User login
Case Reports: An Inconvenient Truth
The cardiology literature is filled with randomized, controlled clinical trials (RCTs), some "mega," some not. The calculation of a journal impact factor is heavily influenced by the publication of the results of these trials, and there is often great fanfare at the time of the major meetings when those highly anticipated Late Breakers are presented and simultaneously published in the New England Journal of Medicine or JAMA.
We seem to cite these large studies in our everyday practice: "As the RALES study showed ..." or "... as demonstrated in the RE-LY study ..." Our fellows know "trials speak" though cataloguing all the inclusion criteria, exclusion criteria, primary end points, secondary end points, P values, etc, is rather daunting.
The TIMI family of studies is now up to 57 and it would likely take someone like Raymond Babbitt (Dustin Hoffman in Rain Man) to recall the results of all of them.
So where does this leave the anti-RCT, the case report? As I tell my fellows, case reports are difficult to publish, and even case series can be a challenge.
I am convinced, however, that there is a role for the simple, straightforward "show and tell" that case reports often resemble. After all, we see one patient at a time, and that’s what case reports are all about. They can make you think about your own patient experience. Have you seen that phenomenon before? If so, what happened? If not, should you be thinking about it?
Medicine does not progress by anecdotes, but we can still learn from them. The caveat, of course, is that the path to bad medicine is paved with case reports. Recall the old line about certain unnamed surgical colleagues and how their practice evolves: "One is a case report, two is a series, and three is adoption in the OR."
We won’t go that far, of course. But when confronted with a choice between perusing some case reports or dissecting the latest 40,000+ patient study, I admit to enjoying the former a lot more than the latter. Does that mean I’d rather read the sports section over Dostoyevsky? I’ll give you the answer but only after TIMI 100 is published!
Dr. Paul J. Hauptman is Professor of Internal Medicine and Assistant Dean of Clinical-Translational Research at Saint Louis University and Director of Heart Failure at Saint Louis University Hospital. He currently serves as an Associate Editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
The cardiology literature is filled with randomized, controlled clinical trials (RCTs), some "mega," some not. The calculation of a journal impact factor is heavily influenced by the publication of the results of these trials, and there is often great fanfare at the time of the major meetings when those highly anticipated Late Breakers are presented and simultaneously published in the New England Journal of Medicine or JAMA.
We seem to cite these large studies in our everyday practice: "As the RALES study showed ..." or "... as demonstrated in the RE-LY study ..." Our fellows know "trials speak" though cataloguing all the inclusion criteria, exclusion criteria, primary end points, secondary end points, P values, etc, is rather daunting.
The TIMI family of studies is now up to 57 and it would likely take someone like Raymond Babbitt (Dustin Hoffman in Rain Man) to recall the results of all of them.
So where does this leave the anti-RCT, the case report? As I tell my fellows, case reports are difficult to publish, and even case series can be a challenge.
I am convinced, however, that there is a role for the simple, straightforward "show and tell" that case reports often resemble. After all, we see one patient at a time, and that’s what case reports are all about. They can make you think about your own patient experience. Have you seen that phenomenon before? If so, what happened? If not, should you be thinking about it?
Medicine does not progress by anecdotes, but we can still learn from them. The caveat, of course, is that the path to bad medicine is paved with case reports. Recall the old line about certain unnamed surgical colleagues and how their practice evolves: "One is a case report, two is a series, and three is adoption in the OR."
We won’t go that far, of course. But when confronted with a choice between perusing some case reports or dissecting the latest 40,000+ patient study, I admit to enjoying the former a lot more than the latter. Does that mean I’d rather read the sports section over Dostoyevsky? I’ll give you the answer but only after TIMI 100 is published!
Dr. Paul J. Hauptman is Professor of Internal Medicine and Assistant Dean of Clinical-Translational Research at Saint Louis University and Director of Heart Failure at Saint Louis University Hospital. He currently serves as an Associate Editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
The cardiology literature is filled with randomized, controlled clinical trials (RCTs), some "mega," some not. The calculation of a journal impact factor is heavily influenced by the publication of the results of these trials, and there is often great fanfare at the time of the major meetings when those highly anticipated Late Breakers are presented and simultaneously published in the New England Journal of Medicine or JAMA.
We seem to cite these large studies in our everyday practice: "As the RALES study showed ..." or "... as demonstrated in the RE-LY study ..." Our fellows know "trials speak" though cataloguing all the inclusion criteria, exclusion criteria, primary end points, secondary end points, P values, etc, is rather daunting.
The TIMI family of studies is now up to 57 and it would likely take someone like Raymond Babbitt (Dustin Hoffman in Rain Man) to recall the results of all of them.
So where does this leave the anti-RCT, the case report? As I tell my fellows, case reports are difficult to publish, and even case series can be a challenge.
I am convinced, however, that there is a role for the simple, straightforward "show and tell" that case reports often resemble. After all, we see one patient at a time, and that’s what case reports are all about. They can make you think about your own patient experience. Have you seen that phenomenon before? If so, what happened? If not, should you be thinking about it?
Medicine does not progress by anecdotes, but we can still learn from them. The caveat, of course, is that the path to bad medicine is paved with case reports. Recall the old line about certain unnamed surgical colleagues and how their practice evolves: "One is a case report, two is a series, and three is adoption in the OR."
We won’t go that far, of course. But when confronted with a choice between perusing some case reports or dissecting the latest 40,000+ patient study, I admit to enjoying the former a lot more than the latter. Does that mean I’d rather read the sports section over Dostoyevsky? I’ll give you the answer but only after TIMI 100 is published!
Dr. Paul J. Hauptman is Professor of Internal Medicine and Assistant Dean of Clinical-Translational Research at Saint Louis University and Director of Heart Failure at Saint Louis University Hospital. He currently serves as an Associate Editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
Locum tenens: Tentanda via
With all the chaos in medical care, and yes, in cardiology practice in particular, it seems to me that locum tenens provides an interesting option to our graduating fellows when they are not yet certain about near-term options.
There are just so many questions for them to consider. Do you join a stand-alone practice? If so, what are the chances it will be bought by a hospital or hospital network the day after arrival? What does it mean to join a group that was just purchased? How much job security will be provided? What does partnership mean today, if anything at all?
It is not wrong to suggest that with locum tenens you can try to ride out the proverbial storm while gaining experience practicing in multiple different settings. Of course, if there is a working spouse and/or children of school age, the equation is more complex. But times have changed, and even the academic center has a new appeal for some of our graduating fellows. At least it is familiar and with familiarity comes a sense of security.
I have no reservations in recommending locum tenens as an option: Pack your bags and look around! An echocardiogram, a left heart catheterization, a pacemaker implant: It can be done here ... or there. So tentanda via, the way must be tried.
Of course at some point, it is likely that the travel will no longer seem appealing, and settling into a stable practice environment may be the most reasonable approach (but good luck finding it). Perhaps as a result of this turbulence, I see our fellows thinking about clinical practice in new terms. Even after 6 years or more of post graduate training, they are open to a discussion about nontraditional options. As faculty, we teach ECGs and cath and nuclear and electrophysiology, but we seem to falter when it comes to the intangibles: the future of cardiology practice.
That observation might explain the success of my "career nights" delivered over Chinese food by former trainees who graduated 5-10 years ago and are invited to share their experiences. There is nothing better than a discussion about the changing landscape from colleagues in the thick of it. And that might explain why about a month after yet another dinner of cold sesame noodles at Wonton King, a fellow approaches me to ask "Dr. Hauptman, when are we having our next career night?"
Dr. Paul J. Hauptman is Professor of Internal Medicine and Assistant Dean of Clinical-Translational Research at Saint Louis University and Director of Heart Failure at Saint Louis University Hospital. He currently serves as an Associate Editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
With all the chaos in medical care, and yes, in cardiology practice in particular, it seems to me that locum tenens provides an interesting option to our graduating fellows when they are not yet certain about near-term options.
There are just so many questions for them to consider. Do you join a stand-alone practice? If so, what are the chances it will be bought by a hospital or hospital network the day after arrival? What does it mean to join a group that was just purchased? How much job security will be provided? What does partnership mean today, if anything at all?
It is not wrong to suggest that with locum tenens you can try to ride out the proverbial storm while gaining experience practicing in multiple different settings. Of course, if there is a working spouse and/or children of school age, the equation is more complex. But times have changed, and even the academic center has a new appeal for some of our graduating fellows. At least it is familiar and with familiarity comes a sense of security.
I have no reservations in recommending locum tenens as an option: Pack your bags and look around! An echocardiogram, a left heart catheterization, a pacemaker implant: It can be done here ... or there. So tentanda via, the way must be tried.
Of course at some point, it is likely that the travel will no longer seem appealing, and settling into a stable practice environment may be the most reasonable approach (but good luck finding it). Perhaps as a result of this turbulence, I see our fellows thinking about clinical practice in new terms. Even after 6 years or more of post graduate training, they are open to a discussion about nontraditional options. As faculty, we teach ECGs and cath and nuclear and electrophysiology, but we seem to falter when it comes to the intangibles: the future of cardiology practice.
That observation might explain the success of my "career nights" delivered over Chinese food by former trainees who graduated 5-10 years ago and are invited to share their experiences. There is nothing better than a discussion about the changing landscape from colleagues in the thick of it. And that might explain why about a month after yet another dinner of cold sesame noodles at Wonton King, a fellow approaches me to ask "Dr. Hauptman, when are we having our next career night?"
Dr. Paul J. Hauptman is Professor of Internal Medicine and Assistant Dean of Clinical-Translational Research at Saint Louis University and Director of Heart Failure at Saint Louis University Hospital. He currently serves as an Associate Editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
With all the chaos in medical care, and yes, in cardiology practice in particular, it seems to me that locum tenens provides an interesting option to our graduating fellows when they are not yet certain about near-term options.
There are just so many questions for them to consider. Do you join a stand-alone practice? If so, what are the chances it will be bought by a hospital or hospital network the day after arrival? What does it mean to join a group that was just purchased? How much job security will be provided? What does partnership mean today, if anything at all?
It is not wrong to suggest that with locum tenens you can try to ride out the proverbial storm while gaining experience practicing in multiple different settings. Of course, if there is a working spouse and/or children of school age, the equation is more complex. But times have changed, and even the academic center has a new appeal for some of our graduating fellows. At least it is familiar and with familiarity comes a sense of security.
I have no reservations in recommending locum tenens as an option: Pack your bags and look around! An echocardiogram, a left heart catheterization, a pacemaker implant: It can be done here ... or there. So tentanda via, the way must be tried.
Of course at some point, it is likely that the travel will no longer seem appealing, and settling into a stable practice environment may be the most reasonable approach (but good luck finding it). Perhaps as a result of this turbulence, I see our fellows thinking about clinical practice in new terms. Even after 6 years or more of post graduate training, they are open to a discussion about nontraditional options. As faculty, we teach ECGs and cath and nuclear and electrophysiology, but we seem to falter when it comes to the intangibles: the future of cardiology practice.
That observation might explain the success of my "career nights" delivered over Chinese food by former trainees who graduated 5-10 years ago and are invited to share their experiences. There is nothing better than a discussion about the changing landscape from colleagues in the thick of it. And that might explain why about a month after yet another dinner of cold sesame noodles at Wonton King, a fellow approaches me to ask "Dr. Hauptman, when are we having our next career night?"
Dr. Paul J. Hauptman is Professor of Internal Medicine and Assistant Dean of Clinical-Translational Research at Saint Louis University and Director of Heart Failure at Saint Louis University Hospital. He currently serves as an Associate Editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
A President and a Society
Leaving politics aside, I was struck by a recent announcement from the Heart Rhythm Society that the featured 2013 keynote speaker for the annual scientific sessions will be President Bill Clinton.
According to USA Today, the ex-President made $13.4 million in 2011 from speeches and an estimated $89 million since leaving office in January 2001.
How did he do that?
The article estimates that Clinton has made, on average, $189,000 per speech. Yes, per speech.
Whatever our political leanings may be, I think that we can all agree that $189,000 translates into a lot of RVUs for a 1-hour talk.
So, what does the HRS get out of the event? It’s not clear to me. President Clinton has an impressive delivery and is obviously quite popular. But if I were attending the meeting and paying dues, I might ask whether this is the best use of the Society’s funds. To be fair, the Society’s website states that "President Clinton’s keynote address is made possible in part through the support of VISIT Denver and the Denver Hotel & Hospitality Community," and we don’t know the precise amount of the honorarium. Still, I wonder about the specifics and the intent. Is there a meaningful policy angle that I am missing? Will the former President lobby for the HRS as a result of the speech? Is this intended as a trip down memory lane to a time when "Reinventing Government" was the mantra and regulations were a lot less onerous?
I’ve had the privilege of hearing in person several U.S. presidents and presidential candidates over the years. I’m sure HRS 2013 will leave a lasting impression on some members of the audience. And who knows? Maybe the President will discuss his experience as a cardiac patient.
But the whole affair seems to be "over the top" and even an unnecessary excess. A nice payday for the ex-President but a questionable choice for the cardiology community.
Dr. Paul J. Hauptman is Professor of Internal Medicine and Assistant Dean of Clinical-Translational Research at Saint Louis University and Director of Heart Failure at Saint Louis University Hospital. He currently serves as an Associate Editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
Leaving politics aside, I was struck by a recent announcement from the Heart Rhythm Society that the featured 2013 keynote speaker for the annual scientific sessions will be President Bill Clinton.
According to USA Today, the ex-President made $13.4 million in 2011 from speeches and an estimated $89 million since leaving office in January 2001.
How did he do that?
The article estimates that Clinton has made, on average, $189,000 per speech. Yes, per speech.
Whatever our political leanings may be, I think that we can all agree that $189,000 translates into a lot of RVUs for a 1-hour talk.
So, what does the HRS get out of the event? It’s not clear to me. President Clinton has an impressive delivery and is obviously quite popular. But if I were attending the meeting and paying dues, I might ask whether this is the best use of the Society’s funds. To be fair, the Society’s website states that "President Clinton’s keynote address is made possible in part through the support of VISIT Denver and the Denver Hotel & Hospitality Community," and we don’t know the precise amount of the honorarium. Still, I wonder about the specifics and the intent. Is there a meaningful policy angle that I am missing? Will the former President lobby for the HRS as a result of the speech? Is this intended as a trip down memory lane to a time when "Reinventing Government" was the mantra and regulations were a lot less onerous?
I’ve had the privilege of hearing in person several U.S. presidents and presidential candidates over the years. I’m sure HRS 2013 will leave a lasting impression on some members of the audience. And who knows? Maybe the President will discuss his experience as a cardiac patient.
But the whole affair seems to be "over the top" and even an unnecessary excess. A nice payday for the ex-President but a questionable choice for the cardiology community.
Dr. Paul J. Hauptman is Professor of Internal Medicine and Assistant Dean of Clinical-Translational Research at Saint Louis University and Director of Heart Failure at Saint Louis University Hospital. He currently serves as an Associate Editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
Leaving politics aside, I was struck by a recent announcement from the Heart Rhythm Society that the featured 2013 keynote speaker for the annual scientific sessions will be President Bill Clinton.
According to USA Today, the ex-President made $13.4 million in 2011 from speeches and an estimated $89 million since leaving office in January 2001.
How did he do that?
The article estimates that Clinton has made, on average, $189,000 per speech. Yes, per speech.
Whatever our political leanings may be, I think that we can all agree that $189,000 translates into a lot of RVUs for a 1-hour talk.
So, what does the HRS get out of the event? It’s not clear to me. President Clinton has an impressive delivery and is obviously quite popular. But if I were attending the meeting and paying dues, I might ask whether this is the best use of the Society’s funds. To be fair, the Society’s website states that "President Clinton’s keynote address is made possible in part through the support of VISIT Denver and the Denver Hotel & Hospitality Community," and we don’t know the precise amount of the honorarium. Still, I wonder about the specifics and the intent. Is there a meaningful policy angle that I am missing? Will the former President lobby for the HRS as a result of the speech? Is this intended as a trip down memory lane to a time when "Reinventing Government" was the mantra and regulations were a lot less onerous?
I’ve had the privilege of hearing in person several U.S. presidents and presidential candidates over the years. I’m sure HRS 2013 will leave a lasting impression on some members of the audience. And who knows? Maybe the President will discuss his experience as a cardiac patient.
But the whole affair seems to be "over the top" and even an unnecessary excess. A nice payday for the ex-President but a questionable choice for the cardiology community.
Dr. Paul J. Hauptman is Professor of Internal Medicine and Assistant Dean of Clinical-Translational Research at Saint Louis University and Director of Heart Failure at Saint Louis University Hospital. He currently serves as an Associate Editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
For You, Only Yesterday's Decaffeinated Coffee!
The new conflict of interest rules promulgated by the Federal government are being rolled out and they are quite remarkable (see: http://grants.nih.gov/grants/policy/coi/). Did you know that any travel expense, including a token for a bus ride provided or reimbursed by a pharmaceutical company, device company, specialty society like the American Heart Association, or almost any other entity, counts as a "significant financial interest" (or SFI)?
If that does not convince you that regulation has gone too far, sit tight. But first, I will admit that we are paying the price for the excesses of a few. We still see an echo of those excesses today, and I'm not here to advocate for them.
However, we now have a monitoring regime in place that will require institutions to add layers of oversight and the taxpayer to foot the bill to support state and federal agents who will pore through our books to find the cab ride that was not disclosed.
Yes, we can and should definitively affirm that the degree to which these COI rules now permeate medicine borders on the absurd.
Case in point: At a scientific meeting last year, signs were posted in the vendor display area that included an alert under the word "Coffee" to wit: "If you are a physician from Massachusetts, you cannot accept coffee."
It seems that the vital beverage that was available for automatic dispensing was provided by a pharmaceutical company, not the society hosting the meeting. Based on that brief glimpse into the new world in which we find ourselves, it would certainly appear that the official rules in at least one New England state were beyond strict. Ironic, given that state's Revolutionary War history and the Tea Party.
Although recently Governor Deval Patrick of Massachusetts signed a state budget bill that "loosened things up" a bit in the gift ban arena, if you eat a turkey sandwich in Worcester or Boston or Springfield provided by an industry sponsor, you will need to report the value of that sandwich to the state.
Underlying these rules must be the conceptual bias that we as physicians are like a tabula rasa; that if you provide a cup of coffee or pay for a shared cab ride, we will robotically pivot and prescribe whatever drug, device or intervention you are selling.
Yes, that describes us well.
I was so struck by the coffee experience that I let my mind wander and I came up with two scenarios.
1. A physician wanders into the vendor area and in a moment of temptation and thirst, pours a cup of coffee. A government agent or whistle-blower is staking out the coffee table and as soon as that physician raises the cup to his lips, a SWAT team arrives and shouts "Drop That Cup, Now!" Plea bargaining and a suspended sentence follow.
2. A tiered coffee menu is devised depending on your state's interpretation and/or strengthening of the Federal COI rules. And yes, I am picking on a few states who have a reputation for draconian oversight, and though the degree of regulation does in fact vary, let’s have a little fun:
Yesterday's Decaf: Massachusetts, Vermont, and Minnesota
Americano only, no milk or sweetener: Illinois
Americano or Espresso, open condiment bar: Missouri
Any specialty coffee, any size, any time: Texas
Actually, I'm all for it, as long as the rules apply to everyone. First, to members of Congress, then the lawyers. If we are revealing all under the convenient but misleading rubric of "transparency," it should be equitable. Let's assume everyone is conflicted and let's have everyone watch everyone else. There is a name for this and it ain't capitalism. The word starts with the letter "F" and has seven letters.
I'll likely return to this issue for it provides almost endless opportunities to skewer the rule makers. Until then, I would invest heavily in yesterday''s coffee grounds.
Dr. Paul Hauptman is Professor of Internal Medicine and Assistant Dean of Clinical-Translational Research at Saint Louis University and Director of Heart Failure at Saint Louis University Hospital. He currently serves as an Associate Editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
The new conflict of interest rules promulgated by the Federal government are being rolled out and they are quite remarkable (see: http://grants.nih.gov/grants/policy/coi/). Did you know that any travel expense, including a token for a bus ride provided or reimbursed by a pharmaceutical company, device company, specialty society like the American Heart Association, or almost any other entity, counts as a "significant financial interest" (or SFI)?
If that does not convince you that regulation has gone too far, sit tight. But first, I will admit that we are paying the price for the excesses of a few. We still see an echo of those excesses today, and I'm not here to advocate for them.
However, we now have a monitoring regime in place that will require institutions to add layers of oversight and the taxpayer to foot the bill to support state and federal agents who will pore through our books to find the cab ride that was not disclosed.
Yes, we can and should definitively affirm that the degree to which these COI rules now permeate medicine borders on the absurd.
Case in point: At a scientific meeting last year, signs were posted in the vendor display area that included an alert under the word "Coffee" to wit: "If you are a physician from Massachusetts, you cannot accept coffee."
It seems that the vital beverage that was available for automatic dispensing was provided by a pharmaceutical company, not the society hosting the meeting. Based on that brief glimpse into the new world in which we find ourselves, it would certainly appear that the official rules in at least one New England state were beyond strict. Ironic, given that state's Revolutionary War history and the Tea Party.
Although recently Governor Deval Patrick of Massachusetts signed a state budget bill that "loosened things up" a bit in the gift ban arena, if you eat a turkey sandwich in Worcester or Boston or Springfield provided by an industry sponsor, you will need to report the value of that sandwich to the state.
Underlying these rules must be the conceptual bias that we as physicians are like a tabula rasa; that if you provide a cup of coffee or pay for a shared cab ride, we will robotically pivot and prescribe whatever drug, device or intervention you are selling.
Yes, that describes us well.
I was so struck by the coffee experience that I let my mind wander and I came up with two scenarios.
1. A physician wanders into the vendor area and in a moment of temptation and thirst, pours a cup of coffee. A government agent or whistle-blower is staking out the coffee table and as soon as that physician raises the cup to his lips, a SWAT team arrives and shouts "Drop That Cup, Now!" Plea bargaining and a suspended sentence follow.
2. A tiered coffee menu is devised depending on your state's interpretation and/or strengthening of the Federal COI rules. And yes, I am picking on a few states who have a reputation for draconian oversight, and though the degree of regulation does in fact vary, let’s have a little fun:
Yesterday's Decaf: Massachusetts, Vermont, and Minnesota
Americano only, no milk or sweetener: Illinois
Americano or Espresso, open condiment bar: Missouri
Any specialty coffee, any size, any time: Texas
Actually, I'm all for it, as long as the rules apply to everyone. First, to members of Congress, then the lawyers. If we are revealing all under the convenient but misleading rubric of "transparency," it should be equitable. Let's assume everyone is conflicted and let's have everyone watch everyone else. There is a name for this and it ain't capitalism. The word starts with the letter "F" and has seven letters.
I'll likely return to this issue for it provides almost endless opportunities to skewer the rule makers. Until then, I would invest heavily in yesterday''s coffee grounds.
Dr. Paul Hauptman is Professor of Internal Medicine and Assistant Dean of Clinical-Translational Research at Saint Louis University and Director of Heart Failure at Saint Louis University Hospital. He currently serves as an Associate Editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
The new conflict of interest rules promulgated by the Federal government are being rolled out and they are quite remarkable (see: http://grants.nih.gov/grants/policy/coi/). Did you know that any travel expense, including a token for a bus ride provided or reimbursed by a pharmaceutical company, device company, specialty society like the American Heart Association, or almost any other entity, counts as a "significant financial interest" (or SFI)?
If that does not convince you that regulation has gone too far, sit tight. But first, I will admit that we are paying the price for the excesses of a few. We still see an echo of those excesses today, and I'm not here to advocate for them.
However, we now have a monitoring regime in place that will require institutions to add layers of oversight and the taxpayer to foot the bill to support state and federal agents who will pore through our books to find the cab ride that was not disclosed.
Yes, we can and should definitively affirm that the degree to which these COI rules now permeate medicine borders on the absurd.
Case in point: At a scientific meeting last year, signs were posted in the vendor display area that included an alert under the word "Coffee" to wit: "If you are a physician from Massachusetts, you cannot accept coffee."
It seems that the vital beverage that was available for automatic dispensing was provided by a pharmaceutical company, not the society hosting the meeting. Based on that brief glimpse into the new world in which we find ourselves, it would certainly appear that the official rules in at least one New England state were beyond strict. Ironic, given that state's Revolutionary War history and the Tea Party.
Although recently Governor Deval Patrick of Massachusetts signed a state budget bill that "loosened things up" a bit in the gift ban arena, if you eat a turkey sandwich in Worcester or Boston or Springfield provided by an industry sponsor, you will need to report the value of that sandwich to the state.
Underlying these rules must be the conceptual bias that we as physicians are like a tabula rasa; that if you provide a cup of coffee or pay for a shared cab ride, we will robotically pivot and prescribe whatever drug, device or intervention you are selling.
Yes, that describes us well.
I was so struck by the coffee experience that I let my mind wander and I came up with two scenarios.
1. A physician wanders into the vendor area and in a moment of temptation and thirst, pours a cup of coffee. A government agent or whistle-blower is staking out the coffee table and as soon as that physician raises the cup to his lips, a SWAT team arrives and shouts "Drop That Cup, Now!" Plea bargaining and a suspended sentence follow.
2. A tiered coffee menu is devised depending on your state's interpretation and/or strengthening of the Federal COI rules. And yes, I am picking on a few states who have a reputation for draconian oversight, and though the degree of regulation does in fact vary, let’s have a little fun:
Yesterday's Decaf: Massachusetts, Vermont, and Minnesota
Americano only, no milk or sweetener: Illinois
Americano or Espresso, open condiment bar: Missouri
Any specialty coffee, any size, any time: Texas
Actually, I'm all for it, as long as the rules apply to everyone. First, to members of Congress, then the lawyers. If we are revealing all under the convenient but misleading rubric of "transparency," it should be equitable. Let's assume everyone is conflicted and let's have everyone watch everyone else. There is a name for this and it ain't capitalism. The word starts with the letter "F" and has seven letters.
I'll likely return to this issue for it provides almost endless opportunities to skewer the rule makers. Until then, I would invest heavily in yesterday''s coffee grounds.
Dr. Paul Hauptman is Professor of Internal Medicine and Assistant Dean of Clinical-Translational Research at Saint Louis University and Director of Heart Failure at Saint Louis University Hospital. He currently serves as an Associate Editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
They're at It Again, or, Hummus for All
Yes, the purists are back.
You may recall my review of John Ioannidis’ mini-rant against medical meetings predicated mostly on the basis of their large carbon footprint ("Beating a Path to Medical Meetings"). Now our eating habits are being targeted. Don’t believe me? Check out "Changing Eating Habits for the Medical Profession" by Lesser and colleagues (JAMA 2012;308:983-4) and find out that as physicians, we need to be role models when we open our mouths. We learn that "food served at medical meetings does not seem to adhere to any nutritional guidelines." Apparently, a good meal for us is "a vegetable and hummus," which the authors provide as a specific recommendation for noontime conferences. No pizza for you! Calorie labeling at meetings? In. Snacks of more than 100 calories? Out.
Of course, there is a kernel of wisdom in all this. There are still some providers who smoke, some of us don’t exercise enough, and some are overweight. But that’s not the issue; personal choice is. We can’t be so regulated that our food choices are subject to public oversight and criticism. What’s next? Publicly reported performance measures that evaluate our weekly intake of organic arugula? Medicare reimbursement tied to provider weight (observed versus ideal)? A mandate to ensure that our coffee is brewed with cruelty-free, trade fair beans? Or in the nonfood sphere, requirements that our offices run on solar power?
At moments like this, I am tempted to arrange a delivery of Big Macs and Big Gulps at the next American Heart Association meeting. Bet I’d find a few takers.
Note my disclosures: I have no conflict of interest with any fast food chain, I’m a vegetarian, and no trees were destroyed (to my knowledge) during the writing of this blog. I did, however, eat four pretzels. They contained neither salt nor trans fats. With regrets, I did not dip them in hummus.
Dr. Paul Hauptman is Professor of Internal Medicine and Assistant Dean of Clinical-Translational Research at Saint Louis University and Director of Heart Failure at Saint Louis University Hospital. He currently serves as an Associate Editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
Yes, the purists are back.
You may recall my review of John Ioannidis’ mini-rant against medical meetings predicated mostly on the basis of their large carbon footprint ("Beating a Path to Medical Meetings"). Now our eating habits are being targeted. Don’t believe me? Check out "Changing Eating Habits for the Medical Profession" by Lesser and colleagues (JAMA 2012;308:983-4) and find out that as physicians, we need to be role models when we open our mouths. We learn that "food served at medical meetings does not seem to adhere to any nutritional guidelines." Apparently, a good meal for us is "a vegetable and hummus," which the authors provide as a specific recommendation for noontime conferences. No pizza for you! Calorie labeling at meetings? In. Snacks of more than 100 calories? Out.
Of course, there is a kernel of wisdom in all this. There are still some providers who smoke, some of us don’t exercise enough, and some are overweight. But that’s not the issue; personal choice is. We can’t be so regulated that our food choices are subject to public oversight and criticism. What’s next? Publicly reported performance measures that evaluate our weekly intake of organic arugula? Medicare reimbursement tied to provider weight (observed versus ideal)? A mandate to ensure that our coffee is brewed with cruelty-free, trade fair beans? Or in the nonfood sphere, requirements that our offices run on solar power?
At moments like this, I am tempted to arrange a delivery of Big Macs and Big Gulps at the next American Heart Association meeting. Bet I’d find a few takers.
Note my disclosures: I have no conflict of interest with any fast food chain, I’m a vegetarian, and no trees were destroyed (to my knowledge) during the writing of this blog. I did, however, eat four pretzels. They contained neither salt nor trans fats. With regrets, I did not dip them in hummus.
Dr. Paul Hauptman is Professor of Internal Medicine and Assistant Dean of Clinical-Translational Research at Saint Louis University and Director of Heart Failure at Saint Louis University Hospital. He currently serves as an Associate Editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
Yes, the purists are back.
You may recall my review of John Ioannidis’ mini-rant against medical meetings predicated mostly on the basis of their large carbon footprint ("Beating a Path to Medical Meetings"). Now our eating habits are being targeted. Don’t believe me? Check out "Changing Eating Habits for the Medical Profession" by Lesser and colleagues (JAMA 2012;308:983-4) and find out that as physicians, we need to be role models when we open our mouths. We learn that "food served at medical meetings does not seem to adhere to any nutritional guidelines." Apparently, a good meal for us is "a vegetable and hummus," which the authors provide as a specific recommendation for noontime conferences. No pizza for you! Calorie labeling at meetings? In. Snacks of more than 100 calories? Out.
Of course, there is a kernel of wisdom in all this. There are still some providers who smoke, some of us don’t exercise enough, and some are overweight. But that’s not the issue; personal choice is. We can’t be so regulated that our food choices are subject to public oversight and criticism. What’s next? Publicly reported performance measures that evaluate our weekly intake of organic arugula? Medicare reimbursement tied to provider weight (observed versus ideal)? A mandate to ensure that our coffee is brewed with cruelty-free, trade fair beans? Or in the nonfood sphere, requirements that our offices run on solar power?
At moments like this, I am tempted to arrange a delivery of Big Macs and Big Gulps at the next American Heart Association meeting. Bet I’d find a few takers.
Note my disclosures: I have no conflict of interest with any fast food chain, I’m a vegetarian, and no trees were destroyed (to my knowledge) during the writing of this blog. I did, however, eat four pretzels. They contained neither salt nor trans fats. With regrets, I did not dip them in hummus.
Dr. Paul Hauptman is Professor of Internal Medicine and Assistant Dean of Clinical-Translational Research at Saint Louis University and Director of Heart Failure at Saint Louis University Hospital. He currently serves as an Associate Editor for Circulation: Heart Failure and blogs while staring out his office window at the Arch.
It's a Patient With Heart Failure
A number of years ago, an editor corrected my use of the term "heart failure patient" in the galley proof of a manuscript. Initially I pushed back and asked for some justification. "This is how we write and speak," I added for emphasis. After due consideration, however, I saw the wisdom in this apparently minor editorial change.
Since then, I have found myself correcting the older usage when I review manuscripts in my role as Associate Editor of a Circulation subspecialty journal. When I give lectures, I often correct myself midsentence, since old habits die hard. At one talk, after correcting myself several times, I explained what I was trying to accomplish. Much to my pleasure, a member of the audience came up to me after the talk and told me how much he appreciated my efforts. He said: "I have a daughter with type I diabetes. I would never say that I have a diabetic daughter, nor would I allow anyone else to refer to her in that way. She is my daughter who happens to have and is living with diabetes."
Those simple but graceful words probably summarized it best. When we refer to a "heart failure patient," we inadvertently initiate a process of depersonalization. The patient is suddenly pigeonholed and categorized.
In my opinion, this is not really a case of political correctness run amok. This is a fair and humane way to refer to our patients. So if you catch me using the old verbiage, give me some slack. I’m working on it!
A number of years ago, an editor corrected my use of the term "heart failure patient" in the galley proof of a manuscript. Initially I pushed back and asked for some justification. "This is how we write and speak," I added for emphasis. After due consideration, however, I saw the wisdom in this apparently minor editorial change.
Since then, I have found myself correcting the older usage when I review manuscripts in my role as Associate Editor of a Circulation subspecialty journal. When I give lectures, I often correct myself midsentence, since old habits die hard. At one talk, after correcting myself several times, I explained what I was trying to accomplish. Much to my pleasure, a member of the audience came up to me after the talk and told me how much he appreciated my efforts. He said: "I have a daughter with type I diabetes. I would never say that I have a diabetic daughter, nor would I allow anyone else to refer to her in that way. She is my daughter who happens to have and is living with diabetes."
Those simple but graceful words probably summarized it best. When we refer to a "heart failure patient," we inadvertently initiate a process of depersonalization. The patient is suddenly pigeonholed and categorized.
In my opinion, this is not really a case of political correctness run amok. This is a fair and humane way to refer to our patients. So if you catch me using the old verbiage, give me some slack. I’m working on it!
A number of years ago, an editor corrected my use of the term "heart failure patient" in the galley proof of a manuscript. Initially I pushed back and asked for some justification. "This is how we write and speak," I added for emphasis. After due consideration, however, I saw the wisdom in this apparently minor editorial change.
Since then, I have found myself correcting the older usage when I review manuscripts in my role as Associate Editor of a Circulation subspecialty journal. When I give lectures, I often correct myself midsentence, since old habits die hard. At one talk, after correcting myself several times, I explained what I was trying to accomplish. Much to my pleasure, a member of the audience came up to me after the talk and told me how much he appreciated my efforts. He said: "I have a daughter with type I diabetes. I would never say that I have a diabetic daughter, nor would I allow anyone else to refer to her in that way. She is my daughter who happens to have and is living with diabetes."
Those simple but graceful words probably summarized it best. When we refer to a "heart failure patient," we inadvertently initiate a process of depersonalization. The patient is suddenly pigeonholed and categorized.
In my opinion, this is not really a case of political correctness run amok. This is a fair and humane way to refer to our patients. So if you catch me using the old verbiage, give me some slack. I’m working on it!
Blue Dot, Red Dot, Green Dot
A colleague of mine recently told me about a new "innovation" in her electronic health records (EHR) system, or more precisely, a new metric for the evaluation of workflow in the office.
It seems that a color code has been devised that identifies a patient’s relative "position" in the clinic. For example, a white dot next to the patient’s name on the EHR schedule means "checked in" and green means "patient in room." When the fellow or nurse sees the patient, she or he is supposed to change the dot color to blue. The attending physician is then supposed to change the color to yellow when in the room with the patient, followed by red if an ECG is ordered. Finally, the attending is supposed to change the color to black when the session with the patient is over. Or something like that.
I’ll call it death by metrics. Administrators, however, will delight in being able to report mean times in white vs. blue vs. green vs. red vs. yellow ... you get the point.
Question: Do patients feel better as a consequence of these color changes? Will the practice increase referrals if we decrease the time from blue to yellow?
This reminds me of the recent publicity generated over surgeon and author Atul Gawande’s latest lesson to us all from the real world. It seems we can learn a lot from the Cheesecake Factory and its mechanisms to bring about cost and quality control (Big Med, The New Yorker, Aug. 13, 2012).
A stirring example, no doubt. But of course, during the Roosevelt years, academic progressives told Americans how to run their farms and factories (if you don’t believe me, read Amity Shlaes’s remarkable book, The Forgotten Man). Today’s versions think they know what’s best for the delivery of health care using rather inane examples. While physicians may now be paying the price for a failure to police themselves, we have been instructed – without buy-in, rigorous testing, or scientific evaluation – that electronic health record keeping (along with vertical integration, measurement of quality indicators, etc.) will improve both cost and efficiency. It’s a "feel good" approach, but is really nothing more than a natural experiment.
Blue Dot, Red Dot, Green Dot. I am not sure if the Cheesecake Factory uses a similar system to track the delivery of food platters: I’ll have to ask Dr. Seuss’s Thing One and Thing Two the next time I see them. In the meantime, let’s just hope that experts of a similar ilk are not running our foreign policy and national security apparatus.
Dr. Hauptman is professor of internal medicine and assistant dean of clinical-translational research at Saint Louis University and director of heart failure at Saint Louis University Hospital, and a member of the Cardiology News Editorial Advisory Board.
A colleague of mine recently told me about a new "innovation" in her electronic health records (EHR) system, or more precisely, a new metric for the evaluation of workflow in the office.
It seems that a color code has been devised that identifies a patient’s relative "position" in the clinic. For example, a white dot next to the patient’s name on the EHR schedule means "checked in" and green means "patient in room." When the fellow or nurse sees the patient, she or he is supposed to change the dot color to blue. The attending physician is then supposed to change the color to yellow when in the room with the patient, followed by red if an ECG is ordered. Finally, the attending is supposed to change the color to black when the session with the patient is over. Or something like that.
I’ll call it death by metrics. Administrators, however, will delight in being able to report mean times in white vs. blue vs. green vs. red vs. yellow ... you get the point.
Question: Do patients feel better as a consequence of these color changes? Will the practice increase referrals if we decrease the time from blue to yellow?
This reminds me of the recent publicity generated over surgeon and author Atul Gawande’s latest lesson to us all from the real world. It seems we can learn a lot from the Cheesecake Factory and its mechanisms to bring about cost and quality control (Big Med, The New Yorker, Aug. 13, 2012).
A stirring example, no doubt. But of course, during the Roosevelt years, academic progressives told Americans how to run their farms and factories (if you don’t believe me, read Amity Shlaes’s remarkable book, The Forgotten Man). Today’s versions think they know what’s best for the delivery of health care using rather inane examples. While physicians may now be paying the price for a failure to police themselves, we have been instructed – without buy-in, rigorous testing, or scientific evaluation – that electronic health record keeping (along with vertical integration, measurement of quality indicators, etc.) will improve both cost and efficiency. It’s a "feel good" approach, but is really nothing more than a natural experiment.
Blue Dot, Red Dot, Green Dot. I am not sure if the Cheesecake Factory uses a similar system to track the delivery of food platters: I’ll have to ask Dr. Seuss’s Thing One and Thing Two the next time I see them. In the meantime, let’s just hope that experts of a similar ilk are not running our foreign policy and national security apparatus.
Dr. Hauptman is professor of internal medicine and assistant dean of clinical-translational research at Saint Louis University and director of heart failure at Saint Louis University Hospital, and a member of the Cardiology News Editorial Advisory Board.
A colleague of mine recently told me about a new "innovation" in her electronic health records (EHR) system, or more precisely, a new metric for the evaluation of workflow in the office.
It seems that a color code has been devised that identifies a patient’s relative "position" in the clinic. For example, a white dot next to the patient’s name on the EHR schedule means "checked in" and green means "patient in room." When the fellow or nurse sees the patient, she or he is supposed to change the dot color to blue. The attending physician is then supposed to change the color to yellow when in the room with the patient, followed by red if an ECG is ordered. Finally, the attending is supposed to change the color to black when the session with the patient is over. Or something like that.
I’ll call it death by metrics. Administrators, however, will delight in being able to report mean times in white vs. blue vs. green vs. red vs. yellow ... you get the point.
Question: Do patients feel better as a consequence of these color changes? Will the practice increase referrals if we decrease the time from blue to yellow?
This reminds me of the recent publicity generated over surgeon and author Atul Gawande’s latest lesson to us all from the real world. It seems we can learn a lot from the Cheesecake Factory and its mechanisms to bring about cost and quality control (Big Med, The New Yorker, Aug. 13, 2012).
A stirring example, no doubt. But of course, during the Roosevelt years, academic progressives told Americans how to run their farms and factories (if you don’t believe me, read Amity Shlaes’s remarkable book, The Forgotten Man). Today’s versions think they know what’s best for the delivery of health care using rather inane examples. While physicians may now be paying the price for a failure to police themselves, we have been instructed – without buy-in, rigorous testing, or scientific evaluation – that electronic health record keeping (along with vertical integration, measurement of quality indicators, etc.) will improve both cost and efficiency. It’s a "feel good" approach, but is really nothing more than a natural experiment.
Blue Dot, Red Dot, Green Dot. I am not sure if the Cheesecake Factory uses a similar system to track the delivery of food platters: I’ll have to ask Dr. Seuss’s Thing One and Thing Two the next time I see them. In the meantime, let’s just hope that experts of a similar ilk are not running our foreign policy and national security apparatus.
Dr. Hauptman is professor of internal medicine and assistant dean of clinical-translational research at Saint Louis University and director of heart failure at Saint Louis University Hospital, and a member of the Cardiology News Editorial Advisory Board.
Salut!
I’ve blogged about ongoing threats to medical education (see for example: "Dr. Fred, You Are Not Alone") but I have to admit that there can still be some levity with teaching as well.
Every year, I surprise new third-year medical students and interns midway through morning rounds by stating that it’s time for cocktails.
I send one of them off to secure some Diet Coke and Cran-Apple juice, and then I take over and meticulously mix the two (no ice). The cups are distributed, I say "Salut!" and then we select a nonmedical subject to discuss for a few moments. I often learn that our trainees cannot list the Allies from World War II or name the year Richard Nixon resigned.
Still, the mixture of some sugar and a bit of caffeine gets us back on track. And there is an important and implicit message beyond hydration: It’s about team building and the need to have an occasional moment of good cheer. With all the pressures on rounds, to document and teach and care for sick patients, and document some more, our "salut" represents a temporary safe haven. Don’t knock it until you’ve tried it.
I’ve blogged about ongoing threats to medical education (see for example: "Dr. Fred, You Are Not Alone") but I have to admit that there can still be some levity with teaching as well.
Every year, I surprise new third-year medical students and interns midway through morning rounds by stating that it’s time for cocktails.
I send one of them off to secure some Diet Coke and Cran-Apple juice, and then I take over and meticulously mix the two (no ice). The cups are distributed, I say "Salut!" and then we select a nonmedical subject to discuss for a few moments. I often learn that our trainees cannot list the Allies from World War II or name the year Richard Nixon resigned.
Still, the mixture of some sugar and a bit of caffeine gets us back on track. And there is an important and implicit message beyond hydration: It’s about team building and the need to have an occasional moment of good cheer. With all the pressures on rounds, to document and teach and care for sick patients, and document some more, our "salut" represents a temporary safe haven. Don’t knock it until you’ve tried it.
I’ve blogged about ongoing threats to medical education (see for example: "Dr. Fred, You Are Not Alone") but I have to admit that there can still be some levity with teaching as well.
Every year, I surprise new third-year medical students and interns midway through morning rounds by stating that it’s time for cocktails.
I send one of them off to secure some Diet Coke and Cran-Apple juice, and then I take over and meticulously mix the two (no ice). The cups are distributed, I say "Salut!" and then we select a nonmedical subject to discuss for a few moments. I often learn that our trainees cannot list the Allies from World War II or name the year Richard Nixon resigned.
Still, the mixture of some sugar and a bit of caffeine gets us back on track. And there is an important and implicit message beyond hydration: It’s about team building and the need to have an occasional moment of good cheer. With all the pressures on rounds, to document and teach and care for sick patients, and document some more, our "salut" represents a temporary safe haven. Don’t knock it until you’ve tried it.
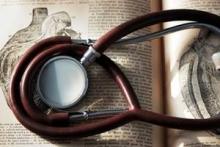
Auscultation Rules!
A paper containing a series of vignettes about the importance of cardiac auscultation recently appeared in the Cleveland Clinic Journal of Medicine (2012;79:536-44). The authors correctly point out that cardiac auscultation can provide useful and at times pivotal information that influences decision-making beyond echocardiography. For example, they describe a case of a patient referred for re-operation after surgery for aortic dissection who had severe aortic insufficiency noted on an echocardiogram; a physical exam and careful auscultation raised questions about the severity of the leak. A repeat echocardiogram failed to demonstrate more than mild-to-moderate AI and surgery was deferred.
It is worthwhile to read papers like this one from time to time, and to recognize that our old physical examination skills do matter. As any cardiology fellow who has trained with me over the last 20 years can attest, I cherish my old HP stethoscope, and I value auscultation. A lot.
I’ll conclude with my own vignette, a story about aortic stenosis and Valentin Fuster. I was a fellow at the Cardiovascular Medicine Division at Mount Sinai Hospital; we overlapped for 1 year. During that time, I heard him tell a medical student, at the bedside of a patient with severe aortic stenosis: "You just listened to the murmur of aortic stenosis. At lunch time, you must come back to this bedside and listen to the murmur of aortic stenosis. And before you go home tonight, you must come here again and listen to the murmur of aortic stenosis. My friend, then you can go home and know that today, you listened to three murmurs of aortic stenosis!"
There is wisdom in that story. Auscultation rules.
Dr. Hauptman is professor of internal medicine and assistant dean of clinical-translational research at Saint Louis University and director of heart failure at Saint Louis University Hospital, and a member of the Cardiology News Editorial Advisory Board.
A paper containing a series of vignettes about the importance of cardiac auscultation recently appeared in the Cleveland Clinic Journal of Medicine (2012;79:536-44). The authors correctly point out that cardiac auscultation can provide useful and at times pivotal information that influences decision-making beyond echocardiography. For example, they describe a case of a patient referred for re-operation after surgery for aortic dissection who had severe aortic insufficiency noted on an echocardiogram; a physical exam and careful auscultation raised questions about the severity of the leak. A repeat echocardiogram failed to demonstrate more than mild-to-moderate AI and surgery was deferred.
It is worthwhile to read papers like this one from time to time, and to recognize that our old physical examination skills do matter. As any cardiology fellow who has trained with me over the last 20 years can attest, I cherish my old HP stethoscope, and I value auscultation. A lot.
I’ll conclude with my own vignette, a story about aortic stenosis and Valentin Fuster. I was a fellow at the Cardiovascular Medicine Division at Mount Sinai Hospital; we overlapped for 1 year. During that time, I heard him tell a medical student, at the bedside of a patient with severe aortic stenosis: "You just listened to the murmur of aortic stenosis. At lunch time, you must come back to this bedside and listen to the murmur of aortic stenosis. And before you go home tonight, you must come here again and listen to the murmur of aortic stenosis. My friend, then you can go home and know that today, you listened to three murmurs of aortic stenosis!"
There is wisdom in that story. Auscultation rules.
Dr. Hauptman is professor of internal medicine and assistant dean of clinical-translational research at Saint Louis University and director of heart failure at Saint Louis University Hospital, and a member of the Cardiology News Editorial Advisory Board.
A paper containing a series of vignettes about the importance of cardiac auscultation recently appeared in the Cleveland Clinic Journal of Medicine (2012;79:536-44). The authors correctly point out that cardiac auscultation can provide useful and at times pivotal information that influences decision-making beyond echocardiography. For example, they describe a case of a patient referred for re-operation after surgery for aortic dissection who had severe aortic insufficiency noted on an echocardiogram; a physical exam and careful auscultation raised questions about the severity of the leak. A repeat echocardiogram failed to demonstrate more than mild-to-moderate AI and surgery was deferred.
It is worthwhile to read papers like this one from time to time, and to recognize that our old physical examination skills do matter. As any cardiology fellow who has trained with me over the last 20 years can attest, I cherish my old HP stethoscope, and I value auscultation. A lot.
I’ll conclude with my own vignette, a story about aortic stenosis and Valentin Fuster. I was a fellow at the Cardiovascular Medicine Division at Mount Sinai Hospital; we overlapped for 1 year. During that time, I heard him tell a medical student, at the bedside of a patient with severe aortic stenosis: "You just listened to the murmur of aortic stenosis. At lunch time, you must come back to this bedside and listen to the murmur of aortic stenosis. And before you go home tonight, you must come here again and listen to the murmur of aortic stenosis. My friend, then you can go home and know that today, you listened to three murmurs of aortic stenosis!"
There is wisdom in that story. Auscultation rules.
Dr. Hauptman is professor of internal medicine and assistant dean of clinical-translational research at Saint Louis University and director of heart failure at Saint Louis University Hospital, and a member of the Cardiology News Editorial Advisory Board.
Quality Scorecards: Mark Twain Was Right
Each month, a hospital quality scorecard is presented to the medical staff for heart failure and myocardial infarction. In it, compliance with the Joint Commission (formerly the Joint Commission on Accreditation of Healthcare Organizations [JCAHO]) performance measures is reported. Each figure is highlighted by a color, and if it is red, it means your performance is below the mean for similar hospitals. It is obviously better to be highlighted in green because that means you are above the mean.
The remarkable observation is that the difference between red and green can be tenths of a percentage point, so at 97.3% you might be red and at 97.8% you might be green.
Does this have any clinical meaning? Of course not. It’s statistical gamesmanship, but with serious overtones – because reimbursement can be tied to this version of your "quality." Aside from the fact that adherence to performance measures is not clearly related to outcomes, at least in patients with early post discharge (JAMA 2007;297:61-70), Mark Twain would remind us in situations like this that there are three types of lies: "Lies, Damn Lies and Statistics."
Unfortunately, the bean counters don’t understand regression to the mean or the lack of value that often accompanies a P value. And they most certainly don’t read Mark Twain anymore.
Dr. Hauptman is professor of internal medicine and assistant dean of clinical-translational research at Saint Louis University and director of heart failure at Saint Louis University Hospital, and a member of the Cardiology News Editorial Advisory Board.
Each month, a hospital quality scorecard is presented to the medical staff for heart failure and myocardial infarction. In it, compliance with the Joint Commission (formerly the Joint Commission on Accreditation of Healthcare Organizations [JCAHO]) performance measures is reported. Each figure is highlighted by a color, and if it is red, it means your performance is below the mean for similar hospitals. It is obviously better to be highlighted in green because that means you are above the mean.
The remarkable observation is that the difference between red and green can be tenths of a percentage point, so at 97.3% you might be red and at 97.8% you might be green.
Does this have any clinical meaning? Of course not. It’s statistical gamesmanship, but with serious overtones – because reimbursement can be tied to this version of your "quality." Aside from the fact that adherence to performance measures is not clearly related to outcomes, at least in patients with early post discharge (JAMA 2007;297:61-70), Mark Twain would remind us in situations like this that there are three types of lies: "Lies, Damn Lies and Statistics."
Unfortunately, the bean counters don’t understand regression to the mean or the lack of value that often accompanies a P value. And they most certainly don’t read Mark Twain anymore.
Dr. Hauptman is professor of internal medicine and assistant dean of clinical-translational research at Saint Louis University and director of heart failure at Saint Louis University Hospital, and a member of the Cardiology News Editorial Advisory Board.
Each month, a hospital quality scorecard is presented to the medical staff for heart failure and myocardial infarction. In it, compliance with the Joint Commission (formerly the Joint Commission on Accreditation of Healthcare Organizations [JCAHO]) performance measures is reported. Each figure is highlighted by a color, and if it is red, it means your performance is below the mean for similar hospitals. It is obviously better to be highlighted in green because that means you are above the mean.
The remarkable observation is that the difference between red and green can be tenths of a percentage point, so at 97.3% you might be red and at 97.8% you might be green.
Does this have any clinical meaning? Of course not. It’s statistical gamesmanship, but with serious overtones – because reimbursement can be tied to this version of your "quality." Aside from the fact that adherence to performance measures is not clearly related to outcomes, at least in patients with early post discharge (JAMA 2007;297:61-70), Mark Twain would remind us in situations like this that there are three types of lies: "Lies, Damn Lies and Statistics."
Unfortunately, the bean counters don’t understand regression to the mean or the lack of value that often accompanies a P value. And they most certainly don’t read Mark Twain anymore.
Dr. Hauptman is professor of internal medicine and assistant dean of clinical-translational research at Saint Louis University and director of heart failure at Saint Louis University Hospital, and a member of the Cardiology News Editorial Advisory Board.