User login
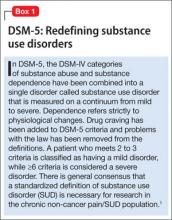
Patients with chronic non-cancer pain (CNCP) and a comorbid substance use disorder (SUD) are difficult to treat. There is a lack of high-quality clinical trials to guide management. This article focuses on current research, guidelines, and recommendations to best manage these patients. We present an analysis of recent statistics, patient characteristics, screening methods, as well as a discussion of changes to DSM-5 regarding substance abuse and addiction (Box 1).1
Opioid use and opioid-related overdoses have increased dramatically over the last decade (Box 2).2-5 Opioids are the primary medication used to treat CNCP, but their use in patients with comorbid SUDs is controversial. It is crucial for psychiatrists and other clinicians to know how to best identify, manage, and treat patients with CNCP/SUD.
Risk factors for CNCP/SUD
Evidence regarding the efficacy of screening methods to identify patients with chronic pain who are at high risk for substance misuse is insufficient. Key risk factors for developing chronic pain may include:
• elevated psychological distress
• negative beliefs and expectations about pain
• pain fear and avoidance
• disability
• anger or hostility
• maladaptive coping strategies
• catastrophic behaviors.5
In addition, these individuals may have a spouse who enables the sick role behavior.
Risk factors for developing a SUD related to prescribed opioids include:
• a history of problematic substance use
• sedative-hypnotic use
• positive family history for substance abuse
• legal problems
• heavy tobacco use
• age <50
• major depressive disorder or anxiety.5
In a review of 38 articles, Morasco et al6 found low-grade evidence with mixed results in attempt to find a correlation among sex, depression, anxiety, and tobacco use with CNCP/SUD. Other data suggest that the risk of addiction once opioids have been started increases with long refill periods and opioid morphine equivalents >120 mg.7 A history of childhood sexual abuse also may be a risk factor for chronic pain and addiction.5
Prevalence
The prevalence of opioid abuse among CNCP patients ranges from 3% to 48%; the highest rates are found among patients visiting the emergency room for opioid refills.7 These patients are more likely to exhibit aberrant behavior with their medications and may be prescribed higher opioid doses than patients who have CNCP only. Adherent CNCP/SUD patients show no difference in response to pain treatment compared with those with CNCP alone.6 Approximately 11.5% of CNCP patients taking opioids demonstrate aberrant medication use.6
Screening: Which method is best?
Data are scarce regarding the best screening methods to identify patients with CNCP/SUD. A survey of 48 patients by Moore et al8 found the combination of a clinical interview and the Screener and Opioid Assessment for Patients with Pain-Revised (SOAPP-R) is 90% sensitive in detecting CNCP/SUD. However, a systematic review by Chou et al9 found only 2 well-designed studies showing that the SOAPP-R weakly predicts future aberrant drug behavior and only 1 study showed that a high risk categorization on the Opioid Risk Tool (ORT) strongly increased the likelihood of predicting future abnormal drug-related behavior. Another well-designed study showed that the Current Opioid Misuse Measure (COMM) weakly raised the likelihood of detecting current aberrant drug behavior. No reliable data supported the efficacy of urine drug screens (UDS), pill counts, or prescription drug monitoring programs (PDMPs) for improving clinical outcomes.9 In a systematic review Starrels et al10 found only low-quality evidence supporting the effectiveness of opioid agreement contracts and UDS.
Treatment strategies
Once a patient with CNCP/SUD has been identified, it is important to categorize the severity of his (her) pain and substance use by using the decision tree (Figure) and screening tools such as SOAPP-R, ORT, and COMM. In a Veterans Administration (VA) study, only 35% of patients with an SUD received substance abuse treatment.11 The 2009 American Pain Society/American Academy of Pain Medicine guidelines recommended that opioids should considered for patients with substance abuse, serious aberrant drug-related behaviors, or psychiatric comorbidities only if frequent monitoring and treatment plan and mental health or addiction consultation were in place.12 These guidelines also recommended discontinuing opioids if repeated atypical behavior, substance abuse, diversion, lack of progress, or intolerable side effects occur. Repeated and more serious behaviors require a multidisciplinary team, expert consultation, therapy restructuring, and possibly discontinuation of opioids.12
The U.S. Office of National Drug Control Policy has created a council of federal agencies to spearhead the Prescription Drug Abuse Prevention Plan, which includes 4 major categories to reduce prescription drug abuse: education, monitoring, proper disposal, and enforcement.13 FDA commissioner Margaret Hamburg supports legislation to combine opioid education with Drug Enforcement Administration registration.14 The FDA began developing the risk evaluation and mitigation strategies in 2007 to educate physicians on proper prescribing of potentially dangerous medications.
Gourlay and Heit proposed a universal precautions method of opioid treatment for all pain patients.15 That includes:
• seeking differential diagnoses and comorbidities
• doing a baseline addiction assessment with UDS and PDMP evaluations
• obtaining informed consent for pain management
• creating pre- and post-treatment goals for pain and function
• evaluating the 4 “As” (analgesic response, increased activity, adverse events, and aberrant behavior)
• reviewing the evolution of the pain and comorbidities
• continuous documentation.5
Other helpful strategies include the Oregon’s SMART (Specific, Measurable, Action-oriented, Realistic, Time-Dependent) goal-setting, which helps physicians negotiate functional goals with patients and plan an exit strategy for those whose quality of life does not improve with opioids.5 Clinicians also can consider a sequential treatment model where patients with severe substance abuse and pain are detoxified of illicit drugs and alcohol before starting pain management. This approach is more effective if the pain is secondary to a more severe substance abuse problem that is not correlated to physical pain and acute rather than chronic.16
Psychotherapeutic interventions
In another VA study, a collaborative care intervention (CCI) combining education, self-efficacy, pain management, and feedback was not impeded by a history of SUD. The authors recommended CCI, stepped care, integrated interventions, and relapse prevention and stressed the importance of social support.17
A 10-week cognitive-behavioral therapy (CBT) program involving 44 patients enrolled in an integrated pain management program for recovering substance abusers found 50% of CNCP/SUD patients were opioid-free at 12 months.16 A combination of medication reduction and education resulted in less pain, increased functioning, decreased emotional distress, and less self-medicating. Additionally, patients reported 35% overall reduction in pain severity based on the McGill Pain Questionnaire but only 25% of patients showed a reliable improvement in their pain. Treatment changes lasted 1 year.16
A meta-analysis of psychological interventions such as CBT, behavioral treatment (BT), and self-regulated treatment (SRT) indicated that CBT and BT are moderately effective at lowering work-related disability and pain intensity for chronic low back pain alone or with multidisciplinary care and moderately lowered work-related disability. CBT had a moderate to large effect, while SRT with biofeedback and relaxation techniques had a large effect on lowering pain intensity. SRT also was shown to lower depression. Return-to-work rates were better with multidisciplinary care that included psychological interventions. These psychological interventions for chronic low back pain lowered self-reported pain, pain interference, depression, and disability while increasing quality of life; the largest effect was on pain intensity.18
A review by Williams et al19 analyzing the effects of BT and CBT on various outcome measures, including chronic pain, found small to moderate benefits for disability, mood, and catastrophic thinking with CBT, which lasted up to 6 months. Only weak improvements in pain were seen with CBT immediately after treatment. BT had a beneficial effect on catastrophic thinking but only right after treatment. CBT’s overall effect in these patients was positive, and changes lasted up to 6 months.
Pharmacologic treatments
Before and during opioid therapy, psychotherapy, physical therapy, and occupational therapy should be used with adjuvant medications appropriate to the pain condition, such as anticonvulsants (gabapentin, pregabalin, topiramate) and antidepressants including tricyclic antidepressants (amitriptyline, desipramine) and serotonin-norepinephrine reuptake inhibitors (duloxetine, venlafaxine, milnacipran).12 When considering opioids for patients with CNCP/SUD, adverse effects and safety is a primary consideration. Benzodiazepines generally should not be used with opioids because of their synergistic sedating effects.5
Opioids are misused more often by overingestion than by altering the delivery route, yet most efforts to create tamper-resistant medications has focused on
snorting or injection, which are considered more dangerous. Current tamper-resistance strategies include:
• creating a hard shell to prevent crushing and altering the medications
• chemical combinations, using agonists and antagonists such as buprenorphine combined with naloxone
• prodrugs, which become activated only in the GI system
• implants or patches.20,21
One prodrug in phase-I testing, compound PF329, becomes activated only in the GI tract by exposure to trypsin. Because it also contains trypsin inhibitors, overingestion will not lead to toxicity.20 These types of technologies may take years to develop and integrate into our therapeutic armamentarium.
If choosing opioid treatment for patients with CNCP/SUD, initially consider weak opioids such as codeine and tramadol.22 Tramadol, a partial μ agonist and weak inhibitor of serotonin and norepinephrine reuptake, is not a controlled substance and is indicated for moderate to severe pain; however, reports of its abuse potential are beginning to emerge. Tramadol has a frequency of abuse and withdrawal of approximately 2/100,000 patients taking the drug.23
Tapentadol has a dual mechanism of action—it combines a potent opioid agonist with a norepinephrine reuptake inhibitor—and is a schedule II medication. The norepinephrine and serotonin reuptake inhibition properties of tramadol and tapentadol can lead to undesired side effects and are less likely to be abused. Dart et al24 found tapentadol immediate release has the lowest abuse rate of all the opioids they studied, well below oxycodone and hydrocodone.
Methadone is a potent analgesic primarily used to treat opioid addiction, but it also is used for CNCP and cancer pain. With chronic use, methadone lacks the euphoric effect of other μ opioids; however, it can increase the QTc interval and has a long, variable half-life. As a result, methadone conversion tables are considered unreliable.
Methadone also has been associated with a disproportionate number of prescription opioid overdoses and deaths; it is present in 30% of all overdoses treated in emergency departments.4 Although methadone constitutes 5% of all opioid prescriptions in the United States, it is associated with one-third of opioid-related deaths, which is more than heroin and cocaine combined.14 Most methadone deaths occur within the first 7 days of initiating therapy, which suggests that patients were started on too high a dosage, were titrated too quickly, or had overestimated their tolerance.4 Reasons for methadone-related deaths are multifactorial and include:
• physician error and lack of knowledge
• patient nonadherence
• unanticipated comorbidities
• polypharmacy
• obstructive sleep apnea
• third-party payer policies listing it as first tier because of its low cost.4
In a Swedish study of 60 patients taking methadone, 75% had good pain relief on an average dose of 81.5 mg/d, whereas 25% had only moderate pain relief at a higher average dose of 157.5 mg/d. The authors described a methadone syndrome that included sedation, weakness, lethargy, weight gain, sweating, and sexual dysfunction, and that decreased the quality of life in 50% of patients.25 Another study found that among patients who died from sudden cardiac death and had methadone present in the toxicology screen, 45% were taking other psychotropics.26 Researchers also found a synergistic effect with benzodiazepines and an independent risk of sudden cardiac death and recommended obtaining pulmonary function tests and an electrocardiogram before starting methadone therapy, especially at higher doses.
Buprenorphine is a schedule III partial ì agonist opioid with a bell-shaped dose-response curve with a ceiling effect on respiratory depression, making it safe with an overdose. Although it is indicated for opioid dependence maintenance, it has been used off-label to treat chronic pain. It causes less euphoria than many other opioids including methadone. Buprenorphine is 25 to 50 times more potent than morphine and has a half-life of 20 to 44 hours but can be abused.27 It is available as a tablet, an injectable, and a 7-day patch. A combination of buprenorphine and naltrexone has a lower abuse potential,28 is administered sublingually and can be prescribed only by certified physicians.29 A subcutaneous implantable form of buprenorphine, which lasts 6 months, is under FDA review.30
Bottom Line
Multidisciplinary care paired with psychological interventions and a treatment plan has some evidence of efficacy in treating pain in patients with chronic non-cancer pain at high risk of substance abuse. Physician education in both pain and addiction is paramount. Frequent supervision, screening, monitoring and careful selection of medications will help physicians optimize outcomes and reduce risks.
Related Resources
- Agency Medical Directors Group. Intra-agency guideline on opioid dosing for chronic non-cancer pain. http://agencymeddirectors.wa.gov/files/opioidgdline.pdf.
- Stevenson E, Cole J, Walker R, et al. Association of chronic noncancer pain with substance abuse treatment outcomes among a community mental health center sample [published online January 3, 2013]. Addictive Disorders and their Treatment. doi: 10.1097/ADT.0b013e31827b0cd9.
Drug Brand Names
Amitriptyline • Elavil Buprenorphine • Subutex
Buprenorphine/naloxone • Suboxone Codeine • Tylenol with Codeine, others
Desipramine • Norpramin Duloxetine • Cymbalta
Gabapentin • Neurontin Methadone • Dolophine
Milnacipran • Savella Morphine • Roxanol
Oxycodone • Percolone, OxyContin Pregabalin • Lyrica
Tapentadol • Nucynta Topiramate • Topamax
Tramadol • Ultram Venlafaxine • Effexor
Hydrocodone/acetaminophen • Vicodin, Lorcet, others
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgements
The authors thank Zita Juska for her editorial assistance with this article.
Featured Audio
Mark Juska, MD, discusses strategies for treating patients with comorbid pain and substance use disorders. Dr. Juska is a Fellow, Department of Anesthesiology, Wayne State University, Detroit, Michigan.
1. Giordano J. Pain and addiction: words, meanings, actions in the age of DSM-5. Practical Pain Management. http://www.practicalpainmanagement.com/resources/ethics/pain-addiction-words-meanings-actions-age-dsm-5. November 1, 2010. Accessed May 28, 2013.
2. The Joint Commission. Facts about pain management. http://www.jointcommission.org/pain_management. Updated February 27, 2013. Accessed May 28, 2013.
3. Volkow ND, McLellan TA. Curtailing diversion and abuse of opioid analgesics without jeopardizing pain treatment. JAMA. 2011;305(13):1346-1347.
4. Webster LR, Cochella S, Dasgupta N, et al. An analysis of the root causes for opioid-related overdose deaths in the United States. Pain Med. 2011;12(suppl 2):S26-35.
5. Miotto K, Kaufman A, Kong A, et al. Managing co-occurring substance use and pain disorders. Psychiatr Clin North Am. 2012;35(2):393-410.
6. Morasco BJ, Gritzner S, Lewis L, et al. Systematic review of prevention, correlates and treatment outcomes for chronic non-cancer pain in patients with comorbid substance use disorders. Pain. 2011;152:488-497.
7. Edlund MJ, Martin BC, Fan MY, et al. Risks for opioid abuse and dependence among recipients of chronic opioid therapy: results from the TROUP Study. Drug Alcohol Depend. 2010;112(1-2):90-98.
8. Moore TM, Jones T, Browder JH, et al. A comparison of common screening methods for predicting aberrant drug-related behavior among patients receiving opioids for chronic pain management. Pain Med. 2009;10(8):1426-1433.
9. Chou R, Fanciullo GJ, Fine PG, et al. Opioids for chronic non cancer pain: prediction and identification of aberrant drug-related behaviors. A review of the evidence for an American Pain Society and American Academy of Pain Medicine clinical practice guidelines. J Pain. 2009;10(2):131-146.
10. Starrels JL, Becker WC, Alford DP, et al. Systematic review: treatment agreements and urine drug testing to reduce opioid misuse in patients with chronic pain. Ann Intern Med. 2010;152(11):712-720.
11. Morasco BJ, Duckart JP, Dobscha SK. Adherence to clinical guidelines for opioid therapy for chronic pain in patients with substance use disorder. J Gen Intern Med. 2011; 26(9):965-971.
12. Chou R, Fanciullo GJ, Fine PG, et al; American Pain Society-American Academy of Pain Medicine Opioids Guidelines Panel. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):
113-130.
13. Office of National Drug Control Policy. Epidemic: responding to America’s prescription drug abuse crisis. http://www.whitehouse.gov/sites/default/files/ondcp/policy-and-research/rx_abuse_plan.pdf. Accessed May 28, 2013.
14. Kuehn BM. Methadone overdose deaths rise with increased prescribing for pain. JAMA. 2012;308(8):749-750.
15. Gourlay DL, Heit HA, Almahrezi A. Universal precautions in pain medicine: a rational approach to the treatment of chronic pain. Pain Med. 2005;6(2):107-112.
16. Currie SR, Hodgins DC, Crabtree A, et al. Outcome from integrated pain management treatment for recovering substance abusers. J Pain. 2003;4(2):91-100.
17. Morasco BJ, Corson K, Turk DC, et al. Association between substance use disorder status and pain-related function following 12 months of treatment in primary care patients with musculoskeletal pain. J Pain. 2011;12(3):352-359.
18. Hoffman BM, Papas RK, Chatkoff DK, et al. Meta-analysis of psychological interventions for chronic low back pain. Health Psychol. 2007;26(1):1-9.
19. Williams AC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev. 2012;11:CD007407. doi: 10.1002/14651858.CD007407.pub3.
20. Moorman-Li R, Motycka CA, Inge LD, et al. A review of abuse-deterrent opioids for chronic nonmalignant pain. P T. 2012;37(7):412-418.
21. Stanos SP, Bruckenthal P, Barkin RL. Strategies to reduce the tampering and subsequent abuse of long-acting opioids: potential risks and benefits of formulations with physical or pharmacologic deterrents to tampering. Mayo Clinic Proc. 2012;87(7):683-694.
22. Substance Abuse and Mental Health Services Administration. Managing chronic pain in adults with or in recovery from substance use disorders. Treatment Improvement Protocol (TIP) Series 54. HHS Publication No. (SMA) 12-4671. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2011.
23. Senay EC, Adams EH, Geller A, et al. Physical dependence on Ultram (tramadol hydrochloride): both opioid-like and atypical withdrawal symptoms occur. Drug Alcohol Depend. 2003;69:233-241.
24. Dart RC, Cicero TJ, Surratt HL, et al. Assessment of the abuse of tapentadol immediate release: the first 24 months. J Opioid Manag. 2012;8(6):395-402.
25. Rhodin A, Grönbladh L, Nilsson LH, et al. Methadone treatment of chronic non-malignant pain and opioid dependence—a long-term follow-up. Eur J Pain. 2006; 10(3):271-278.
26. Chuh SS, Socoteanu C, Reinier K, et al. A community-based evaluation of sudden death associated with therapeutic levels of methadone. Am J Med. 2008;121(1):66-71.
27. Drug Enforcement Administration. Buprenorphine. http://www.deadiversion.usdoj.gov/drug_chem_info/buprenorphine.pdf. Accessed June 6, 2013.
28. Gordon A, Rashiq S, Moulin DE, et al. Buprenorphine transdermal system for opioid therapy in patients with chronic low back pain. Pain Res Manag. 2010;15(3):169-178.
29. Substance Abuse and Mental Health Administration. Buprenorphine. http://buprenorphine.samhsa.gov/about.html. Accessed May 28, 2013.
30. Ling W, Casadonte P, Bigelow G, et al. Buprenorphine implants for treatment of opioid dependence: a randomized controlled trial. JAMA. 2010;304(14):1576-1583.
Patients with chronic non-cancer pain (CNCP) and a comorbid substance use disorder (SUD) are difficult to treat. There is a lack of high-quality clinical trials to guide management. This article focuses on current research, guidelines, and recommendations to best manage these patients. We present an analysis of recent statistics, patient characteristics, screening methods, as well as a discussion of changes to DSM-5 regarding substance abuse and addiction (Box 1).1
Opioid use and opioid-related overdoses have increased dramatically over the last decade (Box 2).2-5 Opioids are the primary medication used to treat CNCP, but their use in patients with comorbid SUDs is controversial. It is crucial for psychiatrists and other clinicians to know how to best identify, manage, and treat patients with CNCP/SUD.
Risk factors for CNCP/SUD
Evidence regarding the efficacy of screening methods to identify patients with chronic pain who are at high risk for substance misuse is insufficient. Key risk factors for developing chronic pain may include:
• elevated psychological distress
• negative beliefs and expectations about pain
• pain fear and avoidance
• disability
• anger or hostility
• maladaptive coping strategies
• catastrophic behaviors.5
In addition, these individuals may have a spouse who enables the sick role behavior.
Risk factors for developing a SUD related to prescribed opioids include:
• a history of problematic substance use
• sedative-hypnotic use
• positive family history for substance abuse
• legal problems
• heavy tobacco use
• age <50
• major depressive disorder or anxiety.5
In a review of 38 articles, Morasco et al6 found low-grade evidence with mixed results in attempt to find a correlation among sex, depression, anxiety, and tobacco use with CNCP/SUD. Other data suggest that the risk of addiction once opioids have been started increases with long refill periods and opioid morphine equivalents >120 mg.7 A history of childhood sexual abuse also may be a risk factor for chronic pain and addiction.5
Prevalence
The prevalence of opioid abuse among CNCP patients ranges from 3% to 48%; the highest rates are found among patients visiting the emergency room for opioid refills.7 These patients are more likely to exhibit aberrant behavior with their medications and may be prescribed higher opioid doses than patients who have CNCP only. Adherent CNCP/SUD patients show no difference in response to pain treatment compared with those with CNCP alone.6 Approximately 11.5% of CNCP patients taking opioids demonstrate aberrant medication use.6
Screening: Which method is best?
Data are scarce regarding the best screening methods to identify patients with CNCP/SUD. A survey of 48 patients by Moore et al8 found the combination of a clinical interview and the Screener and Opioid Assessment for Patients with Pain-Revised (SOAPP-R) is 90% sensitive in detecting CNCP/SUD. However, a systematic review by Chou et al9 found only 2 well-designed studies showing that the SOAPP-R weakly predicts future aberrant drug behavior and only 1 study showed that a high risk categorization on the Opioid Risk Tool (ORT) strongly increased the likelihood of predicting future abnormal drug-related behavior. Another well-designed study showed that the Current Opioid Misuse Measure (COMM) weakly raised the likelihood of detecting current aberrant drug behavior. No reliable data supported the efficacy of urine drug screens (UDS), pill counts, or prescription drug monitoring programs (PDMPs) for improving clinical outcomes.9 In a systematic review Starrels et al10 found only low-quality evidence supporting the effectiveness of opioid agreement contracts and UDS.
Treatment strategies
Once a patient with CNCP/SUD has been identified, it is important to categorize the severity of his (her) pain and substance use by using the decision tree (Figure) and screening tools such as SOAPP-R, ORT, and COMM. In a Veterans Administration (VA) study, only 35% of patients with an SUD received substance abuse treatment.11 The 2009 American Pain Society/American Academy of Pain Medicine guidelines recommended that opioids should considered for patients with substance abuse, serious aberrant drug-related behaviors, or psychiatric comorbidities only if frequent monitoring and treatment plan and mental health or addiction consultation were in place.12 These guidelines also recommended discontinuing opioids if repeated atypical behavior, substance abuse, diversion, lack of progress, or intolerable side effects occur. Repeated and more serious behaviors require a multidisciplinary team, expert consultation, therapy restructuring, and possibly discontinuation of opioids.12
The U.S. Office of National Drug Control Policy has created a council of federal agencies to spearhead the Prescription Drug Abuse Prevention Plan, which includes 4 major categories to reduce prescription drug abuse: education, monitoring, proper disposal, and enforcement.13 FDA commissioner Margaret Hamburg supports legislation to combine opioid education with Drug Enforcement Administration registration.14 The FDA began developing the risk evaluation and mitigation strategies in 2007 to educate physicians on proper prescribing of potentially dangerous medications.
Gourlay and Heit proposed a universal precautions method of opioid treatment for all pain patients.15 That includes:
• seeking differential diagnoses and comorbidities
• doing a baseline addiction assessment with UDS and PDMP evaluations
• obtaining informed consent for pain management
• creating pre- and post-treatment goals for pain and function
• evaluating the 4 “As” (analgesic response, increased activity, adverse events, and aberrant behavior)
• reviewing the evolution of the pain and comorbidities
• continuous documentation.5
Other helpful strategies include the Oregon’s SMART (Specific, Measurable, Action-oriented, Realistic, Time-Dependent) goal-setting, which helps physicians negotiate functional goals with patients and plan an exit strategy for those whose quality of life does not improve with opioids.5 Clinicians also can consider a sequential treatment model where patients with severe substance abuse and pain are detoxified of illicit drugs and alcohol before starting pain management. This approach is more effective if the pain is secondary to a more severe substance abuse problem that is not correlated to physical pain and acute rather than chronic.16
Psychotherapeutic interventions
In another VA study, a collaborative care intervention (CCI) combining education, self-efficacy, pain management, and feedback was not impeded by a history of SUD. The authors recommended CCI, stepped care, integrated interventions, and relapse prevention and stressed the importance of social support.17
A 10-week cognitive-behavioral therapy (CBT) program involving 44 patients enrolled in an integrated pain management program for recovering substance abusers found 50% of CNCP/SUD patients were opioid-free at 12 months.16 A combination of medication reduction and education resulted in less pain, increased functioning, decreased emotional distress, and less self-medicating. Additionally, patients reported 35% overall reduction in pain severity based on the McGill Pain Questionnaire but only 25% of patients showed a reliable improvement in their pain. Treatment changes lasted 1 year.16
A meta-analysis of psychological interventions such as CBT, behavioral treatment (BT), and self-regulated treatment (SRT) indicated that CBT and BT are moderately effective at lowering work-related disability and pain intensity for chronic low back pain alone or with multidisciplinary care and moderately lowered work-related disability. CBT had a moderate to large effect, while SRT with biofeedback and relaxation techniques had a large effect on lowering pain intensity. SRT also was shown to lower depression. Return-to-work rates were better with multidisciplinary care that included psychological interventions. These psychological interventions for chronic low back pain lowered self-reported pain, pain interference, depression, and disability while increasing quality of life; the largest effect was on pain intensity.18
A review by Williams et al19 analyzing the effects of BT and CBT on various outcome measures, including chronic pain, found small to moderate benefits for disability, mood, and catastrophic thinking with CBT, which lasted up to 6 months. Only weak improvements in pain were seen with CBT immediately after treatment. BT had a beneficial effect on catastrophic thinking but only right after treatment. CBT’s overall effect in these patients was positive, and changes lasted up to 6 months.
Pharmacologic treatments
Before and during opioid therapy, psychotherapy, physical therapy, and occupational therapy should be used with adjuvant medications appropriate to the pain condition, such as anticonvulsants (gabapentin, pregabalin, topiramate) and antidepressants including tricyclic antidepressants (amitriptyline, desipramine) and serotonin-norepinephrine reuptake inhibitors (duloxetine, venlafaxine, milnacipran).12 When considering opioids for patients with CNCP/SUD, adverse effects and safety is a primary consideration. Benzodiazepines generally should not be used with opioids because of their synergistic sedating effects.5
Opioids are misused more often by overingestion than by altering the delivery route, yet most efforts to create tamper-resistant medications has focused on
snorting or injection, which are considered more dangerous. Current tamper-resistance strategies include:
• creating a hard shell to prevent crushing and altering the medications
• chemical combinations, using agonists and antagonists such as buprenorphine combined with naloxone
• prodrugs, which become activated only in the GI system
• implants or patches.20,21
One prodrug in phase-I testing, compound PF329, becomes activated only in the GI tract by exposure to trypsin. Because it also contains trypsin inhibitors, overingestion will not lead to toxicity.20 These types of technologies may take years to develop and integrate into our therapeutic armamentarium.
If choosing opioid treatment for patients with CNCP/SUD, initially consider weak opioids such as codeine and tramadol.22 Tramadol, a partial μ agonist and weak inhibitor of serotonin and norepinephrine reuptake, is not a controlled substance and is indicated for moderate to severe pain; however, reports of its abuse potential are beginning to emerge. Tramadol has a frequency of abuse and withdrawal of approximately 2/100,000 patients taking the drug.23
Tapentadol has a dual mechanism of action—it combines a potent opioid agonist with a norepinephrine reuptake inhibitor—and is a schedule II medication. The norepinephrine and serotonin reuptake inhibition properties of tramadol and tapentadol can lead to undesired side effects and are less likely to be abused. Dart et al24 found tapentadol immediate release has the lowest abuse rate of all the opioids they studied, well below oxycodone and hydrocodone.
Methadone is a potent analgesic primarily used to treat opioid addiction, but it also is used for CNCP and cancer pain. With chronic use, methadone lacks the euphoric effect of other μ opioids; however, it can increase the QTc interval and has a long, variable half-life. As a result, methadone conversion tables are considered unreliable.
Methadone also has been associated with a disproportionate number of prescription opioid overdoses and deaths; it is present in 30% of all overdoses treated in emergency departments.4 Although methadone constitutes 5% of all opioid prescriptions in the United States, it is associated with one-third of opioid-related deaths, which is more than heroin and cocaine combined.14 Most methadone deaths occur within the first 7 days of initiating therapy, which suggests that patients were started on too high a dosage, were titrated too quickly, or had overestimated their tolerance.4 Reasons for methadone-related deaths are multifactorial and include:
• physician error and lack of knowledge
• patient nonadherence
• unanticipated comorbidities
• polypharmacy
• obstructive sleep apnea
• third-party payer policies listing it as first tier because of its low cost.4
In a Swedish study of 60 patients taking methadone, 75% had good pain relief on an average dose of 81.5 mg/d, whereas 25% had only moderate pain relief at a higher average dose of 157.5 mg/d. The authors described a methadone syndrome that included sedation, weakness, lethargy, weight gain, sweating, and sexual dysfunction, and that decreased the quality of life in 50% of patients.25 Another study found that among patients who died from sudden cardiac death and had methadone present in the toxicology screen, 45% were taking other psychotropics.26 Researchers also found a synergistic effect with benzodiazepines and an independent risk of sudden cardiac death and recommended obtaining pulmonary function tests and an electrocardiogram before starting methadone therapy, especially at higher doses.
Buprenorphine is a schedule III partial ì agonist opioid with a bell-shaped dose-response curve with a ceiling effect on respiratory depression, making it safe with an overdose. Although it is indicated for opioid dependence maintenance, it has been used off-label to treat chronic pain. It causes less euphoria than many other opioids including methadone. Buprenorphine is 25 to 50 times more potent than morphine and has a half-life of 20 to 44 hours but can be abused.27 It is available as a tablet, an injectable, and a 7-day patch. A combination of buprenorphine and naltrexone has a lower abuse potential,28 is administered sublingually and can be prescribed only by certified physicians.29 A subcutaneous implantable form of buprenorphine, which lasts 6 months, is under FDA review.30
Bottom Line
Multidisciplinary care paired with psychological interventions and a treatment plan has some evidence of efficacy in treating pain in patients with chronic non-cancer pain at high risk of substance abuse. Physician education in both pain and addiction is paramount. Frequent supervision, screening, monitoring and careful selection of medications will help physicians optimize outcomes and reduce risks.
Related Resources
- Agency Medical Directors Group. Intra-agency guideline on opioid dosing for chronic non-cancer pain. http://agencymeddirectors.wa.gov/files/opioidgdline.pdf.
- Stevenson E, Cole J, Walker R, et al. Association of chronic noncancer pain with substance abuse treatment outcomes among a community mental health center sample [published online January 3, 2013]. Addictive Disorders and their Treatment. doi: 10.1097/ADT.0b013e31827b0cd9.
Drug Brand Names
Amitriptyline • Elavil Buprenorphine • Subutex
Buprenorphine/naloxone • Suboxone Codeine • Tylenol with Codeine, others
Desipramine • Norpramin Duloxetine • Cymbalta
Gabapentin • Neurontin Methadone • Dolophine
Milnacipran • Savella Morphine • Roxanol
Oxycodone • Percolone, OxyContin Pregabalin • Lyrica
Tapentadol • Nucynta Topiramate • Topamax
Tramadol • Ultram Venlafaxine • Effexor
Hydrocodone/acetaminophen • Vicodin, Lorcet, others
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgements
The authors thank Zita Juska for her editorial assistance with this article.
Featured Audio
Mark Juska, MD, discusses strategies for treating patients with comorbid pain and substance use disorders. Dr. Juska is a Fellow, Department of Anesthesiology, Wayne State University, Detroit, Michigan.
Patients with chronic non-cancer pain (CNCP) and a comorbid substance use disorder (SUD) are difficult to treat. There is a lack of high-quality clinical trials to guide management. This article focuses on current research, guidelines, and recommendations to best manage these patients. We present an analysis of recent statistics, patient characteristics, screening methods, as well as a discussion of changes to DSM-5 regarding substance abuse and addiction (Box 1).1
Opioid use and opioid-related overdoses have increased dramatically over the last decade (Box 2).2-5 Opioids are the primary medication used to treat CNCP, but their use in patients with comorbid SUDs is controversial. It is crucial for psychiatrists and other clinicians to know how to best identify, manage, and treat patients with CNCP/SUD.
Risk factors for CNCP/SUD
Evidence regarding the efficacy of screening methods to identify patients with chronic pain who are at high risk for substance misuse is insufficient. Key risk factors for developing chronic pain may include:
• elevated psychological distress
• negative beliefs and expectations about pain
• pain fear and avoidance
• disability
• anger or hostility
• maladaptive coping strategies
• catastrophic behaviors.5
In addition, these individuals may have a spouse who enables the sick role behavior.
Risk factors for developing a SUD related to prescribed opioids include:
• a history of problematic substance use
• sedative-hypnotic use
• positive family history for substance abuse
• legal problems
• heavy tobacco use
• age <50
• major depressive disorder or anxiety.5
In a review of 38 articles, Morasco et al6 found low-grade evidence with mixed results in attempt to find a correlation among sex, depression, anxiety, and tobacco use with CNCP/SUD. Other data suggest that the risk of addiction once opioids have been started increases with long refill periods and opioid morphine equivalents >120 mg.7 A history of childhood sexual abuse also may be a risk factor for chronic pain and addiction.5
Prevalence
The prevalence of opioid abuse among CNCP patients ranges from 3% to 48%; the highest rates are found among patients visiting the emergency room for opioid refills.7 These patients are more likely to exhibit aberrant behavior with their medications and may be prescribed higher opioid doses than patients who have CNCP only. Adherent CNCP/SUD patients show no difference in response to pain treatment compared with those with CNCP alone.6 Approximately 11.5% of CNCP patients taking opioids demonstrate aberrant medication use.6
Screening: Which method is best?
Data are scarce regarding the best screening methods to identify patients with CNCP/SUD. A survey of 48 patients by Moore et al8 found the combination of a clinical interview and the Screener and Opioid Assessment for Patients with Pain-Revised (SOAPP-R) is 90% sensitive in detecting CNCP/SUD. However, a systematic review by Chou et al9 found only 2 well-designed studies showing that the SOAPP-R weakly predicts future aberrant drug behavior and only 1 study showed that a high risk categorization on the Opioid Risk Tool (ORT) strongly increased the likelihood of predicting future abnormal drug-related behavior. Another well-designed study showed that the Current Opioid Misuse Measure (COMM) weakly raised the likelihood of detecting current aberrant drug behavior. No reliable data supported the efficacy of urine drug screens (UDS), pill counts, or prescription drug monitoring programs (PDMPs) for improving clinical outcomes.9 In a systematic review Starrels et al10 found only low-quality evidence supporting the effectiveness of opioid agreement contracts and UDS.
Treatment strategies
Once a patient with CNCP/SUD has been identified, it is important to categorize the severity of his (her) pain and substance use by using the decision tree (Figure) and screening tools such as SOAPP-R, ORT, and COMM. In a Veterans Administration (VA) study, only 35% of patients with an SUD received substance abuse treatment.11 The 2009 American Pain Society/American Academy of Pain Medicine guidelines recommended that opioids should considered for patients with substance abuse, serious aberrant drug-related behaviors, or psychiatric comorbidities only if frequent monitoring and treatment plan and mental health or addiction consultation were in place.12 These guidelines also recommended discontinuing opioids if repeated atypical behavior, substance abuse, diversion, lack of progress, or intolerable side effects occur. Repeated and more serious behaviors require a multidisciplinary team, expert consultation, therapy restructuring, and possibly discontinuation of opioids.12
The U.S. Office of National Drug Control Policy has created a council of federal agencies to spearhead the Prescription Drug Abuse Prevention Plan, which includes 4 major categories to reduce prescription drug abuse: education, monitoring, proper disposal, and enforcement.13 FDA commissioner Margaret Hamburg supports legislation to combine opioid education with Drug Enforcement Administration registration.14 The FDA began developing the risk evaluation and mitigation strategies in 2007 to educate physicians on proper prescribing of potentially dangerous medications.
Gourlay and Heit proposed a universal precautions method of opioid treatment for all pain patients.15 That includes:
• seeking differential diagnoses and comorbidities
• doing a baseline addiction assessment with UDS and PDMP evaluations
• obtaining informed consent for pain management
• creating pre- and post-treatment goals for pain and function
• evaluating the 4 “As” (analgesic response, increased activity, adverse events, and aberrant behavior)
• reviewing the evolution of the pain and comorbidities
• continuous documentation.5
Other helpful strategies include the Oregon’s SMART (Specific, Measurable, Action-oriented, Realistic, Time-Dependent) goal-setting, which helps physicians negotiate functional goals with patients and plan an exit strategy for those whose quality of life does not improve with opioids.5 Clinicians also can consider a sequential treatment model where patients with severe substance abuse and pain are detoxified of illicit drugs and alcohol before starting pain management. This approach is more effective if the pain is secondary to a more severe substance abuse problem that is not correlated to physical pain and acute rather than chronic.16
Psychotherapeutic interventions
In another VA study, a collaborative care intervention (CCI) combining education, self-efficacy, pain management, and feedback was not impeded by a history of SUD. The authors recommended CCI, stepped care, integrated interventions, and relapse prevention and stressed the importance of social support.17
A 10-week cognitive-behavioral therapy (CBT) program involving 44 patients enrolled in an integrated pain management program for recovering substance abusers found 50% of CNCP/SUD patients were opioid-free at 12 months.16 A combination of medication reduction and education resulted in less pain, increased functioning, decreased emotional distress, and less self-medicating. Additionally, patients reported 35% overall reduction in pain severity based on the McGill Pain Questionnaire but only 25% of patients showed a reliable improvement in their pain. Treatment changes lasted 1 year.16
A meta-analysis of psychological interventions such as CBT, behavioral treatment (BT), and self-regulated treatment (SRT) indicated that CBT and BT are moderately effective at lowering work-related disability and pain intensity for chronic low back pain alone or with multidisciplinary care and moderately lowered work-related disability. CBT had a moderate to large effect, while SRT with biofeedback and relaxation techniques had a large effect on lowering pain intensity. SRT also was shown to lower depression. Return-to-work rates were better with multidisciplinary care that included psychological interventions. These psychological interventions for chronic low back pain lowered self-reported pain, pain interference, depression, and disability while increasing quality of life; the largest effect was on pain intensity.18
A review by Williams et al19 analyzing the effects of BT and CBT on various outcome measures, including chronic pain, found small to moderate benefits for disability, mood, and catastrophic thinking with CBT, which lasted up to 6 months. Only weak improvements in pain were seen with CBT immediately after treatment. BT had a beneficial effect on catastrophic thinking but only right after treatment. CBT’s overall effect in these patients was positive, and changes lasted up to 6 months.
Pharmacologic treatments
Before and during opioid therapy, psychotherapy, physical therapy, and occupational therapy should be used with adjuvant medications appropriate to the pain condition, such as anticonvulsants (gabapentin, pregabalin, topiramate) and antidepressants including tricyclic antidepressants (amitriptyline, desipramine) and serotonin-norepinephrine reuptake inhibitors (duloxetine, venlafaxine, milnacipran).12 When considering opioids for patients with CNCP/SUD, adverse effects and safety is a primary consideration. Benzodiazepines generally should not be used with opioids because of their synergistic sedating effects.5
Opioids are misused more often by overingestion than by altering the delivery route, yet most efforts to create tamper-resistant medications has focused on
snorting or injection, which are considered more dangerous. Current tamper-resistance strategies include:
• creating a hard shell to prevent crushing and altering the medications
• chemical combinations, using agonists and antagonists such as buprenorphine combined with naloxone
• prodrugs, which become activated only in the GI system
• implants or patches.20,21
One prodrug in phase-I testing, compound PF329, becomes activated only in the GI tract by exposure to trypsin. Because it also contains trypsin inhibitors, overingestion will not lead to toxicity.20 These types of technologies may take years to develop and integrate into our therapeutic armamentarium.
If choosing opioid treatment for patients with CNCP/SUD, initially consider weak opioids such as codeine and tramadol.22 Tramadol, a partial μ agonist and weak inhibitor of serotonin and norepinephrine reuptake, is not a controlled substance and is indicated for moderate to severe pain; however, reports of its abuse potential are beginning to emerge. Tramadol has a frequency of abuse and withdrawal of approximately 2/100,000 patients taking the drug.23
Tapentadol has a dual mechanism of action—it combines a potent opioid agonist with a norepinephrine reuptake inhibitor—and is a schedule II medication. The norepinephrine and serotonin reuptake inhibition properties of tramadol and tapentadol can lead to undesired side effects and are less likely to be abused. Dart et al24 found tapentadol immediate release has the lowest abuse rate of all the opioids they studied, well below oxycodone and hydrocodone.
Methadone is a potent analgesic primarily used to treat opioid addiction, but it also is used for CNCP and cancer pain. With chronic use, methadone lacks the euphoric effect of other μ opioids; however, it can increase the QTc interval and has a long, variable half-life. As a result, methadone conversion tables are considered unreliable.
Methadone also has been associated with a disproportionate number of prescription opioid overdoses and deaths; it is present in 30% of all overdoses treated in emergency departments.4 Although methadone constitutes 5% of all opioid prescriptions in the United States, it is associated with one-third of opioid-related deaths, which is more than heroin and cocaine combined.14 Most methadone deaths occur within the first 7 days of initiating therapy, which suggests that patients were started on too high a dosage, were titrated too quickly, or had overestimated their tolerance.4 Reasons for methadone-related deaths are multifactorial and include:
• physician error and lack of knowledge
• patient nonadherence
• unanticipated comorbidities
• polypharmacy
• obstructive sleep apnea
• third-party payer policies listing it as first tier because of its low cost.4
In a Swedish study of 60 patients taking methadone, 75% had good pain relief on an average dose of 81.5 mg/d, whereas 25% had only moderate pain relief at a higher average dose of 157.5 mg/d. The authors described a methadone syndrome that included sedation, weakness, lethargy, weight gain, sweating, and sexual dysfunction, and that decreased the quality of life in 50% of patients.25 Another study found that among patients who died from sudden cardiac death and had methadone present in the toxicology screen, 45% were taking other psychotropics.26 Researchers also found a synergistic effect with benzodiazepines and an independent risk of sudden cardiac death and recommended obtaining pulmonary function tests and an electrocardiogram before starting methadone therapy, especially at higher doses.
Buprenorphine is a schedule III partial ì agonist opioid with a bell-shaped dose-response curve with a ceiling effect on respiratory depression, making it safe with an overdose. Although it is indicated for opioid dependence maintenance, it has been used off-label to treat chronic pain. It causes less euphoria than many other opioids including methadone. Buprenorphine is 25 to 50 times more potent than morphine and has a half-life of 20 to 44 hours but can be abused.27 It is available as a tablet, an injectable, and a 7-day patch. A combination of buprenorphine and naltrexone has a lower abuse potential,28 is administered sublingually and can be prescribed only by certified physicians.29 A subcutaneous implantable form of buprenorphine, which lasts 6 months, is under FDA review.30
Bottom Line
Multidisciplinary care paired with psychological interventions and a treatment plan has some evidence of efficacy in treating pain in patients with chronic non-cancer pain at high risk of substance abuse. Physician education in both pain and addiction is paramount. Frequent supervision, screening, monitoring and careful selection of medications will help physicians optimize outcomes and reduce risks.
Related Resources
- Agency Medical Directors Group. Intra-agency guideline on opioid dosing for chronic non-cancer pain. http://agencymeddirectors.wa.gov/files/opioidgdline.pdf.
- Stevenson E, Cole J, Walker R, et al. Association of chronic noncancer pain with substance abuse treatment outcomes among a community mental health center sample [published online January 3, 2013]. Addictive Disorders and their Treatment. doi: 10.1097/ADT.0b013e31827b0cd9.
Drug Brand Names
Amitriptyline • Elavil Buprenorphine • Subutex
Buprenorphine/naloxone • Suboxone Codeine • Tylenol with Codeine, others
Desipramine • Norpramin Duloxetine • Cymbalta
Gabapentin • Neurontin Methadone • Dolophine
Milnacipran • Savella Morphine • Roxanol
Oxycodone • Percolone, OxyContin Pregabalin • Lyrica
Tapentadol • Nucynta Topiramate • Topamax
Tramadol • Ultram Venlafaxine • Effexor
Hydrocodone/acetaminophen • Vicodin, Lorcet, others
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgements
The authors thank Zita Juska for her editorial assistance with this article.
Featured Audio
Mark Juska, MD, discusses strategies for treating patients with comorbid pain and substance use disorders. Dr. Juska is a Fellow, Department of Anesthesiology, Wayne State University, Detroit, Michigan.
1. Giordano J. Pain and addiction: words, meanings, actions in the age of DSM-5. Practical Pain Management. http://www.practicalpainmanagement.com/resources/ethics/pain-addiction-words-meanings-actions-age-dsm-5. November 1, 2010. Accessed May 28, 2013.
2. The Joint Commission. Facts about pain management. http://www.jointcommission.org/pain_management. Updated February 27, 2013. Accessed May 28, 2013.
3. Volkow ND, McLellan TA. Curtailing diversion and abuse of opioid analgesics without jeopardizing pain treatment. JAMA. 2011;305(13):1346-1347.
4. Webster LR, Cochella S, Dasgupta N, et al. An analysis of the root causes for opioid-related overdose deaths in the United States. Pain Med. 2011;12(suppl 2):S26-35.
5. Miotto K, Kaufman A, Kong A, et al. Managing co-occurring substance use and pain disorders. Psychiatr Clin North Am. 2012;35(2):393-410.
6. Morasco BJ, Gritzner S, Lewis L, et al. Systematic review of prevention, correlates and treatment outcomes for chronic non-cancer pain in patients with comorbid substance use disorders. Pain. 2011;152:488-497.
7. Edlund MJ, Martin BC, Fan MY, et al. Risks for opioid abuse and dependence among recipients of chronic opioid therapy: results from the TROUP Study. Drug Alcohol Depend. 2010;112(1-2):90-98.
8. Moore TM, Jones T, Browder JH, et al. A comparison of common screening methods for predicting aberrant drug-related behavior among patients receiving opioids for chronic pain management. Pain Med. 2009;10(8):1426-1433.
9. Chou R, Fanciullo GJ, Fine PG, et al. Opioids for chronic non cancer pain: prediction and identification of aberrant drug-related behaviors. A review of the evidence for an American Pain Society and American Academy of Pain Medicine clinical practice guidelines. J Pain. 2009;10(2):131-146.
10. Starrels JL, Becker WC, Alford DP, et al. Systematic review: treatment agreements and urine drug testing to reduce opioid misuse in patients with chronic pain. Ann Intern Med. 2010;152(11):712-720.
11. Morasco BJ, Duckart JP, Dobscha SK. Adherence to clinical guidelines for opioid therapy for chronic pain in patients with substance use disorder. J Gen Intern Med. 2011; 26(9):965-971.
12. Chou R, Fanciullo GJ, Fine PG, et al; American Pain Society-American Academy of Pain Medicine Opioids Guidelines Panel. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):
113-130.
13. Office of National Drug Control Policy. Epidemic: responding to America’s prescription drug abuse crisis. http://www.whitehouse.gov/sites/default/files/ondcp/policy-and-research/rx_abuse_plan.pdf. Accessed May 28, 2013.
14. Kuehn BM. Methadone overdose deaths rise with increased prescribing for pain. JAMA. 2012;308(8):749-750.
15. Gourlay DL, Heit HA, Almahrezi A. Universal precautions in pain medicine: a rational approach to the treatment of chronic pain. Pain Med. 2005;6(2):107-112.
16. Currie SR, Hodgins DC, Crabtree A, et al. Outcome from integrated pain management treatment for recovering substance abusers. J Pain. 2003;4(2):91-100.
17. Morasco BJ, Corson K, Turk DC, et al. Association between substance use disorder status and pain-related function following 12 months of treatment in primary care patients with musculoskeletal pain. J Pain. 2011;12(3):352-359.
18. Hoffman BM, Papas RK, Chatkoff DK, et al. Meta-analysis of psychological interventions for chronic low back pain. Health Psychol. 2007;26(1):1-9.
19. Williams AC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev. 2012;11:CD007407. doi: 10.1002/14651858.CD007407.pub3.
20. Moorman-Li R, Motycka CA, Inge LD, et al. A review of abuse-deterrent opioids for chronic nonmalignant pain. P T. 2012;37(7):412-418.
21. Stanos SP, Bruckenthal P, Barkin RL. Strategies to reduce the tampering and subsequent abuse of long-acting opioids: potential risks and benefits of formulations with physical or pharmacologic deterrents to tampering. Mayo Clinic Proc. 2012;87(7):683-694.
22. Substance Abuse and Mental Health Services Administration. Managing chronic pain in adults with or in recovery from substance use disorders. Treatment Improvement Protocol (TIP) Series 54. HHS Publication No. (SMA) 12-4671. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2011.
23. Senay EC, Adams EH, Geller A, et al. Physical dependence on Ultram (tramadol hydrochloride): both opioid-like and atypical withdrawal symptoms occur. Drug Alcohol Depend. 2003;69:233-241.
24. Dart RC, Cicero TJ, Surratt HL, et al. Assessment of the abuse of tapentadol immediate release: the first 24 months. J Opioid Manag. 2012;8(6):395-402.
25. Rhodin A, Grönbladh L, Nilsson LH, et al. Methadone treatment of chronic non-malignant pain and opioid dependence—a long-term follow-up. Eur J Pain. 2006; 10(3):271-278.
26. Chuh SS, Socoteanu C, Reinier K, et al. A community-based evaluation of sudden death associated with therapeutic levels of methadone. Am J Med. 2008;121(1):66-71.
27. Drug Enforcement Administration. Buprenorphine. http://www.deadiversion.usdoj.gov/drug_chem_info/buprenorphine.pdf. Accessed June 6, 2013.
28. Gordon A, Rashiq S, Moulin DE, et al. Buprenorphine transdermal system for opioid therapy in patients with chronic low back pain. Pain Res Manag. 2010;15(3):169-178.
29. Substance Abuse and Mental Health Administration. Buprenorphine. http://buprenorphine.samhsa.gov/about.html. Accessed May 28, 2013.
30. Ling W, Casadonte P, Bigelow G, et al. Buprenorphine implants for treatment of opioid dependence: a randomized controlled trial. JAMA. 2010;304(14):1576-1583.
1. Giordano J. Pain and addiction: words, meanings, actions in the age of DSM-5. Practical Pain Management. http://www.practicalpainmanagement.com/resources/ethics/pain-addiction-words-meanings-actions-age-dsm-5. November 1, 2010. Accessed May 28, 2013.
2. The Joint Commission. Facts about pain management. http://www.jointcommission.org/pain_management. Updated February 27, 2013. Accessed May 28, 2013.
3. Volkow ND, McLellan TA. Curtailing diversion and abuse of opioid analgesics without jeopardizing pain treatment. JAMA. 2011;305(13):1346-1347.
4. Webster LR, Cochella S, Dasgupta N, et al. An analysis of the root causes for opioid-related overdose deaths in the United States. Pain Med. 2011;12(suppl 2):S26-35.
5. Miotto K, Kaufman A, Kong A, et al. Managing co-occurring substance use and pain disorders. Psychiatr Clin North Am. 2012;35(2):393-410.
6. Morasco BJ, Gritzner S, Lewis L, et al. Systematic review of prevention, correlates and treatment outcomes for chronic non-cancer pain in patients with comorbid substance use disorders. Pain. 2011;152:488-497.
7. Edlund MJ, Martin BC, Fan MY, et al. Risks for opioid abuse and dependence among recipients of chronic opioid therapy: results from the TROUP Study. Drug Alcohol Depend. 2010;112(1-2):90-98.
8. Moore TM, Jones T, Browder JH, et al. A comparison of common screening methods for predicting aberrant drug-related behavior among patients receiving opioids for chronic pain management. Pain Med. 2009;10(8):1426-1433.
9. Chou R, Fanciullo GJ, Fine PG, et al. Opioids for chronic non cancer pain: prediction and identification of aberrant drug-related behaviors. A review of the evidence for an American Pain Society and American Academy of Pain Medicine clinical practice guidelines. J Pain. 2009;10(2):131-146.
10. Starrels JL, Becker WC, Alford DP, et al. Systematic review: treatment agreements and urine drug testing to reduce opioid misuse in patients with chronic pain. Ann Intern Med. 2010;152(11):712-720.
11. Morasco BJ, Duckart JP, Dobscha SK. Adherence to clinical guidelines for opioid therapy for chronic pain in patients with substance use disorder. J Gen Intern Med. 2011; 26(9):965-971.
12. Chou R, Fanciullo GJ, Fine PG, et al; American Pain Society-American Academy of Pain Medicine Opioids Guidelines Panel. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):
113-130.
13. Office of National Drug Control Policy. Epidemic: responding to America’s prescription drug abuse crisis. http://www.whitehouse.gov/sites/default/files/ondcp/policy-and-research/rx_abuse_plan.pdf. Accessed May 28, 2013.
14. Kuehn BM. Methadone overdose deaths rise with increased prescribing for pain. JAMA. 2012;308(8):749-750.
15. Gourlay DL, Heit HA, Almahrezi A. Universal precautions in pain medicine: a rational approach to the treatment of chronic pain. Pain Med. 2005;6(2):107-112.
16. Currie SR, Hodgins DC, Crabtree A, et al. Outcome from integrated pain management treatment for recovering substance abusers. J Pain. 2003;4(2):91-100.
17. Morasco BJ, Corson K, Turk DC, et al. Association between substance use disorder status and pain-related function following 12 months of treatment in primary care patients with musculoskeletal pain. J Pain. 2011;12(3):352-359.
18. Hoffman BM, Papas RK, Chatkoff DK, et al. Meta-analysis of psychological interventions for chronic low back pain. Health Psychol. 2007;26(1):1-9.
19. Williams AC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev. 2012;11:CD007407. doi: 10.1002/14651858.CD007407.pub3.
20. Moorman-Li R, Motycka CA, Inge LD, et al. A review of abuse-deterrent opioids for chronic nonmalignant pain. P T. 2012;37(7):412-418.
21. Stanos SP, Bruckenthal P, Barkin RL. Strategies to reduce the tampering and subsequent abuse of long-acting opioids: potential risks and benefits of formulations with physical or pharmacologic deterrents to tampering. Mayo Clinic Proc. 2012;87(7):683-694.
22. Substance Abuse and Mental Health Services Administration. Managing chronic pain in adults with or in recovery from substance use disorders. Treatment Improvement Protocol (TIP) Series 54. HHS Publication No. (SMA) 12-4671. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2011.
23. Senay EC, Adams EH, Geller A, et al. Physical dependence on Ultram (tramadol hydrochloride): both opioid-like and atypical withdrawal symptoms occur. Drug Alcohol Depend. 2003;69:233-241.
24. Dart RC, Cicero TJ, Surratt HL, et al. Assessment of the abuse of tapentadol immediate release: the first 24 months. J Opioid Manag. 2012;8(6):395-402.
25. Rhodin A, Grönbladh L, Nilsson LH, et al. Methadone treatment of chronic non-malignant pain and opioid dependence—a long-term follow-up. Eur J Pain. 2006; 10(3):271-278.
26. Chuh SS, Socoteanu C, Reinier K, et al. A community-based evaluation of sudden death associated with therapeutic levels of methadone. Am J Med. 2008;121(1):66-71.
27. Drug Enforcement Administration. Buprenorphine. http://www.deadiversion.usdoj.gov/drug_chem_info/buprenorphine.pdf. Accessed June 6, 2013.
28. Gordon A, Rashiq S, Moulin DE, et al. Buprenorphine transdermal system for opioid therapy in patients with chronic low back pain. Pain Res Manag. 2010;15(3):169-178.
29. Substance Abuse and Mental Health Administration. Buprenorphine. http://buprenorphine.samhsa.gov/about.html. Accessed May 28, 2013.
30. Ling W, Casadonte P, Bigelow G, et al. Buprenorphine implants for treatment of opioid dependence: a randomized controlled trial. JAMA. 2010;304(14):1576-1583.