User login
CE/CME No: CR-1406
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Describe the clinical manifestations of vestibular migraine (VM).
• List classifications of medications known to induce vestibular symptoms.
• Describe the office-based tests used to evaluate vestibular function.
• List the diagnostic criteria for VM.
• Discuss the differential diagnosis of VM, including peripheral and central causes of vertigo.
• Discuss pharmacologic and nonpharmacologic treatment options for VM.
FACULTY
Jennifer Hart is an Instructor of Nursing at Wor-Wic Community College in Salisbury, Maryland. Mary Parsons is Director of the Graduate and Second Degree Nursing Programs at Salisbury University in Maryland.
The authors have no financial information to disclose.
ACCREDITATION STATEMENT
Article begins on next page >>
Vestibular migraine (VM) is the most common cause of recurrent dizziness and vertigo but is often unrecognized by health care providers. VM causes significant impairment in level of function and quality of life, and the diagnosis should be considered when symptoms cannot be explained by other etiologies. Information and guidance are provided to raise clinicians’ awareness of VM in order to increase accurate diagnosis, guide management decisions, and improve patient health outcomes.
Headache and dizziness are common reasons for primary care visits. In the general population, the prevalence of migraine is 13% to 16%, while dizziness and vertigo affect approximately 20% to 30%.1 Despite the prevalence of these conditions, many providers are unaware of vestibular migraine (VM) and may overlook it when considering differential diagnoses for these symptoms.
This is not surprising since, until recently, the International Headache Society’s (IHS) International Classification of Headache Disorders (ICHD)—considered the “gold standard” for defining and diagnosing headaches across all medical specialties—included no diagnostic criteria for VM.2 The second edition of the ICHD, ICHD-2, identified vertigo as a symptom of migraine only in the context of basilar migraine.1 Since fewer than 10% of patients with both vertigo and migraine met the criteria for basilar migraine, most VM patients could not be correctly classified under ICHD-2.1
In 2012, the Committee for Classification of Vestibular Disorders of the Bárány Society and the Migraine Classification Subcommittee of the IHS jointly published diagnostic criteria for VM.3 These criteria are included in the beta version of ICHD-3, published on the IHS website on July 3, 2013, for immediate use and field testing before ICHD-3 is finalized.4
DIAGNOSTIC CRITERIA FOR VM
The criteria for diagnosis of VM are as follows4:
A. At least five episodes fulfilling criteria C and D
B. A current or past history of migraine without aura or migraine with aura
C. Vestibular symptoms of moderate or severe intensity, lasting between 5 min and 72 h
D. At least 50% of episodes are associated with at least one of the following migrainous features:
- Headache with at least two of the following four characteristics:
a. Unilateral location
b. Pulsating quality
c. Moderate or severe intensity
d. Aggravation by routine physical activity - Photophobia and phonophobia
- Visual aura
E. Not better accounted for by another ICHD-3 diagnosis or by another vestibular disorder
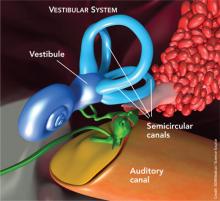
Vestibular symptoms include3
• Spontaneous vertigo, which can be internal (false sensation of self-motion) or external (false sensation that surroundings are spinning)
• Positional vertigo (after change in head position)
• Visually induced vertigo (triggered by a complex or large moving visual stimulus)
• Head motion–induced vertigo
• Head motion–induced dizziness with nausea (dizziness is a sensation of disturbed spatial orientation)
Moderate vestibular symptoms interfere with, but do not prevent, daily activities; severe vestibular symptoms impede them.
On the next page: Diagnosis Overview >>
DIAGNOSIS: OVERVIEW
VM is a diagnosis of exclusion that is considered appropriate when no other peripheral or central vestibular disorder is present to account for the patient’s dizziness.5,6 Asking the patient the right questions will provide clues to the correct diagnosis.7 Most patients with VM present with normal physical, vestibular, and neurologic examinations, especially if examined when symptom-free.5 In contrast, examinations for competing diagnoses often reveal abnormal findings.
Vestibular vs nonvestibular vertigo. Typically, patients have difficulty describing their sensations with words more specific than “dizzy.”8 This lack of clarity is a challenge when the clinician is attempting to differentiate between true vertigo (ie, vertigo caused by vestibular dysfunction) and other types of nonvestibular dizziness. Specific categories of dizziness include vertigo, imbalance, presyncope, and lightheadedness; careful consideration must be given to the causes associated with each (see Table 1).9-11
Clinicians should focus on timing, duration of symptoms, triggers, and any other associated symptoms to determine the diagnosis.8,10 When evaluating a patient, a broad definition of vertigo, including spinning and/or rotational sensations as well as illusions of movement, is recommended.8
Peripheral vs central disorders. True vertigo must be further evaluated to determine whether its etiology is peripheral or central. In VM, a combination of both peripheral and central deficits can be seen.10 Clinicians must consider certain defining features to differentiate between these.
Peripheral Vertigo
If the cause of the patient's vertigo is peripheral, onset is often abrupt and the patient may experience mild-to-moderate imbalance that does not affect his or her ability to walk unassisted. Combined horizontal and rotational nystagmus may occur, which lessens or disappears with focused gaze. The nystagmus does not change direction when the patient gazes to either side and may fade after a few days.
The patient also may report experiencing tinnitus or hearing loss, accompanied by severe nausea or vomiting. Neurologic symptoms are rare in peripherally caused vertigo unless a concurrent diagnosis of migraine is confirmed.
Other symptoms may include weakness, dysarthria, changes in vision or hearing, paresthesias, changes in sensory or motor function, altered level of consciousness, and headache.10
Central Vertigo
Centrally caused vertigo often persists for hours to weeks, and neurologic symptoms are common. Patients have difficulty walking or standing still; problems with balance are severe. The nystagmus is purely horizontal, vertical, or rotational and may last for weeks to months. It is not inhibited with a focused gaze and may change direction with gaze. It is important to note that vertical nystagmus is 80% sensitive for vestibular nuclear or cerebellar central lesions.10
Tinnitus, if it occurs at all, is episodic, and nausea and/or vomiting vary from patient to patient. Patients presenting with central nervous system (CNS) disorders rarely complain of vertigo as their only symptom. Additional descriptions of dizziness may be used to describe the various cranial nerve abnormalities that suggest CNS etiology.9
DIFFERENTIAL DIAGNOSIS
Numerous conditions should be included in the differential when evaluating dizziness and vertigo symptoms. (See also Collie M. Vertigo: diagnosis and management. Clinician Reviews. 2013;23[12]:46-53.)
Peripheral Vertigo
Possible peripheral causes of vertigo include5,6,12,13
• Benign paroxysmal positional vertigo (BPPV)
• Vestibular neuritis
• Labyrinthitis
• Ménière disease
• Superior canal dehiscence
• Perilymphatic fistula
• Otitis media
• Aminoglycoside toxicity
• Trauma
BPPV is characterized by recurrent episodes of intense vertigo that last for seconds to one minute and are provoked by specific head movements. The Dix-Hallpike maneuver provokes vertigo and nystagmus and confirms the diagnosis.14 Vestibular neuritis and labyrinthitis present in similar ways. They are characterized by the onset of intense vertigo that can persist for several days, with nausea, vomiting, and imbalance also present. The main differentiating feature between them is associated hearing loss; vestibular neuritis is not associated with hearing loss, but labyrinthitis is. Both disorders are thought to be caused by inflammation of the vestibular nerve as the result of a viral infection. Patients may report recent upper respiratory infections or influenza like illnesses.10,12
Central Vertigo
Possible central causes of vertigo include5,6,13,15
• Acoustic neuroma (vestibular schwannoma)
• Cerebellar infarction
• Brainstem stroke
• Multiple sclerosis
• Episodic ataxia
• Psychogenic dizziness
Acoustic neuroma (vestibular schwannoma) is a benign growth on the vestibular nerve. Symptoms generally include progressive hearing loss and unilateral tinnitus accompanied by dizziness and imbalance.10 Acute attacks of vertigo are rare, but patients often complain of aural fullness, headache, and/or facial numbness.1,10
Cerebellar infarction usually presents with sudden onset of symptoms at maximal intensity. Risk factors for cerebellar infarction include a history of hypertension, coronary artery disease, diabetes, previous transient ischemic attack, smoking, alcohol consumption, atrial fibrillation, and hyperlipidemia.10
While only 5% of vertigo complaints are the result of CNS disorders, vertigo is an early symptom of brainstem stroke.15 Because of the significant morbidity and mortality associated with stroke, it must be considered in the initial diagnostic workup of vertigo.
Multiple sclerosis (MS) is an autoimmune disease in which the myelin axons in the CNS are destroyed. Dizziness and vertigo are common complaints associated with MS, but these patients will often present with other symptoms suggestive of CNS involvement. Common complaints include, but are not limited to, muscle weakness, fatigue, paresthesias, spasms, ataxia, pain, diplopia, dysarthria, heat intolerance, and urinary frequency.16
Episodic ataxia type 2 (EA2) is an inherited autosomal dominant disorder characterized by attacks of ataxia, vertigo, and nausea that can last from minutes to days. EA2 is often difficult to differentiate from VM due to symptom overlap. Fifty percent of patients with EA2 have a history of migraine headaches; often, there is a family history of similar symptoms.5
On the next page: Ménière Disease Versus VM >>
MÉNIÈRE DISEASE VERSUS VM
When headaches and dizziness coincide, VM is the most probable diagnosis.5 BPPV, Ménière disease, cerebellar disorders, motion sickness, and psychiatric syndromes (major depression and panic disorder) occur more often in patients with migraine than in those without.1 Ménière disease and VM often coexist, and up to 50% of patients with Ménière disease also meet criteria for migraine.5 (For more information, see Pearson T. Ménière disease: a lifelong merry-go-round. Clinician Reviews. 2013;23[10]:38-43.) Because many of their symptoms overlap, differentiating between Ménière disease and VM is critical; key differences in symptom presentation are as follows.17,18
Vertigo. The vertigo of Ménière disease is short-lived, lasting up to 24 hours.17 In contrast, episodes of vertigo with VM can last more than 24 hours; patients may experience a continuous rocking sensation for several weeks or even months.
Hearing loss. Sensorineural hearing loss in patients with Ménière disease is progressive and most often unilateral, but can be bilateral. In patients with VM, sensorineural hearing loss is rare; if it occurs, it is usually episodic and not progressive.17
Tinnitus. Tinnitus is a symptom of both Ménière disease and VM and may be unilateral or bilateral in both. In Ménière disease, patients report tinnitus of significant intensity, low in pitch, and “roaring,” whereas in VM, the tinnitus is usually high-pitched and unobtrusive.
Headache. Unless a concurrent diagnosis of migraine exists, patients with Ménière disease do not present with headache or photophobia. Many patients with VM, though not all, confirm a positive history of headache.
Phonophobia. Phonophobia is a frequent symptom in patients with VM.17
On the next page: Clinical Manifestations >>
CLINICAL MANIFESTATIONS OF VM
The clinical presentation of VM varies for each patient, as do the frequency and duration of episodes. Manifestations of VM may include5,19,20
• Vertigo associated with visual triggers
• Nausea and/or dizziness
• Spontaneous positional vertigo
• Head motion intolerance
• Motion sickness
• Lightheadedness
• Headache
• Chronic disequilibrium
• Inability to concentrate
• Mild hearing loss or tinnitus
• Cervicalgia
• Anxiety
• Panic
• Photophobia
• Phonophobia
• Sensory aura
Visual vertigo, described as vertigo worsened by visual stimulation such as moving scenes, scrolling patterns, and movement of large crowds or traffic, is highly suggestive of VM.19 Aura-type symptoms are of significant diagnostic importance because they may be the only apparent connection between vertigo and migraine.19
The duration of vertigo and dizziness may range from seconds to weeks. These episodes may have no temporal relationship with headaches. Vertigo and dizziness can continue for more than 24 hours for about half of VM patients; in some, symptoms persist for several weeks or more.12 In addition, vertigo and headache may never occur together, which further increases the diagnostic challenge for this disorder.1,5
Although many hypotheses exist, the pathophysiology of VM remains unclear.
Patient History
It is vital to obtain a detailed medical and social history in order to determine possible etiologies for symptoms. Medications in particular must be reviewed with care because many are known to induce vestibular-type symptoms.
Cardiac agents of potential concern for causing dizziness include β-blockers, diuretics, ACE inhibitors, β-blockers, and nitrates. CNS agents associated with dizziness include antipsychotics, dopaminergic drugs, opioids/analgesics, hypnotics, anticonvulsants, tricyclic antidepressants, and muscle relaxants. Anticholinergics, phosphodiesterase type 5 inhibitors, antibacterials, aminoglycosides, fluoroquinolones, and antineoplastics may also lead to dizziness; several of these medications are also known to be ototoxic. Dizziness can also be related to orthostatic hypotension, which is a common adverse effect of many of the listed medications, especially when used in combination.7,9
Diabetes, hypertension, vascular diseases, and neurologic disorders should be considered as causes for vision and proprioception problems.7 Patients may present with a personal history of headaches for years before vestibular symptoms develop.6 Motion sickness is suggestive of a possible migraine diagnosis.19
Positive family history is common for migraineurs.21 Patients ages 30 to 39 are affected most frequently, with an estimated prevalence of 7% in men and 24.4% in women.22
Physical Examination
The focused physical should include cranial nerve assessments, an otoscopic examination, hearing evaluation with a tuning fork, and audiometry, if a hearing deficit is detected. Minor oculomotor abnormalities, such as “weak” nystagmus with vertical, horizontal, torsional, or positional components, may be noted in approximately 70% of patients with VM.5 Various in-office tests (see Table 2) should also be conducted to narrow the possible causes for vertigo and dizziness and rule out more serious disorders.7,10 ,11,23
Diagnostic Workup
Laboratory tests are generally not recommended because they identify the cause of vertigo in only approximately 1% of patients.23 Similarly, routine use of MRI or CT is not recommended, but these modalities may be indicated for patients with focal neurologic deficits or risk factors for cerebrovascular disease, or if acute treatments for peripheral vertigo are unsuccessful.10
On the next page: Treatment >>
TREATMENT OF VM
Nonpharmacologic
Nonpharmacologic measures to prevent VM attacks include the avoidance of “triggers” through dietary restrictions, stress reduction, and healthy lifestyle modifications. Diaries can be used to help identify common triggers to avoid (see Table 3); patients should understand that it may take up to three months before noticeable improvement in symptoms is seen. Once symptoms have resolved, cautious re-introduction of suspect foods may be attempted.24
Vestibular rehabilitation therapy promotes CNS compensation for inner ear deficits and reduces symptoms of disequilibrium and dizziness.25 It is helpful for complications of VM, such as anxiety, visual dependence, or loss of confidence with balance.10
Pharmacologic
Prophylactic drug therapy is the mainstay of medical management for VM when nonpharmacologic measures are inadequate; episodes are frequent and severe; or symptoms are of long duration.5 The drugs’ adverse effect profiles, as well as patient comorbidities, should guide the choice of therapy.26
Abortive migraine therapies have not been shown to be effective for symptoms of dizziness17 and may cause rebound symptoms. Vestibular suppressants (promethazine, dimenhydrinate, and meclizine) can be used for acute episodes of VM.5
According to evidence-based guidelines for the preventive treatment of migraine in adults,26 the pharmacologic options include multiple drug classes stratified by level, depending on the quality of evidence supporting their effectiveness in migraine prevention.
Level A comprises medications with established efficacy. These include divalproex sodium, sodium valproate, topiramate, frovatriptan (for menstrual migraine), metoprolol, propanolol, and timolol.
Level B medications that are “probably effective” include naratriptan, zolmitriptan, amitriptyline, venlafaxine, atenolol, and nadolol.
Medications that are “possibly effective” are in the Level C category and include carbamazepine, nebivolol, pindolol, lisinopril, candesartan, clonidine, guanfacine, and cyproheptadine.
The Level U category drugs are labeled “inadequate or conflicting data to support or refute medication use” and include fluvoxamine, fluoxetine, protriptyline, gabapentin, bisoprolol, cyclandelate, acenocoumarol, warfarin, picotamide, acetazolamide, nicardipine, nifedipine, nimodipine, and verapamil.
Medications that are established as possibly or probably ineffective fall under the category of Other and include clomipramine, lamotrigine, acebutolol, clonazepam, nabumetone, oxcarbazepine, and telmisartan.
When initiating therapy, low doses are recommended because migraineurs’ sensory hypersensitivity is thought to extend to medications.5 Sequence and dosing information, along with contraindications, should be considered when choosing medical therapies (see Table 4).5,12,19,21,26 Patient response to treatment is evaluated after one to three months, and medications should be discontinued if symptoms persist, maximum dose is reached, or significant adverse effects occur.5 A reasonable goal of therapy is to reduce episode frequency by more than 50%.19 Should both lifestyle modifications and medications fail, referral to a specialist for reevaluation of the diagnosis is warranted.8
On the next page: Conclusion >>
CONCLUSION
While VM is considered the most common cause of recurrent vertigo and dizziness, few primary care providers are familiar with the diagnosis. Differentiating among the various causes for these symptoms and determining if the cause is a CNS or peripheral system disorder are essential to narrowing the differential diagnoses.
The inclusion of VM in the ICHD-3 system will increase both clinician awareness and accurate diagnosis of the disorder. Office-based assessments can be performed to evaluate these common complaints, and numerous medical therapies are available to successfully treat patients with VM. Through greater awareness of VM and use of evidence-based diagnostic and treatment guidelines, clinicians can significantly improve quality of life and health outcomes for patients with the disorder.
1. Lempert T, Neuhauser H. Epidemiology of vertigo, migraine and vestibular migraine. J Neurol. 2009;256(3):333-338.
2. The International Headache Society. The International Headache Classification. 2nd ed. www.ihs-classification.org/en/01_einleitung/02_einleitung/. Accessed May 16, 2014.
3. Lempert T, Oleson J, Furman J, et al. Vestibular migraine: diagnostic criteria. J Vestib Res. 2012;22:167-172.
4. Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders. 3rd ed (beta version). Cephalalgia. 2013;33(9):629-808.
5. Cherchi M, Hain T. Migraine-associated vertigo. Otolaryngol Clin Am. 2011;44:367-375.
6. Honaker J, Samy R. Migraine-associated vestibulopathy. Curr Opin Otolaryngol Head Neck Surg. 2008;16:412-415.
7. Shaia WT. Dizziness evaluation. http://emedicine.medscape.com/article/1831429-overview. Accessed May 16, 2014.
8. Watson S. Vertigo and migraine: "how can it be a migraine if I don’t have a headache?" Med Today. 2011;12(12):36-43.
9. Post RE, Dickerson LM. Dizziness: a diagnostic approach. Am Fam Physician. 2010;82(4):361-368.
10. Furman M, Rizzolo D. Evaluating the patient with vertigo: a complex complaint made simple. JAAPA. 2011;24(10):52-58.
11. Kuo CH, Pang T, Chang R. Vertigo – part 1 - assessment in general practice. Aust Fam Physician. 2008;37(5):341-347.
12. Hain, T. Migraine associated vertigo: vestibular migraine. www.dizziness-and-balance.com/disorders/central/migraine/mav.html. Accessed May 16, 2014.
13. Cha YH, Kane MJ, Baloh RW. Familial clustering of migraine, episodic vertigo, and Ménière’s disease. Otol Neurotol. 2008;29(1):93-96.
14. Clark MM. How to sort out a complaint of dizziness. Patient Care. 2003;37: 44-52.
15. Hain TC. Brainstem strokes associated with vertigo or hearing symptoms. www.dizziness-and- balance.com/disorders/central/strokes/brainstem%20strokes.htm. Accessed May 16, 2014.
16. Luzzio C, Dangond F. Multiple sclerosis. http://emedicine.medscape.com/article/1146199-overview. Accessed May 16, 2014.
17. Benson AG. Migraine-associated vertigo. http://emedicine.medscape.com/article/884136-overview#aw2aab6b5. Accessed May 16, 2014.
18. Teggi R, Fabiano B, Recanata P, et al. Case reports on two patients with episodic vertigo, fluctuating hearing loss, and migraine responding to prophylactic drugs for migraine. Ménière disease or migraine-associated vertigo? Acta Otorhinolaryngol Ital. 2010;30(4):217-220.
19. Neuhauser H, Lempert T. Vestibular migraine. Neurol Clin. 2009;27:379-391.
20. Kramer J, Buskirk J. Vestibular migraine a/k/a migraine-associated vertigo. www.vestibular.org/migraine-associated-vertigo-mav. Accessed April 1, 2014.
21. Chawla J. Migraine headache. http://emedicine.medscape.com/article/1142556-overview. Accessed May 16, 2014.
22. Cutrer MF, Bajwa ZH, Sabahat A. Pathophysiology, clinical manifestations, and diagnosis of migraine in adults. www.uptodate.com/contents/patho physiology-clinical-manifestations-and-diagnosis-of-migraine-in-adults. Accessed May 16, 2014.
23. Labuguen R. Initial evaluation of vertigo [published correction appears in Am Fam Physician. 2006;73(10):1704]. Am Fam Physician. 2006;73(2):244-251.
24. Texiedo M. Common migraine food triggers. http://deedee.dbi.udel.edu/MichaelTeixidoMD/patientInfo/migrainesFoodTrig.html. Accessed May 16, 2014.
25. Bisdorff AR. Management of vestibular migraine. Ther Adv Neurol Disord. 2011;4(3):183-191.
26. Silberstein S, Holland S, Freitag F, et al; Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults [published correction appears in Neurology. 2013;80:871]. Neurology. 2012;78(17):1337-1345.
CE/CME No: CR-1406
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Describe the clinical manifestations of vestibular migraine (VM).
• List classifications of medications known to induce vestibular symptoms.
• Describe the office-based tests used to evaluate vestibular function.
• List the diagnostic criteria for VM.
• Discuss the differential diagnosis of VM, including peripheral and central causes of vertigo.
• Discuss pharmacologic and nonpharmacologic treatment options for VM.
FACULTY
Jennifer Hart is an Instructor of Nursing at Wor-Wic Community College in Salisbury, Maryland. Mary Parsons is Director of the Graduate and Second Degree Nursing Programs at Salisbury University in Maryland.
The authors have no financial information to disclose.
ACCREDITATION STATEMENT
Article begins on next page >>
Vestibular migraine (VM) is the most common cause of recurrent dizziness and vertigo but is often unrecognized by health care providers. VM causes significant impairment in level of function and quality of life, and the diagnosis should be considered when symptoms cannot be explained by other etiologies. Information and guidance are provided to raise clinicians’ awareness of VM in order to increase accurate diagnosis, guide management decisions, and improve patient health outcomes.
Headache and dizziness are common reasons for primary care visits. In the general population, the prevalence of migraine is 13% to 16%, while dizziness and vertigo affect approximately 20% to 30%.1 Despite the prevalence of these conditions, many providers are unaware of vestibular migraine (VM) and may overlook it when considering differential diagnoses for these symptoms.
This is not surprising since, until recently, the International Headache Society’s (IHS) International Classification of Headache Disorders (ICHD)—considered the “gold standard” for defining and diagnosing headaches across all medical specialties—included no diagnostic criteria for VM.2 The second edition of the ICHD, ICHD-2, identified vertigo as a symptom of migraine only in the context of basilar migraine.1 Since fewer than 10% of patients with both vertigo and migraine met the criteria for basilar migraine, most VM patients could not be correctly classified under ICHD-2.1
In 2012, the Committee for Classification of Vestibular Disorders of the Bárány Society and the Migraine Classification Subcommittee of the IHS jointly published diagnostic criteria for VM.3 These criteria are included in the beta version of ICHD-3, published on the IHS website on July 3, 2013, for immediate use and field testing before ICHD-3 is finalized.4
DIAGNOSTIC CRITERIA FOR VM
The criteria for diagnosis of VM are as follows4:
A. At least five episodes fulfilling criteria C and D
B. A current or past history of migraine without aura or migraine with aura
C. Vestibular symptoms of moderate or severe intensity, lasting between 5 min and 72 h
D. At least 50% of episodes are associated with at least one of the following migrainous features:
- Headache with at least two of the following four characteristics:
a. Unilateral location
b. Pulsating quality
c. Moderate or severe intensity
d. Aggravation by routine physical activity - Photophobia and phonophobia
- Visual aura
E. Not better accounted for by another ICHD-3 diagnosis or by another vestibular disorder
Vestibular symptoms include3
• Spontaneous vertigo, which can be internal (false sensation of self-motion) or external (false sensation that surroundings are spinning)
• Positional vertigo (after change in head position)
• Visually induced vertigo (triggered by a complex or large moving visual stimulus)
• Head motion–induced vertigo
• Head motion–induced dizziness with nausea (dizziness is a sensation of disturbed spatial orientation)
Moderate vestibular symptoms interfere with, but do not prevent, daily activities; severe vestibular symptoms impede them.
On the next page: Diagnosis Overview >>
DIAGNOSIS: OVERVIEW
VM is a diagnosis of exclusion that is considered appropriate when no other peripheral or central vestibular disorder is present to account for the patient’s dizziness.5,6 Asking the patient the right questions will provide clues to the correct diagnosis.7 Most patients with VM present with normal physical, vestibular, and neurologic examinations, especially if examined when symptom-free.5 In contrast, examinations for competing diagnoses often reveal abnormal findings.
Vestibular vs nonvestibular vertigo. Typically, patients have difficulty describing their sensations with words more specific than “dizzy.”8 This lack of clarity is a challenge when the clinician is attempting to differentiate between true vertigo (ie, vertigo caused by vestibular dysfunction) and other types of nonvestibular dizziness. Specific categories of dizziness include vertigo, imbalance, presyncope, and lightheadedness; careful consideration must be given to the causes associated with each (see Table 1).9-11
Clinicians should focus on timing, duration of symptoms, triggers, and any other associated symptoms to determine the diagnosis.8,10 When evaluating a patient, a broad definition of vertigo, including spinning and/or rotational sensations as well as illusions of movement, is recommended.8
Peripheral vs central disorders. True vertigo must be further evaluated to determine whether its etiology is peripheral or central. In VM, a combination of both peripheral and central deficits can be seen.10 Clinicians must consider certain defining features to differentiate between these.
Peripheral Vertigo
If the cause of the patient's vertigo is peripheral, onset is often abrupt and the patient may experience mild-to-moderate imbalance that does not affect his or her ability to walk unassisted. Combined horizontal and rotational nystagmus may occur, which lessens or disappears with focused gaze. The nystagmus does not change direction when the patient gazes to either side and may fade after a few days.
The patient also may report experiencing tinnitus or hearing loss, accompanied by severe nausea or vomiting. Neurologic symptoms are rare in peripherally caused vertigo unless a concurrent diagnosis of migraine is confirmed.
Other symptoms may include weakness, dysarthria, changes in vision or hearing, paresthesias, changes in sensory or motor function, altered level of consciousness, and headache.10
Central Vertigo
Centrally caused vertigo often persists for hours to weeks, and neurologic symptoms are common. Patients have difficulty walking or standing still; problems with balance are severe. The nystagmus is purely horizontal, vertical, or rotational and may last for weeks to months. It is not inhibited with a focused gaze and may change direction with gaze. It is important to note that vertical nystagmus is 80% sensitive for vestibular nuclear or cerebellar central lesions.10
Tinnitus, if it occurs at all, is episodic, and nausea and/or vomiting vary from patient to patient. Patients presenting with central nervous system (CNS) disorders rarely complain of vertigo as their only symptom. Additional descriptions of dizziness may be used to describe the various cranial nerve abnormalities that suggest CNS etiology.9
DIFFERENTIAL DIAGNOSIS
Numerous conditions should be included in the differential when evaluating dizziness and vertigo symptoms. (See also Collie M. Vertigo: diagnosis and management. Clinician Reviews. 2013;23[12]:46-53.)
Peripheral Vertigo
Possible peripheral causes of vertigo include5,6,12,13
• Benign paroxysmal positional vertigo (BPPV)
• Vestibular neuritis
• Labyrinthitis
• Ménière disease
• Superior canal dehiscence
• Perilymphatic fistula
• Otitis media
• Aminoglycoside toxicity
• Trauma
BPPV is characterized by recurrent episodes of intense vertigo that last for seconds to one minute and are provoked by specific head movements. The Dix-Hallpike maneuver provokes vertigo and nystagmus and confirms the diagnosis.14 Vestibular neuritis and labyrinthitis present in similar ways. They are characterized by the onset of intense vertigo that can persist for several days, with nausea, vomiting, and imbalance also present. The main differentiating feature between them is associated hearing loss; vestibular neuritis is not associated with hearing loss, but labyrinthitis is. Both disorders are thought to be caused by inflammation of the vestibular nerve as the result of a viral infection. Patients may report recent upper respiratory infections or influenza like illnesses.10,12
Central Vertigo
Possible central causes of vertigo include5,6,13,15
• Acoustic neuroma (vestibular schwannoma)
• Cerebellar infarction
• Brainstem stroke
• Multiple sclerosis
• Episodic ataxia
• Psychogenic dizziness
Acoustic neuroma (vestibular schwannoma) is a benign growth on the vestibular nerve. Symptoms generally include progressive hearing loss and unilateral tinnitus accompanied by dizziness and imbalance.10 Acute attacks of vertigo are rare, but patients often complain of aural fullness, headache, and/or facial numbness.1,10
Cerebellar infarction usually presents with sudden onset of symptoms at maximal intensity. Risk factors for cerebellar infarction include a history of hypertension, coronary artery disease, diabetes, previous transient ischemic attack, smoking, alcohol consumption, atrial fibrillation, and hyperlipidemia.10
While only 5% of vertigo complaints are the result of CNS disorders, vertigo is an early symptom of brainstem stroke.15 Because of the significant morbidity and mortality associated with stroke, it must be considered in the initial diagnostic workup of vertigo.
Multiple sclerosis (MS) is an autoimmune disease in which the myelin axons in the CNS are destroyed. Dizziness and vertigo are common complaints associated with MS, but these patients will often present with other symptoms suggestive of CNS involvement. Common complaints include, but are not limited to, muscle weakness, fatigue, paresthesias, spasms, ataxia, pain, diplopia, dysarthria, heat intolerance, and urinary frequency.16
Episodic ataxia type 2 (EA2) is an inherited autosomal dominant disorder characterized by attacks of ataxia, vertigo, and nausea that can last from minutes to days. EA2 is often difficult to differentiate from VM due to symptom overlap. Fifty percent of patients with EA2 have a history of migraine headaches; often, there is a family history of similar symptoms.5
On the next page: Ménière Disease Versus VM >>
MÉNIÈRE DISEASE VERSUS VM
When headaches and dizziness coincide, VM is the most probable diagnosis.5 BPPV, Ménière disease, cerebellar disorders, motion sickness, and psychiatric syndromes (major depression and panic disorder) occur more often in patients with migraine than in those without.1 Ménière disease and VM often coexist, and up to 50% of patients with Ménière disease also meet criteria for migraine.5 (For more information, see Pearson T. Ménière disease: a lifelong merry-go-round. Clinician Reviews. 2013;23[10]:38-43.) Because many of their symptoms overlap, differentiating between Ménière disease and VM is critical; key differences in symptom presentation are as follows.17,18
Vertigo. The vertigo of Ménière disease is short-lived, lasting up to 24 hours.17 In contrast, episodes of vertigo with VM can last more than 24 hours; patients may experience a continuous rocking sensation for several weeks or even months.
Hearing loss. Sensorineural hearing loss in patients with Ménière disease is progressive and most often unilateral, but can be bilateral. In patients with VM, sensorineural hearing loss is rare; if it occurs, it is usually episodic and not progressive.17
Tinnitus. Tinnitus is a symptom of both Ménière disease and VM and may be unilateral or bilateral in both. In Ménière disease, patients report tinnitus of significant intensity, low in pitch, and “roaring,” whereas in VM, the tinnitus is usually high-pitched and unobtrusive.
Headache. Unless a concurrent diagnosis of migraine exists, patients with Ménière disease do not present with headache or photophobia. Many patients with VM, though not all, confirm a positive history of headache.
Phonophobia. Phonophobia is a frequent symptom in patients with VM.17
On the next page: Clinical Manifestations >>
CLINICAL MANIFESTATIONS OF VM
The clinical presentation of VM varies for each patient, as do the frequency and duration of episodes. Manifestations of VM may include5,19,20
• Vertigo associated with visual triggers
• Nausea and/or dizziness
• Spontaneous positional vertigo
• Head motion intolerance
• Motion sickness
• Lightheadedness
• Headache
• Chronic disequilibrium
• Inability to concentrate
• Mild hearing loss or tinnitus
• Cervicalgia
• Anxiety
• Panic
• Photophobia
• Phonophobia
• Sensory aura
Visual vertigo, described as vertigo worsened by visual stimulation such as moving scenes, scrolling patterns, and movement of large crowds or traffic, is highly suggestive of VM.19 Aura-type symptoms are of significant diagnostic importance because they may be the only apparent connection between vertigo and migraine.19
The duration of vertigo and dizziness may range from seconds to weeks. These episodes may have no temporal relationship with headaches. Vertigo and dizziness can continue for more than 24 hours for about half of VM patients; in some, symptoms persist for several weeks or more.12 In addition, vertigo and headache may never occur together, which further increases the diagnostic challenge for this disorder.1,5
Although many hypotheses exist, the pathophysiology of VM remains unclear.
Patient History
It is vital to obtain a detailed medical and social history in order to determine possible etiologies for symptoms. Medications in particular must be reviewed with care because many are known to induce vestibular-type symptoms.
Cardiac agents of potential concern for causing dizziness include β-blockers, diuretics, ACE inhibitors, β-blockers, and nitrates. CNS agents associated with dizziness include antipsychotics, dopaminergic drugs, opioids/analgesics, hypnotics, anticonvulsants, tricyclic antidepressants, and muscle relaxants. Anticholinergics, phosphodiesterase type 5 inhibitors, antibacterials, aminoglycosides, fluoroquinolones, and antineoplastics may also lead to dizziness; several of these medications are also known to be ototoxic. Dizziness can also be related to orthostatic hypotension, which is a common adverse effect of many of the listed medications, especially when used in combination.7,9
Diabetes, hypertension, vascular diseases, and neurologic disorders should be considered as causes for vision and proprioception problems.7 Patients may present with a personal history of headaches for years before vestibular symptoms develop.6 Motion sickness is suggestive of a possible migraine diagnosis.19
Positive family history is common for migraineurs.21 Patients ages 30 to 39 are affected most frequently, with an estimated prevalence of 7% in men and 24.4% in women.22
Physical Examination
The focused physical should include cranial nerve assessments, an otoscopic examination, hearing evaluation with a tuning fork, and audiometry, if a hearing deficit is detected. Minor oculomotor abnormalities, such as “weak” nystagmus with vertical, horizontal, torsional, or positional components, may be noted in approximately 70% of patients with VM.5 Various in-office tests (see Table 2) should also be conducted to narrow the possible causes for vertigo and dizziness and rule out more serious disorders.7,10 ,11,23
Diagnostic Workup
Laboratory tests are generally not recommended because they identify the cause of vertigo in only approximately 1% of patients.23 Similarly, routine use of MRI or CT is not recommended, but these modalities may be indicated for patients with focal neurologic deficits or risk factors for cerebrovascular disease, or if acute treatments for peripheral vertigo are unsuccessful.10
On the next page: Treatment >>
TREATMENT OF VM
Nonpharmacologic
Nonpharmacologic measures to prevent VM attacks include the avoidance of “triggers” through dietary restrictions, stress reduction, and healthy lifestyle modifications. Diaries can be used to help identify common triggers to avoid (see Table 3); patients should understand that it may take up to three months before noticeable improvement in symptoms is seen. Once symptoms have resolved, cautious re-introduction of suspect foods may be attempted.24
Vestibular rehabilitation therapy promotes CNS compensation for inner ear deficits and reduces symptoms of disequilibrium and dizziness.25 It is helpful for complications of VM, such as anxiety, visual dependence, or loss of confidence with balance.10
Pharmacologic
Prophylactic drug therapy is the mainstay of medical management for VM when nonpharmacologic measures are inadequate; episodes are frequent and severe; or symptoms are of long duration.5 The drugs’ adverse effect profiles, as well as patient comorbidities, should guide the choice of therapy.26
Abortive migraine therapies have not been shown to be effective for symptoms of dizziness17 and may cause rebound symptoms. Vestibular suppressants (promethazine, dimenhydrinate, and meclizine) can be used for acute episodes of VM.5
According to evidence-based guidelines for the preventive treatment of migraine in adults,26 the pharmacologic options include multiple drug classes stratified by level, depending on the quality of evidence supporting their effectiveness in migraine prevention.
Level A comprises medications with established efficacy. These include divalproex sodium, sodium valproate, topiramate, frovatriptan (for menstrual migraine), metoprolol, propanolol, and timolol.
Level B medications that are “probably effective” include naratriptan, zolmitriptan, amitriptyline, venlafaxine, atenolol, and nadolol.
Medications that are “possibly effective” are in the Level C category and include carbamazepine, nebivolol, pindolol, lisinopril, candesartan, clonidine, guanfacine, and cyproheptadine.
The Level U category drugs are labeled “inadequate or conflicting data to support or refute medication use” and include fluvoxamine, fluoxetine, protriptyline, gabapentin, bisoprolol, cyclandelate, acenocoumarol, warfarin, picotamide, acetazolamide, nicardipine, nifedipine, nimodipine, and verapamil.
Medications that are established as possibly or probably ineffective fall under the category of Other and include clomipramine, lamotrigine, acebutolol, clonazepam, nabumetone, oxcarbazepine, and telmisartan.
When initiating therapy, low doses are recommended because migraineurs’ sensory hypersensitivity is thought to extend to medications.5 Sequence and dosing information, along with contraindications, should be considered when choosing medical therapies (see Table 4).5,12,19,21,26 Patient response to treatment is evaluated after one to three months, and medications should be discontinued if symptoms persist, maximum dose is reached, or significant adverse effects occur.5 A reasonable goal of therapy is to reduce episode frequency by more than 50%.19 Should both lifestyle modifications and medications fail, referral to a specialist for reevaluation of the diagnosis is warranted.8
On the next page: Conclusion >>
CONCLUSION
While VM is considered the most common cause of recurrent vertigo and dizziness, few primary care providers are familiar with the diagnosis. Differentiating among the various causes for these symptoms and determining if the cause is a CNS or peripheral system disorder are essential to narrowing the differential diagnoses.
The inclusion of VM in the ICHD-3 system will increase both clinician awareness and accurate diagnosis of the disorder. Office-based assessments can be performed to evaluate these common complaints, and numerous medical therapies are available to successfully treat patients with VM. Through greater awareness of VM and use of evidence-based diagnostic and treatment guidelines, clinicians can significantly improve quality of life and health outcomes for patients with the disorder.
CE/CME No: CR-1406
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Describe the clinical manifestations of vestibular migraine (VM).
• List classifications of medications known to induce vestibular symptoms.
• Describe the office-based tests used to evaluate vestibular function.
• List the diagnostic criteria for VM.
• Discuss the differential diagnosis of VM, including peripheral and central causes of vertigo.
• Discuss pharmacologic and nonpharmacologic treatment options for VM.
FACULTY
Jennifer Hart is an Instructor of Nursing at Wor-Wic Community College in Salisbury, Maryland. Mary Parsons is Director of the Graduate and Second Degree Nursing Programs at Salisbury University in Maryland.
The authors have no financial information to disclose.
ACCREDITATION STATEMENT
Article begins on next page >>
Vestibular migraine (VM) is the most common cause of recurrent dizziness and vertigo but is often unrecognized by health care providers. VM causes significant impairment in level of function and quality of life, and the diagnosis should be considered when symptoms cannot be explained by other etiologies. Information and guidance are provided to raise clinicians’ awareness of VM in order to increase accurate diagnosis, guide management decisions, and improve patient health outcomes.
Headache and dizziness are common reasons for primary care visits. In the general population, the prevalence of migraine is 13% to 16%, while dizziness and vertigo affect approximately 20% to 30%.1 Despite the prevalence of these conditions, many providers are unaware of vestibular migraine (VM) and may overlook it when considering differential diagnoses for these symptoms.
This is not surprising since, until recently, the International Headache Society’s (IHS) International Classification of Headache Disorders (ICHD)—considered the “gold standard” for defining and diagnosing headaches across all medical specialties—included no diagnostic criteria for VM.2 The second edition of the ICHD, ICHD-2, identified vertigo as a symptom of migraine only in the context of basilar migraine.1 Since fewer than 10% of patients with both vertigo and migraine met the criteria for basilar migraine, most VM patients could not be correctly classified under ICHD-2.1
In 2012, the Committee for Classification of Vestibular Disorders of the Bárány Society and the Migraine Classification Subcommittee of the IHS jointly published diagnostic criteria for VM.3 These criteria are included in the beta version of ICHD-3, published on the IHS website on July 3, 2013, for immediate use and field testing before ICHD-3 is finalized.4
DIAGNOSTIC CRITERIA FOR VM
The criteria for diagnosis of VM are as follows4:
A. At least five episodes fulfilling criteria C and D
B. A current or past history of migraine without aura or migraine with aura
C. Vestibular symptoms of moderate or severe intensity, lasting between 5 min and 72 h
D. At least 50% of episodes are associated with at least one of the following migrainous features:
- Headache with at least two of the following four characteristics:
a. Unilateral location
b. Pulsating quality
c. Moderate or severe intensity
d. Aggravation by routine physical activity - Photophobia and phonophobia
- Visual aura
E. Not better accounted for by another ICHD-3 diagnosis or by another vestibular disorder
Vestibular symptoms include3
• Spontaneous vertigo, which can be internal (false sensation of self-motion) or external (false sensation that surroundings are spinning)
• Positional vertigo (after change in head position)
• Visually induced vertigo (triggered by a complex or large moving visual stimulus)
• Head motion–induced vertigo
• Head motion–induced dizziness with nausea (dizziness is a sensation of disturbed spatial orientation)
Moderate vestibular symptoms interfere with, but do not prevent, daily activities; severe vestibular symptoms impede them.
On the next page: Diagnosis Overview >>
DIAGNOSIS: OVERVIEW
VM is a diagnosis of exclusion that is considered appropriate when no other peripheral or central vestibular disorder is present to account for the patient’s dizziness.5,6 Asking the patient the right questions will provide clues to the correct diagnosis.7 Most patients with VM present with normal physical, vestibular, and neurologic examinations, especially if examined when symptom-free.5 In contrast, examinations for competing diagnoses often reveal abnormal findings.
Vestibular vs nonvestibular vertigo. Typically, patients have difficulty describing their sensations with words more specific than “dizzy.”8 This lack of clarity is a challenge when the clinician is attempting to differentiate between true vertigo (ie, vertigo caused by vestibular dysfunction) and other types of nonvestibular dizziness. Specific categories of dizziness include vertigo, imbalance, presyncope, and lightheadedness; careful consideration must be given to the causes associated with each (see Table 1).9-11
Clinicians should focus on timing, duration of symptoms, triggers, and any other associated symptoms to determine the diagnosis.8,10 When evaluating a patient, a broad definition of vertigo, including spinning and/or rotational sensations as well as illusions of movement, is recommended.8
Peripheral vs central disorders. True vertigo must be further evaluated to determine whether its etiology is peripheral or central. In VM, a combination of both peripheral and central deficits can be seen.10 Clinicians must consider certain defining features to differentiate between these.
Peripheral Vertigo
If the cause of the patient's vertigo is peripheral, onset is often abrupt and the patient may experience mild-to-moderate imbalance that does not affect his or her ability to walk unassisted. Combined horizontal and rotational nystagmus may occur, which lessens or disappears with focused gaze. The nystagmus does not change direction when the patient gazes to either side and may fade after a few days.
The patient also may report experiencing tinnitus or hearing loss, accompanied by severe nausea or vomiting. Neurologic symptoms are rare in peripherally caused vertigo unless a concurrent diagnosis of migraine is confirmed.
Other symptoms may include weakness, dysarthria, changes in vision or hearing, paresthesias, changes in sensory or motor function, altered level of consciousness, and headache.10
Central Vertigo
Centrally caused vertigo often persists for hours to weeks, and neurologic symptoms are common. Patients have difficulty walking or standing still; problems with balance are severe. The nystagmus is purely horizontal, vertical, or rotational and may last for weeks to months. It is not inhibited with a focused gaze and may change direction with gaze. It is important to note that vertical nystagmus is 80% sensitive for vestibular nuclear or cerebellar central lesions.10
Tinnitus, if it occurs at all, is episodic, and nausea and/or vomiting vary from patient to patient. Patients presenting with central nervous system (CNS) disorders rarely complain of vertigo as their only symptom. Additional descriptions of dizziness may be used to describe the various cranial nerve abnormalities that suggest CNS etiology.9
DIFFERENTIAL DIAGNOSIS
Numerous conditions should be included in the differential when evaluating dizziness and vertigo symptoms. (See also Collie M. Vertigo: diagnosis and management. Clinician Reviews. 2013;23[12]:46-53.)
Peripheral Vertigo
Possible peripheral causes of vertigo include5,6,12,13
• Benign paroxysmal positional vertigo (BPPV)
• Vestibular neuritis
• Labyrinthitis
• Ménière disease
• Superior canal dehiscence
• Perilymphatic fistula
• Otitis media
• Aminoglycoside toxicity
• Trauma
BPPV is characterized by recurrent episodes of intense vertigo that last for seconds to one minute and are provoked by specific head movements. The Dix-Hallpike maneuver provokes vertigo and nystagmus and confirms the diagnosis.14 Vestibular neuritis and labyrinthitis present in similar ways. They are characterized by the onset of intense vertigo that can persist for several days, with nausea, vomiting, and imbalance also present. The main differentiating feature between them is associated hearing loss; vestibular neuritis is not associated with hearing loss, but labyrinthitis is. Both disorders are thought to be caused by inflammation of the vestibular nerve as the result of a viral infection. Patients may report recent upper respiratory infections or influenza like illnesses.10,12
Central Vertigo
Possible central causes of vertigo include5,6,13,15
• Acoustic neuroma (vestibular schwannoma)
• Cerebellar infarction
• Brainstem stroke
• Multiple sclerosis
• Episodic ataxia
• Psychogenic dizziness
Acoustic neuroma (vestibular schwannoma) is a benign growth on the vestibular nerve. Symptoms generally include progressive hearing loss and unilateral tinnitus accompanied by dizziness and imbalance.10 Acute attacks of vertigo are rare, but patients often complain of aural fullness, headache, and/or facial numbness.1,10
Cerebellar infarction usually presents with sudden onset of symptoms at maximal intensity. Risk factors for cerebellar infarction include a history of hypertension, coronary artery disease, diabetes, previous transient ischemic attack, smoking, alcohol consumption, atrial fibrillation, and hyperlipidemia.10
While only 5% of vertigo complaints are the result of CNS disorders, vertigo is an early symptom of brainstem stroke.15 Because of the significant morbidity and mortality associated with stroke, it must be considered in the initial diagnostic workup of vertigo.
Multiple sclerosis (MS) is an autoimmune disease in which the myelin axons in the CNS are destroyed. Dizziness and vertigo are common complaints associated with MS, but these patients will often present with other symptoms suggestive of CNS involvement. Common complaints include, but are not limited to, muscle weakness, fatigue, paresthesias, spasms, ataxia, pain, diplopia, dysarthria, heat intolerance, and urinary frequency.16
Episodic ataxia type 2 (EA2) is an inherited autosomal dominant disorder characterized by attacks of ataxia, vertigo, and nausea that can last from minutes to days. EA2 is often difficult to differentiate from VM due to symptom overlap. Fifty percent of patients with EA2 have a history of migraine headaches; often, there is a family history of similar symptoms.5
On the next page: Ménière Disease Versus VM >>
MÉNIÈRE DISEASE VERSUS VM
When headaches and dizziness coincide, VM is the most probable diagnosis.5 BPPV, Ménière disease, cerebellar disorders, motion sickness, and psychiatric syndromes (major depression and panic disorder) occur more often in patients with migraine than in those without.1 Ménière disease and VM often coexist, and up to 50% of patients with Ménière disease also meet criteria for migraine.5 (For more information, see Pearson T. Ménière disease: a lifelong merry-go-round. Clinician Reviews. 2013;23[10]:38-43.) Because many of their symptoms overlap, differentiating between Ménière disease and VM is critical; key differences in symptom presentation are as follows.17,18
Vertigo. The vertigo of Ménière disease is short-lived, lasting up to 24 hours.17 In contrast, episodes of vertigo with VM can last more than 24 hours; patients may experience a continuous rocking sensation for several weeks or even months.
Hearing loss. Sensorineural hearing loss in patients with Ménière disease is progressive and most often unilateral, but can be bilateral. In patients with VM, sensorineural hearing loss is rare; if it occurs, it is usually episodic and not progressive.17
Tinnitus. Tinnitus is a symptom of both Ménière disease and VM and may be unilateral or bilateral in both. In Ménière disease, patients report tinnitus of significant intensity, low in pitch, and “roaring,” whereas in VM, the tinnitus is usually high-pitched and unobtrusive.
Headache. Unless a concurrent diagnosis of migraine exists, patients with Ménière disease do not present with headache or photophobia. Many patients with VM, though not all, confirm a positive history of headache.
Phonophobia. Phonophobia is a frequent symptom in patients with VM.17
On the next page: Clinical Manifestations >>
CLINICAL MANIFESTATIONS OF VM
The clinical presentation of VM varies for each patient, as do the frequency and duration of episodes. Manifestations of VM may include5,19,20
• Vertigo associated with visual triggers
• Nausea and/or dizziness
• Spontaneous positional vertigo
• Head motion intolerance
• Motion sickness
• Lightheadedness
• Headache
• Chronic disequilibrium
• Inability to concentrate
• Mild hearing loss or tinnitus
• Cervicalgia
• Anxiety
• Panic
• Photophobia
• Phonophobia
• Sensory aura
Visual vertigo, described as vertigo worsened by visual stimulation such as moving scenes, scrolling patterns, and movement of large crowds or traffic, is highly suggestive of VM.19 Aura-type symptoms are of significant diagnostic importance because they may be the only apparent connection between vertigo and migraine.19
The duration of vertigo and dizziness may range from seconds to weeks. These episodes may have no temporal relationship with headaches. Vertigo and dizziness can continue for more than 24 hours for about half of VM patients; in some, symptoms persist for several weeks or more.12 In addition, vertigo and headache may never occur together, which further increases the diagnostic challenge for this disorder.1,5
Although many hypotheses exist, the pathophysiology of VM remains unclear.
Patient History
It is vital to obtain a detailed medical and social history in order to determine possible etiologies for symptoms. Medications in particular must be reviewed with care because many are known to induce vestibular-type symptoms.
Cardiac agents of potential concern for causing dizziness include β-blockers, diuretics, ACE inhibitors, β-blockers, and nitrates. CNS agents associated with dizziness include antipsychotics, dopaminergic drugs, opioids/analgesics, hypnotics, anticonvulsants, tricyclic antidepressants, and muscle relaxants. Anticholinergics, phosphodiesterase type 5 inhibitors, antibacterials, aminoglycosides, fluoroquinolones, and antineoplastics may also lead to dizziness; several of these medications are also known to be ototoxic. Dizziness can also be related to orthostatic hypotension, which is a common adverse effect of many of the listed medications, especially when used in combination.7,9
Diabetes, hypertension, vascular diseases, and neurologic disorders should be considered as causes for vision and proprioception problems.7 Patients may present with a personal history of headaches for years before vestibular symptoms develop.6 Motion sickness is suggestive of a possible migraine diagnosis.19
Positive family history is common for migraineurs.21 Patients ages 30 to 39 are affected most frequently, with an estimated prevalence of 7% in men and 24.4% in women.22
Physical Examination
The focused physical should include cranial nerve assessments, an otoscopic examination, hearing evaluation with a tuning fork, and audiometry, if a hearing deficit is detected. Minor oculomotor abnormalities, such as “weak” nystagmus with vertical, horizontal, torsional, or positional components, may be noted in approximately 70% of patients with VM.5 Various in-office tests (see Table 2) should also be conducted to narrow the possible causes for vertigo and dizziness and rule out more serious disorders.7,10 ,11,23
Diagnostic Workup
Laboratory tests are generally not recommended because they identify the cause of vertigo in only approximately 1% of patients.23 Similarly, routine use of MRI or CT is not recommended, but these modalities may be indicated for patients with focal neurologic deficits or risk factors for cerebrovascular disease, or if acute treatments for peripheral vertigo are unsuccessful.10
On the next page: Treatment >>
TREATMENT OF VM
Nonpharmacologic
Nonpharmacologic measures to prevent VM attacks include the avoidance of “triggers” through dietary restrictions, stress reduction, and healthy lifestyle modifications. Diaries can be used to help identify common triggers to avoid (see Table 3); patients should understand that it may take up to three months before noticeable improvement in symptoms is seen. Once symptoms have resolved, cautious re-introduction of suspect foods may be attempted.24
Vestibular rehabilitation therapy promotes CNS compensation for inner ear deficits and reduces symptoms of disequilibrium and dizziness.25 It is helpful for complications of VM, such as anxiety, visual dependence, or loss of confidence with balance.10
Pharmacologic
Prophylactic drug therapy is the mainstay of medical management for VM when nonpharmacologic measures are inadequate; episodes are frequent and severe; or symptoms are of long duration.5 The drugs’ adverse effect profiles, as well as patient comorbidities, should guide the choice of therapy.26
Abortive migraine therapies have not been shown to be effective for symptoms of dizziness17 and may cause rebound symptoms. Vestibular suppressants (promethazine, dimenhydrinate, and meclizine) can be used for acute episodes of VM.5
According to evidence-based guidelines for the preventive treatment of migraine in adults,26 the pharmacologic options include multiple drug classes stratified by level, depending on the quality of evidence supporting their effectiveness in migraine prevention.
Level A comprises medications with established efficacy. These include divalproex sodium, sodium valproate, topiramate, frovatriptan (for menstrual migraine), metoprolol, propanolol, and timolol.
Level B medications that are “probably effective” include naratriptan, zolmitriptan, amitriptyline, venlafaxine, atenolol, and nadolol.
Medications that are “possibly effective” are in the Level C category and include carbamazepine, nebivolol, pindolol, lisinopril, candesartan, clonidine, guanfacine, and cyproheptadine.
The Level U category drugs are labeled “inadequate or conflicting data to support or refute medication use” and include fluvoxamine, fluoxetine, protriptyline, gabapentin, bisoprolol, cyclandelate, acenocoumarol, warfarin, picotamide, acetazolamide, nicardipine, nifedipine, nimodipine, and verapamil.
Medications that are established as possibly or probably ineffective fall under the category of Other and include clomipramine, lamotrigine, acebutolol, clonazepam, nabumetone, oxcarbazepine, and telmisartan.
When initiating therapy, low doses are recommended because migraineurs’ sensory hypersensitivity is thought to extend to medications.5 Sequence and dosing information, along with contraindications, should be considered when choosing medical therapies (see Table 4).5,12,19,21,26 Patient response to treatment is evaluated after one to three months, and medications should be discontinued if symptoms persist, maximum dose is reached, or significant adverse effects occur.5 A reasonable goal of therapy is to reduce episode frequency by more than 50%.19 Should both lifestyle modifications and medications fail, referral to a specialist for reevaluation of the diagnosis is warranted.8
On the next page: Conclusion >>
CONCLUSION
While VM is considered the most common cause of recurrent vertigo and dizziness, few primary care providers are familiar with the diagnosis. Differentiating among the various causes for these symptoms and determining if the cause is a CNS or peripheral system disorder are essential to narrowing the differential diagnoses.
The inclusion of VM in the ICHD-3 system will increase both clinician awareness and accurate diagnosis of the disorder. Office-based assessments can be performed to evaluate these common complaints, and numerous medical therapies are available to successfully treat patients with VM. Through greater awareness of VM and use of evidence-based diagnostic and treatment guidelines, clinicians can significantly improve quality of life and health outcomes for patients with the disorder.
1. Lempert T, Neuhauser H. Epidemiology of vertigo, migraine and vestibular migraine. J Neurol. 2009;256(3):333-338.
2. The International Headache Society. The International Headache Classification. 2nd ed. www.ihs-classification.org/en/01_einleitung/02_einleitung/. Accessed May 16, 2014.
3. Lempert T, Oleson J, Furman J, et al. Vestibular migraine: diagnostic criteria. J Vestib Res. 2012;22:167-172.
4. Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders. 3rd ed (beta version). Cephalalgia. 2013;33(9):629-808.
5. Cherchi M, Hain T. Migraine-associated vertigo. Otolaryngol Clin Am. 2011;44:367-375.
6. Honaker J, Samy R. Migraine-associated vestibulopathy. Curr Opin Otolaryngol Head Neck Surg. 2008;16:412-415.
7. Shaia WT. Dizziness evaluation. http://emedicine.medscape.com/article/1831429-overview. Accessed May 16, 2014.
8. Watson S. Vertigo and migraine: "how can it be a migraine if I don’t have a headache?" Med Today. 2011;12(12):36-43.
9. Post RE, Dickerson LM. Dizziness: a diagnostic approach. Am Fam Physician. 2010;82(4):361-368.
10. Furman M, Rizzolo D. Evaluating the patient with vertigo: a complex complaint made simple. JAAPA. 2011;24(10):52-58.
11. Kuo CH, Pang T, Chang R. Vertigo – part 1 - assessment in general practice. Aust Fam Physician. 2008;37(5):341-347.
12. Hain, T. Migraine associated vertigo: vestibular migraine. www.dizziness-and-balance.com/disorders/central/migraine/mav.html. Accessed May 16, 2014.
13. Cha YH, Kane MJ, Baloh RW. Familial clustering of migraine, episodic vertigo, and Ménière’s disease. Otol Neurotol. 2008;29(1):93-96.
14. Clark MM. How to sort out a complaint of dizziness. Patient Care. 2003;37: 44-52.
15. Hain TC. Brainstem strokes associated with vertigo or hearing symptoms. www.dizziness-and- balance.com/disorders/central/strokes/brainstem%20strokes.htm. Accessed May 16, 2014.
16. Luzzio C, Dangond F. Multiple sclerosis. http://emedicine.medscape.com/article/1146199-overview. Accessed May 16, 2014.
17. Benson AG. Migraine-associated vertigo. http://emedicine.medscape.com/article/884136-overview#aw2aab6b5. Accessed May 16, 2014.
18. Teggi R, Fabiano B, Recanata P, et al. Case reports on two patients with episodic vertigo, fluctuating hearing loss, and migraine responding to prophylactic drugs for migraine. Ménière disease or migraine-associated vertigo? Acta Otorhinolaryngol Ital. 2010;30(4):217-220.
19. Neuhauser H, Lempert T. Vestibular migraine. Neurol Clin. 2009;27:379-391.
20. Kramer J, Buskirk J. Vestibular migraine a/k/a migraine-associated vertigo. www.vestibular.org/migraine-associated-vertigo-mav. Accessed April 1, 2014.
21. Chawla J. Migraine headache. http://emedicine.medscape.com/article/1142556-overview. Accessed May 16, 2014.
22. Cutrer MF, Bajwa ZH, Sabahat A. Pathophysiology, clinical manifestations, and diagnosis of migraine in adults. www.uptodate.com/contents/patho physiology-clinical-manifestations-and-diagnosis-of-migraine-in-adults. Accessed May 16, 2014.
23. Labuguen R. Initial evaluation of vertigo [published correction appears in Am Fam Physician. 2006;73(10):1704]. Am Fam Physician. 2006;73(2):244-251.
24. Texiedo M. Common migraine food triggers. http://deedee.dbi.udel.edu/MichaelTeixidoMD/patientInfo/migrainesFoodTrig.html. Accessed May 16, 2014.
25. Bisdorff AR. Management of vestibular migraine. Ther Adv Neurol Disord. 2011;4(3):183-191.
26. Silberstein S, Holland S, Freitag F, et al; Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults [published correction appears in Neurology. 2013;80:871]. Neurology. 2012;78(17):1337-1345.
1. Lempert T, Neuhauser H. Epidemiology of vertigo, migraine and vestibular migraine. J Neurol. 2009;256(3):333-338.
2. The International Headache Society. The International Headache Classification. 2nd ed. www.ihs-classification.org/en/01_einleitung/02_einleitung/. Accessed May 16, 2014.
3. Lempert T, Oleson J, Furman J, et al. Vestibular migraine: diagnostic criteria. J Vestib Res. 2012;22:167-172.
4. Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders. 3rd ed (beta version). Cephalalgia. 2013;33(9):629-808.
5. Cherchi M, Hain T. Migraine-associated vertigo. Otolaryngol Clin Am. 2011;44:367-375.
6. Honaker J, Samy R. Migraine-associated vestibulopathy. Curr Opin Otolaryngol Head Neck Surg. 2008;16:412-415.
7. Shaia WT. Dizziness evaluation. http://emedicine.medscape.com/article/1831429-overview. Accessed May 16, 2014.
8. Watson S. Vertigo and migraine: "how can it be a migraine if I don’t have a headache?" Med Today. 2011;12(12):36-43.
9. Post RE, Dickerson LM. Dizziness: a diagnostic approach. Am Fam Physician. 2010;82(4):361-368.
10. Furman M, Rizzolo D. Evaluating the patient with vertigo: a complex complaint made simple. JAAPA. 2011;24(10):52-58.
11. Kuo CH, Pang T, Chang R. Vertigo – part 1 - assessment in general practice. Aust Fam Physician. 2008;37(5):341-347.
12. Hain, T. Migraine associated vertigo: vestibular migraine. www.dizziness-and-balance.com/disorders/central/migraine/mav.html. Accessed May 16, 2014.
13. Cha YH, Kane MJ, Baloh RW. Familial clustering of migraine, episodic vertigo, and Ménière’s disease. Otol Neurotol. 2008;29(1):93-96.
14. Clark MM. How to sort out a complaint of dizziness. Patient Care. 2003;37: 44-52.
15. Hain TC. Brainstem strokes associated with vertigo or hearing symptoms. www.dizziness-and- balance.com/disorders/central/strokes/brainstem%20strokes.htm. Accessed May 16, 2014.
16. Luzzio C, Dangond F. Multiple sclerosis. http://emedicine.medscape.com/article/1146199-overview. Accessed May 16, 2014.
17. Benson AG. Migraine-associated vertigo. http://emedicine.medscape.com/article/884136-overview#aw2aab6b5. Accessed May 16, 2014.
18. Teggi R, Fabiano B, Recanata P, et al. Case reports on two patients with episodic vertigo, fluctuating hearing loss, and migraine responding to prophylactic drugs for migraine. Ménière disease or migraine-associated vertigo? Acta Otorhinolaryngol Ital. 2010;30(4):217-220.
19. Neuhauser H, Lempert T. Vestibular migraine. Neurol Clin. 2009;27:379-391.
20. Kramer J, Buskirk J. Vestibular migraine a/k/a migraine-associated vertigo. www.vestibular.org/migraine-associated-vertigo-mav. Accessed April 1, 2014.
21. Chawla J. Migraine headache. http://emedicine.medscape.com/article/1142556-overview. Accessed May 16, 2014.
22. Cutrer MF, Bajwa ZH, Sabahat A. Pathophysiology, clinical manifestations, and diagnosis of migraine in adults. www.uptodate.com/contents/patho physiology-clinical-manifestations-and-diagnosis-of-migraine-in-adults. Accessed May 16, 2014.
23. Labuguen R. Initial evaluation of vertigo [published correction appears in Am Fam Physician. 2006;73(10):1704]. Am Fam Physician. 2006;73(2):244-251.
24. Texiedo M. Common migraine food triggers. http://deedee.dbi.udel.edu/MichaelTeixidoMD/patientInfo/migrainesFoodTrig.html. Accessed May 16, 2014.
25. Bisdorff AR. Management of vestibular migraine. Ther Adv Neurol Disord. 2011;4(3):183-191.
26. Silberstein S, Holland S, Freitag F, et al; Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults [published correction appears in Neurology. 2013;80:871]. Neurology. 2012;78(17):1337-1345.