User login
The VHA has about 700 community-based outpatient clinics (CBOCs). Often these remote clinics lack onsite specialty services. In 2014, about 3 million of the 9 million veterans in the VHA were enrolled in rural locations, according to the VHA Support Service Center Office of Rural Health. This rural cohort is a substantial veteran population for whom meeting specialty medical care needs can be challenging. Rural veterans often travel long distances to a hub medical center when accessing specialty care. This article describes the North Florida/South Georgia Veterans Health System (NF/SGVHS) telehealth solution to provide veteran-centric specialty care access for rural veterans. The program addresses falls, a major public health problem in the elderly.
The VA is a world leader in clinical video telehealth (CVT). Videoconferencing between clinic sites allows clinicians to make diagnoses and provide and manage care without requiring long distance travel. Clinical video telehelth allows veterans to come to the CBOC, connect to a specialist in a remote VA hospital for consultation and treatment, and save transportation time and related costs. The VA has real-time CVT for polytrauma, mental health, rehabilitation, surgery, weight loss, and numerous other specialties.1,2 The CVT rehabilitation modalities have been successfully used both within the VA and in the community for about 15 years, although rigorous economic and functional outcome data are limited.3-6
Gait and Balance Clinic
The NF/SGVHS spans 50 counties and is one of the VA’s largest health systems for clinical workload and rural geography. In 2014, NF/SGVHS had about 160,000 enrolled veterans, and nearly 70,000 were rural, a slightly higher percentage than the VA nationally.
The Gait and Balance Clinic of the Malcom Randall VAMC in Gainesville, Florida, focuses on evaluating and preventing falls and fall-related injuries in the aging veteran population for all enrolled veterans regardless of location. The NF/SGVHS has a robust CVT program, and in 2014, the physical therapist (PT) initiated a CVT Gait and Balance Clinic pilot. This program increased veteran access from remote clinics to these fall prevention services at NF/SGVHS and positively impacted travel time and related costs.
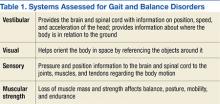
Clinicians refer veterans with falls, dizziness, and vestibular and gait disorders to the Malcom Randall VAMC Gait and Balance Clinic where specially trained PTs provide expert diagnosis and management. The Gait and Balance Clinic is staffed by 2 vestibular-trained PTs and a health technician. The assessments include sophisticated, specialized testing of balance function, determining biologic systems affecting balance. These include the vestibular, visual, sensory, and musculoskeletal systems (Table 1). Therapists provide customized veteran and caregiver education for in-home vestibular exercise programs, fall-reduction strategies, and as-needed adaptive equipment.
Veterans requiring in-depth evaluation attend a weekly Gainesville-based multidisciplinary clinic, staffed by a part-time neurologist, neurology resident trainees, a geriatric medicine fellow, and pharmacy residents and preceptor. Factors affecting gait and balance systems that potentially improve with exercise, such as muscle weakness or vestibular impairments, are mitigated by incorporating into the veteran’s care plan personalized home fall-reduction strategies, exercise programs, and patient and caregiver education.
Specific exercises are designed for each patient’s home environment. The home exercise programs typically include a combination of balance and strength training, vestibular maneuvers, and progressive walking for endurance. In addition to improving patients’ functioning by addressing impairments found on examination, the PTs commonly prescribe assistive devices: rollator walkers, canes, and lower extremity orthoses that reduce fall risk by compensating for deficits in sensory motor systems.The Gait and Balance Clinic receives more than 400 consults annually and experiences a yearly consult growth rate between 2% and 4%, commensurate with the increase in unique veterans due to new NF/SGVHS CBOC and outpatient clinic activations. Thus, there was an imperative to increase access to this focused consult service for an aging veteran population throughout this large health system. The NF/SGVHS improved timeliness and access to this specialty service within the VA by redesigning its Gait and Balance Clinic and initiating a CVT pilot that connected to selected affiliated remote CBOCs.
Falls
Falls are a major public health problem in the aging U.S. population. Sixty-five percent of individuals aged ≥ 60 years experience dizziness or balance loss daily. About 12 million Americans aged ≥ 65 years have dizziness or balance problems that significantly interfere with their quality of life. Resulting falls are a major cause of both nonfatal and fatal injuries in older adults.7-11 Dizziness also is a common experience among patients aged > 75 years.12 During 2014, the VA saw about 140,000 veteran outpatients for the primary diagnoses of accidental falls, dizziness, and gait abnormality (VHA Support Service Center). The PTs at the Malcom Randall VAMC Gait and Balance Clinic address these important clinical problems in their aging patients.
Balance
Balance is a complex skill based on the interaction of dynamic sensorimotor processes. Balance maintains postural control by keeping the body mass (center of gravity) centered on its support base during stance or voluntary dynamic movements and involves regaining stability quickly in response to destabilizing external perturbations. Balance is preserved by postural motor response adjustments to internal and external forces and environmental stimuli.
Balance is classified as either static, maintaining a base of support with minimal movement, or dynamic, maintaining a stable base of support while completing a purposeful movement. Visual, vestibular, and somatosensory signals are sent to the central nervous system, which in turn adjusts body sway and posture by integrating this information and by controlling skeletal muscles to perform appropriate responses for balance. The brain regions involved in gait control include the premotor cortex and parietal lobes.12
Sustaining postural control is critical for the successful and safe performance of most daily activities. Postural instability occurs particularly in elderly individuals due to any combination of decreased sensitivity in sensors, less effective sensory information input to the central nervous system, and reduced muscular capacity. Patients respond to the majority of postural perturbations through movement primarily at the ankles and hips, called the ankle and hip strategy.
The ankle strategy is most effective for countering slow, smaller perturbations. This requires sufficient ankle range of motion and strength to help maintain stability. The ankle muscles and joint receptors also provide proprioceptive information that assist in the correction of postural sway. When larger external forces are applied during stance, postural control of the body relies more on the hip muscles (hip strategy) as opposed to the ankle muscles. The hip flexor and extensor muscles act during the single-limb stance portion of gait and throughout dynamic turning. Thus, weakness in these muscles contributes to instability during gait and dynamic activities. Larger perturbations trigger a stepping strategy to regain postural control.
Stepping strategy involves an attempt to reestablish a new base of support by stepping forward or backward when the center of gravity has exceeded the original base of support. In the elderly, deficiencies of neural input, environmental feedback, central nervous system sensory integration, and motor output lead to impaired balance and falls. Rehabilitation efforts aim to improve the efficiency and integration of the sensory and motor systems.13-19
By addressing balance and postural instability and associated muscular weakness, vestibular-trained PTs are integral to mitigating fall risks and concomitant fall-related injuries in the aging elderly population.
Implementation
The Gait and Balance CVT pilot was approved as an exempt protocol by the NF/SGVHS VA Research and Development Committee and the affiliated University of Florida Institutional Review Board.
A technician at the Gainesville division scheduled a 1-hour appointment for both the outpatient clinic and main hospital clinic. The appointment duration for a face-to-face encounter was the same as the CVT appointment. At the remote site, medical support staff assisted veterans with appointment check-ins, and a telehealth certified technician (TCT) escorted veterans to the examination room for the CVT visits.
The PT’s office had two 18-inch dual computer monitors. One monitor was for the Computerized Patient Record System (CPRS), and the other was for the CVT visit. The PTV’s computer had a speaker with a webcam that panned in or out at the remote site. The webcam’s software was preinstalled. The outpatient clinic examination room is 18 x 20 feet, accommodating various physical examination testing maneuvers.
In the examination room, the TCT accessed a telehealth mobile cart with a preinstalled webcam and speakers. This cart also connected peripheral devices, such as a stethoscope or otoscope (Figures 1A and 1B). The basic webcam cost about $120. The remote site telehealth mobile cart cost ranged from $30,000 to $45,000 per unit, depending on the complexity. The mobile cart can be used for a variety of specialty CVT visits. The VA purchased a software license for the webcam and cart-attached computers.
One of the project’s implementation
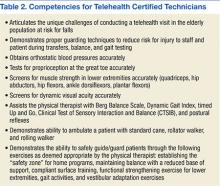
The Malcom Randall VAMC TCTs acquired clinical staff competencies in transfers, balance, and gait testing to prevent injury to both themselves and the patients. Extra safety measures were used when testing balance, such as using the corner of the room and having stable pieces of furniture proximate to the patient, creating a “safety zone” (Table 2). The TCTs were trained to obtain orthostatic blood pressure measurements, test first toe proprioception, screen for lower extremity muscle strength, and screen for dynamic visual acuity (ie, ability to perceive objects accurately while actively moving the head). The TCTs learned to ambulate patients using assistive devices: standard cane, rollator walker and rolling walker.
During the CVT encounter, the PT with the TCTs assistance, performedthe following evaluations: Berg Balance Scale, Dynamic Gait Index, Timed Up and Go, Clinical Test of Sensory Interaction and Balance (CTSIB), and postural reflex testing. The Berg Balance Scale measures 14 balance-related tasks on a 5-point scale (0-4). The DynamicGait Index measures gait during usual steady-state walking, and walking during more challenging tasks. The Timed Up and Go uses the time that a person takes to rise from a chair, walk 3 meters, turn around, walk back to the chair, and sit down. The CTSIB measures how vision, vestibular and somatosensory function impacts balance against the forces of gravity.20-24At the visit’s conclusion, using input the TCT PT educated patients and caregivers on home exercises, maintaining balance, compliant surface training, functional lower extremity exercise strengthening, gait activities, and vestibular adaptation exercises.
Results
The Malcom Randall VAMC partnered with 5 remote clinic sites delivering about 4 to 5 CVT visits weekly with 1 to 2 CVT visits per remote clinic monthly. Some of these sites serve primarily rural veteran enrollees. During the pilot project phase between April 2014 and August 2014, the PT performed 25 CVT encounters with veterans, evaluating gait and balance disorders. Anecdotal informal feedback on the CVT experience was positive for both clinicians and veterans. Moreover, the PT often ordered durable medical equipment during these initial CVT encounters to rapidly employ fall prevention environmental modalities.
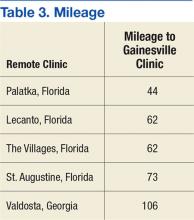
The average round-trip mileage saved per veteran per visit was about 120 miles (Table 3). Reducing the drive time is an important consideration for elderly veterans and their caregivers.
Discussion
The transition from face-to-face to CVT visit was seamless for the PT. Paramount to this success was the TCTs training and related competencies to expect common balance losses during testing. The experienced LPN was a good fit for the TCT role for this particular CVT clinic. Special emphasis in the TCT competency training sessions was given to body and hand positioning to prevent falls in all directions. Placing the hands both in front and behind the patient simultaneously in anticipation of a fall was critical. Walking alongside a patient during gait testing with similar hand placement was also important. Special attention was given during and after the turn when most balance-impaired patients are prone to fall. This provided a feeling of security to both the patient and the remote PT.
Conclusion
Veterans expressed satisfaction to the PTs and TCTs about the reduced travel time and transportation costs. This pilot showed that employing a specialized gait and balance clinic is feasible using CVT technologies with positive results.
Acknowledgments
The authors wish to acknowledge the NF/SGVHS telehealth coordinator, Mr. Indra-Jeet Seenauth, for his invaluable assistance with this pilot clinic and the various telehealth certified technicians for their dedicated support to this clinic and the veterans.
1. U.S. Department of Veterans Affairs. VA telehealth services. U.S. Department of Veterans Affairs Website. http://www.telehealth.va.gov/real-time/index.asp. Updated June 3, 2015. Accessed January 14, 2016.
2. Tuerk PW, Fortney J, Bosworth HB, et al. Toward the development of national telehealth services: the role of Veterans Health Administration and future directions for research. Telemed J E Health.2010;16(1):115-117.
3. Hailey D, Roine R, Ohinmaa A, Dennett L. The status of telerehabilitation in neurological applications. J Telemed Telecare. 2013;19(6):307-310.
4. Kairy D, Lehoux P, Vincent C, Visintin M. A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disabil Rehabil. 2009;31(6):427-447.
5. Lee AC, Harada N. Telehealth as a means of health care delivery for physical therapist practice. Phys Ther. 2012;92(3):463-468.
6. Hoenig H, Tate L, Dumbleton S, et al. A quality assurance study on the accuracy of measuring physical function under current conditions for use of clinical video telehealth. Arch Phys Med Rehabil. 2013;94(5):998-1002.
7. Schiller JS, Kramarow EA, Dey AN. Fall injury episodes among noninstitutionalized older adults: United States, 2001-2003. Adv Data. 2007;(392):1-16.
8. Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall-related injuries in older adults. Am J Public Health. 1992;82(7):1020-1023.
9. Centers for Disease Control and Prevention. Injury--a risk at any stage of life. Centers for Disease. Control and Prevention Website. http://www.cdc.gov/Injury/publications/FactBook/Injury--A_Risk_at_Any_Stage_of_Life2006-a.pdf. Updated September 23, 2009. Accessed January 14, 2016.
10. Centers for Disease Control and Prevention. Injury prevention and control: data and statistics. Centers for Disease Control and Prevention Website. http://www.cdc.gov/injury/wisqars/LeadingCauses.html. Updated March 31, 2015. Accessed January 14, 2016.
11. Centers for Disease Control and Prevention. QuickStats: rate of nonfatal fall injuries receiving medical attention, by age group-National Health Interview Survey, United States, 2012. Centers for Disease Control and Prevention Website. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6329a8.htm. Updated July 25, 2014. Accessed January 14, 2016.
12. Thompson TL, Amedee R. Vertigo: a review of common peripheral and central vestibular disorders. Ochsner J. 2009;9(1):20-26.
13. Sahyoun C, Floyer-Lea A, Johansen-Berg H, Matthews PM. Towards an understanding of gait control: brain activation during the anticipation, preparation and execution of foot movements. Neuroimage. 2004;21(2):568-575.
14. St. George RJ, Fitzpatrick RD, Rogers MW, Lord SR. Choice stepping response and transfer times: effects of age fall risk, and secondary tasks. J Gerontol A Biol Sci Med Sci.2007;62(5):537-542.
15. Vestibular Disorders Association. The human balance system. Vestibular Disorders Association Website. http://vestibular.org/understanding-vestibular-disorder/human-balance-system#. Accessed January 14, 2016.
16. Hausdorff JM, Rios DA, Edelber HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82(8):1050-1056.
17. Soriano TA, DeCherrie LV, Thomas DC. Falls in the community-dwelling older adult: a review for primary care providers. Clin Interv Aging. 2007;2(4):545-554.
18. Bloem BR, Steijns JA, Smits-Engelsman BC. An update on falls. Curr Opin Neurol. 2003;16(1):15-26.
19. Greenwald BD, Burnett DM, Miller MA. Congenital and acquired brain injury.1. Brain injury: epidemiology and pathophysiology. Arch Phys Med Rehabil. 2003;84(3)(suppl 1):S3-S7.
20. Berg KO, Wood-Dauphinee SL, Williams JL, Maki B. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;83(suppl 2):S7-S11.
21. Shumway-Cook A, Woollacott M. Motor Control Theory and Practical Applications. Baltimore, MD: Lippincott Williams & Wilkins; 1995.
22. Podsiadlo D, Richardson S. The timed "Up and Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142-148.
23. Boulgarides, LK, McGinty SM, Willett JA, Barnes CW. Use of clinical and impairment-based tests to predict falls by community-dwelling older adults. Phys Ther. 2003;83(4):328-339.
24. Muir SW, Berg K, Chesworth B, Speechley M. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: a prospective study. Phys Ther. 2008;88(4):449-459.
The VHA has about 700 community-based outpatient clinics (CBOCs). Often these remote clinics lack onsite specialty services. In 2014, about 3 million of the 9 million veterans in the VHA were enrolled in rural locations, according to the VHA Support Service Center Office of Rural Health. This rural cohort is a substantial veteran population for whom meeting specialty medical care needs can be challenging. Rural veterans often travel long distances to a hub medical center when accessing specialty care. This article describes the North Florida/South Georgia Veterans Health System (NF/SGVHS) telehealth solution to provide veteran-centric specialty care access for rural veterans. The program addresses falls, a major public health problem in the elderly.
The VA is a world leader in clinical video telehealth (CVT). Videoconferencing between clinic sites allows clinicians to make diagnoses and provide and manage care without requiring long distance travel. Clinical video telehelth allows veterans to come to the CBOC, connect to a specialist in a remote VA hospital for consultation and treatment, and save transportation time and related costs. The VA has real-time CVT for polytrauma, mental health, rehabilitation, surgery, weight loss, and numerous other specialties.1,2 The CVT rehabilitation modalities have been successfully used both within the VA and in the community for about 15 years, although rigorous economic and functional outcome data are limited.3-6
Gait and Balance Clinic
The NF/SGVHS spans 50 counties and is one of the VA’s largest health systems for clinical workload and rural geography. In 2014, NF/SGVHS had about 160,000 enrolled veterans, and nearly 70,000 were rural, a slightly higher percentage than the VA nationally.
The Gait and Balance Clinic of the Malcom Randall VAMC in Gainesville, Florida, focuses on evaluating and preventing falls and fall-related injuries in the aging veteran population for all enrolled veterans regardless of location. The NF/SGVHS has a robust CVT program, and in 2014, the physical therapist (PT) initiated a CVT Gait and Balance Clinic pilot. This program increased veteran access from remote clinics to these fall prevention services at NF/SGVHS and positively impacted travel time and related costs.
Clinicians refer veterans with falls, dizziness, and vestibular and gait disorders to the Malcom Randall VAMC Gait and Balance Clinic where specially trained PTs provide expert diagnosis and management. The Gait and Balance Clinic is staffed by 2 vestibular-trained PTs and a health technician. The assessments include sophisticated, specialized testing of balance function, determining biologic systems affecting balance. These include the vestibular, visual, sensory, and musculoskeletal systems (Table 1). Therapists provide customized veteran and caregiver education for in-home vestibular exercise programs, fall-reduction strategies, and as-needed adaptive equipment.
Veterans requiring in-depth evaluation attend a weekly Gainesville-based multidisciplinary clinic, staffed by a part-time neurologist, neurology resident trainees, a geriatric medicine fellow, and pharmacy residents and preceptor. Factors affecting gait and balance systems that potentially improve with exercise, such as muscle weakness or vestibular impairments, are mitigated by incorporating into the veteran’s care plan personalized home fall-reduction strategies, exercise programs, and patient and caregiver education.
Specific exercises are designed for each patient’s home environment. The home exercise programs typically include a combination of balance and strength training, vestibular maneuvers, and progressive walking for endurance. In addition to improving patients’ functioning by addressing impairments found on examination, the PTs commonly prescribe assistive devices: rollator walkers, canes, and lower extremity orthoses that reduce fall risk by compensating for deficits in sensory motor systems.The Gait and Balance Clinic receives more than 400 consults annually and experiences a yearly consult growth rate between 2% and 4%, commensurate with the increase in unique veterans due to new NF/SGVHS CBOC and outpatient clinic activations. Thus, there was an imperative to increase access to this focused consult service for an aging veteran population throughout this large health system. The NF/SGVHS improved timeliness and access to this specialty service within the VA by redesigning its Gait and Balance Clinic and initiating a CVT pilot that connected to selected affiliated remote CBOCs.
Falls
Falls are a major public health problem in the aging U.S. population. Sixty-five percent of individuals aged ≥ 60 years experience dizziness or balance loss daily. About 12 million Americans aged ≥ 65 years have dizziness or balance problems that significantly interfere with their quality of life. Resulting falls are a major cause of both nonfatal and fatal injuries in older adults.7-11 Dizziness also is a common experience among patients aged > 75 years.12 During 2014, the VA saw about 140,000 veteran outpatients for the primary diagnoses of accidental falls, dizziness, and gait abnormality (VHA Support Service Center). The PTs at the Malcom Randall VAMC Gait and Balance Clinic address these important clinical problems in their aging patients.
Balance
Balance is a complex skill based on the interaction of dynamic sensorimotor processes. Balance maintains postural control by keeping the body mass (center of gravity) centered on its support base during stance or voluntary dynamic movements and involves regaining stability quickly in response to destabilizing external perturbations. Balance is preserved by postural motor response adjustments to internal and external forces and environmental stimuli.
Balance is classified as either static, maintaining a base of support with minimal movement, or dynamic, maintaining a stable base of support while completing a purposeful movement. Visual, vestibular, and somatosensory signals are sent to the central nervous system, which in turn adjusts body sway and posture by integrating this information and by controlling skeletal muscles to perform appropriate responses for balance. The brain regions involved in gait control include the premotor cortex and parietal lobes.12
Sustaining postural control is critical for the successful and safe performance of most daily activities. Postural instability occurs particularly in elderly individuals due to any combination of decreased sensitivity in sensors, less effective sensory information input to the central nervous system, and reduced muscular capacity. Patients respond to the majority of postural perturbations through movement primarily at the ankles and hips, called the ankle and hip strategy.
The ankle strategy is most effective for countering slow, smaller perturbations. This requires sufficient ankle range of motion and strength to help maintain stability. The ankle muscles and joint receptors also provide proprioceptive information that assist in the correction of postural sway. When larger external forces are applied during stance, postural control of the body relies more on the hip muscles (hip strategy) as opposed to the ankle muscles. The hip flexor and extensor muscles act during the single-limb stance portion of gait and throughout dynamic turning. Thus, weakness in these muscles contributes to instability during gait and dynamic activities. Larger perturbations trigger a stepping strategy to regain postural control.
Stepping strategy involves an attempt to reestablish a new base of support by stepping forward or backward when the center of gravity has exceeded the original base of support. In the elderly, deficiencies of neural input, environmental feedback, central nervous system sensory integration, and motor output lead to impaired balance and falls. Rehabilitation efforts aim to improve the efficiency and integration of the sensory and motor systems.13-19
By addressing balance and postural instability and associated muscular weakness, vestibular-trained PTs are integral to mitigating fall risks and concomitant fall-related injuries in the aging elderly population.
Implementation
The Gait and Balance CVT pilot was approved as an exempt protocol by the NF/SGVHS VA Research and Development Committee and the affiliated University of Florida Institutional Review Board.
A technician at the Gainesville division scheduled a 1-hour appointment for both the outpatient clinic and main hospital clinic. The appointment duration for a face-to-face encounter was the same as the CVT appointment. At the remote site, medical support staff assisted veterans with appointment check-ins, and a telehealth certified technician (TCT) escorted veterans to the examination room for the CVT visits.
The PT’s office had two 18-inch dual computer monitors. One monitor was for the Computerized Patient Record System (CPRS), and the other was for the CVT visit. The PTV’s computer had a speaker with a webcam that panned in or out at the remote site. The webcam’s software was preinstalled. The outpatient clinic examination room is 18 x 20 feet, accommodating various physical examination testing maneuvers.
In the examination room, the TCT accessed a telehealth mobile cart with a preinstalled webcam and speakers. This cart also connected peripheral devices, such as a stethoscope or otoscope (Figures 1A and 1B). The basic webcam cost about $120. The remote site telehealth mobile cart cost ranged from $30,000 to $45,000 per unit, depending on the complexity. The mobile cart can be used for a variety of specialty CVT visits. The VA purchased a software license for the webcam and cart-attached computers.
One of the project’s implementation
The Malcom Randall VAMC TCTs acquired clinical staff competencies in transfers, balance, and gait testing to prevent injury to both themselves and the patients. Extra safety measures were used when testing balance, such as using the corner of the room and having stable pieces of furniture proximate to the patient, creating a “safety zone” (Table 2). The TCTs were trained to obtain orthostatic blood pressure measurements, test first toe proprioception, screen for lower extremity muscle strength, and screen for dynamic visual acuity (ie, ability to perceive objects accurately while actively moving the head). The TCTs learned to ambulate patients using assistive devices: standard cane, rollator walker and rolling walker.
During the CVT encounter, the PT with the TCTs assistance, performedthe following evaluations: Berg Balance Scale, Dynamic Gait Index, Timed Up and Go, Clinical Test of Sensory Interaction and Balance (CTSIB), and postural reflex testing. The Berg Balance Scale measures 14 balance-related tasks on a 5-point scale (0-4). The DynamicGait Index measures gait during usual steady-state walking, and walking during more challenging tasks. The Timed Up and Go uses the time that a person takes to rise from a chair, walk 3 meters, turn around, walk back to the chair, and sit down. The CTSIB measures how vision, vestibular and somatosensory function impacts balance against the forces of gravity.20-24At the visit’s conclusion, using input the TCT PT educated patients and caregivers on home exercises, maintaining balance, compliant surface training, functional lower extremity exercise strengthening, gait activities, and vestibular adaptation exercises.
Results
The Malcom Randall VAMC partnered with 5 remote clinic sites delivering about 4 to 5 CVT visits weekly with 1 to 2 CVT visits per remote clinic monthly. Some of these sites serve primarily rural veteran enrollees. During the pilot project phase between April 2014 and August 2014, the PT performed 25 CVT encounters with veterans, evaluating gait and balance disorders. Anecdotal informal feedback on the CVT experience was positive for both clinicians and veterans. Moreover, the PT often ordered durable medical equipment during these initial CVT encounters to rapidly employ fall prevention environmental modalities.
The average round-trip mileage saved per veteran per visit was about 120 miles (Table 3). Reducing the drive time is an important consideration for elderly veterans and their caregivers.
Discussion
The transition from face-to-face to CVT visit was seamless for the PT. Paramount to this success was the TCTs training and related competencies to expect common balance losses during testing. The experienced LPN was a good fit for the TCT role for this particular CVT clinic. Special emphasis in the TCT competency training sessions was given to body and hand positioning to prevent falls in all directions. Placing the hands both in front and behind the patient simultaneously in anticipation of a fall was critical. Walking alongside a patient during gait testing with similar hand placement was also important. Special attention was given during and after the turn when most balance-impaired patients are prone to fall. This provided a feeling of security to both the patient and the remote PT.
Conclusion
Veterans expressed satisfaction to the PTs and TCTs about the reduced travel time and transportation costs. This pilot showed that employing a specialized gait and balance clinic is feasible using CVT technologies with positive results.
Acknowledgments
The authors wish to acknowledge the NF/SGVHS telehealth coordinator, Mr. Indra-Jeet Seenauth, for his invaluable assistance with this pilot clinic and the various telehealth certified technicians for their dedicated support to this clinic and the veterans.
The VHA has about 700 community-based outpatient clinics (CBOCs). Often these remote clinics lack onsite specialty services. In 2014, about 3 million of the 9 million veterans in the VHA were enrolled in rural locations, according to the VHA Support Service Center Office of Rural Health. This rural cohort is a substantial veteran population for whom meeting specialty medical care needs can be challenging. Rural veterans often travel long distances to a hub medical center when accessing specialty care. This article describes the North Florida/South Georgia Veterans Health System (NF/SGVHS) telehealth solution to provide veteran-centric specialty care access for rural veterans. The program addresses falls, a major public health problem in the elderly.
The VA is a world leader in clinical video telehealth (CVT). Videoconferencing between clinic sites allows clinicians to make diagnoses and provide and manage care without requiring long distance travel. Clinical video telehelth allows veterans to come to the CBOC, connect to a specialist in a remote VA hospital for consultation and treatment, and save transportation time and related costs. The VA has real-time CVT for polytrauma, mental health, rehabilitation, surgery, weight loss, and numerous other specialties.1,2 The CVT rehabilitation modalities have been successfully used both within the VA and in the community for about 15 years, although rigorous economic and functional outcome data are limited.3-6
Gait and Balance Clinic
The NF/SGVHS spans 50 counties and is one of the VA’s largest health systems for clinical workload and rural geography. In 2014, NF/SGVHS had about 160,000 enrolled veterans, and nearly 70,000 were rural, a slightly higher percentage than the VA nationally.
The Gait and Balance Clinic of the Malcom Randall VAMC in Gainesville, Florida, focuses on evaluating and preventing falls and fall-related injuries in the aging veteran population for all enrolled veterans regardless of location. The NF/SGVHS has a robust CVT program, and in 2014, the physical therapist (PT) initiated a CVT Gait and Balance Clinic pilot. This program increased veteran access from remote clinics to these fall prevention services at NF/SGVHS and positively impacted travel time and related costs.
Clinicians refer veterans with falls, dizziness, and vestibular and gait disorders to the Malcom Randall VAMC Gait and Balance Clinic where specially trained PTs provide expert diagnosis and management. The Gait and Balance Clinic is staffed by 2 vestibular-trained PTs and a health technician. The assessments include sophisticated, specialized testing of balance function, determining biologic systems affecting balance. These include the vestibular, visual, sensory, and musculoskeletal systems (Table 1). Therapists provide customized veteran and caregiver education for in-home vestibular exercise programs, fall-reduction strategies, and as-needed adaptive equipment.
Veterans requiring in-depth evaluation attend a weekly Gainesville-based multidisciplinary clinic, staffed by a part-time neurologist, neurology resident trainees, a geriatric medicine fellow, and pharmacy residents and preceptor. Factors affecting gait and balance systems that potentially improve with exercise, such as muscle weakness or vestibular impairments, are mitigated by incorporating into the veteran’s care plan personalized home fall-reduction strategies, exercise programs, and patient and caregiver education.
Specific exercises are designed for each patient’s home environment. The home exercise programs typically include a combination of balance and strength training, vestibular maneuvers, and progressive walking for endurance. In addition to improving patients’ functioning by addressing impairments found on examination, the PTs commonly prescribe assistive devices: rollator walkers, canes, and lower extremity orthoses that reduce fall risk by compensating for deficits in sensory motor systems.The Gait and Balance Clinic receives more than 400 consults annually and experiences a yearly consult growth rate between 2% and 4%, commensurate with the increase in unique veterans due to new NF/SGVHS CBOC and outpatient clinic activations. Thus, there was an imperative to increase access to this focused consult service for an aging veteran population throughout this large health system. The NF/SGVHS improved timeliness and access to this specialty service within the VA by redesigning its Gait and Balance Clinic and initiating a CVT pilot that connected to selected affiliated remote CBOCs.
Falls
Falls are a major public health problem in the aging U.S. population. Sixty-five percent of individuals aged ≥ 60 years experience dizziness or balance loss daily. About 12 million Americans aged ≥ 65 years have dizziness or balance problems that significantly interfere with their quality of life. Resulting falls are a major cause of both nonfatal and fatal injuries in older adults.7-11 Dizziness also is a common experience among patients aged > 75 years.12 During 2014, the VA saw about 140,000 veteran outpatients for the primary diagnoses of accidental falls, dizziness, and gait abnormality (VHA Support Service Center). The PTs at the Malcom Randall VAMC Gait and Balance Clinic address these important clinical problems in their aging patients.
Balance
Balance is a complex skill based on the interaction of dynamic sensorimotor processes. Balance maintains postural control by keeping the body mass (center of gravity) centered on its support base during stance or voluntary dynamic movements and involves regaining stability quickly in response to destabilizing external perturbations. Balance is preserved by postural motor response adjustments to internal and external forces and environmental stimuli.
Balance is classified as either static, maintaining a base of support with minimal movement, or dynamic, maintaining a stable base of support while completing a purposeful movement. Visual, vestibular, and somatosensory signals are sent to the central nervous system, which in turn adjusts body sway and posture by integrating this information and by controlling skeletal muscles to perform appropriate responses for balance. The brain regions involved in gait control include the premotor cortex and parietal lobes.12
Sustaining postural control is critical for the successful and safe performance of most daily activities. Postural instability occurs particularly in elderly individuals due to any combination of decreased sensitivity in sensors, less effective sensory information input to the central nervous system, and reduced muscular capacity. Patients respond to the majority of postural perturbations through movement primarily at the ankles and hips, called the ankle and hip strategy.
The ankle strategy is most effective for countering slow, smaller perturbations. This requires sufficient ankle range of motion and strength to help maintain stability. The ankle muscles and joint receptors also provide proprioceptive information that assist in the correction of postural sway. When larger external forces are applied during stance, postural control of the body relies more on the hip muscles (hip strategy) as opposed to the ankle muscles. The hip flexor and extensor muscles act during the single-limb stance portion of gait and throughout dynamic turning. Thus, weakness in these muscles contributes to instability during gait and dynamic activities. Larger perturbations trigger a stepping strategy to regain postural control.
Stepping strategy involves an attempt to reestablish a new base of support by stepping forward or backward when the center of gravity has exceeded the original base of support. In the elderly, deficiencies of neural input, environmental feedback, central nervous system sensory integration, and motor output lead to impaired balance and falls. Rehabilitation efforts aim to improve the efficiency and integration of the sensory and motor systems.13-19
By addressing balance and postural instability and associated muscular weakness, vestibular-trained PTs are integral to mitigating fall risks and concomitant fall-related injuries in the aging elderly population.
Implementation
The Gait and Balance CVT pilot was approved as an exempt protocol by the NF/SGVHS VA Research and Development Committee and the affiliated University of Florida Institutional Review Board.
A technician at the Gainesville division scheduled a 1-hour appointment for both the outpatient clinic and main hospital clinic. The appointment duration for a face-to-face encounter was the same as the CVT appointment. At the remote site, medical support staff assisted veterans with appointment check-ins, and a telehealth certified technician (TCT) escorted veterans to the examination room for the CVT visits.
The PT’s office had two 18-inch dual computer monitors. One monitor was for the Computerized Patient Record System (CPRS), and the other was for the CVT visit. The PTV’s computer had a speaker with a webcam that panned in or out at the remote site. The webcam’s software was preinstalled. The outpatient clinic examination room is 18 x 20 feet, accommodating various physical examination testing maneuvers.
In the examination room, the TCT accessed a telehealth mobile cart with a preinstalled webcam and speakers. This cart also connected peripheral devices, such as a stethoscope or otoscope (Figures 1A and 1B). The basic webcam cost about $120. The remote site telehealth mobile cart cost ranged from $30,000 to $45,000 per unit, depending on the complexity. The mobile cart can be used for a variety of specialty CVT visits. The VA purchased a software license for the webcam and cart-attached computers.
One of the project’s implementation
The Malcom Randall VAMC TCTs acquired clinical staff competencies in transfers, balance, and gait testing to prevent injury to both themselves and the patients. Extra safety measures were used when testing balance, such as using the corner of the room and having stable pieces of furniture proximate to the patient, creating a “safety zone” (Table 2). The TCTs were trained to obtain orthostatic blood pressure measurements, test first toe proprioception, screen for lower extremity muscle strength, and screen for dynamic visual acuity (ie, ability to perceive objects accurately while actively moving the head). The TCTs learned to ambulate patients using assistive devices: standard cane, rollator walker and rolling walker.
During the CVT encounter, the PT with the TCTs assistance, performedthe following evaluations: Berg Balance Scale, Dynamic Gait Index, Timed Up and Go, Clinical Test of Sensory Interaction and Balance (CTSIB), and postural reflex testing. The Berg Balance Scale measures 14 balance-related tasks on a 5-point scale (0-4). The DynamicGait Index measures gait during usual steady-state walking, and walking during more challenging tasks. The Timed Up and Go uses the time that a person takes to rise from a chair, walk 3 meters, turn around, walk back to the chair, and sit down. The CTSIB measures how vision, vestibular and somatosensory function impacts balance against the forces of gravity.20-24At the visit’s conclusion, using input the TCT PT educated patients and caregivers on home exercises, maintaining balance, compliant surface training, functional lower extremity exercise strengthening, gait activities, and vestibular adaptation exercises.
Results
The Malcom Randall VAMC partnered with 5 remote clinic sites delivering about 4 to 5 CVT visits weekly with 1 to 2 CVT visits per remote clinic monthly. Some of these sites serve primarily rural veteran enrollees. During the pilot project phase between April 2014 and August 2014, the PT performed 25 CVT encounters with veterans, evaluating gait and balance disorders. Anecdotal informal feedback on the CVT experience was positive for both clinicians and veterans. Moreover, the PT often ordered durable medical equipment during these initial CVT encounters to rapidly employ fall prevention environmental modalities.
The average round-trip mileage saved per veteran per visit was about 120 miles (Table 3). Reducing the drive time is an important consideration for elderly veterans and their caregivers.
Discussion
The transition from face-to-face to CVT visit was seamless for the PT. Paramount to this success was the TCTs training and related competencies to expect common balance losses during testing. The experienced LPN was a good fit for the TCT role for this particular CVT clinic. Special emphasis in the TCT competency training sessions was given to body and hand positioning to prevent falls in all directions. Placing the hands both in front and behind the patient simultaneously in anticipation of a fall was critical. Walking alongside a patient during gait testing with similar hand placement was also important. Special attention was given during and after the turn when most balance-impaired patients are prone to fall. This provided a feeling of security to both the patient and the remote PT.
Conclusion
Veterans expressed satisfaction to the PTs and TCTs about the reduced travel time and transportation costs. This pilot showed that employing a specialized gait and balance clinic is feasible using CVT technologies with positive results.
Acknowledgments
The authors wish to acknowledge the NF/SGVHS telehealth coordinator, Mr. Indra-Jeet Seenauth, for his invaluable assistance with this pilot clinic and the various telehealth certified technicians for their dedicated support to this clinic and the veterans.
1. U.S. Department of Veterans Affairs. VA telehealth services. U.S. Department of Veterans Affairs Website. http://www.telehealth.va.gov/real-time/index.asp. Updated June 3, 2015. Accessed January 14, 2016.
2. Tuerk PW, Fortney J, Bosworth HB, et al. Toward the development of national telehealth services: the role of Veterans Health Administration and future directions for research. Telemed J E Health.2010;16(1):115-117.
3. Hailey D, Roine R, Ohinmaa A, Dennett L. The status of telerehabilitation in neurological applications. J Telemed Telecare. 2013;19(6):307-310.
4. Kairy D, Lehoux P, Vincent C, Visintin M. A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disabil Rehabil. 2009;31(6):427-447.
5. Lee AC, Harada N. Telehealth as a means of health care delivery for physical therapist practice. Phys Ther. 2012;92(3):463-468.
6. Hoenig H, Tate L, Dumbleton S, et al. A quality assurance study on the accuracy of measuring physical function under current conditions for use of clinical video telehealth. Arch Phys Med Rehabil. 2013;94(5):998-1002.
7. Schiller JS, Kramarow EA, Dey AN. Fall injury episodes among noninstitutionalized older adults: United States, 2001-2003. Adv Data. 2007;(392):1-16.
8. Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall-related injuries in older adults. Am J Public Health. 1992;82(7):1020-1023.
9. Centers for Disease Control and Prevention. Injury--a risk at any stage of life. Centers for Disease. Control and Prevention Website. http://www.cdc.gov/Injury/publications/FactBook/Injury--A_Risk_at_Any_Stage_of_Life2006-a.pdf. Updated September 23, 2009. Accessed January 14, 2016.
10. Centers for Disease Control and Prevention. Injury prevention and control: data and statistics. Centers for Disease Control and Prevention Website. http://www.cdc.gov/injury/wisqars/LeadingCauses.html. Updated March 31, 2015. Accessed January 14, 2016.
11. Centers for Disease Control and Prevention. QuickStats: rate of nonfatal fall injuries receiving medical attention, by age group-National Health Interview Survey, United States, 2012. Centers for Disease Control and Prevention Website. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6329a8.htm. Updated July 25, 2014. Accessed January 14, 2016.
12. Thompson TL, Amedee R. Vertigo: a review of common peripheral and central vestibular disorders. Ochsner J. 2009;9(1):20-26.
13. Sahyoun C, Floyer-Lea A, Johansen-Berg H, Matthews PM. Towards an understanding of gait control: brain activation during the anticipation, preparation and execution of foot movements. Neuroimage. 2004;21(2):568-575.
14. St. George RJ, Fitzpatrick RD, Rogers MW, Lord SR. Choice stepping response and transfer times: effects of age fall risk, and secondary tasks. J Gerontol A Biol Sci Med Sci.2007;62(5):537-542.
15. Vestibular Disorders Association. The human balance system. Vestibular Disorders Association Website. http://vestibular.org/understanding-vestibular-disorder/human-balance-system#. Accessed January 14, 2016.
16. Hausdorff JM, Rios DA, Edelber HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82(8):1050-1056.
17. Soriano TA, DeCherrie LV, Thomas DC. Falls in the community-dwelling older adult: a review for primary care providers. Clin Interv Aging. 2007;2(4):545-554.
18. Bloem BR, Steijns JA, Smits-Engelsman BC. An update on falls. Curr Opin Neurol. 2003;16(1):15-26.
19. Greenwald BD, Burnett DM, Miller MA. Congenital and acquired brain injury.1. Brain injury: epidemiology and pathophysiology. Arch Phys Med Rehabil. 2003;84(3)(suppl 1):S3-S7.
20. Berg KO, Wood-Dauphinee SL, Williams JL, Maki B. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;83(suppl 2):S7-S11.
21. Shumway-Cook A, Woollacott M. Motor Control Theory and Practical Applications. Baltimore, MD: Lippincott Williams & Wilkins; 1995.
22. Podsiadlo D, Richardson S. The timed "Up and Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142-148.
23. Boulgarides, LK, McGinty SM, Willett JA, Barnes CW. Use of clinical and impairment-based tests to predict falls by community-dwelling older adults. Phys Ther. 2003;83(4):328-339.
24. Muir SW, Berg K, Chesworth B, Speechley M. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: a prospective study. Phys Ther. 2008;88(4):449-459.
1. U.S. Department of Veterans Affairs. VA telehealth services. U.S. Department of Veterans Affairs Website. http://www.telehealth.va.gov/real-time/index.asp. Updated June 3, 2015. Accessed January 14, 2016.
2. Tuerk PW, Fortney J, Bosworth HB, et al. Toward the development of national telehealth services: the role of Veterans Health Administration and future directions for research. Telemed J E Health.2010;16(1):115-117.
3. Hailey D, Roine R, Ohinmaa A, Dennett L. The status of telerehabilitation in neurological applications. J Telemed Telecare. 2013;19(6):307-310.
4. Kairy D, Lehoux P, Vincent C, Visintin M. A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disabil Rehabil. 2009;31(6):427-447.
5. Lee AC, Harada N. Telehealth as a means of health care delivery for physical therapist practice. Phys Ther. 2012;92(3):463-468.
6. Hoenig H, Tate L, Dumbleton S, et al. A quality assurance study on the accuracy of measuring physical function under current conditions for use of clinical video telehealth. Arch Phys Med Rehabil. 2013;94(5):998-1002.
7. Schiller JS, Kramarow EA, Dey AN. Fall injury episodes among noninstitutionalized older adults: United States, 2001-2003. Adv Data. 2007;(392):1-16.
8. Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall-related injuries in older adults. Am J Public Health. 1992;82(7):1020-1023.
9. Centers for Disease Control and Prevention. Injury--a risk at any stage of life. Centers for Disease. Control and Prevention Website. http://www.cdc.gov/Injury/publications/FactBook/Injury--A_Risk_at_Any_Stage_of_Life2006-a.pdf. Updated September 23, 2009. Accessed January 14, 2016.
10. Centers for Disease Control and Prevention. Injury prevention and control: data and statistics. Centers for Disease Control and Prevention Website. http://www.cdc.gov/injury/wisqars/LeadingCauses.html. Updated March 31, 2015. Accessed January 14, 2016.
11. Centers for Disease Control and Prevention. QuickStats: rate of nonfatal fall injuries receiving medical attention, by age group-National Health Interview Survey, United States, 2012. Centers for Disease Control and Prevention Website. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6329a8.htm. Updated July 25, 2014. Accessed January 14, 2016.
12. Thompson TL, Amedee R. Vertigo: a review of common peripheral and central vestibular disorders. Ochsner J. 2009;9(1):20-26.
13. Sahyoun C, Floyer-Lea A, Johansen-Berg H, Matthews PM. Towards an understanding of gait control: brain activation during the anticipation, preparation and execution of foot movements. Neuroimage. 2004;21(2):568-575.
14. St. George RJ, Fitzpatrick RD, Rogers MW, Lord SR. Choice stepping response and transfer times: effects of age fall risk, and secondary tasks. J Gerontol A Biol Sci Med Sci.2007;62(5):537-542.
15. Vestibular Disorders Association. The human balance system. Vestibular Disorders Association Website. http://vestibular.org/understanding-vestibular-disorder/human-balance-system#. Accessed January 14, 2016.
16. Hausdorff JM, Rios DA, Edelber HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82(8):1050-1056.
17. Soriano TA, DeCherrie LV, Thomas DC. Falls in the community-dwelling older adult: a review for primary care providers. Clin Interv Aging. 2007;2(4):545-554.
18. Bloem BR, Steijns JA, Smits-Engelsman BC. An update on falls. Curr Opin Neurol. 2003;16(1):15-26.
19. Greenwald BD, Burnett DM, Miller MA. Congenital and acquired brain injury.1. Brain injury: epidemiology and pathophysiology. Arch Phys Med Rehabil. 2003;84(3)(suppl 1):S3-S7.
20. Berg KO, Wood-Dauphinee SL, Williams JL, Maki B. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;83(suppl 2):S7-S11.
21. Shumway-Cook A, Woollacott M. Motor Control Theory and Practical Applications. Baltimore, MD: Lippincott Williams & Wilkins; 1995.
22. Podsiadlo D, Richardson S. The timed "Up and Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142-148.
23. Boulgarides, LK, McGinty SM, Willett JA, Barnes CW. Use of clinical and impairment-based tests to predict falls by community-dwelling older adults. Phys Ther. 2003;83(4):328-339.
24. Muir SW, Berg K, Chesworth B, Speechley M. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: a prospective study. Phys Ther. 2008;88(4):449-459.