopsy | Cone biopsy at 1 month | Cone biopsy at 1 month | |
| ↓ | ↓ | ↓ | |
| Biopsy: normal | Biopsy: moderately abnormal | Biopsy: moderately abnormal | |
| ↓ | ↓ | ↓ | |
| 2 Pap smears every 6 months: normal | Cure with cone biopsy | Cure with cone biopsy | |
| ↓ | ↓ | ↓ | |
| Pap smear: low-grade abnormal | Colposcopy: normal | Colposcopy: normal | |
| ↓ | ↓ | ↓ | |
| Colposcopy and biopsy at 1 month | 2 Pap smears every 6 months: normal | 2 Pap smears every 6 months: normal | |
| ↓ | |||
| Biopsy: low-grade abnormal | |||
| ↓ | |||
| Colposcopy: normal | |||
| ↓ | |||
| 2 Pap smears every 6 months: normal | |||
| *Intervals are 6 months unless specified otherwise. ECC, endocervical curettage. | |||
Standard gamble
Subjects were asked their preference between the certainty of the scenario under consideration and an uncertain prospect of either having cervical cancer treated by hysterectomy or full health. A probability wheel was used as visual aid.9 The probability of cervical cancer was altered until the subject was indifferent between the certain scenario and the uncertain prospect. Once all 6 scenarios had been scored, each subject was asked about her preference between the certainty of cervical cancer treated by hysterectomy and the uncertain prospect of immediate death or full health, using the same method.
At the end of the interview, both the subject and the interviewer completed evaluation forms including ratings of how well the subject understood the standard gamble rating exercises. Subject confusion was also defined a priori as those placing a higher utility on scenario 3 (observation for a long period followed by cone biopsy), which represented the longest period of uncertainty followed by the most invasive procedure, than on scenario 1 (a single mildly abnormal Pap smear evaluated by observation which then resolved spontaneously), which represented the absence of any invasive procedure.
Statistical analysis
Descriptive statistics were generated for ratings of each scenario for the entire group and with the confused subjects removed. Confused subjects included those who reported they found the interview “very confusing,” those who were recorded by the interviewer as finding the interview “very confusing,” and those whose rankings met the criteria for subject confusion, as described above. Means, standard deviations, medians, and percentiles were calculated for each scenario. The mean differences in adjusted standard gamble ratings between paired scenarios was evaluated using a t distribution. Multiple regression analyses were used to explore how much between-subject variation in the standard gamble scores was explained by the variables listed above.
A simple decision tree (Figure 1) was constructed to contrast preferences for an observational approach vs early colposcopy. Outcome probabilities were derived from meta-analyses of the medical literature,5 from observational data obtained at the same Northern California family planning clinics,10 and, for cone biopsy outcomes, from expert opinion obtained using a modified Delphi process.11 Utilities were assigned to the decision tree based on the standard gamble results. Women having 2 consecutive low-grade abnormal Pap results followed by a normal Pap result were assigned the same utility value as that for women with a single abnormal result. Analysis of the tree, including 1-way and 2-way sensitivity analysis of key variables, was conducted with Data 3.5.
Results
One hundred seventy interviews were completed. Characteristics of the interview subjects are shown in Table 2. A total of 22 subjects were designated “confused.” Analyses including the confused subjects did not alter the pattern of results, but the range in responses was larger. All analyses are presented here with confused subjects removed (n = 148).
Median ratings with 25th–75th percentiles for the paired scenarios rated by the standard gamble are shown as box plots in Figure 2. Mean adjusted scores, standard deviations, and mean differences in scores between paired scenarios are shown in Table 3. Notable findings include the following. (1) For each scenario, the range of responses by either rating method was very large. (2) Mean differences in utilities for observation vs early colposcopy were small. (3) For the paired scenarios in which the outcome was spontaneous resolution, observation was preferred (P = .01); in the paired scenarios in which the outcome was cryotherapy, early colposcopy was preferred (P = .02). (4) In the multiple regression analyses for each scenario, age, education, ethnicity, religiosity, and having known someone with cervical cancer together explained only a small amount of the variability between subjects (range for R2, .09–.22).
The decision model with baseline probabilities is shown in Figure 1. The model was simplified to exclude the outcome of cervical cancer, which is a very rare outcome for women with ASC or LSIL cervical smears who have adequate follow-up.5 In the baseline analysis, the overall utility of early colposcopy was slightly favored over the overall utility of the observation approach (utility of observation = 0.932; utility of early colposcopy = 0.940).
Sensitivity analysis examines the effect of varying elements of the model on the outcome. In sensitivity analyses of probabilities, the early colposcopy branch was favored, but the differences were small. The maximum difference in utilities between branches was 0.012 in these sensitivity analyses. In 1-way sensitivity analysis of branch utilities, threshold utility values to favor the observation branch were 0.986 for spontaneous resolution after observation and 0.898 for early colposcopy. Threshold values for cryotherapy were 0.938 for observation and 0.938 for early colposcopy.
TABLE 2
Characteristics of study subjects (n = 170)
| Characteristics | n (%) |
|---|---|
| Mean age (range), y | 26 (14–53) |
| Education | |
| Less than high school | 58 (34%) |
| High school | 77 (45%) |
| Some college | 35 (20%) |
| Ethnicity | |
| African American | 21 (12%) |
| Caucasian | 84 (49%) |
| Latina | 46 (27%) |
| Other | 21 (12%) |
| Interview language, Spanish | 15 (9%) |
| Prior colposcopy | 23 (14%) |
| Moderately or very religious | 64 (38%) |
| Knows someone with cervical cancer | 43 (25%) |
TABLE 3
Adjusted standard gamble values and paired differences* (n=148)
| Management Strategy | ||||
|---|---|---|---|---|
| Short-term outcome | Observation Mean (SD) | Early colposcopy Mean (SD) | Difference | P value (2 sided) |
| Spontaneous resolution | .96 ±..13) | .93±.20) | .03 ±..15) | .01 |
| Cryotherapy | .93 ±..17) | .95 ±..14) | -.02 ±.11) | .02 |
| Cone biopsy | .91 ±..21) | .92 ±..16) | -.02 ±..17) | .23 |
| *Adjusted to scale so that immediate death had a utility of 0 and “full health with all normal Pap smears” had a utility of 1. | ||||
FIGURE 1Decision model comparing observation with early colposcopy *
FIGURE 2Distribution of individual utilities as assessed by the standard gamble*
Discussion
We found wide variation in women’s preferences for management approaches to a low-grade abnormal Pap smear result. The range of responses was very large and the variation between individuals rating the same scenario was substantially greater than the variation in mean ratings between different scenarios. Measured subject characteristics explained only a small proportion of the observed variation, indicating that other unmeasured factors contributed substantially to the variation. Although 25% of subjects stated they knew someone with cervical cancer, this high percentage seems improbable and more likely reflects knowledge of someone who had an abnormal Pap smear.
The decision model displayed a small preference for immediate colposcopy. This may be related to preference for quicker resolution of the concern about cancer, although it involves more procedures. Small changes in utilities for spontaneous resolution and cryotherapy influenced the model to prefer observation. For cryotherapy, these utility values were within 1 standard deviation of the mean.
Our finding of a wide variation in preferences is supported by other patient preference studies,12-14 including 2 on this subject. Ferris et al assessed triage preferences for the evaluation and management ASC and LSIL.13 They used a questionnaire with a sample of 968 women who presented for care at obstetrics and gynecology and family practice clinics. They found that more women preferred repeat Pap smear when the index smear was ASC, and more women preferred colposcopy when the index smear was LSIL. Among a group of 136 Canadian women with atypia or LSIL referred for colposcopy, Meana et al found that 64% preferred early colposcopy, while 17% preferred observation and 17% had no strong preference.14
The factors contributing to patient preferences are complex. Differences in preferences may be influenced by knowledge and understanding of the disease and possible interventions, risk aversion, access to services, socioeconomics, cultural background, and other factors. While 1 patient may be most interested in establishing a definitive diagnosis and undergoing treatment as soon as possible, another may place priority on avoiding invasive or uncomfortable procedures. How differences in patient preferences influence clinical choices is highlighted by the work of Kuppermann et al.15 These investigators found that utilities for outcomes of prenatal diagnostic testing predicted subsequent testing behavior.
Our findings are limited by our use of a convenience sample of women attending family planning clinics. They may not be representative of women’s preferences in general, or even those of women attending family planning clinics. Outcomes in our study were specified during the preference assessment process; in real decision making, the outcome is always unknown at the time the decision is made. We did not include HPV typing as an option in our clinical scenarios. While HPV typing may have a role for triage of ASC,6,16 it appears not to be useful in management of LSIL.17
Cost-effectiveness analysis would offer important information about which management approach might be favored in the context of resource allocation. For decision making by individual patients and doctors, however, decision analysis is often more relevant. In this case, the “preferred” decision is very sensitive to patient utilities, emphasizing the need for clear physician-patient communication.
Strengths of our study include the diversity of the subjects, the formal process for preference assessment, and the paired scenarios, which allow assessment of preferences for a single management decision, in which 2 separate paths lead to an equivalent ultimate outcome. Our findings are consistent with previous work showing that the sequence of events leading to an outcome will influence utilities for the outcome.18
Application to clinical practice
How might our findings be translated into clinical practice? In clinical situations where different approaches to management are unlikely to result in substantial outcome differences (a “toss-up”), patient preferences are a key aspect of the decision-making process.19 For women with lowgrade Pap abnormalities, several diagnostic options are available and no single option is strongly supported by evidence to offer better outcomes. Our study indicates that no single option is preferred by most women. Under these conditions, engaging the patient in the decision-making process may produce better health outcomes.20 Clinicians should anticipate highly varied preferences, and will need to adopt a flexible approach. Not all patients will want to be actively involved in the decision process, but the desire for information is nearly universal. Flexible use of the questions in Table 4 may help patients to define their preferences and will likely improve their satisfaction and adherence to the treatment plan.
TABLE 4
Questions for patients with an abnormal Pap smear
| What is your understanding of what it means for you to have an abnormal Pap smear showing _____________? |
| There are different options for the next step. Would you like to be involved in deciding which option is preferred for your case? |
| What questions do you have about these options? |
| How important is it to you to have a definite answer as soon as possible? |
| How do you feel about undergoing colposcopy? |
| Would you prefer to have a follow-up Pap smear in ____ months, which might avoid a colposcopy, or would you prefer to have a colposcopy sooner? |
· Acknowledgments ·
The authors thank the staff of Planned Parenthood Mar Monte East for their assistance with subject recruitment and interviews.
- Any of several approaches may be used in managing women who have low-grade Pap smear abnormalities.
- Women’s preferences for a particular management approach to an abnormal Pap smear vary widely.
- Asking patients specific questions about their desire to avoid procedures and tolerance for uncertainty may help to clarify preferences.
The management of women who have low-grade cytologic abnormalities—including atypical squamous cells (ASC) and low-grade squamous intraepithelial lesions (LSIL)—is controversial.1-4 Without strong evidence favoring a single approach, some clinicians recommend immediate colposcopy to obtain a definitive diagnosis and to exclude the presence of a high-grade lesion, while others recommend observation with serial Pap smears, given the tendency for many low-grade lesions to regress spontaneously.5,6 Immediate colposcopy has the advantage of giving a patient a relatively rapid assessment of the nature and extent of her cervical dysplasia; however, the procedure is uncomfortable, and overall management may not be affected. Observation with serial Pap smears may avoid an invasive procedure, but it may also cause anxiety as time passes without a definitive diagnosis.
Eliciting and understanding patient preferences is an important part of clinical decision making. The clinician provides the best available information on the probability of clinical outcomes and the implications of each for the patient’s health. But only the patient knows what these outcomes mean to her well-being (also called “utility”).
Given the clinical disagreement over how to proceed with abnormal ASC and LSIL Pap smear results, the decision should be influenced by a patient’s preference, informed by knowledge of outcomes and costs of alternative approaches. It is unclear which approach women prefer, and whether women’s preferences for specific protocols are associated with sociodemographic characteristics. To understand better how women weigh these trade-offs, we evaluated the preferences of a diverse group of women for contrasting management approaches to the evaluation of a hypothetical low-grade abnormal Pap smear result.
Methods
Study population
Study participants were recruited from the waiting rooms of 5 family planning clinics in Northern California’s Central Valley. Women were eligible for the study if they were 18 years of age or older, or, if minors, they were emancipated and could thus provide informed consent. Potential subjects were excluded if they spoke neither English nor Spanish or if they had never had a Pap smear. The study protocol and informed consent procedures were reviewed and approved by the University of California, Davis, Human Subjects Committee.
Instruments and outcome measures
Interviews were conducted in English or Spanish. Information regarding demographic characteristics, level of education, past experiences with abnormal Pap smears and cervical cancer, and self-rated religiosity was collected with a self-administered questionnaire. The primary outcome measures were utilities (quantified preferences for specific health states) for 6 different scenarios. These were assessed by the standard gamble (SG) method, described in more detail below.7
Possible utility scores range from 0 to 1. A score of 0 represents immediate death; a score of 1 represents full (or ideal) health for the rest of one’s life. Because the scenarios under consideration in this study did not involve any meaningful level of risk of death, we expected utility scores for the scenarios to cluster toward the upper end of the scale. As a result, a measurement instrument based on an “immediate death” versus “full health” scale would be unable to discriminate between different scenarios. To avoid this problem, a scale was used in which the lower end point was a non-death state unambiguously less preferred than each of the scenarios under consideration.8 We used “invasive cervical cancer requiring hysterectomy” as the lower end point (utility of 0) contrasted with “full health with all normal Pap smears” (utility of 1) to generate the original score (SG Dys). In a separate standard gamble, subjects rated invasive cervical cancer versus immediate death (SG Ca), so that all utilities could be converted to the standard scale, using the formula: (1 – SG Ca) (SG Dys) + SG Ca.
The 6 scenarios rated in the study are shown in Table 1. The scenarios represent 3 sets of progressively more invasive interventions for a low-grade abnormal Pap smear: (1) resolution, representing spontaneous regression with treatment not required; (2) a low-grade abnormality requiring treatment with cryotherapy; (3) a more severe abnormality requiring a cervical cone biopsy. Following either spontaneous resolution or treatment, all scenarios assumed the abnormality was resolved. For each of the 3 results, a management strategy based on observation with serial Pap smears was applied in 1 instance, and a strategy of early colposcopy was applied in the other instance, resulting in 6 different pathways to the ultimate outcome; a normal Pap smear. The time frame for these scenarios was 18–36 months.
Trained interviewers used a standardized approach to elicit preferences from each subject. Subjects were read a description of all the procedures involved in the scenarios. Descriptions were accompanied by cards summarizing each procedure in pictures and words, and included information about the possibility of progression and spontaneous regression of the Pap smear abnormality. Subjects were encouraged to ask questions at any point during the interview. Procedure descriptions are available from the authors on request.
TABLE 1
Clinical scenarios classified by management approach and required treatment*
| Spontaneous resolution | Cryotherapy | Cone biopsy | |
|---|---|---|---|
| Observation | Pap smear: low-grade abnormal | Pap smear: low-grade abnormal | Pap smear: low-grade abnormal |
| ↓ | ↓ | ↓ | |
| Pap smear: normal | Pap smear: low-grade abnormal | Pap smear: normal | |
| ↓ | ↓ | ↓ | |
| 2 Pap smears every 6 months: normal | Pap smear: low-grade abnormal | Pap smear: normal | |
| ↓ | ↓ | ||
| Pap smear: low-grade abnormal | Pap smear: normal | ||
| ↓ | ↓ | ||
| Colposcopy and biopsy at 1 month | Colposcopy and biopsy at 1 month | ||
| ↓ | ↓ | ||
| Biopsy: low-grade abnormal | Biopsy: abnormal with ? ECC | ||
| ↓ | ↓ | ||
| Cryotherapy at 1 month | Cone biopsy at 1 month: moderately abnoramal cells | ||
| ↓ | ↓ | ||
| 3 Pap smears every 6 months: normal | Cure with cone biopsy | ||
| ↓ | |||
| 3 Pap smears every 6 months: normal | |||
| Early colposcopy | Pap smear: low-grade abnormal | Pap smear: low-grade abnormal | Pap smear: low-grade abnormal |
| ↓ | ↓ | ↓ | |
| Colposcopy and biopsy at 1 month | Colposcopy and biopsy at 1 month | Colposcopy and biopsy at 1 month | |
| ↓ | ↓ | ↓ | |
| Biopsy: normal | Biopsy: abnormal with ? ECC | Biopsy: abnormal with ? ECC | |
| ↓ | ↓ | ↓ | |
| Second colposcopy and biopsy | Cone biopsy at 1 month | Cone biopsy at 1 month | |
| ↓ | ↓ | ↓ | |
| Biopsy: normal | Biopsy: moderately abnormal | Biopsy: moderately abnormal | |
| ↓ | ↓ | ↓ | |
| 2 Pap smears every 6 months: normal | Cure with cone biopsy | Cure with cone biopsy | |
| ↓ | ↓ | ↓ | |
| Pap smear: low-grade abnormal | Colposcopy: normal | Colposcopy: normal | |
| ↓ | ↓ | ↓ | |
| Colposcopy and biopsy at 1 month | 2 Pap smears every 6 months: normal | 2 Pap smears every 6 months: normal | |
| ↓ | |||
| Biopsy: low-grade abnormal | |||
| ↓ | |||
| Colposcopy: normal | |||
| ↓ | |||
| 2 Pap smears every 6 months: normal | |||
| *Intervals are 6 months unless specified otherwise. ECC, endocervical curettage. | |||
Standard gamble
Subjects were asked their preference between the certainty of the scenario under consideration and an uncertain prospect of either having cervical cancer treated by hysterectomy or full health. A probability wheel was used as visual aid.9 The probability of cervical cancer was altered until the subject was indifferent between the certain scenario and the uncertain prospect. Once all 6 scenarios had been scored, each subject was asked about her preference between the certainty of cervical cancer treated by hysterectomy and the uncertain prospect of immediate death or full health, using the same method.
At the end of the interview, both the subject and the interviewer completed evaluation forms including ratings of how well the subject understood the standard gamble rating exercises. Subject confusion was also defined a priori as those placing a higher utility on scenario 3 (observation for a long period followed by cone biopsy), which represented the longest period of uncertainty followed by the most invasive procedure, than on scenario 1 (a single mildly abnormal Pap smear evaluated by observation which then resolved spontaneously), which represented the absence of any invasive procedure.
Statistical analysis
Descriptive statistics were generated for ratings of each scenario for the entire group and with the confused subjects removed. Confused subjects included those who reported they found the interview “very confusing,” those who were recorded by the interviewer as finding the interview “very confusing,” and those whose rankings met the criteria for subject confusion, as described above. Means, standard deviations, medians, and percentiles were calculated for each scenario. The mean differences in adjusted standard gamble ratings between paired scenarios was evaluated using a t distribution. Multiple regression analyses were used to explore how much between-subject variation in the standard gamble scores was explained by the variables listed above.
A simple decision tree (Figure 1) was constructed to contrast preferences for an observational approach vs early colposcopy. Outcome probabilities were derived from meta-analyses of the medical literature,5 from observational data obtained at the same Northern California family planning clinics,10 and, for cone biopsy outcomes, from expert opinion obtained using a modified Delphi process.11 Utilities were assigned to the decision tree based on the standard gamble results. Women having 2 consecutive low-grade abnormal Pap results followed by a normal Pap result were assigned the same utility value as that for women with a single abnormal result. Analysis of the tree, including 1-way and 2-way sensitivity analysis of key variables, was conducted with Data 3.5.
Results
One hundred seventy interviews were completed. Characteristics of the interview subjects are shown in Table 2. A total of 22 subjects were designated “confused.” Analyses including the confused subjects did not alter the pattern of results, but the range in responses was larger. All analyses are presented here with confused subjects removed (n = 148).
Median ratings with 25th–75th percentiles for the paired scenarios rated by the standard gamble are shown as box plots in Figure 2. Mean adjusted scores, standard deviations, and mean differences in scores between paired scenarios are shown in Table 3. Notable findings include the following. (1) For each scenario, the range of responses by either rating method was very large. (2) Mean differences in utilities for observation vs early colposcopy were small. (3) For the paired scenarios in which the outcome was spontaneous resolution, observation was preferred (P = .01); in the paired scenarios in which the outcome was cryotherapy, early colposcopy was preferred (P = .02). (4) In the multiple regression analyses for each scenario, age, education, ethnicity, religiosity, and having known someone with cervical cancer together explained only a small amount of the variability between subjects (range for R2, .09–.22).
The decision model with baseline probabilities is shown in Figure 1. The model was simplified to exclude the outcome of cervical cancer, which is a very rare outcome for women with ASC or LSIL cervical smears who have adequate follow-up.5 In the baseline analysis, the overall utility of early colposcopy was slightly favored over the overall utility of the observation approach (utility of observation = 0.932; utility of early colposcopy = 0.940).
Sensitivity analysis examines the effect of varying elements of the model on the outcome. In sensitivity analyses of probabilities, the early colposcopy branch was favored, but the differences were small. The maximum difference in utilities between branches was 0.012 in these sensitivity analyses. In 1-way sensitivity analysis of branch utilities, threshold utility values to favor the observation branch were 0.986 for spontaneous resolution after observation and 0.898 for early colposcopy. Threshold values for cryotherapy were 0.938 for observation and 0.938 for early colposcopy.
TABLE 2
Characteristics of study subjects (n = 170)
| Characteristics | n (%) |
|---|---|
| Mean age (range), y | 26 (14–53) |
| Education | |
| Less than high school | 58 (34%) |
| High school | 77 (45%) |
| Some college | 35 (20%) |
| Ethnicity | |
| African American | 21 (12%) |
| Caucasian | 84 (49%) |
| Latina | 46 (27%) |
| Other | 21 (12%) |
| Interview language, Spanish | 15 (9%) |
| Prior colposcopy | 23 (14%) |
| Moderately or very religious | 64 (38%) |
| Knows someone with cervical cancer | 43 (25%) |
TABLE 3
Adjusted standard gamble values and paired differences* (n=148)
| Management Strategy | ||||
|---|---|---|---|---|
| Short-term outcome | Observation Mean (SD) | Early colposcopy Mean (SD) | Difference | P value (2 sided) |
| Spontaneous resolution | .96 ±..13) | .93±.20) | .03 ±..15) | .01 |
| Cryotherapy | .93 ±..17) | .95 ±..14) | -.02 ±.11) | .02 |
| Cone biopsy | .91 ±..21) | .92 ±..16) | -.02 ±..17) | .23 |
| *Adjusted to scale so that immediate death had a utility of 0 and “full health with all normal Pap smears” had a utility of 1. | ||||
FIGURE 1Decision model comparing observation with early colposcopy *
FIGURE 2Distribution of individual utilities as assessed by the standard gamble*
Discussion
We found wide variation in women’s preferences for management approaches to a low-grade abnormal Pap smear result. The range of responses was very large and the variation between individuals rating the same scenario was substantially greater than the variation in mean ratings between different scenarios. Measured subject characteristics explained only a small proportion of the observed variation, indicating that other unmeasured factors contributed substantially to the variation. Although 25% of subjects stated they knew someone with cervical cancer, this high percentage seems improbable and more likely reflects knowledge of someone who had an abnormal Pap smear.
The decision model displayed a small preference for immediate colposcopy. This may be related to preference for quicker resolution of the concern about cancer, although it involves more procedures. Small changes in utilities for spontaneous resolution and cryotherapy influenced the model to prefer observation. For cryotherapy, these utility values were within 1 standard deviation of the mean.
Our finding of a wide variation in preferences is supported by other patient preference studies,12-14 including 2 on this subject. Ferris et al assessed triage preferences for the evaluation and management ASC and LSIL.13 They used a questionnaire with a sample of 968 women who presented for care at obstetrics and gynecology and family practice clinics. They found that more women preferred repeat Pap smear when the index smear was ASC, and more women preferred colposcopy when the index smear was LSIL. Among a group of 136 Canadian women with atypia or LSIL referred for colposcopy, Meana et al found that 64% preferred early colposcopy, while 17% preferred observation and 17% had no strong preference.14
The factors contributing to patient preferences are complex. Differences in preferences may be influenced by knowledge and understanding of the disease and possible interventions, risk aversion, access to services, socioeconomics, cultural background, and other factors. While 1 patient may be most interested in establishing a definitive diagnosis and undergoing treatment as soon as possible, another may place priority on avoiding invasive or uncomfortable procedures. How differences in patient preferences influence clinical choices is highlighted by the work of Kuppermann et al.15 These investigators found that utilities for outcomes of prenatal diagnostic testing predicted subsequent testing behavior.
Our findings are limited by our use of a convenience sample of women attending family planning clinics. They may not be representative of women’s preferences in general, or even those of women attending family planning clinics. Outcomes in our study were specified during the preference assessment process; in real decision making, the outcome is always unknown at the time the decision is made. We did not include HPV typing as an option in our clinical scenarios. While HPV typing may have a role for triage of ASC,6,16 it appears not to be useful in management of LSIL.17
Cost-effectiveness analysis would offer important information about which management approach might be favored in the context of resource allocation. For decision making by individual patients and doctors, however, decision analysis is often more relevant. In this case, the “preferred” decision is very sensitive to patient utilities, emphasizing the need for clear physician-patient communication.
Strengths of our study include the diversity of the subjects, the formal process for preference assessment, and the paired scenarios, which allow assessment of preferences for a single management decision, in which 2 separate paths lead to an equivalent ultimate outcome. Our findings are consistent with previous work showing that the sequence of events leading to an outcome will influence utilities for the outcome.18
Application to clinical practice
How might our findings be translated into clinical practice? In clinical situations where different approaches to management are unlikely to result in substantial outcome differences (a “toss-up”), patient preferences are a key aspect of the decision-making process.19 For women with lowgrade Pap abnormalities, several diagnostic options are available and no single option is strongly supported by evidence to offer better outcomes. Our study indicates that no single option is preferred by most women. Under these conditions, engaging the patient in the decision-making process may produce better health outcomes.20 Clinicians should anticipate highly varied preferences, and will need to adopt a flexible approach. Not all patients will want to be actively involved in the decision process, but the desire for information is nearly universal. Flexible use of the questions in Table 4 may help patients to define their preferences and will likely improve their satisfaction and adherence to the treatment plan.
TABLE 4
Questions for patients with an abnormal Pap smear
| What is your understanding of what it means for you to have an abnormal Pap smear showing _____________? |
| There are different options for the next step. Would you like to be involved in deciding which option is preferred for your case? |
| What questions do you have about these options? |
| How important is it to you to have a definite answer as soon as possible? |
| How do you feel about undergoing colposcopy? |
| Would you prefer to have a follow-up Pap smear in ____ months, which might avoid a colposcopy, or would you prefer to have a colposcopy sooner? |
· Acknowledgments ·
The authors thank the staff of Planned Parenthood Mar Monte East for their assistance with subject recruitment and interviews.
1. Woolf SH. Screening for cervical cancer. In: Goldbloom RB, Lawrence RS, eds. Preventing disease: beyond the rhetoric. New York: Spring-Verlag, 1990:319–23.
2. Kurman RJ, Henson DE, Herbst AL, Noller KL, Schiffman MH. Interim guidelines for management of abnormal cervical cytology. The 1992 National Cancer Institute Workshop. JAMA 1994;271:1866-69.
3. Miller AB, Anderson G, Brisson J, Laidlaw J, Le Pitre N, Malcolmson P, et al. Report of a national workshop on screening for cancer of the cervix. Can Med Assoc J 1991;145:1301-25.
4. American College of Obstetricians and Gynecologists. Cervical cytology: evaluation and management of abnormalities. ACOG technical bulletin no. 183. Washington, DC: American College of Obstetricians and Gynecologists, 1993.
5. Melnikow J, Nuovo J, Willan AR, Chan BK, Howell LP. Natural history of cervical squamous intraepithelial lesions: A meta-analysis. Obstet Gynecol 1998;92:727-34.
6. Wright TC, Cox TJ, Massad LS, Twiggs LB, Wilkonson EJ. Consensus guidelines for the management of women with cervical cytological abnormalities. JAMA 2002;287:2120-29.
7. Drummond MF, O’Brien BJ, Stoddart GL, Torrance GW, eds. Methods for the economic evaluation of health care programs. 2nd edition. New York: Oxford University Press, 1997.
8. Torrance G. Measurement of health state utilities for economic appraisal: A review. J Health Econ., 1986;5:1-30.
9. Furlong W, Feeny D, Torrance GW, Barr R, Horsman J. Guide to design and development of health state utility instrumentation. Centre for Health Economics and Policy Development. Working Paper Series # 90-9. Hamilton, McMaster University, 1990.
10. Melnikow J, Nuovo J, Paliescheskey M, Stewart GK, Howell L, Green B. Detection of high grade cervical dysplasia: Impact of age and Bethesda system-related follow-up criteria. Diagnostic Cytopathol 1997;17:321-25.
11. Fink A, Kosecoff J, Chassin M, Brook RH. Consensus methods: Characteristics and guidelines for use. Am J Pub Health 1984;74:979-83.
12. Nease RF, Kneeland T, O’Connor GT, Sumner W, Lumpkins C, Shaw L, et al. Variation in patient utilities for outcomes of the management of chronic stable angina. JAMA 1995;273:1185-90.
13. Ferris DG, Kriegel D, Cole L, Litaker M, Woodward L. Women’s triage and management p for cervical cytologic reports demonstrating atypical squamous cells of undetermined significance and low grade squamous intraepithelial lesions. Arch Fam Med 1997;6:348-53.
14. Meana M, Steward DE, Lickrish GM, Murphy J, Rosen B. Patient preference for the management of midly abnormal Papanicolaou smears. J Women’s Health and Gender Based Medicine 1999;8:941-7.
15. Kuppermann M, Nease RF, Learman LA, Gates E, Posner SF, Washington AE. How do women value Down syndrome-affected birth and miscarriage? The thirty-five-year-old question. Decis Making 1998;18:468.-
16. Solomon D, Schiffman M, Tarone R. Comparison of three management strategies for patients with atypical squamous cells of undetermined significance: baseline results from a randomized trial. J Natl Cancer Inst 2001;93(4):252-3.
17. The atypical squamous cells of undetermined significance/low grade squamous intraepithelial lesions triage study (ALTS) group. Human papillomavirus testing for triage of women with cytologic evidence of low-grade squamous intra-epithelial lesions: baseline data from a randomized trial. J Natl Cancer Inst,. 2000;92:397-402.
18. Kuppermann M, Shiboski S, Feeny D, Elkin E, Washington AE. Can preference scores for discrete states be used to derive preference scores for an entire path of events? An application to prenatal diagnosis. Med Decis Making 1997;17:42-55.
19. Kassirer JP, Pauker SG. The toss up. N Engl J Med 1981;305:1457-9.
20. Kaplan SH, Greenfield S, Ware JE, Jr. Assessing the effects of physician patient interactions on the outcomes of care. Med Care 1989;27 (Suppl 3):S110-27.
1. Woolf SH. Screening for cervical cancer. In: Goldbloom RB, Lawrence RS, eds. Preventing disease: beyond the rhetoric. New York: Spring-Verlag, 1990:319–23.
2. Kurman RJ, Henson DE, Herbst AL, Noller KL, Schiffman MH. Interim guidelines for management of abnormal cervical cytology. The 1992 National Cancer Institute Workshop. JAMA 1994;271:1866-69.
3. Miller AB, Anderson G, Brisson J, Laidlaw J, Le Pitre N, Malcolmson P, et al. Report of a national workshop on screening for cancer of the cervix. Can Med Assoc J 1991;145:1301-25.
4. American College of Obstetricians and Gynecologists. Cervical cytology: evaluation and management of abnormalities. ACOG technical bulletin no. 183. Washington, DC: American College of Obstetricians and Gynecologists, 1993.
5. Melnikow J, Nuovo J, Willan AR, Chan BK, Howell LP. Natural history of cervical squamous intraepithelial lesions: A meta-analysis. Obstet Gynecol 1998;92:727-34.
6. Wright TC, Cox TJ, Massad LS, Twiggs LB, Wilkonson EJ. Consensus guidelines for the management of women with cervical cytological abnormalities. JAMA 2002;287:2120-29.
7. Drummond MF, O’Brien BJ, Stoddart GL, Torrance GW, eds. Methods for the economic evaluation of health care programs. 2nd edition. New York: Oxford University Press, 1997.
8. Torrance G. Measurement of health state utilities for economic appraisal: A review. J Health Econ., 1986;5:1-30.
9. Furlong W, Feeny D, Torrance GW, Barr R, Horsman J. Guide to design and development of health state utility instrumentation. Centre for Health Economics and Policy Development. Working Paper Series # 90-9. Hamilton, McMaster University, 1990.
10. Melnikow J, Nuovo J, Paliescheskey M, Stewart GK, Howell L, Green B. Detection of high grade cervical dysplasia: Impact of age and Bethesda system-related follow-up criteria. Diagnostic Cytopathol 1997;17:321-25.
11. Fink A, Kosecoff J, Chassin M, Brook RH. Consensus methods: Characteristics and guidelines for use. Am J Pub Health 1984;74:979-83.
12. Nease RF, Kneeland T, O’Connor GT, Sumner W, Lumpkins C, Shaw L, et al. Variation in patient utilities for outcomes of the management of chronic stable angina. JAMA 1995;273:1185-90.
13. Ferris DG, Kriegel D, Cole L, Litaker M, Woodward L. Women’s triage and management p for cervical cytologic reports demonstrating atypical squamous cells of undetermined significance and low grade squamous intraepithelial lesions. Arch Fam Med 1997;6:348-53.
14. Meana M, Steward DE, Lickrish GM, Murphy J, Rosen B. Patient preference for the management of midly abnormal Papanicolaou smears. J Women’s Health and Gender Based Medicine 1999;8:941-7.
15. Kuppermann M, Nease RF, Learman LA, Gates E, Posner SF, Washington AE. How do women value Down syndrome-affected birth and miscarriage? The thirty-five-year-old question. Decis Making 1998;18:468.-
16. Solomon D, Schiffman M, Tarone R. Comparison of three management strategies for patients with atypical squamous cells of undetermined significance: baseline results from a randomized trial. J Natl Cancer Inst 2001;93(4):252-3.
17. The atypical squamous cells of undetermined significance/low grade squamous intraepithelial lesions triage study (ALTS) group. Human papillomavirus testing for triage of women with cytologic evidence of low-grade squamous intra-epithelial lesions: baseline data from a randomized trial. J Natl Cancer Inst,. 2000;92:397-402.
18. Kuppermann M, Shiboski S, Feeny D, Elkin E, Washington AE. Can preference scores for discrete states be used to derive preference scores for an entire path of events? An application to prenatal diagnosis. Med Decis Making 1997;17:42-55.
19. Kassirer JP, Pauker SG. The toss up. N Engl J Med 1981;305:1457-9.
20. Kaplan SH, Greenfield S, Ware JE, Jr. Assessing the effects of physician patient interactions on the outcomes of care. Med Care 1989;27 (Suppl 3):S110-27.