User login
Although the VA has the largest health care system in the U.S., not every VA facility offers medical subspecialty care. As a result, patients are often separated by long distances from services they need.
At the VA Pittsburgh Healthcare System (VAPHS) in Pennsylvania, about 15,700 veterans received care in 2011. The Gastroenterology Department (GD) served many of these patients: 5,800 patients were seen in clinic appointments, 2,500 underwent colonoscopy, and 1,700 underwent esophagogastroduodenoscopy (EGD). Patients traveled up to 150 miles from 3 states for appointments and procedures. Prior to each procedure, a face-to-face appointment was standard practice for most patients to plan procedures and ensure medical stability. Patients expressed dissatisfaction with transportation, cost, time, and inconvenience, particularly when they were required to attend both the preprocedure and procedure appointments.
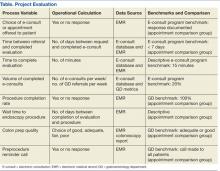
Patient satisfaction, timely care, and appropriate use of resources are important VA goals of care, so the VAPHS developed an electronic consultation (e-consult) program as a component of its long-term strategic plan. The goal was to increase access to care through the use of an e-consult in lieu of a face-to-face appointment for select patients. The e-consult program established guidelines and benchmark goals (Table). The program also established a database to track the benchmarks.
The purpose of this quality improvement (QI) project was to evaluate e-consults in the GD over a 6-month period from January 2012, when e-consults were implemented in the GD, to July 2012. Based on the outcomes, recommendations for program continuation, change, and sustainability were made.
Background
Telemedicine using information technologies has been reported as a viable solution to support health care delivery when distance limits patients’ access to care.1,2 Telemedicine has also been shown to improve efficacy in clinical decision making and reduce costs. It also can increase patient satisfaction by reducing travel and time, minimize duplication of diagnostic testing, and integrate services effectively across multiple sites when an electronic medical record (EMR) is in place.1-5
A randomized controlled trial in 2004 compared a standard outpatient referral appointment with a joint teleconsultation between provider, specialist, and patient.3 In the teleconsultation arm, there was higher patient satisfaction, fewer diagnostic tests (particularly in gastroenterology), and lower patient costs.
A study published in 2009 examined the impact of cardiac, dermatologic, and diabetes teleconsultations on organization and patient outcomes in 950 patients in 30 rural communities.2 Rapid access to care was provided for 85% of the patients. Organizational benefits included resource savings and efficacy improvement measured by a provider opinion Likert scale. Patient benefits included reductions in wait times, transportation savings, avoidance of unnecessary office visits, and ease of use.
A large systematic review of telemedicine services across all medical specialties in 2006 included 106 published studies.4 Clinical outcomes (decision making, diagnosis, and management) were similar between conventional care and telemedicine in specialty care, particularly in neurology and psychiatry. Virtual consults provided equal care to traditional specialty visits.6
Communication and coordination of care via an e-consult instead of a face-to-face clinic visit was evaluated by Horner and colleagues.5 The authors identified e-consult benefits for patients and specialists and that e-consults can reduce unnecessary referrals and appointments by 30%. They concluded that reserved time to complete e-consults must be built into workflow systems and that an advanced EMR was necessary for successful use of e-consults.
Two studies have evaluated satisfaction with e-consults. A preliminary analysis of satisfaction with e-consults was conducted in 2009 by K. L. Rodriguez, PhD, and colleagues (unpublished data). Patients, primary care providers (PCPs), and medical specialists reported overall satisfaction in 8 satisfaction domains. A pilot study of 34 patients in 2011 with inflammatory bowel disease compared a standard patient-GD physician encounter with a video encounter.7 The authors reported patient satisfaction, appointment time, wait times, and quality of care were similar for the 2 groups.
Methods
The GD where this QI project was completed consisted of a clinic staffed by nurse practitioners (NPs) and a procedure lab staffed by gastroenterology physicians. Before e-consult implementation, a NP reviewed and triaged new referrals daily. During the project period, an average of 25 to 35 new referrals were received daily via the EMR. Referrals came mostly from PCPs requesting an evaluation of their patients’ gastroenterology problem. Patients were triaged either to an appointment for evaluation or directly to the GD procedure lab for EGD or colonoscopy.
When e-consults were implemented, several changes occurred. Two providers were assigned to new referral triage, and they were expected to process 20% as e-consults. In the EMR, e-consult note titles, templates, and an e-consult encounter form were created, and staff was given access to the e-consult tracking database. The EMR referral template was amended so the entering provider could say whether a face-to-face appointment was desired or whether an e-consult was acceptable. The patient was to be included in decision making about this choice. Department staff had permission to triage according to judgment and expertise; thus, appointment requests could be triaged to e-consults, and e-consult requests could be triaged to appointments.
To complete an e-consult, the EMR was reviewed for medical diagnoses, medications, diagnostics, and recent physical exam. A summary note outlining an impression, treatment recommendations, and follow-up was entered in the EMR and communicated to the PCP. In most cases, no discussion with the patient occurred. The encounter form was completed, and information was entered into the tracking database. The database was installed on each provider’s computer who processed e-consults. If EGD or colonoscopy was indicated, the scheduler was notified to call the patient. Once a procedure date was established, procedure orders were completed in the EMR, and instructions were mailed to the patient.
Project Description and Evaluation
The project was reviewed by the Institutional Review Board and determined to be a QI project. VA organizational policies were followed for data collection and security. Benchmarks were identified from the e-consult program and from the GD, where available. Process variables were determined to measure benchmark outcomes. (Table)
To identify participants, a retrospective chart review was performed. A total of 203 potential patients were identified from the e-consult program database for the 6-month period between January and July 2012. For comparison, 50 patients who attended an appointment during the same time frame were systematically identified in the EMR. Although this comparison group was eligible for e-consults, they were triaged to in-person appointments and subsequently had colonoscopies completed.
Outcome data were extracted from the e-consult program database and the EMR. The data analysis was descriptive. Summary aggregate data were compared with the benchmarks and comparison patient outcomes. The Table summarizes the process variables, how they were measured, where they came from, and what the comparisons were.
Discussion
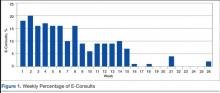
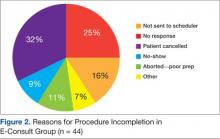
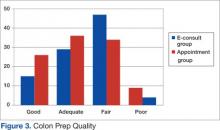
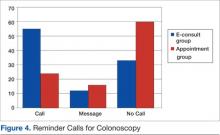
Figure 1 illustrates the volume of completed e-consults from January to July 2012. A gastroenterology procedure was not indicated in 43 patients. A procedure was indicated for 160 patients and completed in 116 patients (72%). One hundred procedures were colonoscopies, and 16 were EGDs. Figure 2 provides reasons why procedures were not completed in 44 patients (27%). Group comparisons of colon prep quality and preprocedure reminder calls are displayed in Figures 3 and 4, respectively.
This project sought to evaluate VAPHS GD e-consults beginning in January 2012. Process variables were established to measure benchmarks in the e-consult program and in the GD. Some benchmarks were met with outcomes that were comparable between the groups, while others were not. To our knowledge, this project is the first to evaluate e-consults in the subspecialty of gastroenterology.
Volume of Completed E-Consults
The benchmark for 20% e-consults was not met (Figure 1). For weeks 1 through 8, the volume was between 10% and 20%. Lower volume in weeks 9 through 15 (late March and April) may have been due to staff vacations. Not only do the outcomes show a downward trend in e-consult volume, they also show a precipitous fall in volume at week 15 to almost no e-consults for the remainder of the project. To explore reasons for this outcome, the workflow process of new referral triage and e-consults was reviewed.
Two providers (1 NP, 1 physician) were assigned to new referral triage and e-consults from weeks 1 through 14. At week 15, the physician was reassigned to perform procedures. From this point, only 1 NP worked on e-consults and referral triage. Competing time demands included an e-consult encounter form, tracking database entry, procedure orders, patient instructions, appointment changes, phone calls, and resolution of medications issues for procedures. The triage NP was also required to see patients in the clinic. Each day, only a half-day was allotted to complete e-consults, new referral triage (25-35/day), and the aforementioned tasks.
Therefore, it became clear that a half-day was not sufficient to meet the 20% benchmark for e-consults. Horner and colleagues also found that dedicated time in workflow processes was necessary to allow for e-consult completion.5
E-Consults vs Appointment Groups
All patients in both groups were offered the choice of e-consult or appointment; this benchmark was met. Of the 203 e-consult patients, 70% requested an appointment, but their evaluation was completed as an e-consult. By design, the appointment group patients chose e-consult but were triaged to appointment due to time constraints and the high volume of new referrals.
Evaluations via e-consult were completed within 2 to 3 days, whereas the mean for appointments was 19 days, with the longest time frame of 44 days. Thus, e-consult evaluations were completed sooner. Rapid access to care was also found by Zanaboni and colleagues.2
When appointments are delayed, patient complaints or status may change, which in turn may affect treatment plans. In addition, the reason for referral may have already resolved by the actual appointment, rendering the appointment unnecessary. This can be viewed as a missed opportunity for another patient to be seen. Ideally, it is best for a patient to be evaluated soon after a new referral is made.
The VA encounter form for an e-consult had only one 5-digit code, which allotted only 15 minutes of work credit. Encounter form codes were established by the Center for Medicare and Medicaid Services (CMS) for billing purposes in the private sector, with coding levels based on information documented in a chart note: review of systems, physical exam, and diagnoses decision making. Because all criteria could not be met in an e-consult, only 1 code was assigned for VAPHS e-consults. The CMS has specific telemedicine codes; it was unknown why they were not used for e-consults.
E-consults took an average of 19 minutes to complete, with 91 completed in ≤ 15 minutes and over half (112) having taken > 15 minutes. Therefore, the actual workload was not captured, and more work was done than was credited. To speculate, e-consults were in their infancy; a learning curve may have existed as staff became accustomed to this new process.
The EMRs were reviewed for the 7 e-consults that took > 30 minutes to complete. Two were in the early stage of e-consult implementation, but the remainder were scattered throughout. Patients in these e-consults had complicated medical histories and perhaps should not have been triaged to e-consult. Theoretically, only uncomplicated patients with simple reasons for gastroenterology referral should be triaged to e-consult, allowing for a shorter time frame and higher volume.
The wait times to procedure were 58 days for the e-consult group and 39 days in the appointment group. Although wait time was originally identified as an outcome, its relevance is questionable after looking at the outcome data. The procedure appointment date was a subjective decision by the patient; many factors affected what date the patient established, including weekday preference, time off from work, caretaker availability, season, and staffing. Many patients rescheduled their initial procedure dates, often several times. These factors are reflected in the variable ranges of wait times.
Colon Prep Quality
Colon prep refers to patient instructions on the day before the procedure and includes a clear liquid diet, drinking a liquid solution to empty bowel contents, and no food or liquid after midnight. Prep quality is stated in the colonoscopy report. During the procedure, the physician makes a visual decision based on presence or absence of stool inside the colon. Prep quality is important, because retained stool can preclude thorough visualization of the colon wall for polyps or abnormalities. In the event of fair and poor preps, the colonoscopy might be aborted and rescheduled or completed, but with the recommendation for another colonoscopy in a short time frame, such as 1 to 3 years.
Forty-four percent of the e-consult group and 62% of the appointment group had good or adequate preps. Thus, more patients in the appointment group achieved good and adequate preps, and far fewer achieved fair or poor preps. One important point was that almost half (47%) of the e-consult group had only a fair prep (Figure 3).
A number of reasons have been identified in the literature, which might help us understand these findings. First, patients may not fully understand or adhere to prep instructions.8-10 Furthermore, certain medical diagnoses are known to affect prep quality (ie, diabetes, thyroid disease, constipation).11,12 Another potential factor is the manner in which prep quality is determined.13,14 However, due to the focus of this QI study, the influential drivers of prep quality can only be inferred from the literature; thus, a future research or QI study is warranted to ascertain the underlying mechanism of colon prep quality in our specific veteran population.
Preprocedure Reminder Calls
Outcomes were essentially reversed between the 2 groups (Figure 4). Between 50% and 60% of the e-consult group received a call, while the same percentage of appointment patients did not. All patients did attend their procedure appointment. A GD goal was to call every patient before their procedure, but the ability to make the calls was staffing-dependent, which may explain these findings.
Most Relevant Findings
Although this project provides a thorough analysis of various benchmarks within this recently implemented e-consult gastroenterology program, 3 findings emerged that were identified as most relevant. First, the benchmark of 20% volume of completed e-consults was not met. A review of the workflow processes revealed that a daily allotment of only a half-day was not sufficient to complete e-consults, referral triage, and related tasks.
Second, outcomes for colon prep quality and preprocedure reminder calls were also relevant. Although beyond the scope of this project, the question arose of a relationship between prep quality and the reminder call: Does the reminder call affect prep quality? The goal of colon prep is to achieve a good or adequate prep. The purpose of the reminder call was to confirm the appointment and to review the colon prep. Among patients in both groups who achieved only a fair prep, 62% in the e-consult group did receive the reminder call; thus, the call seemed to have failed in helping these patients achieve an adequate or good prep. The actual content of colon prep review during the call was unknown, but certainly bears improvement.
Another speculation concerned the prep instruction sheet. Although all patients received the same sheet, e-consult patients received it in the mail and read it themselves, while it was directly reviewed face-to-face with the appointment patients. Questions remain whether a face-to-face review increases the likelihood for a better prep and how to help e-consult patients achieve optimal prep, since they are not seen face-to-face.
Practice Implications and Sustaining Measures
Theoretically, e-consults are a viable alternative to face-to-face appointments. Potential advantages include efficient use of an EMR, avoidance of unnecessary appointments, and improved access to care for patients who require an appointment. Although patient satisfaction was not measured in this project, the literature review revealed that satisfaction was increased through use of various virtual health care modalities, including a preliminary analysis in this facility by the aforementioned 2009 study by K. L. Rodriguez (unpublished data). Based on findings in this project, the following 4 recommendations were made to improve benchmark outcomes and quality of care.
- Provide dedicated time to complete e-consults and related tasks. In this setting, a full day was recommended. An alternative was to hire a NP whose sole responsibility was e-consults.
- Develop a selection process to determine which new referrals are best suited for e-consult. This process will increase e-consult efficiency and decrease the time to complete an e-consult. Recommended selection criteria were (A) gastroenterology referrals only for simple symptoms or issues; (B) referrals only for a procedure; and (C) stable patients with uncomplicated medical histories.
- Sustain the preprocedure reminder phone call. The reminder call helps patients keep appointments and thus reduces a missed opportunity for care.
- Plan a future QI project or research study on patient colon prep quality for colonoscopy. Such a project might evaluate types of colon prep, how prep quality is measured, patient instructions, and the timing/content of pre-procedure reminder phone calls, particularly for e-consult patients.
Conclusion
This QI project provided outcomes for e-consults in the subspecialty of gastroenterology at the VAPHS. Although some benchmark outcomes were met and favorable, others were less favorable. By conducting this benchmark analysis, the areas of needed improvement are now clear. This analysis provides information so recommendations for process improvements can be made.
Quality of care improvement is an ongoing process at VAPHS. Since completion of this project, several processes have been adjusted so that outcomes will be improved. For example, corrective actions were taken for patients who did not complete their gastroenterology procedure. The process for scheduling gastroenterology procedures was adjusted for appointments and cancellations. Ongoing efforts to sustain the reminder phone call were put in place. Changes in NP staffing and time assigned for both clinical and nonclinical work were proposed and are currently under review.
It is the mission of the VA to provide access to care, patient satisfaction, timely care, and appropriate use of resources. Having the ability to highlight our strengths, as well as the willingness to recognize weaknesses, allows us to create new improved processes to provide the best care possible for our veterans.
Acknowledgments
This project was Elena Swann’s capstone for the Doctor of Nursing Practice Program, University of Pittsburgh School of Nursing in Pennsylvania. Rich Laufer, Larry Priscella, and Janie Fleming assisted with the VA Gastroenterology Clinic and procedure metrics. Dr. Melissa Taylor, VA associate chief nurse for research provided project guidance and manuscript revisions. Dr. Sandra Engberg, University of Pittsburgh School of Nursing faculty, assisted with project and manuscript development.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Bashshur RL, Shannon GW, Krupinski EA, et al. National telemedicine initiatives: Essential to healthcare reform. Telemed J E Health. 2009;15(6):600-610.
2. Zanaboni P, Scalvini S, Bernocchi P, Borghi G, Tridico C, Masella C. Teleconsultation service to improve healthcare in rural areas: Acceptance, organizational impact and appropriateness. BMC Health Serv Res. 2009;9:238.
3. Wallace P, Barber J, Clayton W, et al. Virtual outreach: A randomised controlled trial and economic evaluation of joint teleconferenced medical consultations. Health Technol Assess. 2004;8(50):1-106, iii-iv.
4. Hersh WR, Hickam DH, Severance SM, Dana TL, Pyle Krages K, Helfand M. Diagnosis, access and outcomes: Update of a systematic review of telemedicine services. J Telemed Telecare. 2006;12(suppl 2):S3-S31.
5. Horner K, Wagner E, Tufano J. Electronic consultations between primary and specialty care clinicians: Early insights. Issue Brief (Commonw Fund). 2011;23:1-14.
6. Angstman KB, Adamson SC, Furst JW, Houston MS, Rohrer JE. Provider satisfaction with virtual specialist consultations in a family medicine department. Health Care Manag (Frederick). 2009;28(1):14-18.
7. Krier M, Kaltenbach T, McQuaid K, Soetikno R. Potential use of telemedicine to provide outpatient care for inflammatory bowel disease. Am J Gastroenterol. 2011;106(12):2063-2067.
8. Calderwood AH, Lai EJ, Fix OK, Jacobson BC. An endoscopist-blinded, randomized, controlled trial of a simple visual aid to improve bowel preparation for screening colonoscopy. Gastrointest Endosc. 2011;73(2):307-314.
9. Hillyer GC, Basch CH, Basch CE, et al. Gastroenterologists’ perceived barriers to optimal pre-colonoscopy bowel preparation: Results of a national survey. J Cancer Educ. 2012;27(3):526-532.
10. Smith SG, von Wagner C, McGregor LM, et al. The influence of health literacy on comprehension of a colonoscopy preparation information leaflet. Dis Colon Rectum. 2012;55(10):1074-1080.
11. Mittal S, Lin YL, Tan A, Kuo YF, El-Serag HB, Goodwin JS. Limited life expectancy among a subgroup of Medicare beneficiaries receiving screening colonoscopies. Clin Gastroenterol Hepatol. 2014;12(3):443-450.e1.
12. Ko CW, Sonnenberg A. Comparing risks and benefits of colorectal cancer screening in elderly patients. Gastroenterology. 2005;129(4):1163-1170.
13. Ell C, Fischbach W, Keller R, et al; Hintertux Study Group. A randomized, blinded, prospective trial to compare the safety and efficacy of three bowel-cleansing solutions for colonoscopy (HSG-01*). Endoscopy. 2003;35(4):300-304.
14. Jansen SV, Goedhard JG, Winkens B, van Deursen CT. Preparation before colonoscopy: A randomized controlled trial comparing different regimes. Eur J Gastroenterol Hepatol. 2011;23(10):897-902.
Although the VA has the largest health care system in the U.S., not every VA facility offers medical subspecialty care. As a result, patients are often separated by long distances from services they need.
At the VA Pittsburgh Healthcare System (VAPHS) in Pennsylvania, about 15,700 veterans received care in 2011. The Gastroenterology Department (GD) served many of these patients: 5,800 patients were seen in clinic appointments, 2,500 underwent colonoscopy, and 1,700 underwent esophagogastroduodenoscopy (EGD). Patients traveled up to 150 miles from 3 states for appointments and procedures. Prior to each procedure, a face-to-face appointment was standard practice for most patients to plan procedures and ensure medical stability. Patients expressed dissatisfaction with transportation, cost, time, and inconvenience, particularly when they were required to attend both the preprocedure and procedure appointments.
Patient satisfaction, timely care, and appropriate use of resources are important VA goals of care, so the VAPHS developed an electronic consultation (e-consult) program as a component of its long-term strategic plan. The goal was to increase access to care through the use of an e-consult in lieu of a face-to-face appointment for select patients. The e-consult program established guidelines and benchmark goals (Table). The program also established a database to track the benchmarks.
The purpose of this quality improvement (QI) project was to evaluate e-consults in the GD over a 6-month period from January 2012, when e-consults were implemented in the GD, to July 2012. Based on the outcomes, recommendations for program continuation, change, and sustainability were made.
Background
Telemedicine using information technologies has been reported as a viable solution to support health care delivery when distance limits patients’ access to care.1,2 Telemedicine has also been shown to improve efficacy in clinical decision making and reduce costs. It also can increase patient satisfaction by reducing travel and time, minimize duplication of diagnostic testing, and integrate services effectively across multiple sites when an electronic medical record (EMR) is in place.1-5
A randomized controlled trial in 2004 compared a standard outpatient referral appointment with a joint teleconsultation between provider, specialist, and patient.3 In the teleconsultation arm, there was higher patient satisfaction, fewer diagnostic tests (particularly in gastroenterology), and lower patient costs.
A study published in 2009 examined the impact of cardiac, dermatologic, and diabetes teleconsultations on organization and patient outcomes in 950 patients in 30 rural communities.2 Rapid access to care was provided for 85% of the patients. Organizational benefits included resource savings and efficacy improvement measured by a provider opinion Likert scale. Patient benefits included reductions in wait times, transportation savings, avoidance of unnecessary office visits, and ease of use.
A large systematic review of telemedicine services across all medical specialties in 2006 included 106 published studies.4 Clinical outcomes (decision making, diagnosis, and management) were similar between conventional care and telemedicine in specialty care, particularly in neurology and psychiatry. Virtual consults provided equal care to traditional specialty visits.6
Communication and coordination of care via an e-consult instead of a face-to-face clinic visit was evaluated by Horner and colleagues.5 The authors identified e-consult benefits for patients and specialists and that e-consults can reduce unnecessary referrals and appointments by 30%. They concluded that reserved time to complete e-consults must be built into workflow systems and that an advanced EMR was necessary for successful use of e-consults.
Two studies have evaluated satisfaction with e-consults. A preliminary analysis of satisfaction with e-consults was conducted in 2009 by K. L. Rodriguez, PhD, and colleagues (unpublished data). Patients, primary care providers (PCPs), and medical specialists reported overall satisfaction in 8 satisfaction domains. A pilot study of 34 patients in 2011 with inflammatory bowel disease compared a standard patient-GD physician encounter with a video encounter.7 The authors reported patient satisfaction, appointment time, wait times, and quality of care were similar for the 2 groups.
Methods
The GD where this QI project was completed consisted of a clinic staffed by nurse practitioners (NPs) and a procedure lab staffed by gastroenterology physicians. Before e-consult implementation, a NP reviewed and triaged new referrals daily. During the project period, an average of 25 to 35 new referrals were received daily via the EMR. Referrals came mostly from PCPs requesting an evaluation of their patients’ gastroenterology problem. Patients were triaged either to an appointment for evaluation or directly to the GD procedure lab for EGD or colonoscopy.
When e-consults were implemented, several changes occurred. Two providers were assigned to new referral triage, and they were expected to process 20% as e-consults. In the EMR, e-consult note titles, templates, and an e-consult encounter form were created, and staff was given access to the e-consult tracking database. The EMR referral template was amended so the entering provider could say whether a face-to-face appointment was desired or whether an e-consult was acceptable. The patient was to be included in decision making about this choice. Department staff had permission to triage according to judgment and expertise; thus, appointment requests could be triaged to e-consults, and e-consult requests could be triaged to appointments.
To complete an e-consult, the EMR was reviewed for medical diagnoses, medications, diagnostics, and recent physical exam. A summary note outlining an impression, treatment recommendations, and follow-up was entered in the EMR and communicated to the PCP. In most cases, no discussion with the patient occurred. The encounter form was completed, and information was entered into the tracking database. The database was installed on each provider’s computer who processed e-consults. If EGD or colonoscopy was indicated, the scheduler was notified to call the patient. Once a procedure date was established, procedure orders were completed in the EMR, and instructions were mailed to the patient.
Project Description and Evaluation
The project was reviewed by the Institutional Review Board and determined to be a QI project. VA organizational policies were followed for data collection and security. Benchmarks were identified from the e-consult program and from the GD, where available. Process variables were determined to measure benchmark outcomes. (Table)
To identify participants, a retrospective chart review was performed. A total of 203 potential patients were identified from the e-consult program database for the 6-month period between January and July 2012. For comparison, 50 patients who attended an appointment during the same time frame were systematically identified in the EMR. Although this comparison group was eligible for e-consults, they were triaged to in-person appointments and subsequently had colonoscopies completed.
Outcome data were extracted from the e-consult program database and the EMR. The data analysis was descriptive. Summary aggregate data were compared with the benchmarks and comparison patient outcomes. The Table summarizes the process variables, how they were measured, where they came from, and what the comparisons were.
Discussion
Figure 1 illustrates the volume of completed e-consults from January to July 2012. A gastroenterology procedure was not indicated in 43 patients. A procedure was indicated for 160 patients and completed in 116 patients (72%). One hundred procedures were colonoscopies, and 16 were EGDs. Figure 2 provides reasons why procedures were not completed in 44 patients (27%). Group comparisons of colon prep quality and preprocedure reminder calls are displayed in Figures 3 and 4, respectively.
This project sought to evaluate VAPHS GD e-consults beginning in January 2012. Process variables were established to measure benchmarks in the e-consult program and in the GD. Some benchmarks were met with outcomes that were comparable between the groups, while others were not. To our knowledge, this project is the first to evaluate e-consults in the subspecialty of gastroenterology.
Volume of Completed E-Consults
The benchmark for 20% e-consults was not met (Figure 1). For weeks 1 through 8, the volume was between 10% and 20%. Lower volume in weeks 9 through 15 (late March and April) may have been due to staff vacations. Not only do the outcomes show a downward trend in e-consult volume, they also show a precipitous fall in volume at week 15 to almost no e-consults for the remainder of the project. To explore reasons for this outcome, the workflow process of new referral triage and e-consults was reviewed.
Two providers (1 NP, 1 physician) were assigned to new referral triage and e-consults from weeks 1 through 14. At week 15, the physician was reassigned to perform procedures. From this point, only 1 NP worked on e-consults and referral triage. Competing time demands included an e-consult encounter form, tracking database entry, procedure orders, patient instructions, appointment changes, phone calls, and resolution of medications issues for procedures. The triage NP was also required to see patients in the clinic. Each day, only a half-day was allotted to complete e-consults, new referral triage (25-35/day), and the aforementioned tasks.
Therefore, it became clear that a half-day was not sufficient to meet the 20% benchmark for e-consults. Horner and colleagues also found that dedicated time in workflow processes was necessary to allow for e-consult completion.5
E-Consults vs Appointment Groups
All patients in both groups were offered the choice of e-consult or appointment; this benchmark was met. Of the 203 e-consult patients, 70% requested an appointment, but their evaluation was completed as an e-consult. By design, the appointment group patients chose e-consult but were triaged to appointment due to time constraints and the high volume of new referrals.
Evaluations via e-consult were completed within 2 to 3 days, whereas the mean for appointments was 19 days, with the longest time frame of 44 days. Thus, e-consult evaluations were completed sooner. Rapid access to care was also found by Zanaboni and colleagues.2
When appointments are delayed, patient complaints or status may change, which in turn may affect treatment plans. In addition, the reason for referral may have already resolved by the actual appointment, rendering the appointment unnecessary. This can be viewed as a missed opportunity for another patient to be seen. Ideally, it is best for a patient to be evaluated soon after a new referral is made.
The VA encounter form for an e-consult had only one 5-digit code, which allotted only 15 minutes of work credit. Encounter form codes were established by the Center for Medicare and Medicaid Services (CMS) for billing purposes in the private sector, with coding levels based on information documented in a chart note: review of systems, physical exam, and diagnoses decision making. Because all criteria could not be met in an e-consult, only 1 code was assigned for VAPHS e-consults. The CMS has specific telemedicine codes; it was unknown why they were not used for e-consults.
E-consults took an average of 19 minutes to complete, with 91 completed in ≤ 15 minutes and over half (112) having taken > 15 minutes. Therefore, the actual workload was not captured, and more work was done than was credited. To speculate, e-consults were in their infancy; a learning curve may have existed as staff became accustomed to this new process.
The EMRs were reviewed for the 7 e-consults that took > 30 minutes to complete. Two were in the early stage of e-consult implementation, but the remainder were scattered throughout. Patients in these e-consults had complicated medical histories and perhaps should not have been triaged to e-consult. Theoretically, only uncomplicated patients with simple reasons for gastroenterology referral should be triaged to e-consult, allowing for a shorter time frame and higher volume.
The wait times to procedure were 58 days for the e-consult group and 39 days in the appointment group. Although wait time was originally identified as an outcome, its relevance is questionable after looking at the outcome data. The procedure appointment date was a subjective decision by the patient; many factors affected what date the patient established, including weekday preference, time off from work, caretaker availability, season, and staffing. Many patients rescheduled their initial procedure dates, often several times. These factors are reflected in the variable ranges of wait times.
Colon Prep Quality
Colon prep refers to patient instructions on the day before the procedure and includes a clear liquid diet, drinking a liquid solution to empty bowel contents, and no food or liquid after midnight. Prep quality is stated in the colonoscopy report. During the procedure, the physician makes a visual decision based on presence or absence of stool inside the colon. Prep quality is important, because retained stool can preclude thorough visualization of the colon wall for polyps or abnormalities. In the event of fair and poor preps, the colonoscopy might be aborted and rescheduled or completed, but with the recommendation for another colonoscopy in a short time frame, such as 1 to 3 years.
Forty-four percent of the e-consult group and 62% of the appointment group had good or adequate preps. Thus, more patients in the appointment group achieved good and adequate preps, and far fewer achieved fair or poor preps. One important point was that almost half (47%) of the e-consult group had only a fair prep (Figure 3).
A number of reasons have been identified in the literature, which might help us understand these findings. First, patients may not fully understand or adhere to prep instructions.8-10 Furthermore, certain medical diagnoses are known to affect prep quality (ie, diabetes, thyroid disease, constipation).11,12 Another potential factor is the manner in which prep quality is determined.13,14 However, due to the focus of this QI study, the influential drivers of prep quality can only be inferred from the literature; thus, a future research or QI study is warranted to ascertain the underlying mechanism of colon prep quality in our specific veteran population.
Preprocedure Reminder Calls
Outcomes were essentially reversed between the 2 groups (Figure 4). Between 50% and 60% of the e-consult group received a call, while the same percentage of appointment patients did not. All patients did attend their procedure appointment. A GD goal was to call every patient before their procedure, but the ability to make the calls was staffing-dependent, which may explain these findings.
Most Relevant Findings
Although this project provides a thorough analysis of various benchmarks within this recently implemented e-consult gastroenterology program, 3 findings emerged that were identified as most relevant. First, the benchmark of 20% volume of completed e-consults was not met. A review of the workflow processes revealed that a daily allotment of only a half-day was not sufficient to complete e-consults, referral triage, and related tasks.
Second, outcomes for colon prep quality and preprocedure reminder calls were also relevant. Although beyond the scope of this project, the question arose of a relationship between prep quality and the reminder call: Does the reminder call affect prep quality? The goal of colon prep is to achieve a good or adequate prep. The purpose of the reminder call was to confirm the appointment and to review the colon prep. Among patients in both groups who achieved only a fair prep, 62% in the e-consult group did receive the reminder call; thus, the call seemed to have failed in helping these patients achieve an adequate or good prep. The actual content of colon prep review during the call was unknown, but certainly bears improvement.
Another speculation concerned the prep instruction sheet. Although all patients received the same sheet, e-consult patients received it in the mail and read it themselves, while it was directly reviewed face-to-face with the appointment patients. Questions remain whether a face-to-face review increases the likelihood for a better prep and how to help e-consult patients achieve optimal prep, since they are not seen face-to-face.
Practice Implications and Sustaining Measures
Theoretically, e-consults are a viable alternative to face-to-face appointments. Potential advantages include efficient use of an EMR, avoidance of unnecessary appointments, and improved access to care for patients who require an appointment. Although patient satisfaction was not measured in this project, the literature review revealed that satisfaction was increased through use of various virtual health care modalities, including a preliminary analysis in this facility by the aforementioned 2009 study by K. L. Rodriguez (unpublished data). Based on findings in this project, the following 4 recommendations were made to improve benchmark outcomes and quality of care.
- Provide dedicated time to complete e-consults and related tasks. In this setting, a full day was recommended. An alternative was to hire a NP whose sole responsibility was e-consults.
- Develop a selection process to determine which new referrals are best suited for e-consult. This process will increase e-consult efficiency and decrease the time to complete an e-consult. Recommended selection criteria were (A) gastroenterology referrals only for simple symptoms or issues; (B) referrals only for a procedure; and (C) stable patients with uncomplicated medical histories.
- Sustain the preprocedure reminder phone call. The reminder call helps patients keep appointments and thus reduces a missed opportunity for care.
- Plan a future QI project or research study on patient colon prep quality for colonoscopy. Such a project might evaluate types of colon prep, how prep quality is measured, patient instructions, and the timing/content of pre-procedure reminder phone calls, particularly for e-consult patients.
Conclusion
This QI project provided outcomes for e-consults in the subspecialty of gastroenterology at the VAPHS. Although some benchmark outcomes were met and favorable, others were less favorable. By conducting this benchmark analysis, the areas of needed improvement are now clear. This analysis provides information so recommendations for process improvements can be made.
Quality of care improvement is an ongoing process at VAPHS. Since completion of this project, several processes have been adjusted so that outcomes will be improved. For example, corrective actions were taken for patients who did not complete their gastroenterology procedure. The process for scheduling gastroenterology procedures was adjusted for appointments and cancellations. Ongoing efforts to sustain the reminder phone call were put in place. Changes in NP staffing and time assigned for both clinical and nonclinical work were proposed and are currently under review.
It is the mission of the VA to provide access to care, patient satisfaction, timely care, and appropriate use of resources. Having the ability to highlight our strengths, as well as the willingness to recognize weaknesses, allows us to create new improved processes to provide the best care possible for our veterans.
Acknowledgments
This project was Elena Swann’s capstone for the Doctor of Nursing Practice Program, University of Pittsburgh School of Nursing in Pennsylvania. Rich Laufer, Larry Priscella, and Janie Fleming assisted with the VA Gastroenterology Clinic and procedure metrics. Dr. Melissa Taylor, VA associate chief nurse for research provided project guidance and manuscript revisions. Dr. Sandra Engberg, University of Pittsburgh School of Nursing faculty, assisted with project and manuscript development.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Although the VA has the largest health care system in the U.S., not every VA facility offers medical subspecialty care. As a result, patients are often separated by long distances from services they need.
At the VA Pittsburgh Healthcare System (VAPHS) in Pennsylvania, about 15,700 veterans received care in 2011. The Gastroenterology Department (GD) served many of these patients: 5,800 patients were seen in clinic appointments, 2,500 underwent colonoscopy, and 1,700 underwent esophagogastroduodenoscopy (EGD). Patients traveled up to 150 miles from 3 states for appointments and procedures. Prior to each procedure, a face-to-face appointment was standard practice for most patients to plan procedures and ensure medical stability. Patients expressed dissatisfaction with transportation, cost, time, and inconvenience, particularly when they were required to attend both the preprocedure and procedure appointments.
Patient satisfaction, timely care, and appropriate use of resources are important VA goals of care, so the VAPHS developed an electronic consultation (e-consult) program as a component of its long-term strategic plan. The goal was to increase access to care through the use of an e-consult in lieu of a face-to-face appointment for select patients. The e-consult program established guidelines and benchmark goals (Table). The program also established a database to track the benchmarks.
The purpose of this quality improvement (QI) project was to evaluate e-consults in the GD over a 6-month period from January 2012, when e-consults were implemented in the GD, to July 2012. Based on the outcomes, recommendations for program continuation, change, and sustainability were made.
Background
Telemedicine using information technologies has been reported as a viable solution to support health care delivery when distance limits patients’ access to care.1,2 Telemedicine has also been shown to improve efficacy in clinical decision making and reduce costs. It also can increase patient satisfaction by reducing travel and time, minimize duplication of diagnostic testing, and integrate services effectively across multiple sites when an electronic medical record (EMR) is in place.1-5
A randomized controlled trial in 2004 compared a standard outpatient referral appointment with a joint teleconsultation between provider, specialist, and patient.3 In the teleconsultation arm, there was higher patient satisfaction, fewer diagnostic tests (particularly in gastroenterology), and lower patient costs.
A study published in 2009 examined the impact of cardiac, dermatologic, and diabetes teleconsultations on organization and patient outcomes in 950 patients in 30 rural communities.2 Rapid access to care was provided for 85% of the patients. Organizational benefits included resource savings and efficacy improvement measured by a provider opinion Likert scale. Patient benefits included reductions in wait times, transportation savings, avoidance of unnecessary office visits, and ease of use.
A large systematic review of telemedicine services across all medical specialties in 2006 included 106 published studies.4 Clinical outcomes (decision making, diagnosis, and management) were similar between conventional care and telemedicine in specialty care, particularly in neurology and psychiatry. Virtual consults provided equal care to traditional specialty visits.6
Communication and coordination of care via an e-consult instead of a face-to-face clinic visit was evaluated by Horner and colleagues.5 The authors identified e-consult benefits for patients and specialists and that e-consults can reduce unnecessary referrals and appointments by 30%. They concluded that reserved time to complete e-consults must be built into workflow systems and that an advanced EMR was necessary for successful use of e-consults.
Two studies have evaluated satisfaction with e-consults. A preliminary analysis of satisfaction with e-consults was conducted in 2009 by K. L. Rodriguez, PhD, and colleagues (unpublished data). Patients, primary care providers (PCPs), and medical specialists reported overall satisfaction in 8 satisfaction domains. A pilot study of 34 patients in 2011 with inflammatory bowel disease compared a standard patient-GD physician encounter with a video encounter.7 The authors reported patient satisfaction, appointment time, wait times, and quality of care were similar for the 2 groups.
Methods
The GD where this QI project was completed consisted of a clinic staffed by nurse practitioners (NPs) and a procedure lab staffed by gastroenterology physicians. Before e-consult implementation, a NP reviewed and triaged new referrals daily. During the project period, an average of 25 to 35 new referrals were received daily via the EMR. Referrals came mostly from PCPs requesting an evaluation of their patients’ gastroenterology problem. Patients were triaged either to an appointment for evaluation or directly to the GD procedure lab for EGD or colonoscopy.
When e-consults were implemented, several changes occurred. Two providers were assigned to new referral triage, and they were expected to process 20% as e-consults. In the EMR, e-consult note titles, templates, and an e-consult encounter form were created, and staff was given access to the e-consult tracking database. The EMR referral template was amended so the entering provider could say whether a face-to-face appointment was desired or whether an e-consult was acceptable. The patient was to be included in decision making about this choice. Department staff had permission to triage according to judgment and expertise; thus, appointment requests could be triaged to e-consults, and e-consult requests could be triaged to appointments.
To complete an e-consult, the EMR was reviewed for medical diagnoses, medications, diagnostics, and recent physical exam. A summary note outlining an impression, treatment recommendations, and follow-up was entered in the EMR and communicated to the PCP. In most cases, no discussion with the patient occurred. The encounter form was completed, and information was entered into the tracking database. The database was installed on each provider’s computer who processed e-consults. If EGD or colonoscopy was indicated, the scheduler was notified to call the patient. Once a procedure date was established, procedure orders were completed in the EMR, and instructions were mailed to the patient.
Project Description and Evaluation
The project was reviewed by the Institutional Review Board and determined to be a QI project. VA organizational policies were followed for data collection and security. Benchmarks were identified from the e-consult program and from the GD, where available. Process variables were determined to measure benchmark outcomes. (Table)
To identify participants, a retrospective chart review was performed. A total of 203 potential patients were identified from the e-consult program database for the 6-month period between January and July 2012. For comparison, 50 patients who attended an appointment during the same time frame were systematically identified in the EMR. Although this comparison group was eligible for e-consults, they were triaged to in-person appointments and subsequently had colonoscopies completed.
Outcome data were extracted from the e-consult program database and the EMR. The data analysis was descriptive. Summary aggregate data were compared with the benchmarks and comparison patient outcomes. The Table summarizes the process variables, how they were measured, where they came from, and what the comparisons were.
Discussion
Figure 1 illustrates the volume of completed e-consults from January to July 2012. A gastroenterology procedure was not indicated in 43 patients. A procedure was indicated for 160 patients and completed in 116 patients (72%). One hundred procedures were colonoscopies, and 16 were EGDs. Figure 2 provides reasons why procedures were not completed in 44 patients (27%). Group comparisons of colon prep quality and preprocedure reminder calls are displayed in Figures 3 and 4, respectively.
This project sought to evaluate VAPHS GD e-consults beginning in January 2012. Process variables were established to measure benchmarks in the e-consult program and in the GD. Some benchmarks were met with outcomes that were comparable between the groups, while others were not. To our knowledge, this project is the first to evaluate e-consults in the subspecialty of gastroenterology.
Volume of Completed E-Consults
The benchmark for 20% e-consults was not met (Figure 1). For weeks 1 through 8, the volume was between 10% and 20%. Lower volume in weeks 9 through 15 (late March and April) may have been due to staff vacations. Not only do the outcomes show a downward trend in e-consult volume, they also show a precipitous fall in volume at week 15 to almost no e-consults for the remainder of the project. To explore reasons for this outcome, the workflow process of new referral triage and e-consults was reviewed.
Two providers (1 NP, 1 physician) were assigned to new referral triage and e-consults from weeks 1 through 14. At week 15, the physician was reassigned to perform procedures. From this point, only 1 NP worked on e-consults and referral triage. Competing time demands included an e-consult encounter form, tracking database entry, procedure orders, patient instructions, appointment changes, phone calls, and resolution of medications issues for procedures. The triage NP was also required to see patients in the clinic. Each day, only a half-day was allotted to complete e-consults, new referral triage (25-35/day), and the aforementioned tasks.
Therefore, it became clear that a half-day was not sufficient to meet the 20% benchmark for e-consults. Horner and colleagues also found that dedicated time in workflow processes was necessary to allow for e-consult completion.5
E-Consults vs Appointment Groups
All patients in both groups were offered the choice of e-consult or appointment; this benchmark was met. Of the 203 e-consult patients, 70% requested an appointment, but their evaluation was completed as an e-consult. By design, the appointment group patients chose e-consult but were triaged to appointment due to time constraints and the high volume of new referrals.
Evaluations via e-consult were completed within 2 to 3 days, whereas the mean for appointments was 19 days, with the longest time frame of 44 days. Thus, e-consult evaluations were completed sooner. Rapid access to care was also found by Zanaboni and colleagues.2
When appointments are delayed, patient complaints or status may change, which in turn may affect treatment plans. In addition, the reason for referral may have already resolved by the actual appointment, rendering the appointment unnecessary. This can be viewed as a missed opportunity for another patient to be seen. Ideally, it is best for a patient to be evaluated soon after a new referral is made.
The VA encounter form for an e-consult had only one 5-digit code, which allotted only 15 minutes of work credit. Encounter form codes were established by the Center for Medicare and Medicaid Services (CMS) for billing purposes in the private sector, with coding levels based on information documented in a chart note: review of systems, physical exam, and diagnoses decision making. Because all criteria could not be met in an e-consult, only 1 code was assigned for VAPHS e-consults. The CMS has specific telemedicine codes; it was unknown why they were not used for e-consults.
E-consults took an average of 19 minutes to complete, with 91 completed in ≤ 15 minutes and over half (112) having taken > 15 minutes. Therefore, the actual workload was not captured, and more work was done than was credited. To speculate, e-consults were in their infancy; a learning curve may have existed as staff became accustomed to this new process.
The EMRs were reviewed for the 7 e-consults that took > 30 minutes to complete. Two were in the early stage of e-consult implementation, but the remainder were scattered throughout. Patients in these e-consults had complicated medical histories and perhaps should not have been triaged to e-consult. Theoretically, only uncomplicated patients with simple reasons for gastroenterology referral should be triaged to e-consult, allowing for a shorter time frame and higher volume.
The wait times to procedure were 58 days for the e-consult group and 39 days in the appointment group. Although wait time was originally identified as an outcome, its relevance is questionable after looking at the outcome data. The procedure appointment date was a subjective decision by the patient; many factors affected what date the patient established, including weekday preference, time off from work, caretaker availability, season, and staffing. Many patients rescheduled their initial procedure dates, often several times. These factors are reflected in the variable ranges of wait times.
Colon Prep Quality
Colon prep refers to patient instructions on the day before the procedure and includes a clear liquid diet, drinking a liquid solution to empty bowel contents, and no food or liquid after midnight. Prep quality is stated in the colonoscopy report. During the procedure, the physician makes a visual decision based on presence or absence of stool inside the colon. Prep quality is important, because retained stool can preclude thorough visualization of the colon wall for polyps or abnormalities. In the event of fair and poor preps, the colonoscopy might be aborted and rescheduled or completed, but with the recommendation for another colonoscopy in a short time frame, such as 1 to 3 years.
Forty-four percent of the e-consult group and 62% of the appointment group had good or adequate preps. Thus, more patients in the appointment group achieved good and adequate preps, and far fewer achieved fair or poor preps. One important point was that almost half (47%) of the e-consult group had only a fair prep (Figure 3).
A number of reasons have been identified in the literature, which might help us understand these findings. First, patients may not fully understand or adhere to prep instructions.8-10 Furthermore, certain medical diagnoses are known to affect prep quality (ie, diabetes, thyroid disease, constipation).11,12 Another potential factor is the manner in which prep quality is determined.13,14 However, due to the focus of this QI study, the influential drivers of prep quality can only be inferred from the literature; thus, a future research or QI study is warranted to ascertain the underlying mechanism of colon prep quality in our specific veteran population.
Preprocedure Reminder Calls
Outcomes were essentially reversed between the 2 groups (Figure 4). Between 50% and 60% of the e-consult group received a call, while the same percentage of appointment patients did not. All patients did attend their procedure appointment. A GD goal was to call every patient before their procedure, but the ability to make the calls was staffing-dependent, which may explain these findings.
Most Relevant Findings
Although this project provides a thorough analysis of various benchmarks within this recently implemented e-consult gastroenterology program, 3 findings emerged that were identified as most relevant. First, the benchmark of 20% volume of completed e-consults was not met. A review of the workflow processes revealed that a daily allotment of only a half-day was not sufficient to complete e-consults, referral triage, and related tasks.
Second, outcomes for colon prep quality and preprocedure reminder calls were also relevant. Although beyond the scope of this project, the question arose of a relationship between prep quality and the reminder call: Does the reminder call affect prep quality? The goal of colon prep is to achieve a good or adequate prep. The purpose of the reminder call was to confirm the appointment and to review the colon prep. Among patients in both groups who achieved only a fair prep, 62% in the e-consult group did receive the reminder call; thus, the call seemed to have failed in helping these patients achieve an adequate or good prep. The actual content of colon prep review during the call was unknown, but certainly bears improvement.
Another speculation concerned the prep instruction sheet. Although all patients received the same sheet, e-consult patients received it in the mail and read it themselves, while it was directly reviewed face-to-face with the appointment patients. Questions remain whether a face-to-face review increases the likelihood for a better prep and how to help e-consult patients achieve optimal prep, since they are not seen face-to-face.
Practice Implications and Sustaining Measures
Theoretically, e-consults are a viable alternative to face-to-face appointments. Potential advantages include efficient use of an EMR, avoidance of unnecessary appointments, and improved access to care for patients who require an appointment. Although patient satisfaction was not measured in this project, the literature review revealed that satisfaction was increased through use of various virtual health care modalities, including a preliminary analysis in this facility by the aforementioned 2009 study by K. L. Rodriguez (unpublished data). Based on findings in this project, the following 4 recommendations were made to improve benchmark outcomes and quality of care.
- Provide dedicated time to complete e-consults and related tasks. In this setting, a full day was recommended. An alternative was to hire a NP whose sole responsibility was e-consults.
- Develop a selection process to determine which new referrals are best suited for e-consult. This process will increase e-consult efficiency and decrease the time to complete an e-consult. Recommended selection criteria were (A) gastroenterology referrals only for simple symptoms or issues; (B) referrals only for a procedure; and (C) stable patients with uncomplicated medical histories.
- Sustain the preprocedure reminder phone call. The reminder call helps patients keep appointments and thus reduces a missed opportunity for care.
- Plan a future QI project or research study on patient colon prep quality for colonoscopy. Such a project might evaluate types of colon prep, how prep quality is measured, patient instructions, and the timing/content of pre-procedure reminder phone calls, particularly for e-consult patients.
Conclusion
This QI project provided outcomes for e-consults in the subspecialty of gastroenterology at the VAPHS. Although some benchmark outcomes were met and favorable, others were less favorable. By conducting this benchmark analysis, the areas of needed improvement are now clear. This analysis provides information so recommendations for process improvements can be made.
Quality of care improvement is an ongoing process at VAPHS. Since completion of this project, several processes have been adjusted so that outcomes will be improved. For example, corrective actions were taken for patients who did not complete their gastroenterology procedure. The process for scheduling gastroenterology procedures was adjusted for appointments and cancellations. Ongoing efforts to sustain the reminder phone call were put in place. Changes in NP staffing and time assigned for both clinical and nonclinical work were proposed and are currently under review.
It is the mission of the VA to provide access to care, patient satisfaction, timely care, and appropriate use of resources. Having the ability to highlight our strengths, as well as the willingness to recognize weaknesses, allows us to create new improved processes to provide the best care possible for our veterans.
Acknowledgments
This project was Elena Swann’s capstone for the Doctor of Nursing Practice Program, University of Pittsburgh School of Nursing in Pennsylvania. Rich Laufer, Larry Priscella, and Janie Fleming assisted with the VA Gastroenterology Clinic and procedure metrics. Dr. Melissa Taylor, VA associate chief nurse for research provided project guidance and manuscript revisions. Dr. Sandra Engberg, University of Pittsburgh School of Nursing faculty, assisted with project and manuscript development.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Bashshur RL, Shannon GW, Krupinski EA, et al. National telemedicine initiatives: Essential to healthcare reform. Telemed J E Health. 2009;15(6):600-610.
2. Zanaboni P, Scalvini S, Bernocchi P, Borghi G, Tridico C, Masella C. Teleconsultation service to improve healthcare in rural areas: Acceptance, organizational impact and appropriateness. BMC Health Serv Res. 2009;9:238.
3. Wallace P, Barber J, Clayton W, et al. Virtual outreach: A randomised controlled trial and economic evaluation of joint teleconferenced medical consultations. Health Technol Assess. 2004;8(50):1-106, iii-iv.
4. Hersh WR, Hickam DH, Severance SM, Dana TL, Pyle Krages K, Helfand M. Diagnosis, access and outcomes: Update of a systematic review of telemedicine services. J Telemed Telecare. 2006;12(suppl 2):S3-S31.
5. Horner K, Wagner E, Tufano J. Electronic consultations between primary and specialty care clinicians: Early insights. Issue Brief (Commonw Fund). 2011;23:1-14.
6. Angstman KB, Adamson SC, Furst JW, Houston MS, Rohrer JE. Provider satisfaction with virtual specialist consultations in a family medicine department. Health Care Manag (Frederick). 2009;28(1):14-18.
7. Krier M, Kaltenbach T, McQuaid K, Soetikno R. Potential use of telemedicine to provide outpatient care for inflammatory bowel disease. Am J Gastroenterol. 2011;106(12):2063-2067.
8. Calderwood AH, Lai EJ, Fix OK, Jacobson BC. An endoscopist-blinded, randomized, controlled trial of a simple visual aid to improve bowel preparation for screening colonoscopy. Gastrointest Endosc. 2011;73(2):307-314.
9. Hillyer GC, Basch CH, Basch CE, et al. Gastroenterologists’ perceived barriers to optimal pre-colonoscopy bowel preparation: Results of a national survey. J Cancer Educ. 2012;27(3):526-532.
10. Smith SG, von Wagner C, McGregor LM, et al. The influence of health literacy on comprehension of a colonoscopy preparation information leaflet. Dis Colon Rectum. 2012;55(10):1074-1080.
11. Mittal S, Lin YL, Tan A, Kuo YF, El-Serag HB, Goodwin JS. Limited life expectancy among a subgroup of Medicare beneficiaries receiving screening colonoscopies. Clin Gastroenterol Hepatol. 2014;12(3):443-450.e1.
12. Ko CW, Sonnenberg A. Comparing risks and benefits of colorectal cancer screening in elderly patients. Gastroenterology. 2005;129(4):1163-1170.
13. Ell C, Fischbach W, Keller R, et al; Hintertux Study Group. A randomized, blinded, prospective trial to compare the safety and efficacy of three bowel-cleansing solutions for colonoscopy (HSG-01*). Endoscopy. 2003;35(4):300-304.
14. Jansen SV, Goedhard JG, Winkens B, van Deursen CT. Preparation before colonoscopy: A randomized controlled trial comparing different regimes. Eur J Gastroenterol Hepatol. 2011;23(10):897-902.
1. Bashshur RL, Shannon GW, Krupinski EA, et al. National telemedicine initiatives: Essential to healthcare reform. Telemed J E Health. 2009;15(6):600-610.
2. Zanaboni P, Scalvini S, Bernocchi P, Borghi G, Tridico C, Masella C. Teleconsultation service to improve healthcare in rural areas: Acceptance, organizational impact and appropriateness. BMC Health Serv Res. 2009;9:238.
3. Wallace P, Barber J, Clayton W, et al. Virtual outreach: A randomised controlled trial and economic evaluation of joint teleconferenced medical consultations. Health Technol Assess. 2004;8(50):1-106, iii-iv.
4. Hersh WR, Hickam DH, Severance SM, Dana TL, Pyle Krages K, Helfand M. Diagnosis, access and outcomes: Update of a systematic review of telemedicine services. J Telemed Telecare. 2006;12(suppl 2):S3-S31.
5. Horner K, Wagner E, Tufano J. Electronic consultations between primary and specialty care clinicians: Early insights. Issue Brief (Commonw Fund). 2011;23:1-14.
6. Angstman KB, Adamson SC, Furst JW, Houston MS, Rohrer JE. Provider satisfaction with virtual specialist consultations in a family medicine department. Health Care Manag (Frederick). 2009;28(1):14-18.
7. Krier M, Kaltenbach T, McQuaid K, Soetikno R. Potential use of telemedicine to provide outpatient care for inflammatory bowel disease. Am J Gastroenterol. 2011;106(12):2063-2067.
8. Calderwood AH, Lai EJ, Fix OK, Jacobson BC. An endoscopist-blinded, randomized, controlled trial of a simple visual aid to improve bowel preparation for screening colonoscopy. Gastrointest Endosc. 2011;73(2):307-314.
9. Hillyer GC, Basch CH, Basch CE, et al. Gastroenterologists’ perceived barriers to optimal pre-colonoscopy bowel preparation: Results of a national survey. J Cancer Educ. 2012;27(3):526-532.
10. Smith SG, von Wagner C, McGregor LM, et al. The influence of health literacy on comprehension of a colonoscopy preparation information leaflet. Dis Colon Rectum. 2012;55(10):1074-1080.
11. Mittal S, Lin YL, Tan A, Kuo YF, El-Serag HB, Goodwin JS. Limited life expectancy among a subgroup of Medicare beneficiaries receiving screening colonoscopies. Clin Gastroenterol Hepatol. 2014;12(3):443-450.e1.
12. Ko CW, Sonnenberg A. Comparing risks and benefits of colorectal cancer screening in elderly patients. Gastroenterology. 2005;129(4):1163-1170.
13. Ell C, Fischbach W, Keller R, et al; Hintertux Study Group. A randomized, blinded, prospective trial to compare the safety and efficacy of three bowel-cleansing solutions for colonoscopy (HSG-01*). Endoscopy. 2003;35(4):300-304.
14. Jansen SV, Goedhard JG, Winkens B, van Deursen CT. Preparation before colonoscopy: A randomized controlled trial comparing different regimes. Eur J Gastroenterol Hepatol. 2011;23(10):897-902.