Noninvasive Ventilation in Neuromuscular Disease
Sreelatha Naik, MD
Assistant Professor of Medicine
Program Director, Sleep Medicine Fellowship, Divison of Pulmonary, Critical Care and Sleep Medicine
Geisinger Commonwealth School of Medicine
Divison Chief
Geisinger Northeast Region
Divison of Pulmonary, Critical Care and Sleep Medicine
Geisinger Health System
Scranton, PA
Sreelatha Naik, MD, has disclosed the following relevant financial relationships:
Serve(d) as a speaker or a member of a speakers bureau for: 2 talks for ResMed
Kelly LoBrutto, CRNP
Nurse Practitioner
Pulmonary Medicine
Geisinger Health System
Wilkes Barre, PA
Kelly LoBrutto, MSN, has disclosed no relevant financial relationships.

Noninvasive ventilation (NIV) delivers oxygen into the lungs via positive pressure without the need for endotracheal intubation and is typically used in COPD, obesity hypoventilation syndrome, and neuromuscular disease (NMD).1 Clinicians are used to recognizing pulmonary diseases that require ventilation, but NMDs—in which early intervention is critical due to its effect on respiration—are often overlooked. Emerging data show that patients with lung function even at 80% may benefit from early NIV in the long term.2 NMDs that benefit from NIV include amyotrophic lateral sclerosis (ALS), myasthenia gravis, and muscular dystrophies.2-4
New CHEST guidelines for NMD respiratory management provide guidance on the timing of pulmonary function testing, when to initiate NIV, and how to manage sleep-disordered breathing.2 Clinicians should be aware of inconsistencies between CHEST and Medicare/insurance reimbursement guidelines.5 For example, current Medicare/insurance guidelines require vital capacity to be < 50% to treat with NIV, whereas CHEST guidelines recommend a threshold of 80% if a patient is symptomatic based on more recent evidence.5
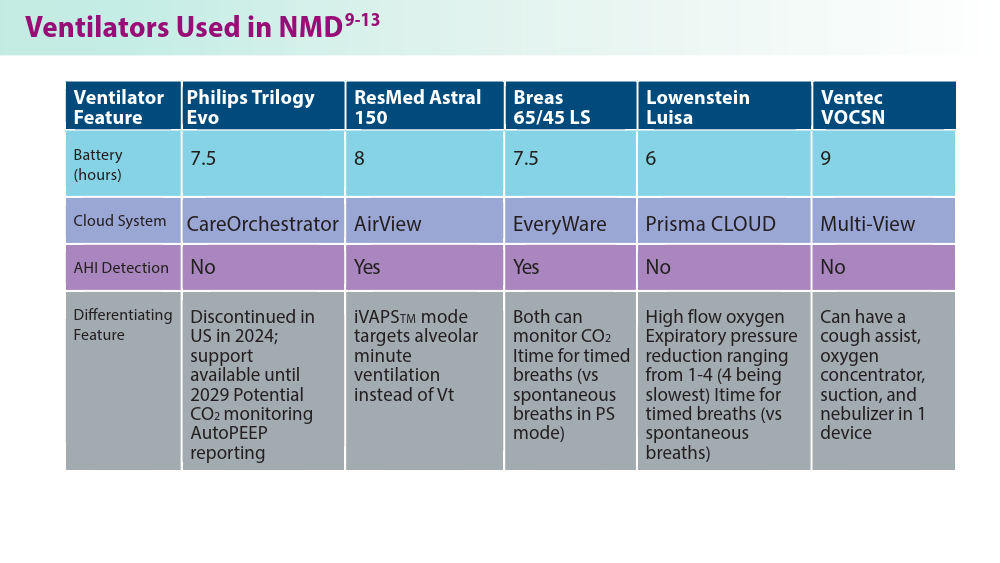
Due largely to increased respiratory fragility during the COVID-19 pandemic, there has been an increased need for NIV and home ventilation (HMV) devices, and the number of available devices has also expanded due to the NIV recall.6,7 These new ventilators each have their own unique features that can optimize to certain conditions and populations and more data is now available to address previously unanswered treatment questions.6 Data on measures, such as mode, observed overall usage, respiratory rates, tidal volumes, and pressures, can now help determine optimal ventilator use and long-term outcomes in NMDs.6
1
-
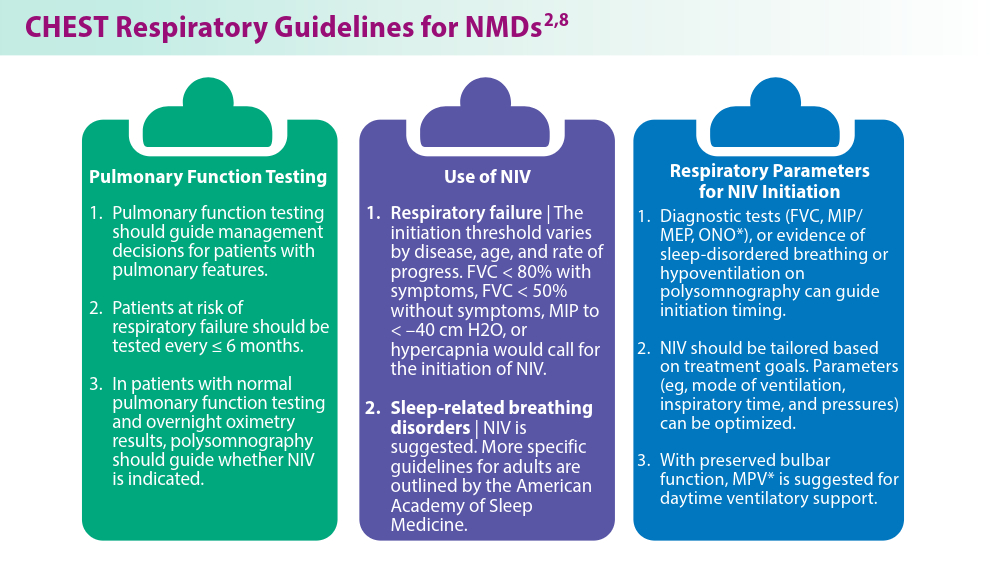
*MPV, mouthpiece ventilation; ONO, overnight oximetry
-
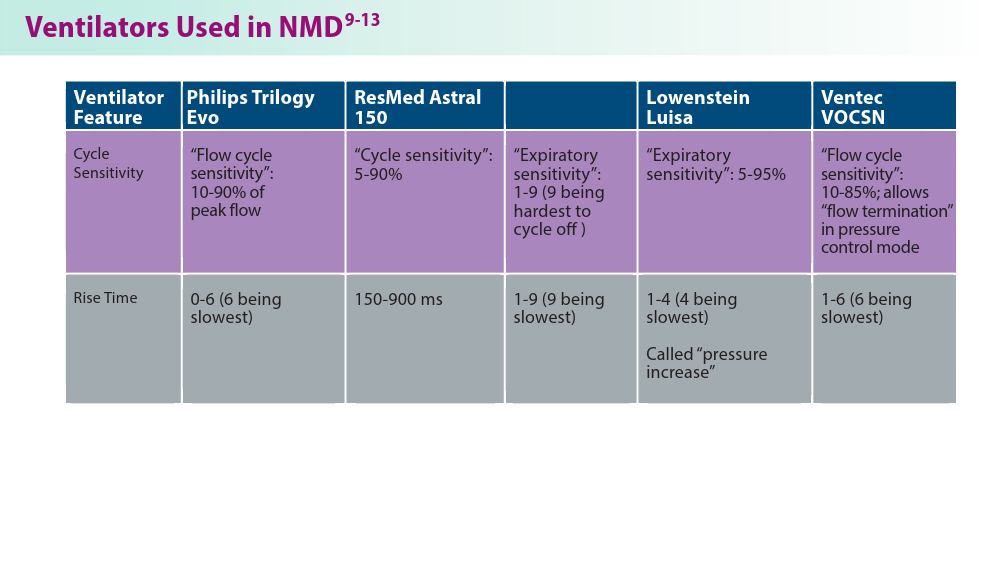
ltime, inspiratory time
-
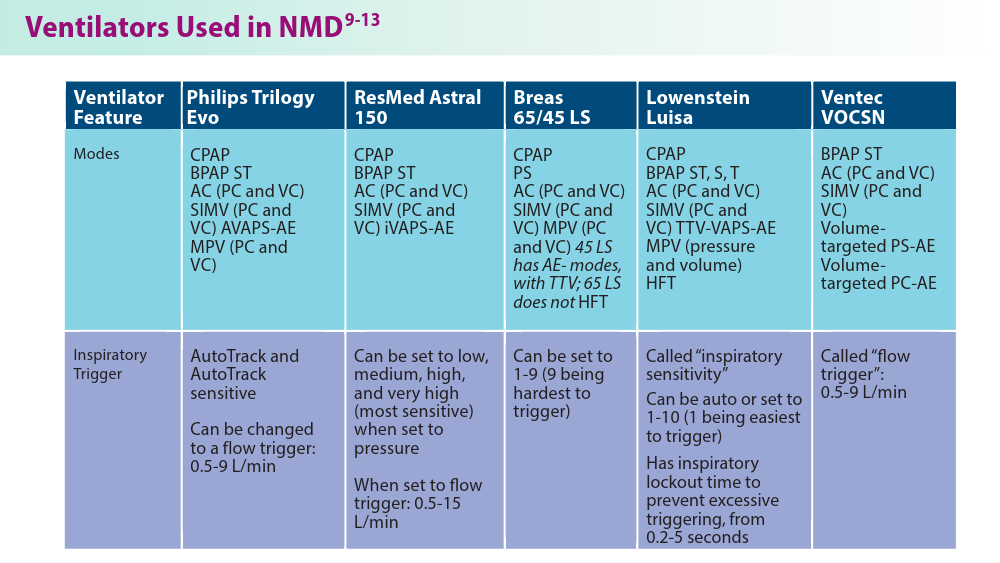
*AC, assist control; AE, automatically adjusting expiratory positive airway pressure; AHI, Apnea-Hypopnea Index; AVAPS, automatic volume assure pressure support; BPAP, bilevel positive airway pressure; CO2, carbon dioxide; CPAP, continuous positive airway pressure; HFT, high-flow therapy; iBR, intelligent backup rate; iVAPS, intelligent volume assured pressure support; PC, pressure control; PEEP, positive end expiratory pressure; PS, pressure support; RR, respiratory rate; S, spontaneous triggering for breaths; SIMV, synchronized intermittent mandatory ventilation; ST, spontaneous triggering, but timed breaths are given if no spontaneous breaths; T, timed breaths only; TTV, targeted tidal volume; VAPS, volume-assured pressure support; VC, volume control; Vt, tidal volume
-