User login
The year 2006 was a busy one for those of us engaged in cervical cancer prevention. The most notable development was approval by the US Food and Drug Administration of the human papillomavirus (HPV) quadrivalent vaccine in June, followed closely by guidelines for its use from the Advisory Committee on Immunization Practices (June) and the American College of Obstetricians and Gynecologists (September). Key issues related to the introduction of the HPV vaccine into clinical practice were reviewed in a roundtable discussion in the January 2007 issue of OBG Management.
Therefore, this update will depart, for the moment, from matters related to the vaccine and concentrate on several other critical areas:
- Testing for high-risk HPV types is useful. Large European cervical cancer screening trials confirm a benefit.
- Condoms and oral contraceptives—are they risk modifiers for HPV infection? Answers (“Yes” and “No,” respectively) come from new data.
- Loop electrosurgical excision carries obstetric risks. In fact, all types of excisional procedures produce similar pregnancy-related morbidity.
- Liquid-based cytology may not be superior to conventional cytology. So suggest new studies and a systematic review of the literature.
HPV testing outperforms cytology for screening
Cuzick J, Clavel C, Petry KU, et al. Overview of the European and North American studies on HPV testing in primary cervical cancer screening. Int J Cancer. 2006;119:1095–1101.
Ronco G, Segnan N, Giorgi-Rossi P, et al. Human papillomavirus testing and liquid-based cytology: results at recruitment from the new technologies for cervical cancer randomized controlled trial. J Natl Cancer Inst. 2006;98:765–774.
HPV DNA testing is more sensitive than cervical cytology, reduces specificity to only a moderate degree, and performs similarly in different parts of Europe and North America. Those are the findings of a review by Cuzick and colleagues of all recent large European and North American cervical cancer screening studies. To date, 4 large European trials and 1 from Mexico have directly compared HPV testing and cytology in women aged 30 years and older. Combined, these trials have enrolled over 60,000 women. In every study, testing for high-risk types of HPV using the commercially available Hybrid Capture 2 HPV DNA assay had a much higher sensitivity for identifying women with cervical intraepithelial neoplasia (CIN) 2,3 or cancer (86–97%) than did cervical cytology (34–74%). Moreover, the combination of cytology and HPV testing had a sensitivity ranging from 94% to 100% in the different studies. The average sensitivity of 98% for the combination of cytology and HPV testing means that there is a less than 1 in 1,000 chance of missing CIN 2,3 or cancer when women are screened with both tests (TABLE 1).
Specificity is reasonable, too
If you worry that using HPV DNA testing in women aged 30 and older will flag too many as high-risk HPV-positive and cause them unnecessary colposcopic examinations or anxiety, here is a comforting finding: The specificity of HPV DNA testing is not as low as many had feared—provided we limit screening to women aged 30 and older. In the 5 trials mentioned, the specificity of HPV DNA testing ranged from 92% to 97%. Even when HPV DNA testing and cytology were used together, the average specificity of the 2 tests combined was 93%. A specificity of 93% means that only 7 of 100 screened women who don’t have CIN 2,3 or cancer will be classified as “positive.”
To put this number into perspective, a 2003 survey of US cytology laboratories found a median rate of abnormal results of 6.9%.1 Therefore, in routine clinical practice, incorporation of HPV DNA testing into screening for women aged 30 and older is not expected to greatly increase the number of women requiring additional follow-up.
The single most important component of management is appropriate counseling. Even though there are fewer of these women than we anticipated, these patients need to be reassured that their risk of having a significant lesion (CIN 2,3 or cancer) is quite low—only about 1 in 20. They also need to know that about two thirds of women—even women aged 30 and older—are HPV-negative when they are retested in 12 months.
In addition, clinicians need to stress that positive HPV status is a risk factor for having or developing cervical disease, not an indication that disease is present. One analogy that patients readily understand is the relationship between other types of health risk factors, such as mild hypertension or mildly elevated serum cholesterol, and disease. These explanations help the patient understand why, in settings where genotyping for HPV 16 and 18 is not available, the best course of action is to wait 12 months and be retested.2
Which test should be used first?
Basic screening principles suggest that, whenever 2 tests are used in combination, the most sensitive test should be used first, with patients who test positive tested again using the second, more specific, test. These principles suggest we should be using HPV testing alone as the initial screening test and limiting the use of cytology to triage HPV-positive women. This sequence of testing could potentially be done in a “reflex” fashion.
The large Italian screening trial by Ronco and colleagues randomized 33,364 women aged 35 to 60 years to 2 different screening strategies: routine conventional cytology or liquid-based cytology with HPV testing.3 In the routine cytology arm, researchers identified only 51 cases of CIN 2,3 or cancer, but in the experimental arm, they identified 75 cases. A breakdown of the initial screening results in the women found to have CIN 2,3 or cancer in the experimental arm shows that cytology adds very little benefit. Only 2 of 75 women with CIN 2,3 or cancer were identified by cytology alone. In contrast, 21 (28%) of the cases of CIN 2,3 or cancer were in women who were high-risk HPV-positive and cytology-negative (TABLE 2).
TABLE 2
How cytology and HPV testing compare: Results from the Italian screening trial
| CYTOLOGY/HPV TEST | TOTAL NO. | CIN 2+ |
|---|---|---|
| ≥ASCUS/positive | 300 | 52 (69%) |
| ≥ASCUS/negative | 594 | 2 (3%) |
| Within normal limits/positive | 885 | 21 (28%) |
| Modified from Ronco G et al | ||
The United States is falling behind other countries in assessing how best to utilize HPV testing for screening. Ongoing trials in The Netherlands, Italy, United Kingdom, Canada, and Finland are evaluating whether cytology can be replaced by HPV DNA testing for screening. Currently, HPV testing is only approved as an adjunct to cytology for cervical cancer screening in the United States, and no similar trials are under way.
OCs not linked to HPV infection, and condoms afford some protection
Vaccarella S, Lazcano-Ponce E, Castro-Garduno JA, et al. Prevalence and determinants of human papillomavirus infection in men attending vasectomy clinics in Mexico. Int J Cancer. 2006;119:1934–1939.
Vaccarella S, Franceschi S, Herrero R, et al. Sexual behavior, condom use, and human papillomavirus: pooled analysis of the IARC human papillomavirus prevalence surveys. Cancer Epidemiol Biomarkers Prev. 2006;15:326–333.
Winer RL, Hughes JP, Feng Q, et al. Condom use and the risk of genital human papillomavirus infection in young women. N Engl J Med. 2006;354:2645–2654.
No question: Anogenital HPV infections are transmitted almost exclusively through intimate sexual contact.3 The standard markers of sexual exposure, such as the number of sexual partners and the number of partners that one’s partner has had, are key risk factors for infection with HPV. Women often ask whether other factors such as oral contraceptive (OC) use, diet, smoking, and condom use affect their risk for infection. But nonsexual risk factors are difficult to evaluate because the strength of sexual risk factors is so high.
To clarify the role played by non-sexual factors, the International Association for Research on Cancer (IARC) pooled data from multiple HPV prevalence studies involving more than 15,000 women from 14 different areas worldwide. This study clearly indicates that the use of OCs is not associated with HPV infection. Current, former, and never users of OCs all had the same risk of being HPV-positive. Therefore, although OCs are a risk factor for cervical cancer, the elevated risk cannot be explained by an increased susceptibility to HPV infection. This study also found that the menopausal transition had no clear effect on HPV infection.
New data show condoms to be more beneficial than not
Condoms are widely recognized as an effective barrier to the sexual transmission of HIV; their efficacy in blocking the transmission of other sexual diseases is less well documented. Most studies that have evaluated the impact of condom use on HPV infection have failed to find a beneficial effect. This may reflect the fact that condoms are often used inconsistently. In addition, there is a tendency to use condoms when having higher-risk sexual encounters, such as with a new partner.
In a recent study from Seattle, Winer and colleagues followed 82 female university students who first initiated sex while enrolled in the study or within 2 weeks of joining the study. The incidence of HPV infection was 38 per 100 patient-years of follow-up among women whose partners used condoms during all acts of intercourse, compared with 89.3 per 100 patient-years of follow-up among women whose partners used condoms less than 5% of the time. Risk reductions were observed for both high- and low-risk types of HPV.
Condoms also appeared to protect against the development of CIN. There were no cases of CIN during 32 patient-years among women whose partners consistently used condoms, compared with 14 cases of incident CIN during 97 patient-years of follow-up among women whose partners did not use condoms or who used them less consistently.
LEEP may have an adverse obstetric impact
Kyrgiou M, Koliopoulos G, Martin-Hirsch P, Arbyn M, Prendiville W, Paraskevaidis E. Obstetric outcomes after conservative treatment for intraepithelial or early invasive cervical lesions: systematic review and meta-analysis. Lancet. 2006;367:489–498.
Although most clinicians recognize that cold-knife conization has the potential to cause adverse obstetric outcomes, the same has not been recognized for loop electrosurgical excisional procedures (LEEP). In fact, most of the studies published in the early 1990s showed that LEEP had little impact on obstetric outcomes. Now we know better: Kyrgiou and colleagues conducted a systematic review and meta-analysis of the published literature on obstetric outcomes after treatment of CIN lesions, and found that all types of excisional procedures produce similar pregnancy-related morbidities.
LEEP had a significant association with preterm delivery (11% risk in treated women versus 7% in untreated women), low-birth-weight infants (8% in treated women versus 4% in untreated women), and premature rupture of membranes (5% in treated women versus 2% in untreated women). Although there were no significant increases in NICU admissions or perinatal mortality among the offspring of women who had undergone LEEP versus those who had not, nonsignificant increases were observed.
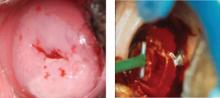
Similar increases in pregnancy-related morbidity were not observed among patients who underwent ablative procedures. This suggests that the amount of tissue that is removed during the LEEP (FIGURE 1) is important. Therefore, when treating CIN 2,3 lesions, especially in young women, consider using an ablative method such as cryotherapy or electrofulguration, unless colposcopy is unsatisfactory or there is a colposcopic or pathologic suspicion that an occult cancer is present.
FIGURE 1 CIN 2,3 and its treatment by LEEP
Is liquid-based cytology as sensitive as we thought?
Davey E, Barratt A, Irwig L, et al. Effect of study design and quality on unsatisfactory rates, cytology classifications, and accuracy in liquid-based versus conventional cervical cytology: a systematic review. Lancet. 2006;367:122–132.
Ronco G, Segnan N, Giorgi-Rossi P, et al. Human papillomavirus testing and liquid-based cytology: results at recruitment from the new technologies for cervical cancer randomized controlled trial. J Natl Cancer Inst. 2006;98:765–774.
Taylor S, Kuhn L, Dupree W, Denny L, De Souza M, Wright TC Jr. Direct comparison of liquid-based and conventional cytology in a South African screening trial. Int J Cancer. 2006;118:957–962.
A major reappraisal of liquid-based cytology (LBC) is under way. When it was first introduced, LBC was believed to provide a significant advantage over conventional cervical cytology in terms of sensitivity for CIN 2,3 or cancer. However, most of the studies that compared the 2 modalities had severe methodological problems. Many utilized historical controls, and most others simply reported increases in the number of cases cytologically diagnosed as squamous intraepithelial lesions (SIL). Very few measured histologic endpoints, and the few studies that did failed to blind the pathologists evaluating the histology to the cytologic findings. Only 1 small study was randomized.
Focus on high-quality studies finds lower sensitivity for LBC
Recently, Davey and colleagues conducted a systematic review of the published literature comparing LBC with conventional cytology. A total of 56 studies were evaluated, 52 of which provided enough information to evaluate differences between the 2 methods in the detection of low-grade squamous intraepithelial lesions (LSIL) and high-grade SIL (HSIL). These 52 studies included more than 1.25 million slides.
None of the studies that were evaluated were judged to be of “ideal quality,” and only 5 were judged to be of “high quality.” When all of the studies are taken into account and combined, there appears to be an increase in the cytologic detection of LSIL and HSIL with the use of LBC. However, further evaluation showed marked differences in the results obtained by studies of different quality.
When only “high-quality” studies are analyzed, there is no indication that LBC increases the detection of HSIL. Davey and colleagues concluded that there is no evidence that LBC reduces the proportion of unsatisfactory slides or outperforms conventional cytology in identifying women with CIN 2,3. They also noted that large randomized trials are needed.
Little difference between modalities in randomized trials
After the systematic review was conducted, 2 large trials comparing LBC with conventional cytology were published. In the first trial, Taylor and colleagues collected samples from South African women and analyzed them in blinded fashion in US laboratories. In their carefully controlled study, 5,652 women received either LBC or conventional cytology (rotated on a 6-month basis), and all women underwent colposcopy and cervical biopsy. No significant difference was observed in the sensitivity of LBC and conventional cytology in the detection of CIN 2,3 or cancer. In fact, there was a nonsignificant increase in sensitivity with conventional cytology, compared with LBC. Positive predictive value was lower with LBC than with conventional cytology. This means that a smaller proportion of women with an abnormal result on LBC had CIN 2,3 or cancer identified at colposcopy than did women who had an abnormal result on conventional cytology.
Similarly, in a large trial from Italy, Ronco and colleagues also failed to find LBC to be more sensitive than conventional cytology. Their trial randomized 33,364 women to LBC or conventional cytology. The use of LBC did not increase the detection of CIN 2,3 or cancer, compared with conventional cytology, but did lead to a dramatic reduction (43%) in positive predictive value due to an increase in the number of abnormal samples.
A similar increase in minor cytologic abnormalities with the use of LBC is now well documented in the United States. According to surveys from the College of American Pathologists, the median percentile reporting rate of LSIL in US laboratories in 2003 was 1.4% for conventional cytology specimens and 2.4% for liquid-based specimens.1
Taken together (TABLE 3), these studies suggest that LBC has no greater sensitivity than conventional cytology and therefore does not solve the problems associated with the poor sensitivity of cervical cytology. However, LBC does have other advantages, the greatest being the availability of residual fluid for “reflex” HPV testing in women with ASC-US and for testing for other pathogens, such as Chlamydia.
TABLE 3
When conventional and liquid-based cytology are compared, the latter isn’t more sensitive
| STUDY | NO. WOMEN | CONVENTIONAL CYTOLOGY | LIQUID-BASED CYTOLOGY | ||
|---|---|---|---|---|---|
| SENSITIVITY* | PPV* | SENSITIVITY* | PPV* | ||
| Taylor et al | 5,652 | 84%† | 11.4 | 71% | 9.4 |
| Ronco et al | 33,364 | 70% | 11.4 | 74%† | 6.5 |
| PPV=positive predictive value | |||||
| *for detection of CIN 2,3 or cancer | |||||
| †Nonsignificant | |||||
Most cytologists find it easier to evaluate LBC specimens than conventional cytology specimens. Nor is it likely that cytology laboratories will want to switch back to conventional cytology now that the conversion to LBC has taken place.
Dr. Wright reports no financial relationships with any company whose products are mentioned in this article.
1. Davey DD, Neal MH, Wilbur DC, Colgan TJ, Styer PE, Mody DR. Bethesda 2001 implementation and reporting rates: 2003 practices of participants in the College of American Pathologists Interlaboratory Comparison Program in Cervicovaginal Cytology. Arch Pathol Lab Med. 2004;128:1224-1229.
2. Wright TC, Jr, Schiffman M, Solomon D, et al. Interim guidance for the use of human papillomavirus DNA testing as an adjunct to cervical cytology for screening. Obstet Gynecol. 2004;103:304-309.
3. Burchell AN, Winer RL, de Sanjose S, Franco EL. Chapter 6: Epidemiology and transmission dynamics of genital HPV infection. Vaccine. 2006;24 Suppl 3:S52-61.
The year 2006 was a busy one for those of us engaged in cervical cancer prevention. The most notable development was approval by the US Food and Drug Administration of the human papillomavirus (HPV) quadrivalent vaccine in June, followed closely by guidelines for its use from the Advisory Committee on Immunization Practices (June) and the American College of Obstetricians and Gynecologists (September). Key issues related to the introduction of the HPV vaccine into clinical practice were reviewed in a roundtable discussion in the January 2007 issue of OBG Management.
Therefore, this update will depart, for the moment, from matters related to the vaccine and concentrate on several other critical areas:
- Testing for high-risk HPV types is useful. Large European cervical cancer screening trials confirm a benefit.
- Condoms and oral contraceptives—are they risk modifiers for HPV infection? Answers (“Yes” and “No,” respectively) come from new data.
- Loop electrosurgical excision carries obstetric risks. In fact, all types of excisional procedures produce similar pregnancy-related morbidity.
- Liquid-based cytology may not be superior to conventional cytology. So suggest new studies and a systematic review of the literature.
HPV testing outperforms cytology for screening
Cuzick J, Clavel C, Petry KU, et al. Overview of the European and North American studies on HPV testing in primary cervical cancer screening. Int J Cancer. 2006;119:1095–1101.
Ronco G, Segnan N, Giorgi-Rossi P, et al. Human papillomavirus testing and liquid-based cytology: results at recruitment from the new technologies for cervical cancer randomized controlled trial. J Natl Cancer Inst. 2006;98:765–774.
HPV DNA testing is more sensitive than cervical cytology, reduces specificity to only a moderate degree, and performs similarly in different parts of Europe and North America. Those are the findings of a review by Cuzick and colleagues of all recent large European and North American cervical cancer screening studies. To date, 4 large European trials and 1 from Mexico have directly compared HPV testing and cytology in women aged 30 years and older. Combined, these trials have enrolled over 60,000 women. In every study, testing for high-risk types of HPV using the commercially available Hybrid Capture 2 HPV DNA assay had a much higher sensitivity for identifying women with cervical intraepithelial neoplasia (CIN) 2,3 or cancer (86–97%) than did cervical cytology (34–74%). Moreover, the combination of cytology and HPV testing had a sensitivity ranging from 94% to 100% in the different studies. The average sensitivity of 98% for the combination of cytology and HPV testing means that there is a less than 1 in 1,000 chance of missing CIN 2,3 or cancer when women are screened with both tests (TABLE 1).
Specificity is reasonable, too
If you worry that using HPV DNA testing in women aged 30 and older will flag too many as high-risk HPV-positive and cause them unnecessary colposcopic examinations or anxiety, here is a comforting finding: The specificity of HPV DNA testing is not as low as many had feared—provided we limit screening to women aged 30 and older. In the 5 trials mentioned, the specificity of HPV DNA testing ranged from 92% to 97%. Even when HPV DNA testing and cytology were used together, the average specificity of the 2 tests combined was 93%. A specificity of 93% means that only 7 of 100 screened women who don’t have CIN 2,3 or cancer will be classified as “positive.”
To put this number into perspective, a 2003 survey of US cytology laboratories found a median rate of abnormal results of 6.9%.1 Therefore, in routine clinical practice, incorporation of HPV DNA testing into screening for women aged 30 and older is not expected to greatly increase the number of women requiring additional follow-up.
The single most important component of management is appropriate counseling. Even though there are fewer of these women than we anticipated, these patients need to be reassured that their risk of having a significant lesion (CIN 2,3 or cancer) is quite low—only about 1 in 20. They also need to know that about two thirds of women—even women aged 30 and older—are HPV-negative when they are retested in 12 months.
In addition, clinicians need to stress that positive HPV status is a risk factor for having or developing cervical disease, not an indication that disease is present. One analogy that patients readily understand is the relationship between other types of health risk factors, such as mild hypertension or mildly elevated serum cholesterol, and disease. These explanations help the patient understand why, in settings where genotyping for HPV 16 and 18 is not available, the best course of action is to wait 12 months and be retested.2
Which test should be used first?
Basic screening principles suggest that, whenever 2 tests are used in combination, the most sensitive test should be used first, with patients who test positive tested again using the second, more specific, test. These principles suggest we should be using HPV testing alone as the initial screening test and limiting the use of cytology to triage HPV-positive women. This sequence of testing could potentially be done in a “reflex” fashion.
The large Italian screening trial by Ronco and colleagues randomized 33,364 women aged 35 to 60 years to 2 different screening strategies: routine conventional cytology or liquid-based cytology with HPV testing.3 In the routine cytology arm, researchers identified only 51 cases of CIN 2,3 or cancer, but in the experimental arm, they identified 75 cases. A breakdown of the initial screening results in the women found to have CIN 2,3 or cancer in the experimental arm shows that cytology adds very little benefit. Only 2 of 75 women with CIN 2,3 or cancer were identified by cytology alone. In contrast, 21 (28%) of the cases of CIN 2,3 or cancer were in women who were high-risk HPV-positive and cytology-negative (TABLE 2).
TABLE 2
How cytology and HPV testing compare: Results from the Italian screening trial
| CYTOLOGY/HPV TEST | TOTAL NO. | CIN 2+ |
|---|---|---|
| ≥ASCUS/positive | 300 | 52 (69%) |
| ≥ASCUS/negative | 594 | 2 (3%) |
| Within normal limits/positive | 885 | 21 (28%) |
| Modified from Ronco G et al | ||
The United States is falling behind other countries in assessing how best to utilize HPV testing for screening. Ongoing trials in The Netherlands, Italy, United Kingdom, Canada, and Finland are evaluating whether cytology can be replaced by HPV DNA testing for screening. Currently, HPV testing is only approved as an adjunct to cytology for cervical cancer screening in the United States, and no similar trials are under way.
OCs not linked to HPV infection, and condoms afford some protection
Vaccarella S, Lazcano-Ponce E, Castro-Garduno JA, et al. Prevalence and determinants of human papillomavirus infection in men attending vasectomy clinics in Mexico. Int J Cancer. 2006;119:1934–1939.
Vaccarella S, Franceschi S, Herrero R, et al. Sexual behavior, condom use, and human papillomavirus: pooled analysis of the IARC human papillomavirus prevalence surveys. Cancer Epidemiol Biomarkers Prev. 2006;15:326–333.
Winer RL, Hughes JP, Feng Q, et al. Condom use and the risk of genital human papillomavirus infection in young women. N Engl J Med. 2006;354:2645–2654.
No question: Anogenital HPV infections are transmitted almost exclusively through intimate sexual contact.3 The standard markers of sexual exposure, such as the number of sexual partners and the number of partners that one’s partner has had, are key risk factors for infection with HPV. Women often ask whether other factors such as oral contraceptive (OC) use, diet, smoking, and condom use affect their risk for infection. But nonsexual risk factors are difficult to evaluate because the strength of sexual risk factors is so high.
To clarify the role played by non-sexual factors, the International Association for Research on Cancer (IARC) pooled data from multiple HPV prevalence studies involving more than 15,000 women from 14 different areas worldwide. This study clearly indicates that the use of OCs is not associated with HPV infection. Current, former, and never users of OCs all had the same risk of being HPV-positive. Therefore, although OCs are a risk factor for cervical cancer, the elevated risk cannot be explained by an increased susceptibility to HPV infection. This study also found that the menopausal transition had no clear effect on HPV infection.
New data show condoms to be more beneficial than not
Condoms are widely recognized as an effective barrier to the sexual transmission of HIV; their efficacy in blocking the transmission of other sexual diseases is less well documented. Most studies that have evaluated the impact of condom use on HPV infection have failed to find a beneficial effect. This may reflect the fact that condoms are often used inconsistently. In addition, there is a tendency to use condoms when having higher-risk sexual encounters, such as with a new partner.
In a recent study from Seattle, Winer and colleagues followed 82 female university students who first initiated sex while enrolled in the study or within 2 weeks of joining the study. The incidence of HPV infection was 38 per 100 patient-years of follow-up among women whose partners used condoms during all acts of intercourse, compared with 89.3 per 100 patient-years of follow-up among women whose partners used condoms less than 5% of the time. Risk reductions were observed for both high- and low-risk types of HPV.
Condoms also appeared to protect against the development of CIN. There were no cases of CIN during 32 patient-years among women whose partners consistently used condoms, compared with 14 cases of incident CIN during 97 patient-years of follow-up among women whose partners did not use condoms or who used them less consistently.
LEEP may have an adverse obstetric impact
Kyrgiou M, Koliopoulos G, Martin-Hirsch P, Arbyn M, Prendiville W, Paraskevaidis E. Obstetric outcomes after conservative treatment for intraepithelial or early invasive cervical lesions: systematic review and meta-analysis. Lancet. 2006;367:489–498.
Although most clinicians recognize that cold-knife conization has the potential to cause adverse obstetric outcomes, the same has not been recognized for loop electrosurgical excisional procedures (LEEP). In fact, most of the studies published in the early 1990s showed that LEEP had little impact on obstetric outcomes. Now we know better: Kyrgiou and colleagues conducted a systematic review and meta-analysis of the published literature on obstetric outcomes after treatment of CIN lesions, and found that all types of excisional procedures produce similar pregnancy-related morbidities.
LEEP had a significant association with preterm delivery (11% risk in treated women versus 7% in untreated women), low-birth-weight infants (8% in treated women versus 4% in untreated women), and premature rupture of membranes (5% in treated women versus 2% in untreated women). Although there were no significant increases in NICU admissions or perinatal mortality among the offspring of women who had undergone LEEP versus those who had not, nonsignificant increases were observed.
Similar increases in pregnancy-related morbidity were not observed among patients who underwent ablative procedures. This suggests that the amount of tissue that is removed during the LEEP (FIGURE 1) is important. Therefore, when treating CIN 2,3 lesions, especially in young women, consider using an ablative method such as cryotherapy or electrofulguration, unless colposcopy is unsatisfactory or there is a colposcopic or pathologic suspicion that an occult cancer is present.
FIGURE 1 CIN 2,3 and its treatment by LEEP
Is liquid-based cytology as sensitive as we thought?
Davey E, Barratt A, Irwig L, et al. Effect of study design and quality on unsatisfactory rates, cytology classifications, and accuracy in liquid-based versus conventional cervical cytology: a systematic review. Lancet. 2006;367:122–132.
Ronco G, Segnan N, Giorgi-Rossi P, et al. Human papillomavirus testing and liquid-based cytology: results at recruitment from the new technologies for cervical cancer randomized controlled trial. J Natl Cancer Inst. 2006;98:765–774.
Taylor S, Kuhn L, Dupree W, Denny L, De Souza M, Wright TC Jr. Direct comparison of liquid-based and conventional cytology in a South African screening trial. Int J Cancer. 2006;118:957–962.
A major reappraisal of liquid-based cytology (LBC) is under way. When it was first introduced, LBC was believed to provide a significant advantage over conventional cervical cytology in terms of sensitivity for CIN 2,3 or cancer. However, most of the studies that compared the 2 modalities had severe methodological problems. Many utilized historical controls, and most others simply reported increases in the number of cases cytologically diagnosed as squamous intraepithelial lesions (SIL). Very few measured histologic endpoints, and the few studies that did failed to blind the pathologists evaluating the histology to the cytologic findings. Only 1 small study was randomized.
Focus on high-quality studies finds lower sensitivity for LBC
Recently, Davey and colleagues conducted a systematic review of the published literature comparing LBC with conventional cytology. A total of 56 studies were evaluated, 52 of which provided enough information to evaluate differences between the 2 methods in the detection of low-grade squamous intraepithelial lesions (LSIL) and high-grade SIL (HSIL). These 52 studies included more than 1.25 million slides.
None of the studies that were evaluated were judged to be of “ideal quality,” and only 5 were judged to be of “high quality.” When all of the studies are taken into account and combined, there appears to be an increase in the cytologic detection of LSIL and HSIL with the use of LBC. However, further evaluation showed marked differences in the results obtained by studies of different quality.
When only “high-quality” studies are analyzed, there is no indication that LBC increases the detection of HSIL. Davey and colleagues concluded that there is no evidence that LBC reduces the proportion of unsatisfactory slides or outperforms conventional cytology in identifying women with CIN 2,3. They also noted that large randomized trials are needed.
Little difference between modalities in randomized trials
After the systematic review was conducted, 2 large trials comparing LBC with conventional cytology were published. In the first trial, Taylor and colleagues collected samples from South African women and analyzed them in blinded fashion in US laboratories. In their carefully controlled study, 5,652 women received either LBC or conventional cytology (rotated on a 6-month basis), and all women underwent colposcopy and cervical biopsy. No significant difference was observed in the sensitivity of LBC and conventional cytology in the detection of CIN 2,3 or cancer. In fact, there was a nonsignificant increase in sensitivity with conventional cytology, compared with LBC. Positive predictive value was lower with LBC than with conventional cytology. This means that a smaller proportion of women with an abnormal result on LBC had CIN 2,3 or cancer identified at colposcopy than did women who had an abnormal result on conventional cytology.
Similarly, in a large trial from Italy, Ronco and colleagues also failed to find LBC to be more sensitive than conventional cytology. Their trial randomized 33,364 women to LBC or conventional cytology. The use of LBC did not increase the detection of CIN 2,3 or cancer, compared with conventional cytology, but did lead to a dramatic reduction (43%) in positive predictive value due to an increase in the number of abnormal samples.
A similar increase in minor cytologic abnormalities with the use of LBC is now well documented in the United States. According to surveys from the College of American Pathologists, the median percentile reporting rate of LSIL in US laboratories in 2003 was 1.4% for conventional cytology specimens and 2.4% for liquid-based specimens.1
Taken together (TABLE 3), these studies suggest that LBC has no greater sensitivity than conventional cytology and therefore does not solve the problems associated with the poor sensitivity of cervical cytology. However, LBC does have other advantages, the greatest being the availability of residual fluid for “reflex” HPV testing in women with ASC-US and for testing for other pathogens, such as Chlamydia.
TABLE 3
When conventional and liquid-based cytology are compared, the latter isn’t more sensitive
| STUDY | NO. WOMEN | CONVENTIONAL CYTOLOGY | LIQUID-BASED CYTOLOGY | ||
|---|---|---|---|---|---|
| SENSITIVITY* | PPV* | SENSITIVITY* | PPV* | ||
| Taylor et al | 5,652 | 84%† | 11.4 | 71% | 9.4 |
| Ronco et al | 33,364 | 70% | 11.4 | 74%† | 6.5 |
| PPV=positive predictive value | |||||
| *for detection of CIN 2,3 or cancer | |||||
| †Nonsignificant | |||||
Most cytologists find it easier to evaluate LBC specimens than conventional cytology specimens. Nor is it likely that cytology laboratories will want to switch back to conventional cytology now that the conversion to LBC has taken place.
Dr. Wright reports no financial relationships with any company whose products are mentioned in this article.
The year 2006 was a busy one for those of us engaged in cervical cancer prevention. The most notable development was approval by the US Food and Drug Administration of the human papillomavirus (HPV) quadrivalent vaccine in June, followed closely by guidelines for its use from the Advisory Committee on Immunization Practices (June) and the American College of Obstetricians and Gynecologists (September). Key issues related to the introduction of the HPV vaccine into clinical practice were reviewed in a roundtable discussion in the January 2007 issue of OBG Management.
Therefore, this update will depart, for the moment, from matters related to the vaccine and concentrate on several other critical areas:
- Testing for high-risk HPV types is useful. Large European cervical cancer screening trials confirm a benefit.
- Condoms and oral contraceptives—are they risk modifiers for HPV infection? Answers (“Yes” and “No,” respectively) come from new data.
- Loop electrosurgical excision carries obstetric risks. In fact, all types of excisional procedures produce similar pregnancy-related morbidity.
- Liquid-based cytology may not be superior to conventional cytology. So suggest new studies and a systematic review of the literature.
HPV testing outperforms cytology for screening
Cuzick J, Clavel C, Petry KU, et al. Overview of the European and North American studies on HPV testing in primary cervical cancer screening. Int J Cancer. 2006;119:1095–1101.
Ronco G, Segnan N, Giorgi-Rossi P, et al. Human papillomavirus testing and liquid-based cytology: results at recruitment from the new technologies for cervical cancer randomized controlled trial. J Natl Cancer Inst. 2006;98:765–774.
HPV DNA testing is more sensitive than cervical cytology, reduces specificity to only a moderate degree, and performs similarly in different parts of Europe and North America. Those are the findings of a review by Cuzick and colleagues of all recent large European and North American cervical cancer screening studies. To date, 4 large European trials and 1 from Mexico have directly compared HPV testing and cytology in women aged 30 years and older. Combined, these trials have enrolled over 60,000 women. In every study, testing for high-risk types of HPV using the commercially available Hybrid Capture 2 HPV DNA assay had a much higher sensitivity for identifying women with cervical intraepithelial neoplasia (CIN) 2,3 or cancer (86–97%) than did cervical cytology (34–74%). Moreover, the combination of cytology and HPV testing had a sensitivity ranging from 94% to 100% in the different studies. The average sensitivity of 98% for the combination of cytology and HPV testing means that there is a less than 1 in 1,000 chance of missing CIN 2,3 or cancer when women are screened with both tests (TABLE 1).
Specificity is reasonable, too
If you worry that using HPV DNA testing in women aged 30 and older will flag too many as high-risk HPV-positive and cause them unnecessary colposcopic examinations or anxiety, here is a comforting finding: The specificity of HPV DNA testing is not as low as many had feared—provided we limit screening to women aged 30 and older. In the 5 trials mentioned, the specificity of HPV DNA testing ranged from 92% to 97%. Even when HPV DNA testing and cytology were used together, the average specificity of the 2 tests combined was 93%. A specificity of 93% means that only 7 of 100 screened women who don’t have CIN 2,3 or cancer will be classified as “positive.”
To put this number into perspective, a 2003 survey of US cytology laboratories found a median rate of abnormal results of 6.9%.1 Therefore, in routine clinical practice, incorporation of HPV DNA testing into screening for women aged 30 and older is not expected to greatly increase the number of women requiring additional follow-up.
The single most important component of management is appropriate counseling. Even though there are fewer of these women than we anticipated, these patients need to be reassured that their risk of having a significant lesion (CIN 2,3 or cancer) is quite low—only about 1 in 20. They also need to know that about two thirds of women—even women aged 30 and older—are HPV-negative when they are retested in 12 months.
In addition, clinicians need to stress that positive HPV status is a risk factor for having or developing cervical disease, not an indication that disease is present. One analogy that patients readily understand is the relationship between other types of health risk factors, such as mild hypertension or mildly elevated serum cholesterol, and disease. These explanations help the patient understand why, in settings where genotyping for HPV 16 and 18 is not available, the best course of action is to wait 12 months and be retested.2
Which test should be used first?
Basic screening principles suggest that, whenever 2 tests are used in combination, the most sensitive test should be used first, with patients who test positive tested again using the second, more specific, test. These principles suggest we should be using HPV testing alone as the initial screening test and limiting the use of cytology to triage HPV-positive women. This sequence of testing could potentially be done in a “reflex” fashion.
The large Italian screening trial by Ronco and colleagues randomized 33,364 women aged 35 to 60 years to 2 different screening strategies: routine conventional cytology or liquid-based cytology with HPV testing.3 In the routine cytology arm, researchers identified only 51 cases of CIN 2,3 or cancer, but in the experimental arm, they identified 75 cases. A breakdown of the initial screening results in the women found to have CIN 2,3 or cancer in the experimental arm shows that cytology adds very little benefit. Only 2 of 75 women with CIN 2,3 or cancer were identified by cytology alone. In contrast, 21 (28%) of the cases of CIN 2,3 or cancer were in women who were high-risk HPV-positive and cytology-negative (TABLE 2).
TABLE 2
How cytology and HPV testing compare: Results from the Italian screening trial
| CYTOLOGY/HPV TEST | TOTAL NO. | CIN 2+ |
|---|---|---|
| ≥ASCUS/positive | 300 | 52 (69%) |
| ≥ASCUS/negative | 594 | 2 (3%) |
| Within normal limits/positive | 885 | 21 (28%) |
| Modified from Ronco G et al | ||
The United States is falling behind other countries in assessing how best to utilize HPV testing for screening. Ongoing trials in The Netherlands, Italy, United Kingdom, Canada, and Finland are evaluating whether cytology can be replaced by HPV DNA testing for screening. Currently, HPV testing is only approved as an adjunct to cytology for cervical cancer screening in the United States, and no similar trials are under way.
OCs not linked to HPV infection, and condoms afford some protection
Vaccarella S, Lazcano-Ponce E, Castro-Garduno JA, et al. Prevalence and determinants of human papillomavirus infection in men attending vasectomy clinics in Mexico. Int J Cancer. 2006;119:1934–1939.
Vaccarella S, Franceschi S, Herrero R, et al. Sexual behavior, condom use, and human papillomavirus: pooled analysis of the IARC human papillomavirus prevalence surveys. Cancer Epidemiol Biomarkers Prev. 2006;15:326–333.
Winer RL, Hughes JP, Feng Q, et al. Condom use and the risk of genital human papillomavirus infection in young women. N Engl J Med. 2006;354:2645–2654.
No question: Anogenital HPV infections are transmitted almost exclusively through intimate sexual contact.3 The standard markers of sexual exposure, such as the number of sexual partners and the number of partners that one’s partner has had, are key risk factors for infection with HPV. Women often ask whether other factors such as oral contraceptive (OC) use, diet, smoking, and condom use affect their risk for infection. But nonsexual risk factors are difficult to evaluate because the strength of sexual risk factors is so high.
To clarify the role played by non-sexual factors, the International Association for Research on Cancer (IARC) pooled data from multiple HPV prevalence studies involving more than 15,000 women from 14 different areas worldwide. This study clearly indicates that the use of OCs is not associated with HPV infection. Current, former, and never users of OCs all had the same risk of being HPV-positive. Therefore, although OCs are a risk factor for cervical cancer, the elevated risk cannot be explained by an increased susceptibility to HPV infection. This study also found that the menopausal transition had no clear effect on HPV infection.
New data show condoms to be more beneficial than not
Condoms are widely recognized as an effective barrier to the sexual transmission of HIV; their efficacy in blocking the transmission of other sexual diseases is less well documented. Most studies that have evaluated the impact of condom use on HPV infection have failed to find a beneficial effect. This may reflect the fact that condoms are often used inconsistently. In addition, there is a tendency to use condoms when having higher-risk sexual encounters, such as with a new partner.
In a recent study from Seattle, Winer and colleagues followed 82 female university students who first initiated sex while enrolled in the study or within 2 weeks of joining the study. The incidence of HPV infection was 38 per 100 patient-years of follow-up among women whose partners used condoms during all acts of intercourse, compared with 89.3 per 100 patient-years of follow-up among women whose partners used condoms less than 5% of the time. Risk reductions were observed for both high- and low-risk types of HPV.
Condoms also appeared to protect against the development of CIN. There were no cases of CIN during 32 patient-years among women whose partners consistently used condoms, compared with 14 cases of incident CIN during 97 patient-years of follow-up among women whose partners did not use condoms or who used them less consistently.
LEEP may have an adverse obstetric impact
Kyrgiou M, Koliopoulos G, Martin-Hirsch P, Arbyn M, Prendiville W, Paraskevaidis E. Obstetric outcomes after conservative treatment for intraepithelial or early invasive cervical lesions: systematic review and meta-analysis. Lancet. 2006;367:489–498.
Although most clinicians recognize that cold-knife conization has the potential to cause adverse obstetric outcomes, the same has not been recognized for loop electrosurgical excisional procedures (LEEP). In fact, most of the studies published in the early 1990s showed that LEEP had little impact on obstetric outcomes. Now we know better: Kyrgiou and colleagues conducted a systematic review and meta-analysis of the published literature on obstetric outcomes after treatment of CIN lesions, and found that all types of excisional procedures produce similar pregnancy-related morbidities.
LEEP had a significant association with preterm delivery (11% risk in treated women versus 7% in untreated women), low-birth-weight infants (8% in treated women versus 4% in untreated women), and premature rupture of membranes (5% in treated women versus 2% in untreated women). Although there were no significant increases in NICU admissions or perinatal mortality among the offspring of women who had undergone LEEP versus those who had not, nonsignificant increases were observed.
Similar increases in pregnancy-related morbidity were not observed among patients who underwent ablative procedures. This suggests that the amount of tissue that is removed during the LEEP (FIGURE 1) is important. Therefore, when treating CIN 2,3 lesions, especially in young women, consider using an ablative method such as cryotherapy or electrofulguration, unless colposcopy is unsatisfactory or there is a colposcopic or pathologic suspicion that an occult cancer is present.
FIGURE 1 CIN 2,3 and its treatment by LEEP
Is liquid-based cytology as sensitive as we thought?
Davey E, Barratt A, Irwig L, et al. Effect of study design and quality on unsatisfactory rates, cytology classifications, and accuracy in liquid-based versus conventional cervical cytology: a systematic review. Lancet. 2006;367:122–132.
Ronco G, Segnan N, Giorgi-Rossi P, et al. Human papillomavirus testing and liquid-based cytology: results at recruitment from the new technologies for cervical cancer randomized controlled trial. J Natl Cancer Inst. 2006;98:765–774.
Taylor S, Kuhn L, Dupree W, Denny L, De Souza M, Wright TC Jr. Direct comparison of liquid-based and conventional cytology in a South African screening trial. Int J Cancer. 2006;118:957–962.
A major reappraisal of liquid-based cytology (LBC) is under way. When it was first introduced, LBC was believed to provide a significant advantage over conventional cervical cytology in terms of sensitivity for CIN 2,3 or cancer. However, most of the studies that compared the 2 modalities had severe methodological problems. Many utilized historical controls, and most others simply reported increases in the number of cases cytologically diagnosed as squamous intraepithelial lesions (SIL). Very few measured histologic endpoints, and the few studies that did failed to blind the pathologists evaluating the histology to the cytologic findings. Only 1 small study was randomized.
Focus on high-quality studies finds lower sensitivity for LBC
Recently, Davey and colleagues conducted a systematic review of the published literature comparing LBC with conventional cytology. A total of 56 studies were evaluated, 52 of which provided enough information to evaluate differences between the 2 methods in the detection of low-grade squamous intraepithelial lesions (LSIL) and high-grade SIL (HSIL). These 52 studies included more than 1.25 million slides.
None of the studies that were evaluated were judged to be of “ideal quality,” and only 5 were judged to be of “high quality.” When all of the studies are taken into account and combined, there appears to be an increase in the cytologic detection of LSIL and HSIL with the use of LBC. However, further evaluation showed marked differences in the results obtained by studies of different quality.
When only “high-quality” studies are analyzed, there is no indication that LBC increases the detection of HSIL. Davey and colleagues concluded that there is no evidence that LBC reduces the proportion of unsatisfactory slides or outperforms conventional cytology in identifying women with CIN 2,3. They also noted that large randomized trials are needed.
Little difference between modalities in randomized trials
After the systematic review was conducted, 2 large trials comparing LBC with conventional cytology were published. In the first trial, Taylor and colleagues collected samples from South African women and analyzed them in blinded fashion in US laboratories. In their carefully controlled study, 5,652 women received either LBC or conventional cytology (rotated on a 6-month basis), and all women underwent colposcopy and cervical biopsy. No significant difference was observed in the sensitivity of LBC and conventional cytology in the detection of CIN 2,3 or cancer. In fact, there was a nonsignificant increase in sensitivity with conventional cytology, compared with LBC. Positive predictive value was lower with LBC than with conventional cytology. This means that a smaller proportion of women with an abnormal result on LBC had CIN 2,3 or cancer identified at colposcopy than did women who had an abnormal result on conventional cytology.
Similarly, in a large trial from Italy, Ronco and colleagues also failed to find LBC to be more sensitive than conventional cytology. Their trial randomized 33,364 women to LBC or conventional cytology. The use of LBC did not increase the detection of CIN 2,3 or cancer, compared with conventional cytology, but did lead to a dramatic reduction (43%) in positive predictive value due to an increase in the number of abnormal samples.
A similar increase in minor cytologic abnormalities with the use of LBC is now well documented in the United States. According to surveys from the College of American Pathologists, the median percentile reporting rate of LSIL in US laboratories in 2003 was 1.4% for conventional cytology specimens and 2.4% for liquid-based specimens.1
Taken together (TABLE 3), these studies suggest that LBC has no greater sensitivity than conventional cytology and therefore does not solve the problems associated with the poor sensitivity of cervical cytology. However, LBC does have other advantages, the greatest being the availability of residual fluid for “reflex” HPV testing in women with ASC-US and for testing for other pathogens, such as Chlamydia.
TABLE 3
When conventional and liquid-based cytology are compared, the latter isn’t more sensitive
| STUDY | NO. WOMEN | CONVENTIONAL CYTOLOGY | LIQUID-BASED CYTOLOGY | ||
|---|---|---|---|---|---|
| SENSITIVITY* | PPV* | SENSITIVITY* | PPV* | ||
| Taylor et al | 5,652 | 84%† | 11.4 | 71% | 9.4 |
| Ronco et al | 33,364 | 70% | 11.4 | 74%† | 6.5 |
| PPV=positive predictive value | |||||
| *for detection of CIN 2,3 or cancer | |||||
| †Nonsignificant | |||||
Most cytologists find it easier to evaluate LBC specimens than conventional cytology specimens. Nor is it likely that cytology laboratories will want to switch back to conventional cytology now that the conversion to LBC has taken place.
Dr. Wright reports no financial relationships with any company whose products are mentioned in this article.
1. Davey DD, Neal MH, Wilbur DC, Colgan TJ, Styer PE, Mody DR. Bethesda 2001 implementation and reporting rates: 2003 practices of participants in the College of American Pathologists Interlaboratory Comparison Program in Cervicovaginal Cytology. Arch Pathol Lab Med. 2004;128:1224-1229.
2. Wright TC, Jr, Schiffman M, Solomon D, et al. Interim guidance for the use of human papillomavirus DNA testing as an adjunct to cervical cytology for screening. Obstet Gynecol. 2004;103:304-309.
3. Burchell AN, Winer RL, de Sanjose S, Franco EL. Chapter 6: Epidemiology and transmission dynamics of genital HPV infection. Vaccine. 2006;24 Suppl 3:S52-61.
1. Davey DD, Neal MH, Wilbur DC, Colgan TJ, Styer PE, Mody DR. Bethesda 2001 implementation and reporting rates: 2003 practices of participants in the College of American Pathologists Interlaboratory Comparison Program in Cervicovaginal Cytology. Arch Pathol Lab Med. 2004;128:1224-1229.
2. Wright TC, Jr, Schiffman M, Solomon D, et al. Interim guidance for the use of human papillomavirus DNA testing as an adjunct to cervical cytology for screening. Obstet Gynecol. 2004;103:304-309.
3. Burchell AN, Winer RL, de Sanjose S, Franco EL. Chapter 6: Epidemiology and transmission dynamics of genital HPV infection. Vaccine. 2006;24 Suppl 3:S52-61.