User login
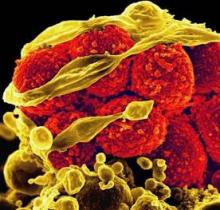
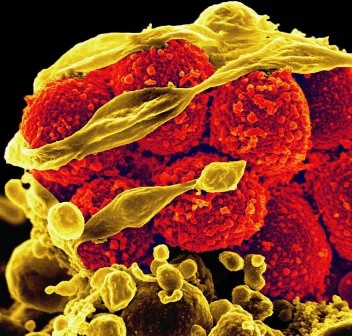
SAN FRANCISCO – An early switch to daptomycin improved clinical outcomes compared with dose-adjusted vancomycin in patients with methicillin-resistant Staphylococcus aureus bacteremia and a vancomycin minimum inhibitory concentration greater than 1 mcg/mL.
The findings come from the first matched comparison of daptomycin as early therapy versus dose-optimized vancomycin for this patient population.
"Continued vancomycin use is an independent predictor of clinical failure" in these patients, lead study investigator Kyle P. Murray, Pharm.D., said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Dr. Murray and his associates at Detroit Medical Center and the Anti-Infective Research Laboratory at Wayne State University in Detroit evaluated data from 170 inpatients who had MRSA bacteremia and a vancomycin minimum inhibitory concentration (MIC) greater than 1 mcg/mL and were treated with daptomycin (at least 6 mg/kg daily) or vancomycin (a target trough of 15-20 mcg/mL). The patients were matched 1:1 on the basis of age, Pittsburgh bacteremia score, and their primary site of infection. The researchers excluded patients who had pneumonia or whose primary site of infection was an intravenous catheter, daptomycin-treated patients who received more than 72 hours of initial vancomycin, and patients who required renal replacement therapy.
The primary outcome was clinical failure, defined as either microbiological failure (bacteremia persisting for 7 or more days from the initial positive blood culture) or mortality within 30 days of the initial positive culture.
Baseline characteristics were similar between the daptomycin and vancomycin groups in terms of age (a median of 57 vs. 56 years, respectively), Pittsburgh bacteremia score (2 in each group), and Charlson comorbidity index score (5 vs. 4). The median daptomycin dose was 8.4 mg/kg per day and the median initial vancomycin trough was 12.9 mcg /mL. After dose adjustment, the median vancomycin trough was 17.6 mcg /mL.
Dr. Murray reported that 48% of patients in the vancomycin group experienced clinical failure compared with 20% of those in the daptomycin group, a difference that reached statistical significance with a P value of less than .001. There were also significant differences between the vancomycin and daptomycin groups in 30-day mortality (13% vs. 3.5%, respectively; P = .047) the proportion of patients with persistent bacteremia (42% vs. 19%; P = .001), and in the duration of bacteremia (a median of 3 vs. 5 days; P = .003). There were no significant differences between the treatment groups in the proportion of patients who were readmitted after 30 days (20% vs. 25%; P = .381).
After performing multivariate logistic regression analysis and adjusting for certain clinical variables, Dr. Murray and his associates observed three significant predictors of clinical failure: ICU admission (OR 5.8; P less than .001), vancomycin treatment (OR 4.5; P less than .001), and intravenous drug use (OR 3.0; P = .004).
Dr. Murray had no financial conflicts to disclose. Other coauthors disclosed having a consultant role with, receiving grant support from, or being a member of the speakers bureau for Merck, Pfizer, Cubist Pharmaceuticals, Astellas, Forest Pharmaceuticals, and Rib-X Pharmaceuticals.
The meeting was sponsored by the American Society for Microbiology.
SAN FRANCISCO – An early switch to daptomycin improved clinical outcomes compared with dose-adjusted vancomycin in patients with methicillin-resistant Staphylococcus aureus bacteremia and a vancomycin minimum inhibitory concentration greater than 1 mcg/mL.
The findings come from the first matched comparison of daptomycin as early therapy versus dose-optimized vancomycin for this patient population.
"Continued vancomycin use is an independent predictor of clinical failure" in these patients, lead study investigator Kyle P. Murray, Pharm.D., said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Dr. Murray and his associates at Detroit Medical Center and the Anti-Infective Research Laboratory at Wayne State University in Detroit evaluated data from 170 inpatients who had MRSA bacteremia and a vancomycin minimum inhibitory concentration (MIC) greater than 1 mcg/mL and were treated with daptomycin (at least 6 mg/kg daily) or vancomycin (a target trough of 15-20 mcg/mL). The patients were matched 1:1 on the basis of age, Pittsburgh bacteremia score, and their primary site of infection. The researchers excluded patients who had pneumonia or whose primary site of infection was an intravenous catheter, daptomycin-treated patients who received more than 72 hours of initial vancomycin, and patients who required renal replacement therapy.
The primary outcome was clinical failure, defined as either microbiological failure (bacteremia persisting for 7 or more days from the initial positive blood culture) or mortality within 30 days of the initial positive culture.
Baseline characteristics were similar between the daptomycin and vancomycin groups in terms of age (a median of 57 vs. 56 years, respectively), Pittsburgh bacteremia score (2 in each group), and Charlson comorbidity index score (5 vs. 4). The median daptomycin dose was 8.4 mg/kg per day and the median initial vancomycin trough was 12.9 mcg /mL. After dose adjustment, the median vancomycin trough was 17.6 mcg /mL.
Dr. Murray reported that 48% of patients in the vancomycin group experienced clinical failure compared with 20% of those in the daptomycin group, a difference that reached statistical significance with a P value of less than .001. There were also significant differences between the vancomycin and daptomycin groups in 30-day mortality (13% vs. 3.5%, respectively; P = .047) the proportion of patients with persistent bacteremia (42% vs. 19%; P = .001), and in the duration of bacteremia (a median of 3 vs. 5 days; P = .003). There were no significant differences between the treatment groups in the proportion of patients who were readmitted after 30 days (20% vs. 25%; P = .381).
After performing multivariate logistic regression analysis and adjusting for certain clinical variables, Dr. Murray and his associates observed three significant predictors of clinical failure: ICU admission (OR 5.8; P less than .001), vancomycin treatment (OR 4.5; P less than .001), and intravenous drug use (OR 3.0; P = .004).
Dr. Murray had no financial conflicts to disclose. Other coauthors disclosed having a consultant role with, receiving grant support from, or being a member of the speakers bureau for Merck, Pfizer, Cubist Pharmaceuticals, Astellas, Forest Pharmaceuticals, and Rib-X Pharmaceuticals.
The meeting was sponsored by the American Society for Microbiology.
SAN FRANCISCO – An early switch to daptomycin improved clinical outcomes compared with dose-adjusted vancomycin in patients with methicillin-resistant Staphylococcus aureus bacteremia and a vancomycin minimum inhibitory concentration greater than 1 mcg/mL.
The findings come from the first matched comparison of daptomycin as early therapy versus dose-optimized vancomycin for this patient population.
"Continued vancomycin use is an independent predictor of clinical failure" in these patients, lead study investigator Kyle P. Murray, Pharm.D., said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Dr. Murray and his associates at Detroit Medical Center and the Anti-Infective Research Laboratory at Wayne State University in Detroit evaluated data from 170 inpatients who had MRSA bacteremia and a vancomycin minimum inhibitory concentration (MIC) greater than 1 mcg/mL and were treated with daptomycin (at least 6 mg/kg daily) or vancomycin (a target trough of 15-20 mcg/mL). The patients were matched 1:1 on the basis of age, Pittsburgh bacteremia score, and their primary site of infection. The researchers excluded patients who had pneumonia or whose primary site of infection was an intravenous catheter, daptomycin-treated patients who received more than 72 hours of initial vancomycin, and patients who required renal replacement therapy.
The primary outcome was clinical failure, defined as either microbiological failure (bacteremia persisting for 7 or more days from the initial positive blood culture) or mortality within 30 days of the initial positive culture.
Baseline characteristics were similar between the daptomycin and vancomycin groups in terms of age (a median of 57 vs. 56 years, respectively), Pittsburgh bacteremia score (2 in each group), and Charlson comorbidity index score (5 vs. 4). The median daptomycin dose was 8.4 mg/kg per day and the median initial vancomycin trough was 12.9 mcg /mL. After dose adjustment, the median vancomycin trough was 17.6 mcg /mL.
Dr. Murray reported that 48% of patients in the vancomycin group experienced clinical failure compared with 20% of those in the daptomycin group, a difference that reached statistical significance with a P value of less than .001. There were also significant differences between the vancomycin and daptomycin groups in 30-day mortality (13% vs. 3.5%, respectively; P = .047) the proportion of patients with persistent bacteremia (42% vs. 19%; P = .001), and in the duration of bacteremia (a median of 3 vs. 5 days; P = .003). There were no significant differences between the treatment groups in the proportion of patients who were readmitted after 30 days (20% vs. 25%; P = .381).
After performing multivariate logistic regression analysis and adjusting for certain clinical variables, Dr. Murray and his associates observed three significant predictors of clinical failure: ICU admission (OR 5.8; P less than .001), vancomycin treatment (OR 4.5; P less than .001), and intravenous drug use (OR 3.0; P = .004).
Dr. Murray had no financial conflicts to disclose. Other coauthors disclosed having a consultant role with, receiving grant support from, or being a member of the speakers bureau for Merck, Pfizer, Cubist Pharmaceuticals, Astellas, Forest Pharmaceuticals, and Rib-X Pharmaceuticals.
The meeting was sponsored by the American Society for Microbiology.
AT THE ANNUAL INTERSCIENCE CONFERENCE ON ANTIMICROBIAL AGENTS AND CHEMOTHERAPY