User login
Type 2 diabetes mellitus (T2DM) is a significant, growing health problem that results in increased morbidity and mortality. In adults, T2DM accounts for about 90% to 95% of all diagnosed cases of diabetes.1 Diabetes is the leading cause of kidney failure and blindness; moreover, diabetic patients are 2 to 4 times more likely to die of complications of heart disease and/or have a stroke.2 Other complications of diabetes include nervous system damage and nontraumatic lower limb amputation. Increased morbidity and mortality not only diminishes quality of life (QOL) for patients with diabetes, but also produces a financial health care burden. The cost of diabetes in the U.S. in 2012 was more than $245 billion compared with $174 billion in 2007.1
The Centers for Disease Control and Prevention (CDC) predicts that 1 in 3 American adults will develop diabetes by 2050; thus, optimal approaches to diabetic care need to be developed and evaluated to determine best practices.3,4 Better control of blood sugar, cholesterol, and blood pressure levels in people with diabetes will help reduce the risk of complications of kidney disease, eye disease, nervous system disease, heart attack, and stroke.5 Optimal approaches to diabetes management must now be developed to prepare for the forecasted increase of T2DM.
A review of the literature confirms that lack of continuity of care often leads to patient dissatisfaction with health care, to fragmented health care, and a greater propensity to disregard a defined health care treatment plan.6,7 In addition to improved patient satisfaction and adherence to medical management, improved continuity of care is cost-effective. A longitudinal study based on claims data from 2000 to 2008, using the continuity of care index, indicated that improved continuity of care was associated with less health care waste and lower health care expenses for patients with T2DM.8 An average savings of $737 in total health care expenses per person was achieved with better continuity of care.8 These studies demonstrate that improving continuity of care improves outcomes in patients with diabetes and helps prevent excessive health care costs and waste.
Medical Center NonContinuity
Lack of continuity of care has been identified as a potential obstacle to optimal diabetic outcomes at William Beaumont Army Medical Center (WBAMC) in El Paso, Texas, based on a recent data analysis provided by TRICARE Regional Office West.9,10 As of March 2010, 56,936 patients were enrolled in TRICARE Prime. Of these patients, only 29.92% had appointments with their assigned primary care manager (PCM).9
In 2009, WBAMC developed a database to track the Healthcare Effectiveness Data and Information Set (HEDIS) measures to monitor A1c as well as other indicators of performance of health care services, such as mammography, Pap smear, bone densitometry, and colorectal screening. A recent American Diabetic Association expert committee recommendation endorsed the use of A1c value > 6.5% to confirm the diagnosis of diabetes.11 The A1c test may be confirmed with a repeat test unless clinical symptoms exist or the patient has random glucose levels > 200 mg/dL. Importantly, individuals with an A1c between 6% and 6.5% have a higher risk for developing diabetes and may be diagnosed with prediabetes.3
From 2008 to 2009, the HEDIS database tracking the progress of A1c demonstrated a 0.3% positive change and improvement in A1c ≤ 9% (normal 4%-6%). The goal for people with diabetes is A1c < 7%. Uncontrolled diabetes, (ie, A1c > 9%), is associated with greater diabetes-related complications.12 Using the HEDIS benchmark of ≥ 9%, the HEDIS A1c data for fiscal year (FY) 2008 were 71.1 (p50) and 81 (p90), and for FY 2009 were 72.2 (p50) and 81.3 (p90), reflecting p90 0.3% improvement.13 Therefore, these data reflect poor outcomes of patients with T2DM with A1c levels that were not controlled at WBAMC.
Uncontrolled diabetes accrues significant health care costs and adverse diabetic outcomes.10 Consequently, the WBAMC clinical operations division, which was tasked to monitor the HEDIS database, identified and contacted individuals to schedule health care appointments. The primary endeavor was an attempt to substantially increase benchmarks and maintain levels of A1c < 9%, demonstrate improvement in quality of care, and reduce health care costs. Unfortunately, these goals were not met for the aggregate of patients with T2DM.
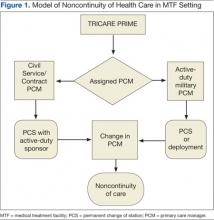
Figure 1 illustrates how the diabetic population at WBAMC had experienced decreased continuity of care and the adverse effects on their diabetes management. Figure 1 also illustrates how beneficiaries of TRICARE are assigned a PCM and how this process results in a lack of continuity of care for patients with T2DM. An Army medical center (MEDCEN) typically uses PCMs who may be a physician, nurse practitioner (NP), or physician assistant. Unfortunately, the majority of these PCMs are active-duty military or civil service personnel who commonly undergo permanent change of station moves or deployments every 3 years. Additionally, military providers are often rotated through department-chief positions, thereby dissolving their patient relationships.
Frequent rotations offer a valid means to foster leadership skills much needed in a military conflict zone and maximize military professional development; however, rotations also contribute to the lack of continuity of patient care. This PCM instability and the distinctive military dynamic volatility are characteristic of standard military operating procedure and are unlikely to change.
New solutions are needed to promote improved continuity of care for patients with diabetes at a MEDCEN. According to Lt Gen Eric Schoomaker, former Surgeon General of the Army, “The Patient-Centered Medical Home concept is being adopted throughout the military health system.”14 The goal of the trend toward patient-centered medical home (PCMH) care delivery is to improve access to high-quality health care services.13
Patient-Centered Medical Home
The term patient-centered medical home was introduced in 1967 by the American Academy of Pediatrics (AAP).15 In 2008, PCMH principles became integral in most health care reform initiatives.16 In most PCMH models, increased continuity of care is the single common denominator of practice. Continuity of care is defined as intensified integration, coordination, and sharing of information between disciplines that result in improved patient outcomes.10,17,18
In 2007, a consensus statement was provided by the American Academy of Family Practice, the AAP, American College of Physicians, and the American Osteopathic Association stating that quality and safety are hallmarks of the PCMH and may improve outcomes for chronic disease, such as diabetes.19
Quality improvement is vital in health care organizations because of demands by government agencies, health maintenance organizations, and the public to continually improve services and to provide the highest quality health care at the best cost.20 Diabetes has become a public health crisis, as previously discussed, and a comprehensive approach to care management is essential. Developing an optimal process for diabetes health care and methods for evaluation of the delivery process is foundational for all stakeholders involved, including health care organizations, health care providers, and patients.20
Diabetic outcomes were evaluated at a recent 2-year trial PCMH approach T2DM clinic at a MEDCEN at WBAMC. The purpose of the project was to determine whether a PCMH approach improves disease management compared with routine primary care management.
Methods
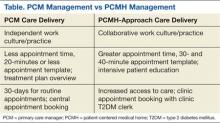
The process and manner of care delivery was the focus of this analysis and evaluation, not clinician knowledge of treatment management. A comparison of care delivery approaches of PCM management and PCMH care delivery is displayed in the Table. The treatment algorithm for T2DM was not in question, because guidelines for practice are established based on scientific evidence, and medication management is based on evidence-based practice.21,22 Evaluation consisted of T2DM delivery of care process and the efficacy of outcome achieved by the specified delivery of care: (a) increased access to care; (b) intensive, repeated education; and (3) a multidisciplinary approach focused on patient empowerment. The following is a description of the specified delivery of care.
Increased Access to Care
Increased access to care addressed through frequent telecommunication provided by the registered nurse (RN) case manager who regularly called patients within 72 hours of insulin adjustment or 24 hours for insulin initiation or significant medication changes. Additionally, the diabetes team providers requested a follow-up appointment in 1 week when injectable medication was added or changes were made in insulin management. One exception was for the addition of livaglutide, in which a 2-week follow-up was made, to allow for titration of the medication. For oral medication adjustment, a 1-month follow-up was generally made, with a 2-month follow-up when a glucose histogram indicated optimal glycemic control, an average blood glucose of 7% (estimated average glucose of 154 mg/dL) or less. Time for appointments was increased by 10 minutes for a total of 30-minute appointments, compared with 20 minutes for PCM delivery.
Informational continuity was thought to be improved by use of an electronic medical record (EMR), allowing for an uninterrupted patient record. Providers were expected to document medication reconciliation with a clear explanation of medication adjustments listed in the plan. Patient teaching was documented, describing the specific patient education concerns addressed. Other data included a glucometer statistical report from the last appointment to the current appointment, to track negative or positive changes in glycemic control.
Patient Education
The management technique used in the clinic was intensive, repeated education with the goal of improving learning and retention with repeated instruction and positive reinforcement. Skinner theorized that learning is the acquisition of new behavior through conditioning (eg, repeated instruction), is in close proximity of time, and is likely to result in learning retention, which remain relevant education practice.23,24 The T2DM clinic operates on Skinner’s principles of repeated, intensive education. For example, patients must bring their glucometer to every appointment. The statistical analysis downloaded from the glucometer provides immediate reinforcement and information about patients’ glycemic control. Patients are typically excited to see an improvement from previous levels and are encouraged to continue behavior modification. Conversely, statistical analysis demonstrating poor glycemic control generally encourages the patient to make needed lifestyle changes. Thus, changes in behavior due to intensive, repeated education, followed by a reinforcing stimulus results in an increased probability of that behavior occurring in the future.23,25 The interdisciplinary team provides education during each T2DM patient encounter.
Multidisciplinary Approach
The multidisciplinary team formed at the trial T2DM clinic consisted of a medical doctor, family NP, pharmacist, RN, licensed vocational nurse, and registered dietician. The team members were each encouraged to obtain Certified Diabetes Educator (CDE) certification. For the first 6 months of developing the clinic, staff scheduled weekly team-building meetings to encourage esprit de corps. The weekly meetings were also used to discuss difficult patient cases. The RN case manager provided the patients with individualized plans to help them meet specified goals and provided easy accessibility for patient questions and concerns. The pharmacist was integral in helping patients understand the role of their medication and was also certified to make medication adjustments related to diabetes.
A recent Institute of Medicine (IOM) report encouraged the expansion of roles for nurse practitioners (NPs) in coordination and primary care delivery.26 The IOM collaborative statement is based on numerous studies showing that NPs provided equivalent quality of care compared with that of primary care physicians in routine chronic disease management.26 Nurse case managers functioned as an integral part of the intensive therapy involved in the landmark Diabetes Control and Complication Trial.27
The intended policy analysis and outcome evaluation was confined to data collected from a disease-specific (T2DM) clinic with a PCMH approach developed April 2011 at WBAMC. Data were obtained from the WBAMC database designed to track the HEDIS measures.
Enrollees of the clinic were restricted to patients diagnosed with T2DM who were TRICARE beneficiaries. Males and females, aged > 20 years with an established A1c > 6.5% comprised the patient population of the clinic. Individuals who were managed by WBAMC or were TRICARE standard beneficiaries were excluded from the study. Because patients with T1DM have a different pathology than those with T2DM, they were referred to endocrinology. Patients with gestational diabetes were referred to obstetrics for management.
Data Collection
Existing data in the Armed Forces Health Longitudinal Technology Application (AHLTA) EMR were used for this analysis. Data were accessed by a Common Access Card (CAC card) enhanced security system accessed only through secure CAC applications.
Diabetic outcomes of glycemic control as measured by the A1c value were examined prior to clinic enrollment (time 1: PCM care delivery) and subsequently (time 2: PCMH care delivery) at the health care provider’s discretion. The second time varied between 2 and 6 months, depending on (1) provider need to determine quickly (2 months) whether a downward trend was occurring because of multiple comorbidities; (2) provider discretion to wait an additional 3 months (A1c turnover x 2 = 6 months), while medication adjustments are being made; and (3) according to feasibility of follow-up based on patient’s scheduling. Low-density lipoprotein cholesterol (LDL-C) was also examined at both PCM care delivery and PCMH care delivery.
The endpoints of a reduction in A1c by 1% and an LDL-C that is ≤ 100 mg/dL determined improved diabetes outcomes. Existing data (eg, glycemic control [A1c], lipid control [LDL-C]), from April 1, 2011, to December 31, 2011, were logged in a clinic database. These data served to demonstrate the effectiveness of the T2DM PCMH approach to clinic management. The PCMH principles that were examined included the standard operating procedure for the T2DM-PCMH clinic: frequent appointments > 2 in a 3-month period), a multidisciplinary team, and intensive, repeated education.
Data analysis was conducted with descriptive statistics (frequencies, means, SDs) and t test analysis to determine relationships between variables of A1c, LDL-C, and frequency of visits. Improved diabetic outcomes, as previously defined, inferred that developing principles of a T2DM-PCMH clinic based on the principles of a PCMH provided a solution to optimal T2DM management compared with routine primary care delivery, consisting of a TRICARE-assigned PCM.
Results
A total of 638 unique patients were seen at the T2DM-PCMH clinic. Of these, 237 patient records in the database met the inclusion criteria and were acceptable for analysis and evaluation. Patients were omitted for the following reasons: 255 patients did not meet protocol of a minimum 2 visits during the evaluation period, 77 patients were omitted due to no second A1c available, 65 patients did not meet the clinic protocol of a A1c of > 6.5%, and 4 were omitted because no A1c was available for pre- or postanalysis. Data analysis and evaluation of the remaining 237 acceptable patients demonstrated that a T2DM-PCMH approach provided improved diabetic care compared with routine, PCM management.
Patients enrolled at the WBAMC T2DM clinic demonstrated clinically significant improvement (P < .001), and 80.5% achieved > 1% improvement in glycemic control. The greatest number of visits of 26 visits, an outlier not typical of the frequency of patient visits, was attributed to brittle T2DM requiring more frequent monitoring. Most patients had 3 T2DM-PCMH clinic appointments (2 were the minimum visits described in clinic protocol).
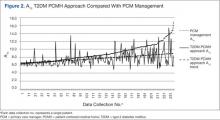
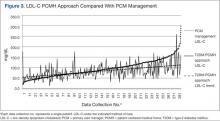
Low-density lipoprotein cholesterol levels were analyzed to determine whether patients with diabetes managed at the WBAMC T2DM clinic also had improved lipid control. A total of 638 patients had an initial LDL-C level drawn prior to clinic management. Of these patients, 282 were acceptable for analysis (Figure 2). Low-density lipoprotein cholesterol data were omitted because 93 did not have a paired pre- and postvalues, 8 values were invalid due to nonfasting laboratory status; and 255 values were omitted due to having < 2 clinic visits. Results of the data analysis demonstrated that LDL-C was well managed by the T2DM clinic, with levels ≤ 100 mg/dL (P < .001) (Figure 3).
Discussion
The WBAMC T2DM clinic was formed as a trial clinic at a medical treatment facility (MTF) MEDCEN due to the failure of routine PCM care to improve outcomes in the management of the diabetes population (A1c < 7.0%). Overall, improved endpoints of A1c, LDL-C were achieved with the disease-specific PCMH approach compared with routine PCM approach. The results indicate that disease-specific management leads to improved diabetic endpoints (A1c reduction by at least 1% and LDL-C < 100 mg/dL). The clinic’s protocol (listed in the methods) was intended to improve continuity.
A review of the literature confirmed that continuity of care is integral to patient satisfaction and improved diabetes management.8,10,17,28,29 The results of the study were consistent with those in the literature. The review of the literature established that patients who develop a trusting relationship with the health care provider as the T2DM clinic promoted (eg, frequent patient appointments, telecommunication by nurse, and patient participation) are more likely to follow medical therapy and take a proactive role in disease management.6,28,30
Conclusion
This study demonstrated that PCMH-delivered care offers a solution to suboptimal management of chronic disease, such as T2DM, and that chronic disease is best managed by implementation of a disease-specific PCMH. It is recommended that a MTF develop other disease-specific PCMH and pilot-test these programs. Long-term follow-up studies and additional data collection, such as blood pressure control, abdominal circumference, body mass index, and triglyceride levels would be useful to determine effectiveness.
Based on principles of a PCMH, the efficacy of the T2DM clinic at WBAMC demonstrated that improved diabetes management was achieved by increased continuity of care; intensive, repeated patient education; and a multidisciplinary team approach. The CDC identifies self-management training as foundational to improving health outcomes and QOL for individuals with diabetes.1 Primary care providers in a MTF may improve diabetic patient outcomes by referring patients to a T2DM clinic, such as the WBAMC T2DM clinic. The multidisciplinary team facilitated patient empowerment by educating patients on the management of their disease and the problem-solving and coping skills required to manage a chronic disease.
The WBAMC T2DM-PCMH based mission of fostering patient empowerment and a team approach is a comprehensive approach to diabetes care. Currently, the PCMH model is being adapted by the military in the latest health care reform initiatives.14 However, the move toward the PCMH model does not incorporate disease-specific PCMH clinics. This study demonstrates that the disease-specific PCMH approach provides improved disease management and may be effective in other chronic disease management. A benefit of the T2DM-PCMH approach is the reduced burden of escalating health care costs related to increased morbidity and mortality, which is associated with the growing health care problem of poorly controlled T2DM.1,4,31
The disease-specific clinic evaluated at WBAMC provides an effective solution to fragmented health care for the optimal management of T2DM. The clinic’s conceptual framework of increased access to care, with consistent education at closer time intervals when compared with PCM management resulted in improved continuity and T2DM control. Future research in this area should assess measurable cost reduction. Improved disease management as demonstrated by the T2DM disease-specific clinic at WBAMC provides sufficient incentive to incorporate similar T2DM continuity clinics and changes throughout MTFs.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Centers for Disease Control and Prevention (CDC). National Diabetes Fact Sheet, 2014. CDC Website. http://www.cdc.gov/diabetes/data/statistics/2014StatisticsReport.html. Updated October 24, 2014. Accessed November 6, 2014.
2. American Diabetes Association. National Diabetes Fact Sheet. Statistics about diabetes. American Diabetes Association Website. http://www.diabetes.org/diabetes-basics/diabetes-statistics. Released June 10, 2014. Accessed November 6, 2014.
3. Centers for Disease Control and Prevention (CDC). Number of Americans with diabetes rises to nearly 26 million [press release]. CDC Website. http://www.cdc.gov/media/releases/2011/p0126_diabetes.html. Published January 26, 2011. Accessed November 6, 2014.
4. Huang ES, Basu A, O’Grady M, Capretta JC. Projecting the future diabetes population size and related costs for the U.S. Diabetes Care. 2009;32(12):2225-2229.
5. National Library of Medicine. Diabetes. PubMed Website. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0002194. Reviewed May 24, 2013. Accessed November 6, 2014.
6. Chu-Weininger MY, Balkrishnan R. Consumer satisfaction with primary care provider choice and associated trust. BMC Health Serv Res. 2006;6:139.
7. Alazri MH, Neal RD, Heywood P, Leese B. Patients’ experience of continuity of care of type 2 diabetes: A focus group study in primary care. Br J Gen Prac. 2006;56(528):488-495.
8. Chen CC, Chen SH. Better continuity of care reduces costs for diabetic patients. Am J Manag Care. 2011;17(6):420-427.
9. TRICARE Regional Office-West. Military Treatment Facility (MTF) Profile of William Beaumont Army Medical Center, FY2010 Q2. El Paso, TX. Published March 2010.
10. Worrall G, Knight J. Continuity of care is good for elderly people with diabetes: Retrospective cohort study of mortality and hospitalization. Can Fam Physician. 2011;57(1):e6-e20.
11. Kerr M. ADA 2009: Expert committee recommends use of hemoglobin A1c for diagnosis. Medscape Website. http://www.medscape.com/viewarticle/704021. Published June 7, 2009. Accessed November 7, 2014.
12. Drexler AJ. Lessons learned from landmark trials of type 2 diabetes mellitus and potential applications to clinical practice. Postgrad Med. 2003;Spec No:15-26.
13. Office of Evidence-Based Practice Quality Management Division U.S. Army Medical Command. Population Health: Update of HEDIS measures. U.S. Army Medical Department Office of Quality Management Website. https://www.qmo.amedd.army.mil/HEDIS/HEDIS_MeasuresAcrossAMEDD.pdf. Published April 2010. Accessed November 2014.
14. Schoomaker E. Army medicine: Bringing value and inspiring trust. U.S. Medicine. 2011:10-13.
15. Sia C, Tonniges TF, Osterhus E, Taba S. History of the medical home concept. Pediatrics. 2004;113(5 suppl):1473-1478.
16. Kugler JP. Military Health System Patient Centered Medical Home Guide. Defense Health Agency Website. http://www.tricare.mil/tma/ocmo/download/MHSPCMHGuide.pdf. Published June 2011. Accessed November 11, 2014.
17. Naithani S, Gulliford M. Morgan M. Patients’ perceptions and experiences of ‘continuity of care’ in diabetes. Health Expect. 2006;9(2):118-129.
18. O’Malley AS, Cunningham PJ. Patient experiences with coordination of care: The benefit of continuity and primary care physician as referral source. J Gen Intern Med. 2009;24(2):170-177.
19. American Academy of Family Practice, American Academy of Pediatrics, American College of Physicians, and the American Osteopathic Association. Joint principles of the patient-centered medical home. American Academy of Family Practice Website. http://www.aafp.org/dam/AAFP/documents/practice_management/pcmh/initiatives/PCMHJoint.pdf. Published February 2007. Accessed November 7, 2014.
20. Meyer JA, Silow-Carroll S, Kutyla T, Stepnick LS, Rybowski LS. Hospital Quality: Ingredients for Success--Overview and Lessons Learned. New York, New York: The Commonwealth Fund; 2004.
21. Polit DF, Beck CT. Nursing Research: Generating and Assessing Evidence for Nursing Practice. 8th ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2008.
22. American Association of Clinical Endocrinologists. American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice. American Association of Clinical Endocrinologists Website. https://www.aace.com/files/dm-guidelines-ccp.pdf. Accessed November 7, 2014.
23. Skinner BF. The Behavior of Organisms: An Experimental Analysis. New York, NY: Appleton-Century; 1938.
24. Staddon JE, Cerutti DT. Operant conditioning. Annu Rev Psychol. 2003;54:115-144.
25. Bruner RF. Repetition Is the First Principle of All Learning. Social Science Research network Website. http://papers.ssrn.com/sol3/papers.cfm?abstract_id=224340. Posted August 26, 2001. Accessed November 7, 2014.
26. Institute of Medicine. The Future Of Nursing: Leading Change, Advancing Health. Washington, DC: National Academics Press; 2011.
27. Willens D, Cripps R, Wilson A, Wolff K, Rothman R. Interdisciplinary team care for diabetic patients by primary care physicians, advance practice nurses and clinical pharmacists. Clin Diabetes. 2011;29(2):60-68.
28. Renders CM, Valk GD, Griffin S, Wagner EH, Eijk JT, Assendelft WJ. Interventions to improve the management of diabetes mellitus in primary care, outpatient and community settings. Cochrane Database Syst Rev. 2001;(1):CD001481.
29. Health Affairs. Patient-centered medical homes. Health Affairs Website. http://www.healthaffairs.org. Dated September 14, 2010. Accessed November 7, 2014.
30. Berry LL, Parish JT, Janakiraman R, et al. Patients’ commitment to their primary physician and why it matters. Ann Fam Med. 2008;6(1):6-13.
31. Glasgow RE, Wagner EH, Kaplan RM, Vinicor F, Smith L, Norman J. If diabetes is a public health problem, why not treat it as one? A population-based approach to chronic illness. Ann Behav Med. 1999;21(2):159-170.
Type 2 diabetes mellitus (T2DM) is a significant, growing health problem that results in increased morbidity and mortality. In adults, T2DM accounts for about 90% to 95% of all diagnosed cases of diabetes.1 Diabetes is the leading cause of kidney failure and blindness; moreover, diabetic patients are 2 to 4 times more likely to die of complications of heart disease and/or have a stroke.2 Other complications of diabetes include nervous system damage and nontraumatic lower limb amputation. Increased morbidity and mortality not only diminishes quality of life (QOL) for patients with diabetes, but also produces a financial health care burden. The cost of diabetes in the U.S. in 2012 was more than $245 billion compared with $174 billion in 2007.1
The Centers for Disease Control and Prevention (CDC) predicts that 1 in 3 American adults will develop diabetes by 2050; thus, optimal approaches to diabetic care need to be developed and evaluated to determine best practices.3,4 Better control of blood sugar, cholesterol, and blood pressure levels in people with diabetes will help reduce the risk of complications of kidney disease, eye disease, nervous system disease, heart attack, and stroke.5 Optimal approaches to diabetes management must now be developed to prepare for the forecasted increase of T2DM.
A review of the literature confirms that lack of continuity of care often leads to patient dissatisfaction with health care, to fragmented health care, and a greater propensity to disregard a defined health care treatment plan.6,7 In addition to improved patient satisfaction and adherence to medical management, improved continuity of care is cost-effective. A longitudinal study based on claims data from 2000 to 2008, using the continuity of care index, indicated that improved continuity of care was associated with less health care waste and lower health care expenses for patients with T2DM.8 An average savings of $737 in total health care expenses per person was achieved with better continuity of care.8 These studies demonstrate that improving continuity of care improves outcomes in patients with diabetes and helps prevent excessive health care costs and waste.
Medical Center NonContinuity
Lack of continuity of care has been identified as a potential obstacle to optimal diabetic outcomes at William Beaumont Army Medical Center (WBAMC) in El Paso, Texas, based on a recent data analysis provided by TRICARE Regional Office West.9,10 As of March 2010, 56,936 patients were enrolled in TRICARE Prime. Of these patients, only 29.92% had appointments with their assigned primary care manager (PCM).9
In 2009, WBAMC developed a database to track the Healthcare Effectiveness Data and Information Set (HEDIS) measures to monitor A1c as well as other indicators of performance of health care services, such as mammography, Pap smear, bone densitometry, and colorectal screening. A recent American Diabetic Association expert committee recommendation endorsed the use of A1c value > 6.5% to confirm the diagnosis of diabetes.11 The A1c test may be confirmed with a repeat test unless clinical symptoms exist or the patient has random glucose levels > 200 mg/dL. Importantly, individuals with an A1c between 6% and 6.5% have a higher risk for developing diabetes and may be diagnosed with prediabetes.3
From 2008 to 2009, the HEDIS database tracking the progress of A1c demonstrated a 0.3% positive change and improvement in A1c ≤ 9% (normal 4%-6%). The goal for people with diabetes is A1c < 7%. Uncontrolled diabetes, (ie, A1c > 9%), is associated with greater diabetes-related complications.12 Using the HEDIS benchmark of ≥ 9%, the HEDIS A1c data for fiscal year (FY) 2008 were 71.1 (p50) and 81 (p90), and for FY 2009 were 72.2 (p50) and 81.3 (p90), reflecting p90 0.3% improvement.13 Therefore, these data reflect poor outcomes of patients with T2DM with A1c levels that were not controlled at WBAMC.
Uncontrolled diabetes accrues significant health care costs and adverse diabetic outcomes.10 Consequently, the WBAMC clinical operations division, which was tasked to monitor the HEDIS database, identified and contacted individuals to schedule health care appointments. The primary endeavor was an attempt to substantially increase benchmarks and maintain levels of A1c < 9%, demonstrate improvement in quality of care, and reduce health care costs. Unfortunately, these goals were not met for the aggregate of patients with T2DM.
Figure 1 illustrates how the diabetic population at WBAMC had experienced decreased continuity of care and the adverse effects on their diabetes management. Figure 1 also illustrates how beneficiaries of TRICARE are assigned a PCM and how this process results in a lack of continuity of care for patients with T2DM. An Army medical center (MEDCEN) typically uses PCMs who may be a physician, nurse practitioner (NP), or physician assistant. Unfortunately, the majority of these PCMs are active-duty military or civil service personnel who commonly undergo permanent change of station moves or deployments every 3 years. Additionally, military providers are often rotated through department-chief positions, thereby dissolving their patient relationships.
Frequent rotations offer a valid means to foster leadership skills much needed in a military conflict zone and maximize military professional development; however, rotations also contribute to the lack of continuity of patient care. This PCM instability and the distinctive military dynamic volatility are characteristic of standard military operating procedure and are unlikely to change.
New solutions are needed to promote improved continuity of care for patients with diabetes at a MEDCEN. According to Lt Gen Eric Schoomaker, former Surgeon General of the Army, “The Patient-Centered Medical Home concept is being adopted throughout the military health system.”14 The goal of the trend toward patient-centered medical home (PCMH) care delivery is to improve access to high-quality health care services.13
Patient-Centered Medical Home
The term patient-centered medical home was introduced in 1967 by the American Academy of Pediatrics (AAP).15 In 2008, PCMH principles became integral in most health care reform initiatives.16 In most PCMH models, increased continuity of care is the single common denominator of practice. Continuity of care is defined as intensified integration, coordination, and sharing of information between disciplines that result in improved patient outcomes.10,17,18
In 2007, a consensus statement was provided by the American Academy of Family Practice, the AAP, American College of Physicians, and the American Osteopathic Association stating that quality and safety are hallmarks of the PCMH and may improve outcomes for chronic disease, such as diabetes.19
Quality improvement is vital in health care organizations because of demands by government agencies, health maintenance organizations, and the public to continually improve services and to provide the highest quality health care at the best cost.20 Diabetes has become a public health crisis, as previously discussed, and a comprehensive approach to care management is essential. Developing an optimal process for diabetes health care and methods for evaluation of the delivery process is foundational for all stakeholders involved, including health care organizations, health care providers, and patients.20
Diabetic outcomes were evaluated at a recent 2-year trial PCMH approach T2DM clinic at a MEDCEN at WBAMC. The purpose of the project was to determine whether a PCMH approach improves disease management compared with routine primary care management.
Methods
The process and manner of care delivery was the focus of this analysis and evaluation, not clinician knowledge of treatment management. A comparison of care delivery approaches of PCM management and PCMH care delivery is displayed in the Table. The treatment algorithm for T2DM was not in question, because guidelines for practice are established based on scientific evidence, and medication management is based on evidence-based practice.21,22 Evaluation consisted of T2DM delivery of care process and the efficacy of outcome achieved by the specified delivery of care: (a) increased access to care; (b) intensive, repeated education; and (3) a multidisciplinary approach focused on patient empowerment. The following is a description of the specified delivery of care.
Increased Access to Care
Increased access to care addressed through frequent telecommunication provided by the registered nurse (RN) case manager who regularly called patients within 72 hours of insulin adjustment or 24 hours for insulin initiation or significant medication changes. Additionally, the diabetes team providers requested a follow-up appointment in 1 week when injectable medication was added or changes were made in insulin management. One exception was for the addition of livaglutide, in which a 2-week follow-up was made, to allow for titration of the medication. For oral medication adjustment, a 1-month follow-up was generally made, with a 2-month follow-up when a glucose histogram indicated optimal glycemic control, an average blood glucose of 7% (estimated average glucose of 154 mg/dL) or less. Time for appointments was increased by 10 minutes for a total of 30-minute appointments, compared with 20 minutes for PCM delivery.
Informational continuity was thought to be improved by use of an electronic medical record (EMR), allowing for an uninterrupted patient record. Providers were expected to document medication reconciliation with a clear explanation of medication adjustments listed in the plan. Patient teaching was documented, describing the specific patient education concerns addressed. Other data included a glucometer statistical report from the last appointment to the current appointment, to track negative or positive changes in glycemic control.
Patient Education
The management technique used in the clinic was intensive, repeated education with the goal of improving learning and retention with repeated instruction and positive reinforcement. Skinner theorized that learning is the acquisition of new behavior through conditioning (eg, repeated instruction), is in close proximity of time, and is likely to result in learning retention, which remain relevant education practice.23,24 The T2DM clinic operates on Skinner’s principles of repeated, intensive education. For example, patients must bring their glucometer to every appointment. The statistical analysis downloaded from the glucometer provides immediate reinforcement and information about patients’ glycemic control. Patients are typically excited to see an improvement from previous levels and are encouraged to continue behavior modification. Conversely, statistical analysis demonstrating poor glycemic control generally encourages the patient to make needed lifestyle changes. Thus, changes in behavior due to intensive, repeated education, followed by a reinforcing stimulus results in an increased probability of that behavior occurring in the future.23,25 The interdisciplinary team provides education during each T2DM patient encounter.
Multidisciplinary Approach
The multidisciplinary team formed at the trial T2DM clinic consisted of a medical doctor, family NP, pharmacist, RN, licensed vocational nurse, and registered dietician. The team members were each encouraged to obtain Certified Diabetes Educator (CDE) certification. For the first 6 months of developing the clinic, staff scheduled weekly team-building meetings to encourage esprit de corps. The weekly meetings were also used to discuss difficult patient cases. The RN case manager provided the patients with individualized plans to help them meet specified goals and provided easy accessibility for patient questions and concerns. The pharmacist was integral in helping patients understand the role of their medication and was also certified to make medication adjustments related to diabetes.
A recent Institute of Medicine (IOM) report encouraged the expansion of roles for nurse practitioners (NPs) in coordination and primary care delivery.26 The IOM collaborative statement is based on numerous studies showing that NPs provided equivalent quality of care compared with that of primary care physicians in routine chronic disease management.26 Nurse case managers functioned as an integral part of the intensive therapy involved in the landmark Diabetes Control and Complication Trial.27
The intended policy analysis and outcome evaluation was confined to data collected from a disease-specific (T2DM) clinic with a PCMH approach developed April 2011 at WBAMC. Data were obtained from the WBAMC database designed to track the HEDIS measures.
Enrollees of the clinic were restricted to patients diagnosed with T2DM who were TRICARE beneficiaries. Males and females, aged > 20 years with an established A1c > 6.5% comprised the patient population of the clinic. Individuals who were managed by WBAMC or were TRICARE standard beneficiaries were excluded from the study. Because patients with T1DM have a different pathology than those with T2DM, they were referred to endocrinology. Patients with gestational diabetes were referred to obstetrics for management.
Data Collection
Existing data in the Armed Forces Health Longitudinal Technology Application (AHLTA) EMR were used for this analysis. Data were accessed by a Common Access Card (CAC card) enhanced security system accessed only through secure CAC applications.
Diabetic outcomes of glycemic control as measured by the A1c value were examined prior to clinic enrollment (time 1: PCM care delivery) and subsequently (time 2: PCMH care delivery) at the health care provider’s discretion. The second time varied between 2 and 6 months, depending on (1) provider need to determine quickly (2 months) whether a downward trend was occurring because of multiple comorbidities; (2) provider discretion to wait an additional 3 months (A1c turnover x 2 = 6 months), while medication adjustments are being made; and (3) according to feasibility of follow-up based on patient’s scheduling. Low-density lipoprotein cholesterol (LDL-C) was also examined at both PCM care delivery and PCMH care delivery.
The endpoints of a reduction in A1c by 1% and an LDL-C that is ≤ 100 mg/dL determined improved diabetes outcomes. Existing data (eg, glycemic control [A1c], lipid control [LDL-C]), from April 1, 2011, to December 31, 2011, were logged in a clinic database. These data served to demonstrate the effectiveness of the T2DM PCMH approach to clinic management. The PCMH principles that were examined included the standard operating procedure for the T2DM-PCMH clinic: frequent appointments > 2 in a 3-month period), a multidisciplinary team, and intensive, repeated education.
Data analysis was conducted with descriptive statistics (frequencies, means, SDs) and t test analysis to determine relationships between variables of A1c, LDL-C, and frequency of visits. Improved diabetic outcomes, as previously defined, inferred that developing principles of a T2DM-PCMH clinic based on the principles of a PCMH provided a solution to optimal T2DM management compared with routine primary care delivery, consisting of a TRICARE-assigned PCM.
Results
A total of 638 unique patients were seen at the T2DM-PCMH clinic. Of these, 237 patient records in the database met the inclusion criteria and were acceptable for analysis and evaluation. Patients were omitted for the following reasons: 255 patients did not meet protocol of a minimum 2 visits during the evaluation period, 77 patients were omitted due to no second A1c available, 65 patients did not meet the clinic protocol of a A1c of > 6.5%, and 4 were omitted because no A1c was available for pre- or postanalysis. Data analysis and evaluation of the remaining 237 acceptable patients demonstrated that a T2DM-PCMH approach provided improved diabetic care compared with routine, PCM management.
Patients enrolled at the WBAMC T2DM clinic demonstrated clinically significant improvement (P < .001), and 80.5% achieved > 1% improvement in glycemic control. The greatest number of visits of 26 visits, an outlier not typical of the frequency of patient visits, was attributed to brittle T2DM requiring more frequent monitoring. Most patients had 3 T2DM-PCMH clinic appointments (2 were the minimum visits described in clinic protocol).
Low-density lipoprotein cholesterol levels were analyzed to determine whether patients with diabetes managed at the WBAMC T2DM clinic also had improved lipid control. A total of 638 patients had an initial LDL-C level drawn prior to clinic management. Of these patients, 282 were acceptable for analysis (Figure 2). Low-density lipoprotein cholesterol data were omitted because 93 did not have a paired pre- and postvalues, 8 values were invalid due to nonfasting laboratory status; and 255 values were omitted due to having < 2 clinic visits. Results of the data analysis demonstrated that LDL-C was well managed by the T2DM clinic, with levels ≤ 100 mg/dL (P < .001) (Figure 3).
Discussion
The WBAMC T2DM clinic was formed as a trial clinic at a medical treatment facility (MTF) MEDCEN due to the failure of routine PCM care to improve outcomes in the management of the diabetes population (A1c < 7.0%). Overall, improved endpoints of A1c, LDL-C were achieved with the disease-specific PCMH approach compared with routine PCM approach. The results indicate that disease-specific management leads to improved diabetic endpoints (A1c reduction by at least 1% and LDL-C < 100 mg/dL). The clinic’s protocol (listed in the methods) was intended to improve continuity.
A review of the literature confirmed that continuity of care is integral to patient satisfaction and improved diabetes management.8,10,17,28,29 The results of the study were consistent with those in the literature. The review of the literature established that patients who develop a trusting relationship with the health care provider as the T2DM clinic promoted (eg, frequent patient appointments, telecommunication by nurse, and patient participation) are more likely to follow medical therapy and take a proactive role in disease management.6,28,30
Conclusion
This study demonstrated that PCMH-delivered care offers a solution to suboptimal management of chronic disease, such as T2DM, and that chronic disease is best managed by implementation of a disease-specific PCMH. It is recommended that a MTF develop other disease-specific PCMH and pilot-test these programs. Long-term follow-up studies and additional data collection, such as blood pressure control, abdominal circumference, body mass index, and triglyceride levels would be useful to determine effectiveness.
Based on principles of a PCMH, the efficacy of the T2DM clinic at WBAMC demonstrated that improved diabetes management was achieved by increased continuity of care; intensive, repeated patient education; and a multidisciplinary team approach. The CDC identifies self-management training as foundational to improving health outcomes and QOL for individuals with diabetes.1 Primary care providers in a MTF may improve diabetic patient outcomes by referring patients to a T2DM clinic, such as the WBAMC T2DM clinic. The multidisciplinary team facilitated patient empowerment by educating patients on the management of their disease and the problem-solving and coping skills required to manage a chronic disease.
The WBAMC T2DM-PCMH based mission of fostering patient empowerment and a team approach is a comprehensive approach to diabetes care. Currently, the PCMH model is being adapted by the military in the latest health care reform initiatives.14 However, the move toward the PCMH model does not incorporate disease-specific PCMH clinics. This study demonstrates that the disease-specific PCMH approach provides improved disease management and may be effective in other chronic disease management. A benefit of the T2DM-PCMH approach is the reduced burden of escalating health care costs related to increased morbidity and mortality, which is associated with the growing health care problem of poorly controlled T2DM.1,4,31
The disease-specific clinic evaluated at WBAMC provides an effective solution to fragmented health care for the optimal management of T2DM. The clinic’s conceptual framework of increased access to care, with consistent education at closer time intervals when compared with PCM management resulted in improved continuity and T2DM control. Future research in this area should assess measurable cost reduction. Improved disease management as demonstrated by the T2DM disease-specific clinic at WBAMC provides sufficient incentive to incorporate similar T2DM continuity clinics and changes throughout MTFs.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Type 2 diabetes mellitus (T2DM) is a significant, growing health problem that results in increased morbidity and mortality. In adults, T2DM accounts for about 90% to 95% of all diagnosed cases of diabetes.1 Diabetes is the leading cause of kidney failure and blindness; moreover, diabetic patients are 2 to 4 times more likely to die of complications of heart disease and/or have a stroke.2 Other complications of diabetes include nervous system damage and nontraumatic lower limb amputation. Increased morbidity and mortality not only diminishes quality of life (QOL) for patients with diabetes, but also produces a financial health care burden. The cost of diabetes in the U.S. in 2012 was more than $245 billion compared with $174 billion in 2007.1
The Centers for Disease Control and Prevention (CDC) predicts that 1 in 3 American adults will develop diabetes by 2050; thus, optimal approaches to diabetic care need to be developed and evaluated to determine best practices.3,4 Better control of blood sugar, cholesterol, and blood pressure levels in people with diabetes will help reduce the risk of complications of kidney disease, eye disease, nervous system disease, heart attack, and stroke.5 Optimal approaches to diabetes management must now be developed to prepare for the forecasted increase of T2DM.
A review of the literature confirms that lack of continuity of care often leads to patient dissatisfaction with health care, to fragmented health care, and a greater propensity to disregard a defined health care treatment plan.6,7 In addition to improved patient satisfaction and adherence to medical management, improved continuity of care is cost-effective. A longitudinal study based on claims data from 2000 to 2008, using the continuity of care index, indicated that improved continuity of care was associated with less health care waste and lower health care expenses for patients with T2DM.8 An average savings of $737 in total health care expenses per person was achieved with better continuity of care.8 These studies demonstrate that improving continuity of care improves outcomes in patients with diabetes and helps prevent excessive health care costs and waste.
Medical Center NonContinuity
Lack of continuity of care has been identified as a potential obstacle to optimal diabetic outcomes at William Beaumont Army Medical Center (WBAMC) in El Paso, Texas, based on a recent data analysis provided by TRICARE Regional Office West.9,10 As of March 2010, 56,936 patients were enrolled in TRICARE Prime. Of these patients, only 29.92% had appointments with their assigned primary care manager (PCM).9
In 2009, WBAMC developed a database to track the Healthcare Effectiveness Data and Information Set (HEDIS) measures to monitor A1c as well as other indicators of performance of health care services, such as mammography, Pap smear, bone densitometry, and colorectal screening. A recent American Diabetic Association expert committee recommendation endorsed the use of A1c value > 6.5% to confirm the diagnosis of diabetes.11 The A1c test may be confirmed with a repeat test unless clinical symptoms exist or the patient has random glucose levels > 200 mg/dL. Importantly, individuals with an A1c between 6% and 6.5% have a higher risk for developing diabetes and may be diagnosed with prediabetes.3
From 2008 to 2009, the HEDIS database tracking the progress of A1c demonstrated a 0.3% positive change and improvement in A1c ≤ 9% (normal 4%-6%). The goal for people with diabetes is A1c < 7%. Uncontrolled diabetes, (ie, A1c > 9%), is associated with greater diabetes-related complications.12 Using the HEDIS benchmark of ≥ 9%, the HEDIS A1c data for fiscal year (FY) 2008 were 71.1 (p50) and 81 (p90), and for FY 2009 were 72.2 (p50) and 81.3 (p90), reflecting p90 0.3% improvement.13 Therefore, these data reflect poor outcomes of patients with T2DM with A1c levels that were not controlled at WBAMC.
Uncontrolled diabetes accrues significant health care costs and adverse diabetic outcomes.10 Consequently, the WBAMC clinical operations division, which was tasked to monitor the HEDIS database, identified and contacted individuals to schedule health care appointments. The primary endeavor was an attempt to substantially increase benchmarks and maintain levels of A1c < 9%, demonstrate improvement in quality of care, and reduce health care costs. Unfortunately, these goals were not met for the aggregate of patients with T2DM.
Figure 1 illustrates how the diabetic population at WBAMC had experienced decreased continuity of care and the adverse effects on their diabetes management. Figure 1 also illustrates how beneficiaries of TRICARE are assigned a PCM and how this process results in a lack of continuity of care for patients with T2DM. An Army medical center (MEDCEN) typically uses PCMs who may be a physician, nurse practitioner (NP), or physician assistant. Unfortunately, the majority of these PCMs are active-duty military or civil service personnel who commonly undergo permanent change of station moves or deployments every 3 years. Additionally, military providers are often rotated through department-chief positions, thereby dissolving their patient relationships.
Frequent rotations offer a valid means to foster leadership skills much needed in a military conflict zone and maximize military professional development; however, rotations also contribute to the lack of continuity of patient care. This PCM instability and the distinctive military dynamic volatility are characteristic of standard military operating procedure and are unlikely to change.
New solutions are needed to promote improved continuity of care for patients with diabetes at a MEDCEN. According to Lt Gen Eric Schoomaker, former Surgeon General of the Army, “The Patient-Centered Medical Home concept is being adopted throughout the military health system.”14 The goal of the trend toward patient-centered medical home (PCMH) care delivery is to improve access to high-quality health care services.13
Patient-Centered Medical Home
The term patient-centered medical home was introduced in 1967 by the American Academy of Pediatrics (AAP).15 In 2008, PCMH principles became integral in most health care reform initiatives.16 In most PCMH models, increased continuity of care is the single common denominator of practice. Continuity of care is defined as intensified integration, coordination, and sharing of information between disciplines that result in improved patient outcomes.10,17,18
In 2007, a consensus statement was provided by the American Academy of Family Practice, the AAP, American College of Physicians, and the American Osteopathic Association stating that quality and safety are hallmarks of the PCMH and may improve outcomes for chronic disease, such as diabetes.19
Quality improvement is vital in health care organizations because of demands by government agencies, health maintenance organizations, and the public to continually improve services and to provide the highest quality health care at the best cost.20 Diabetes has become a public health crisis, as previously discussed, and a comprehensive approach to care management is essential. Developing an optimal process for diabetes health care and methods for evaluation of the delivery process is foundational for all stakeholders involved, including health care organizations, health care providers, and patients.20
Diabetic outcomes were evaluated at a recent 2-year trial PCMH approach T2DM clinic at a MEDCEN at WBAMC. The purpose of the project was to determine whether a PCMH approach improves disease management compared with routine primary care management.
Methods
The process and manner of care delivery was the focus of this analysis and evaluation, not clinician knowledge of treatment management. A comparison of care delivery approaches of PCM management and PCMH care delivery is displayed in the Table. The treatment algorithm for T2DM was not in question, because guidelines for practice are established based on scientific evidence, and medication management is based on evidence-based practice.21,22 Evaluation consisted of T2DM delivery of care process and the efficacy of outcome achieved by the specified delivery of care: (a) increased access to care; (b) intensive, repeated education; and (3) a multidisciplinary approach focused on patient empowerment. The following is a description of the specified delivery of care.
Increased Access to Care
Increased access to care addressed through frequent telecommunication provided by the registered nurse (RN) case manager who regularly called patients within 72 hours of insulin adjustment or 24 hours for insulin initiation or significant medication changes. Additionally, the diabetes team providers requested a follow-up appointment in 1 week when injectable medication was added or changes were made in insulin management. One exception was for the addition of livaglutide, in which a 2-week follow-up was made, to allow for titration of the medication. For oral medication adjustment, a 1-month follow-up was generally made, with a 2-month follow-up when a glucose histogram indicated optimal glycemic control, an average blood glucose of 7% (estimated average glucose of 154 mg/dL) or less. Time for appointments was increased by 10 minutes for a total of 30-minute appointments, compared with 20 minutes for PCM delivery.
Informational continuity was thought to be improved by use of an electronic medical record (EMR), allowing for an uninterrupted patient record. Providers were expected to document medication reconciliation with a clear explanation of medication adjustments listed in the plan. Patient teaching was documented, describing the specific patient education concerns addressed. Other data included a glucometer statistical report from the last appointment to the current appointment, to track negative or positive changes in glycemic control.
Patient Education
The management technique used in the clinic was intensive, repeated education with the goal of improving learning and retention with repeated instruction and positive reinforcement. Skinner theorized that learning is the acquisition of new behavior through conditioning (eg, repeated instruction), is in close proximity of time, and is likely to result in learning retention, which remain relevant education practice.23,24 The T2DM clinic operates on Skinner’s principles of repeated, intensive education. For example, patients must bring their glucometer to every appointment. The statistical analysis downloaded from the glucometer provides immediate reinforcement and information about patients’ glycemic control. Patients are typically excited to see an improvement from previous levels and are encouraged to continue behavior modification. Conversely, statistical analysis demonstrating poor glycemic control generally encourages the patient to make needed lifestyle changes. Thus, changes in behavior due to intensive, repeated education, followed by a reinforcing stimulus results in an increased probability of that behavior occurring in the future.23,25 The interdisciplinary team provides education during each T2DM patient encounter.
Multidisciplinary Approach
The multidisciplinary team formed at the trial T2DM clinic consisted of a medical doctor, family NP, pharmacist, RN, licensed vocational nurse, and registered dietician. The team members were each encouraged to obtain Certified Diabetes Educator (CDE) certification. For the first 6 months of developing the clinic, staff scheduled weekly team-building meetings to encourage esprit de corps. The weekly meetings were also used to discuss difficult patient cases. The RN case manager provided the patients with individualized plans to help them meet specified goals and provided easy accessibility for patient questions and concerns. The pharmacist was integral in helping patients understand the role of their medication and was also certified to make medication adjustments related to diabetes.
A recent Institute of Medicine (IOM) report encouraged the expansion of roles for nurse practitioners (NPs) in coordination and primary care delivery.26 The IOM collaborative statement is based on numerous studies showing that NPs provided equivalent quality of care compared with that of primary care physicians in routine chronic disease management.26 Nurse case managers functioned as an integral part of the intensive therapy involved in the landmark Diabetes Control and Complication Trial.27
The intended policy analysis and outcome evaluation was confined to data collected from a disease-specific (T2DM) clinic with a PCMH approach developed April 2011 at WBAMC. Data were obtained from the WBAMC database designed to track the HEDIS measures.
Enrollees of the clinic were restricted to patients diagnosed with T2DM who were TRICARE beneficiaries. Males and females, aged > 20 years with an established A1c > 6.5% comprised the patient population of the clinic. Individuals who were managed by WBAMC or were TRICARE standard beneficiaries were excluded from the study. Because patients with T1DM have a different pathology than those with T2DM, they were referred to endocrinology. Patients with gestational diabetes were referred to obstetrics for management.
Data Collection
Existing data in the Armed Forces Health Longitudinal Technology Application (AHLTA) EMR were used for this analysis. Data were accessed by a Common Access Card (CAC card) enhanced security system accessed only through secure CAC applications.
Diabetic outcomes of glycemic control as measured by the A1c value were examined prior to clinic enrollment (time 1: PCM care delivery) and subsequently (time 2: PCMH care delivery) at the health care provider’s discretion. The second time varied between 2 and 6 months, depending on (1) provider need to determine quickly (2 months) whether a downward trend was occurring because of multiple comorbidities; (2) provider discretion to wait an additional 3 months (A1c turnover x 2 = 6 months), while medication adjustments are being made; and (3) according to feasibility of follow-up based on patient’s scheduling. Low-density lipoprotein cholesterol (LDL-C) was also examined at both PCM care delivery and PCMH care delivery.
The endpoints of a reduction in A1c by 1% and an LDL-C that is ≤ 100 mg/dL determined improved diabetes outcomes. Existing data (eg, glycemic control [A1c], lipid control [LDL-C]), from April 1, 2011, to December 31, 2011, were logged in a clinic database. These data served to demonstrate the effectiveness of the T2DM PCMH approach to clinic management. The PCMH principles that were examined included the standard operating procedure for the T2DM-PCMH clinic: frequent appointments > 2 in a 3-month period), a multidisciplinary team, and intensive, repeated education.
Data analysis was conducted with descriptive statistics (frequencies, means, SDs) and t test analysis to determine relationships between variables of A1c, LDL-C, and frequency of visits. Improved diabetic outcomes, as previously defined, inferred that developing principles of a T2DM-PCMH clinic based on the principles of a PCMH provided a solution to optimal T2DM management compared with routine primary care delivery, consisting of a TRICARE-assigned PCM.
Results
A total of 638 unique patients were seen at the T2DM-PCMH clinic. Of these, 237 patient records in the database met the inclusion criteria and were acceptable for analysis and evaluation. Patients were omitted for the following reasons: 255 patients did not meet protocol of a minimum 2 visits during the evaluation period, 77 patients were omitted due to no second A1c available, 65 patients did not meet the clinic protocol of a A1c of > 6.5%, and 4 were omitted because no A1c was available for pre- or postanalysis. Data analysis and evaluation of the remaining 237 acceptable patients demonstrated that a T2DM-PCMH approach provided improved diabetic care compared with routine, PCM management.
Patients enrolled at the WBAMC T2DM clinic demonstrated clinically significant improvement (P < .001), and 80.5% achieved > 1% improvement in glycemic control. The greatest number of visits of 26 visits, an outlier not typical of the frequency of patient visits, was attributed to brittle T2DM requiring more frequent monitoring. Most patients had 3 T2DM-PCMH clinic appointments (2 were the minimum visits described in clinic protocol).
Low-density lipoprotein cholesterol levels were analyzed to determine whether patients with diabetes managed at the WBAMC T2DM clinic also had improved lipid control. A total of 638 patients had an initial LDL-C level drawn prior to clinic management. Of these patients, 282 were acceptable for analysis (Figure 2). Low-density lipoprotein cholesterol data were omitted because 93 did not have a paired pre- and postvalues, 8 values were invalid due to nonfasting laboratory status; and 255 values were omitted due to having < 2 clinic visits. Results of the data analysis demonstrated that LDL-C was well managed by the T2DM clinic, with levels ≤ 100 mg/dL (P < .001) (Figure 3).
Discussion
The WBAMC T2DM clinic was formed as a trial clinic at a medical treatment facility (MTF) MEDCEN due to the failure of routine PCM care to improve outcomes in the management of the diabetes population (A1c < 7.0%). Overall, improved endpoints of A1c, LDL-C were achieved with the disease-specific PCMH approach compared with routine PCM approach. The results indicate that disease-specific management leads to improved diabetic endpoints (A1c reduction by at least 1% and LDL-C < 100 mg/dL). The clinic’s protocol (listed in the methods) was intended to improve continuity.
A review of the literature confirmed that continuity of care is integral to patient satisfaction and improved diabetes management.8,10,17,28,29 The results of the study were consistent with those in the literature. The review of the literature established that patients who develop a trusting relationship with the health care provider as the T2DM clinic promoted (eg, frequent patient appointments, telecommunication by nurse, and patient participation) are more likely to follow medical therapy and take a proactive role in disease management.6,28,30
Conclusion
This study demonstrated that PCMH-delivered care offers a solution to suboptimal management of chronic disease, such as T2DM, and that chronic disease is best managed by implementation of a disease-specific PCMH. It is recommended that a MTF develop other disease-specific PCMH and pilot-test these programs. Long-term follow-up studies and additional data collection, such as blood pressure control, abdominal circumference, body mass index, and triglyceride levels would be useful to determine effectiveness.
Based on principles of a PCMH, the efficacy of the T2DM clinic at WBAMC demonstrated that improved diabetes management was achieved by increased continuity of care; intensive, repeated patient education; and a multidisciplinary team approach. The CDC identifies self-management training as foundational to improving health outcomes and QOL for individuals with diabetes.1 Primary care providers in a MTF may improve diabetic patient outcomes by referring patients to a T2DM clinic, such as the WBAMC T2DM clinic. The multidisciplinary team facilitated patient empowerment by educating patients on the management of their disease and the problem-solving and coping skills required to manage a chronic disease.
The WBAMC T2DM-PCMH based mission of fostering patient empowerment and a team approach is a comprehensive approach to diabetes care. Currently, the PCMH model is being adapted by the military in the latest health care reform initiatives.14 However, the move toward the PCMH model does not incorporate disease-specific PCMH clinics. This study demonstrates that the disease-specific PCMH approach provides improved disease management and may be effective in other chronic disease management. A benefit of the T2DM-PCMH approach is the reduced burden of escalating health care costs related to increased morbidity and mortality, which is associated with the growing health care problem of poorly controlled T2DM.1,4,31
The disease-specific clinic evaluated at WBAMC provides an effective solution to fragmented health care for the optimal management of T2DM. The clinic’s conceptual framework of increased access to care, with consistent education at closer time intervals when compared with PCM management resulted in improved continuity and T2DM control. Future research in this area should assess measurable cost reduction. Improved disease management as demonstrated by the T2DM disease-specific clinic at WBAMC provides sufficient incentive to incorporate similar T2DM continuity clinics and changes throughout MTFs.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Centers for Disease Control and Prevention (CDC). National Diabetes Fact Sheet, 2014. CDC Website. http://www.cdc.gov/diabetes/data/statistics/2014StatisticsReport.html. Updated October 24, 2014. Accessed November 6, 2014.
2. American Diabetes Association. National Diabetes Fact Sheet. Statistics about diabetes. American Diabetes Association Website. http://www.diabetes.org/diabetes-basics/diabetes-statistics. Released June 10, 2014. Accessed November 6, 2014.
3. Centers for Disease Control and Prevention (CDC). Number of Americans with diabetes rises to nearly 26 million [press release]. CDC Website. http://www.cdc.gov/media/releases/2011/p0126_diabetes.html. Published January 26, 2011. Accessed November 6, 2014.
4. Huang ES, Basu A, O’Grady M, Capretta JC. Projecting the future diabetes population size and related costs for the U.S. Diabetes Care. 2009;32(12):2225-2229.
5. National Library of Medicine. Diabetes. PubMed Website. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0002194. Reviewed May 24, 2013. Accessed November 6, 2014.
6. Chu-Weininger MY, Balkrishnan R. Consumer satisfaction with primary care provider choice and associated trust. BMC Health Serv Res. 2006;6:139.
7. Alazri MH, Neal RD, Heywood P, Leese B. Patients’ experience of continuity of care of type 2 diabetes: A focus group study in primary care. Br J Gen Prac. 2006;56(528):488-495.
8. Chen CC, Chen SH. Better continuity of care reduces costs for diabetic patients. Am J Manag Care. 2011;17(6):420-427.
9. TRICARE Regional Office-West. Military Treatment Facility (MTF) Profile of William Beaumont Army Medical Center, FY2010 Q2. El Paso, TX. Published March 2010.
10. Worrall G, Knight J. Continuity of care is good for elderly people with diabetes: Retrospective cohort study of mortality and hospitalization. Can Fam Physician. 2011;57(1):e6-e20.
11. Kerr M. ADA 2009: Expert committee recommends use of hemoglobin A1c for diagnosis. Medscape Website. http://www.medscape.com/viewarticle/704021. Published June 7, 2009. Accessed November 7, 2014.
12. Drexler AJ. Lessons learned from landmark trials of type 2 diabetes mellitus and potential applications to clinical practice. Postgrad Med. 2003;Spec No:15-26.
13. Office of Evidence-Based Practice Quality Management Division U.S. Army Medical Command. Population Health: Update of HEDIS measures. U.S. Army Medical Department Office of Quality Management Website. https://www.qmo.amedd.army.mil/HEDIS/HEDIS_MeasuresAcrossAMEDD.pdf. Published April 2010. Accessed November 2014.
14. Schoomaker E. Army medicine: Bringing value and inspiring trust. U.S. Medicine. 2011:10-13.
15. Sia C, Tonniges TF, Osterhus E, Taba S. History of the medical home concept. Pediatrics. 2004;113(5 suppl):1473-1478.
16. Kugler JP. Military Health System Patient Centered Medical Home Guide. Defense Health Agency Website. http://www.tricare.mil/tma/ocmo/download/MHSPCMHGuide.pdf. Published June 2011. Accessed November 11, 2014.
17. Naithani S, Gulliford M. Morgan M. Patients’ perceptions and experiences of ‘continuity of care’ in diabetes. Health Expect. 2006;9(2):118-129.
18. O’Malley AS, Cunningham PJ. Patient experiences with coordination of care: The benefit of continuity and primary care physician as referral source. J Gen Intern Med. 2009;24(2):170-177.
19. American Academy of Family Practice, American Academy of Pediatrics, American College of Physicians, and the American Osteopathic Association. Joint principles of the patient-centered medical home. American Academy of Family Practice Website. http://www.aafp.org/dam/AAFP/documents/practice_management/pcmh/initiatives/PCMHJoint.pdf. Published February 2007. Accessed November 7, 2014.
20. Meyer JA, Silow-Carroll S, Kutyla T, Stepnick LS, Rybowski LS. Hospital Quality: Ingredients for Success--Overview and Lessons Learned. New York, New York: The Commonwealth Fund; 2004.
21. Polit DF, Beck CT. Nursing Research: Generating and Assessing Evidence for Nursing Practice. 8th ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2008.
22. American Association of Clinical Endocrinologists. American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice. American Association of Clinical Endocrinologists Website. https://www.aace.com/files/dm-guidelines-ccp.pdf. Accessed November 7, 2014.
23. Skinner BF. The Behavior of Organisms: An Experimental Analysis. New York, NY: Appleton-Century; 1938.
24. Staddon JE, Cerutti DT. Operant conditioning. Annu Rev Psychol. 2003;54:115-144.
25. Bruner RF. Repetition Is the First Principle of All Learning. Social Science Research network Website. http://papers.ssrn.com/sol3/papers.cfm?abstract_id=224340. Posted August 26, 2001. Accessed November 7, 2014.
26. Institute of Medicine. The Future Of Nursing: Leading Change, Advancing Health. Washington, DC: National Academics Press; 2011.
27. Willens D, Cripps R, Wilson A, Wolff K, Rothman R. Interdisciplinary team care for diabetic patients by primary care physicians, advance practice nurses and clinical pharmacists. Clin Diabetes. 2011;29(2):60-68.
28. Renders CM, Valk GD, Griffin S, Wagner EH, Eijk JT, Assendelft WJ. Interventions to improve the management of diabetes mellitus in primary care, outpatient and community settings. Cochrane Database Syst Rev. 2001;(1):CD001481.
29. Health Affairs. Patient-centered medical homes. Health Affairs Website. http://www.healthaffairs.org. Dated September 14, 2010. Accessed November 7, 2014.
30. Berry LL, Parish JT, Janakiraman R, et al. Patients’ commitment to their primary physician and why it matters. Ann Fam Med. 2008;6(1):6-13.
31. Glasgow RE, Wagner EH, Kaplan RM, Vinicor F, Smith L, Norman J. If diabetes is a public health problem, why not treat it as one? A population-based approach to chronic illness. Ann Behav Med. 1999;21(2):159-170.
1. Centers for Disease Control and Prevention (CDC). National Diabetes Fact Sheet, 2014. CDC Website. http://www.cdc.gov/diabetes/data/statistics/2014StatisticsReport.html. Updated October 24, 2014. Accessed November 6, 2014.
2. American Diabetes Association. National Diabetes Fact Sheet. Statistics about diabetes. American Diabetes Association Website. http://www.diabetes.org/diabetes-basics/diabetes-statistics. Released June 10, 2014. Accessed November 6, 2014.
3. Centers for Disease Control and Prevention (CDC). Number of Americans with diabetes rises to nearly 26 million [press release]. CDC Website. http://www.cdc.gov/media/releases/2011/p0126_diabetes.html. Published January 26, 2011. Accessed November 6, 2014.
4. Huang ES, Basu A, O’Grady M, Capretta JC. Projecting the future diabetes population size and related costs for the U.S. Diabetes Care. 2009;32(12):2225-2229.
5. National Library of Medicine. Diabetes. PubMed Website. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0002194. Reviewed May 24, 2013. Accessed November 6, 2014.
6. Chu-Weininger MY, Balkrishnan R. Consumer satisfaction with primary care provider choice and associated trust. BMC Health Serv Res. 2006;6:139.
7. Alazri MH, Neal RD, Heywood P, Leese B. Patients’ experience of continuity of care of type 2 diabetes: A focus group study in primary care. Br J Gen Prac. 2006;56(528):488-495.
8. Chen CC, Chen SH. Better continuity of care reduces costs for diabetic patients. Am J Manag Care. 2011;17(6):420-427.
9. TRICARE Regional Office-West. Military Treatment Facility (MTF) Profile of William Beaumont Army Medical Center, FY2010 Q2. El Paso, TX. Published March 2010.
10. Worrall G, Knight J. Continuity of care is good for elderly people with diabetes: Retrospective cohort study of mortality and hospitalization. Can Fam Physician. 2011;57(1):e6-e20.
11. Kerr M. ADA 2009: Expert committee recommends use of hemoglobin A1c for diagnosis. Medscape Website. http://www.medscape.com/viewarticle/704021. Published June 7, 2009. Accessed November 7, 2014.
12. Drexler AJ. Lessons learned from landmark trials of type 2 diabetes mellitus and potential applications to clinical practice. Postgrad Med. 2003;Spec No:15-26.
13. Office of Evidence-Based Practice Quality Management Division U.S. Army Medical Command. Population Health: Update of HEDIS measures. U.S. Army Medical Department Office of Quality Management Website. https://www.qmo.amedd.army.mil/HEDIS/HEDIS_MeasuresAcrossAMEDD.pdf. Published April 2010. Accessed November 2014.
14. Schoomaker E. Army medicine: Bringing value and inspiring trust. U.S. Medicine. 2011:10-13.
15. Sia C, Tonniges TF, Osterhus E, Taba S. History of the medical home concept. Pediatrics. 2004;113(5 suppl):1473-1478.
16. Kugler JP. Military Health System Patient Centered Medical Home Guide. Defense Health Agency Website. http://www.tricare.mil/tma/ocmo/download/MHSPCMHGuide.pdf. Published June 2011. Accessed November 11, 2014.
17. Naithani S, Gulliford M. Morgan M. Patients’ perceptions and experiences of ‘continuity of care’ in diabetes. Health Expect. 2006;9(2):118-129.
18. O’Malley AS, Cunningham PJ. Patient experiences with coordination of care: The benefit of continuity and primary care physician as referral source. J Gen Intern Med. 2009;24(2):170-177.
19. American Academy of Family Practice, American Academy of Pediatrics, American College of Physicians, and the American Osteopathic Association. Joint principles of the patient-centered medical home. American Academy of Family Practice Website. http://www.aafp.org/dam/AAFP/documents/practice_management/pcmh/initiatives/PCMHJoint.pdf. Published February 2007. Accessed November 7, 2014.
20. Meyer JA, Silow-Carroll S, Kutyla T, Stepnick LS, Rybowski LS. Hospital Quality: Ingredients for Success--Overview and Lessons Learned. New York, New York: The Commonwealth Fund; 2004.
21. Polit DF, Beck CT. Nursing Research: Generating and Assessing Evidence for Nursing Practice. 8th ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2008.
22. American Association of Clinical Endocrinologists. American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice. American Association of Clinical Endocrinologists Website. https://www.aace.com/files/dm-guidelines-ccp.pdf. Accessed November 7, 2014.
23. Skinner BF. The Behavior of Organisms: An Experimental Analysis. New York, NY: Appleton-Century; 1938.
24. Staddon JE, Cerutti DT. Operant conditioning. Annu Rev Psychol. 2003;54:115-144.
25. Bruner RF. Repetition Is the First Principle of All Learning. Social Science Research network Website. http://papers.ssrn.com/sol3/papers.cfm?abstract_id=224340. Posted August 26, 2001. Accessed November 7, 2014.
26. Institute of Medicine. The Future Of Nursing: Leading Change, Advancing Health. Washington, DC: National Academics Press; 2011.
27. Willens D, Cripps R, Wilson A, Wolff K, Rothman R. Interdisciplinary team care for diabetic patients by primary care physicians, advance practice nurses and clinical pharmacists. Clin Diabetes. 2011;29(2):60-68.
28. Renders CM, Valk GD, Griffin S, Wagner EH, Eijk JT, Assendelft WJ. Interventions to improve the management of diabetes mellitus in primary care, outpatient and community settings. Cochrane Database Syst Rev. 2001;(1):CD001481.
29. Health Affairs. Patient-centered medical homes. Health Affairs Website. http://www.healthaffairs.org. Dated September 14, 2010. Accessed November 7, 2014.
30. Berry LL, Parish JT, Janakiraman R, et al. Patients’ commitment to their primary physician and why it matters. Ann Fam Med. 2008;6(1):6-13.
31. Glasgow RE, Wagner EH, Kaplan RM, Vinicor F, Smith L, Norman J. If diabetes is a public health problem, why not treat it as one? A population-based approach to chronic illness. Ann Behav Med. 1999;21(2):159-170.