Takotsubo cardiomyopathy (TCM) is a transient left ventricular (LV) wall motion abnormality often associated with acute medical illnesses, catastrophic life events, and intense physical or emotional stress.1,2 Takotsubo cardiomyopathy also is known as stress-induced transient cardiomyopathy, apical ballooning syndrome, ampulla cardiomyopathy, and broken heart syndrome. The first reported case occurred in 1990 in Japan and accounts for 2% of all suspected acute coronary syndromes. Postmenopausal women seem to be at a higher risk for developing the disease, as about 90% of takotsubo cardiomyopathy occurs in postmenopausal women.3
Diagnosis of TCM is difficult, and there is an ongoing debate about the diagnostic criteria. The Mayo Clinic proposed the following criteria: (1) transient hypokinesis, akinesis, or dyskinesis of the LV mid-segments with or without apical involvement; the regional wall motion abnormalities extend beyond a single epicardial vascular distribution; a stressful trigger is often but not always present; (2) absence of obstructive coronary disease or angiographic evidence of acute plaque rupture; (3) new electrocardiographic abnormalities (either ST-segment elevation and/or T-wave inversion) or modest elevation in cardiac troponin; and (4) absence of pheochromocytoma and myocarditis.4
Depending on the part of the LV involved, TCM can be classified into apical ballooning variant (most common), an inverted or reverse takotsubo variant (basal akinesis with hyper dynamic apex), or a midventricular takotsubo variant.5
Several investigators have proposed the role of catecholamine in the pathogeneses of TCM.6,7 Previous case reports have shown that the clinical circumstances with elevated catecholamine can result in TCM.8,9 The authors recently encountered a case of a patient who developed apical ballooning TCM after an inadvertent injection of a high dose of epinephrine.
Case Report
A 60-year-old man with a history of hypertension, alcohol abuse, tobacco use, non-Hodgkin lymphoma, and recently diagnosed squamous cell carcinoma of the right glossopalatine fossa was admitted to the chemotherapy infusion clinic at the Kansas City VAMC to receive his first dose of cetuximab. Forty-five minutes after starting the test-dose infusion, the patient developed shortness of breath along with hives on his trunk and extremities. His blood pressure was 80/50 mm Hg; heart rate, 100 bpm; 16 breaths per minute respiration rate; and oxygen saturation by pulse oximetry was 90% on ambient air. The patient reported no chest pain, and a cardiac examination was unremarkable without wheezing on lung auscultation.
A clinical diagnosis of acute anaphylaxis reaction was considered; the test dose of cetuximab was discontinued, and the patient was given 50 mg of diphenhydramine, followed by an inadvertent administration of 1 mg of epinephrine intravenously (recommended dose 0.1 mg). After 3 minutes of administration of the medication, the patient’s blood pressure increased to190/110 with a pulse rate of 120 bpm.
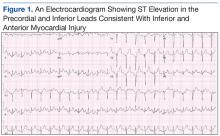
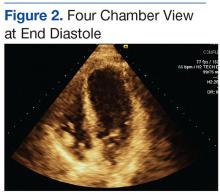
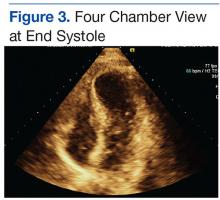
An electrocardiogram (EKG) showed ST elevation in the precordial and inferior leads consistent with inferior and anterior myocardial injury (Figure 1). Pertinent laboratory studies revealed normal serum potassium (4.4 mEq/L), elevated serum glucose (219 mg/dL), and elevated troponin-I, (1.180 ng/mL; reference range 0-0.3 ng/mL). An emergent transthoracic echocardiogram showed a LV ejection fraction of 40% with akinesis involving the apical anterior, mid and distal anteroseptal, and anterolateral wall with no significant valvular abnormalities (Figures 2 and 3).
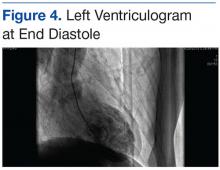
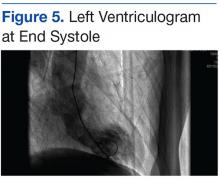
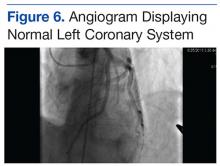
Given these echocardiographic findings, persistent EKG changes, and elevated troponin levels, an emergent coronary angiography along with left ventriculography was performed. The left ventriculogram demonstrated apical ballooning consistent with TCM (Figures 4 and 5). The left epicardial coronary arteries did not reveal any obstructive disease (Figure 6).
The subsequent hospital course was unremarkable, and the patient was discharged on guideline-directed medications for systolic dysfunction (ie, beta blockers and angiotensin-converting-enzyme inhibitors). Serum levels of epinephrine were not checked. A follow-up echocardiogram performed after 8 weeks showed complete recovery of the LV function (Figures 7a and 7b). The temporal sequence of events was highly suggestive of TCM, possibly due to the supratherapeutic dose of epinephrine.
Discussion
The pathogenesis of stress-induced cardiomyopathy is not fully understood. Various hypotheses have been suggested, including catecholamine excess, coronary vasospasm, microvascular dysfunction, and dynamic midcavity or LV outflow tract obstruction.1,10 The hypothesis implicating catecholamine excess in the pathogenesis of TCM is supported by animal studies.7 These studies suggest that catecholamines possibly play a role by “direct toxicity to myocardial cells” as evidenced by histologic findings of myofibrillar degeneration, contraction band necrosis, and leukocyte infiltration in harvested hearts from experimental animals and patients undergoing autopsy.7,11 Similarly, cultured cardiomyocytes exposed to high doses of epinephrine showed apoptic changes. Pretreatment of these cells with α- and β-adrenoreceptor blockers significantly attenuated these changes.7
However, myocardial necrosis alone cannot explain the entire picture, because most patients with TCM regain full recovery of LV function within several days of the event, and the degree of LV dysfunction is inconsistent with the mild elevations in cardiac
biomarkers. This explanation leads to the second hypothesis that proposes a “signal trafficking” role of catecholamines. According to this theory, the supraphysiologic doses of the catecholamines induce a switch in receptor coupling from Gs to Gi-proteins thus decreasing the contractility of the muscle. This switch protects the cardiac myocytes from excess stimulation and slows the apoptosis.7The role of estrogen also has been implicated in the pathogenesis of TCM. From a prevalence standpoint, almost 90% of TCM occurs in postmenopausal women.11,12 Estrogen plays a critical role in protecting the myocardium, possibly by down regulating β-adrenergic receptors. Postmenopausal women who do not receive estrogen replacement therapy lose this protection and may be more vulnerable to the catecholamine surge that is associated with stress.11 Overall, the catecholamines play a central role in the pathogenesis. This case suggests that exogenous administration of epinephrine in suprapharmacologic doses can be sufficient to replicate the stressful situation and induce TCM.