User login
From Musgrove Park Hospital, Taunton, England.
Abstract
- Objective: To describe a redesign of the clinical pathway for patients undergoing elective spinal surgery in order to improve quality of care and reduce length of stay.
- Methods: A multidisciplinary team undertook a process-mapping exercise and shadowed patients to analyse problems with the existing clinical pathway. Further ideas were taken from best evidence and other published enhanced recovery programs. Change ideas were tested using Plan-Do-Study-Act cycles. Measures included length of hospital stay, compliance with the pathway, and patient satisfaction.
- Results: The new pathway, the SpinaL Enhanced Recovery Program, is now used by 99% of elective spinal surgery patients with 100% of patients rating their care as good or excellent. Length of stay was reduced by 52%, improving from 5.7 days at the start of the intervention to 2.7 days. The pathway improved reliability of care, with preoperative carbohydrate drinks used in 83% of patients.
- Conclusion: The pathway improved reliability of care in our institution with excellent patient satisfaction and a significant reduction in length of hospital stay.
Enhanced recovery programs (ERPs) have been developed in many surgical specialties to improve patient outcomes and recovery after elective surgery. They involve multiple interventions throughout the patient journey, from preoperative patient education to postoperative mobilization and analgesia schedules. A meta-analysis of 38 trials involving 5099 participants showed ERPs could reduce length of stay and overall complication rates across surgical specialties [1].
There have been few studies of ERP for spinal surgery populations [2]. Most of them have studied selected patients or selected interventions such as analgesia schedules and did not use quality improvement methodology. For example, a small retrospective study compared patients undergoing multilevel spinal fusion surgery before and after introduction of a multimodal analgesia regimen [3]. A review of innovative perioperative and intraoperative treatment algorithms showed that they can influence postoperative recovery and patient outcomes from lumbar spinal surgery [4]. A study from the same group found that patient education and a “fast-track” pathway reduced length of hospital stay and improved patient satisfaction for patients undergoing 1- or 2- level lumbar spinal fusion [5].
At our hospital, a meeting of the clinicians and staff involved in elective spinal surgery was held to discuss the service. Leadership came from a consultant anesthesiologist and a consultant spinal surgeon, who recognized that care was not as efficient as it could be. A multidisciplinary team was formed consisting of 30 members, including surgeons, clinical nurse practitioners, physiotherapists, occupational therapists, and secretarial staff. The team undertook a process-mapping exercise that revealed that patients followed an ill-defined care pathway with variability in administrative processes and clinical care. Patient feedback and reports from both secretarial and community staff revealed that communications from the spinal team could be inconsistent, and patients had unclear expectations of their care and recovery. Lengths of stay for the same procedure could vary by 3 days.
With support from the hospital’s chief executive and medical director, the team embarked on a process to redesign the clinical pathway for patients undergoing elective spinal surgery at our hospital. We developed the SpinaL Enhanced Recovery Program; our primary aims were to to have 95% of patients managed according to the new pathway, to reduce length of stay by 30% without a rise in readmission rates, and to improve patient satisfaction.
Methods
Ethical Issues
This work met criteria for operational improvement activities and as such was exempt from ethics review. The team engaged patients who had undergone spinal surgery to serve as representatives to ensure that the improvements studied were important to them.
Setting and Patients
Our institution is a District General Hospital that serves a population of over 340,000 and has 3 consultant spinal surgeons. They work with 5 anesthesiologists on a regular basis and the patients are cared for by 3 clinical nurse practitioners. The patients are cared for on an elective orthopedic ward with nursing staff, physiotherapists, and occupational therapists who work regularly with spinal surgery patients. The mean age of our spinal surgery patients is 55 years and 55% are female. By age-group, 6.6% are aged 1–16 years, 50.8% aged 17–65 years, and 42.6% over 65 years. We define elective spinal surgery as non-emergency surgery, including discectomy, decompression, fusion and realignment operations to the cervical, thoracic and lumbar spine.
Developing the Pathway
To develop the new pathway, input from the expert team of anesthesiologists and surgeons, other clinicians and staff, as well as patients were sought. Four patients were approached prior to surgery and asked for their thoughts on the existing clinical pathway. They were then shadowed during their journey by clinical staff to see where improvements to their clinical care could be made.
In addition to gathering input from staff and patients, we reviewed the literature for the best available evidence. We found a Cochrane review of 27 trials involving 1976 surgical patients that concluded that preoperative carbohydrate drinks reduced length of stay [6]. Similarly, although laxatives have not been shown to improve length of stay [7], it is known that constipation is exacerbated by opioid analgesia and causes distress [8].
Finally, we examined the ERPs for patients undergoing hip and knee replacement that already existed in our institution. We found they used standardized anesthetic regimens as well as “patient passports,” leaflets given to give patients telling them what to expect during and following joint replacement surgery. They were also implementing methods to help patients set daily aims on the ward.
PDSA Cycles
We began PDSA testing in November 2013. Below we describe selected pathway changes that we expected to be challenging because they involved many staff from different groups. Interventions that involved fewer people or a smaller group (eg, a change in anesthetic regimen or surgical technique) were easier to implement.
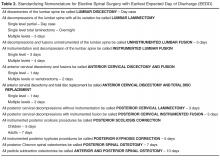
Standardizing Nomenclature
The spinal consultants agreed to 12 descriptions of elective spinal surgery to improve communication between team members (Table 2). They were able to reduce the number of procedure descriptions from 135 to just 12. Theatre staff could determine from the procedure descriptions which equipment was required for the operation and ensure it was available at the time needed. Anesthetic staff felt better able to prepare for their operating lists with a prescription for preoperative, intraoperative, and postoperative analgesia.
They also defined an earliest expected day of discharge (EEDD) (Table 2), which was distributed to all members of the team. This information helped ward nurses and therapists were better able to plan to mobilize patients appropriately postoperatively and ensure consistency in communication of expected length of stay to patients.
Perioperative Laxatives
Laxatives were prescribed initially for one patient and we checked to see if the patient and nursing staff were happy with the change. In the next test cycle all patients on one consultant’s list were prescribed laxatives. To track laxative use, a data collection sheet was attached to the patient's medical records on admission. With improved data collection, laxatives were then prescribed on admission for all elective spinal patients. The process has now become routine, occurring even when key change agents are absent.
Preoperative Carbohydrate Drinks
Preoperative high-calorie drinks were initially prescribed for one surgeon’s patients who were predicted to be staying 2 or more nights in the hospital. The preoperative assessment clinic (POAC) staff were asked to give these patients preoperative carbohydrate drinks at their pre-assessment clinic, and patients would self-administer their carbohydrate drinks preoperatively. However, POAC staff found it too difficult to give drinks to some patients and not to others, so it was decided that all patients should receive a drink. The clinical nurse practitioners note that the drink is given on the data collection sheet. However, it was observed that when team champions did not remind staff to administer the preoperative carbohydrate drinks, they were not given. We then asked the surgical admissions lounge staff if they would give preoperative carbohydrate drinks to patients and they agreed. This worked better than using POAC staff.
Patient Daily Aims
Members of the team felt that setting daily aims with patients would help optimize and prepare them for discharge. A laminated sheet with handwritten aims was trialed with 1 patient. He found it very useful, particularly the aims on diet and mobilization. When tested on all patients for a week, not only did they find it useful but nursing staff felt it improved communication between shifts. With greater staff buy-in and a move into a new purpose-built ward, we used white boards that were affixed to the door to the ensuite bathroom in each single patient room. Aims were discussed on ward rounds with patients by consultants or clinical nurse practitioners, and the goals agreed upon with patients before being written on the white boards. They included goals such as removal of urinary catheters, mobilization independently or with staff, and requirements such as radiographs to check position of instrumentation. Spot-checks on the ward showed good compliance with setting daily aims and high rates of satisfaction from patients.
Hospital at Home
The Hospital at Home team consists of experienced community-based nurses who provide wound care and analgesia advice for selected patients postdischarge to prevent readmission. This team supported early discharge for patients undergoing hip and knee replacements, and when approached they felt they could offer wound care and analgesia advice in the community for spinal surgery patients. This was tested with one patient with a wound who had daily care at home for 8 days following discharge from hospital. A further 2 patients were later cared for by the Hospital at Home team, with a total of 7 bed days saved. It has now become routine for the team to accept spinal patients when they have the capacity.
Outcomes
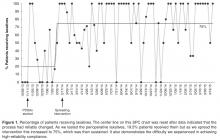
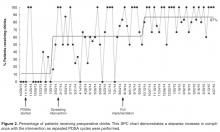
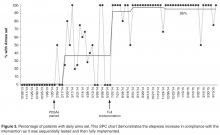
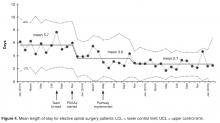
Working with the IT department and data collection tools attached to the medical records, we collected data on key measures every 2 weeks. Statistical process control charts (Process Improvement Products, Austin, TX) [9,10] were used to analyze the data.
Length of stay was reduced by 52% (Figure 4), improving from an average of 6 days during the baseline period to 2.9 days by April 2015. Readmissions for elective spinal surgery patients did not increase and in fact were reduced from 7% to 3%.
By October 2014, 99% of eligible patients were managed on the new pathway and most patients were receiving key
Discussion
The new pathway, the SpinaL Enhanced Recovery Program, improved reliability of care in our institution, with excellent patient satisfaction. It also exceeded its target in reducing length of stay for elective spinal surgery patients
One of the main strengths of this work was the use of small scale testing for each change idea using PDSA cycles, ramping up the idea prior to full implementation. The team could see the impact of changes on a small scale, then make adaptations in the next cycle to increase the likelihood of success.
The development and implementation of the pathway has led to a positive culture change. The spinal team has taken ownership of the pathway and continues to monitor its impact. Seeing the impact of their work on improving the quality of patient care has enhanced the team’s self-efficacy.
The methods used to plan and study our interventions, as well as some of the change ideas themselves, may be helpful for other elective spinal surgical teams. The simple application of the interventions without the improvement process may not have delivered the same outcome. Meeting regularly as a team to discuss ideas and implement new interventions with the guidance of a quality improvement advisor (M.W.) was felt to be the most important factor for success. The team also felt that it was important to collect data by any means possible to monitor interventions and motivate staff before better automated systems were implemented.
The SpinaL Enhanced Recovery Program pathway has now become “business as usual,” and the team plans to incorporate the process and outcome measures onto a monthly performance dashboard to continue to monitor the interventions. Further interventions are planned, including improving preoperative education with a patient pathway video. The team has started to try to stagger admissions for all-day theatre lists, to avoid patients having to wait all day for an afternoon operation. Further improvements in the reliability of care will also potentially allow the team to run controlled studies of single interventions to see how these can impact quality of patient care in a stable process.
Acknowledgments: The authors acknowledge Deborah Ray, Institute for Healthcare Improvement; Sandra Murray, Associates in Healthcare Improvement; Matthew Beebee, Clinical Nurse Practitioner Spinal Surgery; Debbie Vile and Lorraine Sandford, Clinical Nurse Practitioners Spinal Surgery; Sophie Hudson and Sallie Durman, Secretaries; Eleanor Palfreman, Occupational Therapist; Sarah Woodhill, Physiotherapist; Lee Scott, Improvement Nurse; Gervaise Khan-Davis, Directorate Manager; and “SG,” previous patient.
Corresponding author: Dr Julia Blackburn, Musgrove Park Hospital, Taunton, England, TA1 5DA, jlrkblackburn@doctors.org.uk.
Financial disclosures: None.
1. Nicholson A, Lowe MC, Parker J, et al. Systematic review and meta-analysis of enhanced recovery programmes in surgical patients. Br J Surg 2014;101:172–88.
2. Venkata H, Van Dellen J. A perspective on the use of an Enhanced Recovery Programme in open, non-instrumented, ‘day-surgery’ for degenerative lumbar and cervical spinal conditions. J Neurosurg Sci 2016.
3. Mathiesen O, Dahl B, Thomsen B, et al. A comprehensive multimodal pain treatment reduces opioid consumption after multilevel spine surgery. Eur Spine J 2013;22:2089–96.
4. Fleege C, Almajali A, Rauschmann M, et al. Improve of surgical outcome in spinal fusion surgery. Evidence based peri- and intra-operative aspects to reduce complications and earlier recovery. Der Orthopade 2014;43:1070–8.
5. Fleege C, Arabmotlagh M, Almajali A, et al. Pre- and postoperative fast-track treatment concepts in spinal surgery. Patient information and patient cooperation. Der Orthopade 2014;43:1062.
6. Smith MD, McCall J, Plank L, et al. Preoperative carbohydrate treatment for enhancing recovery after elective surgery. Cochrane Database Syst Rev 2014;8:CD009161.
7. Hendry PO, van Dam RM, Bukkems SF, et al. Randomized clinical trial of laxatives and oral nutritional supplements within an enhanced recovery after surgery protocol following liver resection. Br J Surg 2010;97:1198–206.
8. Marciniak CM, Toledo S, Lee J, et al. Lubiprostone vs senna in postoperative orthopedic surgery patients with opioid-induced constipation: a double-blind, active-comparator trial. World J Gastroenterol 2014;20:16323–33.
9. Benneyan J, Lloyd R, Plsek P. Statistical process control as a tool for research and healthcare improvement. Qual Safety Health Care 2003;12:458–64.
10. Portela MC, Pronovost PJ, Woodcock T, et al. How to study improvement interventions: a brief overview of possible study types. BMJ Qual Safety 2015;24:325–36.
From Musgrove Park Hospital, Taunton, England.
Abstract
- Objective: To describe a redesign of the clinical pathway for patients undergoing elective spinal surgery in order to improve quality of care and reduce length of stay.
- Methods: A multidisciplinary team undertook a process-mapping exercise and shadowed patients to analyse problems with the existing clinical pathway. Further ideas were taken from best evidence and other published enhanced recovery programs. Change ideas were tested using Plan-Do-Study-Act cycles. Measures included length of hospital stay, compliance with the pathway, and patient satisfaction.
- Results: The new pathway, the SpinaL Enhanced Recovery Program, is now used by 99% of elective spinal surgery patients with 100% of patients rating their care as good or excellent. Length of stay was reduced by 52%, improving from 5.7 days at the start of the intervention to 2.7 days. The pathway improved reliability of care, with preoperative carbohydrate drinks used in 83% of patients.
- Conclusion: The pathway improved reliability of care in our institution with excellent patient satisfaction and a significant reduction in length of hospital stay.
Enhanced recovery programs (ERPs) have been developed in many surgical specialties to improve patient outcomes and recovery after elective surgery. They involve multiple interventions throughout the patient journey, from preoperative patient education to postoperative mobilization and analgesia schedules. A meta-analysis of 38 trials involving 5099 participants showed ERPs could reduce length of stay and overall complication rates across surgical specialties [1].
There have been few studies of ERP for spinal surgery populations [2]. Most of them have studied selected patients or selected interventions such as analgesia schedules and did not use quality improvement methodology. For example, a small retrospective study compared patients undergoing multilevel spinal fusion surgery before and after introduction of a multimodal analgesia regimen [3]. A review of innovative perioperative and intraoperative treatment algorithms showed that they can influence postoperative recovery and patient outcomes from lumbar spinal surgery [4]. A study from the same group found that patient education and a “fast-track” pathway reduced length of hospital stay and improved patient satisfaction for patients undergoing 1- or 2- level lumbar spinal fusion [5].
At our hospital, a meeting of the clinicians and staff involved in elective spinal surgery was held to discuss the service. Leadership came from a consultant anesthesiologist and a consultant spinal surgeon, who recognized that care was not as efficient as it could be. A multidisciplinary team was formed consisting of 30 members, including surgeons, clinical nurse practitioners, physiotherapists, occupational therapists, and secretarial staff. The team undertook a process-mapping exercise that revealed that patients followed an ill-defined care pathway with variability in administrative processes and clinical care. Patient feedback and reports from both secretarial and community staff revealed that communications from the spinal team could be inconsistent, and patients had unclear expectations of their care and recovery. Lengths of stay for the same procedure could vary by 3 days.
With support from the hospital’s chief executive and medical director, the team embarked on a process to redesign the clinical pathway for patients undergoing elective spinal surgery at our hospital. We developed the SpinaL Enhanced Recovery Program; our primary aims were to to have 95% of patients managed according to the new pathway, to reduce length of stay by 30% without a rise in readmission rates, and to improve patient satisfaction.
Methods
Ethical Issues
This work met criteria for operational improvement activities and as such was exempt from ethics review. The team engaged patients who had undergone spinal surgery to serve as representatives to ensure that the improvements studied were important to them.
Setting and Patients
Our institution is a District General Hospital that serves a population of over 340,000 and has 3 consultant spinal surgeons. They work with 5 anesthesiologists on a regular basis and the patients are cared for by 3 clinical nurse practitioners. The patients are cared for on an elective orthopedic ward with nursing staff, physiotherapists, and occupational therapists who work regularly with spinal surgery patients. The mean age of our spinal surgery patients is 55 years and 55% are female. By age-group, 6.6% are aged 1–16 years, 50.8% aged 17–65 years, and 42.6% over 65 years. We define elective spinal surgery as non-emergency surgery, including discectomy, decompression, fusion and realignment operations to the cervical, thoracic and lumbar spine.
Developing the Pathway
To develop the new pathway, input from the expert team of anesthesiologists and surgeons, other clinicians and staff, as well as patients were sought. Four patients were approached prior to surgery and asked for their thoughts on the existing clinical pathway. They were then shadowed during their journey by clinical staff to see where improvements to their clinical care could be made.
In addition to gathering input from staff and patients, we reviewed the literature for the best available evidence. We found a Cochrane review of 27 trials involving 1976 surgical patients that concluded that preoperative carbohydrate drinks reduced length of stay [6]. Similarly, although laxatives have not been shown to improve length of stay [7], it is known that constipation is exacerbated by opioid analgesia and causes distress [8].
Finally, we examined the ERPs for patients undergoing hip and knee replacement that already existed in our institution. We found they used standardized anesthetic regimens as well as “patient passports,” leaflets given to give patients telling them what to expect during and following joint replacement surgery. They were also implementing methods to help patients set daily aims on the ward.
PDSA Cycles
We began PDSA testing in November 2013. Below we describe selected pathway changes that we expected to be challenging because they involved many staff from different groups. Interventions that involved fewer people or a smaller group (eg, a change in anesthetic regimen or surgical technique) were easier to implement.
Standardizing Nomenclature
The spinal consultants agreed to 12 descriptions of elective spinal surgery to improve communication between team members (Table 2). They were able to reduce the number of procedure descriptions from 135 to just 12. Theatre staff could determine from the procedure descriptions which equipment was required for the operation and ensure it was available at the time needed. Anesthetic staff felt better able to prepare for their operating lists with a prescription for preoperative, intraoperative, and postoperative analgesia.
They also defined an earliest expected day of discharge (EEDD) (Table 2), which was distributed to all members of the team. This information helped ward nurses and therapists were better able to plan to mobilize patients appropriately postoperatively and ensure consistency in communication of expected length of stay to patients.
Perioperative Laxatives
Laxatives were prescribed initially for one patient and we checked to see if the patient and nursing staff were happy with the change. In the next test cycle all patients on one consultant’s list were prescribed laxatives. To track laxative use, a data collection sheet was attached to the patient's medical records on admission. With improved data collection, laxatives were then prescribed on admission for all elective spinal patients. The process has now become routine, occurring even when key change agents are absent.
Preoperative Carbohydrate Drinks
Preoperative high-calorie drinks were initially prescribed for one surgeon’s patients who were predicted to be staying 2 or more nights in the hospital. The preoperative assessment clinic (POAC) staff were asked to give these patients preoperative carbohydrate drinks at their pre-assessment clinic, and patients would self-administer their carbohydrate drinks preoperatively. However, POAC staff found it too difficult to give drinks to some patients and not to others, so it was decided that all patients should receive a drink. The clinical nurse practitioners note that the drink is given on the data collection sheet. However, it was observed that when team champions did not remind staff to administer the preoperative carbohydrate drinks, they were not given. We then asked the surgical admissions lounge staff if they would give preoperative carbohydrate drinks to patients and they agreed. This worked better than using POAC staff.
Patient Daily Aims
Members of the team felt that setting daily aims with patients would help optimize and prepare them for discharge. A laminated sheet with handwritten aims was trialed with 1 patient. He found it very useful, particularly the aims on diet and mobilization. When tested on all patients for a week, not only did they find it useful but nursing staff felt it improved communication between shifts. With greater staff buy-in and a move into a new purpose-built ward, we used white boards that were affixed to the door to the ensuite bathroom in each single patient room. Aims were discussed on ward rounds with patients by consultants or clinical nurse practitioners, and the goals agreed upon with patients before being written on the white boards. They included goals such as removal of urinary catheters, mobilization independently or with staff, and requirements such as radiographs to check position of instrumentation. Spot-checks on the ward showed good compliance with setting daily aims and high rates of satisfaction from patients.
Hospital at Home
The Hospital at Home team consists of experienced community-based nurses who provide wound care and analgesia advice for selected patients postdischarge to prevent readmission. This team supported early discharge for patients undergoing hip and knee replacements, and when approached they felt they could offer wound care and analgesia advice in the community for spinal surgery patients. This was tested with one patient with a wound who had daily care at home for 8 days following discharge from hospital. A further 2 patients were later cared for by the Hospital at Home team, with a total of 7 bed days saved. It has now become routine for the team to accept spinal patients when they have the capacity.
Outcomes
Working with the IT department and data collection tools attached to the medical records, we collected data on key measures every 2 weeks. Statistical process control charts (Process Improvement Products, Austin, TX) [9,10] were used to analyze the data.
Length of stay was reduced by 52% (Figure 4), improving from an average of 6 days during the baseline period to 2.9 days by April 2015. Readmissions for elective spinal surgery patients did not increase and in fact were reduced from 7% to 3%.
By October 2014, 99% of eligible patients were managed on the new pathway and most patients were receiving key
Discussion
The new pathway, the SpinaL Enhanced Recovery Program, improved reliability of care in our institution, with excellent patient satisfaction. It also exceeded its target in reducing length of stay for elective spinal surgery patients
One of the main strengths of this work was the use of small scale testing for each change idea using PDSA cycles, ramping up the idea prior to full implementation. The team could see the impact of changes on a small scale, then make adaptations in the next cycle to increase the likelihood of success.
The development and implementation of the pathway has led to a positive culture change. The spinal team has taken ownership of the pathway and continues to monitor its impact. Seeing the impact of their work on improving the quality of patient care has enhanced the team’s self-efficacy.
The methods used to plan and study our interventions, as well as some of the change ideas themselves, may be helpful for other elective spinal surgical teams. The simple application of the interventions without the improvement process may not have delivered the same outcome. Meeting regularly as a team to discuss ideas and implement new interventions with the guidance of a quality improvement advisor (M.W.) was felt to be the most important factor for success. The team also felt that it was important to collect data by any means possible to monitor interventions and motivate staff before better automated systems were implemented.
The SpinaL Enhanced Recovery Program pathway has now become “business as usual,” and the team plans to incorporate the process and outcome measures onto a monthly performance dashboard to continue to monitor the interventions. Further interventions are planned, including improving preoperative education with a patient pathway video. The team has started to try to stagger admissions for all-day theatre lists, to avoid patients having to wait all day for an afternoon operation. Further improvements in the reliability of care will also potentially allow the team to run controlled studies of single interventions to see how these can impact quality of patient care in a stable process.
Acknowledgments: The authors acknowledge Deborah Ray, Institute for Healthcare Improvement; Sandra Murray, Associates in Healthcare Improvement; Matthew Beebee, Clinical Nurse Practitioner Spinal Surgery; Debbie Vile and Lorraine Sandford, Clinical Nurse Practitioners Spinal Surgery; Sophie Hudson and Sallie Durman, Secretaries; Eleanor Palfreman, Occupational Therapist; Sarah Woodhill, Physiotherapist; Lee Scott, Improvement Nurse; Gervaise Khan-Davis, Directorate Manager; and “SG,” previous patient.
Corresponding author: Dr Julia Blackburn, Musgrove Park Hospital, Taunton, England, TA1 5DA, jlrkblackburn@doctors.org.uk.
Financial disclosures: None.
From Musgrove Park Hospital, Taunton, England.
Abstract
- Objective: To describe a redesign of the clinical pathway for patients undergoing elective spinal surgery in order to improve quality of care and reduce length of stay.
- Methods: A multidisciplinary team undertook a process-mapping exercise and shadowed patients to analyse problems with the existing clinical pathway. Further ideas were taken from best evidence and other published enhanced recovery programs. Change ideas were tested using Plan-Do-Study-Act cycles. Measures included length of hospital stay, compliance with the pathway, and patient satisfaction.
- Results: The new pathway, the SpinaL Enhanced Recovery Program, is now used by 99% of elective spinal surgery patients with 100% of patients rating their care as good or excellent. Length of stay was reduced by 52%, improving from 5.7 days at the start of the intervention to 2.7 days. The pathway improved reliability of care, with preoperative carbohydrate drinks used in 83% of patients.
- Conclusion: The pathway improved reliability of care in our institution with excellent patient satisfaction and a significant reduction in length of hospital stay.
Enhanced recovery programs (ERPs) have been developed in many surgical specialties to improve patient outcomes and recovery after elective surgery. They involve multiple interventions throughout the patient journey, from preoperative patient education to postoperative mobilization and analgesia schedules. A meta-analysis of 38 trials involving 5099 participants showed ERPs could reduce length of stay and overall complication rates across surgical specialties [1].
There have been few studies of ERP for spinal surgery populations [2]. Most of them have studied selected patients or selected interventions such as analgesia schedules and did not use quality improvement methodology. For example, a small retrospective study compared patients undergoing multilevel spinal fusion surgery before and after introduction of a multimodal analgesia regimen [3]. A review of innovative perioperative and intraoperative treatment algorithms showed that they can influence postoperative recovery and patient outcomes from lumbar spinal surgery [4]. A study from the same group found that patient education and a “fast-track” pathway reduced length of hospital stay and improved patient satisfaction for patients undergoing 1- or 2- level lumbar spinal fusion [5].
At our hospital, a meeting of the clinicians and staff involved in elective spinal surgery was held to discuss the service. Leadership came from a consultant anesthesiologist and a consultant spinal surgeon, who recognized that care was not as efficient as it could be. A multidisciplinary team was formed consisting of 30 members, including surgeons, clinical nurse practitioners, physiotherapists, occupational therapists, and secretarial staff. The team undertook a process-mapping exercise that revealed that patients followed an ill-defined care pathway with variability in administrative processes and clinical care. Patient feedback and reports from both secretarial and community staff revealed that communications from the spinal team could be inconsistent, and patients had unclear expectations of their care and recovery. Lengths of stay for the same procedure could vary by 3 days.
With support from the hospital’s chief executive and medical director, the team embarked on a process to redesign the clinical pathway for patients undergoing elective spinal surgery at our hospital. We developed the SpinaL Enhanced Recovery Program; our primary aims were to to have 95% of patients managed according to the new pathway, to reduce length of stay by 30% without a rise in readmission rates, and to improve patient satisfaction.
Methods
Ethical Issues
This work met criteria for operational improvement activities and as such was exempt from ethics review. The team engaged patients who had undergone spinal surgery to serve as representatives to ensure that the improvements studied were important to them.
Setting and Patients
Our institution is a District General Hospital that serves a population of over 340,000 and has 3 consultant spinal surgeons. They work with 5 anesthesiologists on a regular basis and the patients are cared for by 3 clinical nurse practitioners. The patients are cared for on an elective orthopedic ward with nursing staff, physiotherapists, and occupational therapists who work regularly with spinal surgery patients. The mean age of our spinal surgery patients is 55 years and 55% are female. By age-group, 6.6% are aged 1–16 years, 50.8% aged 17–65 years, and 42.6% over 65 years. We define elective spinal surgery as non-emergency surgery, including discectomy, decompression, fusion and realignment operations to the cervical, thoracic and lumbar spine.
Developing the Pathway
To develop the new pathway, input from the expert team of anesthesiologists and surgeons, other clinicians and staff, as well as patients were sought. Four patients were approached prior to surgery and asked for their thoughts on the existing clinical pathway. They were then shadowed during their journey by clinical staff to see where improvements to their clinical care could be made.
In addition to gathering input from staff and patients, we reviewed the literature for the best available evidence. We found a Cochrane review of 27 trials involving 1976 surgical patients that concluded that preoperative carbohydrate drinks reduced length of stay [6]. Similarly, although laxatives have not been shown to improve length of stay [7], it is known that constipation is exacerbated by opioid analgesia and causes distress [8].
Finally, we examined the ERPs for patients undergoing hip and knee replacement that already existed in our institution. We found they used standardized anesthetic regimens as well as “patient passports,” leaflets given to give patients telling them what to expect during and following joint replacement surgery. They were also implementing methods to help patients set daily aims on the ward.
PDSA Cycles
We began PDSA testing in November 2013. Below we describe selected pathway changes that we expected to be challenging because they involved many staff from different groups. Interventions that involved fewer people or a smaller group (eg, a change in anesthetic regimen or surgical technique) were easier to implement.
Standardizing Nomenclature
The spinal consultants agreed to 12 descriptions of elective spinal surgery to improve communication between team members (Table 2). They were able to reduce the number of procedure descriptions from 135 to just 12. Theatre staff could determine from the procedure descriptions which equipment was required for the operation and ensure it was available at the time needed. Anesthetic staff felt better able to prepare for their operating lists with a prescription for preoperative, intraoperative, and postoperative analgesia.
They also defined an earliest expected day of discharge (EEDD) (Table 2), which was distributed to all members of the team. This information helped ward nurses and therapists were better able to plan to mobilize patients appropriately postoperatively and ensure consistency in communication of expected length of stay to patients.
Perioperative Laxatives
Laxatives were prescribed initially for one patient and we checked to see if the patient and nursing staff were happy with the change. In the next test cycle all patients on one consultant’s list were prescribed laxatives. To track laxative use, a data collection sheet was attached to the patient's medical records on admission. With improved data collection, laxatives were then prescribed on admission for all elective spinal patients. The process has now become routine, occurring even when key change agents are absent.
Preoperative Carbohydrate Drinks
Preoperative high-calorie drinks were initially prescribed for one surgeon’s patients who were predicted to be staying 2 or more nights in the hospital. The preoperative assessment clinic (POAC) staff were asked to give these patients preoperative carbohydrate drinks at their pre-assessment clinic, and patients would self-administer their carbohydrate drinks preoperatively. However, POAC staff found it too difficult to give drinks to some patients and not to others, so it was decided that all patients should receive a drink. The clinical nurse practitioners note that the drink is given on the data collection sheet. However, it was observed that when team champions did not remind staff to administer the preoperative carbohydrate drinks, they were not given. We then asked the surgical admissions lounge staff if they would give preoperative carbohydrate drinks to patients and they agreed. This worked better than using POAC staff.
Patient Daily Aims
Members of the team felt that setting daily aims with patients would help optimize and prepare them for discharge. A laminated sheet with handwritten aims was trialed with 1 patient. He found it very useful, particularly the aims on diet and mobilization. When tested on all patients for a week, not only did they find it useful but nursing staff felt it improved communication between shifts. With greater staff buy-in and a move into a new purpose-built ward, we used white boards that were affixed to the door to the ensuite bathroom in each single patient room. Aims were discussed on ward rounds with patients by consultants or clinical nurse practitioners, and the goals agreed upon with patients before being written on the white boards. They included goals such as removal of urinary catheters, mobilization independently or with staff, and requirements such as radiographs to check position of instrumentation. Spot-checks on the ward showed good compliance with setting daily aims and high rates of satisfaction from patients.
Hospital at Home
The Hospital at Home team consists of experienced community-based nurses who provide wound care and analgesia advice for selected patients postdischarge to prevent readmission. This team supported early discharge for patients undergoing hip and knee replacements, and when approached they felt they could offer wound care and analgesia advice in the community for spinal surgery patients. This was tested with one patient with a wound who had daily care at home for 8 days following discharge from hospital. A further 2 patients were later cared for by the Hospital at Home team, with a total of 7 bed days saved. It has now become routine for the team to accept spinal patients when they have the capacity.
Outcomes
Working with the IT department and data collection tools attached to the medical records, we collected data on key measures every 2 weeks. Statistical process control charts (Process Improvement Products, Austin, TX) [9,10] were used to analyze the data.
Length of stay was reduced by 52% (Figure 4), improving from an average of 6 days during the baseline period to 2.9 days by April 2015. Readmissions for elective spinal surgery patients did not increase and in fact were reduced from 7% to 3%.
By October 2014, 99% of eligible patients were managed on the new pathway and most patients were receiving key
Discussion
The new pathway, the SpinaL Enhanced Recovery Program, improved reliability of care in our institution, with excellent patient satisfaction. It also exceeded its target in reducing length of stay for elective spinal surgery patients
One of the main strengths of this work was the use of small scale testing for each change idea using PDSA cycles, ramping up the idea prior to full implementation. The team could see the impact of changes on a small scale, then make adaptations in the next cycle to increase the likelihood of success.
The development and implementation of the pathway has led to a positive culture change. The spinal team has taken ownership of the pathway and continues to monitor its impact. Seeing the impact of their work on improving the quality of patient care has enhanced the team’s self-efficacy.
The methods used to plan and study our interventions, as well as some of the change ideas themselves, may be helpful for other elective spinal surgical teams. The simple application of the interventions without the improvement process may not have delivered the same outcome. Meeting regularly as a team to discuss ideas and implement new interventions with the guidance of a quality improvement advisor (M.W.) was felt to be the most important factor for success. The team also felt that it was important to collect data by any means possible to monitor interventions and motivate staff before better automated systems were implemented.
The SpinaL Enhanced Recovery Program pathway has now become “business as usual,” and the team plans to incorporate the process and outcome measures onto a monthly performance dashboard to continue to monitor the interventions. Further interventions are planned, including improving preoperative education with a patient pathway video. The team has started to try to stagger admissions for all-day theatre lists, to avoid patients having to wait all day for an afternoon operation. Further improvements in the reliability of care will also potentially allow the team to run controlled studies of single interventions to see how these can impact quality of patient care in a stable process.
Acknowledgments: The authors acknowledge Deborah Ray, Institute for Healthcare Improvement; Sandra Murray, Associates in Healthcare Improvement; Matthew Beebee, Clinical Nurse Practitioner Spinal Surgery; Debbie Vile and Lorraine Sandford, Clinical Nurse Practitioners Spinal Surgery; Sophie Hudson and Sallie Durman, Secretaries; Eleanor Palfreman, Occupational Therapist; Sarah Woodhill, Physiotherapist; Lee Scott, Improvement Nurse; Gervaise Khan-Davis, Directorate Manager; and “SG,” previous patient.
Corresponding author: Dr Julia Blackburn, Musgrove Park Hospital, Taunton, England, TA1 5DA, jlrkblackburn@doctors.org.uk.
Financial disclosures: None.
1. Nicholson A, Lowe MC, Parker J, et al. Systematic review and meta-analysis of enhanced recovery programmes in surgical patients. Br J Surg 2014;101:172–88.
2. Venkata H, Van Dellen J. A perspective on the use of an Enhanced Recovery Programme in open, non-instrumented, ‘day-surgery’ for degenerative lumbar and cervical spinal conditions. J Neurosurg Sci 2016.
3. Mathiesen O, Dahl B, Thomsen B, et al. A comprehensive multimodal pain treatment reduces opioid consumption after multilevel spine surgery. Eur Spine J 2013;22:2089–96.
4. Fleege C, Almajali A, Rauschmann M, et al. Improve of surgical outcome in spinal fusion surgery. Evidence based peri- and intra-operative aspects to reduce complications and earlier recovery. Der Orthopade 2014;43:1070–8.
5. Fleege C, Arabmotlagh M, Almajali A, et al. Pre- and postoperative fast-track treatment concepts in spinal surgery. Patient information and patient cooperation. Der Orthopade 2014;43:1062.
6. Smith MD, McCall J, Plank L, et al. Preoperative carbohydrate treatment for enhancing recovery after elective surgery. Cochrane Database Syst Rev 2014;8:CD009161.
7. Hendry PO, van Dam RM, Bukkems SF, et al. Randomized clinical trial of laxatives and oral nutritional supplements within an enhanced recovery after surgery protocol following liver resection. Br J Surg 2010;97:1198–206.
8. Marciniak CM, Toledo S, Lee J, et al. Lubiprostone vs senna in postoperative orthopedic surgery patients with opioid-induced constipation: a double-blind, active-comparator trial. World J Gastroenterol 2014;20:16323–33.
9. Benneyan J, Lloyd R, Plsek P. Statistical process control as a tool for research and healthcare improvement. Qual Safety Health Care 2003;12:458–64.
10. Portela MC, Pronovost PJ, Woodcock T, et al. How to study improvement interventions: a brief overview of possible study types. BMJ Qual Safety 2015;24:325–36.
1. Nicholson A, Lowe MC, Parker J, et al. Systematic review and meta-analysis of enhanced recovery programmes in surgical patients. Br J Surg 2014;101:172–88.
2. Venkata H, Van Dellen J. A perspective on the use of an Enhanced Recovery Programme in open, non-instrumented, ‘day-surgery’ for degenerative lumbar and cervical spinal conditions. J Neurosurg Sci 2016.
3. Mathiesen O, Dahl B, Thomsen B, et al. A comprehensive multimodal pain treatment reduces opioid consumption after multilevel spine surgery. Eur Spine J 2013;22:2089–96.
4. Fleege C, Almajali A, Rauschmann M, et al. Improve of surgical outcome in spinal fusion surgery. Evidence based peri- and intra-operative aspects to reduce complications and earlier recovery. Der Orthopade 2014;43:1070–8.
5. Fleege C, Arabmotlagh M, Almajali A, et al. Pre- and postoperative fast-track treatment concepts in spinal surgery. Patient information and patient cooperation. Der Orthopade 2014;43:1062.
6. Smith MD, McCall J, Plank L, et al. Preoperative carbohydrate treatment for enhancing recovery after elective surgery. Cochrane Database Syst Rev 2014;8:CD009161.
7. Hendry PO, van Dam RM, Bukkems SF, et al. Randomized clinical trial of laxatives and oral nutritional supplements within an enhanced recovery after surgery protocol following liver resection. Br J Surg 2010;97:1198–206.
8. Marciniak CM, Toledo S, Lee J, et al. Lubiprostone vs senna in postoperative orthopedic surgery patients with opioid-induced constipation: a double-blind, active-comparator trial. World J Gastroenterol 2014;20:16323–33.
9. Benneyan J, Lloyd R, Plsek P. Statistical process control as a tool for research and healthcare improvement. Qual Safety Health Care 2003;12:458–64.
10. Portela MC, Pronovost PJ, Woodcock T, et al. How to study improvement interventions: a brief overview of possible study types. BMJ Qual Safety 2015;24:325–36.