User login
The telltale heart: What HDL reveals about a woman’s risk
JUDY’S CASE
“WHAT’S MY RISK?”
At her periodic gynecologic exam, Judy, a 58-year-old white woman, expresses concern about her heart health in light of her 62-year-old sister’s recent heart attack. Further questioning reveals that her father died of a heart attack at age 56, and her brother, 52, has high blood pressure and adult-onset diabetes.
Judy has not experienced any symptoms of cardiovascular disease, such as chest pain or tightness with exertion, and she doesn’t smoke. The last time her cholesterol was checked was about 15 years earlier, at which time it was “OK.” She admits she is not very physically active and has gained about 30 lb over the past 10 years. Her vital signs and physical exam are entirely normal except for borderline high blood pressure at 140/90 mm Hg, weight of 170 lb (height: 68 inches), and a waist circumference of 37 inches.
What is her cardiovascular risk?
Judy has physical findings suggestive of metabolic syndrome in addition to the significant family history of cardiovascular disease (CVD). Although her current risk of a cardiac event appears to be low, she is likely to deteriorate if the hypertension and excess body weight are not addressed.
To predict her level of risk more precisely, the physician asks Judy to return in 2 weeks for a blood pressure recheck, and instructs her to perform additional readings on her own. The clinician also refers Judy for a fasting lipid panel and blood glucose level.
In women, CVD is especially lethal
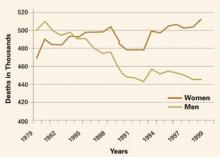
Contrary to earlier assumptions, CVD now appears to be more lethal in women than in men and warrants aggressive efforts to prevent it and manage risk factors (FIGURE). This article focuses on improving high-density lipoprotein (HDL) cholesterol, a key factor in women at risk.
This approach differs slightly from the National Cholesterol Education Program Adult Treatment Panel III (NCEP/ATP III) guidelines, which target low-density lipoprotein (LDL) cholesterol as the primary lipid risk factor for intervention.1
FIGURE Women surpass men in CVD deaths
Over the past 25 years, the trend in deaths attributable to cardiovascular disease has been upward for women, while it is shifting downward for men.
Why focus on HDL?
Improvement in HDL is the strongest predictor of reduced risk for cardiac events. So says an analysis of 17 major lipid intervention trials between 1987 and 2003 (n = 44,170).2
Another study3 demonstrated that HDL cholesterol is the stronger predictor of CVD risk in women. In addition, several large observational studies have shown that increasing HDL cholesterol by 1 mg/dL in men reduces CVD risk by 2%, whereas increasing HDL in women by 1 mg/dL decreases CVD risk by 3%.4
Higher HDL levels may explain later onset of CVD in women. The advantage that women have over men in CVD risk prior to menopause seems to be at least partly due to their higher levels of HDL cholesterol: The average HDL level in women is 56 mg/dL, versus 46 mg/dL in men. This advantage begins to disappear after menopause, presumably because of changes in hormone levels and decreasing HDL-2 cholesterol, the most cardioprotective HDL fraction.
Other reasons to focus on HDL. In addition to the increased CVD risk associated with menopause, women of all ages in the United States have an increasing tendency—at almost epidemic rates—toward obesity and metabolic syndrome, which are known CVD risk factors.5 The dyslipidemia seen with those conditions is characterized by low HDL cholesterol and high triglycerides. Thus, maintaining healthy HDL levels is clearly an important goal for overall cardiovascular health, especially in women.
In addition, HDL is the key lipoprotein associated with reverse cholesterol transport, the process of carrying excess cholesterol from peripheral tissues to the liver for catabolism.
JUDY’S CASE
METABOLIC SYNDROME CONFIRMED
At her return visit, Judy’s blood pressure remains 140/90 mm Hg, with outside readings ranging from 135 to 145 mm Hg systolic and 85 to 95 mm Hg diastolic. Her laboratory tests reveal fasting blood glucose of 115 mg/dL, total cholesterol of 220 mg/dL, LDL cholesterol of 120 mg/dL, HDL cholesterol of 35 mg/dL, and triglycerides of 300 mg/dL.
What are her key heart-health issues?
Individualized management—recommended by NCEP/ATP III guidelines— should focus on reversing the metabolic defects of insulin resistance: hypertension, obesity, glucose intolerance, and dyslipidemia.
At present, Judy’s 10-year risk of a cardiac event is 4% by Framingham risk scoring, but it is likely to increase if the metabolic syndrome is not addressed.
How to preserve healthy HDL levels
Diet and regular aerobic exercise are recommended by the NCEP/ATP III guidelines, especially for obese patients with metabolic syndrome. However, dietary changes do not raise HDL cholesterol. In fact, dieting to lose weight will almost certainly lower HDL levels. That’s because people who eat a diet very low in fat tend to replace the fat calories with carbohydrates, and a low-fat, high-carbohydrate diet will reduce all cholesterol fractions—but HDL cholesterol will decrease disproportionately.6
Recommend complex carbohydrates and moderate fat intake
To avoid excessive reduction in HDL cholesterol, any weight-loss diet should involve moderate fat intake (35% of total calories) and emphasize monounsaturated fats such as olive or canola oil, along with complex carbohydrates found in fruits, vegetables, and whole grains.7 After weight loss is stabilized, HDL cholesterol tends to increase somewhat, but may not return all the way to baseline.
New guidelines on how to intervene
Most women who die suddenly from coronary heart disease had no previous symptoms, and that makes prevention all the more important.
Though it hasn’t been long since the first woman-centered recommendations on preventing cardiovascular disease,19 our understanding of preventive interventions has improved enormously. Thus, the American Heart Association convened a new expert panel to review and, where necessary, revise the original guidelines.20 Here are some of the highlights.
Forget “haves” and “have-nots”
Lori Mosca and the other members of the expert panel observe that “the concept of CVD as a categorical, ‘have-or-have-not’ condition has been replaced with a growing appreciation for the existence of a continuum of CVD risk.”20
For example, the low-risk category (<10% risk of a coronary heart disease event in the next 10 years, according to the Framingham Risk Score for women) would include women with optimal levels of risk factors and a heart-healthy lifestyle, as well as women with metabolic syndrome but no other risk factors. In contrast, women with established coronary heart disease, diabetes mellitus, or chronic kidney disease would fall into the high-risk group (>20% risk). Those with multiple risk factors or markedly elevated levels of a single risk factor fall somewhere in between.
The 5 lifestyle laws
Women are advised to consistently:
- eat plenty of fruits and vegetables, whole grains, and low-fat or nonfat dairy items
- avoid smoking and smokeless tobacco
- perform at least 30 minutes of moderate-intensity activity, such as brisk walking, most days
- achieve and maintain a body mass index between 18.5 and 25.9 kg/m2 and a waist circumference less than 35 inches
- consider omega-3 fatty acid supplementation, especially if risk is high. The guidelines extol the benefits of fish, which contain omega-3 fatty acids, but warn against consumption of fish likely to contain unsafe levels of mercury (shark, sword-fish, king mackerel, and tilefish) by gravidas and women of reproductive age.
BP and cholesterol control
- Blood pressure. Maintain at or below 120/80 mm Hg through lifestyle approaches, or drug therapy when BP is 140/90 mm Hg or higher.
- Dietary fat and cholesterol. Keep saturated fat intake to less than 7% of calories, and cholesterol below 200 mg/dL with high risk or elevated LDL.
- LDL-cholesterol. Use drug therapy (preferably statins) if risk is high and LDL is below 100 mg/dL. Add lifestyle adjustments if risk is high and LDL cholesterol is at or above 100 mg/dL.
What not to take to prevent CVD
The guidelines warn against prescribing—or continuing—estrogen-progestin therapy to prevent CVD. Nor should other forms of menopausal hormone therapy, such as unopposed estrogen, be prescribed or continued unless new findings indicate a beneficial role.
Also discouraged are antioxidant vitamin supplements to prevent CVD.
Look for depression
Especially women with CVD should be referred or treated when depression is found, as it can hamper a woman’s efforts at prevention.
The full text of the guidelines can be viewed at
http://circ.ahajournals.org/cgi/content/full/109/5/672.
Regular exercise raises HDL
One way to avoid an overall reduction in HDL levels with weight loss is to prescribe exercise in conjunction with it. Regular exercise is an excellent way to raise HDL cholesterol levels. Studies suggest that, for women, the volume of exercise is more important than intensity. Thus, women should strive to walk 7 to 14 miles per week or otherwise expend approximately 1,200 to 1,600 Kcal.8,9
Regular exercise is recommended as one of the NCEP/ATP III therapeutic lifestyle changes that directly benefit cardiovascular health and blood pressure and help the individual maintain optimal body weight. Although exercise raises HDL levels, it does so more easily in men than in women. HDL cholesterol increases in men with both intensity and volume of exercise.10 Women appear to derive slightly less of a benefit, perhaps because their HDL levels are already generally higher.
In women, studies have reported an increase in HDL cholesterol as high as 15% for both premenopausal and post-menopausal women who follow moderate exercise regimens—and the lower the baseline HDL level, the greater the increase.8
Exercise level was inversely associated with cardiovascular risk in the Women’s Health Initiative,9 which followed a cohort of 73,743 women prospectively for an average of 3.2 years. Women at the highest quintile of exercise level reduced their CVD risk by 53% over the lowest quintile, and moderate activity such as walking led to risk reductions similar to those involving more vigorous activities.
Recommend alcohol—or not?
Moderate alcohol consumption—1 to 3 drinks per day, or 15 to 45 g ethanol— improves lipoprotein levels and reduces CVD risk. The flavonoids in red wines also reduce platelet aggregation and clotting tendencies. However, advising a patient to consume alcohol to reduce her CVD risk is controversial; many physicians are reluctant to do so due to obvious concerns over toxicity and dependency.
Response to alcohol may vary by menopausal status. In 1 study,11 pre-menopausal women decreased their LDL cholesterol by 12% (P=.01) after 3 glasses of wine daily for 3 weeks, but there was no significant increase in HDL levels.
In the same study, postmenopausal women increased HDL levels by 12% (P=.03), but their LDL cholesterol decreased only minimally.11
Another study12 in postmenopausal women who consumed 0, 1, or 2 drinks daily (0, 15, or 30 g ethanol) for 8 weeks showed a significant decrease of 4% in LDL cholesterol at 1 drink (15 g), but no significant further decrease at 2 drinks (30 g). In the same study, HDL increased non-significantly at 1 drink (15 g), but increased significantly (5%) at 2 drinks (30 g). There may be a threshold of 30 g ethanol daily for postmenopausal women to benefit significantly from alcohol consumption.
JUDY’S CASE
LIFESTYLE RECOMMENDATIONS
The foundation of Judy’s management should be the triad of weight loss, exercise, and a diet that limits refined carbohydrates and emphasizes fiber, fruits and vegetables, whole grains, and healthy fats (ie, olive, canola, and fish oils).
In prescribing exercise, emphasize quantity over intensity, such as 14 miles of walking weekly or 60 to 90 minutes daily of aerobic activity.
Since she has no history of cardiac symptoms, and low-intensity, high-quantity exercise is advised, she does not need a screening cardiac stress test before beginning her regimen.
Pantethine
Pantethine is an over-the-counter (OTC) nutritional supplement that combines the B vitamin pantothenic acid with the amino acid cysteamine. Although pantothenic acid alone has no lipid-lowering effects, pantethine does: It lowers LDL cholesterol, very-low-density lipoprotein (VLDL) cholesterol, and triglycerides, and raises HDL levels. The exact mechanism of action is unknown, but it is thought to involve primarily the effects of cysteamine on lipid metabolism in the liver.
Recommended dose. At 600 to 900 mg daily, the typical response is an increase of up to 18% in HDL cholesterol and reductions in LDL cholesterol, VLDL cholesterol, and triglycerides of 13%, 20%, and 26%, respectively.13
In a recent US study, pantethine significantly raised HDL-2 cholesterol, the more cardioprotective fraction of HDL, and increased the particle size of LDL cholesterol, rendering it less atherogenic.14
Pantethine also reduces visceral fat. The same study14 reported a significant reduction in visceral fat, a component of metabolic syndrome, as measured by computerized dual-energy x-ray absorptiometry in individuals taking 900 mg daily for 6 weeks. This reduction appears to be primarily an effect of pantothenic acid and had been demonstrated in animal studies.
No side effects. Pantethine is exceptionally well tolerated, with virtually no side effects. An occasional person will experience gastrointestinal upset and diarrhea, which resolve when the drug is discontinued.
Recommend formulations that contain Pantesin (Daiichi Fine Chemicals, New York City), a pharmaceutical grade of pantethine, because extensive research confirms the benefits I have described. Otherwise, make sure the manufacturer is a reputable company, with scientific studies to support its claims of safety, efficacy, and bioavailability.
Nicotinic acid
Nicotinic acid (NA), another B vitamin available OTC as a nutritional supplement, is the most effective agent for raising HDL levels.
Recommended dose. A divided dose of 3,000 mg daily of the immediate-release form of NA can raise HDL levels as much as 30%. Unfortunately, that form of NA has a high incidence of adverse effects, such as flushing, itching, and GI upset.15
Sustained-release NA is generally well tolerated, but somewhat less effective at raising HDL. A lower dose of sustained-release NA (1,000 to 1,500 mg daily) is recommended to avoid liver toxicity and typically leads to HDL increases as high as 20%.15
NA offers additional benefits to the lipid profile, typically lowering LDL cholesterol by 20%, triglycerides by 15%, and lipoprotein(a) by 15%.15
Monitor all forms of NA with liver enzymes, blood glucose, and uric acid because treatment can elevate these markers.
Give NA preparations extra scrutiny. The general caveats about quality and bioavailability apply especially to NA. Nonprescription products on the market that contain nicotinamide and inositol hexanicotinate are advertised as “no-flush” niacin because they do not cause cutaneous side effects, but they also have no lipid benefits.
Cost. NA is relatively inexpensive, and good-quality sustained-release products such as Endur-acin (Endurance Products, Tigard, Ore) can be purchased OTC for 12 cents per 500-mg tablet or a daily cost of 24 to 36 cents.16
Sustained-release NA is also available by prescription (Niaspan, Kos Pharmaceuticals, Cranbury, NJ), but it is considerably more expensive ($1.98 per 500-mg tablet, or $3.96 to $5.94 daily) and has not been shown to be more effective or better tolerated than the better OTC products.16
JUDY’S CASE
RAISING HDL WITHOUT DRUGS
Judy’s lipid abnormalities would benefit from a supplement of pantethine (300 mg thrice daily) or NA (1,000 mg thrice daily of plain/quick release or 500 mg twice daily of sustained release to reduce flushing side effects).
Her greatest risk with her current lipid levels is low HDL, and the best agent to raise these levels is NA.
Pantethine also raises HDL and selectively improves the HDL-2 subfraction, which is most cardioprotective. Both supplements also improve the other lipid abnormalities.
In addition, referral to a dietician for detailed instruction in food choices and preparation may be useful.
Pharmacologic therapies
Hormone replacement therapy (HRT) is no longer recommended to prevent CVD and should be given only for menopausal symptoms during the perimenopausal years—despite the fact that estrogen has been shown to raise HDL cholesterol by 8% in postmenopausal women.17
Estrogens increase HDL by increasing production of apoA-1, the main lipoprotein in HDL, and by decreasing HDL catabolism by inhibiting hepatic lipase. The 17-hydroxyprogesterone component of HRT given to women with an intact uterus to prevent endometrial cancer has no significant lipid effects.
Paradoxically, the increased CVD risk found in the HRT arm of the Women’s Health Initiative17 was in the face of improved HDL (8%) and LDL (–14%) cholesterol and appeared to be the result of increased thrombotic events.
Further analysis of Women’s Health Initiative data showed that women who were still within 10 years of menopause actually did experience a reduction in CVD risk. That observation, along with some primate research on HRT, suggests that the risk or benefit of HRT with respect to CVD may be a matter of timing. See “Emerging hypothesis may explain estrogen paradox”
At the 2004 American Heart Association meeting, Dr. Thomas Clarkson, who has conducted primate research on hormone replacement therapy (HRT) and the risk of cardiovascular disease (CVD), described the emerging hypothesis that may explain the HRT paradox of increased CVD risk despite evidence of benefit in observational studies.21
Estrogen is a potent upregulator of matrix metal-loproteases. These proteolytic enzymes are a normal constituent of the endometrium and important in its remodeling with each menstrual cycle. Matrix metal-loproteases are also found in the fibrous cap that seals off the necrotic core of an advanced atheroma from the vascular lumen. Most perimenopausal women have enjoyed estrogen’s protective effect throughout their reproductive years and thus have developedlittle advanced atherosclerotic disease.
Ten or more years past menopause, however, clinically significant atherosclerotic lesions often develop in women who have been without the protection of estrogen. If estrogen is added at this stage, it causes increased matrix metalloprotease activity in the fibrous cap of any atheroma. This proteolytic activity can destabilize the fibrous cap, allowing necrotic core material to come in contact with the bloodstream.
This necrotic material is highly thrombogenic and stimulates clot formation in the vascular lumen. Clarkson demonstrated this process in research on perimenopausal and postmenopausal primates.
This hypothesis will soon be tested in a clinical trial in humans; CVD risk is expected to decrease by 50% to 70% in women who have taken HRT continuously from perimenopause.
Statins and other HDL-modifying drugs
The statins are a first choice for LDL reduction, but lead to only modest increases (4%–10%) in HDL levels.18 Fibric acid derivatives are somewhat more effective; they lead to increases in HDL of 6% to 18%. Both types of drugs are considerably more expensive than OTC NA and not as effective at raising HDL.
Combining statins with other agents that raise HDL has been tried: The NA–statin combination can be effective in managing dyslipidemias of both LDL and HDL. Fibric acid derivatives should not be used with statins because of the increased risk of serious myopathies.18
JUDY’S CASE
THERAPEUTIC TARGETS
Judy’s goals should include:
- reducing blood pressure to less than 120/80 mm Hg,
- decreasing weight to about 140 lb,
- achieving a waist measurement of less than 35 inches,
- reducing fasting blood glucose to less than 100 mg/dL,
- decreasing triglycerides to less than 150 mg/dL, total cholesterol to less than 200 mg/dL, and LDL levels to less than 100 mg/dL, and
- raising HDL to more than 45 mg/dL.
All these parameters should be checked every 3 months until the goals are achieved.
If Judy fails to progress or develops symptoms of heart disease, she should be referred to a cardiologist for further evaluation and more aggressive treatment.
The author reports no conflicts relevant to this article.
1. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285:2486-2497.
2. Alsheikh-Ali A, Abourjaily HM, Stanek EJ, et al. Increases in HDL-cholesterol are the strongest predictors of risk reduction in lipid intervention trials. Circulation. 2004;110(17 suppl 3):III-813.
3. Jacobs DR, Jr, Meban IL, Bangdiwala SI, et al. High density lipoprotein cholesterol as a predictor of cardiovascular disease mortality in men and women: the follow-up study of the Lipid Research Clinics Prevalence Study. Am J Epidemiol. 1990;131:32-47.
4. Gordon DJ, Probstfiel JL, Garrison RJ, et al. High-density lipoprotein cholesterol and cardiovascular disease: four prospective American studies. Circulation. 1989;79:8-15.
5. Hu Fb, Willet WC, Li T, et al. Adiposity as compared with physical activity in predicting mortality among women. N Engl J Med. 2004;351:2694-2703.
6. Mensink RP, Zock PL, Kester A, et al. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr. 2003;77:1146-1155.
7. Pereira MA, Swain J, Goldfine AB, et al. Effects of a low-glycemic load diet on resting energy expenditure and heart disease risk factors during weight loss. JAMA. 2004;292:2482-2490.
8. Kokkinos PF, Holland JC, Pittaras AE, et al. Cardiorespiratory fitness and coronary heart disease risk factor association in women. J Am Coll Cardiol. 1995;26:358-364.
9. Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347:716-725.
10. Kokkinos PE, Fernhall B. Physical activity and high density lipoprotein cholesterol levels: what is the relationship? Sports Med. 1999;28:307-314.
11. Van Der Gaag MS, Sterksma A, Schaafsma G, et al. Moderate alcohol consumption lowers risk factors for cardiovascular disease in postmenopausal women fed a controlled diet. Am J Clin Nutr. 2002;75:593-599.
12. Baer DJ, Judd JT, Clevidence BA, et al. Moderate alcohol consumption and changes in postprandial lipoproteins of premenopausal and postmenopausal women: a diet-controlled randomized intervention study. J Womens Health Gend Based Med. 2000;9:607-616.
13. Pins JJ, Keenan JM. Pantethine: a new option in managing dyslipidemia. J Am College Nutr. 2005 [in press].
14. Pins JJ, First S, Shamliyan T, Keenan J. Pantethine beneficially affects apolipoprotein A-1, apolipoprotein B, low-density lipoprotein particle size but not high-sensitivity C-reactive protein in a dyslipidemic population. Circulation. 2004;110(17 suppl 3):III-778.
15. Crouse JR, 3rd. New developments in the use of niacin for treatment of hyperlipidemia: new considerations in the use of an old drug. Coron Artery Dis. 1996;7:321-326.
16. Retail pharmacy quote. Walgreen’s Pharmacy, Minneapolis, Minn. January 2005.
17. Risks and benefits of estrogen plus progestin in healthy post-menopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
18. Hersberger M, von Eckardstein A. Low high-density lipoprotein cholesterol: physical background, clinical importance and drug treatment. Drugs. 2003;63:1907-1945.
19. Mosca L, Grundy SM, Judelson D, et al. Guide to preventive cardiology for women. AHA/ACC scientific statement, consensus panel statement. irculation. 1999;99:2480-2484.
20. Mosca L, Appel LJ, Benjamin EJ, et al. AHA Guidelines: evidence-based guidelines for cardiovascular disease prevention in women. Circulation. 2004;109:672-693.
21. Clarkson T. Women’s Heart Health Symposium. Presented at the American Heart Association annual meeting, Nov 9, 2004, New Orleans.
JUDY’S CASE
“WHAT’S MY RISK?”
At her periodic gynecologic exam, Judy, a 58-year-old white woman, expresses concern about her heart health in light of her 62-year-old sister’s recent heart attack. Further questioning reveals that her father died of a heart attack at age 56, and her brother, 52, has high blood pressure and adult-onset diabetes.
Judy has not experienced any symptoms of cardiovascular disease, such as chest pain or tightness with exertion, and she doesn’t smoke. The last time her cholesterol was checked was about 15 years earlier, at which time it was “OK.” She admits she is not very physically active and has gained about 30 lb over the past 10 years. Her vital signs and physical exam are entirely normal except for borderline high blood pressure at 140/90 mm Hg, weight of 170 lb (height: 68 inches), and a waist circumference of 37 inches.
What is her cardiovascular risk?
Judy has physical findings suggestive of metabolic syndrome in addition to the significant family history of cardiovascular disease (CVD). Although her current risk of a cardiac event appears to be low, she is likely to deteriorate if the hypertension and excess body weight are not addressed.
To predict her level of risk more precisely, the physician asks Judy to return in 2 weeks for a blood pressure recheck, and instructs her to perform additional readings on her own. The clinician also refers Judy for a fasting lipid panel and blood glucose level.
In women, CVD is especially lethal
Contrary to earlier assumptions, CVD now appears to be more lethal in women than in men and warrants aggressive efforts to prevent it and manage risk factors (FIGURE). This article focuses on improving high-density lipoprotein (HDL) cholesterol, a key factor in women at risk.
This approach differs slightly from the National Cholesterol Education Program Adult Treatment Panel III (NCEP/ATP III) guidelines, which target low-density lipoprotein (LDL) cholesterol as the primary lipid risk factor for intervention.1
FIGURE Women surpass men in CVD deaths
Over the past 25 years, the trend in deaths attributable to cardiovascular disease has been upward for women, while it is shifting downward for men.
Why focus on HDL?
Improvement in HDL is the strongest predictor of reduced risk for cardiac events. So says an analysis of 17 major lipid intervention trials between 1987 and 2003 (n = 44,170).2
Another study3 demonstrated that HDL cholesterol is the stronger predictor of CVD risk in women. In addition, several large observational studies have shown that increasing HDL cholesterol by 1 mg/dL in men reduces CVD risk by 2%, whereas increasing HDL in women by 1 mg/dL decreases CVD risk by 3%.4
Higher HDL levels may explain later onset of CVD in women. The advantage that women have over men in CVD risk prior to menopause seems to be at least partly due to their higher levels of HDL cholesterol: The average HDL level in women is 56 mg/dL, versus 46 mg/dL in men. This advantage begins to disappear after menopause, presumably because of changes in hormone levels and decreasing HDL-2 cholesterol, the most cardioprotective HDL fraction.
Other reasons to focus on HDL. In addition to the increased CVD risk associated with menopause, women of all ages in the United States have an increasing tendency—at almost epidemic rates—toward obesity and metabolic syndrome, which are known CVD risk factors.5 The dyslipidemia seen with those conditions is characterized by low HDL cholesterol and high triglycerides. Thus, maintaining healthy HDL levels is clearly an important goal for overall cardiovascular health, especially in women.
In addition, HDL is the key lipoprotein associated with reverse cholesterol transport, the process of carrying excess cholesterol from peripheral tissues to the liver for catabolism.
JUDY’S CASE
METABOLIC SYNDROME CONFIRMED
At her return visit, Judy’s blood pressure remains 140/90 mm Hg, with outside readings ranging from 135 to 145 mm Hg systolic and 85 to 95 mm Hg diastolic. Her laboratory tests reveal fasting blood glucose of 115 mg/dL, total cholesterol of 220 mg/dL, LDL cholesterol of 120 mg/dL, HDL cholesterol of 35 mg/dL, and triglycerides of 300 mg/dL.
What are her key heart-health issues?
Individualized management—recommended by NCEP/ATP III guidelines— should focus on reversing the metabolic defects of insulin resistance: hypertension, obesity, glucose intolerance, and dyslipidemia.
At present, Judy’s 10-year risk of a cardiac event is 4% by Framingham risk scoring, but it is likely to increase if the metabolic syndrome is not addressed.
How to preserve healthy HDL levels
Diet and regular aerobic exercise are recommended by the NCEP/ATP III guidelines, especially for obese patients with metabolic syndrome. However, dietary changes do not raise HDL cholesterol. In fact, dieting to lose weight will almost certainly lower HDL levels. That’s because people who eat a diet very low in fat tend to replace the fat calories with carbohydrates, and a low-fat, high-carbohydrate diet will reduce all cholesterol fractions—but HDL cholesterol will decrease disproportionately.6
Recommend complex carbohydrates and moderate fat intake
To avoid excessive reduction in HDL cholesterol, any weight-loss diet should involve moderate fat intake (35% of total calories) and emphasize monounsaturated fats such as olive or canola oil, along with complex carbohydrates found in fruits, vegetables, and whole grains.7 After weight loss is stabilized, HDL cholesterol tends to increase somewhat, but may not return all the way to baseline.
New guidelines on how to intervene
Most women who die suddenly from coronary heart disease had no previous symptoms, and that makes prevention all the more important.
Though it hasn’t been long since the first woman-centered recommendations on preventing cardiovascular disease,19 our understanding of preventive interventions has improved enormously. Thus, the American Heart Association convened a new expert panel to review and, where necessary, revise the original guidelines.20 Here are some of the highlights.
Forget “haves” and “have-nots”
Lori Mosca and the other members of the expert panel observe that “the concept of CVD as a categorical, ‘have-or-have-not’ condition has been replaced with a growing appreciation for the existence of a continuum of CVD risk.”20
For example, the low-risk category (<10% risk of a coronary heart disease event in the next 10 years, according to the Framingham Risk Score for women) would include women with optimal levels of risk factors and a heart-healthy lifestyle, as well as women with metabolic syndrome but no other risk factors. In contrast, women with established coronary heart disease, diabetes mellitus, or chronic kidney disease would fall into the high-risk group (>20% risk). Those with multiple risk factors or markedly elevated levels of a single risk factor fall somewhere in between.
The 5 lifestyle laws
Women are advised to consistently:
- eat plenty of fruits and vegetables, whole grains, and low-fat or nonfat dairy items
- avoid smoking and smokeless tobacco
- perform at least 30 minutes of moderate-intensity activity, such as brisk walking, most days
- achieve and maintain a body mass index between 18.5 and 25.9 kg/m2 and a waist circumference less than 35 inches
- consider omega-3 fatty acid supplementation, especially if risk is high. The guidelines extol the benefits of fish, which contain omega-3 fatty acids, but warn against consumption of fish likely to contain unsafe levels of mercury (shark, sword-fish, king mackerel, and tilefish) by gravidas and women of reproductive age.
BP and cholesterol control
- Blood pressure. Maintain at or below 120/80 mm Hg through lifestyle approaches, or drug therapy when BP is 140/90 mm Hg or higher.
- Dietary fat and cholesterol. Keep saturated fat intake to less than 7% of calories, and cholesterol below 200 mg/dL with high risk or elevated LDL.
- LDL-cholesterol. Use drug therapy (preferably statins) if risk is high and LDL is below 100 mg/dL. Add lifestyle adjustments if risk is high and LDL cholesterol is at or above 100 mg/dL.
What not to take to prevent CVD
The guidelines warn against prescribing—or continuing—estrogen-progestin therapy to prevent CVD. Nor should other forms of menopausal hormone therapy, such as unopposed estrogen, be prescribed or continued unless new findings indicate a beneficial role.
Also discouraged are antioxidant vitamin supplements to prevent CVD.
Look for depression
Especially women with CVD should be referred or treated when depression is found, as it can hamper a woman’s efforts at prevention.
The full text of the guidelines can be viewed at
http://circ.ahajournals.org/cgi/content/full/109/5/672.
Regular exercise raises HDL
One way to avoid an overall reduction in HDL levels with weight loss is to prescribe exercise in conjunction with it. Regular exercise is an excellent way to raise HDL cholesterol levels. Studies suggest that, for women, the volume of exercise is more important than intensity. Thus, women should strive to walk 7 to 14 miles per week or otherwise expend approximately 1,200 to 1,600 Kcal.8,9
Regular exercise is recommended as one of the NCEP/ATP III therapeutic lifestyle changes that directly benefit cardiovascular health and blood pressure and help the individual maintain optimal body weight. Although exercise raises HDL levels, it does so more easily in men than in women. HDL cholesterol increases in men with both intensity and volume of exercise.10 Women appear to derive slightly less of a benefit, perhaps because their HDL levels are already generally higher.
In women, studies have reported an increase in HDL cholesterol as high as 15% for both premenopausal and post-menopausal women who follow moderate exercise regimens—and the lower the baseline HDL level, the greater the increase.8
Exercise level was inversely associated with cardiovascular risk in the Women’s Health Initiative,9 which followed a cohort of 73,743 women prospectively for an average of 3.2 years. Women at the highest quintile of exercise level reduced their CVD risk by 53% over the lowest quintile, and moderate activity such as walking led to risk reductions similar to those involving more vigorous activities.
Recommend alcohol—or not?
Moderate alcohol consumption—1 to 3 drinks per day, or 15 to 45 g ethanol— improves lipoprotein levels and reduces CVD risk. The flavonoids in red wines also reduce platelet aggregation and clotting tendencies. However, advising a patient to consume alcohol to reduce her CVD risk is controversial; many physicians are reluctant to do so due to obvious concerns over toxicity and dependency.
Response to alcohol may vary by menopausal status. In 1 study,11 pre-menopausal women decreased their LDL cholesterol by 12% (P=.01) after 3 glasses of wine daily for 3 weeks, but there was no significant increase in HDL levels.
In the same study, postmenopausal women increased HDL levels by 12% (P=.03), but their LDL cholesterol decreased only minimally.11
Another study12 in postmenopausal women who consumed 0, 1, or 2 drinks daily (0, 15, or 30 g ethanol) for 8 weeks showed a significant decrease of 4% in LDL cholesterol at 1 drink (15 g), but no significant further decrease at 2 drinks (30 g). In the same study, HDL increased non-significantly at 1 drink (15 g), but increased significantly (5%) at 2 drinks (30 g). There may be a threshold of 30 g ethanol daily for postmenopausal women to benefit significantly from alcohol consumption.
JUDY’S CASE
LIFESTYLE RECOMMENDATIONS
The foundation of Judy’s management should be the triad of weight loss, exercise, and a diet that limits refined carbohydrates and emphasizes fiber, fruits and vegetables, whole grains, and healthy fats (ie, olive, canola, and fish oils).
In prescribing exercise, emphasize quantity over intensity, such as 14 miles of walking weekly or 60 to 90 minutes daily of aerobic activity.
Since she has no history of cardiac symptoms, and low-intensity, high-quantity exercise is advised, she does not need a screening cardiac stress test before beginning her regimen.
Pantethine
Pantethine is an over-the-counter (OTC) nutritional supplement that combines the B vitamin pantothenic acid with the amino acid cysteamine. Although pantothenic acid alone has no lipid-lowering effects, pantethine does: It lowers LDL cholesterol, very-low-density lipoprotein (VLDL) cholesterol, and triglycerides, and raises HDL levels. The exact mechanism of action is unknown, but it is thought to involve primarily the effects of cysteamine on lipid metabolism in the liver.
Recommended dose. At 600 to 900 mg daily, the typical response is an increase of up to 18% in HDL cholesterol and reductions in LDL cholesterol, VLDL cholesterol, and triglycerides of 13%, 20%, and 26%, respectively.13
In a recent US study, pantethine significantly raised HDL-2 cholesterol, the more cardioprotective fraction of HDL, and increased the particle size of LDL cholesterol, rendering it less atherogenic.14
Pantethine also reduces visceral fat. The same study14 reported a significant reduction in visceral fat, a component of metabolic syndrome, as measured by computerized dual-energy x-ray absorptiometry in individuals taking 900 mg daily for 6 weeks. This reduction appears to be primarily an effect of pantothenic acid and had been demonstrated in animal studies.
No side effects. Pantethine is exceptionally well tolerated, with virtually no side effects. An occasional person will experience gastrointestinal upset and diarrhea, which resolve when the drug is discontinued.
Recommend formulations that contain Pantesin (Daiichi Fine Chemicals, New York City), a pharmaceutical grade of pantethine, because extensive research confirms the benefits I have described. Otherwise, make sure the manufacturer is a reputable company, with scientific studies to support its claims of safety, efficacy, and bioavailability.
Nicotinic acid
Nicotinic acid (NA), another B vitamin available OTC as a nutritional supplement, is the most effective agent for raising HDL levels.
Recommended dose. A divided dose of 3,000 mg daily of the immediate-release form of NA can raise HDL levels as much as 30%. Unfortunately, that form of NA has a high incidence of adverse effects, such as flushing, itching, and GI upset.15
Sustained-release NA is generally well tolerated, but somewhat less effective at raising HDL. A lower dose of sustained-release NA (1,000 to 1,500 mg daily) is recommended to avoid liver toxicity and typically leads to HDL increases as high as 20%.15
NA offers additional benefits to the lipid profile, typically lowering LDL cholesterol by 20%, triglycerides by 15%, and lipoprotein(a) by 15%.15
Monitor all forms of NA with liver enzymes, blood glucose, and uric acid because treatment can elevate these markers.
Give NA preparations extra scrutiny. The general caveats about quality and bioavailability apply especially to NA. Nonprescription products on the market that contain nicotinamide and inositol hexanicotinate are advertised as “no-flush” niacin because they do not cause cutaneous side effects, but they also have no lipid benefits.
Cost. NA is relatively inexpensive, and good-quality sustained-release products such as Endur-acin (Endurance Products, Tigard, Ore) can be purchased OTC for 12 cents per 500-mg tablet or a daily cost of 24 to 36 cents.16
Sustained-release NA is also available by prescription (Niaspan, Kos Pharmaceuticals, Cranbury, NJ), but it is considerably more expensive ($1.98 per 500-mg tablet, or $3.96 to $5.94 daily) and has not been shown to be more effective or better tolerated than the better OTC products.16
JUDY’S CASE
RAISING HDL WITHOUT DRUGS
Judy’s lipid abnormalities would benefit from a supplement of pantethine (300 mg thrice daily) or NA (1,000 mg thrice daily of plain/quick release or 500 mg twice daily of sustained release to reduce flushing side effects).
Her greatest risk with her current lipid levels is low HDL, and the best agent to raise these levels is NA.
Pantethine also raises HDL and selectively improves the HDL-2 subfraction, which is most cardioprotective. Both supplements also improve the other lipid abnormalities.
In addition, referral to a dietician for detailed instruction in food choices and preparation may be useful.
Pharmacologic therapies
Hormone replacement therapy (HRT) is no longer recommended to prevent CVD and should be given only for menopausal symptoms during the perimenopausal years—despite the fact that estrogen has been shown to raise HDL cholesterol by 8% in postmenopausal women.17
Estrogens increase HDL by increasing production of apoA-1, the main lipoprotein in HDL, and by decreasing HDL catabolism by inhibiting hepatic lipase. The 17-hydroxyprogesterone component of HRT given to women with an intact uterus to prevent endometrial cancer has no significant lipid effects.
Paradoxically, the increased CVD risk found in the HRT arm of the Women’s Health Initiative17 was in the face of improved HDL (8%) and LDL (–14%) cholesterol and appeared to be the result of increased thrombotic events.
Further analysis of Women’s Health Initiative data showed that women who were still within 10 years of menopause actually did experience a reduction in CVD risk. That observation, along with some primate research on HRT, suggests that the risk or benefit of HRT with respect to CVD may be a matter of timing. See “Emerging hypothesis may explain estrogen paradox”
At the 2004 American Heart Association meeting, Dr. Thomas Clarkson, who has conducted primate research on hormone replacement therapy (HRT) and the risk of cardiovascular disease (CVD), described the emerging hypothesis that may explain the HRT paradox of increased CVD risk despite evidence of benefit in observational studies.21
Estrogen is a potent upregulator of matrix metal-loproteases. These proteolytic enzymes are a normal constituent of the endometrium and important in its remodeling with each menstrual cycle. Matrix metal-loproteases are also found in the fibrous cap that seals off the necrotic core of an advanced atheroma from the vascular lumen. Most perimenopausal women have enjoyed estrogen’s protective effect throughout their reproductive years and thus have developedlittle advanced atherosclerotic disease.
Ten or more years past menopause, however, clinically significant atherosclerotic lesions often develop in women who have been without the protection of estrogen. If estrogen is added at this stage, it causes increased matrix metalloprotease activity in the fibrous cap of any atheroma. This proteolytic activity can destabilize the fibrous cap, allowing necrotic core material to come in contact with the bloodstream.
This necrotic material is highly thrombogenic and stimulates clot formation in the vascular lumen. Clarkson demonstrated this process in research on perimenopausal and postmenopausal primates.
This hypothesis will soon be tested in a clinical trial in humans; CVD risk is expected to decrease by 50% to 70% in women who have taken HRT continuously from perimenopause.
Statins and other HDL-modifying drugs
The statins are a first choice for LDL reduction, but lead to only modest increases (4%–10%) in HDL levels.18 Fibric acid derivatives are somewhat more effective; they lead to increases in HDL of 6% to 18%. Both types of drugs are considerably more expensive than OTC NA and not as effective at raising HDL.
Combining statins with other agents that raise HDL has been tried: The NA–statin combination can be effective in managing dyslipidemias of both LDL and HDL. Fibric acid derivatives should not be used with statins because of the increased risk of serious myopathies.18
JUDY’S CASE
THERAPEUTIC TARGETS
Judy’s goals should include:
- reducing blood pressure to less than 120/80 mm Hg,
- decreasing weight to about 140 lb,
- achieving a waist measurement of less than 35 inches,
- reducing fasting blood glucose to less than 100 mg/dL,
- decreasing triglycerides to less than 150 mg/dL, total cholesterol to less than 200 mg/dL, and LDL levels to less than 100 mg/dL, and
- raising HDL to more than 45 mg/dL.
All these parameters should be checked every 3 months until the goals are achieved.
If Judy fails to progress or develops symptoms of heart disease, she should be referred to a cardiologist for further evaluation and more aggressive treatment.
The author reports no conflicts relevant to this article.
JUDY’S CASE
“WHAT’S MY RISK?”
At her periodic gynecologic exam, Judy, a 58-year-old white woman, expresses concern about her heart health in light of her 62-year-old sister’s recent heart attack. Further questioning reveals that her father died of a heart attack at age 56, and her brother, 52, has high blood pressure and adult-onset diabetes.
Judy has not experienced any symptoms of cardiovascular disease, such as chest pain or tightness with exertion, and she doesn’t smoke. The last time her cholesterol was checked was about 15 years earlier, at which time it was “OK.” She admits she is not very physically active and has gained about 30 lb over the past 10 years. Her vital signs and physical exam are entirely normal except for borderline high blood pressure at 140/90 mm Hg, weight of 170 lb (height: 68 inches), and a waist circumference of 37 inches.
What is her cardiovascular risk?
Judy has physical findings suggestive of metabolic syndrome in addition to the significant family history of cardiovascular disease (CVD). Although her current risk of a cardiac event appears to be low, she is likely to deteriorate if the hypertension and excess body weight are not addressed.
To predict her level of risk more precisely, the physician asks Judy to return in 2 weeks for a blood pressure recheck, and instructs her to perform additional readings on her own. The clinician also refers Judy for a fasting lipid panel and blood glucose level.
In women, CVD is especially lethal
Contrary to earlier assumptions, CVD now appears to be more lethal in women than in men and warrants aggressive efforts to prevent it and manage risk factors (FIGURE). This article focuses on improving high-density lipoprotein (HDL) cholesterol, a key factor in women at risk.
This approach differs slightly from the National Cholesterol Education Program Adult Treatment Panel III (NCEP/ATP III) guidelines, which target low-density lipoprotein (LDL) cholesterol as the primary lipid risk factor for intervention.1
FIGURE Women surpass men in CVD deaths
Over the past 25 years, the trend in deaths attributable to cardiovascular disease has been upward for women, while it is shifting downward for men.
Why focus on HDL?
Improvement in HDL is the strongest predictor of reduced risk for cardiac events. So says an analysis of 17 major lipid intervention trials between 1987 and 2003 (n = 44,170).2
Another study3 demonstrated that HDL cholesterol is the stronger predictor of CVD risk in women. In addition, several large observational studies have shown that increasing HDL cholesterol by 1 mg/dL in men reduces CVD risk by 2%, whereas increasing HDL in women by 1 mg/dL decreases CVD risk by 3%.4
Higher HDL levels may explain later onset of CVD in women. The advantage that women have over men in CVD risk prior to menopause seems to be at least partly due to their higher levels of HDL cholesterol: The average HDL level in women is 56 mg/dL, versus 46 mg/dL in men. This advantage begins to disappear after menopause, presumably because of changes in hormone levels and decreasing HDL-2 cholesterol, the most cardioprotective HDL fraction.
Other reasons to focus on HDL. In addition to the increased CVD risk associated with menopause, women of all ages in the United States have an increasing tendency—at almost epidemic rates—toward obesity and metabolic syndrome, which are known CVD risk factors.5 The dyslipidemia seen with those conditions is characterized by low HDL cholesterol and high triglycerides. Thus, maintaining healthy HDL levels is clearly an important goal for overall cardiovascular health, especially in women.
In addition, HDL is the key lipoprotein associated with reverse cholesterol transport, the process of carrying excess cholesterol from peripheral tissues to the liver for catabolism.
JUDY’S CASE
METABOLIC SYNDROME CONFIRMED
At her return visit, Judy’s blood pressure remains 140/90 mm Hg, with outside readings ranging from 135 to 145 mm Hg systolic and 85 to 95 mm Hg diastolic. Her laboratory tests reveal fasting blood glucose of 115 mg/dL, total cholesterol of 220 mg/dL, LDL cholesterol of 120 mg/dL, HDL cholesterol of 35 mg/dL, and triglycerides of 300 mg/dL.
What are her key heart-health issues?
Individualized management—recommended by NCEP/ATP III guidelines— should focus on reversing the metabolic defects of insulin resistance: hypertension, obesity, glucose intolerance, and dyslipidemia.
At present, Judy’s 10-year risk of a cardiac event is 4% by Framingham risk scoring, but it is likely to increase if the metabolic syndrome is not addressed.
How to preserve healthy HDL levels
Diet and regular aerobic exercise are recommended by the NCEP/ATP III guidelines, especially for obese patients with metabolic syndrome. However, dietary changes do not raise HDL cholesterol. In fact, dieting to lose weight will almost certainly lower HDL levels. That’s because people who eat a diet very low in fat tend to replace the fat calories with carbohydrates, and a low-fat, high-carbohydrate diet will reduce all cholesterol fractions—but HDL cholesterol will decrease disproportionately.6
Recommend complex carbohydrates and moderate fat intake
To avoid excessive reduction in HDL cholesterol, any weight-loss diet should involve moderate fat intake (35% of total calories) and emphasize monounsaturated fats such as olive or canola oil, along with complex carbohydrates found in fruits, vegetables, and whole grains.7 After weight loss is stabilized, HDL cholesterol tends to increase somewhat, but may not return all the way to baseline.
New guidelines on how to intervene
Most women who die suddenly from coronary heart disease had no previous symptoms, and that makes prevention all the more important.
Though it hasn’t been long since the first woman-centered recommendations on preventing cardiovascular disease,19 our understanding of preventive interventions has improved enormously. Thus, the American Heart Association convened a new expert panel to review and, where necessary, revise the original guidelines.20 Here are some of the highlights.
Forget “haves” and “have-nots”
Lori Mosca and the other members of the expert panel observe that “the concept of CVD as a categorical, ‘have-or-have-not’ condition has been replaced with a growing appreciation for the existence of a continuum of CVD risk.”20
For example, the low-risk category (<10% risk of a coronary heart disease event in the next 10 years, according to the Framingham Risk Score for women) would include women with optimal levels of risk factors and a heart-healthy lifestyle, as well as women with metabolic syndrome but no other risk factors. In contrast, women with established coronary heart disease, diabetes mellitus, or chronic kidney disease would fall into the high-risk group (>20% risk). Those with multiple risk factors or markedly elevated levels of a single risk factor fall somewhere in between.
The 5 lifestyle laws
Women are advised to consistently:
- eat plenty of fruits and vegetables, whole grains, and low-fat or nonfat dairy items
- avoid smoking and smokeless tobacco
- perform at least 30 minutes of moderate-intensity activity, such as brisk walking, most days
- achieve and maintain a body mass index between 18.5 and 25.9 kg/m2 and a waist circumference less than 35 inches
- consider omega-3 fatty acid supplementation, especially if risk is high. The guidelines extol the benefits of fish, which contain omega-3 fatty acids, but warn against consumption of fish likely to contain unsafe levels of mercury (shark, sword-fish, king mackerel, and tilefish) by gravidas and women of reproductive age.
BP and cholesterol control
- Blood pressure. Maintain at or below 120/80 mm Hg through lifestyle approaches, or drug therapy when BP is 140/90 mm Hg or higher.
- Dietary fat and cholesterol. Keep saturated fat intake to less than 7% of calories, and cholesterol below 200 mg/dL with high risk or elevated LDL.
- LDL-cholesterol. Use drug therapy (preferably statins) if risk is high and LDL is below 100 mg/dL. Add lifestyle adjustments if risk is high and LDL cholesterol is at or above 100 mg/dL.
What not to take to prevent CVD
The guidelines warn against prescribing—or continuing—estrogen-progestin therapy to prevent CVD. Nor should other forms of menopausal hormone therapy, such as unopposed estrogen, be prescribed or continued unless new findings indicate a beneficial role.
Also discouraged are antioxidant vitamin supplements to prevent CVD.
Look for depression
Especially women with CVD should be referred or treated when depression is found, as it can hamper a woman’s efforts at prevention.
The full text of the guidelines can be viewed at
http://circ.ahajournals.org/cgi/content/full/109/5/672.
Regular exercise raises HDL
One way to avoid an overall reduction in HDL levels with weight loss is to prescribe exercise in conjunction with it. Regular exercise is an excellent way to raise HDL cholesterol levels. Studies suggest that, for women, the volume of exercise is more important than intensity. Thus, women should strive to walk 7 to 14 miles per week or otherwise expend approximately 1,200 to 1,600 Kcal.8,9
Regular exercise is recommended as one of the NCEP/ATP III therapeutic lifestyle changes that directly benefit cardiovascular health and blood pressure and help the individual maintain optimal body weight. Although exercise raises HDL levels, it does so more easily in men than in women. HDL cholesterol increases in men with both intensity and volume of exercise.10 Women appear to derive slightly less of a benefit, perhaps because their HDL levels are already generally higher.
In women, studies have reported an increase in HDL cholesterol as high as 15% for both premenopausal and post-menopausal women who follow moderate exercise regimens—and the lower the baseline HDL level, the greater the increase.8
Exercise level was inversely associated with cardiovascular risk in the Women’s Health Initiative,9 which followed a cohort of 73,743 women prospectively for an average of 3.2 years. Women at the highest quintile of exercise level reduced their CVD risk by 53% over the lowest quintile, and moderate activity such as walking led to risk reductions similar to those involving more vigorous activities.
Recommend alcohol—or not?
Moderate alcohol consumption—1 to 3 drinks per day, or 15 to 45 g ethanol— improves lipoprotein levels and reduces CVD risk. The flavonoids in red wines also reduce platelet aggregation and clotting tendencies. However, advising a patient to consume alcohol to reduce her CVD risk is controversial; many physicians are reluctant to do so due to obvious concerns over toxicity and dependency.
Response to alcohol may vary by menopausal status. In 1 study,11 pre-menopausal women decreased their LDL cholesterol by 12% (P=.01) after 3 glasses of wine daily for 3 weeks, but there was no significant increase in HDL levels.
In the same study, postmenopausal women increased HDL levels by 12% (P=.03), but their LDL cholesterol decreased only minimally.11
Another study12 in postmenopausal women who consumed 0, 1, or 2 drinks daily (0, 15, or 30 g ethanol) for 8 weeks showed a significant decrease of 4% in LDL cholesterol at 1 drink (15 g), but no significant further decrease at 2 drinks (30 g). In the same study, HDL increased non-significantly at 1 drink (15 g), but increased significantly (5%) at 2 drinks (30 g). There may be a threshold of 30 g ethanol daily for postmenopausal women to benefit significantly from alcohol consumption.
JUDY’S CASE
LIFESTYLE RECOMMENDATIONS
The foundation of Judy’s management should be the triad of weight loss, exercise, and a diet that limits refined carbohydrates and emphasizes fiber, fruits and vegetables, whole grains, and healthy fats (ie, olive, canola, and fish oils).
In prescribing exercise, emphasize quantity over intensity, such as 14 miles of walking weekly or 60 to 90 minutes daily of aerobic activity.
Since she has no history of cardiac symptoms, and low-intensity, high-quantity exercise is advised, she does not need a screening cardiac stress test before beginning her regimen.
Pantethine
Pantethine is an over-the-counter (OTC) nutritional supplement that combines the B vitamin pantothenic acid with the amino acid cysteamine. Although pantothenic acid alone has no lipid-lowering effects, pantethine does: It lowers LDL cholesterol, very-low-density lipoprotein (VLDL) cholesterol, and triglycerides, and raises HDL levels. The exact mechanism of action is unknown, but it is thought to involve primarily the effects of cysteamine on lipid metabolism in the liver.
Recommended dose. At 600 to 900 mg daily, the typical response is an increase of up to 18% in HDL cholesterol and reductions in LDL cholesterol, VLDL cholesterol, and triglycerides of 13%, 20%, and 26%, respectively.13
In a recent US study, pantethine significantly raised HDL-2 cholesterol, the more cardioprotective fraction of HDL, and increased the particle size of LDL cholesterol, rendering it less atherogenic.14
Pantethine also reduces visceral fat. The same study14 reported a significant reduction in visceral fat, a component of metabolic syndrome, as measured by computerized dual-energy x-ray absorptiometry in individuals taking 900 mg daily for 6 weeks. This reduction appears to be primarily an effect of pantothenic acid and had been demonstrated in animal studies.
No side effects. Pantethine is exceptionally well tolerated, with virtually no side effects. An occasional person will experience gastrointestinal upset and diarrhea, which resolve when the drug is discontinued.
Recommend formulations that contain Pantesin (Daiichi Fine Chemicals, New York City), a pharmaceutical grade of pantethine, because extensive research confirms the benefits I have described. Otherwise, make sure the manufacturer is a reputable company, with scientific studies to support its claims of safety, efficacy, and bioavailability.
Nicotinic acid
Nicotinic acid (NA), another B vitamin available OTC as a nutritional supplement, is the most effective agent for raising HDL levels.
Recommended dose. A divided dose of 3,000 mg daily of the immediate-release form of NA can raise HDL levels as much as 30%. Unfortunately, that form of NA has a high incidence of adverse effects, such as flushing, itching, and GI upset.15
Sustained-release NA is generally well tolerated, but somewhat less effective at raising HDL. A lower dose of sustained-release NA (1,000 to 1,500 mg daily) is recommended to avoid liver toxicity and typically leads to HDL increases as high as 20%.15
NA offers additional benefits to the lipid profile, typically lowering LDL cholesterol by 20%, triglycerides by 15%, and lipoprotein(a) by 15%.15
Monitor all forms of NA with liver enzymes, blood glucose, and uric acid because treatment can elevate these markers.
Give NA preparations extra scrutiny. The general caveats about quality and bioavailability apply especially to NA. Nonprescription products on the market that contain nicotinamide and inositol hexanicotinate are advertised as “no-flush” niacin because they do not cause cutaneous side effects, but they also have no lipid benefits.
Cost. NA is relatively inexpensive, and good-quality sustained-release products such as Endur-acin (Endurance Products, Tigard, Ore) can be purchased OTC for 12 cents per 500-mg tablet or a daily cost of 24 to 36 cents.16
Sustained-release NA is also available by prescription (Niaspan, Kos Pharmaceuticals, Cranbury, NJ), but it is considerably more expensive ($1.98 per 500-mg tablet, or $3.96 to $5.94 daily) and has not been shown to be more effective or better tolerated than the better OTC products.16
JUDY’S CASE
RAISING HDL WITHOUT DRUGS
Judy’s lipid abnormalities would benefit from a supplement of pantethine (300 mg thrice daily) or NA (1,000 mg thrice daily of plain/quick release or 500 mg twice daily of sustained release to reduce flushing side effects).
Her greatest risk with her current lipid levels is low HDL, and the best agent to raise these levels is NA.
Pantethine also raises HDL and selectively improves the HDL-2 subfraction, which is most cardioprotective. Both supplements also improve the other lipid abnormalities.
In addition, referral to a dietician for detailed instruction in food choices and preparation may be useful.
Pharmacologic therapies
Hormone replacement therapy (HRT) is no longer recommended to prevent CVD and should be given only for menopausal symptoms during the perimenopausal years—despite the fact that estrogen has been shown to raise HDL cholesterol by 8% in postmenopausal women.17
Estrogens increase HDL by increasing production of apoA-1, the main lipoprotein in HDL, and by decreasing HDL catabolism by inhibiting hepatic lipase. The 17-hydroxyprogesterone component of HRT given to women with an intact uterus to prevent endometrial cancer has no significant lipid effects.
Paradoxically, the increased CVD risk found in the HRT arm of the Women’s Health Initiative17 was in the face of improved HDL (8%) and LDL (–14%) cholesterol and appeared to be the result of increased thrombotic events.
Further analysis of Women’s Health Initiative data showed that women who were still within 10 years of menopause actually did experience a reduction in CVD risk. That observation, along with some primate research on HRT, suggests that the risk or benefit of HRT with respect to CVD may be a matter of timing. See “Emerging hypothesis may explain estrogen paradox”
At the 2004 American Heart Association meeting, Dr. Thomas Clarkson, who has conducted primate research on hormone replacement therapy (HRT) and the risk of cardiovascular disease (CVD), described the emerging hypothesis that may explain the HRT paradox of increased CVD risk despite evidence of benefit in observational studies.21
Estrogen is a potent upregulator of matrix metal-loproteases. These proteolytic enzymes are a normal constituent of the endometrium and important in its remodeling with each menstrual cycle. Matrix metal-loproteases are also found in the fibrous cap that seals off the necrotic core of an advanced atheroma from the vascular lumen. Most perimenopausal women have enjoyed estrogen’s protective effect throughout their reproductive years and thus have developedlittle advanced atherosclerotic disease.
Ten or more years past menopause, however, clinically significant atherosclerotic lesions often develop in women who have been without the protection of estrogen. If estrogen is added at this stage, it causes increased matrix metalloprotease activity in the fibrous cap of any atheroma. This proteolytic activity can destabilize the fibrous cap, allowing necrotic core material to come in contact with the bloodstream.
This necrotic material is highly thrombogenic and stimulates clot formation in the vascular lumen. Clarkson demonstrated this process in research on perimenopausal and postmenopausal primates.
This hypothesis will soon be tested in a clinical trial in humans; CVD risk is expected to decrease by 50% to 70% in women who have taken HRT continuously from perimenopause.
Statins and other HDL-modifying drugs
The statins are a first choice for LDL reduction, but lead to only modest increases (4%–10%) in HDL levels.18 Fibric acid derivatives are somewhat more effective; they lead to increases in HDL of 6% to 18%. Both types of drugs are considerably more expensive than OTC NA and not as effective at raising HDL.
Combining statins with other agents that raise HDL has been tried: The NA–statin combination can be effective in managing dyslipidemias of both LDL and HDL. Fibric acid derivatives should not be used with statins because of the increased risk of serious myopathies.18
JUDY’S CASE
THERAPEUTIC TARGETS
Judy’s goals should include:
- reducing blood pressure to less than 120/80 mm Hg,
- decreasing weight to about 140 lb,
- achieving a waist measurement of less than 35 inches,
- reducing fasting blood glucose to less than 100 mg/dL,
- decreasing triglycerides to less than 150 mg/dL, total cholesterol to less than 200 mg/dL, and LDL levels to less than 100 mg/dL, and
- raising HDL to more than 45 mg/dL.
All these parameters should be checked every 3 months until the goals are achieved.
If Judy fails to progress or develops symptoms of heart disease, she should be referred to a cardiologist for further evaluation and more aggressive treatment.
The author reports no conflicts relevant to this article.
1. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285:2486-2497.
2. Alsheikh-Ali A, Abourjaily HM, Stanek EJ, et al. Increases in HDL-cholesterol are the strongest predictors of risk reduction in lipid intervention trials. Circulation. 2004;110(17 suppl 3):III-813.
3. Jacobs DR, Jr, Meban IL, Bangdiwala SI, et al. High density lipoprotein cholesterol as a predictor of cardiovascular disease mortality in men and women: the follow-up study of the Lipid Research Clinics Prevalence Study. Am J Epidemiol. 1990;131:32-47.
4. Gordon DJ, Probstfiel JL, Garrison RJ, et al. High-density lipoprotein cholesterol and cardiovascular disease: four prospective American studies. Circulation. 1989;79:8-15.
5. Hu Fb, Willet WC, Li T, et al. Adiposity as compared with physical activity in predicting mortality among women. N Engl J Med. 2004;351:2694-2703.
6. Mensink RP, Zock PL, Kester A, et al. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr. 2003;77:1146-1155.
7. Pereira MA, Swain J, Goldfine AB, et al. Effects of a low-glycemic load diet on resting energy expenditure and heart disease risk factors during weight loss. JAMA. 2004;292:2482-2490.
8. Kokkinos PF, Holland JC, Pittaras AE, et al. Cardiorespiratory fitness and coronary heart disease risk factor association in women. J Am Coll Cardiol. 1995;26:358-364.
9. Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347:716-725.
10. Kokkinos PE, Fernhall B. Physical activity and high density lipoprotein cholesterol levels: what is the relationship? Sports Med. 1999;28:307-314.
11. Van Der Gaag MS, Sterksma A, Schaafsma G, et al. Moderate alcohol consumption lowers risk factors for cardiovascular disease in postmenopausal women fed a controlled diet. Am J Clin Nutr. 2002;75:593-599.
12. Baer DJ, Judd JT, Clevidence BA, et al. Moderate alcohol consumption and changes in postprandial lipoproteins of premenopausal and postmenopausal women: a diet-controlled randomized intervention study. J Womens Health Gend Based Med. 2000;9:607-616.
13. Pins JJ, Keenan JM. Pantethine: a new option in managing dyslipidemia. J Am College Nutr. 2005 [in press].
14. Pins JJ, First S, Shamliyan T, Keenan J. Pantethine beneficially affects apolipoprotein A-1, apolipoprotein B, low-density lipoprotein particle size but not high-sensitivity C-reactive protein in a dyslipidemic population. Circulation. 2004;110(17 suppl 3):III-778.
15. Crouse JR, 3rd. New developments in the use of niacin for treatment of hyperlipidemia: new considerations in the use of an old drug. Coron Artery Dis. 1996;7:321-326.
16. Retail pharmacy quote. Walgreen’s Pharmacy, Minneapolis, Minn. January 2005.
17. Risks and benefits of estrogen plus progestin in healthy post-menopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
18. Hersberger M, von Eckardstein A. Low high-density lipoprotein cholesterol: physical background, clinical importance and drug treatment. Drugs. 2003;63:1907-1945.
19. Mosca L, Grundy SM, Judelson D, et al. Guide to preventive cardiology for women. AHA/ACC scientific statement, consensus panel statement. irculation. 1999;99:2480-2484.
20. Mosca L, Appel LJ, Benjamin EJ, et al. AHA Guidelines: evidence-based guidelines for cardiovascular disease prevention in women. Circulation. 2004;109:672-693.
21. Clarkson T. Women’s Heart Health Symposium. Presented at the American Heart Association annual meeting, Nov 9, 2004, New Orleans.
1. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285:2486-2497.
2. Alsheikh-Ali A, Abourjaily HM, Stanek EJ, et al. Increases in HDL-cholesterol are the strongest predictors of risk reduction in lipid intervention trials. Circulation. 2004;110(17 suppl 3):III-813.
3. Jacobs DR, Jr, Meban IL, Bangdiwala SI, et al. High density lipoprotein cholesterol as a predictor of cardiovascular disease mortality in men and women: the follow-up study of the Lipid Research Clinics Prevalence Study. Am J Epidemiol. 1990;131:32-47.
4. Gordon DJ, Probstfiel JL, Garrison RJ, et al. High-density lipoprotein cholesterol and cardiovascular disease: four prospective American studies. Circulation. 1989;79:8-15.
5. Hu Fb, Willet WC, Li T, et al. Adiposity as compared with physical activity in predicting mortality among women. N Engl J Med. 2004;351:2694-2703.
6. Mensink RP, Zock PL, Kester A, et al. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr. 2003;77:1146-1155.
7. Pereira MA, Swain J, Goldfine AB, et al. Effects of a low-glycemic load diet on resting energy expenditure and heart disease risk factors during weight loss. JAMA. 2004;292:2482-2490.
8. Kokkinos PF, Holland JC, Pittaras AE, et al. Cardiorespiratory fitness and coronary heart disease risk factor association in women. J Am Coll Cardiol. 1995;26:358-364.
9. Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347:716-725.
10. Kokkinos PE, Fernhall B. Physical activity and high density lipoprotein cholesterol levels: what is the relationship? Sports Med. 1999;28:307-314.
11. Van Der Gaag MS, Sterksma A, Schaafsma G, et al. Moderate alcohol consumption lowers risk factors for cardiovascular disease in postmenopausal women fed a controlled diet. Am J Clin Nutr. 2002;75:593-599.
12. Baer DJ, Judd JT, Clevidence BA, et al. Moderate alcohol consumption and changes in postprandial lipoproteins of premenopausal and postmenopausal women: a diet-controlled randomized intervention study. J Womens Health Gend Based Med. 2000;9:607-616.
13. Pins JJ, Keenan JM. Pantethine: a new option in managing dyslipidemia. J Am College Nutr. 2005 [in press].
14. Pins JJ, First S, Shamliyan T, Keenan J. Pantethine beneficially affects apolipoprotein A-1, apolipoprotein B, low-density lipoprotein particle size but not high-sensitivity C-reactive protein in a dyslipidemic population. Circulation. 2004;110(17 suppl 3):III-778.
15. Crouse JR, 3rd. New developments in the use of niacin for treatment of hyperlipidemia: new considerations in the use of an old drug. Coron Artery Dis. 1996;7:321-326.
16. Retail pharmacy quote. Walgreen’s Pharmacy, Minneapolis, Minn. January 2005.
17. Risks and benefits of estrogen plus progestin in healthy post-menopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
18. Hersberger M, von Eckardstein A. Low high-density lipoprotein cholesterol: physical background, clinical importance and drug treatment. Drugs. 2003;63:1907-1945.
19. Mosca L, Grundy SM, Judelson D, et al. Guide to preventive cardiology for women. AHA/ACC scientific statement, consensus panel statement. irculation. 1999;99:2480-2484.
20. Mosca L, Appel LJ, Benjamin EJ, et al. AHA Guidelines: evidence-based guidelines for cardiovascular disease prevention in women. Circulation. 2004;109:672-693.
21. Clarkson T. Women’s Heart Health Symposium. Presented at the American Heart Association annual meeting, Nov 9, 2004, New Orleans.