User login
Stimulants for kids with ADHD—how to proceed safely
› Complete a thorough, cardiac-focused history and physical examination before starting stimulants for attention deficit hyperactivity disorder (ADHD) in a child or adolescent. C
› Avoid using stimulants in children or adolescents with comorbid conditions associated with sudden cardiac death, including hypertrophic cardiomyopathy, long QT interval syndrome, and preexcitation syndromes such as Wolff-Parkinson-White syndrome. C
› Monitor all children and adolescents who are taking stimulants for tachycardia, hypertension, palpitations, and chest pain. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE › A young patient has been struggling in school. His worried mother, having had several conferences with the child’s teachers, brings him to the family physician (FP), where he is given a diagnosis of attention deficit hyperactivity disorder (ADHD). The FP considers prescribing a stimulant medication, but first plans on conducting a more thorough family history and exam. She also debates the merits of ordering an electrocardiogram (EKG) to screen for conditions that could lead to sudden cardiac death.
If you were caring for this patient, how would you proceed?
That’s a good question, given the debate that has surrounded this subject since the US Food and Drug Administration (FDA) first learned of 25 cases of sudden death that were linked to stimulant medications.1 The majority of the cases, which were reported to the FDA’s Adverse Event Reporting System between 1999 and 2003, involved amphetamines or methylphenidate in patients under the age of 19.1 In 2008, the American Heart Association (AHA) issued a scientific statement advocating that physicians perform a proper family history and physical exam that includes blood pressure (BP) and an EKG before prescribing a stimulant for children and adolescents.2 The inclusion of EKG screening was intended to increase the likelihood of identifying patients with potentially life-threatening conditions that could lead to sudden cardiac death (SCD).2
Not everyone, however, agreed.
Later that year, the American Academy of Pediatrics (AAP) challenged the routine use of EKGs in this screening process, citing a lack of evidence between stimulant use and the induction of potentially lethal arrhythmias.3 And in 2011, the European Guideline Group also concluded that there was no evidence to suggest an incremental benefit for routine EKG assessment of ADHD patients before initiation of medication.4
Underscoring the uncertainty surrounding the subject are the findings of a 2012 survey of 525 randomly selected US pediatricians.5 Nearly a quarter of the respondents expressed concerns over the risk for SCD in children receiving stimulants for ADHD, and a slightly higher number—30%—worried that the risks for legal liability were high enough to warrant cardiac assessment.5
So how should the prudent FP proceed? In this review, we will describe how to thoroughly screen children and adolescents for their risk of SCD before prescribing stimulants for ADHD. We’ll also summarize what the evidence tells us about whether—and when—you should order an EKG. But first, a word about the pharmacology of stimulants.
How stimulants might increase SCD risk
Stimulants have been used to treat ADHD for more than 40 years6 and are a first-line of therapy for children with ADHD. Stimulants increase attention span by releasing dopamine and norepinephrine at synapses in the frontal cortex, brain stem, and midbrain.
The effect on heart rate and BP. In clinical trials with small samples sizes, children and adolescents receiving stimulants to treat ADHD experienced a minimal rise in heart rate and BP. As measured by 24-hour ambulatory BP monitoring, 13 subjects in a double-blind, randomized, placebo/stimulant crossover trial had slightly elevated total diastolic BP (69.7 vs 65.8 mm Hg; P=.02), waking diastolic BP (75.5 vs 72.3 mm Hg; P=.03), and total heart rate (85.5 vs 79.9 beats per minutes [bpm]; P=.004) while receiving stimulants.7 Other investigators noted similar findings among 17 boys ages 7 to 11 years.8
Whether prolonged childhood exposure to stimulants increases the risk for developing hypertension or tachycardia is unknown. A 10-year follow-up study of 579 children between the ages of 7 to 9 years found stimulants had no effect on systolic or diastolic BP.9 Stimulants use did, however, lead to a higher heart rate (84.2±12.4 vs 79.1±12.0 bpm) during treatment.9 No stimulant-related QT interval changes—which some have proposed might explain SCD in ADHD patients—have been reported in pediatric patients.10 Researchers have noted small increases in mean QTc intervals in adults treated with stimulants for ADHD, but none were >480 msec.11
Steps you should always take before prescribing a stimulant
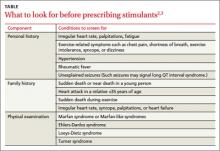
Before prescribing stimulants to children or adolescents with ADHD, complete an in-depth cardiac history and physical examination, as recommended by the AHA and AAP (TABLE),2,3 to identify conditions that increase the likelihood of SCD, such as hypertrophic cardiomyopathy (HCM), long QT interval syndrome (LQTS), and preexcitation syndromes such as Wolff-Parkinson-White syndrome (WPW).
Confirm, for instance, that your patient has a normal heart rate, rhythm, and BP, and no pathological murmurs. In a survey of families with a child or young adult who had sudden cardiac arrest, 72% reported the patient had at least one cardiovascular symptom within 19 to 71 months of SCD, and 27% reported having a family member with a history of SCD before age 50.12 For patients with no such complaints or family history, the news is good. Two large studies found that in the absence of any suspected or overt cardiac disease, children with ADHD who were receiving stimulant therapy had no increased risk of SCD.13,14
What about patients with this common heart problem? Physicians face a dilemma when a stimulant is needed and the patient has a common acyanotic congenital heart lesion, such as a small atrial or ventricular septal defect, which is considered nonlethal. Based on limited data, there is no evidence that the risk of SCD is higher when these patients take stimulants.15
Should you order that EKG—or not?
Currently, the AHA still favors an EKG, though in a correction to its original statement, it adjusted the language to say that EKG could be “useful,” in addition to an in-depth cardiac history and physical examination.16
Opposition to routine EKG screening in these patients stems from the procedure’s extremely low yield and relatively high false positive findings, which may result in higher financial and psychological burdens for patients and families. Thomas et al17 reported that at a single center, the number of EKGs ordered with an indication of “stimulant medication screening” quadrupled during 2009, the year after the AHA published its recommendations. Of 372 patients referred for EKG, 24 (6.4%) had abnormal findings and 18 were referred for further evaluation, but none were found to have cardiac disease. ADHD therapy was delayed in 6 patients because of the EKG.
In a similar evaluation of 1470 ADHD patients ages 21 years and younger, Mahle et al18 noted that 119 patients (8.1%) had an abnormal EKG, 78 of whom (65%) were already receiving stimulants. Five patients had cardiac disease, including 2 who had a preexcitation syndrome. Overall, the positive predictive value was low (4.2%).18 Other research, including a study lead by one of this article’s authors (SKM), has found similar increases in the number of EKGs ordered for patients with ADHD.19
Cost vs benefit. In the Mahle et al18 study described above, the mean cost of EKG screening, including further testing for patients with abnormal initial results, was $58 per child. The mean cost to identify a true-positive result was $17,162.18
In 2012, Leslie et al20 used simulation models to estimate the societal cost of routine EKG screening to prevent SCD in children with ADHD. Their findings: The cost would be high relative to its health benefits—approximately $91,000 to $204,000 per life year saved. Furthermore, these researchers found that ordering an EKG to screen for 3 common cardiac conditions linked to SCD (HCM, WPW, and LQTS) would add <2 days to a patient’s projected life expectancy.20
Our recommendations
We believe stimulants can safely be used in the treatment of children and adolescents with ADHD, given the evidence that suggests a low risk of SCD. That said, it is prudent to avoid prescribing stimulants for children who have an underlying condition that may deteriorate secondary to increased blood pressure or heart rate.
We agree with the current AHA and AAP recommendations that physicians should obtain an in-depth cardiac history and physical examination, with emphasis on screening for cardiac disorders that may put a child at risk for SCD, such as HCM, LQTS, and preexcitation syndromes. For instance, a history of a family member with palpitations should prompt an EKG, which may reveal familial preexcitation syndrome. Similarly, an EKG is in order if you suspect LQTS based on a parent’s description of a family member’s death after hearing a loud noise, such as fireworks.
It often takes active probing to uncover a history of sudden death in the family that a parent may not consider relevant. For example, one of the authors (SKM) cared for a 6-year-old boy who presented with a history of syncope after his hand got caught in a door jam. On further probing, his mother revealed that her father had died at age 30 while he was taking astemizole, an allergy drug known to prolong the QT interval. Subsequent EKGs revealed that both the boy and his mother had LQTS.
For patients already taking stimulants, we recommend monitoring BP and heart rate and ordering an EKG only if the patient exhibits cardiac symptoms or there are concerns based on follow-up history and physical examination. Should a patient develop palpitations while taking a therapeutic dose of stimulants, a detailed history of the onset and duration of symptoms is important. For example, tachycardia that has a gradual onset and occurs with exercise is suggestive of physiological sinus tachycardia. In our judgment, most patients who experience symptoms that suggest sinus tachycardia simply require downward readjustment of their medication or a switch to a nonstimulant.
However, if the patient or family history prompts you to suspect other arrhythmias such as ectopic beats or supraventricular tachycardia, immediate assessment either in an emergency department or in the physician’s office may be required, because obtaining an EKG during symptoms is crucial for the diagnosis. Similarly, unexplained exercise intolerance or the onset of chest pain associated with exercise, dizziness, syncope, seizures, or dyspnea requires immediate cardiovascular assessment.
And finally, whether your patient has just started taking medication for his or her ADHD or has been on the medication for some time, it’s important to periodically reassess the need to continue the stimulant therapy; ADHD symptoms may decrease during mid- to late adolescence and into adulthood.21
CASE › The FP completed a thorough physical exam and found no evidence of any conditions that would increase the likelihood of SCD in the young patient. There was no history of SCD in the boy’s family, either. Based on these findings, the FP opted to forgo an EKG. She prescribed lisdexamfetamine, starting with 20 mg/d (the lowest dose available) and then monitored his course by telephone. Eventually, 30 mg was found to be an effective dose. At a 6-week follow-up visit, the boy’s ADHD symptoms were substantially reduced, without any adverse effects—cardiac or otherwise.
CORRESPONDENCE
Sudhir Ken Mehta, Cleveland Clinic Children’s Hospital, 9500 Euclid Avenue, Cleveland, OH 44111; kemeht@ccf.org
1. Safety review: Follow up review of AERS search identifying cases of sudden death occurring with drugs used for the treatment of Attention Deficit Hyperactivity Disorder (ADHD). US Food and Drug Administration Web site. Available at: http://www.fda.gov/ohrms/dockets/ac/06/briefing/2006-4210b_07_01_safetyreview.pdf. Accessed January 17, 2014.
2. Vetter VL, Elia J, Erickson C, et al. Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactivity disorder: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee and the Council on Cardiovascular Nursing. Circulation. 2008;117:2407-2423.
3. Perrin JM, Friedman RA, Knilans TK; Black Box Working Group; Section on Cardiology and Cardiac Surgery. Cardiovascular monitoring and stimulant drugs for attention-deficit/hyperactivity disorder. Pediatrics. 2008;122:451-453.
4. Graham J, Banaschewski T, Buitelaar J, et al; European Guidelines Group. European guidelines on managing adverse effects of medication for ADHD. Eur Child Adolesc Psychiatry. 2011;20:17-37.
5. Leslie LK, Rodday AM, Saunders TS, et al. Cardiac screening prior to stimulant treatment of ADHD: a survey of US-based pediatricians. Pediatrics. 2012;129:222-230.
6. Conners CK. Symposium: behavior modification by drugs. II. Psychological effects of stimulant drugs in children with minimal brain dysfunction. Pediatrics. 1972;49:702-708.
7. Samuels JA, Franco K, Wan F, et al. Effect of stimulants on 24-h ambulatory blood pressure in children with ADHD: a double-blind, randomized, cross-over trial. Pediatr Nephrol. 2006;21:92-95.
8. Stowe CD, Gardner SF, Gist CC, et al. 24-hour ambulatory blood pressure monitoring in male children receiving stimulant therapy. Ann Pharmacother. 2002;36:1142-1149.
9. Vitiello B, Elliott GR, Swanson JM, et al. Blood pressure and heart rate over 10 years in the multimodal treatment study of children with ADHD. Am J Psychiatry. 2012;169:167-177.
10. Hammerness P, Wilens T, Mick E, et al. Cardiovascular effects of longer-term, high-dose OROS methylphenidate in adolescents with attention deficit hyperactivity disorder. J Pediatr. 2009;155:84-89,89.e1.
11. Weisler RH, Biederman J, Spencer TJ, et al. Long-term cardiovascular effects of mixed amphetamine salts extended release in adults with ADHD. CNS Spectr. 2005;10(suppl 20):35-43.
12. Drezner JA, Fudge J, Harmon KG, et al. Warning symptoms and family history in children and young adults with sudden cardiac arrest. J Am Board Fam Med. 2012;25:408-415.
13. Cooper WO, Habel LA, Sox CM, et al. ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med. 2011;365:1896-1904.
14. Schelleman H, Bilker WB, Strom BL, et al. Cardiovascular events and death in children exposed and unexposed to ADHD agents. Pediatrics. 2011;127:1102-1110.
15. Winterstein AG, Gerhard T, Kubilis P, et al. Cardiovascular safety of central nervous system stimulants in children and adolescents: population based cohort study. BMJ. 2012;345:e4627.
16. Vetter VL, Elia J, Erickson C, et al. Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactivity disorder: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee and the Council on Cardiovascular Nursing [published correction appears in Circulation. 2009;120:e55-e59]. Circulation. 2008;117:2407-2423.
17. Thomas PE, Carlo WF, Decker JA, et al. Impact of the American Heart Association scientific statement on screening electrocardiograms and stimulant medications. Arch Pediatr Adolesc Med. 2011;165:166-170.
18. Mahle WT, Hebson C, Strieper MJ. Electrocardiographic screening in children with attention-deficit hyperactivity disorder. Am J Cardiol. 2009;104:1296-1299.
19. Mehta SK, Richards N, Jacobs I. Children and adolescents with attention deficit hyperactivity disorder in a pediatric cardiology office. Cardiol Young. 2010;20(suppl 3):167.
20. Leslie LK, Cohen JT, Newburger JW, et al. Costs and benefits of targeted screening for causes of sudden cardiac death in children and adolescents. Circulation. 2012;125:2621-2629.
21. Mannuzza S, Klein RG, Bessler A, et al. Adult psychiatric status of hyperactive boys grown up. Am J Psychiatry. 1998;155:493-488.
› Complete a thorough, cardiac-focused history and physical examination before starting stimulants for attention deficit hyperactivity disorder (ADHD) in a child or adolescent. C
› Avoid using stimulants in children or adolescents with comorbid conditions associated with sudden cardiac death, including hypertrophic cardiomyopathy, long QT interval syndrome, and preexcitation syndromes such as Wolff-Parkinson-White syndrome. C
› Monitor all children and adolescents who are taking stimulants for tachycardia, hypertension, palpitations, and chest pain. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE › A young patient has been struggling in school. His worried mother, having had several conferences with the child’s teachers, brings him to the family physician (FP), where he is given a diagnosis of attention deficit hyperactivity disorder (ADHD). The FP considers prescribing a stimulant medication, but first plans on conducting a more thorough family history and exam. She also debates the merits of ordering an electrocardiogram (EKG) to screen for conditions that could lead to sudden cardiac death.
If you were caring for this patient, how would you proceed?
That’s a good question, given the debate that has surrounded this subject since the US Food and Drug Administration (FDA) first learned of 25 cases of sudden death that were linked to stimulant medications.1 The majority of the cases, which were reported to the FDA’s Adverse Event Reporting System between 1999 and 2003, involved amphetamines or methylphenidate in patients under the age of 19.1 In 2008, the American Heart Association (AHA) issued a scientific statement advocating that physicians perform a proper family history and physical exam that includes blood pressure (BP) and an EKG before prescribing a stimulant for children and adolescents.2 The inclusion of EKG screening was intended to increase the likelihood of identifying patients with potentially life-threatening conditions that could lead to sudden cardiac death (SCD).2
Not everyone, however, agreed.
Later that year, the American Academy of Pediatrics (AAP) challenged the routine use of EKGs in this screening process, citing a lack of evidence between stimulant use and the induction of potentially lethal arrhythmias.3 And in 2011, the European Guideline Group also concluded that there was no evidence to suggest an incremental benefit for routine EKG assessment of ADHD patients before initiation of medication.4
Underscoring the uncertainty surrounding the subject are the findings of a 2012 survey of 525 randomly selected US pediatricians.5 Nearly a quarter of the respondents expressed concerns over the risk for SCD in children receiving stimulants for ADHD, and a slightly higher number—30%—worried that the risks for legal liability were high enough to warrant cardiac assessment.5
So how should the prudent FP proceed? In this review, we will describe how to thoroughly screen children and adolescents for their risk of SCD before prescribing stimulants for ADHD. We’ll also summarize what the evidence tells us about whether—and when—you should order an EKG. But first, a word about the pharmacology of stimulants.
How stimulants might increase SCD risk
Stimulants have been used to treat ADHD for more than 40 years6 and are a first-line of therapy for children with ADHD. Stimulants increase attention span by releasing dopamine and norepinephrine at synapses in the frontal cortex, brain stem, and midbrain.
The effect on heart rate and BP. In clinical trials with small samples sizes, children and adolescents receiving stimulants to treat ADHD experienced a minimal rise in heart rate and BP. As measured by 24-hour ambulatory BP monitoring, 13 subjects in a double-blind, randomized, placebo/stimulant crossover trial had slightly elevated total diastolic BP (69.7 vs 65.8 mm Hg; P=.02), waking diastolic BP (75.5 vs 72.3 mm Hg; P=.03), and total heart rate (85.5 vs 79.9 beats per minutes [bpm]; P=.004) while receiving stimulants.7 Other investigators noted similar findings among 17 boys ages 7 to 11 years.8
Whether prolonged childhood exposure to stimulants increases the risk for developing hypertension or tachycardia is unknown. A 10-year follow-up study of 579 children between the ages of 7 to 9 years found stimulants had no effect on systolic or diastolic BP.9 Stimulants use did, however, lead to a higher heart rate (84.2±12.4 vs 79.1±12.0 bpm) during treatment.9 No stimulant-related QT interval changes—which some have proposed might explain SCD in ADHD patients—have been reported in pediatric patients.10 Researchers have noted small increases in mean QTc intervals in adults treated with stimulants for ADHD, but none were >480 msec.11
Steps you should always take before prescribing a stimulant
Before prescribing stimulants to children or adolescents with ADHD, complete an in-depth cardiac history and physical examination, as recommended by the AHA and AAP (TABLE),2,3 to identify conditions that increase the likelihood of SCD, such as hypertrophic cardiomyopathy (HCM), long QT interval syndrome (LQTS), and preexcitation syndromes such as Wolff-Parkinson-White syndrome (WPW).
Confirm, for instance, that your patient has a normal heart rate, rhythm, and BP, and no pathological murmurs. In a survey of families with a child or young adult who had sudden cardiac arrest, 72% reported the patient had at least one cardiovascular symptom within 19 to 71 months of SCD, and 27% reported having a family member with a history of SCD before age 50.12 For patients with no such complaints or family history, the news is good. Two large studies found that in the absence of any suspected or overt cardiac disease, children with ADHD who were receiving stimulant therapy had no increased risk of SCD.13,14
What about patients with this common heart problem? Physicians face a dilemma when a stimulant is needed and the patient has a common acyanotic congenital heart lesion, such as a small atrial or ventricular septal defect, which is considered nonlethal. Based on limited data, there is no evidence that the risk of SCD is higher when these patients take stimulants.15
Should you order that EKG—or not?
Currently, the AHA still favors an EKG, though in a correction to its original statement, it adjusted the language to say that EKG could be “useful,” in addition to an in-depth cardiac history and physical examination.16
Opposition to routine EKG screening in these patients stems from the procedure’s extremely low yield and relatively high false positive findings, which may result in higher financial and psychological burdens for patients and families. Thomas et al17 reported that at a single center, the number of EKGs ordered with an indication of “stimulant medication screening” quadrupled during 2009, the year after the AHA published its recommendations. Of 372 patients referred for EKG, 24 (6.4%) had abnormal findings and 18 were referred for further evaluation, but none were found to have cardiac disease. ADHD therapy was delayed in 6 patients because of the EKG.
In a similar evaluation of 1470 ADHD patients ages 21 years and younger, Mahle et al18 noted that 119 patients (8.1%) had an abnormal EKG, 78 of whom (65%) were already receiving stimulants. Five patients had cardiac disease, including 2 who had a preexcitation syndrome. Overall, the positive predictive value was low (4.2%).18 Other research, including a study lead by one of this article’s authors (SKM), has found similar increases in the number of EKGs ordered for patients with ADHD.19
Cost vs benefit. In the Mahle et al18 study described above, the mean cost of EKG screening, including further testing for patients with abnormal initial results, was $58 per child. The mean cost to identify a true-positive result was $17,162.18
In 2012, Leslie et al20 used simulation models to estimate the societal cost of routine EKG screening to prevent SCD in children with ADHD. Their findings: The cost would be high relative to its health benefits—approximately $91,000 to $204,000 per life year saved. Furthermore, these researchers found that ordering an EKG to screen for 3 common cardiac conditions linked to SCD (HCM, WPW, and LQTS) would add <2 days to a patient’s projected life expectancy.20
Our recommendations
We believe stimulants can safely be used in the treatment of children and adolescents with ADHD, given the evidence that suggests a low risk of SCD. That said, it is prudent to avoid prescribing stimulants for children who have an underlying condition that may deteriorate secondary to increased blood pressure or heart rate.
We agree with the current AHA and AAP recommendations that physicians should obtain an in-depth cardiac history and physical examination, with emphasis on screening for cardiac disorders that may put a child at risk for SCD, such as HCM, LQTS, and preexcitation syndromes. For instance, a history of a family member with palpitations should prompt an EKG, which may reveal familial preexcitation syndrome. Similarly, an EKG is in order if you suspect LQTS based on a parent’s description of a family member’s death after hearing a loud noise, such as fireworks.
It often takes active probing to uncover a history of sudden death in the family that a parent may not consider relevant. For example, one of the authors (SKM) cared for a 6-year-old boy who presented with a history of syncope after his hand got caught in a door jam. On further probing, his mother revealed that her father had died at age 30 while he was taking astemizole, an allergy drug known to prolong the QT interval. Subsequent EKGs revealed that both the boy and his mother had LQTS.
For patients already taking stimulants, we recommend monitoring BP and heart rate and ordering an EKG only if the patient exhibits cardiac symptoms or there are concerns based on follow-up history and physical examination. Should a patient develop palpitations while taking a therapeutic dose of stimulants, a detailed history of the onset and duration of symptoms is important. For example, tachycardia that has a gradual onset and occurs with exercise is suggestive of physiological sinus tachycardia. In our judgment, most patients who experience symptoms that suggest sinus tachycardia simply require downward readjustment of their medication or a switch to a nonstimulant.
However, if the patient or family history prompts you to suspect other arrhythmias such as ectopic beats or supraventricular tachycardia, immediate assessment either in an emergency department or in the physician’s office may be required, because obtaining an EKG during symptoms is crucial for the diagnosis. Similarly, unexplained exercise intolerance or the onset of chest pain associated with exercise, dizziness, syncope, seizures, or dyspnea requires immediate cardiovascular assessment.
And finally, whether your patient has just started taking medication for his or her ADHD or has been on the medication for some time, it’s important to periodically reassess the need to continue the stimulant therapy; ADHD symptoms may decrease during mid- to late adolescence and into adulthood.21
CASE › The FP completed a thorough physical exam and found no evidence of any conditions that would increase the likelihood of SCD in the young patient. There was no history of SCD in the boy’s family, either. Based on these findings, the FP opted to forgo an EKG. She prescribed lisdexamfetamine, starting with 20 mg/d (the lowest dose available) and then monitored his course by telephone. Eventually, 30 mg was found to be an effective dose. At a 6-week follow-up visit, the boy’s ADHD symptoms were substantially reduced, without any adverse effects—cardiac or otherwise.
CORRESPONDENCE
Sudhir Ken Mehta, Cleveland Clinic Children’s Hospital, 9500 Euclid Avenue, Cleveland, OH 44111; kemeht@ccf.org
› Complete a thorough, cardiac-focused history and physical examination before starting stimulants for attention deficit hyperactivity disorder (ADHD) in a child or adolescent. C
› Avoid using stimulants in children or adolescents with comorbid conditions associated with sudden cardiac death, including hypertrophic cardiomyopathy, long QT interval syndrome, and preexcitation syndromes such as Wolff-Parkinson-White syndrome. C
› Monitor all children and adolescents who are taking stimulants for tachycardia, hypertension, palpitations, and chest pain. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE › A young patient has been struggling in school. His worried mother, having had several conferences with the child’s teachers, brings him to the family physician (FP), where he is given a diagnosis of attention deficit hyperactivity disorder (ADHD). The FP considers prescribing a stimulant medication, but first plans on conducting a more thorough family history and exam. She also debates the merits of ordering an electrocardiogram (EKG) to screen for conditions that could lead to sudden cardiac death.
If you were caring for this patient, how would you proceed?
That’s a good question, given the debate that has surrounded this subject since the US Food and Drug Administration (FDA) first learned of 25 cases of sudden death that were linked to stimulant medications.1 The majority of the cases, which were reported to the FDA’s Adverse Event Reporting System between 1999 and 2003, involved amphetamines or methylphenidate in patients under the age of 19.1 In 2008, the American Heart Association (AHA) issued a scientific statement advocating that physicians perform a proper family history and physical exam that includes blood pressure (BP) and an EKG before prescribing a stimulant for children and adolescents.2 The inclusion of EKG screening was intended to increase the likelihood of identifying patients with potentially life-threatening conditions that could lead to sudden cardiac death (SCD).2
Not everyone, however, agreed.
Later that year, the American Academy of Pediatrics (AAP) challenged the routine use of EKGs in this screening process, citing a lack of evidence between stimulant use and the induction of potentially lethal arrhythmias.3 And in 2011, the European Guideline Group also concluded that there was no evidence to suggest an incremental benefit for routine EKG assessment of ADHD patients before initiation of medication.4
Underscoring the uncertainty surrounding the subject are the findings of a 2012 survey of 525 randomly selected US pediatricians.5 Nearly a quarter of the respondents expressed concerns over the risk for SCD in children receiving stimulants for ADHD, and a slightly higher number—30%—worried that the risks for legal liability were high enough to warrant cardiac assessment.5
So how should the prudent FP proceed? In this review, we will describe how to thoroughly screen children and adolescents for their risk of SCD before prescribing stimulants for ADHD. We’ll also summarize what the evidence tells us about whether—and when—you should order an EKG. But first, a word about the pharmacology of stimulants.
How stimulants might increase SCD risk
Stimulants have been used to treat ADHD for more than 40 years6 and are a first-line of therapy for children with ADHD. Stimulants increase attention span by releasing dopamine and norepinephrine at synapses in the frontal cortex, brain stem, and midbrain.
The effect on heart rate and BP. In clinical trials with small samples sizes, children and adolescents receiving stimulants to treat ADHD experienced a minimal rise in heart rate and BP. As measured by 24-hour ambulatory BP monitoring, 13 subjects in a double-blind, randomized, placebo/stimulant crossover trial had slightly elevated total diastolic BP (69.7 vs 65.8 mm Hg; P=.02), waking diastolic BP (75.5 vs 72.3 mm Hg; P=.03), and total heart rate (85.5 vs 79.9 beats per minutes [bpm]; P=.004) while receiving stimulants.7 Other investigators noted similar findings among 17 boys ages 7 to 11 years.8
Whether prolonged childhood exposure to stimulants increases the risk for developing hypertension or tachycardia is unknown. A 10-year follow-up study of 579 children between the ages of 7 to 9 years found stimulants had no effect on systolic or diastolic BP.9 Stimulants use did, however, lead to a higher heart rate (84.2±12.4 vs 79.1±12.0 bpm) during treatment.9 No stimulant-related QT interval changes—which some have proposed might explain SCD in ADHD patients—have been reported in pediatric patients.10 Researchers have noted small increases in mean QTc intervals in adults treated with stimulants for ADHD, but none were >480 msec.11
Steps you should always take before prescribing a stimulant
Before prescribing stimulants to children or adolescents with ADHD, complete an in-depth cardiac history and physical examination, as recommended by the AHA and AAP (TABLE),2,3 to identify conditions that increase the likelihood of SCD, such as hypertrophic cardiomyopathy (HCM), long QT interval syndrome (LQTS), and preexcitation syndromes such as Wolff-Parkinson-White syndrome (WPW).
Confirm, for instance, that your patient has a normal heart rate, rhythm, and BP, and no pathological murmurs. In a survey of families with a child or young adult who had sudden cardiac arrest, 72% reported the patient had at least one cardiovascular symptom within 19 to 71 months of SCD, and 27% reported having a family member with a history of SCD before age 50.12 For patients with no such complaints or family history, the news is good. Two large studies found that in the absence of any suspected or overt cardiac disease, children with ADHD who were receiving stimulant therapy had no increased risk of SCD.13,14
What about patients with this common heart problem? Physicians face a dilemma when a stimulant is needed and the patient has a common acyanotic congenital heart lesion, such as a small atrial or ventricular septal defect, which is considered nonlethal. Based on limited data, there is no evidence that the risk of SCD is higher when these patients take stimulants.15
Should you order that EKG—or not?
Currently, the AHA still favors an EKG, though in a correction to its original statement, it adjusted the language to say that EKG could be “useful,” in addition to an in-depth cardiac history and physical examination.16
Opposition to routine EKG screening in these patients stems from the procedure’s extremely low yield and relatively high false positive findings, which may result in higher financial and psychological burdens for patients and families. Thomas et al17 reported that at a single center, the number of EKGs ordered with an indication of “stimulant medication screening” quadrupled during 2009, the year after the AHA published its recommendations. Of 372 patients referred for EKG, 24 (6.4%) had abnormal findings and 18 were referred for further evaluation, but none were found to have cardiac disease. ADHD therapy was delayed in 6 patients because of the EKG.
In a similar evaluation of 1470 ADHD patients ages 21 years and younger, Mahle et al18 noted that 119 patients (8.1%) had an abnormal EKG, 78 of whom (65%) were already receiving stimulants. Five patients had cardiac disease, including 2 who had a preexcitation syndrome. Overall, the positive predictive value was low (4.2%).18 Other research, including a study lead by one of this article’s authors (SKM), has found similar increases in the number of EKGs ordered for patients with ADHD.19
Cost vs benefit. In the Mahle et al18 study described above, the mean cost of EKG screening, including further testing for patients with abnormal initial results, was $58 per child. The mean cost to identify a true-positive result was $17,162.18
In 2012, Leslie et al20 used simulation models to estimate the societal cost of routine EKG screening to prevent SCD in children with ADHD. Their findings: The cost would be high relative to its health benefits—approximately $91,000 to $204,000 per life year saved. Furthermore, these researchers found that ordering an EKG to screen for 3 common cardiac conditions linked to SCD (HCM, WPW, and LQTS) would add <2 days to a patient’s projected life expectancy.20
Our recommendations
We believe stimulants can safely be used in the treatment of children and adolescents with ADHD, given the evidence that suggests a low risk of SCD. That said, it is prudent to avoid prescribing stimulants for children who have an underlying condition that may deteriorate secondary to increased blood pressure or heart rate.
We agree with the current AHA and AAP recommendations that physicians should obtain an in-depth cardiac history and physical examination, with emphasis on screening for cardiac disorders that may put a child at risk for SCD, such as HCM, LQTS, and preexcitation syndromes. For instance, a history of a family member with palpitations should prompt an EKG, which may reveal familial preexcitation syndrome. Similarly, an EKG is in order if you suspect LQTS based on a parent’s description of a family member’s death after hearing a loud noise, such as fireworks.
It often takes active probing to uncover a history of sudden death in the family that a parent may not consider relevant. For example, one of the authors (SKM) cared for a 6-year-old boy who presented with a history of syncope after his hand got caught in a door jam. On further probing, his mother revealed that her father had died at age 30 while he was taking astemizole, an allergy drug known to prolong the QT interval. Subsequent EKGs revealed that both the boy and his mother had LQTS.
For patients already taking stimulants, we recommend monitoring BP and heart rate and ordering an EKG only if the patient exhibits cardiac symptoms or there are concerns based on follow-up history and physical examination. Should a patient develop palpitations while taking a therapeutic dose of stimulants, a detailed history of the onset and duration of symptoms is important. For example, tachycardia that has a gradual onset and occurs with exercise is suggestive of physiological sinus tachycardia. In our judgment, most patients who experience symptoms that suggest sinus tachycardia simply require downward readjustment of their medication or a switch to a nonstimulant.
However, if the patient or family history prompts you to suspect other arrhythmias such as ectopic beats or supraventricular tachycardia, immediate assessment either in an emergency department or in the physician’s office may be required, because obtaining an EKG during symptoms is crucial for the diagnosis. Similarly, unexplained exercise intolerance or the onset of chest pain associated with exercise, dizziness, syncope, seizures, or dyspnea requires immediate cardiovascular assessment.
And finally, whether your patient has just started taking medication for his or her ADHD or has been on the medication for some time, it’s important to periodically reassess the need to continue the stimulant therapy; ADHD symptoms may decrease during mid- to late adolescence and into adulthood.21
CASE › The FP completed a thorough physical exam and found no evidence of any conditions that would increase the likelihood of SCD in the young patient. There was no history of SCD in the boy’s family, either. Based on these findings, the FP opted to forgo an EKG. She prescribed lisdexamfetamine, starting with 20 mg/d (the lowest dose available) and then monitored his course by telephone. Eventually, 30 mg was found to be an effective dose. At a 6-week follow-up visit, the boy’s ADHD symptoms were substantially reduced, without any adverse effects—cardiac or otherwise.
CORRESPONDENCE
Sudhir Ken Mehta, Cleveland Clinic Children’s Hospital, 9500 Euclid Avenue, Cleveland, OH 44111; kemeht@ccf.org
1. Safety review: Follow up review of AERS search identifying cases of sudden death occurring with drugs used for the treatment of Attention Deficit Hyperactivity Disorder (ADHD). US Food and Drug Administration Web site. Available at: http://www.fda.gov/ohrms/dockets/ac/06/briefing/2006-4210b_07_01_safetyreview.pdf. Accessed January 17, 2014.
2. Vetter VL, Elia J, Erickson C, et al. Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactivity disorder: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee and the Council on Cardiovascular Nursing. Circulation. 2008;117:2407-2423.
3. Perrin JM, Friedman RA, Knilans TK; Black Box Working Group; Section on Cardiology and Cardiac Surgery. Cardiovascular monitoring and stimulant drugs for attention-deficit/hyperactivity disorder. Pediatrics. 2008;122:451-453.
4. Graham J, Banaschewski T, Buitelaar J, et al; European Guidelines Group. European guidelines on managing adverse effects of medication for ADHD. Eur Child Adolesc Psychiatry. 2011;20:17-37.
5. Leslie LK, Rodday AM, Saunders TS, et al. Cardiac screening prior to stimulant treatment of ADHD: a survey of US-based pediatricians. Pediatrics. 2012;129:222-230.
6. Conners CK. Symposium: behavior modification by drugs. II. Psychological effects of stimulant drugs in children with minimal brain dysfunction. Pediatrics. 1972;49:702-708.
7. Samuels JA, Franco K, Wan F, et al. Effect of stimulants on 24-h ambulatory blood pressure in children with ADHD: a double-blind, randomized, cross-over trial. Pediatr Nephrol. 2006;21:92-95.
8. Stowe CD, Gardner SF, Gist CC, et al. 24-hour ambulatory blood pressure monitoring in male children receiving stimulant therapy. Ann Pharmacother. 2002;36:1142-1149.
9. Vitiello B, Elliott GR, Swanson JM, et al. Blood pressure and heart rate over 10 years in the multimodal treatment study of children with ADHD. Am J Psychiatry. 2012;169:167-177.
10. Hammerness P, Wilens T, Mick E, et al. Cardiovascular effects of longer-term, high-dose OROS methylphenidate in adolescents with attention deficit hyperactivity disorder. J Pediatr. 2009;155:84-89,89.e1.
11. Weisler RH, Biederman J, Spencer TJ, et al. Long-term cardiovascular effects of mixed amphetamine salts extended release in adults with ADHD. CNS Spectr. 2005;10(suppl 20):35-43.
12. Drezner JA, Fudge J, Harmon KG, et al. Warning symptoms and family history in children and young adults with sudden cardiac arrest. J Am Board Fam Med. 2012;25:408-415.
13. Cooper WO, Habel LA, Sox CM, et al. ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med. 2011;365:1896-1904.
14. Schelleman H, Bilker WB, Strom BL, et al. Cardiovascular events and death in children exposed and unexposed to ADHD agents. Pediatrics. 2011;127:1102-1110.
15. Winterstein AG, Gerhard T, Kubilis P, et al. Cardiovascular safety of central nervous system stimulants in children and adolescents: population based cohort study. BMJ. 2012;345:e4627.
16. Vetter VL, Elia J, Erickson C, et al. Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactivity disorder: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee and the Council on Cardiovascular Nursing [published correction appears in Circulation. 2009;120:e55-e59]. Circulation. 2008;117:2407-2423.
17. Thomas PE, Carlo WF, Decker JA, et al. Impact of the American Heart Association scientific statement on screening electrocardiograms and stimulant medications. Arch Pediatr Adolesc Med. 2011;165:166-170.
18. Mahle WT, Hebson C, Strieper MJ. Electrocardiographic screening in children with attention-deficit hyperactivity disorder. Am J Cardiol. 2009;104:1296-1299.
19. Mehta SK, Richards N, Jacobs I. Children and adolescents with attention deficit hyperactivity disorder in a pediatric cardiology office. Cardiol Young. 2010;20(suppl 3):167.
20. Leslie LK, Cohen JT, Newburger JW, et al. Costs and benefits of targeted screening for causes of sudden cardiac death in children and adolescents. Circulation. 2012;125:2621-2629.
21. Mannuzza S, Klein RG, Bessler A, et al. Adult psychiatric status of hyperactive boys grown up. Am J Psychiatry. 1998;155:493-488.
1. Safety review: Follow up review of AERS search identifying cases of sudden death occurring with drugs used for the treatment of Attention Deficit Hyperactivity Disorder (ADHD). US Food and Drug Administration Web site. Available at: http://www.fda.gov/ohrms/dockets/ac/06/briefing/2006-4210b_07_01_safetyreview.pdf. Accessed January 17, 2014.
2. Vetter VL, Elia J, Erickson C, et al. Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactivity disorder: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee and the Council on Cardiovascular Nursing. Circulation. 2008;117:2407-2423.
3. Perrin JM, Friedman RA, Knilans TK; Black Box Working Group; Section on Cardiology and Cardiac Surgery. Cardiovascular monitoring and stimulant drugs for attention-deficit/hyperactivity disorder. Pediatrics. 2008;122:451-453.
4. Graham J, Banaschewski T, Buitelaar J, et al; European Guidelines Group. European guidelines on managing adverse effects of medication for ADHD. Eur Child Adolesc Psychiatry. 2011;20:17-37.
5. Leslie LK, Rodday AM, Saunders TS, et al. Cardiac screening prior to stimulant treatment of ADHD: a survey of US-based pediatricians. Pediatrics. 2012;129:222-230.
6. Conners CK. Symposium: behavior modification by drugs. II. Psychological effects of stimulant drugs in children with minimal brain dysfunction. Pediatrics. 1972;49:702-708.
7. Samuels JA, Franco K, Wan F, et al. Effect of stimulants on 24-h ambulatory blood pressure in children with ADHD: a double-blind, randomized, cross-over trial. Pediatr Nephrol. 2006;21:92-95.
8. Stowe CD, Gardner SF, Gist CC, et al. 24-hour ambulatory blood pressure monitoring in male children receiving stimulant therapy. Ann Pharmacother. 2002;36:1142-1149.
9. Vitiello B, Elliott GR, Swanson JM, et al. Blood pressure and heart rate over 10 years in the multimodal treatment study of children with ADHD. Am J Psychiatry. 2012;169:167-177.
10. Hammerness P, Wilens T, Mick E, et al. Cardiovascular effects of longer-term, high-dose OROS methylphenidate in adolescents with attention deficit hyperactivity disorder. J Pediatr. 2009;155:84-89,89.e1.
11. Weisler RH, Biederman J, Spencer TJ, et al. Long-term cardiovascular effects of mixed amphetamine salts extended release in adults with ADHD. CNS Spectr. 2005;10(suppl 20):35-43.
12. Drezner JA, Fudge J, Harmon KG, et al. Warning symptoms and family history in children and young adults with sudden cardiac arrest. J Am Board Fam Med. 2012;25:408-415.
13. Cooper WO, Habel LA, Sox CM, et al. ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med. 2011;365:1896-1904.
14. Schelleman H, Bilker WB, Strom BL, et al. Cardiovascular events and death in children exposed and unexposed to ADHD agents. Pediatrics. 2011;127:1102-1110.
15. Winterstein AG, Gerhard T, Kubilis P, et al. Cardiovascular safety of central nervous system stimulants in children and adolescents: population based cohort study. BMJ. 2012;345:e4627.
16. Vetter VL, Elia J, Erickson C, et al. Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactivity disorder: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee and the Council on Cardiovascular Nursing [published correction appears in Circulation. 2009;120:e55-e59]. Circulation. 2008;117:2407-2423.
17. Thomas PE, Carlo WF, Decker JA, et al. Impact of the American Heart Association scientific statement on screening electrocardiograms and stimulant medications. Arch Pediatr Adolesc Med. 2011;165:166-170.
18. Mahle WT, Hebson C, Strieper MJ. Electrocardiographic screening in children with attention-deficit hyperactivity disorder. Am J Cardiol. 2009;104:1296-1299.
19. Mehta SK, Richards N, Jacobs I. Children and adolescents with attention deficit hyperactivity disorder in a pediatric cardiology office. Cardiol Young. 2010;20(suppl 3):167.
20. Leslie LK, Cohen JT, Newburger JW, et al. Costs and benefits of targeted screening for causes of sudden cardiac death in children and adolescents. Circulation. 2012;125:2621-2629.
21. Mannuzza S, Klein RG, Bessler A, et al. Adult psychiatric status of hyperactive boys grown up. Am J Psychiatry. 1998;155:493-488.