User login
Use PRESS to craft a concise psychodynamic formulation
More and more time is being allocated to training psychiatric residents in cognitive-behavioral therapy and crafting a cognitive-behavioral formulation. However, the psychodynamic formulation, once considered the backbone of psychiatry, should not be forgotten. The psychodynamic formulation is a cohesive portrait of an individual’s inner world based on the biopsychosocial approach.1 The purpose in crafting a psychodynamic formulation is to create a succinct and focused case conceptualization that can guide treatment and anticipate possible outcomes.2,3 To teach this in a simple, practical, and relatable way, we propose an approach that can be summarized with the acronym PRESS.
Psychologically minded
Can the patient be introspective and contemplate his (her) thoughts and feelings before acting? Without the capacity to look within—distinct from intelligence—a patient could struggle with the psychodynamic approach and could benefit from a more supportive form of psychotherapy.4
Relationships
Examine the patient’s relationships with others:
• Who are the prominent people in his (her) life?
• What are his interpersonal relations like?
• How does he (she) recall important relationships from the past?
• Do these relationships appear to be recurring?4
Just as themes and patterns recur, so do relationships. Predict how the patient’s relationship pattern could be recreated in the therapeutic dynamic and how this could influence treatment. Then, by examining this transference and countertransference data, you can illustrate a pattern from past relationships that is being recreated in the doctor-patient relationship.3,5
Ego strength
Determining how the patient expresses or inhibits wishes and exhibits impulse control can shed light onto how he operates on a daily basis:
• Does he have the ability to regulate his impulses?
• Is he capable of anticipating the consequences of inappropriate action?
• Does he show a lack of insight and judgment by exhibiting too many repetitive maladaptive behaviors?
Additionally, how does the patient keep unwanted fantasies, wishes, and memories out of conscious awareness?
Identifying which constellation of defense mechanisms the patient is using can help categorize his level of functioning and personality type, and identify anxiety-provoking thoughts and events.1,6 Often, one of these situations has consciously or subconsciously triggered the need for psychotherapy.
Stimulus
The hallmark of any psychodynamic formulation starts with a concise summarizing statement that describes the fundamental details about the patient and his motivation for treatment.2 Determining the patient’s impetus for treatment is 2-fold: Why does the patient want to receive treatment? Why now?
Superego
Review the patient’s ego ideal—what one should not do—and the moral conscience— what one should do.1 Do there seem to be any deficits (recurrent shoplifting, criminality, etc.)? Who contributed to his sense of right and wrong, and how harsh or lax is it? Is the patient self-defeating or self-punishing? Contrarily, does the patient seem to have little conscience?
Acknowledgment
Franklin Maleson, MD, provided advice and input to the authors.
Disclosures
The authors report no financial relationships with any companies whose products are mentioned in this article or with manufacturers of competing products.
1. Gabbard GO. Long-term psychodynamic psychotherapy: a basic text. Arlington, VA: American Psychiatric Publishing; 2010.
2. Perry S, Cooper AM, Michels R. The psychodynamic formulation: its purpose, structure, and clinical application. Am J Psychiatry. 1987;144(5):543-550.
3. Kassaw K, Gabbard GO. Creating a psychodynamic formulation from a clinical evaluation. Am J Psychiatry. 2002;159(5):721-726.
4. Ursano RJ, Sonnenberg SM, Lazar SG. Concise guide to psychodynamic psychotherapy. Arlington, VA: American Psychiatric Publishing; 2004.
5. Faden J, McFadden RF. The avoidant psychotherapy patient. Current Psychiatry. 2012;11(8):44-47,A.
6. Blackman JS. 101 Defenses: how the mind shields itself. New York, NY: Brunner-Routledge; 2004.
More and more time is being allocated to training psychiatric residents in cognitive-behavioral therapy and crafting a cognitive-behavioral formulation. However, the psychodynamic formulation, once considered the backbone of psychiatry, should not be forgotten. The psychodynamic formulation is a cohesive portrait of an individual’s inner world based on the biopsychosocial approach.1 The purpose in crafting a psychodynamic formulation is to create a succinct and focused case conceptualization that can guide treatment and anticipate possible outcomes.2,3 To teach this in a simple, practical, and relatable way, we propose an approach that can be summarized with the acronym PRESS.
Psychologically minded
Can the patient be introspective and contemplate his (her) thoughts and feelings before acting? Without the capacity to look within—distinct from intelligence—a patient could struggle with the psychodynamic approach and could benefit from a more supportive form of psychotherapy.4
Relationships
Examine the patient’s relationships with others:
• Who are the prominent people in his (her) life?
• What are his interpersonal relations like?
• How does he (she) recall important relationships from the past?
• Do these relationships appear to be recurring?4
Just as themes and patterns recur, so do relationships. Predict how the patient’s relationship pattern could be recreated in the therapeutic dynamic and how this could influence treatment. Then, by examining this transference and countertransference data, you can illustrate a pattern from past relationships that is being recreated in the doctor-patient relationship.3,5
Ego strength
Determining how the patient expresses or inhibits wishes and exhibits impulse control can shed light onto how he operates on a daily basis:
• Does he have the ability to regulate his impulses?
• Is he capable of anticipating the consequences of inappropriate action?
• Does he show a lack of insight and judgment by exhibiting too many repetitive maladaptive behaviors?
Additionally, how does the patient keep unwanted fantasies, wishes, and memories out of conscious awareness?
Identifying which constellation of defense mechanisms the patient is using can help categorize his level of functioning and personality type, and identify anxiety-provoking thoughts and events.1,6 Often, one of these situations has consciously or subconsciously triggered the need for psychotherapy.
Stimulus
The hallmark of any psychodynamic formulation starts with a concise summarizing statement that describes the fundamental details about the patient and his motivation for treatment.2 Determining the patient’s impetus for treatment is 2-fold: Why does the patient want to receive treatment? Why now?
Superego
Review the patient’s ego ideal—what one should not do—and the moral conscience— what one should do.1 Do there seem to be any deficits (recurrent shoplifting, criminality, etc.)? Who contributed to his sense of right and wrong, and how harsh or lax is it? Is the patient self-defeating or self-punishing? Contrarily, does the patient seem to have little conscience?
Acknowledgment
Franklin Maleson, MD, provided advice and input to the authors.
Disclosures
The authors report no financial relationships with any companies whose products are mentioned in this article or with manufacturers of competing products.
More and more time is being allocated to training psychiatric residents in cognitive-behavioral therapy and crafting a cognitive-behavioral formulation. However, the psychodynamic formulation, once considered the backbone of psychiatry, should not be forgotten. The psychodynamic formulation is a cohesive portrait of an individual’s inner world based on the biopsychosocial approach.1 The purpose in crafting a psychodynamic formulation is to create a succinct and focused case conceptualization that can guide treatment and anticipate possible outcomes.2,3 To teach this in a simple, practical, and relatable way, we propose an approach that can be summarized with the acronym PRESS.
Psychologically minded
Can the patient be introspective and contemplate his (her) thoughts and feelings before acting? Without the capacity to look within—distinct from intelligence—a patient could struggle with the psychodynamic approach and could benefit from a more supportive form of psychotherapy.4
Relationships
Examine the patient’s relationships with others:
• Who are the prominent people in his (her) life?
• What are his interpersonal relations like?
• How does he (she) recall important relationships from the past?
• Do these relationships appear to be recurring?4
Just as themes and patterns recur, so do relationships. Predict how the patient’s relationship pattern could be recreated in the therapeutic dynamic and how this could influence treatment. Then, by examining this transference and countertransference data, you can illustrate a pattern from past relationships that is being recreated in the doctor-patient relationship.3,5
Ego strength
Determining how the patient expresses or inhibits wishes and exhibits impulse control can shed light onto how he operates on a daily basis:
• Does he have the ability to regulate his impulses?
• Is he capable of anticipating the consequences of inappropriate action?
• Does he show a lack of insight and judgment by exhibiting too many repetitive maladaptive behaviors?
Additionally, how does the patient keep unwanted fantasies, wishes, and memories out of conscious awareness?
Identifying which constellation of defense mechanisms the patient is using can help categorize his level of functioning and personality type, and identify anxiety-provoking thoughts and events.1,6 Often, one of these situations has consciously or subconsciously triggered the need for psychotherapy.
Stimulus
The hallmark of any psychodynamic formulation starts with a concise summarizing statement that describes the fundamental details about the patient and his motivation for treatment.2 Determining the patient’s impetus for treatment is 2-fold: Why does the patient want to receive treatment? Why now?
Superego
Review the patient’s ego ideal—what one should not do—and the moral conscience— what one should do.1 Do there seem to be any deficits (recurrent shoplifting, criminality, etc.)? Who contributed to his sense of right and wrong, and how harsh or lax is it? Is the patient self-defeating or self-punishing? Contrarily, does the patient seem to have little conscience?
Acknowledgment
Franklin Maleson, MD, provided advice and input to the authors.
Disclosures
The authors report no financial relationships with any companies whose products are mentioned in this article or with manufacturers of competing products.
1. Gabbard GO. Long-term psychodynamic psychotherapy: a basic text. Arlington, VA: American Psychiatric Publishing; 2010.
2. Perry S, Cooper AM, Michels R. The psychodynamic formulation: its purpose, structure, and clinical application. Am J Psychiatry. 1987;144(5):543-550.
3. Kassaw K, Gabbard GO. Creating a psychodynamic formulation from a clinical evaluation. Am J Psychiatry. 2002;159(5):721-726.
4. Ursano RJ, Sonnenberg SM, Lazar SG. Concise guide to psychodynamic psychotherapy. Arlington, VA: American Psychiatric Publishing; 2004.
5. Faden J, McFadden RF. The avoidant psychotherapy patient. Current Psychiatry. 2012;11(8):44-47,A.
6. Blackman JS. 101 Defenses: how the mind shields itself. New York, NY: Brunner-Routledge; 2004.
1. Gabbard GO. Long-term psychodynamic psychotherapy: a basic text. Arlington, VA: American Psychiatric Publishing; 2010.
2. Perry S, Cooper AM, Michels R. The psychodynamic formulation: its purpose, structure, and clinical application. Am J Psychiatry. 1987;144(5):543-550.
3. Kassaw K, Gabbard GO. Creating a psychodynamic formulation from a clinical evaluation. Am J Psychiatry. 2002;159(5):721-726.
4. Ursano RJ, Sonnenberg SM, Lazar SG. Concise guide to psychodynamic psychotherapy. Arlington, VA: American Psychiatric Publishing; 2004.
5. Faden J, McFadden RF. The avoidant psychotherapy patient. Current Psychiatry. 2012;11(8):44-47,A.
6. Blackman JS. 101 Defenses: how the mind shields itself. New York, NY: Brunner-Routledge; 2004.
6 ‘D’s: Next steps after an insufficient antipsychotic response
There are a lack of research on, and strategies for dealing with, an insufficient response to antipsychotics. Treatment often is guided by what is described in published case reports or anecdotal evidence, rather than the findings of systematic studies.
We propose that a patient be considered “difficult-to-treat” or “treatment-resistant” after experiencing limited or negative responses to 3 different antipsychotics—with ≥1 being a second-generation antipsychotic (SGA)—that the patient has taken for at least 6 to 8 weeks at the maximum recommended dosage. Furthermore, switching to clozapine is an important strategy; do not consider it solely a last resort.
These 6 ‘D’s can remind you of other problems to consider when evaluating a treatment-resistant patient.
Diagnosis. Is the diagnosis, including the presence of comorbid conditions, accurate? Are significant psychosocial stressors undermining treatment response? Treat any comorbid conditions and consider instituting adjunctive psychosocial interventions, including cognitive-behavioral therapy.
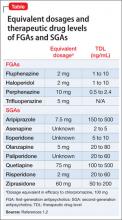
Dosage. Have the patient try the maximum recommended dosage if he (she) can tolerate it. Equivalent dosages of antipsychotics are shown in the Table,1,2 and can guide off-label use of higher dosages. Research does not support use of chlorpromazine equivalents >1,000 mg/d, and usually should not be employed. If using a higher than normal dosage, perform an ECG before the increase.3
Beneficial and adverse effects should be monitored carefully. Reduce the dosage after 3 months if the risk-benefit ratio does not justify the higher dosage.3
Duration. Try a treatment for at least 6 weeks at the maximum tolerated
dosage—even extending it to 12 weeks—before considering abandoning it because of insufficient response.
Drug interactions. Use a drug interaction tool to ensure drug-drug interactions are not reducing antipsychotic levels. A recent increase in smoking or decrease in caffeine intake can reduce the blood level of olanzapine and clozapine.4 Ultra-rapid metabolizers of cytochrome P450 isoenzymes may have a lower blood level of antipsychotic.
Consider pharmacogenetic testing in patients in whom you observe an unexpected lack of efficacy or adverse effects at customary dosages.
Double up. You might need to add another medication to the antipsychotic. Symptoms might help determine which medication to add:
- a combination of an SGA and a first-generation antipsychotic may be more effective than antipsychotic monotherapy5
- for prominent negative symptoms, consider using 2 SGAs of different potency together. Use caution when prescribing ziprasidone with another antipsychotic because this could prolong the QTc interval
- if a mood stabilizer is appropriate, consider lamotrigine because of its possible potentiating effect on SGAs6
- benzodiazepines can be used to reduce agitation or anxiety but are ineffective for psychosis.7
Drug levels. Measurement of the blood level of the drug is most useful when administering clozapine; focus on the clozapine, not on the norclozapine level that also is reported. Ensure a clozapine level of 350 to 600 ng/mL.
Therapeutic levels have been established for most antipsychotics (Table).1,2 Occasionally, knowing these levels can be helpful in evaluating patients for potential problems with absorption and metabolism of the drug, and with nonadherence.
Disclosures
Drs. Faden and Pinninti report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products. Dr. Mago receives grant/research support from Bristol-Myers Squibb, Forest Institute, Genomind, and Shire.
1. Gardner DM, Murphy AL, O’Donnell H, et al. International consensus study of antipsychotic dosing. Am J Psychiatry. 2010;167(6):686-693.
2. Hiemke C, Baumann P, Bergemann N, et al. AGNP consensus guidelines for therapeutic drug monitoring in psychiatry: update 2011. Pharmacopsychiatry. 2011;44(6):195-235.
3. Royal College of Psychiatrists. Consensus statement on high-dose antipsychotic medication. http://www.rcpsych.ac.uk/files/pdfversion/CR138.pdf. Published May 2006. Accessed March 26, 2013.
4. Pinninti NR, Mago R, de Leon J. Coffee, cigarettes and meds: what are the metabolic effects? Psychiatric Times. 2005;22(6):20-23.
5. Correll CU, Rummel-Kluge C, Corves C, et al. Antipsychotic combinations vs monotherapy in schizophrenia: a meta-analysis of randomized controlled trials. Schizophr Bull. 2009;35(2):443-457.
6. Citrome L. Treatment-resistant schizophrenia: what can we do about it? Current Psychiatry. 2011;10(6):52-58.
7. Volz A, Khorsand V, Gillies D, et al. Benzodiazepines for schizophrenia. Cochrane Database Syst Rev. 2007;(1): CD006391.
There are a lack of research on, and strategies for dealing with, an insufficient response to antipsychotics. Treatment often is guided by what is described in published case reports or anecdotal evidence, rather than the findings of systematic studies.
We propose that a patient be considered “difficult-to-treat” or “treatment-resistant” after experiencing limited or negative responses to 3 different antipsychotics—with ≥1 being a second-generation antipsychotic (SGA)—that the patient has taken for at least 6 to 8 weeks at the maximum recommended dosage. Furthermore, switching to clozapine is an important strategy; do not consider it solely a last resort.
These 6 ‘D’s can remind you of other problems to consider when evaluating a treatment-resistant patient.
Diagnosis. Is the diagnosis, including the presence of comorbid conditions, accurate? Are significant psychosocial stressors undermining treatment response? Treat any comorbid conditions and consider instituting adjunctive psychosocial interventions, including cognitive-behavioral therapy.
Dosage. Have the patient try the maximum recommended dosage if he (she) can tolerate it. Equivalent dosages of antipsychotics are shown in the Table,1,2 and can guide off-label use of higher dosages. Research does not support use of chlorpromazine equivalents >1,000 mg/d, and usually should not be employed. If using a higher than normal dosage, perform an ECG before the increase.3
Beneficial and adverse effects should be monitored carefully. Reduce the dosage after 3 months if the risk-benefit ratio does not justify the higher dosage.3
Duration. Try a treatment for at least 6 weeks at the maximum tolerated
dosage—even extending it to 12 weeks—before considering abandoning it because of insufficient response.
Drug interactions. Use a drug interaction tool to ensure drug-drug interactions are not reducing antipsychotic levels. A recent increase in smoking or decrease in caffeine intake can reduce the blood level of olanzapine and clozapine.4 Ultra-rapid metabolizers of cytochrome P450 isoenzymes may have a lower blood level of antipsychotic.
Consider pharmacogenetic testing in patients in whom you observe an unexpected lack of efficacy or adverse effects at customary dosages.
Double up. You might need to add another medication to the antipsychotic. Symptoms might help determine which medication to add:
- a combination of an SGA and a first-generation antipsychotic may be more effective than antipsychotic monotherapy5
- for prominent negative symptoms, consider using 2 SGAs of different potency together. Use caution when prescribing ziprasidone with another antipsychotic because this could prolong the QTc interval
- if a mood stabilizer is appropriate, consider lamotrigine because of its possible potentiating effect on SGAs6
- benzodiazepines can be used to reduce agitation or anxiety but are ineffective for psychosis.7
Drug levels. Measurement of the blood level of the drug is most useful when administering clozapine; focus on the clozapine, not on the norclozapine level that also is reported. Ensure a clozapine level of 350 to 600 ng/mL.
Therapeutic levels have been established for most antipsychotics (Table).1,2 Occasionally, knowing these levels can be helpful in evaluating patients for potential problems with absorption and metabolism of the drug, and with nonadherence.
Disclosures
Drs. Faden and Pinninti report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products. Dr. Mago receives grant/research support from Bristol-Myers Squibb, Forest Institute, Genomind, and Shire.
There are a lack of research on, and strategies for dealing with, an insufficient response to antipsychotics. Treatment often is guided by what is described in published case reports or anecdotal evidence, rather than the findings of systematic studies.
We propose that a patient be considered “difficult-to-treat” or “treatment-resistant” after experiencing limited or negative responses to 3 different antipsychotics—with ≥1 being a second-generation antipsychotic (SGA)—that the patient has taken for at least 6 to 8 weeks at the maximum recommended dosage. Furthermore, switching to clozapine is an important strategy; do not consider it solely a last resort.
These 6 ‘D’s can remind you of other problems to consider when evaluating a treatment-resistant patient.
Diagnosis. Is the diagnosis, including the presence of comorbid conditions, accurate? Are significant psychosocial stressors undermining treatment response? Treat any comorbid conditions and consider instituting adjunctive psychosocial interventions, including cognitive-behavioral therapy.
Dosage. Have the patient try the maximum recommended dosage if he (she) can tolerate it. Equivalent dosages of antipsychotics are shown in the Table,1,2 and can guide off-label use of higher dosages. Research does not support use of chlorpromazine equivalents >1,000 mg/d, and usually should not be employed. If using a higher than normal dosage, perform an ECG before the increase.3
Beneficial and adverse effects should be monitored carefully. Reduce the dosage after 3 months if the risk-benefit ratio does not justify the higher dosage.3
Duration. Try a treatment for at least 6 weeks at the maximum tolerated
dosage—even extending it to 12 weeks—before considering abandoning it because of insufficient response.
Drug interactions. Use a drug interaction tool to ensure drug-drug interactions are not reducing antipsychotic levels. A recent increase in smoking or decrease in caffeine intake can reduce the blood level of olanzapine and clozapine.4 Ultra-rapid metabolizers of cytochrome P450 isoenzymes may have a lower blood level of antipsychotic.
Consider pharmacogenetic testing in patients in whom you observe an unexpected lack of efficacy or adverse effects at customary dosages.
Double up. You might need to add another medication to the antipsychotic. Symptoms might help determine which medication to add:
- a combination of an SGA and a first-generation antipsychotic may be more effective than antipsychotic monotherapy5
- for prominent negative symptoms, consider using 2 SGAs of different potency together. Use caution when prescribing ziprasidone with another antipsychotic because this could prolong the QTc interval
- if a mood stabilizer is appropriate, consider lamotrigine because of its possible potentiating effect on SGAs6
- benzodiazepines can be used to reduce agitation or anxiety but are ineffective for psychosis.7
Drug levels. Measurement of the blood level of the drug is most useful when administering clozapine; focus on the clozapine, not on the norclozapine level that also is reported. Ensure a clozapine level of 350 to 600 ng/mL.
Therapeutic levels have been established for most antipsychotics (Table).1,2 Occasionally, knowing these levels can be helpful in evaluating patients for potential problems with absorption and metabolism of the drug, and with nonadherence.
Disclosures
Drs. Faden and Pinninti report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products. Dr. Mago receives grant/research support from Bristol-Myers Squibb, Forest Institute, Genomind, and Shire.
1. Gardner DM, Murphy AL, O’Donnell H, et al. International consensus study of antipsychotic dosing. Am J Psychiatry. 2010;167(6):686-693.
2. Hiemke C, Baumann P, Bergemann N, et al. AGNP consensus guidelines for therapeutic drug monitoring in psychiatry: update 2011. Pharmacopsychiatry. 2011;44(6):195-235.
3. Royal College of Psychiatrists. Consensus statement on high-dose antipsychotic medication. http://www.rcpsych.ac.uk/files/pdfversion/CR138.pdf. Published May 2006. Accessed March 26, 2013.
4. Pinninti NR, Mago R, de Leon J. Coffee, cigarettes and meds: what are the metabolic effects? Psychiatric Times. 2005;22(6):20-23.
5. Correll CU, Rummel-Kluge C, Corves C, et al. Antipsychotic combinations vs monotherapy in schizophrenia: a meta-analysis of randomized controlled trials. Schizophr Bull. 2009;35(2):443-457.
6. Citrome L. Treatment-resistant schizophrenia: what can we do about it? Current Psychiatry. 2011;10(6):52-58.
7. Volz A, Khorsand V, Gillies D, et al. Benzodiazepines for schizophrenia. Cochrane Database Syst Rev. 2007;(1): CD006391.
1. Gardner DM, Murphy AL, O’Donnell H, et al. International consensus study of antipsychotic dosing. Am J Psychiatry. 2010;167(6):686-693.
2. Hiemke C, Baumann P, Bergemann N, et al. AGNP consensus guidelines for therapeutic drug monitoring in psychiatry: update 2011. Pharmacopsychiatry. 2011;44(6):195-235.
3. Royal College of Psychiatrists. Consensus statement on high-dose antipsychotic medication. http://www.rcpsych.ac.uk/files/pdfversion/CR138.pdf. Published May 2006. Accessed March 26, 2013.
4. Pinninti NR, Mago R, de Leon J. Coffee, cigarettes and meds: what are the metabolic effects? Psychiatric Times. 2005;22(6):20-23.
5. Correll CU, Rummel-Kluge C, Corves C, et al. Antipsychotic combinations vs monotherapy in schizophrenia: a meta-analysis of randomized controlled trials. Schizophr Bull. 2009;35(2):443-457.
6. Citrome L. Treatment-resistant schizophrenia: what can we do about it? Current Psychiatry. 2011;10(6):52-58.
7. Volz A, Khorsand V, Gillies D, et al. Benzodiazepines for schizophrenia. Cochrane Database Syst Rev. 2007;(1): CD006391.
The avoidant psychotherapy patient
CASE: Unexplained panic
Mr. J, age 35, is a married, unemployed musician who presents for outpatient treatment for panic attacks. He experienced his first panic attack at his oldest son’s baptism 12 years ago, but does not know why it occurred at that moment. He rarely has panic attacks now, but wants to continue medication management. He denies depressive symptoms, saying, “I’m the most optimistic person in the world.” Mr. J tried several medications for his panic attacks before clonazepam, 2 mg/d, proved effective, but always has been vehemently opposed to antidepressants. Despite his insistence that he needs only medication management, Mr. J chooses to enroll in a resident-run psychotherapy clinic.
In sessions, Mr. J describes his father, who also has panic disorder, as a powerful figure who is physically and emotionally abusive, but also charismatic, charming, and “impossible not to love.” However, Mr. J felt his father was impossible to live with, and moved out at age 18 to marry his high school sweetheart. They have 3 children, ages 12, 10, and 8. Mr. J worked for his father at his construction company, but was not able to satisfy him or live up to his standards so he quit because he was tired of being cut down and emasculated.
Mr. J’s parents divorced 15 years ago after his mother had an affair with her husband’s friend. His father learned of the affair and threatened his wife with a handgun. Although Mr. J and his mother were close before her affair, he has been unable to forgive or empathize with her, and rarely speaks to her. Mr. J’s mother could not protect him from his father’s abuse, and later compounded her failure by abandoning her husband and son through her sexual affair. Growing up with a father he did not respect or get comfort from and sharing a common fear and alliance with his mother likely made it difficult for Mr. J to navigate his Oedipal phase,1 and made her abandonment even more painful.
When Mr. J was 6 years old, he was molested by one of his father’s friends. His father stabbed the man in the shoulder when he found out about the molestation and received probation. Although Mr. J knows he was molested, he does not remember it and has repressed most of his childhood.
The authors’ observations
I (JF) wanted to discuss with Mr. J why his first panic attack occurred during such a symbolic occasion. His panic could be the result of a struggle between a murderous wish toward his father and paternal protective instinct toward his son. The baptism placed his son in a highly vulnerable position, which reminded Mr. J of his own vulnerability and impotent rage toward his father. Anxiety often results when an individual has 2 opposing wishes,2 and a murderous wish often is involved when anxiety progresses to panic. Getting to the root of this with Mr. J could allow for further psychological growth.3 His murderous wishes and fantasies are ego-dystonic, and panic could be a way of punishing himself for these thoughts. When Mr. J identified himself as his son during the baptism, he likely was flooded with thoughts that his defenses were no longer able to repress. Seeing his son submerged in the baptismal font brought back an aspect of his own life that he had completely split off from consciousness, and likely will take time to process. Considering the current therapeutic dynamic, I decided that it was not the best time to address this potential conflict; however, I could have chosen a manualized form of psychodynamic psychotherapy for panic disorder.4 See Table 1 for an outline of the phases of psychodynamic psychotherapy for panic disorder.
Although Mr. J’s initial willingness to discuss his past was encouraging, he refused to schedule more than 1 session every 4 weeks. He also began to keep the content of our sessions superficial, which caused me angst because he seemed to be withholding information and would not come more frequently. Although I was not proud of my feelings, I had to be honest with myself that I had started to dislike Mr. J.
Table 1
Psychodynamic psychotherapy for panic disorder
| Phase | Comments |
|---|---|
| Treatment of acute panic | Therapy focuses on discovering the conscious and unconscious meaning of panic symptoms |
| Treatment of panic vulnerability | Core dynamic conflicts related to panic are understood and altered. Tasks include addressing the nature of the transference and working through them |
| Termination | The therapist directly addresses patients’ difficulties with separation and independence as they emerge in treatment. After treatment, patients may be better able to manage separations, anger, and independence |
| Source: Adapted from reference 4 | |
Countertransference reactions
Countertransference is a therapist's emotional reaction to a patient. Just as patients form reactions based on past relationships brought to present, therapists develop similar reactions.5 Noting one’s countertransference provides a window into how the patient’s thoughts and actions evoke feelings in others. It also can shed light on an aspect of the doctor-patient relationship that may have gone unnoticed.2
Countertransference hatred can occur when a therapist begins to dislike a patient. Typically, patients with borderline personality disorder, masochistic tendencies, or suicidality arouse strong countertransference reactions6; however, any patient can evoke these emotions. This type of hateful patient can precipitate antitherapeutic feelings such as aversion or malice that can be a major obstacle to treatment.7 Aversion leads the therapist to withdraw from the patient, and malice can trigger cruel impulses.
Maltsberger and Buie7 identified 5 defenses therapists may use to combat countertransference hatred (Table 2). When treating Mr. J, I used several of these defenses, including projection and turning against the self to protect myself from this challenging patient. In turning against the self, I became doubtful and critical of my skills and increasingly submissive to Mr. J. Additionally, I projected this countertransference hatred onto Mr. J, focusing on the negative transference that he brought to our therapeutic encounters. On an unconscious level, I may have feared retribution from Mr. J.
I became so frustrated with Mr. J that I reduced the frequency of our sessions to once every 6 weeks, which I realized could be evidence of my feelings regarding Mr. J’s minimization and avoidant style.
Table 2
Defenses against countertransference hate
| Defense mechanism | Description |
|---|---|
| Repression | Remaining unconscious of feelings of hate; may manifest as difficulty paying attention to what the patient is saying or feeling bored or tired |
| Turning against oneself | Doubting one’s capacity to help the patient; may feel inadequate, helpless, and hopeless. May lead to giving up on the patient because the therapist feels incompetent |
| Reaction formation | Turning hatred into the opposite emotion. The therapist may be too preoccupied with being helpful or overly concerned about the patient’s welfare and comfort |
| Projection | Feeling that the patient hates the therapist, leading to feelings of dread and fear |
| Distortion of reality | Devaluing the patient and seeing the patient as a hopeless case or a dangerous person. The therapist may feel indifference, pity, or anger toward the patient |
| Source: Reference 7 | |
TREATMENT: A breakthrough
Mr. J presents with obvious unease at the first visit after we had decreased the frequency of our sessions. At this point, Mr. J opens up to me. He says he has not been truthful with me, and has had worsening depression, anhedonia, and agoraphobia over the past year. He also reveals that he has homosexual fantasies that he cannot stop, which disturb him because he says he is heterosexual. He agrees to come once a week, and reluctantly admits that he desperately needs help.
Although Mr. J only takes clonazepam and citalopram, 20 mg/d, which I prescribed after he admitted to depression and anxiety, he has hyperlipidemia and a family history of heart disease. In addition to being a musician and working at his father’s construction company, he has worked as a security guard, bounty hunter, and computer technician. His careers have been solitary in nature, and, with the exception of computer work, permitted an outlet for aggression. However, he recently started taking online college classes and wants to become a music teacher because he feels he has a lot to offer children as a result of his life experiences. His fantasy of being a teacher shows considerably less aggression, and could be a sign of psychological growth.
Mr. J is struggling financially and his home is on the verge of foreclosure. Early in treatment he told me that he stopped paying his mortgage, but demonstrated blind optimism that things would “work out.” I asked if this was a wise decision, but he seemed confident and dismissive of my concerns. Although he now struggles with this situation, I consider this healthier than his constant pseudo-happy state, and a sign of psychological development.8 Despite his financial stressors, he wants to pursue his dream of being a famous musician, and says he “could never work a 9-to-5 job in a cubicle.”
The authors’ observations
I do not think it’s a coincidence that Mr. J stopped minimizing his symptoms when we decreased the frequency of his sessions. I had viewed our sessions as unproductive and blamed Mr. J for wasting both of our time with his resistance and minimization and had begun to dislike him. I felt impotent because he had been controlling each session with long, elaborate stories that had little relevance to his panic attacks, and I could not redirect him or get him to focus on pertinent issues. It was as if I was an audience for him, and provided nothing useful. However, I was interested in these superficial stories because Mr. J was charming and engaging. He likely reenacted his relationship with his father with me. Mr. J’s superficial relationship with me caused me to dislike him, and, similar to his father, reject him. This rejection likely was damaging because I was unable to anticipate his needs, which would have been to increase—rather than decrease—the frequency of our sessions. Just like his father, I was not able to take care of him.
Mr. J is deeply conflicted about his father. He states that his father “is a monster who instills fear and intimidation into everyone around him, but he’s charismatic, and I’ll always love him.” His view of his domineering father likely developed into a castration anxiety because he was afraid of competing for his mother’s love, contributing to a muddled sexual identity. This was intensified when Mr. J was sexually abused; he may have been stimulated by the molestation, adding to his confusion. Although Mr. J has repressed the abuse and split off most of his childhood, he suffers from shame, guilt, and depression because of his ego-dystonic homosexual fantasies. Homosexuality is at odds with his self-image and contributes to his anxiety and panic attacks. He cannot adequately discharge this dangerous libidinal energy, and as he becomes more conscious of it, his anxiety intensifies.
OUTCOME: Overcoming fear
As Mr. J sits crying in my office, he says he hasn’t cried in front of another man in years. I wonder aloud what his father would think of this situation. His states that his father does not respect any type of weakness and probably would “knock his teeth in.” Overcoming this fear of opening up will be a goal of Mr. J’s treatment. His unbridled optimism borders on pathologic, and is a defense against reality.8 Additionally, his reluctance to accept that he is suffering from depression, which he perceives as a weakness, will be a struggle throughout therapy. He likely will continue to minimize his symptoms when possible, making the true depths of his illness difficult to grasp.
Related Resources
- Waska R. Using countertransference: analytic contact, projective identification, and transference phantasy states. Am J Psychother. 2008;62(4):333-351.
- Gabbard GO, Litowitz BE, Williams P. Textbook of psychoanalysis. Arlington, VA: American Psychiatric Publishing, Inc; 2011.
Drug Brand Names
- Citalopram • Celexa
- Clonazepam • Klonopin
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Blos P. Son and father: before and beyond the Oedipus complex. New York NY: Free Press/Macmillan; 1985.
2. Ursano RJ, Sonnenberg SM, Lazar SG. Concise guide to psychodynamic psychotherapy. Arlington VA: American Psychiatric Publishing; 2004.
3. Akhtar S. Comprehensive dictionary of psychoanalysis. London United Kingdom: Kamac Books; 2009.
4. Busch FN, Milrod BL, Singer MB. Theory and technique in psychodynamic treatment of panic disorder. J Psychother Pract Res. 1999;8(3):234-242.
5. Freud S. The future prospects of psycho-analytic therapy. The standard edition of the complete psychological works of Sigmund Freud volume XI (1910): five lectures on psycho-analysis, Leonardo da Vinci and other works. London, United Kingdom: Hogarth Press; 1957:139–152.
6. Winnicott DW. Hate in the counter-transference. J Psychother Pract Res. 1994;3(4):348-356.
7. Maltsberger JT, Buie DH. Countertransference hate in the treatment of suicidal patients. Arch Gen Psychiatry. 1974;30(5):625-633.
8. Akhtar S. “Someday…” and “if only…” fantasies: pathological optimism and inordinate nostalgia as related forms of idealization. J Am Psychoanal Assoc. 1996;44(3):723-753.
CASE: Unexplained panic
Mr. J, age 35, is a married, unemployed musician who presents for outpatient treatment for panic attacks. He experienced his first panic attack at his oldest son’s baptism 12 years ago, but does not know why it occurred at that moment. He rarely has panic attacks now, but wants to continue medication management. He denies depressive symptoms, saying, “I’m the most optimistic person in the world.” Mr. J tried several medications for his panic attacks before clonazepam, 2 mg/d, proved effective, but always has been vehemently opposed to antidepressants. Despite his insistence that he needs only medication management, Mr. J chooses to enroll in a resident-run psychotherapy clinic.
In sessions, Mr. J describes his father, who also has panic disorder, as a powerful figure who is physically and emotionally abusive, but also charismatic, charming, and “impossible not to love.” However, Mr. J felt his father was impossible to live with, and moved out at age 18 to marry his high school sweetheart. They have 3 children, ages 12, 10, and 8. Mr. J worked for his father at his construction company, but was not able to satisfy him or live up to his standards so he quit because he was tired of being cut down and emasculated.
Mr. J’s parents divorced 15 years ago after his mother had an affair with her husband’s friend. His father learned of the affair and threatened his wife with a handgun. Although Mr. J and his mother were close before her affair, he has been unable to forgive or empathize with her, and rarely speaks to her. Mr. J’s mother could not protect him from his father’s abuse, and later compounded her failure by abandoning her husband and son through her sexual affair. Growing up with a father he did not respect or get comfort from and sharing a common fear and alliance with his mother likely made it difficult for Mr. J to navigate his Oedipal phase,1 and made her abandonment even more painful.
When Mr. J was 6 years old, he was molested by one of his father’s friends. His father stabbed the man in the shoulder when he found out about the molestation and received probation. Although Mr. J knows he was molested, he does not remember it and has repressed most of his childhood.
The authors’ observations
I (JF) wanted to discuss with Mr. J why his first panic attack occurred during such a symbolic occasion. His panic could be the result of a struggle between a murderous wish toward his father and paternal protective instinct toward his son. The baptism placed his son in a highly vulnerable position, which reminded Mr. J of his own vulnerability and impotent rage toward his father. Anxiety often results when an individual has 2 opposing wishes,2 and a murderous wish often is involved when anxiety progresses to panic. Getting to the root of this with Mr. J could allow for further psychological growth.3 His murderous wishes and fantasies are ego-dystonic, and panic could be a way of punishing himself for these thoughts. When Mr. J identified himself as his son during the baptism, he likely was flooded with thoughts that his defenses were no longer able to repress. Seeing his son submerged in the baptismal font brought back an aspect of his own life that he had completely split off from consciousness, and likely will take time to process. Considering the current therapeutic dynamic, I decided that it was not the best time to address this potential conflict; however, I could have chosen a manualized form of psychodynamic psychotherapy for panic disorder.4 See Table 1 for an outline of the phases of psychodynamic psychotherapy for panic disorder.
Although Mr. J’s initial willingness to discuss his past was encouraging, he refused to schedule more than 1 session every 4 weeks. He also began to keep the content of our sessions superficial, which caused me angst because he seemed to be withholding information and would not come more frequently. Although I was not proud of my feelings, I had to be honest with myself that I had started to dislike Mr. J.
Table 1
Psychodynamic psychotherapy for panic disorder
| Phase | Comments |
|---|---|
| Treatment of acute panic | Therapy focuses on discovering the conscious and unconscious meaning of panic symptoms |
| Treatment of panic vulnerability | Core dynamic conflicts related to panic are understood and altered. Tasks include addressing the nature of the transference and working through them |
| Termination | The therapist directly addresses patients’ difficulties with separation and independence as they emerge in treatment. After treatment, patients may be better able to manage separations, anger, and independence |
| Source: Adapted from reference 4 | |
Countertransference reactions
Countertransference is a therapist's emotional reaction to a patient. Just as patients form reactions based on past relationships brought to present, therapists develop similar reactions.5 Noting one’s countertransference provides a window into how the patient’s thoughts and actions evoke feelings in others. It also can shed light on an aspect of the doctor-patient relationship that may have gone unnoticed.2
Countertransference hatred can occur when a therapist begins to dislike a patient. Typically, patients with borderline personality disorder, masochistic tendencies, or suicidality arouse strong countertransference reactions6; however, any patient can evoke these emotions. This type of hateful patient can precipitate antitherapeutic feelings such as aversion or malice that can be a major obstacle to treatment.7 Aversion leads the therapist to withdraw from the patient, and malice can trigger cruel impulses.
Maltsberger and Buie7 identified 5 defenses therapists may use to combat countertransference hatred (Table 2). When treating Mr. J, I used several of these defenses, including projection and turning against the self to protect myself from this challenging patient. In turning against the self, I became doubtful and critical of my skills and increasingly submissive to Mr. J. Additionally, I projected this countertransference hatred onto Mr. J, focusing on the negative transference that he brought to our therapeutic encounters. On an unconscious level, I may have feared retribution from Mr. J.
I became so frustrated with Mr. J that I reduced the frequency of our sessions to once every 6 weeks, which I realized could be evidence of my feelings regarding Mr. J’s minimization and avoidant style.
Table 2
Defenses against countertransference hate
| Defense mechanism | Description |
|---|---|
| Repression | Remaining unconscious of feelings of hate; may manifest as difficulty paying attention to what the patient is saying or feeling bored or tired |
| Turning against oneself | Doubting one’s capacity to help the patient; may feel inadequate, helpless, and hopeless. May lead to giving up on the patient because the therapist feels incompetent |
| Reaction formation | Turning hatred into the opposite emotion. The therapist may be too preoccupied with being helpful or overly concerned about the patient’s welfare and comfort |
| Projection | Feeling that the patient hates the therapist, leading to feelings of dread and fear |
| Distortion of reality | Devaluing the patient and seeing the patient as a hopeless case or a dangerous person. The therapist may feel indifference, pity, or anger toward the patient |
| Source: Reference 7 | |
TREATMENT: A breakthrough
Mr. J presents with obvious unease at the first visit after we had decreased the frequency of our sessions. At this point, Mr. J opens up to me. He says he has not been truthful with me, and has had worsening depression, anhedonia, and agoraphobia over the past year. He also reveals that he has homosexual fantasies that he cannot stop, which disturb him because he says he is heterosexual. He agrees to come once a week, and reluctantly admits that he desperately needs help.
Although Mr. J only takes clonazepam and citalopram, 20 mg/d, which I prescribed after he admitted to depression and anxiety, he has hyperlipidemia and a family history of heart disease. In addition to being a musician and working at his father’s construction company, he has worked as a security guard, bounty hunter, and computer technician. His careers have been solitary in nature, and, with the exception of computer work, permitted an outlet for aggression. However, he recently started taking online college classes and wants to become a music teacher because he feels he has a lot to offer children as a result of his life experiences. His fantasy of being a teacher shows considerably less aggression, and could be a sign of psychological growth.
Mr. J is struggling financially and his home is on the verge of foreclosure. Early in treatment he told me that he stopped paying his mortgage, but demonstrated blind optimism that things would “work out.” I asked if this was a wise decision, but he seemed confident and dismissive of my concerns. Although he now struggles with this situation, I consider this healthier than his constant pseudo-happy state, and a sign of psychological development.8 Despite his financial stressors, he wants to pursue his dream of being a famous musician, and says he “could never work a 9-to-5 job in a cubicle.”
The authors’ observations
I do not think it’s a coincidence that Mr. J stopped minimizing his symptoms when we decreased the frequency of his sessions. I had viewed our sessions as unproductive and blamed Mr. J for wasting both of our time with his resistance and minimization and had begun to dislike him. I felt impotent because he had been controlling each session with long, elaborate stories that had little relevance to his panic attacks, and I could not redirect him or get him to focus on pertinent issues. It was as if I was an audience for him, and provided nothing useful. However, I was interested in these superficial stories because Mr. J was charming and engaging. He likely reenacted his relationship with his father with me. Mr. J’s superficial relationship with me caused me to dislike him, and, similar to his father, reject him. This rejection likely was damaging because I was unable to anticipate his needs, which would have been to increase—rather than decrease—the frequency of our sessions. Just like his father, I was not able to take care of him.
Mr. J is deeply conflicted about his father. He states that his father “is a monster who instills fear and intimidation into everyone around him, but he’s charismatic, and I’ll always love him.” His view of his domineering father likely developed into a castration anxiety because he was afraid of competing for his mother’s love, contributing to a muddled sexual identity. This was intensified when Mr. J was sexually abused; he may have been stimulated by the molestation, adding to his confusion. Although Mr. J has repressed the abuse and split off most of his childhood, he suffers from shame, guilt, and depression because of his ego-dystonic homosexual fantasies. Homosexuality is at odds with his self-image and contributes to his anxiety and panic attacks. He cannot adequately discharge this dangerous libidinal energy, and as he becomes more conscious of it, his anxiety intensifies.
OUTCOME: Overcoming fear
As Mr. J sits crying in my office, he says he hasn’t cried in front of another man in years. I wonder aloud what his father would think of this situation. His states that his father does not respect any type of weakness and probably would “knock his teeth in.” Overcoming this fear of opening up will be a goal of Mr. J’s treatment. His unbridled optimism borders on pathologic, and is a defense against reality.8 Additionally, his reluctance to accept that he is suffering from depression, which he perceives as a weakness, will be a struggle throughout therapy. He likely will continue to minimize his symptoms when possible, making the true depths of his illness difficult to grasp.
Related Resources
- Waska R. Using countertransference: analytic contact, projective identification, and transference phantasy states. Am J Psychother. 2008;62(4):333-351.
- Gabbard GO, Litowitz BE, Williams P. Textbook of psychoanalysis. Arlington, VA: American Psychiatric Publishing, Inc; 2011.
Drug Brand Names
- Citalopram • Celexa
- Clonazepam • Klonopin
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Unexplained panic
Mr. J, age 35, is a married, unemployed musician who presents for outpatient treatment for panic attacks. He experienced his first panic attack at his oldest son’s baptism 12 years ago, but does not know why it occurred at that moment. He rarely has panic attacks now, but wants to continue medication management. He denies depressive symptoms, saying, “I’m the most optimistic person in the world.” Mr. J tried several medications for his panic attacks before clonazepam, 2 mg/d, proved effective, but always has been vehemently opposed to antidepressants. Despite his insistence that he needs only medication management, Mr. J chooses to enroll in a resident-run psychotherapy clinic.
In sessions, Mr. J describes his father, who also has panic disorder, as a powerful figure who is physically and emotionally abusive, but also charismatic, charming, and “impossible not to love.” However, Mr. J felt his father was impossible to live with, and moved out at age 18 to marry his high school sweetheart. They have 3 children, ages 12, 10, and 8. Mr. J worked for his father at his construction company, but was not able to satisfy him or live up to his standards so he quit because he was tired of being cut down and emasculated.
Mr. J’s parents divorced 15 years ago after his mother had an affair with her husband’s friend. His father learned of the affair and threatened his wife with a handgun. Although Mr. J and his mother were close before her affair, he has been unable to forgive or empathize with her, and rarely speaks to her. Mr. J’s mother could not protect him from his father’s abuse, and later compounded her failure by abandoning her husband and son through her sexual affair. Growing up with a father he did not respect or get comfort from and sharing a common fear and alliance with his mother likely made it difficult for Mr. J to navigate his Oedipal phase,1 and made her abandonment even more painful.
When Mr. J was 6 years old, he was molested by one of his father’s friends. His father stabbed the man in the shoulder when he found out about the molestation and received probation. Although Mr. J knows he was molested, he does not remember it and has repressed most of his childhood.
The authors’ observations
I (JF) wanted to discuss with Mr. J why his first panic attack occurred during such a symbolic occasion. His panic could be the result of a struggle between a murderous wish toward his father and paternal protective instinct toward his son. The baptism placed his son in a highly vulnerable position, which reminded Mr. J of his own vulnerability and impotent rage toward his father. Anxiety often results when an individual has 2 opposing wishes,2 and a murderous wish often is involved when anxiety progresses to panic. Getting to the root of this with Mr. J could allow for further psychological growth.3 His murderous wishes and fantasies are ego-dystonic, and panic could be a way of punishing himself for these thoughts. When Mr. J identified himself as his son during the baptism, he likely was flooded with thoughts that his defenses were no longer able to repress. Seeing his son submerged in the baptismal font brought back an aspect of his own life that he had completely split off from consciousness, and likely will take time to process. Considering the current therapeutic dynamic, I decided that it was not the best time to address this potential conflict; however, I could have chosen a manualized form of psychodynamic psychotherapy for panic disorder.4 See Table 1 for an outline of the phases of psychodynamic psychotherapy for panic disorder.
Although Mr. J’s initial willingness to discuss his past was encouraging, he refused to schedule more than 1 session every 4 weeks. He also began to keep the content of our sessions superficial, which caused me angst because he seemed to be withholding information and would not come more frequently. Although I was not proud of my feelings, I had to be honest with myself that I had started to dislike Mr. J.
Table 1
Psychodynamic psychotherapy for panic disorder
| Phase | Comments |
|---|---|
| Treatment of acute panic | Therapy focuses on discovering the conscious and unconscious meaning of panic symptoms |
| Treatment of panic vulnerability | Core dynamic conflicts related to panic are understood and altered. Tasks include addressing the nature of the transference and working through them |
| Termination | The therapist directly addresses patients’ difficulties with separation and independence as they emerge in treatment. After treatment, patients may be better able to manage separations, anger, and independence |
| Source: Adapted from reference 4 | |
Countertransference reactions
Countertransference is a therapist's emotional reaction to a patient. Just as patients form reactions based on past relationships brought to present, therapists develop similar reactions.5 Noting one’s countertransference provides a window into how the patient’s thoughts and actions evoke feelings in others. It also can shed light on an aspect of the doctor-patient relationship that may have gone unnoticed.2
Countertransference hatred can occur when a therapist begins to dislike a patient. Typically, patients with borderline personality disorder, masochistic tendencies, or suicidality arouse strong countertransference reactions6; however, any patient can evoke these emotions. This type of hateful patient can precipitate antitherapeutic feelings such as aversion or malice that can be a major obstacle to treatment.7 Aversion leads the therapist to withdraw from the patient, and malice can trigger cruel impulses.
Maltsberger and Buie7 identified 5 defenses therapists may use to combat countertransference hatred (Table 2). When treating Mr. J, I used several of these defenses, including projection and turning against the self to protect myself from this challenging patient. In turning against the self, I became doubtful and critical of my skills and increasingly submissive to Mr. J. Additionally, I projected this countertransference hatred onto Mr. J, focusing on the negative transference that he brought to our therapeutic encounters. On an unconscious level, I may have feared retribution from Mr. J.
I became so frustrated with Mr. J that I reduced the frequency of our sessions to once every 6 weeks, which I realized could be evidence of my feelings regarding Mr. J’s minimization and avoidant style.
Table 2
Defenses against countertransference hate
| Defense mechanism | Description |
|---|---|
| Repression | Remaining unconscious of feelings of hate; may manifest as difficulty paying attention to what the patient is saying or feeling bored or tired |
| Turning against oneself | Doubting one’s capacity to help the patient; may feel inadequate, helpless, and hopeless. May lead to giving up on the patient because the therapist feels incompetent |
| Reaction formation | Turning hatred into the opposite emotion. The therapist may be too preoccupied with being helpful or overly concerned about the patient’s welfare and comfort |
| Projection | Feeling that the patient hates the therapist, leading to feelings of dread and fear |
| Distortion of reality | Devaluing the patient and seeing the patient as a hopeless case or a dangerous person. The therapist may feel indifference, pity, or anger toward the patient |
| Source: Reference 7 | |
TREATMENT: A breakthrough
Mr. J presents with obvious unease at the first visit after we had decreased the frequency of our sessions. At this point, Mr. J opens up to me. He says he has not been truthful with me, and has had worsening depression, anhedonia, and agoraphobia over the past year. He also reveals that he has homosexual fantasies that he cannot stop, which disturb him because he says he is heterosexual. He agrees to come once a week, and reluctantly admits that he desperately needs help.
Although Mr. J only takes clonazepam and citalopram, 20 mg/d, which I prescribed after he admitted to depression and anxiety, he has hyperlipidemia and a family history of heart disease. In addition to being a musician and working at his father’s construction company, he has worked as a security guard, bounty hunter, and computer technician. His careers have been solitary in nature, and, with the exception of computer work, permitted an outlet for aggression. However, he recently started taking online college classes and wants to become a music teacher because he feels he has a lot to offer children as a result of his life experiences. His fantasy of being a teacher shows considerably less aggression, and could be a sign of psychological growth.
Mr. J is struggling financially and his home is on the verge of foreclosure. Early in treatment he told me that he stopped paying his mortgage, but demonstrated blind optimism that things would “work out.” I asked if this was a wise decision, but he seemed confident and dismissive of my concerns. Although he now struggles with this situation, I consider this healthier than his constant pseudo-happy state, and a sign of psychological development.8 Despite his financial stressors, he wants to pursue his dream of being a famous musician, and says he “could never work a 9-to-5 job in a cubicle.”
The authors’ observations
I do not think it’s a coincidence that Mr. J stopped minimizing his symptoms when we decreased the frequency of his sessions. I had viewed our sessions as unproductive and blamed Mr. J for wasting both of our time with his resistance and minimization and had begun to dislike him. I felt impotent because he had been controlling each session with long, elaborate stories that had little relevance to his panic attacks, and I could not redirect him or get him to focus on pertinent issues. It was as if I was an audience for him, and provided nothing useful. However, I was interested in these superficial stories because Mr. J was charming and engaging. He likely reenacted his relationship with his father with me. Mr. J’s superficial relationship with me caused me to dislike him, and, similar to his father, reject him. This rejection likely was damaging because I was unable to anticipate his needs, which would have been to increase—rather than decrease—the frequency of our sessions. Just like his father, I was not able to take care of him.
Mr. J is deeply conflicted about his father. He states that his father “is a monster who instills fear and intimidation into everyone around him, but he’s charismatic, and I’ll always love him.” His view of his domineering father likely developed into a castration anxiety because he was afraid of competing for his mother’s love, contributing to a muddled sexual identity. This was intensified when Mr. J was sexually abused; he may have been stimulated by the molestation, adding to his confusion. Although Mr. J has repressed the abuse and split off most of his childhood, he suffers from shame, guilt, and depression because of his ego-dystonic homosexual fantasies. Homosexuality is at odds with his self-image and contributes to his anxiety and panic attacks. He cannot adequately discharge this dangerous libidinal energy, and as he becomes more conscious of it, his anxiety intensifies.
OUTCOME: Overcoming fear
As Mr. J sits crying in my office, he says he hasn’t cried in front of another man in years. I wonder aloud what his father would think of this situation. His states that his father does not respect any type of weakness and probably would “knock his teeth in.” Overcoming this fear of opening up will be a goal of Mr. J’s treatment. His unbridled optimism borders on pathologic, and is a defense against reality.8 Additionally, his reluctance to accept that he is suffering from depression, which he perceives as a weakness, will be a struggle throughout therapy. He likely will continue to minimize his symptoms when possible, making the true depths of his illness difficult to grasp.
Related Resources
- Waska R. Using countertransference: analytic contact, projective identification, and transference phantasy states. Am J Psychother. 2008;62(4):333-351.
- Gabbard GO, Litowitz BE, Williams P. Textbook of psychoanalysis. Arlington, VA: American Psychiatric Publishing, Inc; 2011.
Drug Brand Names
- Citalopram • Celexa
- Clonazepam • Klonopin
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Blos P. Son and father: before and beyond the Oedipus complex. New York NY: Free Press/Macmillan; 1985.
2. Ursano RJ, Sonnenberg SM, Lazar SG. Concise guide to psychodynamic psychotherapy. Arlington VA: American Psychiatric Publishing; 2004.
3. Akhtar S. Comprehensive dictionary of psychoanalysis. London United Kingdom: Kamac Books; 2009.
4. Busch FN, Milrod BL, Singer MB. Theory and technique in psychodynamic treatment of panic disorder. J Psychother Pract Res. 1999;8(3):234-242.
5. Freud S. The future prospects of psycho-analytic therapy. The standard edition of the complete psychological works of Sigmund Freud volume XI (1910): five lectures on psycho-analysis, Leonardo da Vinci and other works. London, United Kingdom: Hogarth Press; 1957:139–152.
6. Winnicott DW. Hate in the counter-transference. J Psychother Pract Res. 1994;3(4):348-356.
7. Maltsberger JT, Buie DH. Countertransference hate in the treatment of suicidal patients. Arch Gen Psychiatry. 1974;30(5):625-633.
8. Akhtar S. “Someday…” and “if only…” fantasies: pathological optimism and inordinate nostalgia as related forms of idealization. J Am Psychoanal Assoc. 1996;44(3):723-753.
1. Blos P. Son and father: before and beyond the Oedipus complex. New York NY: Free Press/Macmillan; 1985.
2. Ursano RJ, Sonnenberg SM, Lazar SG. Concise guide to psychodynamic psychotherapy. Arlington VA: American Psychiatric Publishing; 2004.
3. Akhtar S. Comprehensive dictionary of psychoanalysis. London United Kingdom: Kamac Books; 2009.
4. Busch FN, Milrod BL, Singer MB. Theory and technique in psychodynamic treatment of panic disorder. J Psychother Pract Res. 1999;8(3):234-242.
5. Freud S. The future prospects of psycho-analytic therapy. The standard edition of the complete psychological works of Sigmund Freud volume XI (1910): five lectures on psycho-analysis, Leonardo da Vinci and other works. London, United Kingdom: Hogarth Press; 1957:139–152.
6. Winnicott DW. Hate in the counter-transference. J Psychother Pract Res. 1994;3(4):348-356.
7. Maltsberger JT, Buie DH. Countertransference hate in the treatment of suicidal patients. Arch Gen Psychiatry. 1974;30(5):625-633.
8. Akhtar S. “Someday…” and “if only…” fantasies: pathological optimism and inordinate nostalgia as related forms of idealization. J Am Psychoanal Assoc. 1996;44(3):723-753.