User login
In the August 2016 issue of OBG
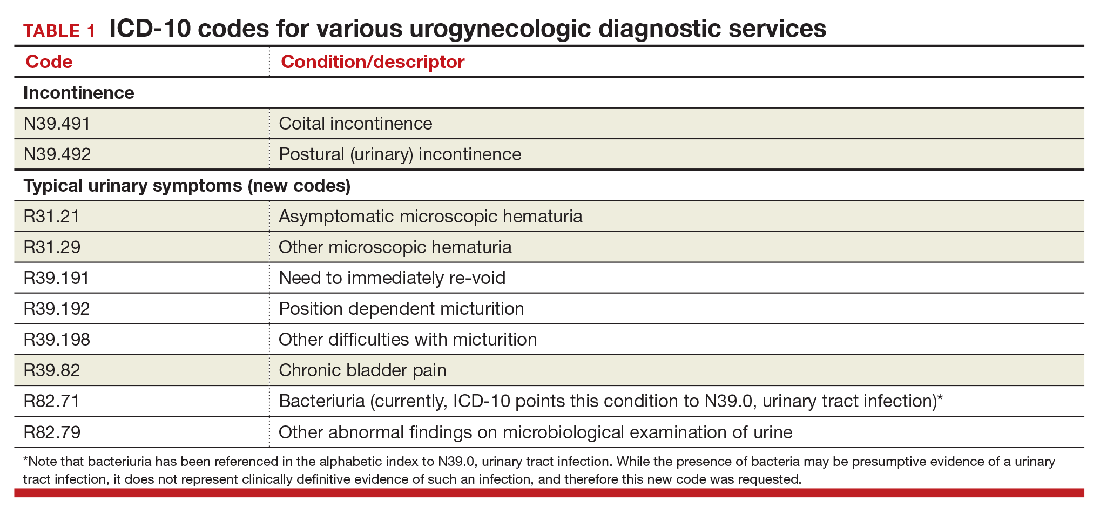
Urogynecology diagnostic codes
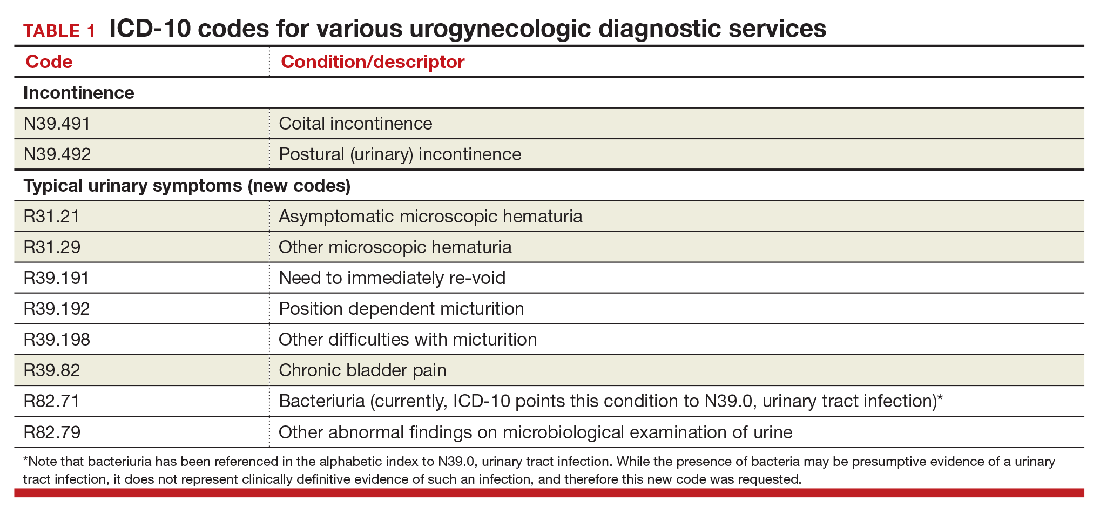
Urogynecologists will find a large number of changes to codes they can select on October 1, 2016. While some codes improve reporting for conditions or symptoms related to urinary issues, many more concern postoperative complications following surgery for devices and grafts applied to the genitourinary system.
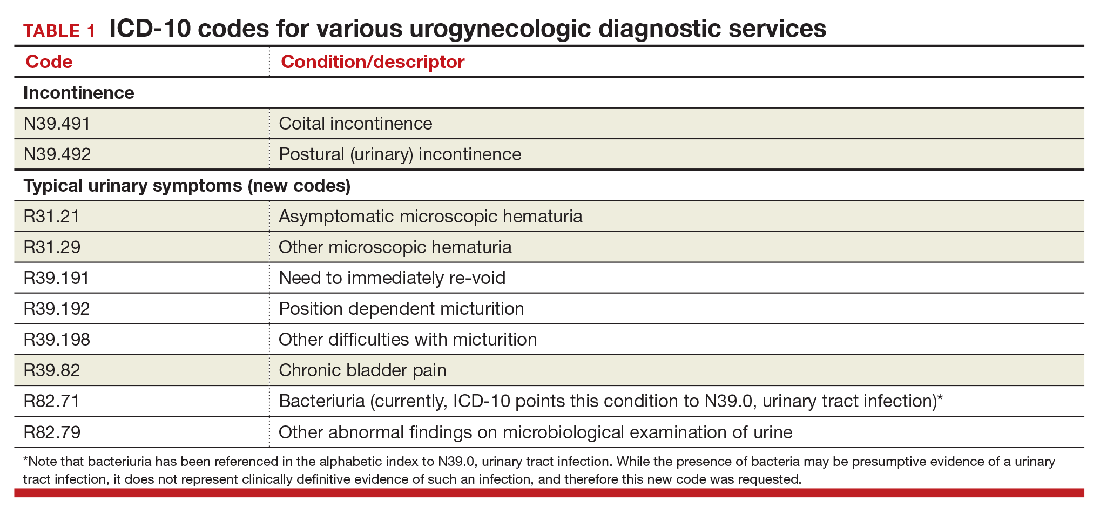
The American Urological Association requested new codes to align with a 2009 joint report on the terminology for female pelvic floor dysfunction.1 These codes, along with others, are listed in TABLE 1.
Urinary procedure complication codes
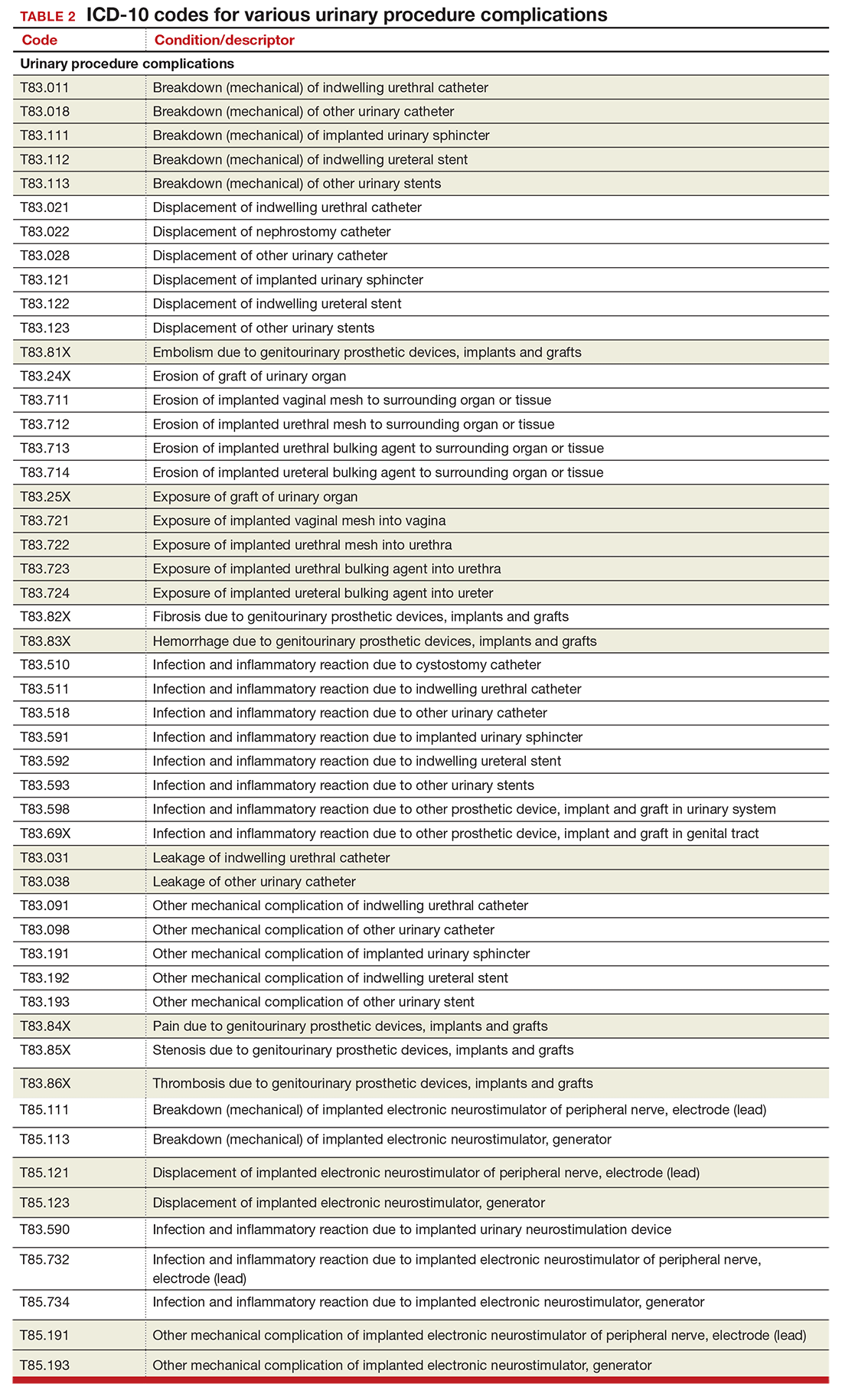
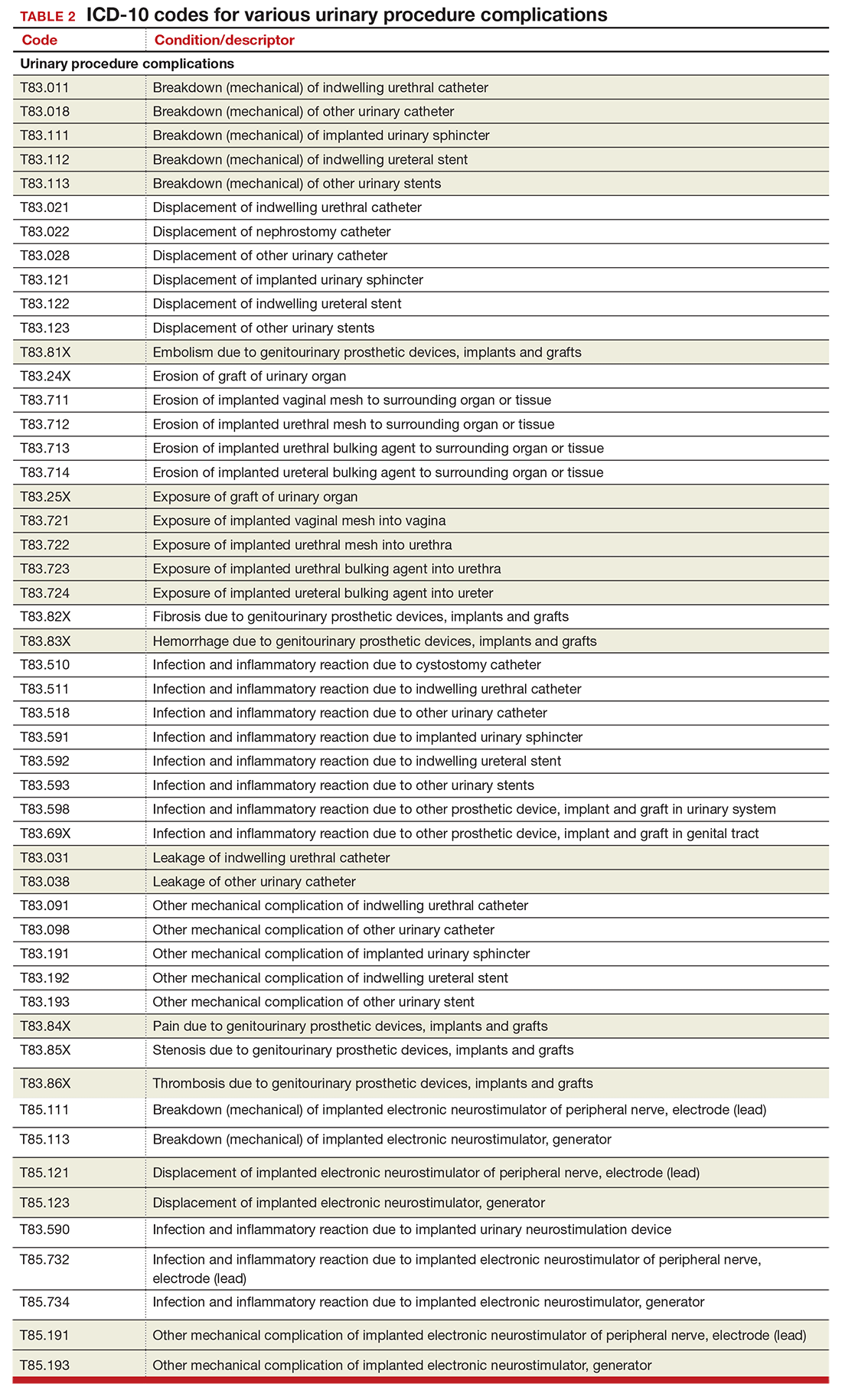
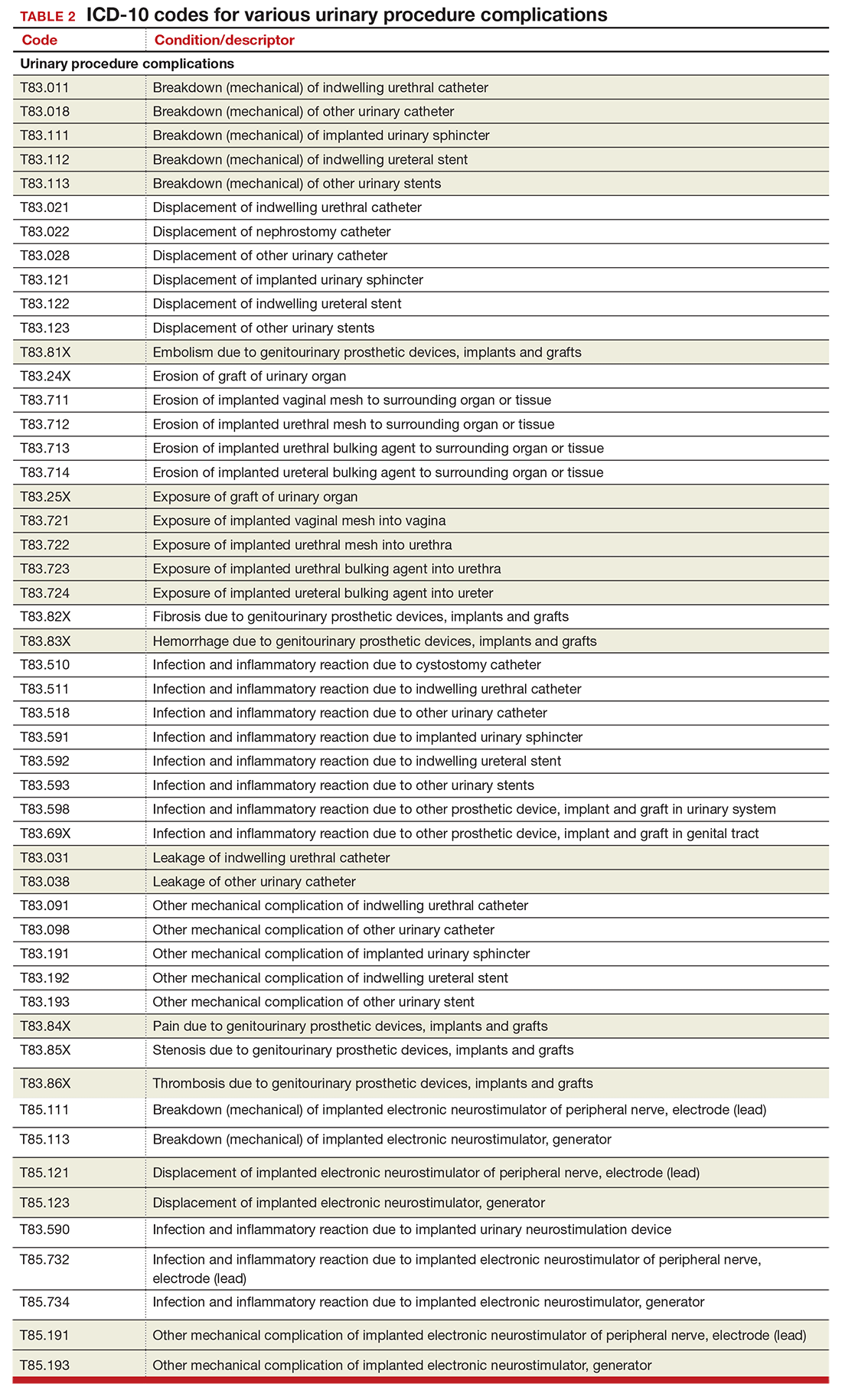
Not every urogynecologist will have an issue after surgery for incontinence, but if they do, there are tons of new and revised codes to address every possible complication the patient may have (TABLE 2). Each of these codes is reported based on whether the complication is being actively treated (initial encounter: final character is A), is being followed up after treatment (subsequent encounter: final character is D), or is caused by another condition (sequela: final character is S).
Gynecology-related diagnostic codes
Laterality
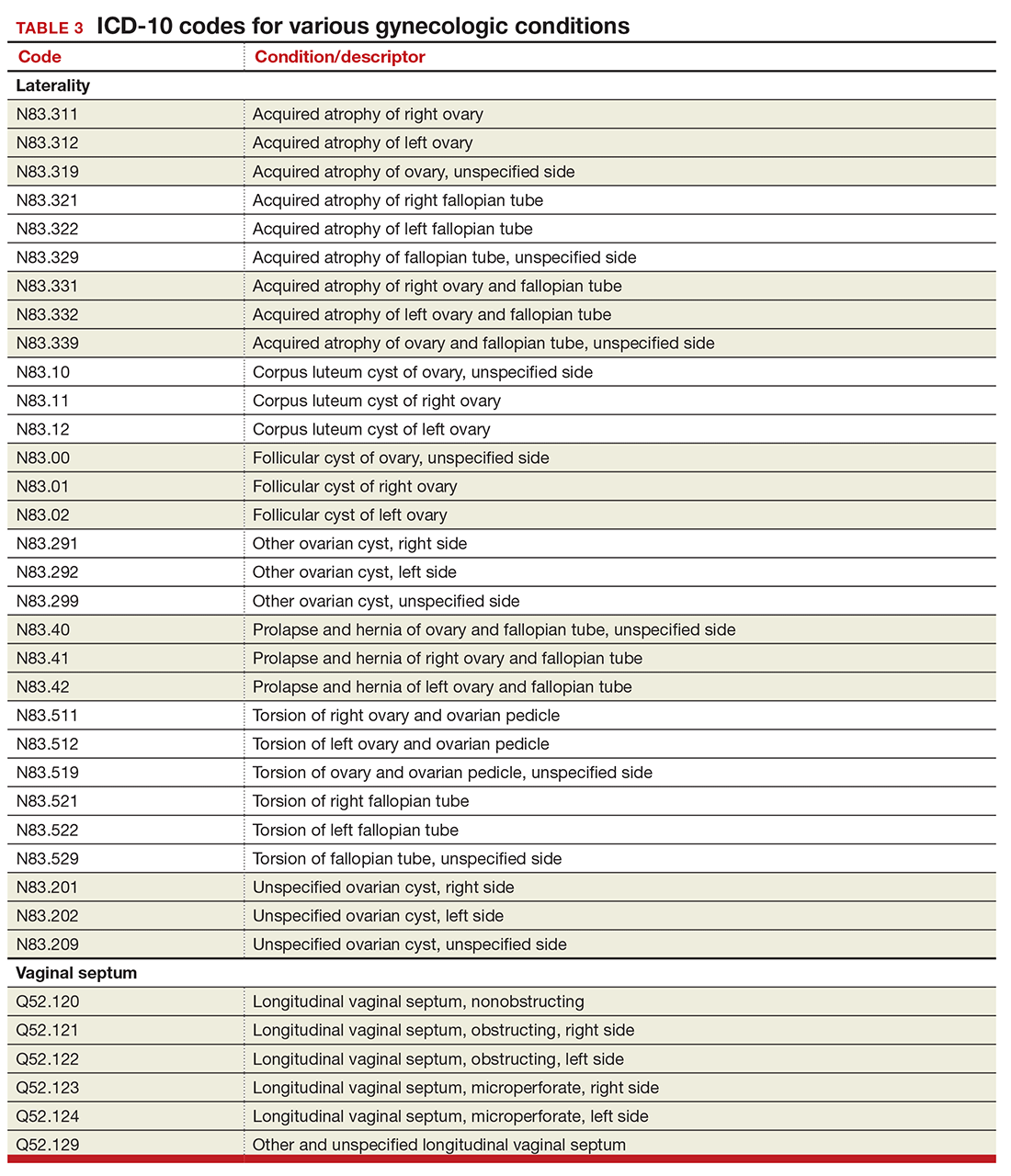
If there are 2 organs in the genitourinary system, the chances are good that there is now a right and a left designation code in ICD-10. Documentation should be clear, of course, and if the condition exists on both the right and the left side (even if only one side is being treated actively), list both codes, as there is no bilateral designation in the codes (TABLE 3). And while there is a code for “unspecified side,” providers normally do know which side, so use of this code should be avoided, if possible.
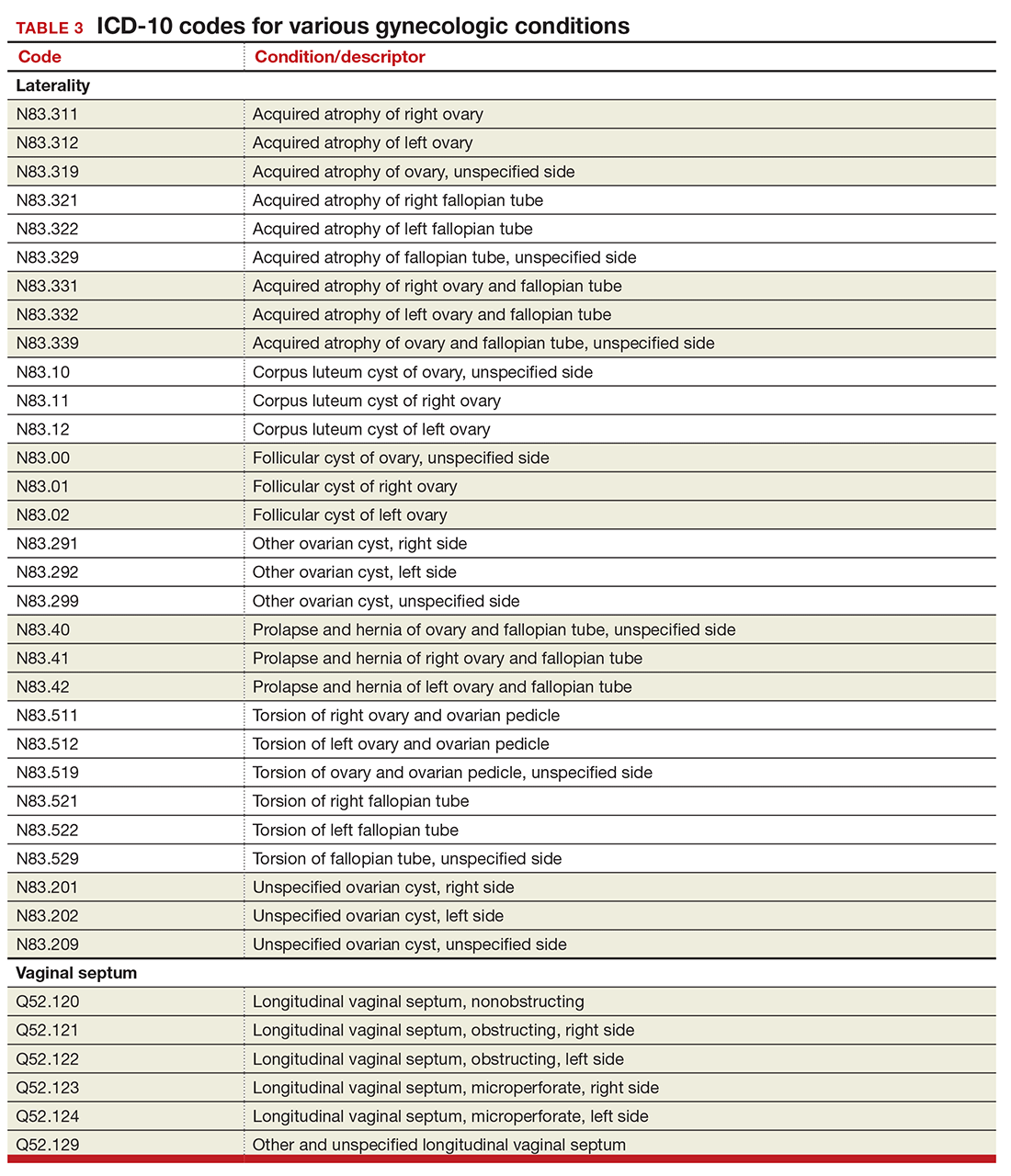
Vaginal septum
The right and left designations extend to the congenital codes for vaginal septum, but they go one step further. The American Congress of Obstetricians and Gynecologists (ACOG) requested that the codes for longitudinal vaginal septum be expanded to differentiate a nonobstructing vaginal septum from an obstructing vaginal septum, in addition to adding laterality to these codes (TABLE 3).2
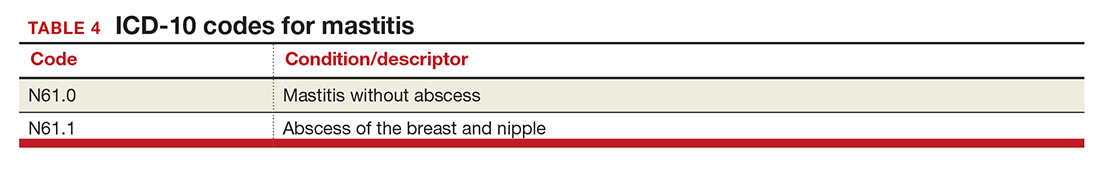
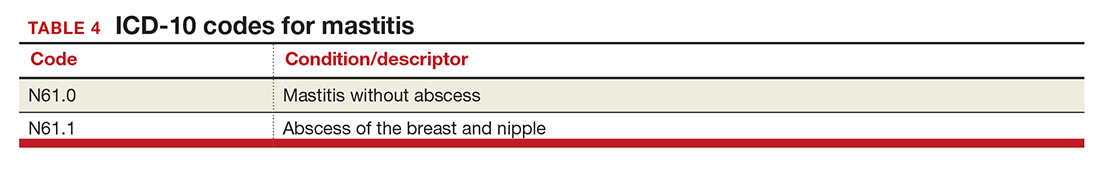
Mastitis
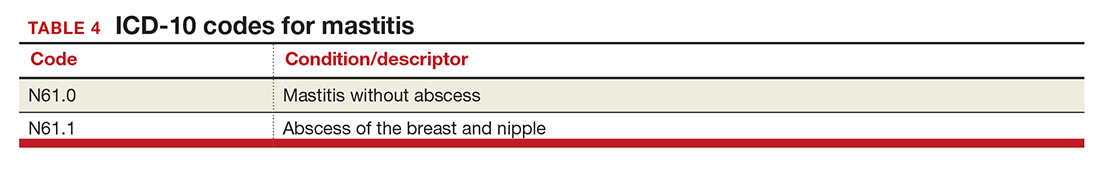
There are now 2 new codes for inflammation of the breast; one describes mastitis without abscess, while the other code includes an abscess of the breast and nipple (TABLE 4). Once again, documentation will lead to the most specific code to describe the findings.
Childhood and prepubertal concerns
The single code for hypertrophy of the vulva has been expanded to include asymmetric labium majus enlargement. This code was requested by ACOG because this is a known clinical diagnosis and the currently available vulvar codes are inadequate for capturing this condition. The vulvar enlargement appears to be in response to hormonal surges during prepuberty and early puberty. Adult hypertrophy, either congenital or acquired from childbirth or as a late result of an old injury, would be reported by the “other specified” code (TABLE 5).
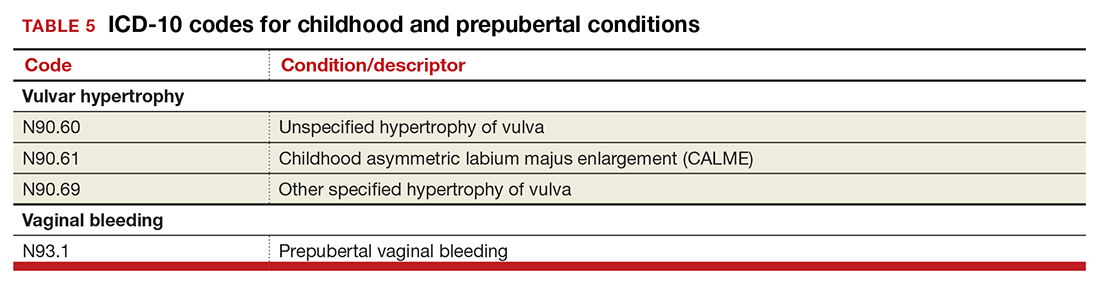
The causes of prepubertal bleeding vary and include the presence of a foreign object, tumors, or fluctuations in hormones, but prepubertal bleeding differs from the bleeding associated with normal menstruation. For that reason, ACOG requested a code that better captures the nature of the condition before a thorough work-up has pinpointed the cause (TABLE 5). Once the cause of the bleeding is known, a more specific diagnosis would then be reported (eg, D28.1, Benign neoplasm of vagina, or T19.2XXA, Foreign body in vulva and vagina, initial encounter).
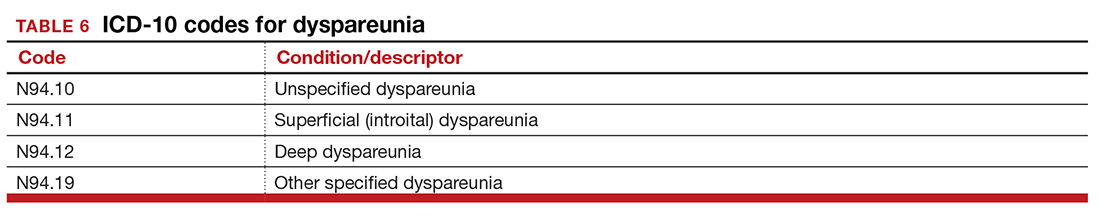
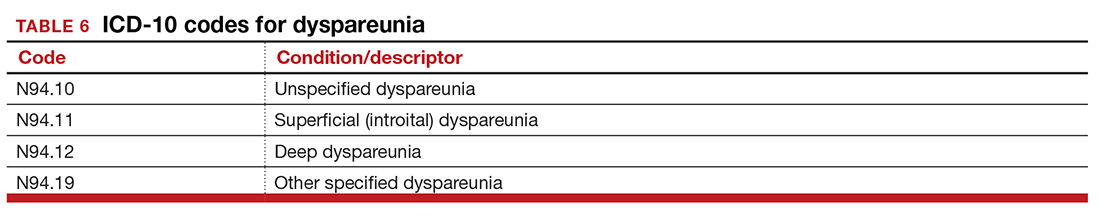
Dypareunia
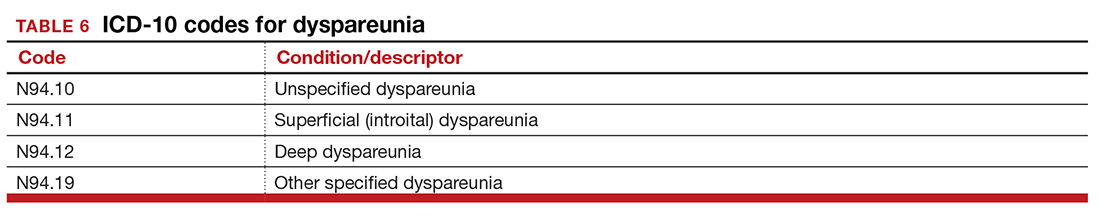
Additional documentation for dyspareunia will now be required to ensure that the most specific code is reported. In this case, the clinician should identify whether the pain is superficial or deep to better report on female pelvic floor dysfunction and to support the different treatments based on the location of the pain (TABLE 6). Deep dyspareunia would be felt in the mid or upper vagina.
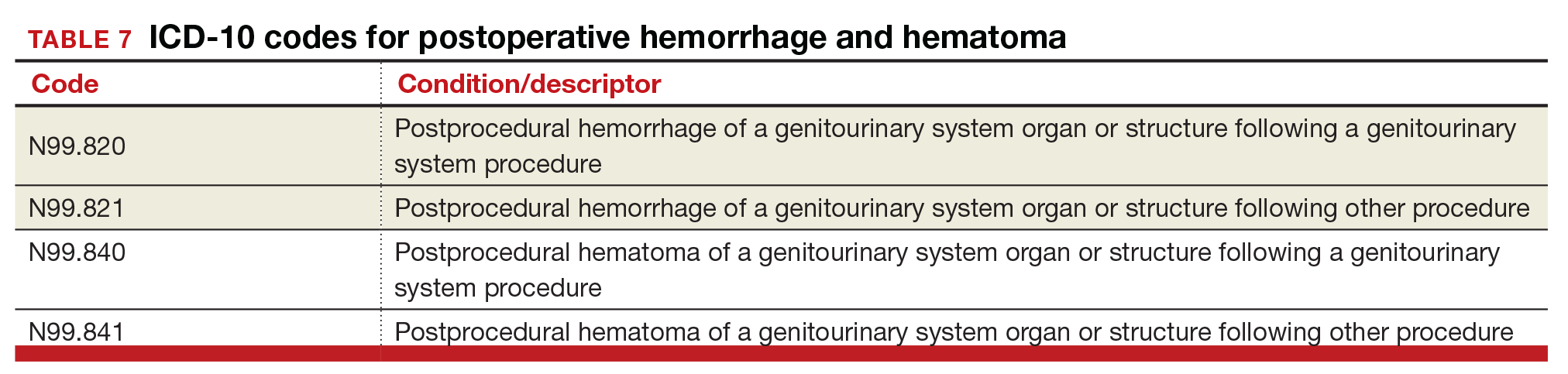
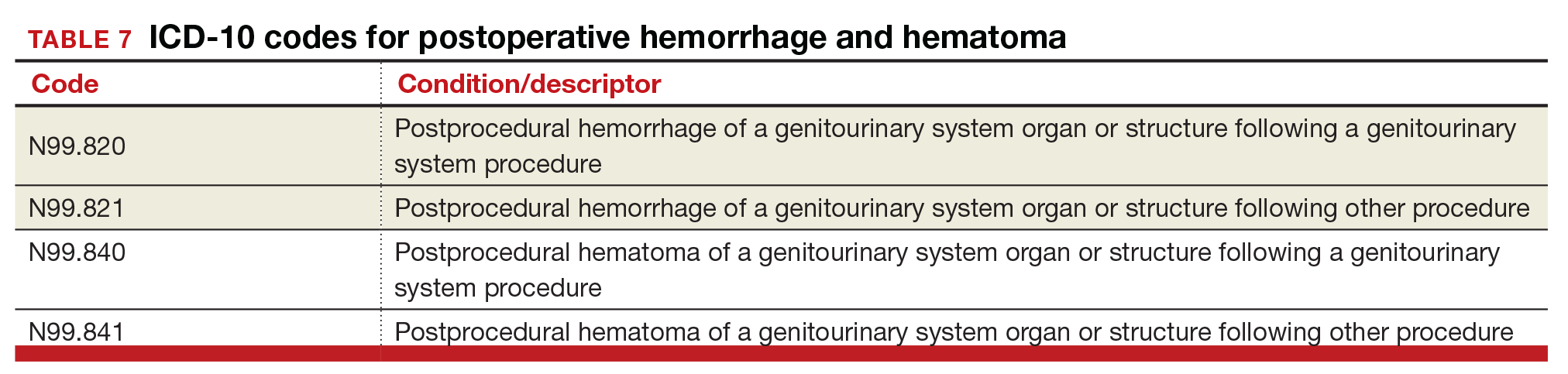
Postoperative hemorrhage and hematoma
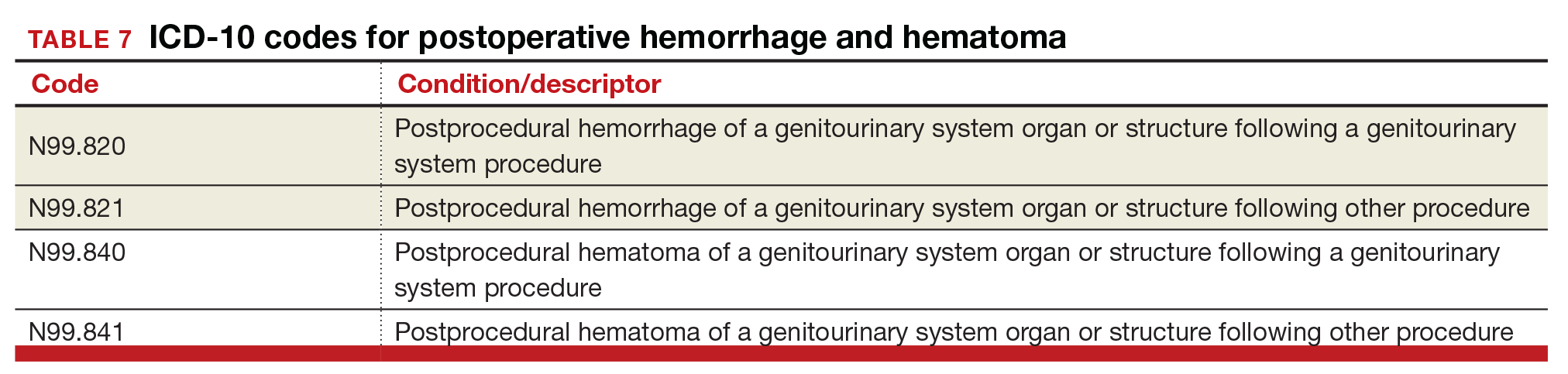
The codes for postprocedural hemorrhage and hematomas have received a face-lift: the single codes for these 2 complications will be split so that each can be reported separately (TABLE 7). Note that the new codes require that the condition be found following the initial surgery, and the code selected depends on whether the surgery involved the genitourinary system or another system.
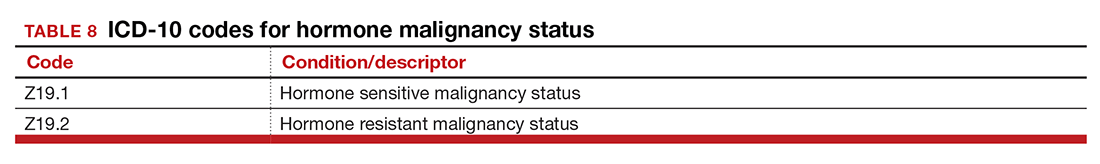
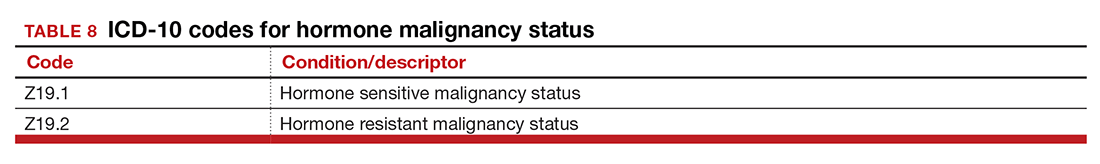
Hormone malignancy status
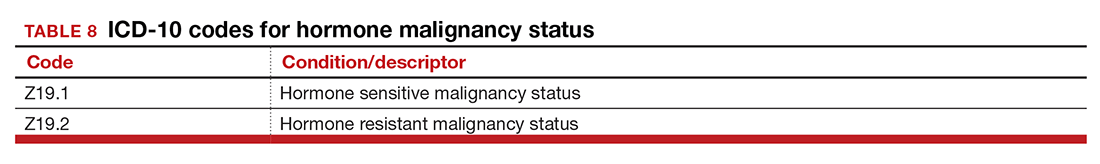
The new Z19 codes will augment information known about a patient’s neoplasm (TABLE 8). The ICD-10 rule states that the type and location of the neoplasm are always coded first, followed by one of the new Z19 codes, if known.
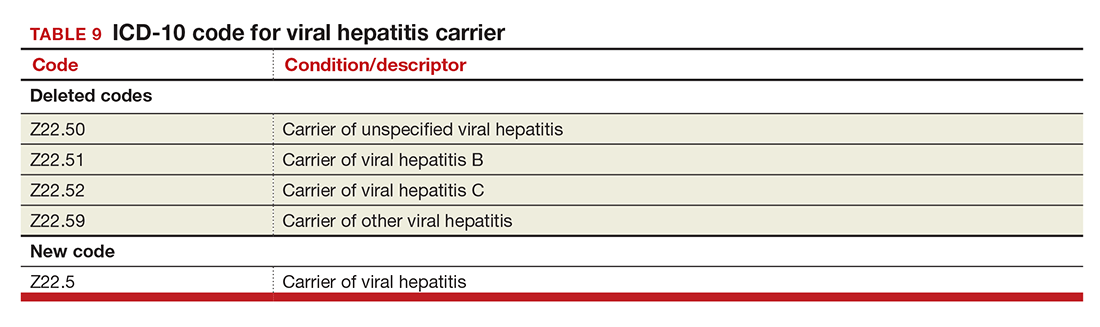
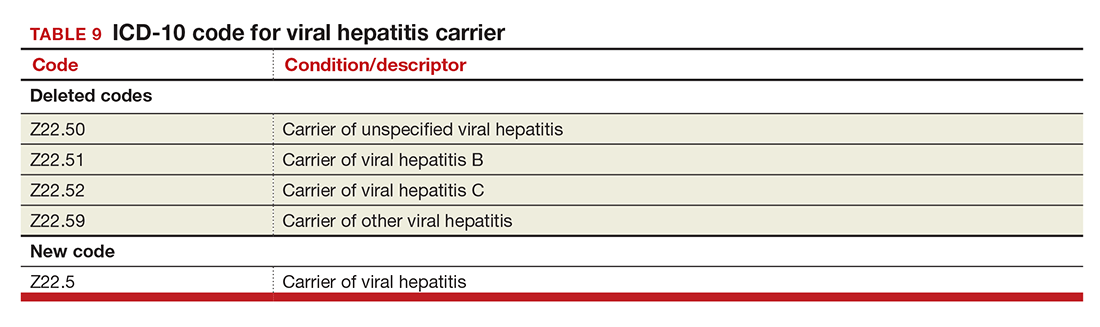
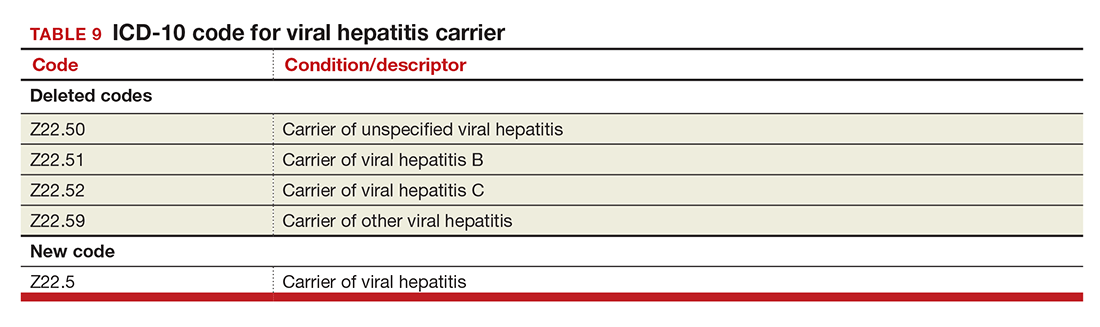
Viral hepatitis carrier
The more specific code for type of viral hepatitis the patient is a carrier of has been bundled into a single code for viral hepatitis (TABLE 9). Carrier status in ICD-10 is defined as a person who harbors the specific organisms of a disease, does not currently have any symptoms, but is capable of transmitting the infection.
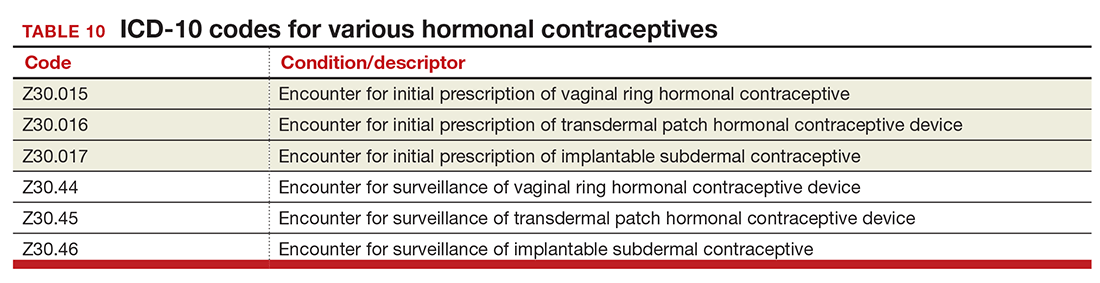
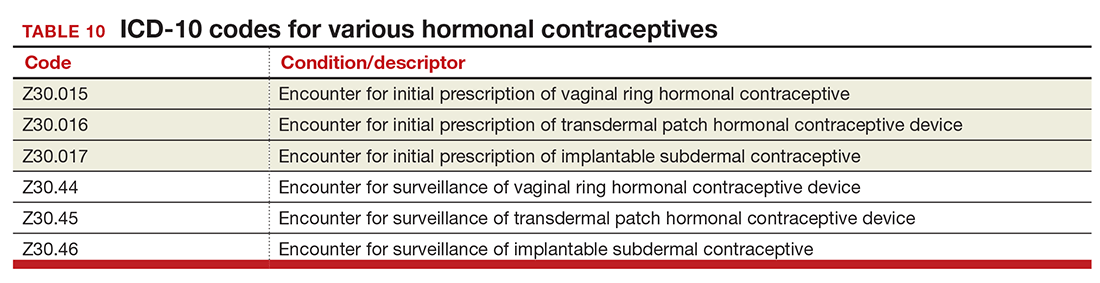
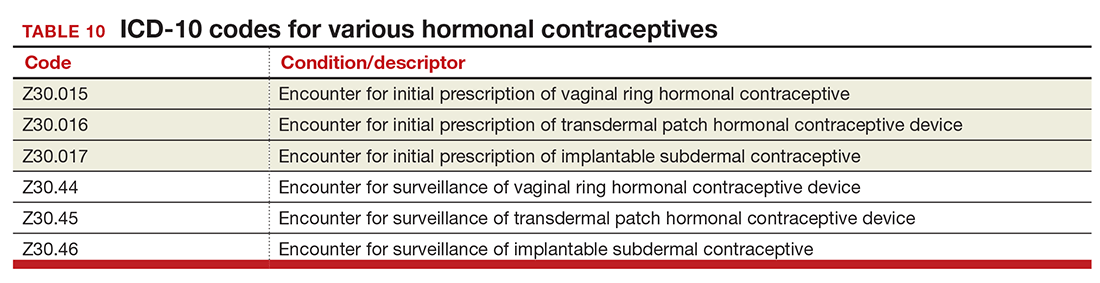
Contraception
The good news is that the ICD-9 code for contraceptive subdermal implants has been added to ICD-10 coding. In addition, the codes for contraceptive methods have been expanded to also include vaginal rings and transdermal patches (TABLE 10).
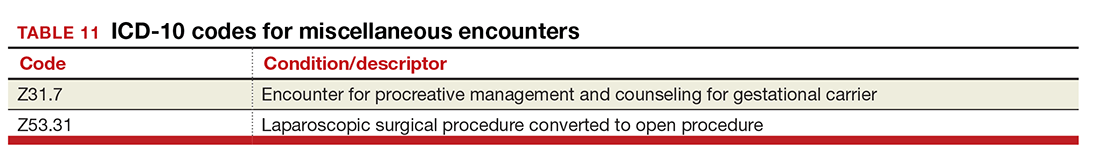
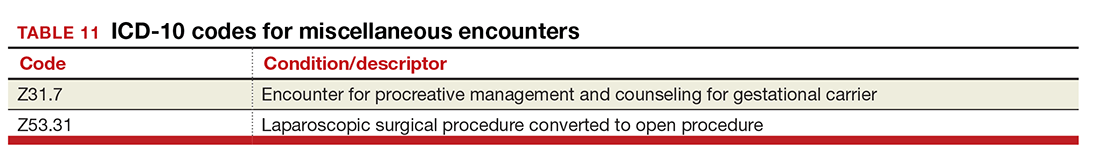
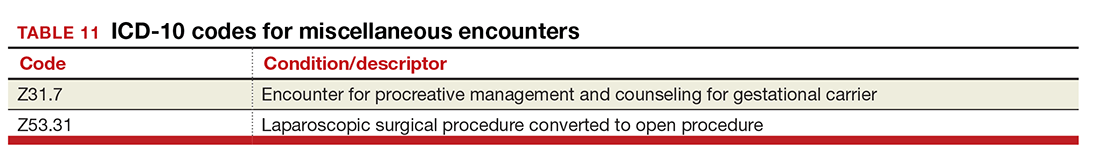
Miscellaneous code changes
Counseling a patient prior to pregnancy just got easier with the addition of a code for gestational carriers. Also, the old ICD-9 code that let a payer know that a procedure was converted from a laparoscopic to an open abdominal procedure is back (TABLE 11).
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee Meeting: diagnosis agenda. September 23–24, 2014;28–29. https://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed August 30, 2016.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee Meeting: diagnosis agenda. March 18–19, 2015. http://www.cdc.gov/nchs/data/icd/Tentative_Agenda_March%202015_Final.pdf. Accessed August 30, 2016.
In the August 2016 issue of OBG
Urogynecology diagnostic codes
Urogynecologists will find a large number of changes to codes they can select on October 1, 2016. While some codes improve reporting for conditions or symptoms related to urinary issues, many more concern postoperative complications following surgery for devices and grafts applied to the genitourinary system.
The American Urological Association requested new codes to align with a 2009 joint report on the terminology for female pelvic floor dysfunction.1 These codes, along with others, are listed in TABLE 1.
Urinary procedure complication codes
Not every urogynecologist will have an issue after surgery for incontinence, but if they do, there are tons of new and revised codes to address every possible complication the patient may have (TABLE 2). Each of these codes is reported based on whether the complication is being actively treated (initial encounter: final character is A), is being followed up after treatment (subsequent encounter: final character is D), or is caused by another condition (sequela: final character is S).
Gynecology-related diagnostic codes
Laterality
If there are 2 organs in the genitourinary system, the chances are good that there is now a right and a left designation code in ICD-10. Documentation should be clear, of course, and if the condition exists on both the right and the left side (even if only one side is being treated actively), list both codes, as there is no bilateral designation in the codes (TABLE 3). And while there is a code for “unspecified side,” providers normally do know which side, so use of this code should be avoided, if possible.
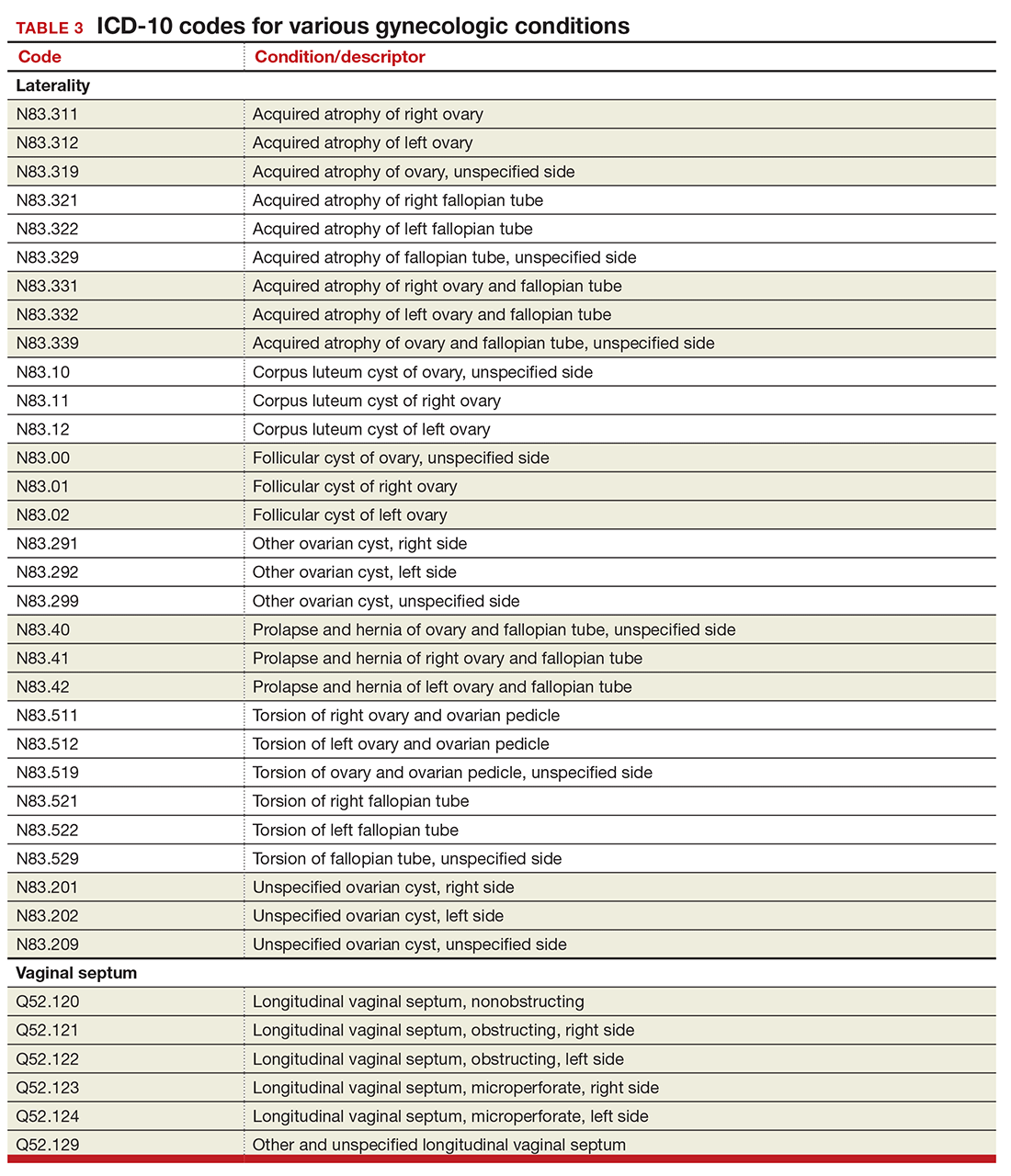
Vaginal septum
The right and left designations extend to the congenital codes for vaginal septum, but they go one step further. The American Congress of Obstetricians and Gynecologists (ACOG) requested that the codes for longitudinal vaginal septum be expanded to differentiate a nonobstructing vaginal septum from an obstructing vaginal septum, in addition to adding laterality to these codes (TABLE 3).2
Mastitis
There are now 2 new codes for inflammation of the breast; one describes mastitis without abscess, while the other code includes an abscess of the breast and nipple (TABLE 4). Once again, documentation will lead to the most specific code to describe the findings.
Childhood and prepubertal concerns
The single code for hypertrophy of the vulva has been expanded to include asymmetric labium majus enlargement. This code was requested by ACOG because this is a known clinical diagnosis and the currently available vulvar codes are inadequate for capturing this condition. The vulvar enlargement appears to be in response to hormonal surges during prepuberty and early puberty. Adult hypertrophy, either congenital or acquired from childbirth or as a late result of an old injury, would be reported by the “other specified” code (TABLE 5).
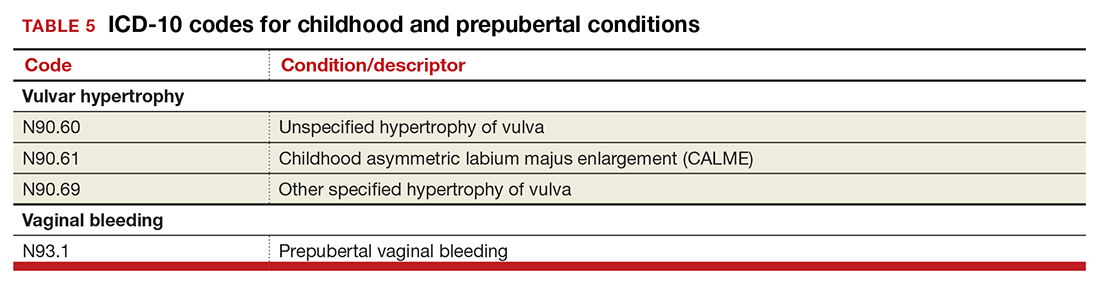
The causes of prepubertal bleeding vary and include the presence of a foreign object, tumors, or fluctuations in hormones, but prepubertal bleeding differs from the bleeding associated with normal menstruation. For that reason, ACOG requested a code that better captures the nature of the condition before a thorough work-up has pinpointed the cause (TABLE 5). Once the cause of the bleeding is known, a more specific diagnosis would then be reported (eg, D28.1, Benign neoplasm of vagina, or T19.2XXA, Foreign body in vulva and vagina, initial encounter).
Dypareunia
Additional documentation for dyspareunia will now be required to ensure that the most specific code is reported. In this case, the clinician should identify whether the pain is superficial or deep to better report on female pelvic floor dysfunction and to support the different treatments based on the location of the pain (TABLE 6). Deep dyspareunia would be felt in the mid or upper vagina.
Postoperative hemorrhage and hematoma
The codes for postprocedural hemorrhage and hematomas have received a face-lift: the single codes for these 2 complications will be split so that each can be reported separately (TABLE 7). Note that the new codes require that the condition be found following the initial surgery, and the code selected depends on whether the surgery involved the genitourinary system or another system.
Hormone malignancy status
The new Z19 codes will augment information known about a patient’s neoplasm (TABLE 8). The ICD-10 rule states that the type and location of the neoplasm are always coded first, followed by one of the new Z19 codes, if known.
Viral hepatitis carrier
The more specific code for type of viral hepatitis the patient is a carrier of has been bundled into a single code for viral hepatitis (TABLE 9). Carrier status in ICD-10 is defined as a person who harbors the specific organisms of a disease, does not currently have any symptoms, but is capable of transmitting the infection.
Contraception
The good news is that the ICD-9 code for contraceptive subdermal implants has been added to ICD-10 coding. In addition, the codes for contraceptive methods have been expanded to also include vaginal rings and transdermal patches (TABLE 10).
Miscellaneous code changes
Counseling a patient prior to pregnancy just got easier with the addition of a code for gestational carriers. Also, the old ICD-9 code that let a payer know that a procedure was converted from a laparoscopic to an open abdominal procedure is back (TABLE 11).
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
In the August 2016 issue of OBG
Urogynecology diagnostic codes
Urogynecologists will find a large number of changes to codes they can select on October 1, 2016. While some codes improve reporting for conditions or symptoms related to urinary issues, many more concern postoperative complications following surgery for devices and grafts applied to the genitourinary system.
The American Urological Association requested new codes to align with a 2009 joint report on the terminology for female pelvic floor dysfunction.1 These codes, along with others, are listed in TABLE 1.
Urinary procedure complication codes
Not every urogynecologist will have an issue after surgery for incontinence, but if they do, there are tons of new and revised codes to address every possible complication the patient may have (TABLE 2). Each of these codes is reported based on whether the complication is being actively treated (initial encounter: final character is A), is being followed up after treatment (subsequent encounter: final character is D), or is caused by another condition (sequela: final character is S).
Gynecology-related diagnostic codes
Laterality
If there are 2 organs in the genitourinary system, the chances are good that there is now a right and a left designation code in ICD-10. Documentation should be clear, of course, and if the condition exists on both the right and the left side (even if only one side is being treated actively), list both codes, as there is no bilateral designation in the codes (TABLE 3). And while there is a code for “unspecified side,” providers normally do know which side, so use of this code should be avoided, if possible.
Vaginal septum
The right and left designations extend to the congenital codes for vaginal septum, but they go one step further. The American Congress of Obstetricians and Gynecologists (ACOG) requested that the codes for longitudinal vaginal septum be expanded to differentiate a nonobstructing vaginal septum from an obstructing vaginal septum, in addition to adding laterality to these codes (TABLE 3).2
Mastitis
There are now 2 new codes for inflammation of the breast; one describes mastitis without abscess, while the other code includes an abscess of the breast and nipple (TABLE 4). Once again, documentation will lead to the most specific code to describe the findings.
Childhood and prepubertal concerns
The single code for hypertrophy of the vulva has been expanded to include asymmetric labium majus enlargement. This code was requested by ACOG because this is a known clinical diagnosis and the currently available vulvar codes are inadequate for capturing this condition. The vulvar enlargement appears to be in response to hormonal surges during prepuberty and early puberty. Adult hypertrophy, either congenital or acquired from childbirth or as a late result of an old injury, would be reported by the “other specified” code (TABLE 5).
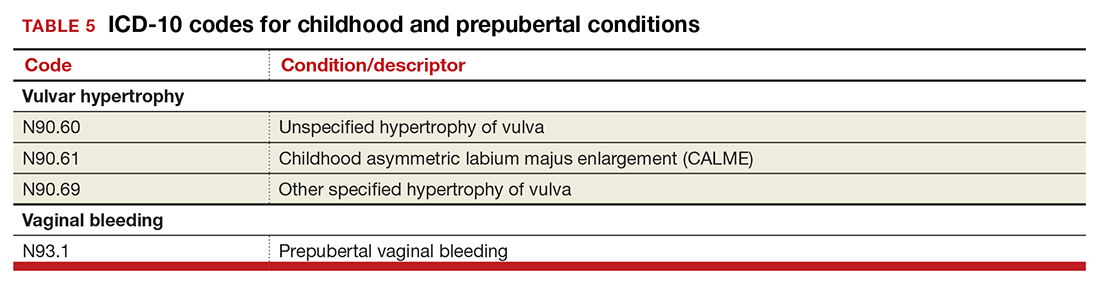
The causes of prepubertal bleeding vary and include the presence of a foreign object, tumors, or fluctuations in hormones, but prepubertal bleeding differs from the bleeding associated with normal menstruation. For that reason, ACOG requested a code that better captures the nature of the condition before a thorough work-up has pinpointed the cause (TABLE 5). Once the cause of the bleeding is known, a more specific diagnosis would then be reported (eg, D28.1, Benign neoplasm of vagina, or T19.2XXA, Foreign body in vulva and vagina, initial encounter).
Dypareunia
Additional documentation for dyspareunia will now be required to ensure that the most specific code is reported. In this case, the clinician should identify whether the pain is superficial or deep to better report on female pelvic floor dysfunction and to support the different treatments based on the location of the pain (TABLE 6). Deep dyspareunia would be felt in the mid or upper vagina.
Postoperative hemorrhage and hematoma
The codes for postprocedural hemorrhage and hematomas have received a face-lift: the single codes for these 2 complications will be split so that each can be reported separately (TABLE 7). Note that the new codes require that the condition be found following the initial surgery, and the code selected depends on whether the surgery involved the genitourinary system or another system.
Hormone malignancy status
The new Z19 codes will augment information known about a patient’s neoplasm (TABLE 8). The ICD-10 rule states that the type and location of the neoplasm are always coded first, followed by one of the new Z19 codes, if known.
Viral hepatitis carrier
The more specific code for type of viral hepatitis the patient is a carrier of has been bundled into a single code for viral hepatitis (TABLE 9). Carrier status in ICD-10 is defined as a person who harbors the specific organisms of a disease, does not currently have any symptoms, but is capable of transmitting the infection.
Contraception
The good news is that the ICD-9 code for contraceptive subdermal implants has been added to ICD-10 coding. In addition, the codes for contraceptive methods have been expanded to also include vaginal rings and transdermal patches (TABLE 10).
Miscellaneous code changes
Counseling a patient prior to pregnancy just got easier with the addition of a code for gestational carriers. Also, the old ICD-9 code that let a payer know that a procedure was converted from a laparoscopic to an open abdominal procedure is back (TABLE 11).
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee Meeting: diagnosis agenda. September 23–24, 2014;28–29. https://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed August 30, 2016.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee Meeting: diagnosis agenda. March 18–19, 2015. http://www.cdc.gov/nchs/data/icd/Tentative_Agenda_March%202015_Final.pdf. Accessed August 30, 2016.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee Meeting: diagnosis agenda. September 23–24, 2014;28–29. https://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed August 30, 2016.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee Meeting: diagnosis agenda. March 18–19, 2015. http://www.cdc.gov/nchs/data/icd/Tentative_Agenda_March%202015_Final.pdf. Accessed August 30, 2016.
In this Article
- Urogynecology dx codes
- Gynecology dx codes
- Codes for hormonal contraceptives