User login
Stem-cell treatment for cardiac disease recently launched into advanced clinical trials, as a flurry of early-phase studies over the last year collectively confirmed the treatment as safe but left its efficacy unresolved.
At least two phase III trials are now underway and others are possibly imminent. But until these pivotal studies begin to yield outcome results in about 4 years, stem-cell treatment remains a question mark – an appealing idea fueled by hints of effectiveness but also dogged by failures that prompt skepticism about its future.
The gush of recent early-phase studies also hint at possible explanations for the variability in the success of stem cell treatment. The studies examined a broad range of cell types and patients. (Click here to see a chart of the studies.) The results imply that select types of bone marrow cells may be more effective as therapy and that the number and potency of stem cells decrease with age.
Clinical testing of stem cells for heart disease has hit its stride more than a decade after the first-in-human report in 2001 of a patient treated following an acute myocardial infarction (Dtsch. Med. Wochenschr. 2001;126:932-8), which was followed by the first randomized clinical trial, also in myocardial infarction patients, reported in 2004 (Lancet 2004;364:141-8).
"So far, stem-cell treatment has been safe in all the areas where it’s been used. I’m very satisfied" with the progress, said Dr. Emerson C. Perin, an interventional cardiologist and medical director of the Stem Cell Center at the Texas Heart Institute and one of the U.S. researchers who has worked longest on stem-cell clinical studies. Those working on clinical investigations of stem cells "haven’t done anything stupid to kill it, and we’ve gone from a crawl to a walk," he said in an interview.
Development of stem cell therapies "has been on a normal track; each step takes time. It’s very similar to what happened with fibrinolytic therapy for treating acute myocardial infarctions" in the 1980s and 1990s, said Dr. Timothy D. Henry, an interventional cardiologist, director of research at the Minneapolis Heart Institute Foundation, and another very active stem cell researcher. "It was a good 10 years before we got lytics up and going. People want [stem cells] to be a magic bullet. I think some people have put unrealistic expectations on stem cells, but it’s like any other treatment. You need to do a trial and find out the relative risks and benefits, and that takes time," he said in an interview.
A different take on the past decade of stem-cell work came from another researcher in the field, Dr. Eduardo Marbán. "The pace of progress has been disappointingly slow, marked by numerous examples of clinical studies prematurely undertaken without benefit of adequate preclinical data. We are lucky that no one has been killed," said Dr. Marbán, professor and director of the Cedars-Sinai Heart Institute in Los Angeles. But despite whatever role luck may have played, Dr. Marbán agreed on the bottom line: "The major accomplishment of the 11-year experience has been the convincing demonstration that most forms of cell therapy are safe, if administered via the intracoronary route." Then he added the elephant in the room: "Efficacy is another matter.
record. Why subject patients to risk in receiving a cell product that has not been extensively validated in vitro and in small and large animals? Yet this has been done over and over again" by investigators running clinical trials of stem cells and other cells for heart disease, Dr. Marbán said in an interview.
Making It to Phase III: REPAIR-AMI/BAMI
The recent surge of study results, and the path to phase III may be best exemplified by the landmark phase II trial done by German investigators, the Reinfusion of Enriched Progenitor Cells and Infarct Remodeling in Acute Myocardial Infarction (REPAIR-AMI) trial (N. Engl. J. Med. 2006;355:1210-21). The multicenter German study randomized 204 patients an average of 4 days following an acute myocardial infarction (MI) to receive either an intracoronary infusion of autologous bone marrow cells processed to enrich for progenitor cells, or placebo.
Last November, at the annual Scientific Sessions of the American Heart Association, the group presented 5-year follow-up results for 200 of the 204 patients. Helped by the lengthy follow-up, the researchers found that the stem-cell treatment cut the cumulative rate of death, recurrent MI, or need for revascularization from 64% in the control arm to 42%, a statistically significant difference in a prespecified end point of the study.
This striking change in a very meaningful clinical outcome contrasted with the modest change in a surrogate end point at 4 months (first reported in the 2006 article), and led to the launch of the largest phase III study of stem cells for heart disease, the Effect of Intracoronary Reinfusion of Bone Marrow Derived Mononuclear Cells (BM-MNC) on All-Cause Mortality in Acute Myocardial Infarction (BAMI), a 3,000-patient, multi-center study funded by the European Union. The study will enroll patients within 3-6 days after reperfusion therapy of an acute MI if they have a left ventricular ejection fraction of 45% or less. The primary end point is a reduction in all-cause mortality, a design that will allow BAMI to use standard care as its control instead of a sham infusion.
"We discussed the end point with the EMA [European Medicines Agency], and they said that if you use only death as the end point we can do it with a state-of-the-art control. I think that is the proper way, because some people believe that intracoronary instrumentation by itself carries a risk that could also affect placebo groups," said Dr. Andreas M. Zeiher, professor and chairman of medicine at Goethe University in Frankfurt, Germany, speaking last November at the American Heart Association meeting.
Dr. Zeiher, who led the team that ran REPAIR-AMI and spearheaded organization of the BAMI trial, also stressed the need to avoid heparin when handling and administering autologous bone marrow cells to achieve optimal results. "Heparin interferes with a process that is absolutely crucial for these cells to extravasate during infusion to enter ischemic tissue," he said during a talk in March at the American College of Cardiology Scientific Session in Chicago. "Heparin in the syringe more or less completely abolishes the migratory capacity of the [bone-marrow] cells." Dr. Zeiher reviewed the methods and results of more than 20 stem-cell studies and found those that used heparin-treated bone-marrow cells had little clinical effect, when studies that avoided heparin or neutralized the drug with serum the cell treatments proved effective. REPAIR-AMI used serum to neutralize heparin, and BAMI will use bivalirudin as an anticoagulant and no heparin, he said.
In contrast to the success in REPAIR-AMI, no efficacy signal occurred in a Norwegian study of bone-marrow mononuclear cells injected into the hearts of 47 acute MI patients in the Autologous Stem-Cell Transplantation in Acute Myocardial Infarction (ASTAMI) study, which coincidently appeared in the same issue of The New England Journal of Medicine as the REPAIR-AMI report (N. Engl. J. Med. 2006;355:1199-209). The lack of success in ASTAMI juxtaposed against the efficacy signal in REPAIR-AMI (a signal later confirmed and strengthened by longer follow-up) provides an example in microcosm of the uneven road that stem cell therapy traversed over the past 11 years. Also worth noting: in ASTAMI the investigators used heparin.
"Heparin interferes with a process that is absolutely crucial for these cells to extravasate during infusion to enter ischemic tissuu," Dr. Andreas M. Zeiher said.
Dr. Zeiher’s heparin explanation for outcome differences among many stem-cell studies is "an interesting hypothesis," said Dr. Robert D. Simari, a cardiologist and professor of medicine at the Mayo Clinic in Rochester, Minn. There are likely several important differences" between the stem-cell trials that have been positive and those that have failed. Trials have differed in their design, patient populations, their stem cell products, and in the end points they have used to measure success, said Dr. Simari, who also chairs the steering committee of the Cardiovascular Cell Therapy Research Network (CCTRN), a research group of seven U.S. centers organized by the National Heart Lung and Blood Institute to run early-phase clinical trials with cell treatments.
Also in the Phase III Act: ACT34-CMI/RENEW
Another cell therapy success story now advancing to a phase III trial is led by Dr. Douglas W. Losordo using autologous CD34+ cells injected into the myocardium of patients with refractory angina. He and his associates published results last August from a phase II study with167 patients, the Double-blind, Prospective, Randomized, Placebo-controlled Study to Determine the Tolerability, Efficacy, Safety, and Dose Range of Intramyocardial Injections of G-CSF Mobilized Auto–CD34+ Cells for Reduction of Angina Episodes in Patients With Refractory Chronic Myocardial Ischemia (ACT34-CMI).
The researchers obtained the autologous cell preparation used in ACT34-CMI by first treating each patient with granulocyte colony stimulating factor daily for 4 or 5 days to mobilize their CD34+ cells. The day following the last dose of drug, each patient underwent leukopheresis to collect mononuclear cells. The cell material then underwent further ex vivo enrichment for CD34+ cells using a commercially-available magnetic cell selection device marketed by Baxter Healthcare. Patients received 100,000 CD34+ cells/kg, 500,000 CD34+ cells/kg, or placebo as intramyocardial injections at 10 sites identified by electromechanical endocardial mapping. Dr. Losordo and his associates said they used CD34+ cells because of evidence these cells, called endothelial progenitor cells, can stimulate neovascularization in ischemic tissue, and improved function in animal models of acute and chronic myocardial ischemia. The patients enrolled in ACT34-CMI all had Canadian Cardiovascular Society class III or IV chronic refractory angina despite optimal medial treatment.
The study, done at 26 U.S. centers, found that at 6 and 12 months after treatment, 54 patients who received the low-dose injections had significantly fewer angina episodes per week than the 53 patients who received placebo infections, the study’s primary end point. Patients who received the higher-dose injections also had fewer angina episodes than the controls, but the difference was not statistically significant at either 6- or 12-month follow-up. The low-dose patients also had statistically significant improvement in their total exercise time in an exercise tolerance test compared with the placebo patients; the high-dose patients also had better exercise times, but not significantly better than the controls.
Speaking at the American College of Cardiology meeting in Chicago in March, Dr. Losordo presented 2-year follow-up data on the patients in ACT34-CMI. At 2 years, the low-dose patients continued to have a significantly lower rate of weekly angina counts than control patients, while the high-dose patients continued to have a numerically lower rate that was not significantly different from the controls. The cumulative, 2-year rate of death, MI, or hospitalization for acute coronary syndrome was 30% in the control patients, 18% in the low-dose patients, and 14% in the high-dose patients. Although these between group differences were not statistically significant, the trends were "in the right direction," said Dr. Losordo, an interventional cardiologist at Northwestern University in Chicago, and vice president for new therapeutic development at Baxter International. Baxter sponsored ACT34-CMI, as well as the phase III study now starting based on the phase II results.
The phase III study, A Prospective, Randomized, Double-blinded, Active-control and Unblinded Standard of Care (SOC) Controlled Study to Determine the Efficacy and Safety of Targeted Intramyocardial Delivery of Autologous CD34+ Cells (Auto-CD34+ Cells) for Increasing Exercise Capacity During Standardized Exercise Testing in Subjects With Refractory Angina Pectoris and Chronic Myocardial Ischemia (RENEW), will enroll about 450 refractory angina patients at 50 U.S. sites, randomizing them to CD34+ treatment, placebo treatment, or no treatment and optimal standard care. The primary efficacy outcome will be change in total exercise time on an exercise tolerance test after 12 months.
Choosing the Right Cells
The success of the ACT34-CMI study, and the decision by Dr. Losordo and Baxter to move on to the phase III RENEW trial, highlights what may be a possible advantage to using selected stem and progenitor cells compared with the strategy of using an unselected cell population, such as the bone-marrow cells used in many of the studies of the past 11 years.
More evidence favoring cell selection came recently in results reported by Dr. Perin from the First Mononuclear Cells Injected in the United States Conducted by the Cardiovascular Cell Therapy Research Network (FOCUS-CCTRN) study, which he presented in March at the American College of Cardiology meeting in Chicago. The phase II study enrolled 92 patients with chronic heart failure and a left ventricular ejection fraction of 45% or less. Patients received a transendocardial injection of 100 million autologous bone-marrow cells or placebo. The primary end points were 6-month changes in left ventricular end systolic volume, in maximal oxygen consumption, and the extent of ischemic myocardial defects measured by single photon emission tomography. The results showed no statistically significant improvement for any of these three end points in the patients treated with bone-marrow cells compared with the controls, and were simultaneously reported in an article published online (JAMA 2012; March 24 [doi:10.1001/jama.2012.418]).
Despite the study’s failure for its prespecified end points, it also showed signals of efficacy and possibly highlighted some important lessons on how to best apply stem cell therapy in the future. On the efficacy side, the 61 patients who received bone-marrow cell injections had an average 1.4% improvement in their left ventricular ejection fraction, compared with an average 1.3% decline in the 31 placebo patients, an overall between-group difference of 2.7% that was statistically significant. Further analysis showed that patients who received bone-marrow cell preparations that had higher levels of either CD34+ cell or CD133+ cells had greater increases in their left ventricular ejection fractions. Also, when the researchers analyzed responses in subgroups divided by their age, patients 62 years old or younger (62 years old was the median age in the study) who received bone-marrow cells had a statistically significant, 4.7% improvement in their left ventricular ejection fraction after 6 months compared with placebo patients, while among patients greater than 62 years old treatment with autologous bone-marrow cells produced no significant improvement in ejection fraction compared with the controls.
"It could very well be that [unfractionated] bone marrow is a weaker product than using a specific cell type," said Dr. Perin. "Now we’ll start using parts of bone marrow, specific cells or cell combinations," he predicted, although he added that additional analysis of the FOCUS-CCTRN data must occur before he and his associates decide which cell types show the most promise. "Even though it’s not answered perfectly, the results definitely point us toward" using more selected types of bone marrow cells, he said.
"The most important lesson FOCUS-CCTRN showed was that as patients get older the number and potency of their stem cells decreases. It showed that if you give cells that aren’t potent they won’t work," said Dr. Henry, a co-investigator of the study and an active member of CCTRN. "That’s a really important insight, because if you treat patients with 100 mg of a beta blocker you get a consistent effect, but if you treat patients with autologous stem cells, every patient gets something different."
Development of stem cell therapies "has been on a normal track; each step takes time. It’s very similar to what happened with fibrinolytic therapy for treating acute myocardial infarctions" in the 1980s and 1990s, said Dr. Timothy D. Henry.
"The FOCUS results showed some evidence of an effect, but there are a number of ways to make it better," Dr. Henry said. One approach is to use selected cells, such as CD34+ cells. Another strategy is to deliver allogenic cells obtained initially from young and healthy donors, a way to avoid the issue of older patients and those with co-morbidities who may have compromised stem cells.
Administering selected or allogenic cells has another potential advantage: it opens the door to commercial involvement with a potentially saleable product, a strategy that can attract the interest of a company willing to shoulder the cost of a phase III trial.
"A challenge with [unprocessed] bone marrow is it’s too easy. Bone marrow is inexpensive, and anyone can do it," Dr. Henry noted. That’s one reason why it took several years for the REPAIR-AMI strategy to advance into a phase III trial, eventually moving forward when it received financial backing from the European Union. In contrast, the promising ACT34-CMI strategy quickly jumped to the phase III level, aided by financial support from Baxter.
But others cautioned against drawing too many inferences from FOCUS-CCTRN because it was a negative study and hence all its results must be considered suspect.
"I do not believe that post-hoc analysis of cell potency should be used to guide future trials. FOCUS was negative; the subgroup analyses and cell potency assays were attempts to glean some positivity from that study after the fact," said Dr. Marbán.
More Phase III Studies Coming, with Commercial Support
Another example of a selected, allogenic cell preparation with commercial support is the study of mesenchymal precursor cells (MPC), bone-marrow cells obtained from young, healthy donors and delivered by transendocardial injection to 45 patients with cardiomyopathy, New York Heart Association class II or III heart failure, and impaired left ventricular function in a phase II study presented by Dr. Perin last November at the American Heart Association’s Scientific Sessions in Orlando. The MPC preparation he and his associates tested was an "off-the-shelf" stem-cell product made by the Australian-based company Mesoblast.
The injections were safe, and the three different amounts of cells delivered showed various signs of efficacy. The lowest dose of cells tested showed a statistically significant improvement in left ventricular ejection fraction at 3 months compared with placebo; the highest cell dose tested showed a statistically significant improvement in left ventricular end-systolic volume at 12 months compared with the placebo control; and collectively, all three cell doses tested produced a statistically significant 20% reduction in the rate of major adverse coronary events compared with the placebo patients during a follow-up of up to 3 years, Dr. Perin reported last November.
"Given the very positive results we saw in the phase II trial, it would be logical to move on to a bigger trial," said Dr. Perin in an interview, but he added that he was unable to provide details about possible additional trials with this MPC product.
Another commercially-backed stem-cell product poised for a larger trial is cardiopoietic stem cells, made by a proprietary, patented method that uses a patient’s autologous bone-marrow stem cells and treats them in vitro to produce cells that are then injected into a patient’s myocardium where they produce new heart muscle. Researchers at the Mayo Clinic in Rochester, Minn. developed this process, and Mayo licensed it to a Belgian company, Cardio 3 BioSciences.
The company released results in November 2010 from the C-Cure study done in Belgium, Serbia, and Switzerland that enrolled 45-patients with severe ischemic heart failure. Six months after treatment, the 21 patients who received injections of the stem cells had an average 18% relative increase in their left ventricular ejection fraction compared with baseline, versus a 4% relative increase over baseline among 24 control patients. Speaking in March at the American College of Cardiology meeting, Dr. André Terzic, who led the study, provided a few more details from the results. Average ejection fraction in the actively-treated patients rose from 28% at baseline to 33%. The treatment was especially effective for the patients who entered the study with an ejection fraction below 28%, said Dr. Terzic, a professor of medicine and cardiology, and director of the Center for Regenerative Medicine at the Mayo Clinic. The 6-month results also showed other indications of benefit in the patients treated with the cardiopoietic stem cells, including significantly increased left ventricular end systolic volume, and reduced left ventricular mass index.
Cardio 3 Biosciences is now planning to start a "late phase II" or phase III trial with this material, said Dr. Simari, who is not directly involved in these studies.
What Comes Next?
Despite 11 years of work, "it’s still very early in the field. We’re still trying to figure out the cells and out targets," said Dr. Simari. "This is the haze of early days, of learning from groups of 10, 20, or 80 patients. Only in retrospect, and as we get to larger trials will the truth emerge. Right now, there is a lot of work needed and few headlines, and it will probably stay that way for awhile. This is not a game for people with short attention spans.
"The business model for autologous cells remains uncertain," he added. "For allogenic products that are generated from young, healthy donors and made into thousands of doses, the business model is different and the costs might be more reasonable. Hopefully, as our knowledge grows, we will develop treatments that end up costing less."
"I have no doubt that cell treatment is one of the great avenues of future medicine; it’s just a matter of figuring it out," said Dr. Perin. "Having phase III trials now starting is a step forward. Things are starting to come into focus. Unless something totally unforeseen happens, we will eventually have an approved product," he predicted.
Dr. Perin said that he has been a consultant to Amorcyte, Teva, Cytori, and Aldagen. Dr. Henry said that he has served on steering committees for and received research grants from Aastrom and Mesoblast. Dr. Marbán said that he is a founder of and holds equity in Capricor. Dr. Simari said that he had no disclosures. Dr. Zeiher said he is a cofounder of and scientific advisor to t2cure, a company set up to run the BAMI trial, sponsored by the European Union Dr. Losordo is an employee of Baxter International. Dr. Terzic said that he has received research grants from Cardio 3 BioSciences.
Stem-cell treatment for cardiac disease recently launched into advanced clinical trials, as a flurry of early-phase studies over the last year collectively confirmed the treatment as safe but left its efficacy unresolved.
At least two phase III trials are now underway and others are possibly imminent. But until these pivotal studies begin to yield outcome results in about 4 years, stem-cell treatment remains a question mark – an appealing idea fueled by hints of effectiveness but also dogged by failures that prompt skepticism about its future.
The gush of recent early-phase studies also hint at possible explanations for the variability in the success of stem cell treatment. The studies examined a broad range of cell types and patients. (Click here to see a chart of the studies.) The results imply that select types of bone marrow cells may be more effective as therapy and that the number and potency of stem cells decrease with age.
Clinical testing of stem cells for heart disease has hit its stride more than a decade after the first-in-human report in 2001 of a patient treated following an acute myocardial infarction (Dtsch. Med. Wochenschr. 2001;126:932-8), which was followed by the first randomized clinical trial, also in myocardial infarction patients, reported in 2004 (Lancet 2004;364:141-8).
"So far, stem-cell treatment has been safe in all the areas where it’s been used. I’m very satisfied" with the progress, said Dr. Emerson C. Perin, an interventional cardiologist and medical director of the Stem Cell Center at the Texas Heart Institute and one of the U.S. researchers who has worked longest on stem-cell clinical studies. Those working on clinical investigations of stem cells "haven’t done anything stupid to kill it, and we’ve gone from a crawl to a walk," he said in an interview.
Development of stem cell therapies "has been on a normal track; each step takes time. It’s very similar to what happened with fibrinolytic therapy for treating acute myocardial infarctions" in the 1980s and 1990s, said Dr. Timothy D. Henry, an interventional cardiologist, director of research at the Minneapolis Heart Institute Foundation, and another very active stem cell researcher. "It was a good 10 years before we got lytics up and going. People want [stem cells] to be a magic bullet. I think some people have put unrealistic expectations on stem cells, but it’s like any other treatment. You need to do a trial and find out the relative risks and benefits, and that takes time," he said in an interview.
A different take on the past decade of stem-cell work came from another researcher in the field, Dr. Eduardo Marbán. "The pace of progress has been disappointingly slow, marked by numerous examples of clinical studies prematurely undertaken without benefit of adequate preclinical data. We are lucky that no one has been killed," said Dr. Marbán, professor and director of the Cedars-Sinai Heart Institute in Los Angeles. But despite whatever role luck may have played, Dr. Marbán agreed on the bottom line: "The major accomplishment of the 11-year experience has been the convincing demonstration that most forms of cell therapy are safe, if administered via the intracoronary route." Then he added the elephant in the room: "Efficacy is another matter.
record. Why subject patients to risk in receiving a cell product that has not been extensively validated in vitro and in small and large animals? Yet this has been done over and over again" by investigators running clinical trials of stem cells and other cells for heart disease, Dr. Marbán said in an interview.
Making It to Phase III: REPAIR-AMI/BAMI
The recent surge of study results, and the path to phase III may be best exemplified by the landmark phase II trial done by German investigators, the Reinfusion of Enriched Progenitor Cells and Infarct Remodeling in Acute Myocardial Infarction (REPAIR-AMI) trial (N. Engl. J. Med. 2006;355:1210-21). The multicenter German study randomized 204 patients an average of 4 days following an acute myocardial infarction (MI) to receive either an intracoronary infusion of autologous bone marrow cells processed to enrich for progenitor cells, or placebo.
Last November, at the annual Scientific Sessions of the American Heart Association, the group presented 5-year follow-up results for 200 of the 204 patients. Helped by the lengthy follow-up, the researchers found that the stem-cell treatment cut the cumulative rate of death, recurrent MI, or need for revascularization from 64% in the control arm to 42%, a statistically significant difference in a prespecified end point of the study.
This striking change in a very meaningful clinical outcome contrasted with the modest change in a surrogate end point at 4 months (first reported in the 2006 article), and led to the launch of the largest phase III study of stem cells for heart disease, the Effect of Intracoronary Reinfusion of Bone Marrow Derived Mononuclear Cells (BM-MNC) on All-Cause Mortality in Acute Myocardial Infarction (BAMI), a 3,000-patient, multi-center study funded by the European Union. The study will enroll patients within 3-6 days after reperfusion therapy of an acute MI if they have a left ventricular ejection fraction of 45% or less. The primary end point is a reduction in all-cause mortality, a design that will allow BAMI to use standard care as its control instead of a sham infusion.
"We discussed the end point with the EMA [European Medicines Agency], and they said that if you use only death as the end point we can do it with a state-of-the-art control. I think that is the proper way, because some people believe that intracoronary instrumentation by itself carries a risk that could also affect placebo groups," said Dr. Andreas M. Zeiher, professor and chairman of medicine at Goethe University in Frankfurt, Germany, speaking last November at the American Heart Association meeting.
Dr. Zeiher, who led the team that ran REPAIR-AMI and spearheaded organization of the BAMI trial, also stressed the need to avoid heparin when handling and administering autologous bone marrow cells to achieve optimal results. "Heparin interferes with a process that is absolutely crucial for these cells to extravasate during infusion to enter ischemic tissue," he said during a talk in March at the American College of Cardiology Scientific Session in Chicago. "Heparin in the syringe more or less completely abolishes the migratory capacity of the [bone-marrow] cells." Dr. Zeiher reviewed the methods and results of more than 20 stem-cell studies and found those that used heparin-treated bone-marrow cells had little clinical effect, when studies that avoided heparin or neutralized the drug with serum the cell treatments proved effective. REPAIR-AMI used serum to neutralize heparin, and BAMI will use bivalirudin as an anticoagulant and no heparin, he said.
In contrast to the success in REPAIR-AMI, no efficacy signal occurred in a Norwegian study of bone-marrow mononuclear cells injected into the hearts of 47 acute MI patients in the Autologous Stem-Cell Transplantation in Acute Myocardial Infarction (ASTAMI) study, which coincidently appeared in the same issue of The New England Journal of Medicine as the REPAIR-AMI report (N. Engl. J. Med. 2006;355:1199-209). The lack of success in ASTAMI juxtaposed against the efficacy signal in REPAIR-AMI (a signal later confirmed and strengthened by longer follow-up) provides an example in microcosm of the uneven road that stem cell therapy traversed over the past 11 years. Also worth noting: in ASTAMI the investigators used heparin.
"Heparin interferes with a process that is absolutely crucial for these cells to extravasate during infusion to enter ischemic tissuu," Dr. Andreas M. Zeiher said.
Dr. Zeiher’s heparin explanation for outcome differences among many stem-cell studies is "an interesting hypothesis," said Dr. Robert D. Simari, a cardiologist and professor of medicine at the Mayo Clinic in Rochester, Minn. There are likely several important differences" between the stem-cell trials that have been positive and those that have failed. Trials have differed in their design, patient populations, their stem cell products, and in the end points they have used to measure success, said Dr. Simari, who also chairs the steering committee of the Cardiovascular Cell Therapy Research Network (CCTRN), a research group of seven U.S. centers organized by the National Heart Lung and Blood Institute to run early-phase clinical trials with cell treatments.
Also in the Phase III Act: ACT34-CMI/RENEW
Another cell therapy success story now advancing to a phase III trial is led by Dr. Douglas W. Losordo using autologous CD34+ cells injected into the myocardium of patients with refractory angina. He and his associates published results last August from a phase II study with167 patients, the Double-blind, Prospective, Randomized, Placebo-controlled Study to Determine the Tolerability, Efficacy, Safety, and Dose Range of Intramyocardial Injections of G-CSF Mobilized Auto–CD34+ Cells for Reduction of Angina Episodes in Patients With Refractory Chronic Myocardial Ischemia (ACT34-CMI).
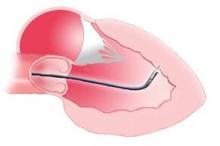
The researchers obtained the autologous cell preparation used in ACT34-CMI by first treating each patient with granulocyte colony stimulating factor daily for 4 or 5 days to mobilize their CD34+ cells. The day following the last dose of drug, each patient underwent leukopheresis to collect mononuclear cells. The cell material then underwent further ex vivo enrichment for CD34+ cells using a commercially-available magnetic cell selection device marketed by Baxter Healthcare. Patients received 100,000 CD34+ cells/kg, 500,000 CD34+ cells/kg, or placebo as intramyocardial injections at 10 sites identified by electromechanical endocardial mapping. Dr. Losordo and his associates said they used CD34+ cells because of evidence these cells, called endothelial progenitor cells, can stimulate neovascularization in ischemic tissue, and improved function in animal models of acute and chronic myocardial ischemia. The patients enrolled in ACT34-CMI all had Canadian Cardiovascular Society class III or IV chronic refractory angina despite optimal medial treatment.
The study, done at 26 U.S. centers, found that at 6 and 12 months after treatment, 54 patients who received the low-dose injections had significantly fewer angina episodes per week than the 53 patients who received placebo infections, the study’s primary end point. Patients who received the higher-dose injections also had fewer angina episodes than the controls, but the difference was not statistically significant at either 6- or 12-month follow-up. The low-dose patients also had statistically significant improvement in their total exercise time in an exercise tolerance test compared with the placebo patients; the high-dose patients also had better exercise times, but not significantly better than the controls.
Speaking at the American College of Cardiology meeting in Chicago in March, Dr. Losordo presented 2-year follow-up data on the patients in ACT34-CMI. At 2 years, the low-dose patients continued to have a significantly lower rate of weekly angina counts than control patients, while the high-dose patients continued to have a numerically lower rate that was not significantly different from the controls. The cumulative, 2-year rate of death, MI, or hospitalization for acute coronary syndrome was 30% in the control patients, 18% in the low-dose patients, and 14% in the high-dose patients. Although these between group differences were not statistically significant, the trends were "in the right direction," said Dr. Losordo, an interventional cardiologist at Northwestern University in Chicago, and vice president for new therapeutic development at Baxter International. Baxter sponsored ACT34-CMI, as well as the phase III study now starting based on the phase II results.
The phase III study, A Prospective, Randomized, Double-blinded, Active-control and Unblinded Standard of Care (SOC) Controlled Study to Determine the Efficacy and Safety of Targeted Intramyocardial Delivery of Autologous CD34+ Cells (Auto-CD34+ Cells) for Increasing Exercise Capacity During Standardized Exercise Testing in Subjects With Refractory Angina Pectoris and Chronic Myocardial Ischemia (RENEW), will enroll about 450 refractory angina patients at 50 U.S. sites, randomizing them to CD34+ treatment, placebo treatment, or no treatment and optimal standard care. The primary efficacy outcome will be change in total exercise time on an exercise tolerance test after 12 months.
Choosing the Right Cells
The success of the ACT34-CMI study, and the decision by Dr. Losordo and Baxter to move on to the phase III RENEW trial, highlights what may be a possible advantage to using selected stem and progenitor cells compared with the strategy of using an unselected cell population, such as the bone-marrow cells used in many of the studies of the past 11 years.
More evidence favoring cell selection came recently in results reported by Dr. Perin from the First Mononuclear Cells Injected in the United States Conducted by the Cardiovascular Cell Therapy Research Network (FOCUS-CCTRN) study, which he presented in March at the American College of Cardiology meeting in Chicago. The phase II study enrolled 92 patients with chronic heart failure and a left ventricular ejection fraction of 45% or less. Patients received a transendocardial injection of 100 million autologous bone-marrow cells or placebo. The primary end points were 6-month changes in left ventricular end systolic volume, in maximal oxygen consumption, and the extent of ischemic myocardial defects measured by single photon emission tomography. The results showed no statistically significant improvement for any of these three end points in the patients treated with bone-marrow cells compared with the controls, and were simultaneously reported in an article published online (JAMA 2012; March 24 [doi:10.1001/jama.2012.418]).
Despite the study’s failure for its prespecified end points, it also showed signals of efficacy and possibly highlighted some important lessons on how to best apply stem cell therapy in the future. On the efficacy side, the 61 patients who received bone-marrow cell injections had an average 1.4% improvement in their left ventricular ejection fraction, compared with an average 1.3% decline in the 31 placebo patients, an overall between-group difference of 2.7% that was statistically significant. Further analysis showed that patients who received bone-marrow cell preparations that had higher levels of either CD34+ cell or CD133+ cells had greater increases in their left ventricular ejection fractions. Also, when the researchers analyzed responses in subgroups divided by their age, patients 62 years old or younger (62 years old was the median age in the study) who received bone-marrow cells had a statistically significant, 4.7% improvement in their left ventricular ejection fraction after 6 months compared with placebo patients, while among patients greater than 62 years old treatment with autologous bone-marrow cells produced no significant improvement in ejection fraction compared with the controls.
"It could very well be that [unfractionated] bone marrow is a weaker product than using a specific cell type," said Dr. Perin. "Now we’ll start using parts of bone marrow, specific cells or cell combinations," he predicted, although he added that additional analysis of the FOCUS-CCTRN data must occur before he and his associates decide which cell types show the most promise. "Even though it’s not answered perfectly, the results definitely point us toward" using more selected types of bone marrow cells, he said.
"The most important lesson FOCUS-CCTRN showed was that as patients get older the number and potency of their stem cells decreases. It showed that if you give cells that aren’t potent they won’t work," said Dr. Henry, a co-investigator of the study and an active member of CCTRN. "That’s a really important insight, because if you treat patients with 100 mg of a beta blocker you get a consistent effect, but if you treat patients with autologous stem cells, every patient gets something different."
Development of stem cell therapies "has been on a normal track; each step takes time. It’s very similar to what happened with fibrinolytic therapy for treating acute myocardial infarctions" in the 1980s and 1990s, said Dr. Timothy D. Henry.
"The FOCUS results showed some evidence of an effect, but there are a number of ways to make it better," Dr. Henry said. One approach is to use selected cells, such as CD34+ cells. Another strategy is to deliver allogenic cells obtained initially from young and healthy donors, a way to avoid the issue of older patients and those with co-morbidities who may have compromised stem cells.
Administering selected or allogenic cells has another potential advantage: it opens the door to commercial involvement with a potentially saleable product, a strategy that can attract the interest of a company willing to shoulder the cost of a phase III trial.
"A challenge with [unprocessed] bone marrow is it’s too easy. Bone marrow is inexpensive, and anyone can do it," Dr. Henry noted. That’s one reason why it took several years for the REPAIR-AMI strategy to advance into a phase III trial, eventually moving forward when it received financial backing from the European Union. In contrast, the promising ACT34-CMI strategy quickly jumped to the phase III level, aided by financial support from Baxter.
But others cautioned against drawing too many inferences from FOCUS-CCTRN because it was a negative study and hence all its results must be considered suspect.
"I do not believe that post-hoc analysis of cell potency should be used to guide future trials. FOCUS was negative; the subgroup analyses and cell potency assays were attempts to glean some positivity from that study after the fact," said Dr. Marbán.
More Phase III Studies Coming, with Commercial Support
Another example of a selected, allogenic cell preparation with commercial support is the study of mesenchymal precursor cells (MPC), bone-marrow cells obtained from young, healthy donors and delivered by transendocardial injection to 45 patients with cardiomyopathy, New York Heart Association class II or III heart failure, and impaired left ventricular function in a phase II study presented by Dr. Perin last November at the American Heart Association’s Scientific Sessions in Orlando. The MPC preparation he and his associates tested was an "off-the-shelf" stem-cell product made by the Australian-based company Mesoblast.
The injections were safe, and the three different amounts of cells delivered showed various signs of efficacy. The lowest dose of cells tested showed a statistically significant improvement in left ventricular ejection fraction at 3 months compared with placebo; the highest cell dose tested showed a statistically significant improvement in left ventricular end-systolic volume at 12 months compared with the placebo control; and collectively, all three cell doses tested produced a statistically significant 20% reduction in the rate of major adverse coronary events compared with the placebo patients during a follow-up of up to 3 years, Dr. Perin reported last November.
"Given the very positive results we saw in the phase II trial, it would be logical to move on to a bigger trial," said Dr. Perin in an interview, but he added that he was unable to provide details about possible additional trials with this MPC product.
Another commercially-backed stem-cell product poised for a larger trial is cardiopoietic stem cells, made by a proprietary, patented method that uses a patient’s autologous bone-marrow stem cells and treats them in vitro to produce cells that are then injected into a patient’s myocardium where they produce new heart muscle. Researchers at the Mayo Clinic in Rochester, Minn. developed this process, and Mayo licensed it to a Belgian company, Cardio 3 BioSciences.
The company released results in November 2010 from the C-Cure study done in Belgium, Serbia, and Switzerland that enrolled 45-patients with severe ischemic heart failure. Six months after treatment, the 21 patients who received injections of the stem cells had an average 18% relative increase in their left ventricular ejection fraction compared with baseline, versus a 4% relative increase over baseline among 24 control patients. Speaking in March at the American College of Cardiology meeting, Dr. André Terzic, who led the study, provided a few more details from the results. Average ejection fraction in the actively-treated patients rose from 28% at baseline to 33%. The treatment was especially effective for the patients who entered the study with an ejection fraction below 28%, said Dr. Terzic, a professor of medicine and cardiology, and director of the Center for Regenerative Medicine at the Mayo Clinic. The 6-month results also showed other indications of benefit in the patients treated with the cardiopoietic stem cells, including significantly increased left ventricular end systolic volume, and reduced left ventricular mass index.
Cardio 3 Biosciences is now planning to start a "late phase II" or phase III trial with this material, said Dr. Simari, who is not directly involved in these studies.
What Comes Next?
Despite 11 years of work, "it’s still very early in the field. We’re still trying to figure out the cells and out targets," said Dr. Simari. "This is the haze of early days, of learning from groups of 10, 20, or 80 patients. Only in retrospect, and as we get to larger trials will the truth emerge. Right now, there is a lot of work needed and few headlines, and it will probably stay that way for awhile. This is not a game for people with short attention spans.
"The business model for autologous cells remains uncertain," he added. "For allogenic products that are generated from young, healthy donors and made into thousands of doses, the business model is different and the costs might be more reasonable. Hopefully, as our knowledge grows, we will develop treatments that end up costing less."
"I have no doubt that cell treatment is one of the great avenues of future medicine; it’s just a matter of figuring it out," said Dr. Perin. "Having phase III trials now starting is a step forward. Things are starting to come into focus. Unless something totally unforeseen happens, we will eventually have an approved product," he predicted.
Dr. Perin said that he has been a consultant to Amorcyte, Teva, Cytori, and Aldagen. Dr. Henry said that he has served on steering committees for and received research grants from Aastrom and Mesoblast. Dr. Marbán said that he is a founder of and holds equity in Capricor. Dr. Simari said that he had no disclosures. Dr. Zeiher said he is a cofounder of and scientific advisor to t2cure, a company set up to run the BAMI trial, sponsored by the European Union Dr. Losordo is an employee of Baxter International. Dr. Terzic said that he has received research grants from Cardio 3 BioSciences.
Stem-cell treatment for cardiac disease recently launched into advanced clinical trials, as a flurry of early-phase studies over the last year collectively confirmed the treatment as safe but left its efficacy unresolved.
At least two phase III trials are now underway and others are possibly imminent. But until these pivotal studies begin to yield outcome results in about 4 years, stem-cell treatment remains a question mark – an appealing idea fueled by hints of effectiveness but also dogged by failures that prompt skepticism about its future.
The gush of recent early-phase studies also hint at possible explanations for the variability in the success of stem cell treatment. The studies examined a broad range of cell types and patients. (Click here to see a chart of the studies.) The results imply that select types of bone marrow cells may be more effective as therapy and that the number and potency of stem cells decrease with age.
Clinical testing of stem cells for heart disease has hit its stride more than a decade after the first-in-human report in 2001 of a patient treated following an acute myocardial infarction (Dtsch. Med. Wochenschr. 2001;126:932-8), which was followed by the first randomized clinical trial, also in myocardial infarction patients, reported in 2004 (Lancet 2004;364:141-8).
"So far, stem-cell treatment has been safe in all the areas where it’s been used. I’m very satisfied" with the progress, said Dr. Emerson C. Perin, an interventional cardiologist and medical director of the Stem Cell Center at the Texas Heart Institute and one of the U.S. researchers who has worked longest on stem-cell clinical studies. Those working on clinical investigations of stem cells "haven’t done anything stupid to kill it, and we’ve gone from a crawl to a walk," he said in an interview.
Development of stem cell therapies "has been on a normal track; each step takes time. It’s very similar to what happened with fibrinolytic therapy for treating acute myocardial infarctions" in the 1980s and 1990s, said Dr. Timothy D. Henry, an interventional cardiologist, director of research at the Minneapolis Heart Institute Foundation, and another very active stem cell researcher. "It was a good 10 years before we got lytics up and going. People want [stem cells] to be a magic bullet. I think some people have put unrealistic expectations on stem cells, but it’s like any other treatment. You need to do a trial and find out the relative risks and benefits, and that takes time," he said in an interview.
A different take on the past decade of stem-cell work came from another researcher in the field, Dr. Eduardo Marbán. "The pace of progress has been disappointingly slow, marked by numerous examples of clinical studies prematurely undertaken without benefit of adequate preclinical data. We are lucky that no one has been killed," said Dr. Marbán, professor and director of the Cedars-Sinai Heart Institute in Los Angeles. But despite whatever role luck may have played, Dr. Marbán agreed on the bottom line: "The major accomplishment of the 11-year experience has been the convincing demonstration that most forms of cell therapy are safe, if administered via the intracoronary route." Then he added the elephant in the room: "Efficacy is another matter.
record. Why subject patients to risk in receiving a cell product that has not been extensively validated in vitro and in small and large animals? Yet this has been done over and over again" by investigators running clinical trials of stem cells and other cells for heart disease, Dr. Marbán said in an interview.
Making It to Phase III: REPAIR-AMI/BAMI
The recent surge of study results, and the path to phase III may be best exemplified by the landmark phase II trial done by German investigators, the Reinfusion of Enriched Progenitor Cells and Infarct Remodeling in Acute Myocardial Infarction (REPAIR-AMI) trial (N. Engl. J. Med. 2006;355:1210-21). The multicenter German study randomized 204 patients an average of 4 days following an acute myocardial infarction (MI) to receive either an intracoronary infusion of autologous bone marrow cells processed to enrich for progenitor cells, or placebo.
Last November, at the annual Scientific Sessions of the American Heart Association, the group presented 5-year follow-up results for 200 of the 204 patients. Helped by the lengthy follow-up, the researchers found that the stem-cell treatment cut the cumulative rate of death, recurrent MI, or need for revascularization from 64% in the control arm to 42%, a statistically significant difference in a prespecified end point of the study.
This striking change in a very meaningful clinical outcome contrasted with the modest change in a surrogate end point at 4 months (first reported in the 2006 article), and led to the launch of the largest phase III study of stem cells for heart disease, the Effect of Intracoronary Reinfusion of Bone Marrow Derived Mononuclear Cells (BM-MNC) on All-Cause Mortality in Acute Myocardial Infarction (BAMI), a 3,000-patient, multi-center study funded by the European Union. The study will enroll patients within 3-6 days after reperfusion therapy of an acute MI if they have a left ventricular ejection fraction of 45% or less. The primary end point is a reduction in all-cause mortality, a design that will allow BAMI to use standard care as its control instead of a sham infusion.
"We discussed the end point with the EMA [European Medicines Agency], and they said that if you use only death as the end point we can do it with a state-of-the-art control. I think that is the proper way, because some people believe that intracoronary instrumentation by itself carries a risk that could also affect placebo groups," said Dr. Andreas M. Zeiher, professor and chairman of medicine at Goethe University in Frankfurt, Germany, speaking last November at the American Heart Association meeting.
Dr. Zeiher, who led the team that ran REPAIR-AMI and spearheaded organization of the BAMI trial, also stressed the need to avoid heparin when handling and administering autologous bone marrow cells to achieve optimal results. "Heparin interferes with a process that is absolutely crucial for these cells to extravasate during infusion to enter ischemic tissue," he said during a talk in March at the American College of Cardiology Scientific Session in Chicago. "Heparin in the syringe more or less completely abolishes the migratory capacity of the [bone-marrow] cells." Dr. Zeiher reviewed the methods and results of more than 20 stem-cell studies and found those that used heparin-treated bone-marrow cells had little clinical effect, when studies that avoided heparin or neutralized the drug with serum the cell treatments proved effective. REPAIR-AMI used serum to neutralize heparin, and BAMI will use bivalirudin as an anticoagulant and no heparin, he said.
In contrast to the success in REPAIR-AMI, no efficacy signal occurred in a Norwegian study of bone-marrow mononuclear cells injected into the hearts of 47 acute MI patients in the Autologous Stem-Cell Transplantation in Acute Myocardial Infarction (ASTAMI) study, which coincidently appeared in the same issue of The New England Journal of Medicine as the REPAIR-AMI report (N. Engl. J. Med. 2006;355:1199-209). The lack of success in ASTAMI juxtaposed against the efficacy signal in REPAIR-AMI (a signal later confirmed and strengthened by longer follow-up) provides an example in microcosm of the uneven road that stem cell therapy traversed over the past 11 years. Also worth noting: in ASTAMI the investigators used heparin.
"Heparin interferes with a process that is absolutely crucial for these cells to extravasate during infusion to enter ischemic tissuu," Dr. Andreas M. Zeiher said.
Dr. Zeiher’s heparin explanation for outcome differences among many stem-cell studies is "an interesting hypothesis," said Dr. Robert D. Simari, a cardiologist and professor of medicine at the Mayo Clinic in Rochester, Minn. There are likely several important differences" between the stem-cell trials that have been positive and those that have failed. Trials have differed in their design, patient populations, their stem cell products, and in the end points they have used to measure success, said Dr. Simari, who also chairs the steering committee of the Cardiovascular Cell Therapy Research Network (CCTRN), a research group of seven U.S. centers organized by the National Heart Lung and Blood Institute to run early-phase clinical trials with cell treatments.
Also in the Phase III Act: ACT34-CMI/RENEW
Another cell therapy success story now advancing to a phase III trial is led by Dr. Douglas W. Losordo using autologous CD34+ cells injected into the myocardium of patients with refractory angina. He and his associates published results last August from a phase II study with167 patients, the Double-blind, Prospective, Randomized, Placebo-controlled Study to Determine the Tolerability, Efficacy, Safety, and Dose Range of Intramyocardial Injections of G-CSF Mobilized Auto–CD34+ Cells for Reduction of Angina Episodes in Patients With Refractory Chronic Myocardial Ischemia (ACT34-CMI).
The researchers obtained the autologous cell preparation used in ACT34-CMI by first treating each patient with granulocyte colony stimulating factor daily for 4 or 5 days to mobilize their CD34+ cells. The day following the last dose of drug, each patient underwent leukopheresis to collect mononuclear cells. The cell material then underwent further ex vivo enrichment for CD34+ cells using a commercially-available magnetic cell selection device marketed by Baxter Healthcare. Patients received 100,000 CD34+ cells/kg, 500,000 CD34+ cells/kg, or placebo as intramyocardial injections at 10 sites identified by electromechanical endocardial mapping. Dr. Losordo and his associates said they used CD34+ cells because of evidence these cells, called endothelial progenitor cells, can stimulate neovascularization in ischemic tissue, and improved function in animal models of acute and chronic myocardial ischemia. The patients enrolled in ACT34-CMI all had Canadian Cardiovascular Society class III or IV chronic refractory angina despite optimal medial treatment.
The study, done at 26 U.S. centers, found that at 6 and 12 months after treatment, 54 patients who received the low-dose injections had significantly fewer angina episodes per week than the 53 patients who received placebo infections, the study’s primary end point. Patients who received the higher-dose injections also had fewer angina episodes than the controls, but the difference was not statistically significant at either 6- or 12-month follow-up. The low-dose patients also had statistically significant improvement in their total exercise time in an exercise tolerance test compared with the placebo patients; the high-dose patients also had better exercise times, but not significantly better than the controls.
Speaking at the American College of Cardiology meeting in Chicago in March, Dr. Losordo presented 2-year follow-up data on the patients in ACT34-CMI. At 2 years, the low-dose patients continued to have a significantly lower rate of weekly angina counts than control patients, while the high-dose patients continued to have a numerically lower rate that was not significantly different from the controls. The cumulative, 2-year rate of death, MI, or hospitalization for acute coronary syndrome was 30% in the control patients, 18% in the low-dose patients, and 14% in the high-dose patients. Although these between group differences were not statistically significant, the trends were "in the right direction," said Dr. Losordo, an interventional cardiologist at Northwestern University in Chicago, and vice president for new therapeutic development at Baxter International. Baxter sponsored ACT34-CMI, as well as the phase III study now starting based on the phase II results.
The phase III study, A Prospective, Randomized, Double-blinded, Active-control and Unblinded Standard of Care (SOC) Controlled Study to Determine the Efficacy and Safety of Targeted Intramyocardial Delivery of Autologous CD34+ Cells (Auto-CD34+ Cells) for Increasing Exercise Capacity During Standardized Exercise Testing in Subjects With Refractory Angina Pectoris and Chronic Myocardial Ischemia (RENEW), will enroll about 450 refractory angina patients at 50 U.S. sites, randomizing them to CD34+ treatment, placebo treatment, or no treatment and optimal standard care. The primary efficacy outcome will be change in total exercise time on an exercise tolerance test after 12 months.
Choosing the Right Cells
The success of the ACT34-CMI study, and the decision by Dr. Losordo and Baxter to move on to the phase III RENEW trial, highlights what may be a possible advantage to using selected stem and progenitor cells compared with the strategy of using an unselected cell population, such as the bone-marrow cells used in many of the studies of the past 11 years.
More evidence favoring cell selection came recently in results reported by Dr. Perin from the First Mononuclear Cells Injected in the United States Conducted by the Cardiovascular Cell Therapy Research Network (FOCUS-CCTRN) study, which he presented in March at the American College of Cardiology meeting in Chicago. The phase II study enrolled 92 patients with chronic heart failure and a left ventricular ejection fraction of 45% or less. Patients received a transendocardial injection of 100 million autologous bone-marrow cells or placebo. The primary end points were 6-month changes in left ventricular end systolic volume, in maximal oxygen consumption, and the extent of ischemic myocardial defects measured by single photon emission tomography. The results showed no statistically significant improvement for any of these three end points in the patients treated with bone-marrow cells compared with the controls, and were simultaneously reported in an article published online (JAMA 2012; March 24 [doi:10.1001/jama.2012.418]).
Despite the study’s failure for its prespecified end points, it also showed signals of efficacy and possibly highlighted some important lessons on how to best apply stem cell therapy in the future. On the efficacy side, the 61 patients who received bone-marrow cell injections had an average 1.4% improvement in their left ventricular ejection fraction, compared with an average 1.3% decline in the 31 placebo patients, an overall between-group difference of 2.7% that was statistically significant. Further analysis showed that patients who received bone-marrow cell preparations that had higher levels of either CD34+ cell or CD133+ cells had greater increases in their left ventricular ejection fractions. Also, when the researchers analyzed responses in subgroups divided by their age, patients 62 years old or younger (62 years old was the median age in the study) who received bone-marrow cells had a statistically significant, 4.7% improvement in their left ventricular ejection fraction after 6 months compared with placebo patients, while among patients greater than 62 years old treatment with autologous bone-marrow cells produced no significant improvement in ejection fraction compared with the controls.
"It could very well be that [unfractionated] bone marrow is a weaker product than using a specific cell type," said Dr. Perin. "Now we’ll start using parts of bone marrow, specific cells or cell combinations," he predicted, although he added that additional analysis of the FOCUS-CCTRN data must occur before he and his associates decide which cell types show the most promise. "Even though it’s not answered perfectly, the results definitely point us toward" using more selected types of bone marrow cells, he said.
"The most important lesson FOCUS-CCTRN showed was that as patients get older the number and potency of their stem cells decreases. It showed that if you give cells that aren’t potent they won’t work," said Dr. Henry, a co-investigator of the study and an active member of CCTRN. "That’s a really important insight, because if you treat patients with 100 mg of a beta blocker you get a consistent effect, but if you treat patients with autologous stem cells, every patient gets something different."
Development of stem cell therapies "has been on a normal track; each step takes time. It’s very similar to what happened with fibrinolytic therapy for treating acute myocardial infarctions" in the 1980s and 1990s, said Dr. Timothy D. Henry.
"The FOCUS results showed some evidence of an effect, but there are a number of ways to make it better," Dr. Henry said. One approach is to use selected cells, such as CD34+ cells. Another strategy is to deliver allogenic cells obtained initially from young and healthy donors, a way to avoid the issue of older patients and those with co-morbidities who may have compromised stem cells.
Administering selected or allogenic cells has another potential advantage: it opens the door to commercial involvement with a potentially saleable product, a strategy that can attract the interest of a company willing to shoulder the cost of a phase III trial.
"A challenge with [unprocessed] bone marrow is it’s too easy. Bone marrow is inexpensive, and anyone can do it," Dr. Henry noted. That’s one reason why it took several years for the REPAIR-AMI strategy to advance into a phase III trial, eventually moving forward when it received financial backing from the European Union. In contrast, the promising ACT34-CMI strategy quickly jumped to the phase III level, aided by financial support from Baxter.
But others cautioned against drawing too many inferences from FOCUS-CCTRN because it was a negative study and hence all its results must be considered suspect.
"I do not believe that post-hoc analysis of cell potency should be used to guide future trials. FOCUS was negative; the subgroup analyses and cell potency assays were attempts to glean some positivity from that study after the fact," said Dr. Marbán.
More Phase III Studies Coming, with Commercial Support
Another example of a selected, allogenic cell preparation with commercial support is the study of mesenchymal precursor cells (MPC), bone-marrow cells obtained from young, healthy donors and delivered by transendocardial injection to 45 patients with cardiomyopathy, New York Heart Association class II or III heart failure, and impaired left ventricular function in a phase II study presented by Dr. Perin last November at the American Heart Association’s Scientific Sessions in Orlando. The MPC preparation he and his associates tested was an "off-the-shelf" stem-cell product made by the Australian-based company Mesoblast.
The injections were safe, and the three different amounts of cells delivered showed various signs of efficacy. The lowest dose of cells tested showed a statistically significant improvement in left ventricular ejection fraction at 3 months compared with placebo; the highest cell dose tested showed a statistically significant improvement in left ventricular end-systolic volume at 12 months compared with the placebo control; and collectively, all three cell doses tested produced a statistically significant 20% reduction in the rate of major adverse coronary events compared with the placebo patients during a follow-up of up to 3 years, Dr. Perin reported last November.
"Given the very positive results we saw in the phase II trial, it would be logical to move on to a bigger trial," said Dr. Perin in an interview, but he added that he was unable to provide details about possible additional trials with this MPC product.
Another commercially-backed stem-cell product poised for a larger trial is cardiopoietic stem cells, made by a proprietary, patented method that uses a patient’s autologous bone-marrow stem cells and treats them in vitro to produce cells that are then injected into a patient’s myocardium where they produce new heart muscle. Researchers at the Mayo Clinic in Rochester, Minn. developed this process, and Mayo licensed it to a Belgian company, Cardio 3 BioSciences.
The company released results in November 2010 from the C-Cure study done in Belgium, Serbia, and Switzerland that enrolled 45-patients with severe ischemic heart failure. Six months after treatment, the 21 patients who received injections of the stem cells had an average 18% relative increase in their left ventricular ejection fraction compared with baseline, versus a 4% relative increase over baseline among 24 control patients. Speaking in March at the American College of Cardiology meeting, Dr. André Terzic, who led the study, provided a few more details from the results. Average ejection fraction in the actively-treated patients rose from 28% at baseline to 33%. The treatment was especially effective for the patients who entered the study with an ejection fraction below 28%, said Dr. Terzic, a professor of medicine and cardiology, and director of the Center for Regenerative Medicine at the Mayo Clinic. The 6-month results also showed other indications of benefit in the patients treated with the cardiopoietic stem cells, including significantly increased left ventricular end systolic volume, and reduced left ventricular mass index.
Cardio 3 Biosciences is now planning to start a "late phase II" or phase III trial with this material, said Dr. Simari, who is not directly involved in these studies.
What Comes Next?
Despite 11 years of work, "it’s still very early in the field. We’re still trying to figure out the cells and out targets," said Dr. Simari. "This is the haze of early days, of learning from groups of 10, 20, or 80 patients. Only in retrospect, and as we get to larger trials will the truth emerge. Right now, there is a lot of work needed and few headlines, and it will probably stay that way for awhile. This is not a game for people with short attention spans.
"The business model for autologous cells remains uncertain," he added. "For allogenic products that are generated from young, healthy donors and made into thousands of doses, the business model is different and the costs might be more reasonable. Hopefully, as our knowledge grows, we will develop treatments that end up costing less."
"I have no doubt that cell treatment is one of the great avenues of future medicine; it’s just a matter of figuring it out," said Dr. Perin. "Having phase III trials now starting is a step forward. Things are starting to come into focus. Unless something totally unforeseen happens, we will eventually have an approved product," he predicted.
Dr. Perin said that he has been a consultant to Amorcyte, Teva, Cytori, and Aldagen. Dr. Henry said that he has served on steering committees for and received research grants from Aastrom and Mesoblast. Dr. Marbán said that he is a founder of and holds equity in Capricor. Dr. Simari said that he had no disclosures. Dr. Zeiher said he is a cofounder of and scientific advisor to t2cure, a company set up to run the BAMI trial, sponsored by the European Union Dr. Losordo is an employee of Baxter International. Dr. Terzic said that he has received research grants from Cardio 3 BioSciences.