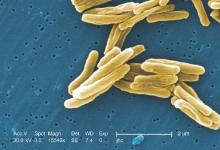
Tuberculosis caused by Mycobacterium africanum West Africa 2 is significantly less likely to be detected by a MPT64 rapid antigen test than is M. tuberculosis, according to a research team based in the Gambia.
A total of 173 MGIT culture-positive sputum samples were included in the study, and the initial MPT64 test was negative in 23 samples. Just over 90% of M. tuberculosis (MTB) samples converted to positive on day 0, while only 78.4% of M. africanum West Africa 2 (MAF2) samples converted. After 10 days, 97.5% of MTB samples were positive, while conversion of MAF2 samples remained low at 84.3%.
In a comparison of the mRNA transcript from samples of six MTB and five MAF2 patients who had not been treated for TB, the MTP64 gene was about 2.5 times more abundant in the MTB samples than the MAF2 samples. No association was found between conversion to positivity and sex, age, therapy, or mycobacterial growth units.
“Given the relatively low cost, limited technical expertise, and shorter turnaround time associated with using rapid speciation tests, compared to alternative speciation methods, MPT64 rapid tests will likely remain one of the preferred options for timely diagnosis of suspected TB despite the possibility of false negative results. Therefore, a negative MPT64 result would require confirmation by an alternative method, such as molecular tests or culture on p-nitrobenzoic acid, depending on laboratory infrastructure and resources,” the investigators noted.
Read the full study in PLoS Neglected Tropical Diseases (doi:10.1371/journal.pntd.0004801).