User login
Hysteroscopic mechanical morcellators have gained popularity given their ease of use. Consequently, the resectoscope loop is being used less frequently, which has resulted in less familiarity with this device. The resectoscope loop, however, not only is cost effective but also allows for multiple distinct advantages, such as cold loop dissection of myomas and the ability to obtain electrosurgical hemostasis during operative hysteroscopy.
In this article, we review the basics of electrosurgical principles, compare outcomes associated with monopolar and bipolar resectoscopes, and discuss tips and tricks for optimizing surgical techniques when using the resectoscope loop for hysteroscopic myomectomy.
Evolution of hysteroscopy
The term hysteroscopy comes from the Greek words hystera, for uterus, and skopeo, meaning “to see.” The idea to investigate the uterus dates back to the year 1000 when physicians used a mirror with light to peer into the vaginal vault.
The first known successful hysteroscopy occurred in 1869 when Pantaleoni used an endoscope with a light source to identify uterine polyps in a 60-year-old woman with abnormal uterine bleeding. In 1898, Simon Duplay and Spiro Clado published the first textbook on hysteroscopy in which they described several models of hysteroscopic instruments and techniques.
In the 1950s, Harold Horace Hopkins and Karl Storz modified the shape and length of lenses within the endoscope by substituting longer cylindrical lenses for the old spherical lenses; this permitted improved image brightness and sharpness as well as a smaller diameter of the hysteroscope. Between the 1970s and 1980s, technological improvements allowed for the creation of practical and usable hysteroscopic instruments such as the resectoscope. The resectoscope, originally used in urology for transurethral resection of the prostate, was modified for hysteroscopy by incorporating the use of electrosurgical currents to aid in procedures.
Over the past few decades, continued refinements in technology have improved visualization and surgical techniques. For example, image clarity has been markedly improved, and narrow hysteroscope diameters, as small as 3 to 5 mm, require minimal to no cervical dilation.
Monopolar and bipolar resectoscopes
Electrosurgery is the application of an alternating electrical current to tissue to achieve the clinical effects of surgical cutting or hemostasis via cell vaporization or coagulation. Current runs from the electrosurgical unit (ESU) to the active electrode of the surgical instrument, then goes from the active electrode through the patient’s tissue to the return electrode, and then travels back to the ESU. This flow of current creates an electrical circuit (FIGURE).
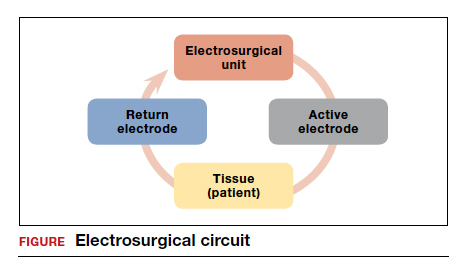
All electrosurgical devices have an active and a return electrode. The difference between monopolar and bipolar resectoscope devices lies in how the resectoscope loop is constructed. Bipolar resectoscope loops house the active and return electrodes on the same tip of the surgical device, which limits how much of the current flows through the patient. Alternatively, monopolar resectoscopes have only the active electrode on the tip of the device and the return electrode is off the surgical field, so the current flows through more of the patient. On monopolar electrosurgical devices, the current runs from the ESU to the active electrode (monopolar loop), which is then applied to tissue to produce the desired tissue effect. The current then travels via a path of least resistance from the surgical field through the patient to the return electrode, which is usually placed on the patient’s thigh, and then back to the ESU. The return electrode is often referred to as the grounding pad.
Continue to: How monopolar energy works...
How monopolar energy works
When first developed, all resectoscopes used monopolar energy. As such, throughout the 1990s, the monopolar resectoscope was the gold standard for performing electrosurgical hysteroscopy. Because the current travels a long distance between the active and the return electrode in a monopolar setup, a hypotonic, nonelectrolyte-rich medium (a poor conductor), such as glycine 1.5%, mannitol 5%, or sorbitol 3%, must be used. If an electrolyte-rich medium, such as normal saline, is used with a monopolar device, the current would be dispersed throughout the medium outside the operative field, causing unwanted tissue effects.
Although nonelectrolyte distension media improve visibility when encountering bleeding, they can be associated with hyponatremia, hyperglycemia, and even lifethreatening cerebral edema. Furthermore, glycine use is contraindicated in patients with renal or hepatic failure since oxidative deamination may cause hyperammonemia. Because of these numerous risk factors, the fluid deficit for hypotonic, nonelectrolyte distension media is limited to 1,000 mL, with a suggested maximum fluid deficit of 750 mL for elderly or fragile patients. Additionally, because the return electrode is off the surgical field in monopolar surgery, there is a risk of current diversion to the cervix, vagina, or vulva because the current travels between the active electrode on the surgical field to the return electrode on the patient’s thigh. The risk of current diversion is greater if there is damage to electrode insulation, loss of contact between the external sheath and the cervix, or direct coupling between the electrode and the surrounding tissue.
Advantages of the bipolar resectoscope
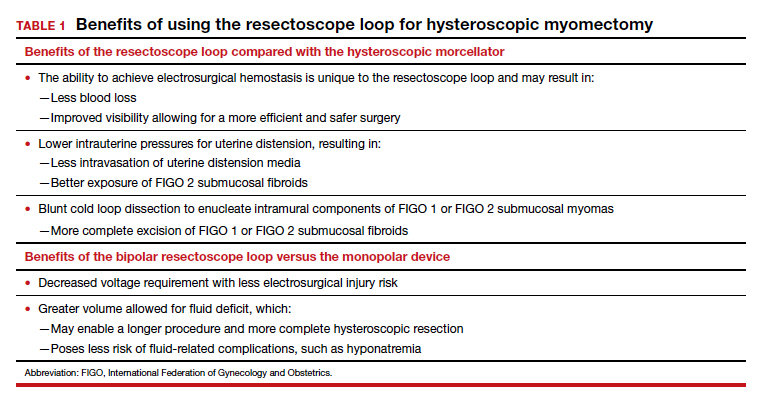
Because of the potential risks associated with the monopolar resectoscope, over the past 25 years the bipolar resectoscope emerged as an alternative due to its numerous benefits (TABLE 1).
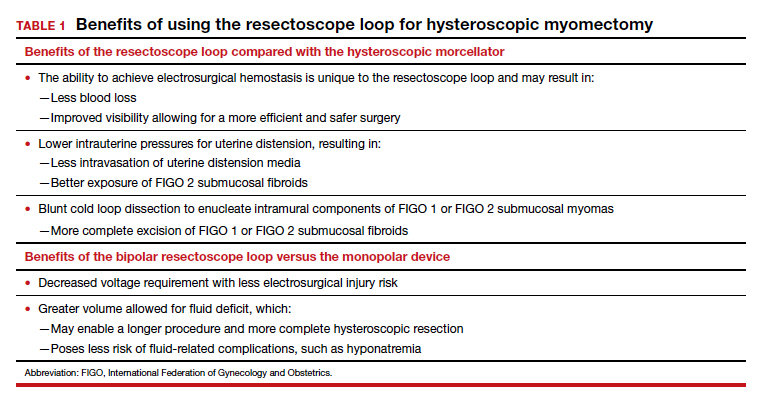
Unlike monopolar resectoscopes, bipolar resectoscopes require an electrolyte-rich distension medium such as 0.9% normal saline or lactated Ringer’s. These isotonic distension media allow a much higher fluid deficit (2,500 mL for healthy patients, 1,500 mL for elderly patients or patients with comorbidities) as the isotonic solution is safer to use. Furthermore, it allows for lower voltage settings and decreased electrical spread compared to the monopolar resectoscope since the current stays between the 2 electrodes. Because isotonic media are miscible with blood, however, a potential drawback is that in cases with bleeding, visibility may be more limited compared to hypotonic distension media.
Evidence on fertility outcomes
Several studies have compared operative and fertility outcomes with the use of monopolar versus bipolar hysteroscopy.
In a randomized controlled trial (RCT) comparing outcomes after hysteroscopy with a monopolar (glycine 1.5%) versus bipolar (0.9% normal saline) 26 French resectoscope loop, Berg and colleagues found that the only significant difference between the 2 groups was that the change in serum sodium pre and postoperatively was greater in the monopolar group despite having a smaller mean fluid deficit (765 mL vs 1,227 mL).1
Similarly, in a study of fertility outcomes after monopolar versus bipolar hysteroscopic myomectomy with use of a 26 French resectoscope Collins knife, Roy and colleagues found no significant differences in postoperative pregnancy rates or successful pregnancy outcomes, operative time, fluid deficit, or improvement in menstrual symptoms.2 However, the monopolar group had a much higher incidence of postoperative hyponatremia (30% vs 0%) that required additional days of hospitalization despite similar fluid deficits of between 600 and 700 mL.2
Similar findings were noted in another RCT that compared operative outcomes between monopolar and bipolar resectoscope usage during metroplasty for infertility, with a postoperative hyponatremia incidence of 17.1% in the monopolar group versus 0% in the bipolar group despite similar fluid deficits.3 Energy type had no effect on reproductive outcomes in either group.3
Continue to: How does the resectoscope compare with mechanical tissue removal systems?...
How does the resectoscope compare with mechanical tissue removal systems?
In 2005, the first hysteroscopic mechanical tissue removal system was introduced in the United States, providing an additional treatment method for such intrauterine masses as fibroids and polyps.
Advantages. Rather than using an electrical current, these tissue removal systems use a rotating blade with suction that is introduced through a specially designed rigid hysteroscopic sheath. As the instrument incises the pathology, the tissue is removed from the intrauterine cavity and collected in a specimen bag inside the fluid management system. This immediate removal of tissue allows for insertion of the device only once during initial entry, decreasing both the risk of perforation and operative times. Furthermore, mechanical tissue removal systems can be used with isotonic media, negating the risks associated with hypotonic media. Currently, the 2 mechanical tissue removal systems available in the United States are the TruClear and the MyoSure hysteroscopic tissue removal systems.
Studies comparing mechanical tissue removal of polyps and myomas with conventional resectoscope resection have found that mechanical tissue removal is associated with reduced operative time, fluid deficit, and number of instrument insertions.4-8 However, studies have found no significant difference in postoperative patient satisfaction.7,9
Additionally, hysteroscopic tissue removal systems have an easier learning curve. Van Dongen and colleagues conducted an RCT to compare resident-in-training comfort levels when learning to use both a mechanical tissue removal system and a traditional resectoscope; they found increased comfort with the hysteroscopic tissue removal system, suggesting greater ease of use.10
Drawbacks. Despite their many benefits, mechanical tissue removal systems have some disadvantages when compared with the resectoscope. First, mechanical tissue removal systems are associated with higher instrument costs. In addition, they have extremely limited ability to achieve hemostasis when encountering blood vessels during resection, resulting in poor visibility especially when resecting large myomas with feeding vessels.
Hysteroscopic mechanical tissue removal systems typically use higher intrauterine pressures for uterine distension compared with the resectoscope, especially when trying to improve visibility in a bloody surgical field. Increasing the intrauterine pressure with the distension media allows for compression of the blood vessels. As a result, however, submucosal fibroids classified as FIGO 2 (International Federation of Gynecology and Obstetrics) may be less visible since the higher intrauterine pressure can compress both blood vessels and submucosal fibroids
Additionally, mechanical tissue removal systems have limited ability to resect the intramural component of FIGO 1 or FIGO 2 submucosal fibroids since the intramural portion is embedded in the myometrium. Use of the resectoscope loop instead allows for a technique called the cold loop dissection, which uses the resectoscope loop to bluntly dissect and enucleate the intramural component of FIGO 1 and FIGO 2 submucosal myomas from the surrounding myometrium without activating the current. This blunt cold loop dissection technique allows for a deeper and more thorough resection. Often, if the pseudocapsule plane is identified, even the intramural component of FIGO 1 or FIGO 2 submucosal fibroids can be resected, enabling complete removal.
Lastly, mechanical tissue removal systems are not always faster than resectoscopes for all pathology. We prefer using the resectoscope for larger myomas (>3 cm) as the resectoscope allows for resection and removal of larger myoma chips, helping to decrease operative times. Given the many benefits of the resectoscope, we argue that the resectoscope loop remains a crucial instrument in operative gynecology and that learners should continue to hone their hysteroscopic skills with both the resectoscope and mechanical tissue removal systems.
Tips and tricks for hysteroscopic myomectomy with the resectoscope loop
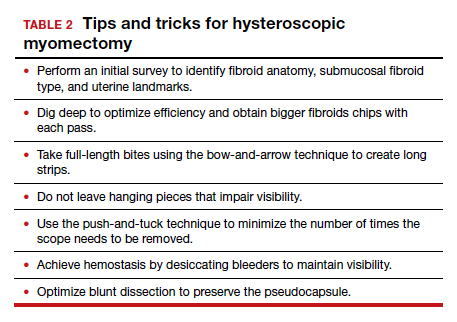
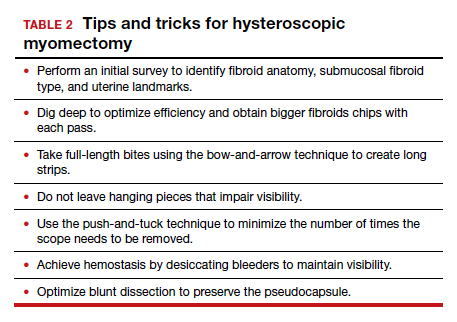
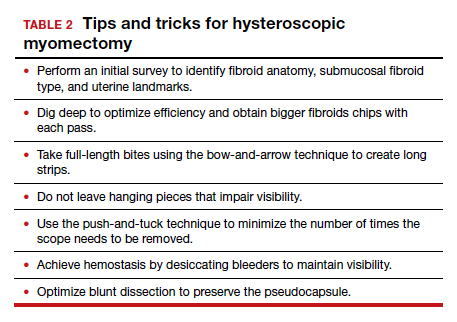
In the video below, "Bipolar resectoscope: Optimizing safe myomectomy," we review specific surgical techniques for optimizing outcomes and safety with the resectoscope loop. These include:
- bow-and-arrow technique
- identification of the fibroid anatomy (pseudocapsule plane)
- blunt cold loop dissection
- the push-and-tuck method
- efficient electrosurgical hemostasis (TABLE 2).
Although we use bipolar energy during this resection, the resection technique using the monopolar loop is the same.

The takeaway
The resectoscope loop is a valuable tool that offers gynecologic surgeons a wider range of techniques for myomectomy. It also offers several surgical and clinical advantages. It is important to train residents in the use of both hysteroscopic mechanical tissue removal systems and resectoscope loops. ●
- Berg A, Sandvik L, Langebrekke A, et al. A randomized trial comparing monopolar electrodes using glycine 1.5% with two different types of bipolar electrodes (TCRis, Versapoint) using saline, in hysteroscopic surgery. Fertil Steril. 2009;91:1273- 1278.
- Roy KK, Metta S, Kansal Y, et al. A prospective randomized study comparing unipolar versus bipolar hysteroscopic myomectomy in infertile women. J Hum Reprod Sci. 2017;10:185-193.
- Roy KK, Kansal Y, Subbaiah M, et al. Hysteroscopic septal resection using unipolar resectoscope versus bipolar resectoscope: prospective, randomized study. J Obstet Gynaecol Res. 2015;41:952-956.
- Borg MH, Shehata A. Uterine morcellator versus resectoscopy in the management of heavy menstrual flow in reproductiveage women. J Gyn Res. 2016;2:1-8.
- Emanuel MH, Wamsteker K. The intra uterine morcellator: a new hysteroscopic operating technique to remove intrauterine polyps and myomas. J Minim Invasive Gynecol. 2005;12:62-66.
- Smith PP, Middleton LJ, Connor M, et al. Hysteroscopic morcellation compared with electrical resection of endometrial polyps: a randomized controlled trial. Obstet Gynecol. 2014;123:745-751.
- Vitale SG, Sapia F, Rapisarda AMC, et al. Hysteroscopic morcellation of submucous myomas: a systematic review. Biomed Res Int. 2017;2017:6848250.
- Stoll F, Lecointre L, Meyer N, et al. Randomized study comparing a reusable morcellator with a resectoscope in the hysteroscopic treatment of uterine polyps: the RESMO study. J Minimal Invasive Gyn. 2021;28:801-810.
- Lee MM, Matsuzono T. Hysteroscopic intrauterine morcellation of submucosal fibroids: preliminary results in Hong Kong and comparisons with conventional hysteroscopic monopolar loop resection. Hong Kong Med J. 2016;22:56-61.
- van Dongen H, Emanuel MH, Wolterbeek R, et al. Hysteroscopic morcellator for removal of intrauterine polyps and myomas: a randomized controlled pilot study among residents in training. J Minim Invasive Gynecol. 2008;15:466-471.
Hysteroscopic mechanical morcellators have gained popularity given their ease of use. Consequently, the resectoscope loop is being used less frequently, which has resulted in less familiarity with this device. The resectoscope loop, however, not only is cost effective but also allows for multiple distinct advantages, such as cold loop dissection of myomas and the ability to obtain electrosurgical hemostasis during operative hysteroscopy.
In this article, we review the basics of electrosurgical principles, compare outcomes associated with monopolar and bipolar resectoscopes, and discuss tips and tricks for optimizing surgical techniques when using the resectoscope loop for hysteroscopic myomectomy.
Evolution of hysteroscopy
The term hysteroscopy comes from the Greek words hystera, for uterus, and skopeo, meaning “to see.” The idea to investigate the uterus dates back to the year 1000 when physicians used a mirror with light to peer into the vaginal vault.
The first known successful hysteroscopy occurred in 1869 when Pantaleoni used an endoscope with a light source to identify uterine polyps in a 60-year-old woman with abnormal uterine bleeding. In 1898, Simon Duplay and Spiro Clado published the first textbook on hysteroscopy in which they described several models of hysteroscopic instruments and techniques.
In the 1950s, Harold Horace Hopkins and Karl Storz modified the shape and length of lenses within the endoscope by substituting longer cylindrical lenses for the old spherical lenses; this permitted improved image brightness and sharpness as well as a smaller diameter of the hysteroscope. Between the 1970s and 1980s, technological improvements allowed for the creation of practical and usable hysteroscopic instruments such as the resectoscope. The resectoscope, originally used in urology for transurethral resection of the prostate, was modified for hysteroscopy by incorporating the use of electrosurgical currents to aid in procedures.
Over the past few decades, continued refinements in technology have improved visualization and surgical techniques. For example, image clarity has been markedly improved, and narrow hysteroscope diameters, as small as 3 to 5 mm, require minimal to no cervical dilation.
Monopolar and bipolar resectoscopes
Electrosurgery is the application of an alternating electrical current to tissue to achieve the clinical effects of surgical cutting or hemostasis via cell vaporization or coagulation. Current runs from the electrosurgical unit (ESU) to the active electrode of the surgical instrument, then goes from the active electrode through the patient’s tissue to the return electrode, and then travels back to the ESU. This flow of current creates an electrical circuit (FIGURE).
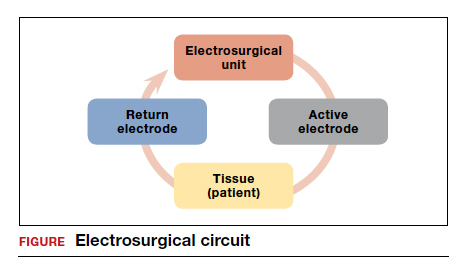
All electrosurgical devices have an active and a return electrode. The difference between monopolar and bipolar resectoscope devices lies in how the resectoscope loop is constructed. Bipolar resectoscope loops house the active and return electrodes on the same tip of the surgical device, which limits how much of the current flows through the patient. Alternatively, monopolar resectoscopes have only the active electrode on the tip of the device and the return electrode is off the surgical field, so the current flows through more of the patient. On monopolar electrosurgical devices, the current runs from the ESU to the active electrode (monopolar loop), which is then applied to tissue to produce the desired tissue effect. The current then travels via a path of least resistance from the surgical field through the patient to the return electrode, which is usually placed on the patient’s thigh, and then back to the ESU. The return electrode is often referred to as the grounding pad.
Continue to: How monopolar energy works...
How monopolar energy works
When first developed, all resectoscopes used monopolar energy. As such, throughout the 1990s, the monopolar resectoscope was the gold standard for performing electrosurgical hysteroscopy. Because the current travels a long distance between the active and the return electrode in a monopolar setup, a hypotonic, nonelectrolyte-rich medium (a poor conductor), such as glycine 1.5%, mannitol 5%, or sorbitol 3%, must be used. If an electrolyte-rich medium, such as normal saline, is used with a monopolar device, the current would be dispersed throughout the medium outside the operative field, causing unwanted tissue effects.
Although nonelectrolyte distension media improve visibility when encountering bleeding, they can be associated with hyponatremia, hyperglycemia, and even lifethreatening cerebral edema. Furthermore, glycine use is contraindicated in patients with renal or hepatic failure since oxidative deamination may cause hyperammonemia. Because of these numerous risk factors, the fluid deficit for hypotonic, nonelectrolyte distension media is limited to 1,000 mL, with a suggested maximum fluid deficit of 750 mL for elderly or fragile patients. Additionally, because the return electrode is off the surgical field in monopolar surgery, there is a risk of current diversion to the cervix, vagina, or vulva because the current travels between the active electrode on the surgical field to the return electrode on the patient’s thigh. The risk of current diversion is greater if there is damage to electrode insulation, loss of contact between the external sheath and the cervix, or direct coupling between the electrode and the surrounding tissue.
Advantages of the bipolar resectoscope
Because of the potential risks associated with the monopolar resectoscope, over the past 25 years the bipolar resectoscope emerged as an alternative due to its numerous benefits (TABLE 1).
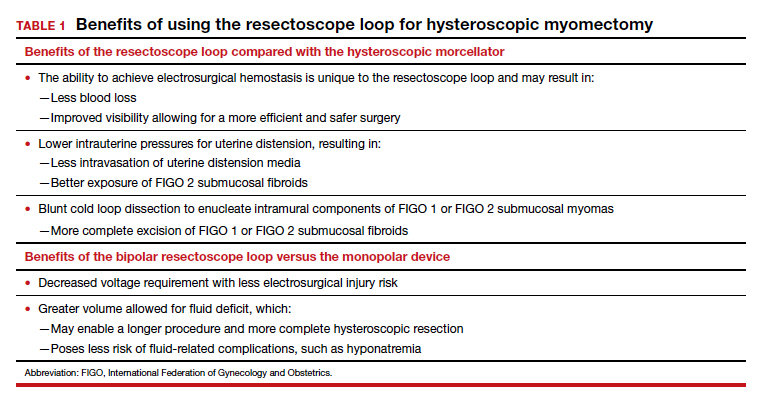
Unlike monopolar resectoscopes, bipolar resectoscopes require an electrolyte-rich distension medium such as 0.9% normal saline or lactated Ringer’s. These isotonic distension media allow a much higher fluid deficit (2,500 mL for healthy patients, 1,500 mL for elderly patients or patients with comorbidities) as the isotonic solution is safer to use. Furthermore, it allows for lower voltage settings and decreased electrical spread compared to the monopolar resectoscope since the current stays between the 2 electrodes. Because isotonic media are miscible with blood, however, a potential drawback is that in cases with bleeding, visibility may be more limited compared to hypotonic distension media.
Evidence on fertility outcomes
Several studies have compared operative and fertility outcomes with the use of monopolar versus bipolar hysteroscopy.
In a randomized controlled trial (RCT) comparing outcomes after hysteroscopy with a monopolar (glycine 1.5%) versus bipolar (0.9% normal saline) 26 French resectoscope loop, Berg and colleagues found that the only significant difference between the 2 groups was that the change in serum sodium pre and postoperatively was greater in the monopolar group despite having a smaller mean fluid deficit (765 mL vs 1,227 mL).1
Similarly, in a study of fertility outcomes after monopolar versus bipolar hysteroscopic myomectomy with use of a 26 French resectoscope Collins knife, Roy and colleagues found no significant differences in postoperative pregnancy rates or successful pregnancy outcomes, operative time, fluid deficit, or improvement in menstrual symptoms.2 However, the monopolar group had a much higher incidence of postoperative hyponatremia (30% vs 0%) that required additional days of hospitalization despite similar fluid deficits of between 600 and 700 mL.2
Similar findings were noted in another RCT that compared operative outcomes between monopolar and bipolar resectoscope usage during metroplasty for infertility, with a postoperative hyponatremia incidence of 17.1% in the monopolar group versus 0% in the bipolar group despite similar fluid deficits.3 Energy type had no effect on reproductive outcomes in either group.3
Continue to: How does the resectoscope compare with mechanical tissue removal systems?...
How does the resectoscope compare with mechanical tissue removal systems?
In 2005, the first hysteroscopic mechanical tissue removal system was introduced in the United States, providing an additional treatment method for such intrauterine masses as fibroids and polyps.
Advantages. Rather than using an electrical current, these tissue removal systems use a rotating blade with suction that is introduced through a specially designed rigid hysteroscopic sheath. As the instrument incises the pathology, the tissue is removed from the intrauterine cavity and collected in a specimen bag inside the fluid management system. This immediate removal of tissue allows for insertion of the device only once during initial entry, decreasing both the risk of perforation and operative times. Furthermore, mechanical tissue removal systems can be used with isotonic media, negating the risks associated with hypotonic media. Currently, the 2 mechanical tissue removal systems available in the United States are the TruClear and the MyoSure hysteroscopic tissue removal systems.
Studies comparing mechanical tissue removal of polyps and myomas with conventional resectoscope resection have found that mechanical tissue removal is associated with reduced operative time, fluid deficit, and number of instrument insertions.4-8 However, studies have found no significant difference in postoperative patient satisfaction.7,9
Additionally, hysteroscopic tissue removal systems have an easier learning curve. Van Dongen and colleagues conducted an RCT to compare resident-in-training comfort levels when learning to use both a mechanical tissue removal system and a traditional resectoscope; they found increased comfort with the hysteroscopic tissue removal system, suggesting greater ease of use.10
Drawbacks. Despite their many benefits, mechanical tissue removal systems have some disadvantages when compared with the resectoscope. First, mechanical tissue removal systems are associated with higher instrument costs. In addition, they have extremely limited ability to achieve hemostasis when encountering blood vessels during resection, resulting in poor visibility especially when resecting large myomas with feeding vessels.
Hysteroscopic mechanical tissue removal systems typically use higher intrauterine pressures for uterine distension compared with the resectoscope, especially when trying to improve visibility in a bloody surgical field. Increasing the intrauterine pressure with the distension media allows for compression of the blood vessels. As a result, however, submucosal fibroids classified as FIGO 2 (International Federation of Gynecology and Obstetrics) may be less visible since the higher intrauterine pressure can compress both blood vessels and submucosal fibroids
Additionally, mechanical tissue removal systems have limited ability to resect the intramural component of FIGO 1 or FIGO 2 submucosal fibroids since the intramural portion is embedded in the myometrium. Use of the resectoscope loop instead allows for a technique called the cold loop dissection, which uses the resectoscope loop to bluntly dissect and enucleate the intramural component of FIGO 1 and FIGO 2 submucosal myomas from the surrounding myometrium without activating the current. This blunt cold loop dissection technique allows for a deeper and more thorough resection. Often, if the pseudocapsule plane is identified, even the intramural component of FIGO 1 or FIGO 2 submucosal fibroids can be resected, enabling complete removal.
Lastly, mechanical tissue removal systems are not always faster than resectoscopes for all pathology. We prefer using the resectoscope for larger myomas (>3 cm) as the resectoscope allows for resection and removal of larger myoma chips, helping to decrease operative times. Given the many benefits of the resectoscope, we argue that the resectoscope loop remains a crucial instrument in operative gynecology and that learners should continue to hone their hysteroscopic skills with both the resectoscope and mechanical tissue removal systems.
Tips and tricks for hysteroscopic myomectomy with the resectoscope loop
In the video below, "Bipolar resectoscope: Optimizing safe myomectomy," we review specific surgical techniques for optimizing outcomes and safety with the resectoscope loop. These include:
- bow-and-arrow technique
- identification of the fibroid anatomy (pseudocapsule plane)
- blunt cold loop dissection
- the push-and-tuck method
- efficient electrosurgical hemostasis (TABLE 2).
Although we use bipolar energy during this resection, the resection technique using the monopolar loop is the same.

The takeaway
The resectoscope loop is a valuable tool that offers gynecologic surgeons a wider range of techniques for myomectomy. It also offers several surgical and clinical advantages. It is important to train residents in the use of both hysteroscopic mechanical tissue removal systems and resectoscope loops. ●
Hysteroscopic mechanical morcellators have gained popularity given their ease of use. Consequently, the resectoscope loop is being used less frequently, which has resulted in less familiarity with this device. The resectoscope loop, however, not only is cost effective but also allows for multiple distinct advantages, such as cold loop dissection of myomas and the ability to obtain electrosurgical hemostasis during operative hysteroscopy.
In this article, we review the basics of electrosurgical principles, compare outcomes associated with monopolar and bipolar resectoscopes, and discuss tips and tricks for optimizing surgical techniques when using the resectoscope loop for hysteroscopic myomectomy.
Evolution of hysteroscopy
The term hysteroscopy comes from the Greek words hystera, for uterus, and skopeo, meaning “to see.” The idea to investigate the uterus dates back to the year 1000 when physicians used a mirror with light to peer into the vaginal vault.
The first known successful hysteroscopy occurred in 1869 when Pantaleoni used an endoscope with a light source to identify uterine polyps in a 60-year-old woman with abnormal uterine bleeding. In 1898, Simon Duplay and Spiro Clado published the first textbook on hysteroscopy in which they described several models of hysteroscopic instruments and techniques.
In the 1950s, Harold Horace Hopkins and Karl Storz modified the shape and length of lenses within the endoscope by substituting longer cylindrical lenses for the old spherical lenses; this permitted improved image brightness and sharpness as well as a smaller diameter of the hysteroscope. Between the 1970s and 1980s, technological improvements allowed for the creation of practical and usable hysteroscopic instruments such as the resectoscope. The resectoscope, originally used in urology for transurethral resection of the prostate, was modified for hysteroscopy by incorporating the use of electrosurgical currents to aid in procedures.
Over the past few decades, continued refinements in technology have improved visualization and surgical techniques. For example, image clarity has been markedly improved, and narrow hysteroscope diameters, as small as 3 to 5 mm, require minimal to no cervical dilation.
Monopolar and bipolar resectoscopes
Electrosurgery is the application of an alternating electrical current to tissue to achieve the clinical effects of surgical cutting or hemostasis via cell vaporization or coagulation. Current runs from the electrosurgical unit (ESU) to the active electrode of the surgical instrument, then goes from the active electrode through the patient’s tissue to the return electrode, and then travels back to the ESU. This flow of current creates an electrical circuit (FIGURE).
All electrosurgical devices have an active and a return electrode. The difference between monopolar and bipolar resectoscope devices lies in how the resectoscope loop is constructed. Bipolar resectoscope loops house the active and return electrodes on the same tip of the surgical device, which limits how much of the current flows through the patient. Alternatively, monopolar resectoscopes have only the active electrode on the tip of the device and the return electrode is off the surgical field, so the current flows through more of the patient. On monopolar electrosurgical devices, the current runs from the ESU to the active electrode (monopolar loop), which is then applied to tissue to produce the desired tissue effect. The current then travels via a path of least resistance from the surgical field through the patient to the return electrode, which is usually placed on the patient’s thigh, and then back to the ESU. The return electrode is often referred to as the grounding pad.
Continue to: How monopolar energy works...
How monopolar energy works
When first developed, all resectoscopes used monopolar energy. As such, throughout the 1990s, the monopolar resectoscope was the gold standard for performing electrosurgical hysteroscopy. Because the current travels a long distance between the active and the return electrode in a monopolar setup, a hypotonic, nonelectrolyte-rich medium (a poor conductor), such as glycine 1.5%, mannitol 5%, or sorbitol 3%, must be used. If an electrolyte-rich medium, such as normal saline, is used with a monopolar device, the current would be dispersed throughout the medium outside the operative field, causing unwanted tissue effects.
Although nonelectrolyte distension media improve visibility when encountering bleeding, they can be associated with hyponatremia, hyperglycemia, and even lifethreatening cerebral edema. Furthermore, glycine use is contraindicated in patients with renal or hepatic failure since oxidative deamination may cause hyperammonemia. Because of these numerous risk factors, the fluid deficit for hypotonic, nonelectrolyte distension media is limited to 1,000 mL, with a suggested maximum fluid deficit of 750 mL for elderly or fragile patients. Additionally, because the return electrode is off the surgical field in monopolar surgery, there is a risk of current diversion to the cervix, vagina, or vulva because the current travels between the active electrode on the surgical field to the return electrode on the patient’s thigh. The risk of current diversion is greater if there is damage to electrode insulation, loss of contact between the external sheath and the cervix, or direct coupling between the electrode and the surrounding tissue.
Advantages of the bipolar resectoscope
Because of the potential risks associated with the monopolar resectoscope, over the past 25 years the bipolar resectoscope emerged as an alternative due to its numerous benefits (TABLE 1).
Unlike monopolar resectoscopes, bipolar resectoscopes require an electrolyte-rich distension medium such as 0.9% normal saline or lactated Ringer’s. These isotonic distension media allow a much higher fluid deficit (2,500 mL for healthy patients, 1,500 mL for elderly patients or patients with comorbidities) as the isotonic solution is safer to use. Furthermore, it allows for lower voltage settings and decreased electrical spread compared to the monopolar resectoscope since the current stays between the 2 electrodes. Because isotonic media are miscible with blood, however, a potential drawback is that in cases with bleeding, visibility may be more limited compared to hypotonic distension media.
Evidence on fertility outcomes
Several studies have compared operative and fertility outcomes with the use of monopolar versus bipolar hysteroscopy.
In a randomized controlled trial (RCT) comparing outcomes after hysteroscopy with a monopolar (glycine 1.5%) versus bipolar (0.9% normal saline) 26 French resectoscope loop, Berg and colleagues found that the only significant difference between the 2 groups was that the change in serum sodium pre and postoperatively was greater in the monopolar group despite having a smaller mean fluid deficit (765 mL vs 1,227 mL).1
Similarly, in a study of fertility outcomes after monopolar versus bipolar hysteroscopic myomectomy with use of a 26 French resectoscope Collins knife, Roy and colleagues found no significant differences in postoperative pregnancy rates or successful pregnancy outcomes, operative time, fluid deficit, or improvement in menstrual symptoms.2 However, the monopolar group had a much higher incidence of postoperative hyponatremia (30% vs 0%) that required additional days of hospitalization despite similar fluid deficits of between 600 and 700 mL.2
Similar findings were noted in another RCT that compared operative outcomes between monopolar and bipolar resectoscope usage during metroplasty for infertility, with a postoperative hyponatremia incidence of 17.1% in the monopolar group versus 0% in the bipolar group despite similar fluid deficits.3 Energy type had no effect on reproductive outcomes in either group.3
Continue to: How does the resectoscope compare with mechanical tissue removal systems?...
How does the resectoscope compare with mechanical tissue removal systems?
In 2005, the first hysteroscopic mechanical tissue removal system was introduced in the United States, providing an additional treatment method for such intrauterine masses as fibroids and polyps.
Advantages. Rather than using an electrical current, these tissue removal systems use a rotating blade with suction that is introduced through a specially designed rigid hysteroscopic sheath. As the instrument incises the pathology, the tissue is removed from the intrauterine cavity and collected in a specimen bag inside the fluid management system. This immediate removal of tissue allows for insertion of the device only once during initial entry, decreasing both the risk of perforation and operative times. Furthermore, mechanical tissue removal systems can be used with isotonic media, negating the risks associated with hypotonic media. Currently, the 2 mechanical tissue removal systems available in the United States are the TruClear and the MyoSure hysteroscopic tissue removal systems.
Studies comparing mechanical tissue removal of polyps and myomas with conventional resectoscope resection have found that mechanical tissue removal is associated with reduced operative time, fluid deficit, and number of instrument insertions.4-8 However, studies have found no significant difference in postoperative patient satisfaction.7,9
Additionally, hysteroscopic tissue removal systems have an easier learning curve. Van Dongen and colleagues conducted an RCT to compare resident-in-training comfort levels when learning to use both a mechanical tissue removal system and a traditional resectoscope; they found increased comfort with the hysteroscopic tissue removal system, suggesting greater ease of use.10
Drawbacks. Despite their many benefits, mechanical tissue removal systems have some disadvantages when compared with the resectoscope. First, mechanical tissue removal systems are associated with higher instrument costs. In addition, they have extremely limited ability to achieve hemostasis when encountering blood vessels during resection, resulting in poor visibility especially when resecting large myomas with feeding vessels.
Hysteroscopic mechanical tissue removal systems typically use higher intrauterine pressures for uterine distension compared with the resectoscope, especially when trying to improve visibility in a bloody surgical field. Increasing the intrauterine pressure with the distension media allows for compression of the blood vessels. As a result, however, submucosal fibroids classified as FIGO 2 (International Federation of Gynecology and Obstetrics) may be less visible since the higher intrauterine pressure can compress both blood vessels and submucosal fibroids
Additionally, mechanical tissue removal systems have limited ability to resect the intramural component of FIGO 1 or FIGO 2 submucosal fibroids since the intramural portion is embedded in the myometrium. Use of the resectoscope loop instead allows for a technique called the cold loop dissection, which uses the resectoscope loop to bluntly dissect and enucleate the intramural component of FIGO 1 and FIGO 2 submucosal myomas from the surrounding myometrium without activating the current. This blunt cold loop dissection technique allows for a deeper and more thorough resection. Often, if the pseudocapsule plane is identified, even the intramural component of FIGO 1 or FIGO 2 submucosal fibroids can be resected, enabling complete removal.
Lastly, mechanical tissue removal systems are not always faster than resectoscopes for all pathology. We prefer using the resectoscope for larger myomas (>3 cm) as the resectoscope allows for resection and removal of larger myoma chips, helping to decrease operative times. Given the many benefits of the resectoscope, we argue that the resectoscope loop remains a crucial instrument in operative gynecology and that learners should continue to hone their hysteroscopic skills with both the resectoscope and mechanical tissue removal systems.
Tips and tricks for hysteroscopic myomectomy with the resectoscope loop
In the video below, "Bipolar resectoscope: Optimizing safe myomectomy," we review specific surgical techniques for optimizing outcomes and safety with the resectoscope loop. These include:
- bow-and-arrow technique
- identification of the fibroid anatomy (pseudocapsule plane)
- blunt cold loop dissection
- the push-and-tuck method
- efficient electrosurgical hemostasis (TABLE 2).
Although we use bipolar energy during this resection, the resection technique using the monopolar loop is the same.

The takeaway
The resectoscope loop is a valuable tool that offers gynecologic surgeons a wider range of techniques for myomectomy. It also offers several surgical and clinical advantages. It is important to train residents in the use of both hysteroscopic mechanical tissue removal systems and resectoscope loops. ●
- Berg A, Sandvik L, Langebrekke A, et al. A randomized trial comparing monopolar electrodes using glycine 1.5% with two different types of bipolar electrodes (TCRis, Versapoint) using saline, in hysteroscopic surgery. Fertil Steril. 2009;91:1273- 1278.
- Roy KK, Metta S, Kansal Y, et al. A prospective randomized study comparing unipolar versus bipolar hysteroscopic myomectomy in infertile women. J Hum Reprod Sci. 2017;10:185-193.
- Roy KK, Kansal Y, Subbaiah M, et al. Hysteroscopic septal resection using unipolar resectoscope versus bipolar resectoscope: prospective, randomized study. J Obstet Gynaecol Res. 2015;41:952-956.
- Borg MH, Shehata A. Uterine morcellator versus resectoscopy in the management of heavy menstrual flow in reproductiveage women. J Gyn Res. 2016;2:1-8.
- Emanuel MH, Wamsteker K. The intra uterine morcellator: a new hysteroscopic operating technique to remove intrauterine polyps and myomas. J Minim Invasive Gynecol. 2005;12:62-66.
- Smith PP, Middleton LJ, Connor M, et al. Hysteroscopic morcellation compared with electrical resection of endometrial polyps: a randomized controlled trial. Obstet Gynecol. 2014;123:745-751.
- Vitale SG, Sapia F, Rapisarda AMC, et al. Hysteroscopic morcellation of submucous myomas: a systematic review. Biomed Res Int. 2017;2017:6848250.
- Stoll F, Lecointre L, Meyer N, et al. Randomized study comparing a reusable morcellator with a resectoscope in the hysteroscopic treatment of uterine polyps: the RESMO study. J Minimal Invasive Gyn. 2021;28:801-810.
- Lee MM, Matsuzono T. Hysteroscopic intrauterine morcellation of submucosal fibroids: preliminary results in Hong Kong and comparisons with conventional hysteroscopic monopolar loop resection. Hong Kong Med J. 2016;22:56-61.
- van Dongen H, Emanuel MH, Wolterbeek R, et al. Hysteroscopic morcellator for removal of intrauterine polyps and myomas: a randomized controlled pilot study among residents in training. J Minim Invasive Gynecol. 2008;15:466-471.
- Berg A, Sandvik L, Langebrekke A, et al. A randomized trial comparing monopolar electrodes using glycine 1.5% with two different types of bipolar electrodes (TCRis, Versapoint) using saline, in hysteroscopic surgery. Fertil Steril. 2009;91:1273- 1278.
- Roy KK, Metta S, Kansal Y, et al. A prospective randomized study comparing unipolar versus bipolar hysteroscopic myomectomy in infertile women. J Hum Reprod Sci. 2017;10:185-193.
- Roy KK, Kansal Y, Subbaiah M, et al. Hysteroscopic septal resection using unipolar resectoscope versus bipolar resectoscope: prospective, randomized study. J Obstet Gynaecol Res. 2015;41:952-956.
- Borg MH, Shehata A. Uterine morcellator versus resectoscopy in the management of heavy menstrual flow in reproductiveage women. J Gyn Res. 2016;2:1-8.
- Emanuel MH, Wamsteker K. The intra uterine morcellator: a new hysteroscopic operating technique to remove intrauterine polyps and myomas. J Minim Invasive Gynecol. 2005;12:62-66.
- Smith PP, Middleton LJ, Connor M, et al. Hysteroscopic morcellation compared with electrical resection of endometrial polyps: a randomized controlled trial. Obstet Gynecol. 2014;123:745-751.
- Vitale SG, Sapia F, Rapisarda AMC, et al. Hysteroscopic morcellation of submucous myomas: a systematic review. Biomed Res Int. 2017;2017:6848250.
- Stoll F, Lecointre L, Meyer N, et al. Randomized study comparing a reusable morcellator with a resectoscope in the hysteroscopic treatment of uterine polyps: the RESMO study. J Minimal Invasive Gyn. 2021;28:801-810.
- Lee MM, Matsuzono T. Hysteroscopic intrauterine morcellation of submucosal fibroids: preliminary results in Hong Kong and comparisons with conventional hysteroscopic monopolar loop resection. Hong Kong Med J. 2016;22:56-61.
- van Dongen H, Emanuel MH, Wolterbeek R, et al. Hysteroscopic morcellator for removal of intrauterine polyps and myomas: a randomized controlled pilot study among residents in training. J Minim Invasive Gynecol. 2008;15:466-471.