User login
OBJECTIVE: To determine the demographic, behavioral, and clinical factors associated with breastfeeding termination in the first 12 weeks postpartum.
STUDY DESIGN: This was a prospective cohort study.
POPULATION: Breastfeeding women in Michigan and Nebraska were interviewed by telephone at 3, 6, 9, and 12 weeks postpartum or until breastfeeding termination.
OUTCOMES MEASURED: We measured associations of demographic, clinical, and breastfeeding variables with weaning during the first 12 weeks postpartum.
RESULTS: A total of 946 women participated; 75% breastfed until 12 weeks. Women older than 30 years and women with at least a bachelor’s degree were more likely to continue breastfeeding in any given week. Mastitis, breast or nipple pain, bottle use, and milk expression in the first 3 weeks were all associated with termination. Beyond 3 weeks, women who expressed breast milk were 75% less likely to discontinue breastfeeding than women who did not. Women who used a bottle for some feedings during weeks 4 to 12 were 98% less likely to discontinue breastfeeding than women who did not use a bottle. "Not enough milk" was the most common reason given for termination in weeks 1 through 3 (37%) and weeks 4 through 6 (35%); “return to work” was the most common reason given in weeks 7 through 9 (53%) and weeks 10 through 12 (58%).
CONCLUSIONS: Younger women and less educated women need additional support in their breastfeeding efforts. Counseling and assistance should be provided to women with pain and mastitis. Exclusive breastfeeding for the first 3 weeks should be recommended. After the first 3 weeks, bottles and manual expression are not associated with weaning and may improve the likelihood of continuing breastfeeding, at least until 12 weeks.
- Younger and less educated women may need extra support for long-term breastfeeding success.
- Exclusive breastfeeding for the first 3 weeks decreases the risk of early weaning. At least 7 daily feedings of 10 or more minutes per feeding are recommended.
- The use of bottles and manual expression of milk after 3 weeks does not increase the risk of early weaning.
Family physicians are strongly encouraged to support and promote breastfeeding, the optimal form of infant nutrition.1 Despite its known benefits (fewer infant infections2-6 and decreased maternal risks of premenopausal breast cancer7 and post-menopausal hip fractures8), only 64% of mothers initiated breastfeeding in 19989 and only 29% of mothers fed their 6-month-old infant by breast, well below the Healthy People 2010 goal of 50% breastfeeding at 6 months.10 Clearly, determining the factors that influence breastfeeding beyond the early postpartum period would be beneficial.
Returning to work is a consistent risk factor for weaning.11-14 The impact of early bottle-feeding on the duration of breastfeeding has been studied with less consistent results.15,20 Insufficient milk supply is a common subjective reason given for termination.15,19,21,22 Older women and those with a higher level of education are at less risk of early breastfeeding termination.9,11,15,16,21,23,24
Few investigators have described how breastfeeding patterns may affect breastfeeding duration. Little is known about the effects of timing, frequency, and duration of individual breastfeedings, or the roles of breast pain and infection, sleep, and manual expression on early weaning. We studied women who indicated their intent to breastfeed prenatally to identify demographic factors and breastfeeding patterns associated with weaning in the first 12 weeks postpartum.
Methods
Population
We interviewed breastfeeding women by telephone at 3, 6, 9, and 12 weeks postpartum to investigate lactation mastitis risk factors and predictors of weaning. Pregnant women intending to breastfeed were recruited from 2 geographic sites between June 1994 and January 1998. In suburban Detroit, Michigan, women attending orientation at a freestanding birthing center were asked to participate. In Omaha, Nebraska, women at a single large company were recruited when applying for maternity leave.
Data collection
During the computer-assisted interview, subjects were asked to recall each of the previous 3 weeks. The initial interview, which collected demographic information, typically lasted 15 to 20 minutes; subsequent interviews were shorter. The survey addressed breastfeeding practices and recent health events. Exclusive breastfeeders were women who fed their infants only by breast. We did not collect information on pacifiers; therefore, exclusively breastfed infants may have also received pacifiers. Women who manually expressed or used a device to assist in expression were classified as “pumping” their breasts. Respondents were asked if they had bottle-fed the infant; they were not asked about bottle contents or volume.
Subjects were queried on potential difficulties including breast or nipple pain while nursing, nipple cracks, and mastitis (diagnosed by a health care provider), as well as other health problems and behaviors. Subjects who had stopped breastfeeding in the previous 3 weeks were asked when and why, given a list of possible explanations and an open-ended opportunity. Respondents could provide multiple reasons for termination.
Data analysis
Kaplan-Meier estimates describe the distribution of weaning times for the 2 sites. A log-rank test was used to assess group differences. Relationships between demographic factors and time of weaning were assessed by Cox regression analysis. Discrete survival analysis was used to determine whether variables measured on a weekly basis were related to breastfeeding cessation. Hazard ratios describe the association of the exposures between women who stopped breastfeeding at a given time and those who continued. Because breastfeeding cessation was a rare event in later weeks of the study, as were certain clinical or behavioral breastfeeding factors, weeks 4-12 were collapsed into a single interval. Two variables, number of daily feedings and duration of each feeding, were examined only in the first 3 weeks because the information was often missing beyond 3 weeks. All analyses were performed using the Statistical Package for the Social Sciences.25
Results
Description of subjects
A total of 1057 women agreed to be contacted. Of those, 946 (89.5%) participated in at least 1 interview. Of the 111 women who did not participate, 11 refused and 100 could not be located. Six hundred fifty-eight (69.6%) women completed all 4 interviews. The 56 women who entered the study at week 6 because they could not be reached for the first interview were similar in all factors to women who entered earlier. Of the 946, 711 (75.2%) were from Michigan and 235 (24.8%) were from Nebraska.
Subjects from Michigan were significantly more likely than those from Nebraska to be older than 30 years (52.0% vs 38.3%), have at least a bachelor’s degree (62.9% vs 48.5%), have 3 or more children (38.5% vs 19.6%), and have had a vaginal delivery (99.6% vs 77.0%) (Table W1).* The groups were similar in race, household income, and marital status.
Demographic factors
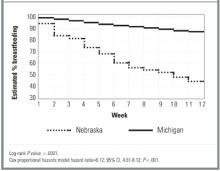
A total of 673 women (71.1%) continued breastfeeding until 12 weeks; 28% were exclusive breastfeeders. Michigan women were more likely to breastfeed at weeks 2 through 12 than their Nebraskan counterparts (P < .0001, Figure). A college degree was associated with 40% less weaning (Table 1). Age and annual household income were directly related to continued breastfeeding at both sites. Number of children in the household was not associated with termination. Previous breastfeeding experience showed a nonsignificant but consistent trend toward lower weaning risk.
TABLE 1
Relationships of demographics and other characteristics with time to weaning, by site
| Characteristic | Michigan women HR* (95% CI) | Nebraska women HR* (95% CI) |
|---|---|---|
| Older than 30 years | 0.5 (0.3,0.8) | 0.7 (0.5, 1.1) |
| BA/BS or higher | 0.6 (0.4, 0.9) | 0.6 (0.4, 0.8) |
| Number of children in household | ||
| 1 | 1.0 | 1.0 |
| 2 | 1.0 (0.6, 1.6) | 0.7 (0.5, 1.2) |
| 3 or more | 0.6 (0.4, 1.0) | 0.9 (0.6, 1.5) |
| Household income ≥ $50,000 | 0.8 (0.5, 1.3) | 0.7 (0.5, 1.0) |
| Breastfed previously | 0.7 (0.5, 1.1) | 0.7 (0.5, 1.1) |
| Nonvaginal birth | † | 0.9 (0.6, 1.4) |
| NOTE: Bold numbers are significant at P < .05. | ||
| HR denotes hazard ratio; CI, confidence interval; BA, bachelor of arts degree; BS, bachelor of science degree. | ||
| *A hazard ratio of <1 indicates that subjects with this characteristic were less likely to wean during the 12 weeks. Unless otherwise noted, the referent group is the converse (eg, age < 30 years is the referent group for those older than 30 years). | ||
| †Too few observations to provide meaningful results. | ||
FIGURE
Probability of breastfeeding, by site, by postpartum week
Clinical and behavioral factors
Because time to weaning differed significantly by site, the survival analyses of clinical and behavioral factors were performed separately for Michigan and Nebraska and controlled for education, age, and previous breastfeeding experience.
During the first 3 weeks, Michigan women with mastitis were nearly 6 times more likely than Michigan women without mastitis to stop breast-feeding in the week of diagnosis (Table 2). Women from Nebraska showed nonsignificant results in the same direction in weeks 4 to 12. (No women from Nebraska with mastitis terminated during weeks 1 through 3.) Although nipple sores and cracks were not associated with weaning, breast pain was associated with weaning. For each day of pain in the first 3 weeks, there was a 10% increase in risk of cessation among Michigan women and a 26% increase among Nebraska women. The association between pain and weaning in weeks 4 through 12 is less clear. In these later weeks, women who reported pain were unexpectedly 75% to 80% more likely to continue breastfeeding than women who did not report pain, yet for Nebraska women the number of days with pain remained significantly associated with breastfeeding cessation.
Subjective depression and breastfeeding cessation were not related. The association between daily sleep and weaning varied by site. During weeks 4 through 12, Michigan women with more daily sleep were less likely to terminate. An opposite, but marginally significant trend, was observed for Nebraska women. Weaning was not associated with outside household help. Nonvaginal birth was not associated with weaning for Nebraska women. (There were only 2 cesarean sections in the Michigan group.)
Michigan women who expressed breast milk during the first 3 weeks were twice as likely to stop breastfeeding as those who did not pump. During the same period, Michigan women who used a bottle for some feedings were 9 times more likely to wean than nonbottle users. Respondents in Nebraska showed similar nonsignificant trends in the first 3 weeks. By contrast, during weeks 4 through 12, both Nebraska and Michigan women who pumped were about 75% less likely to wean, while women who used a bottle for some feedings were 98% less likely to stop breastfeeding.
Breast milk expression increased gradually over time, from 30% of women pumping an average of 3 times per day in the first 3 weeks to 45% of women pumping 5 times per day in the last 3 weeks. To determine if pumping and bottle-feeding had an effect independent of pain or mastitis on weaning in the first 3 weeks, we performed additional analyses controlling for pain, cracks and sores, and mastitis in the same week. The results were similar to those presented in Table 2. Michigan women who pumped were 3 times more likely to wean than those who did not pump (hazard ratio [HR] = 3.0, 95% confidence interval [CI], 1.3 - 6.7), while for Nebraska women there was no association between pumping and weaning (HR = 0.6, 95% CI, 0.3 - 1.5). Bottle-feeding was again significantly associated with weaning in weeks 1 through 3 for Michigan women (HR = 10.9, 95% CI, 4.5 - 26.7) and not associated in Nebraskans (HR = 0.8, 95% CI, 0.4 - 2.0).
Duration and frequency of feedings were investigated as weaning risk factors. There appeared to be a threshold for both variables during the first 3 weeks in Michigan women. Michigan women who breastfed less than 10 minutes per feeding were nearly 5 times more likely to stop breastfeeding than women who breastfed longer. Michigan women who breastfed 6 or fewer times per day were 8 times more likely to stop than those who breastfed more often. Results for Nebraska women fell in the same direction but were not statistically significant.
TABLE 2
Relationships of clinical and behavioral factors to breastfeeding cessation in the same week, adjusted for mother’s age, education, and previous breastfeeding experience
| Variable | Week | Michigan women HR (95% CI) | Nebraska women HR (95% CI) |
|---|---|---|---|
| Mastitis | 1 - 3 | 5.7 (1.3 - 25.9) | ‡ |
| 4 - 12 | ‡ | 2.1 (0.3 - 17.4) | |
| Engorgement | 1 - 3 | 0.6 (0.2 - 1.5) | 0.8 (0.3 - 2.1) |
| 4 - 12 | ‡ | 3.2 (0.6 - 15.8) | |
| Nipple sores/cracks | 1 - 3 | 1.1 (0.4 - 2.6) | 0.9 (0.4 - 2.3) |
| 4 - 12 | 2.6 (0.8 - 8.5) | 2.9 (0.8 - 10.7) | |
| Any pain † | 1 - 3 | 14.7 (6.8 - 32.0)§ | 9.1 (3.9 - 21.2)† |
| 4 - 12 | 0.3 (0.1 - 0.7) | 0.2 (0.1 - 0.5)† | |
| Days with pain* | 1 - 3 | 1.1 (1.0 - 1.2) | 1.3 (1.0 - 1.5) |
| 4 - 12 | 1.1 (1.0 - 1.2) | 1.1 (1.0 - 1.2) | |
| Returned to work | 1 - 3 | 0.4 (0.1 - 3.0) | ‡ |
| 4 - 12 | 2.1 (1.1 - 4.0) | 0.8 (0.4 - 1.7) | |
| Depressed | 1 - 3 | 0.9 (0.3 - 3.0) | 1.0 (0.4 - 2.6) |
| 4 - 12 | 0.9 (0.4 - 2.2) | 1.3 (0.6 - 2.7) | |
| Daily sleep hours | 1 - 3 | 0.9 (0.7 - 1.1) | 0.9 (0.8 - 1.2) |
| 4 - 12 | 0.7 (0.5 - 0.9) | 1.2 (1.0 - 1.5) | |
| Outside household help | 1 - 3 | 2.0 (0.8 - 4.8) | 0.9 (0.4 - 2.1) |
| 4 - 12 | 0.7 (0.3 - 2.6) | 0.7 (0.2 - 2.1) | |
| Pumping | 1 - 3 | 2.2 (1.1 - 4.6) | 1.3 (0.6 - 2.5) |
| 4 - 12 | 0.2 (0.1 - 0.5)§ | 0.3 (0.1 - 0.5) § | |
| Bottle feeding | 1 - 3 | 9.5 (4.3 - 21.0) § | 1.8 (0.9 - 3.5) |
| 4 - 12 | 0.03 (0.003 - 0.2) § | 0.02 (0.004 - 0.1) § | |
| Minutes per feeding | 1 - 3 | 1.0 (0.9, 1.0) | 1.1 (1.0, 1.1) |
| Less than 10 minutes per feeding | 1 - 3 | 4.8 (1.7, 13.4) | 2.2 (0.6, 8.1) |
| Feedings per day | 1 - 3 | 0.7 (0.6, 0.8) § | 0.9 (0.8, 1.1) |
| Less than 7 feedings/day | 1 - 3 | 8.1 (3.4, 19.2) § | 1.8 (0.7, 4.6) |
| NOTE: Bold numbers significant at P = .05 or less; those marked with § are significant at P = .001 or less. | |||
| HR denotes hazard ratio; CI, confidence interval. | |||
| *Subjects answered affirmatively to any of the following types of pain: pain when latching on, pain while nursing, pain when not nursing. | |||
| † Measured in 3-week periods. | |||
| ‡ Indicates there were too few observations to provide meaningful results; for example, there were no Nebraska women who had mastitis and stopped breastfeeding in the same week during weeks 1-3. | |||
Subjective factors
At each interview, women who had stopped breastfeeding in the previous 3 weeks were asked why they had made that decision. Most women (75%) provided only one reason. At the first interview, insufficient milk supply (37.3%) and breast pain or mastitis (32.9%) were the most common reasons for termination (Table 3). Insufficient milk supply was the reason most often given (35.0%) during weeks 4 through 6. At both weeks 9 and 12, return to work was the reason given most often (53.1% and 58.3%, respectively).
TABLE 3
Percentage of women citing given reason for termination of breastfeeding
| Week 3 | Week 6 | Week 9 | Week 12 | |
|---|---|---|---|---|
| Reason | (n = 67) | (n = 60) | (n = 32) | (n = 36) |
| Insufficient milk supply | 37.3 | 35.0 | 25.0 | 13.9 |
| Inconvenient | 17.9 | 25.0 | 21.9 | 33.3 |
| Returned to work | 4.5 | 31.7 | 53.1 | 58.3 |
| Breast pain or infection | 32.9 | 23.3 | 0 | 5.6 |
| Baby stopped nursing | 7.5 | 5.0 | 3.1 | 11.1 |
| Other | 22.4 | 18.3 | 3.1 | 5.6 |
| NOTE: Percentages total more than 100% because respondents could cite multiple reasons. | ||||
Discussion
Mastitis, pain, and days with pain in the first 3 weeks were important clinical factors associated with breastfeeding cessation in this cohort of women who prenatally self-identified as intending to breastfeed. Women who intend to breastfeed should be counseled regarding these possible complications, their temporary nature, prevention, and treatment. Mastitis is not an indication for breastfeeding termination; in fact, increased feedings and milk expression are considered treatment.26,27 Women who reported pain the first 3 weeks were more likely to stop breastfeeding than women who reported pain after the first 3 weeks. It is difficult to explain this finding; perhaps there are women who have pain during their entire breastfeeding career and yet continue to breastfeed because they are more pain-tolerant, have less severe or frequent pain than those who wean, or are more committed to breastfeeding.
Other clinical factors investigated were depression and daily sleep hours. Weaning was not associated with subjective depression. However, subjects did not undergo formal psychological testing as in the study that reported an association.24 The relationship between daily sleep hours and termination was not consistent, and likely not clinically significant.
The demographic risk factors related to breast-feeding termination in our study are similar to those previously reported,14,15,20,21,23,24 namely, younger maternal age and lower educational level. Investigations of parity have been inconsistent.16,28 We found no association of weaning with parity. Prior breastfeeding experience has been reported as improving breastfeeding rates15,28; our results are consistent with those findings, but not significantly so. All subjects had access to prenatal breastfeeding education and postnatal breastfeeding support, which may have diminished the differences between women with breastfeeding experience and those without experience.20
Michigan and Nebraska women who pumped or bottle-fed during weeks 4 through 12 were significantly less likely to terminate breastfeeding. In contrast, Michigan women who pumped or bottle-fed during the first 3 weeks postpartum were more likely to terminate even after controlling for pain and mastitis. A commitment to exclusive breastfeeding may be necessary in the early postpartum period for long-term success.15,19 To our knowledge, the seemingly protective effect associated with pumping and bottle-feeding after the first 3 weeks has not been previously reported.
Breastfeeding 6 or fewer times per day and feedings of 10 minutes or less were associated with termination during the first 3 weeks. Other studies also indicate that the ratio of breast to bottle feedings is important for long-term success. Feinstein and colleagues15 found that more than one daily bottle of formula supplementation was associated with shorter breastfeeding duration, which was minimized if there were 7 or more breastfeedings per day. Another study found no weaning difference between women who offered their infant only one bottle daily during weeks 2 through 6 and a bottle-avoiding group.17
The most frequent reasons given for termination were similar to those reported by others, namely, insufficient milk supply and return to work.11-15,21,22 Insufficient milk supply was a more common reason in the first few weeks after birth; return to work became an increasingly common reason after week 6.
We were unable to examine the role of pacifiers or smoking in breastfeedng termination because pacifier information was not collected and there were too few smokers for meaningful analysis. Smoking has been consistently reported as associated with early cessation.15,20,29,30 Although pacifier use does not appear to be directly related,31,32 it has been proposed as a marker for breastfeeding problems. The homogeneity of the sample limits our ability to make generalizations regarding other populations, such as women of color. However, the large sample size and the similarity of termination risk factors between 2 different populations of women lend confidence to our conclusions. As we did not assess mothers’ intentions, some of the variables found associated with termination might be intentional activities of weaning rather than risk factors for termination. The significant difference in termination risk between the sites also may be related to mothers’ intentions or level of commitment. The Michigan women may have intended to breastfeed longer from the outset. The Michigan recruitment site was an alternative birthing center. Women being delivered there may be more persistent in their breast-feeding efforts. Both sites provided access to breast-feeding support personnel, but the Michigan women, as a group, may have been more motivated to continue.
Our results provide clinically useful information. Additional support may be needed for younger and less educated women. Special efforts should be made for early diagnosis and treatment of mastitis and breast pain, particularly during the first 3 weeks. Exclusive breastfeeding without bottle supplementation should be recommended for the first 3 weeks, with at least 7 feedings per day. Each feeding should preferably last more than 10 minutes.
These results should also reassure breastfeeding women and their providers regarding the use of bottles. Bottle-feeding after 3 weeks does not appear to jeopardize breastfeeding success up to 12 weeks and may even improve it.
* Table W1 appears on the JFP Web site at www.jfponline.com.
Acknowledgments
This study was supported by National Institutes of Health grant #30866.
1. American Academy of Family Physicians. Policies on Health Issues: Infant Health. URL: http://aafp.org/policy/issues/i3.html
2. Beaudry M, Dufour R, Marcoux S. Relation between infant feeding and infections during the first six months of life. J Pediatr 1995;126:696-702.
3. Dewey K, Heinig M, Nommsen-Rivers LA. Differences in morbidity between breast-fed and formula-fed infants. J Pediatr 1995;126:191-7.
4. Duncan B, Ey J, Holberg CJ, Wright AL, Martinez FD, Taussig LM. Exclusive breast-feeding for at least 4 months protects against otitis media. Pediatrics 1993;91:867-72.
5. Raisler J, Alexander C, O’Campo P. Breast-feeding and infant illness: a dose-reponse relationship? Am J Public Health 2000;90:1478-9.
6. Hanson LA. Breastfeeding provides passive and likely long-lasting active immunity. Ann Allergy Asthma Immunol 1998;81:523-33.
7. Newcomb P, Storer B, Longnecker M, et al. Lactation and a reduced risk of premenopausal breast cancer. N Engl J Med 1994;330:81-7.
8. Cumming RG, Klinieberg RJ. Breastfeeding and other reproductive factors and the risk of hip fractures in elderly women. Int J Epidemiol 1993;22:884-91.
9. Mother’s Survey, Ross Products Division, Abbot Laboratories, Inc. Columbus OH, 1998.
10. U.S. Department of Health and Human Services. Healthy People 2010. (Conference edition in 2 volumes.) Washington, DC: January 2000.
11. Gielen AC, Faden RR, O’Campo P, Brown CH, Paige DM. Maternal employment during the early postpartum period: effects on initiation and continuation of breastfeeding. Pediatrics 1991;87:298-305.
12. Fein SB, Roe B. The effect of work status on initiation and duration of breast-feeding. Am J Public Health 1998;88:1042-6.
13. Kurinij N, Shiono PH, Ezrine SF, Rhoads GG. Does maternal employment affect breast-feeding? Am J Public Health 1989;79:1247-50.
14. Kearney MH, Cronenwett L. Breastfeeding and employment. J Obstet Gynecol Neonatal Nurs 1991;20:471-80.
15. Feinstein JM, Berkelhamer JE, Gruszka ME, Wong CA, Carey AE. Factors related to early termination of breast-feeding in an urban population. Pediatrics 1986;78:210-5.
16. Ryan AS, Wysong JL, Martinez GA, Simon SD. Duration of breast-feeding patterns established in the hospital. Clin Pediatr 1990;29:99-107.
17. Cronenwett L, Strukel T, Kearney M, et al. Single daily bottle use in the early weeks postpartum and breast-feeding outcomes. Pediatrics 1992;90:760-6.
18. Gray-Donald K, Kramer MS, Munday S, Leduc DG. Effect of formula supplementation in the hospital on the duration of breast-feeding; a controlled clinical trial. Pediatrics 1985;75:514-8.
19. Hill PD, Humenick SS, Brennan ML, Woolley D. Does early supplementation affect long-term breastfeeding? Clin Pediatr 1997;June:345-350.
20. Wright HJ, Walker PC. Prediction of duration of breast feeding in primiparas. J Epidemiol Comm Health 1983;37:89-94.
21. Hawkins LM, Nichols FH, Tanner JL. Predictors of the duration of breastfeeding in low-income women. Birth 1987;14:204-9.
22. Hill PD, Aldag JC. Insufficient milk supply among black and white breast-feeding mothers. Res Nurs Health 1993;16:203-11.
23. Kurinij N, Shiono PH, Rhoads GG. Breast-feeding incidence and duration in black and white women. Pediatrics 1988;81:365-71.
24. Cooper PJ, Murray L, Stein A. Psychosocial factors associated with the early termination of breast-feeding. J Psychosom Res 1993;37:171-6.
25. Statistical Package for the Social Sciences. Chicago, IL: SPSS Inc; 1998.
26. Marshall B, Hepper J. Zirbel. Sporadic mastitis: an infection that need not interrupt lactation. JAMA 1975;233:1377-9.
27. Lawrence R. Mastitis. In: Breastfeeding: a guide for the medical profession. 4th ed. St. Louis: Mosby; 1994.
28. Hill PD, Humenick SS, Argubright T, Aldag JC. Effects of parity and weaning practices on breastfeeding duration. Public Health Nurs 1997;14:227-34.
29. Hill PD, Aldag JC. Smoking and breastfeeding status. Res Nurs Health 1996;19:125-32.
30. Woodward A, Hand K. Smoking and reduced duration of breast-feeding. Med J Australia 1988;148:477-8.
31. Victora CG, Behague DP, Barros FC, Olinto MT, Weiderpass E. Pacifier use and short breastfeeding duration: cause, consequence, or coincidence. Pediatrics 1997;99:445-3.
32. Howard CR, Howard FM, Lanphear B, deBlieck EA, Eberly S, Lawrence RA. The effects of early pacifier use on breastfeeding duration? Pediatrics 1999;103:E33.-
OBJECTIVE: To determine the demographic, behavioral, and clinical factors associated with breastfeeding termination in the first 12 weeks postpartum.
STUDY DESIGN: This was a prospective cohort study.
POPULATION: Breastfeeding women in Michigan and Nebraska were interviewed by telephone at 3, 6, 9, and 12 weeks postpartum or until breastfeeding termination.
OUTCOMES MEASURED: We measured associations of demographic, clinical, and breastfeeding variables with weaning during the first 12 weeks postpartum.
RESULTS: A total of 946 women participated; 75% breastfed until 12 weeks. Women older than 30 years and women with at least a bachelor’s degree were more likely to continue breastfeeding in any given week. Mastitis, breast or nipple pain, bottle use, and milk expression in the first 3 weeks were all associated with termination. Beyond 3 weeks, women who expressed breast milk were 75% less likely to discontinue breastfeeding than women who did not. Women who used a bottle for some feedings during weeks 4 to 12 were 98% less likely to discontinue breastfeeding than women who did not use a bottle. "Not enough milk" was the most common reason given for termination in weeks 1 through 3 (37%) and weeks 4 through 6 (35%); “return to work” was the most common reason given in weeks 7 through 9 (53%) and weeks 10 through 12 (58%).
CONCLUSIONS: Younger women and less educated women need additional support in their breastfeeding efforts. Counseling and assistance should be provided to women with pain and mastitis. Exclusive breastfeeding for the first 3 weeks should be recommended. After the first 3 weeks, bottles and manual expression are not associated with weaning and may improve the likelihood of continuing breastfeeding, at least until 12 weeks.
- Younger and less educated women may need extra support for long-term breastfeeding success.
- Exclusive breastfeeding for the first 3 weeks decreases the risk of early weaning. At least 7 daily feedings of 10 or more minutes per feeding are recommended.
- The use of bottles and manual expression of milk after 3 weeks does not increase the risk of early weaning.
Family physicians are strongly encouraged to support and promote breastfeeding, the optimal form of infant nutrition.1 Despite its known benefits (fewer infant infections2-6 and decreased maternal risks of premenopausal breast cancer7 and post-menopausal hip fractures8), only 64% of mothers initiated breastfeeding in 19989 and only 29% of mothers fed their 6-month-old infant by breast, well below the Healthy People 2010 goal of 50% breastfeeding at 6 months.10 Clearly, determining the factors that influence breastfeeding beyond the early postpartum period would be beneficial.
Returning to work is a consistent risk factor for weaning.11-14 The impact of early bottle-feeding on the duration of breastfeeding has been studied with less consistent results.15,20 Insufficient milk supply is a common subjective reason given for termination.15,19,21,22 Older women and those with a higher level of education are at less risk of early breastfeeding termination.9,11,15,16,21,23,24
Few investigators have described how breastfeeding patterns may affect breastfeeding duration. Little is known about the effects of timing, frequency, and duration of individual breastfeedings, or the roles of breast pain and infection, sleep, and manual expression on early weaning. We studied women who indicated their intent to breastfeed prenatally to identify demographic factors and breastfeeding patterns associated with weaning in the first 12 weeks postpartum.
Methods
Population
We interviewed breastfeeding women by telephone at 3, 6, 9, and 12 weeks postpartum to investigate lactation mastitis risk factors and predictors of weaning. Pregnant women intending to breastfeed were recruited from 2 geographic sites between June 1994 and January 1998. In suburban Detroit, Michigan, women attending orientation at a freestanding birthing center were asked to participate. In Omaha, Nebraska, women at a single large company were recruited when applying for maternity leave.
Data collection
During the computer-assisted interview, subjects were asked to recall each of the previous 3 weeks. The initial interview, which collected demographic information, typically lasted 15 to 20 minutes; subsequent interviews were shorter. The survey addressed breastfeeding practices and recent health events. Exclusive breastfeeders were women who fed their infants only by breast. We did not collect information on pacifiers; therefore, exclusively breastfed infants may have also received pacifiers. Women who manually expressed or used a device to assist in expression were classified as “pumping” their breasts. Respondents were asked if they had bottle-fed the infant; they were not asked about bottle contents or volume.
Subjects were queried on potential difficulties including breast or nipple pain while nursing, nipple cracks, and mastitis (diagnosed by a health care provider), as well as other health problems and behaviors. Subjects who had stopped breastfeeding in the previous 3 weeks were asked when and why, given a list of possible explanations and an open-ended opportunity. Respondents could provide multiple reasons for termination.
Data analysis
Kaplan-Meier estimates describe the distribution of weaning times for the 2 sites. A log-rank test was used to assess group differences. Relationships between demographic factors and time of weaning were assessed by Cox regression analysis. Discrete survival analysis was used to determine whether variables measured on a weekly basis were related to breastfeeding cessation. Hazard ratios describe the association of the exposures between women who stopped breastfeeding at a given time and those who continued. Because breastfeeding cessation was a rare event in later weeks of the study, as were certain clinical or behavioral breastfeeding factors, weeks 4-12 were collapsed into a single interval. Two variables, number of daily feedings and duration of each feeding, were examined only in the first 3 weeks because the information was often missing beyond 3 weeks. All analyses were performed using the Statistical Package for the Social Sciences.25
Results
Description of subjects
A total of 1057 women agreed to be contacted. Of those, 946 (89.5%) participated in at least 1 interview. Of the 111 women who did not participate, 11 refused and 100 could not be located. Six hundred fifty-eight (69.6%) women completed all 4 interviews. The 56 women who entered the study at week 6 because they could not be reached for the first interview were similar in all factors to women who entered earlier. Of the 946, 711 (75.2%) were from Michigan and 235 (24.8%) were from Nebraska.
Subjects from Michigan were significantly more likely than those from Nebraska to be older than 30 years (52.0% vs 38.3%), have at least a bachelor’s degree (62.9% vs 48.5%), have 3 or more children (38.5% vs 19.6%), and have had a vaginal delivery (99.6% vs 77.0%) (Table W1).* The groups were similar in race, household income, and marital status.
Demographic factors
A total of 673 women (71.1%) continued breastfeeding until 12 weeks; 28% were exclusive breastfeeders. Michigan women were more likely to breastfeed at weeks 2 through 12 than their Nebraskan counterparts (P < .0001, Figure). A college degree was associated with 40% less weaning (Table 1). Age and annual household income were directly related to continued breastfeeding at both sites. Number of children in the household was not associated with termination. Previous breastfeeding experience showed a nonsignificant but consistent trend toward lower weaning risk.
TABLE 1
Relationships of demographics and other characteristics with time to weaning, by site
| Characteristic | Michigan women HR* (95% CI) | Nebraska women HR* (95% CI) |
|---|---|---|
| Older than 30 years | 0.5 (0.3,0.8) | 0.7 (0.5, 1.1) |
| BA/BS or higher | 0.6 (0.4, 0.9) | 0.6 (0.4, 0.8) |
| Number of children in household | ||
| 1 | 1.0 | 1.0 |
| 2 | 1.0 (0.6, 1.6) | 0.7 (0.5, 1.2) |
| 3 or more | 0.6 (0.4, 1.0) | 0.9 (0.6, 1.5) |
| Household income ≥ $50,000 | 0.8 (0.5, 1.3) | 0.7 (0.5, 1.0) |
| Breastfed previously | 0.7 (0.5, 1.1) | 0.7 (0.5, 1.1) |
| Nonvaginal birth | † | 0.9 (0.6, 1.4) |
| NOTE: Bold numbers are significant at P < .05. | ||
| HR denotes hazard ratio; CI, confidence interval; BA, bachelor of arts degree; BS, bachelor of science degree. | ||
| *A hazard ratio of <1 indicates that subjects with this characteristic were less likely to wean during the 12 weeks. Unless otherwise noted, the referent group is the converse (eg, age < 30 years is the referent group for those older than 30 years). | ||
| †Too few observations to provide meaningful results. | ||
FIGURE
Probability of breastfeeding, by site, by postpartum week
Clinical and behavioral factors
Because time to weaning differed significantly by site, the survival analyses of clinical and behavioral factors were performed separately for Michigan and Nebraska and controlled for education, age, and previous breastfeeding experience.
During the first 3 weeks, Michigan women with mastitis were nearly 6 times more likely than Michigan women without mastitis to stop breast-feeding in the week of diagnosis (Table 2). Women from Nebraska showed nonsignificant results in the same direction in weeks 4 to 12. (No women from Nebraska with mastitis terminated during weeks 1 through 3.) Although nipple sores and cracks were not associated with weaning, breast pain was associated with weaning. For each day of pain in the first 3 weeks, there was a 10% increase in risk of cessation among Michigan women and a 26% increase among Nebraska women. The association between pain and weaning in weeks 4 through 12 is less clear. In these later weeks, women who reported pain were unexpectedly 75% to 80% more likely to continue breastfeeding than women who did not report pain, yet for Nebraska women the number of days with pain remained significantly associated with breastfeeding cessation.
Subjective depression and breastfeeding cessation were not related. The association between daily sleep and weaning varied by site. During weeks 4 through 12, Michigan women with more daily sleep were less likely to terminate. An opposite, but marginally significant trend, was observed for Nebraska women. Weaning was not associated with outside household help. Nonvaginal birth was not associated with weaning for Nebraska women. (There were only 2 cesarean sections in the Michigan group.)
Michigan women who expressed breast milk during the first 3 weeks were twice as likely to stop breastfeeding as those who did not pump. During the same period, Michigan women who used a bottle for some feedings were 9 times more likely to wean than nonbottle users. Respondents in Nebraska showed similar nonsignificant trends in the first 3 weeks. By contrast, during weeks 4 through 12, both Nebraska and Michigan women who pumped were about 75% less likely to wean, while women who used a bottle for some feedings were 98% less likely to stop breastfeeding.
Breast milk expression increased gradually over time, from 30% of women pumping an average of 3 times per day in the first 3 weeks to 45% of women pumping 5 times per day in the last 3 weeks. To determine if pumping and bottle-feeding had an effect independent of pain or mastitis on weaning in the first 3 weeks, we performed additional analyses controlling for pain, cracks and sores, and mastitis in the same week. The results were similar to those presented in Table 2. Michigan women who pumped were 3 times more likely to wean than those who did not pump (hazard ratio [HR] = 3.0, 95% confidence interval [CI], 1.3 - 6.7), while for Nebraska women there was no association between pumping and weaning (HR = 0.6, 95% CI, 0.3 - 1.5). Bottle-feeding was again significantly associated with weaning in weeks 1 through 3 for Michigan women (HR = 10.9, 95% CI, 4.5 - 26.7) and not associated in Nebraskans (HR = 0.8, 95% CI, 0.4 - 2.0).
Duration and frequency of feedings were investigated as weaning risk factors. There appeared to be a threshold for both variables during the first 3 weeks in Michigan women. Michigan women who breastfed less than 10 minutes per feeding were nearly 5 times more likely to stop breastfeeding than women who breastfed longer. Michigan women who breastfed 6 or fewer times per day were 8 times more likely to stop than those who breastfed more often. Results for Nebraska women fell in the same direction but were not statistically significant.
TABLE 2
Relationships of clinical and behavioral factors to breastfeeding cessation in the same week, adjusted for mother’s age, education, and previous breastfeeding experience
| Variable | Week | Michigan women HR (95% CI) | Nebraska women HR (95% CI) |
|---|---|---|---|
| Mastitis | 1 - 3 | 5.7 (1.3 - 25.9) | ‡ |
| 4 - 12 | ‡ | 2.1 (0.3 - 17.4) | |
| Engorgement | 1 - 3 | 0.6 (0.2 - 1.5) | 0.8 (0.3 - 2.1) |
| 4 - 12 | ‡ | 3.2 (0.6 - 15.8) | |
| Nipple sores/cracks | 1 - 3 | 1.1 (0.4 - 2.6) | 0.9 (0.4 - 2.3) |
| 4 - 12 | 2.6 (0.8 - 8.5) | 2.9 (0.8 - 10.7) | |
| Any pain † | 1 - 3 | 14.7 (6.8 - 32.0)§ | 9.1 (3.9 - 21.2)† |
| 4 - 12 | 0.3 (0.1 - 0.7) | 0.2 (0.1 - 0.5)† | |
| Days with pain* | 1 - 3 | 1.1 (1.0 - 1.2) | 1.3 (1.0 - 1.5) |
| 4 - 12 | 1.1 (1.0 - 1.2) | 1.1 (1.0 - 1.2) | |
| Returned to work | 1 - 3 | 0.4 (0.1 - 3.0) | ‡ |
| 4 - 12 | 2.1 (1.1 - 4.0) | 0.8 (0.4 - 1.7) | |
| Depressed | 1 - 3 | 0.9 (0.3 - 3.0) | 1.0 (0.4 - 2.6) |
| 4 - 12 | 0.9 (0.4 - 2.2) | 1.3 (0.6 - 2.7) | |
| Daily sleep hours | 1 - 3 | 0.9 (0.7 - 1.1) | 0.9 (0.8 - 1.2) |
| 4 - 12 | 0.7 (0.5 - 0.9) | 1.2 (1.0 - 1.5) | |
| Outside household help | 1 - 3 | 2.0 (0.8 - 4.8) | 0.9 (0.4 - 2.1) |
| 4 - 12 | 0.7 (0.3 - 2.6) | 0.7 (0.2 - 2.1) | |
| Pumping | 1 - 3 | 2.2 (1.1 - 4.6) | 1.3 (0.6 - 2.5) |
| 4 - 12 | 0.2 (0.1 - 0.5)§ | 0.3 (0.1 - 0.5) § | |
| Bottle feeding | 1 - 3 | 9.5 (4.3 - 21.0) § | 1.8 (0.9 - 3.5) |
| 4 - 12 | 0.03 (0.003 - 0.2) § | 0.02 (0.004 - 0.1) § | |
| Minutes per feeding | 1 - 3 | 1.0 (0.9, 1.0) | 1.1 (1.0, 1.1) |
| Less than 10 minutes per feeding | 1 - 3 | 4.8 (1.7, 13.4) | 2.2 (0.6, 8.1) |
| Feedings per day | 1 - 3 | 0.7 (0.6, 0.8) § | 0.9 (0.8, 1.1) |
| Less than 7 feedings/day | 1 - 3 | 8.1 (3.4, 19.2) § | 1.8 (0.7, 4.6) |
| NOTE: Bold numbers significant at P = .05 or less; those marked with § are significant at P = .001 or less. | |||
| HR denotes hazard ratio; CI, confidence interval. | |||
| *Subjects answered affirmatively to any of the following types of pain: pain when latching on, pain while nursing, pain when not nursing. | |||
| † Measured in 3-week periods. | |||
| ‡ Indicates there were too few observations to provide meaningful results; for example, there were no Nebraska women who had mastitis and stopped breastfeeding in the same week during weeks 1-3. | |||
Subjective factors
At each interview, women who had stopped breastfeeding in the previous 3 weeks were asked why they had made that decision. Most women (75%) provided only one reason. At the first interview, insufficient milk supply (37.3%) and breast pain or mastitis (32.9%) were the most common reasons for termination (Table 3). Insufficient milk supply was the reason most often given (35.0%) during weeks 4 through 6. At both weeks 9 and 12, return to work was the reason given most often (53.1% and 58.3%, respectively).
TABLE 3
Percentage of women citing given reason for termination of breastfeeding
| Week 3 | Week 6 | Week 9 | Week 12 | |
|---|---|---|---|---|
| Reason | (n = 67) | (n = 60) | (n = 32) | (n = 36) |
| Insufficient milk supply | 37.3 | 35.0 | 25.0 | 13.9 |
| Inconvenient | 17.9 | 25.0 | 21.9 | 33.3 |
| Returned to work | 4.5 | 31.7 | 53.1 | 58.3 |
| Breast pain or infection | 32.9 | 23.3 | 0 | 5.6 |
| Baby stopped nursing | 7.5 | 5.0 | 3.1 | 11.1 |
| Other | 22.4 | 18.3 | 3.1 | 5.6 |
| NOTE: Percentages total more than 100% because respondents could cite multiple reasons. | ||||
Discussion
Mastitis, pain, and days with pain in the first 3 weeks were important clinical factors associated with breastfeeding cessation in this cohort of women who prenatally self-identified as intending to breastfeed. Women who intend to breastfeed should be counseled regarding these possible complications, their temporary nature, prevention, and treatment. Mastitis is not an indication for breastfeeding termination; in fact, increased feedings and milk expression are considered treatment.26,27 Women who reported pain the first 3 weeks were more likely to stop breastfeeding than women who reported pain after the first 3 weeks. It is difficult to explain this finding; perhaps there are women who have pain during their entire breastfeeding career and yet continue to breastfeed because they are more pain-tolerant, have less severe or frequent pain than those who wean, or are more committed to breastfeeding.
Other clinical factors investigated were depression and daily sleep hours. Weaning was not associated with subjective depression. However, subjects did not undergo formal psychological testing as in the study that reported an association.24 The relationship between daily sleep hours and termination was not consistent, and likely not clinically significant.
The demographic risk factors related to breast-feeding termination in our study are similar to those previously reported,14,15,20,21,23,24 namely, younger maternal age and lower educational level. Investigations of parity have been inconsistent.16,28 We found no association of weaning with parity. Prior breastfeeding experience has been reported as improving breastfeeding rates15,28; our results are consistent with those findings, but not significantly so. All subjects had access to prenatal breastfeeding education and postnatal breastfeeding support, which may have diminished the differences between women with breastfeeding experience and those without experience.20
Michigan and Nebraska women who pumped or bottle-fed during weeks 4 through 12 were significantly less likely to terminate breastfeeding. In contrast, Michigan women who pumped or bottle-fed during the first 3 weeks postpartum were more likely to terminate even after controlling for pain and mastitis. A commitment to exclusive breastfeeding may be necessary in the early postpartum period for long-term success.15,19 To our knowledge, the seemingly protective effect associated with pumping and bottle-feeding after the first 3 weeks has not been previously reported.
Breastfeeding 6 or fewer times per day and feedings of 10 minutes or less were associated with termination during the first 3 weeks. Other studies also indicate that the ratio of breast to bottle feedings is important for long-term success. Feinstein and colleagues15 found that more than one daily bottle of formula supplementation was associated with shorter breastfeeding duration, which was minimized if there were 7 or more breastfeedings per day. Another study found no weaning difference between women who offered their infant only one bottle daily during weeks 2 through 6 and a bottle-avoiding group.17
The most frequent reasons given for termination were similar to those reported by others, namely, insufficient milk supply and return to work.11-15,21,22 Insufficient milk supply was a more common reason in the first few weeks after birth; return to work became an increasingly common reason after week 6.
We were unable to examine the role of pacifiers or smoking in breastfeedng termination because pacifier information was not collected and there were too few smokers for meaningful analysis. Smoking has been consistently reported as associated with early cessation.15,20,29,30 Although pacifier use does not appear to be directly related,31,32 it has been proposed as a marker for breastfeeding problems. The homogeneity of the sample limits our ability to make generalizations regarding other populations, such as women of color. However, the large sample size and the similarity of termination risk factors between 2 different populations of women lend confidence to our conclusions. As we did not assess mothers’ intentions, some of the variables found associated with termination might be intentional activities of weaning rather than risk factors for termination. The significant difference in termination risk between the sites also may be related to mothers’ intentions or level of commitment. The Michigan women may have intended to breastfeed longer from the outset. The Michigan recruitment site was an alternative birthing center. Women being delivered there may be more persistent in their breast-feeding efforts. Both sites provided access to breast-feeding support personnel, but the Michigan women, as a group, may have been more motivated to continue.
Our results provide clinically useful information. Additional support may be needed for younger and less educated women. Special efforts should be made for early diagnosis and treatment of mastitis and breast pain, particularly during the first 3 weeks. Exclusive breastfeeding without bottle supplementation should be recommended for the first 3 weeks, with at least 7 feedings per day. Each feeding should preferably last more than 10 minutes.
These results should also reassure breastfeeding women and their providers regarding the use of bottles. Bottle-feeding after 3 weeks does not appear to jeopardize breastfeeding success up to 12 weeks and may even improve it.
* Table W1 appears on the JFP Web site at www.jfponline.com.
Acknowledgments
This study was supported by National Institutes of Health grant #30866.
OBJECTIVE: To determine the demographic, behavioral, and clinical factors associated with breastfeeding termination in the first 12 weeks postpartum.
STUDY DESIGN: This was a prospective cohort study.
POPULATION: Breastfeeding women in Michigan and Nebraska were interviewed by telephone at 3, 6, 9, and 12 weeks postpartum or until breastfeeding termination.
OUTCOMES MEASURED: We measured associations of demographic, clinical, and breastfeeding variables with weaning during the first 12 weeks postpartum.
RESULTS: A total of 946 women participated; 75% breastfed until 12 weeks. Women older than 30 years and women with at least a bachelor’s degree were more likely to continue breastfeeding in any given week. Mastitis, breast or nipple pain, bottle use, and milk expression in the first 3 weeks were all associated with termination. Beyond 3 weeks, women who expressed breast milk were 75% less likely to discontinue breastfeeding than women who did not. Women who used a bottle for some feedings during weeks 4 to 12 were 98% less likely to discontinue breastfeeding than women who did not use a bottle. "Not enough milk" was the most common reason given for termination in weeks 1 through 3 (37%) and weeks 4 through 6 (35%); “return to work” was the most common reason given in weeks 7 through 9 (53%) and weeks 10 through 12 (58%).
CONCLUSIONS: Younger women and less educated women need additional support in their breastfeeding efforts. Counseling and assistance should be provided to women with pain and mastitis. Exclusive breastfeeding for the first 3 weeks should be recommended. After the first 3 weeks, bottles and manual expression are not associated with weaning and may improve the likelihood of continuing breastfeeding, at least until 12 weeks.
- Younger and less educated women may need extra support for long-term breastfeeding success.
- Exclusive breastfeeding for the first 3 weeks decreases the risk of early weaning. At least 7 daily feedings of 10 or more minutes per feeding are recommended.
- The use of bottles and manual expression of milk after 3 weeks does not increase the risk of early weaning.
Family physicians are strongly encouraged to support and promote breastfeeding, the optimal form of infant nutrition.1 Despite its known benefits (fewer infant infections2-6 and decreased maternal risks of premenopausal breast cancer7 and post-menopausal hip fractures8), only 64% of mothers initiated breastfeeding in 19989 and only 29% of mothers fed their 6-month-old infant by breast, well below the Healthy People 2010 goal of 50% breastfeeding at 6 months.10 Clearly, determining the factors that influence breastfeeding beyond the early postpartum period would be beneficial.
Returning to work is a consistent risk factor for weaning.11-14 The impact of early bottle-feeding on the duration of breastfeeding has been studied with less consistent results.15,20 Insufficient milk supply is a common subjective reason given for termination.15,19,21,22 Older women and those with a higher level of education are at less risk of early breastfeeding termination.9,11,15,16,21,23,24
Few investigators have described how breastfeeding patterns may affect breastfeeding duration. Little is known about the effects of timing, frequency, and duration of individual breastfeedings, or the roles of breast pain and infection, sleep, and manual expression on early weaning. We studied women who indicated their intent to breastfeed prenatally to identify demographic factors and breastfeeding patterns associated with weaning in the first 12 weeks postpartum.
Methods
Population
We interviewed breastfeeding women by telephone at 3, 6, 9, and 12 weeks postpartum to investigate lactation mastitis risk factors and predictors of weaning. Pregnant women intending to breastfeed were recruited from 2 geographic sites between June 1994 and January 1998. In suburban Detroit, Michigan, women attending orientation at a freestanding birthing center were asked to participate. In Omaha, Nebraska, women at a single large company were recruited when applying for maternity leave.
Data collection
During the computer-assisted interview, subjects were asked to recall each of the previous 3 weeks. The initial interview, which collected demographic information, typically lasted 15 to 20 minutes; subsequent interviews were shorter. The survey addressed breastfeeding practices and recent health events. Exclusive breastfeeders were women who fed their infants only by breast. We did not collect information on pacifiers; therefore, exclusively breastfed infants may have also received pacifiers. Women who manually expressed or used a device to assist in expression were classified as “pumping” their breasts. Respondents were asked if they had bottle-fed the infant; they were not asked about bottle contents or volume.
Subjects were queried on potential difficulties including breast or nipple pain while nursing, nipple cracks, and mastitis (diagnosed by a health care provider), as well as other health problems and behaviors. Subjects who had stopped breastfeeding in the previous 3 weeks were asked when and why, given a list of possible explanations and an open-ended opportunity. Respondents could provide multiple reasons for termination.
Data analysis
Kaplan-Meier estimates describe the distribution of weaning times for the 2 sites. A log-rank test was used to assess group differences. Relationships between demographic factors and time of weaning were assessed by Cox regression analysis. Discrete survival analysis was used to determine whether variables measured on a weekly basis were related to breastfeeding cessation. Hazard ratios describe the association of the exposures between women who stopped breastfeeding at a given time and those who continued. Because breastfeeding cessation was a rare event in later weeks of the study, as were certain clinical or behavioral breastfeeding factors, weeks 4-12 were collapsed into a single interval. Two variables, number of daily feedings and duration of each feeding, were examined only in the first 3 weeks because the information was often missing beyond 3 weeks. All analyses were performed using the Statistical Package for the Social Sciences.25
Results
Description of subjects
A total of 1057 women agreed to be contacted. Of those, 946 (89.5%) participated in at least 1 interview. Of the 111 women who did not participate, 11 refused and 100 could not be located. Six hundred fifty-eight (69.6%) women completed all 4 interviews. The 56 women who entered the study at week 6 because they could not be reached for the first interview were similar in all factors to women who entered earlier. Of the 946, 711 (75.2%) were from Michigan and 235 (24.8%) were from Nebraska.
Subjects from Michigan were significantly more likely than those from Nebraska to be older than 30 years (52.0% vs 38.3%), have at least a bachelor’s degree (62.9% vs 48.5%), have 3 or more children (38.5% vs 19.6%), and have had a vaginal delivery (99.6% vs 77.0%) (Table W1).* The groups were similar in race, household income, and marital status.
Demographic factors
A total of 673 women (71.1%) continued breastfeeding until 12 weeks; 28% were exclusive breastfeeders. Michigan women were more likely to breastfeed at weeks 2 through 12 than their Nebraskan counterparts (P < .0001, Figure). A college degree was associated with 40% less weaning (Table 1). Age and annual household income were directly related to continued breastfeeding at both sites. Number of children in the household was not associated with termination. Previous breastfeeding experience showed a nonsignificant but consistent trend toward lower weaning risk.
TABLE 1
Relationships of demographics and other characteristics with time to weaning, by site
| Characteristic | Michigan women HR* (95% CI) | Nebraska women HR* (95% CI) |
|---|---|---|
| Older than 30 years | 0.5 (0.3,0.8) | 0.7 (0.5, 1.1) |
| BA/BS or higher | 0.6 (0.4, 0.9) | 0.6 (0.4, 0.8) |
| Number of children in household | ||
| 1 | 1.0 | 1.0 |
| 2 | 1.0 (0.6, 1.6) | 0.7 (0.5, 1.2) |
| 3 or more | 0.6 (0.4, 1.0) | 0.9 (0.6, 1.5) |
| Household income ≥ $50,000 | 0.8 (0.5, 1.3) | 0.7 (0.5, 1.0) |
| Breastfed previously | 0.7 (0.5, 1.1) | 0.7 (0.5, 1.1) |
| Nonvaginal birth | † | 0.9 (0.6, 1.4) |
| NOTE: Bold numbers are significant at P < .05. | ||
| HR denotes hazard ratio; CI, confidence interval; BA, bachelor of arts degree; BS, bachelor of science degree. | ||
| *A hazard ratio of <1 indicates that subjects with this characteristic were less likely to wean during the 12 weeks. Unless otherwise noted, the referent group is the converse (eg, age < 30 years is the referent group for those older than 30 years). | ||
| †Too few observations to provide meaningful results. | ||
FIGURE
Probability of breastfeeding, by site, by postpartum week
Clinical and behavioral factors
Because time to weaning differed significantly by site, the survival analyses of clinical and behavioral factors were performed separately for Michigan and Nebraska and controlled for education, age, and previous breastfeeding experience.
During the first 3 weeks, Michigan women with mastitis were nearly 6 times more likely than Michigan women without mastitis to stop breast-feeding in the week of diagnosis (Table 2). Women from Nebraska showed nonsignificant results in the same direction in weeks 4 to 12. (No women from Nebraska with mastitis terminated during weeks 1 through 3.) Although nipple sores and cracks were not associated with weaning, breast pain was associated with weaning. For each day of pain in the first 3 weeks, there was a 10% increase in risk of cessation among Michigan women and a 26% increase among Nebraska women. The association between pain and weaning in weeks 4 through 12 is less clear. In these later weeks, women who reported pain were unexpectedly 75% to 80% more likely to continue breastfeeding than women who did not report pain, yet for Nebraska women the number of days with pain remained significantly associated with breastfeeding cessation.
Subjective depression and breastfeeding cessation were not related. The association between daily sleep and weaning varied by site. During weeks 4 through 12, Michigan women with more daily sleep were less likely to terminate. An opposite, but marginally significant trend, was observed for Nebraska women. Weaning was not associated with outside household help. Nonvaginal birth was not associated with weaning for Nebraska women. (There were only 2 cesarean sections in the Michigan group.)
Michigan women who expressed breast milk during the first 3 weeks were twice as likely to stop breastfeeding as those who did not pump. During the same period, Michigan women who used a bottle for some feedings were 9 times more likely to wean than nonbottle users. Respondents in Nebraska showed similar nonsignificant trends in the first 3 weeks. By contrast, during weeks 4 through 12, both Nebraska and Michigan women who pumped were about 75% less likely to wean, while women who used a bottle for some feedings were 98% less likely to stop breastfeeding.
Breast milk expression increased gradually over time, from 30% of women pumping an average of 3 times per day in the first 3 weeks to 45% of women pumping 5 times per day in the last 3 weeks. To determine if pumping and bottle-feeding had an effect independent of pain or mastitis on weaning in the first 3 weeks, we performed additional analyses controlling for pain, cracks and sores, and mastitis in the same week. The results were similar to those presented in Table 2. Michigan women who pumped were 3 times more likely to wean than those who did not pump (hazard ratio [HR] = 3.0, 95% confidence interval [CI], 1.3 - 6.7), while for Nebraska women there was no association between pumping and weaning (HR = 0.6, 95% CI, 0.3 - 1.5). Bottle-feeding was again significantly associated with weaning in weeks 1 through 3 for Michigan women (HR = 10.9, 95% CI, 4.5 - 26.7) and not associated in Nebraskans (HR = 0.8, 95% CI, 0.4 - 2.0).
Duration and frequency of feedings were investigated as weaning risk factors. There appeared to be a threshold for both variables during the first 3 weeks in Michigan women. Michigan women who breastfed less than 10 minutes per feeding were nearly 5 times more likely to stop breastfeeding than women who breastfed longer. Michigan women who breastfed 6 or fewer times per day were 8 times more likely to stop than those who breastfed more often. Results for Nebraska women fell in the same direction but were not statistically significant.
TABLE 2
Relationships of clinical and behavioral factors to breastfeeding cessation in the same week, adjusted for mother’s age, education, and previous breastfeeding experience
| Variable | Week | Michigan women HR (95% CI) | Nebraska women HR (95% CI) |
|---|---|---|---|
| Mastitis | 1 - 3 | 5.7 (1.3 - 25.9) | ‡ |
| 4 - 12 | ‡ | 2.1 (0.3 - 17.4) | |
| Engorgement | 1 - 3 | 0.6 (0.2 - 1.5) | 0.8 (0.3 - 2.1) |
| 4 - 12 | ‡ | 3.2 (0.6 - 15.8) | |
| Nipple sores/cracks | 1 - 3 | 1.1 (0.4 - 2.6) | 0.9 (0.4 - 2.3) |
| 4 - 12 | 2.6 (0.8 - 8.5) | 2.9 (0.8 - 10.7) | |
| Any pain † | 1 - 3 | 14.7 (6.8 - 32.0)§ | 9.1 (3.9 - 21.2)† |
| 4 - 12 | 0.3 (0.1 - 0.7) | 0.2 (0.1 - 0.5)† | |
| Days with pain* | 1 - 3 | 1.1 (1.0 - 1.2) | 1.3 (1.0 - 1.5) |
| 4 - 12 | 1.1 (1.0 - 1.2) | 1.1 (1.0 - 1.2) | |
| Returned to work | 1 - 3 | 0.4 (0.1 - 3.0) | ‡ |
| 4 - 12 | 2.1 (1.1 - 4.0) | 0.8 (0.4 - 1.7) | |
| Depressed | 1 - 3 | 0.9 (0.3 - 3.0) | 1.0 (0.4 - 2.6) |
| 4 - 12 | 0.9 (0.4 - 2.2) | 1.3 (0.6 - 2.7) | |
| Daily sleep hours | 1 - 3 | 0.9 (0.7 - 1.1) | 0.9 (0.8 - 1.2) |
| 4 - 12 | 0.7 (0.5 - 0.9) | 1.2 (1.0 - 1.5) | |
| Outside household help | 1 - 3 | 2.0 (0.8 - 4.8) | 0.9 (0.4 - 2.1) |
| 4 - 12 | 0.7 (0.3 - 2.6) | 0.7 (0.2 - 2.1) | |
| Pumping | 1 - 3 | 2.2 (1.1 - 4.6) | 1.3 (0.6 - 2.5) |
| 4 - 12 | 0.2 (0.1 - 0.5)§ | 0.3 (0.1 - 0.5) § | |
| Bottle feeding | 1 - 3 | 9.5 (4.3 - 21.0) § | 1.8 (0.9 - 3.5) |
| 4 - 12 | 0.03 (0.003 - 0.2) § | 0.02 (0.004 - 0.1) § | |
| Minutes per feeding | 1 - 3 | 1.0 (0.9, 1.0) | 1.1 (1.0, 1.1) |
| Less than 10 minutes per feeding | 1 - 3 | 4.8 (1.7, 13.4) | 2.2 (0.6, 8.1) |
| Feedings per day | 1 - 3 | 0.7 (0.6, 0.8) § | 0.9 (0.8, 1.1) |
| Less than 7 feedings/day | 1 - 3 | 8.1 (3.4, 19.2) § | 1.8 (0.7, 4.6) |
| NOTE: Bold numbers significant at P = .05 or less; those marked with § are significant at P = .001 or less. | |||
| HR denotes hazard ratio; CI, confidence interval. | |||
| *Subjects answered affirmatively to any of the following types of pain: pain when latching on, pain while nursing, pain when not nursing. | |||
| † Measured in 3-week periods. | |||
| ‡ Indicates there were too few observations to provide meaningful results; for example, there were no Nebraska women who had mastitis and stopped breastfeeding in the same week during weeks 1-3. | |||
Subjective factors
At each interview, women who had stopped breastfeeding in the previous 3 weeks were asked why they had made that decision. Most women (75%) provided only one reason. At the first interview, insufficient milk supply (37.3%) and breast pain or mastitis (32.9%) were the most common reasons for termination (Table 3). Insufficient milk supply was the reason most often given (35.0%) during weeks 4 through 6. At both weeks 9 and 12, return to work was the reason given most often (53.1% and 58.3%, respectively).
TABLE 3
Percentage of women citing given reason for termination of breastfeeding
| Week 3 | Week 6 | Week 9 | Week 12 | |
|---|---|---|---|---|
| Reason | (n = 67) | (n = 60) | (n = 32) | (n = 36) |
| Insufficient milk supply | 37.3 | 35.0 | 25.0 | 13.9 |
| Inconvenient | 17.9 | 25.0 | 21.9 | 33.3 |
| Returned to work | 4.5 | 31.7 | 53.1 | 58.3 |
| Breast pain or infection | 32.9 | 23.3 | 0 | 5.6 |
| Baby stopped nursing | 7.5 | 5.0 | 3.1 | 11.1 |
| Other | 22.4 | 18.3 | 3.1 | 5.6 |
| NOTE: Percentages total more than 100% because respondents could cite multiple reasons. | ||||
Discussion
Mastitis, pain, and days with pain in the first 3 weeks were important clinical factors associated with breastfeeding cessation in this cohort of women who prenatally self-identified as intending to breastfeed. Women who intend to breastfeed should be counseled regarding these possible complications, their temporary nature, prevention, and treatment. Mastitis is not an indication for breastfeeding termination; in fact, increased feedings and milk expression are considered treatment.26,27 Women who reported pain the first 3 weeks were more likely to stop breastfeeding than women who reported pain after the first 3 weeks. It is difficult to explain this finding; perhaps there are women who have pain during their entire breastfeeding career and yet continue to breastfeed because they are more pain-tolerant, have less severe or frequent pain than those who wean, or are more committed to breastfeeding.
Other clinical factors investigated were depression and daily sleep hours. Weaning was not associated with subjective depression. However, subjects did not undergo formal psychological testing as in the study that reported an association.24 The relationship between daily sleep hours and termination was not consistent, and likely not clinically significant.
The demographic risk factors related to breast-feeding termination in our study are similar to those previously reported,14,15,20,21,23,24 namely, younger maternal age and lower educational level. Investigations of parity have been inconsistent.16,28 We found no association of weaning with parity. Prior breastfeeding experience has been reported as improving breastfeeding rates15,28; our results are consistent with those findings, but not significantly so. All subjects had access to prenatal breastfeeding education and postnatal breastfeeding support, which may have diminished the differences between women with breastfeeding experience and those without experience.20
Michigan and Nebraska women who pumped or bottle-fed during weeks 4 through 12 were significantly less likely to terminate breastfeeding. In contrast, Michigan women who pumped or bottle-fed during the first 3 weeks postpartum were more likely to terminate even after controlling for pain and mastitis. A commitment to exclusive breastfeeding may be necessary in the early postpartum period for long-term success.15,19 To our knowledge, the seemingly protective effect associated with pumping and bottle-feeding after the first 3 weeks has not been previously reported.
Breastfeeding 6 or fewer times per day and feedings of 10 minutes or less were associated with termination during the first 3 weeks. Other studies also indicate that the ratio of breast to bottle feedings is important for long-term success. Feinstein and colleagues15 found that more than one daily bottle of formula supplementation was associated with shorter breastfeeding duration, which was minimized if there were 7 or more breastfeedings per day. Another study found no weaning difference between women who offered their infant only one bottle daily during weeks 2 through 6 and a bottle-avoiding group.17
The most frequent reasons given for termination were similar to those reported by others, namely, insufficient milk supply and return to work.11-15,21,22 Insufficient milk supply was a more common reason in the first few weeks after birth; return to work became an increasingly common reason after week 6.
We were unable to examine the role of pacifiers or smoking in breastfeedng termination because pacifier information was not collected and there were too few smokers for meaningful analysis. Smoking has been consistently reported as associated with early cessation.15,20,29,30 Although pacifier use does not appear to be directly related,31,32 it has been proposed as a marker for breastfeeding problems. The homogeneity of the sample limits our ability to make generalizations regarding other populations, such as women of color. However, the large sample size and the similarity of termination risk factors between 2 different populations of women lend confidence to our conclusions. As we did not assess mothers’ intentions, some of the variables found associated with termination might be intentional activities of weaning rather than risk factors for termination. The significant difference in termination risk between the sites also may be related to mothers’ intentions or level of commitment. The Michigan women may have intended to breastfeed longer from the outset. The Michigan recruitment site was an alternative birthing center. Women being delivered there may be more persistent in their breast-feeding efforts. Both sites provided access to breast-feeding support personnel, but the Michigan women, as a group, may have been more motivated to continue.
Our results provide clinically useful information. Additional support may be needed for younger and less educated women. Special efforts should be made for early diagnosis and treatment of mastitis and breast pain, particularly during the first 3 weeks. Exclusive breastfeeding without bottle supplementation should be recommended for the first 3 weeks, with at least 7 feedings per day. Each feeding should preferably last more than 10 minutes.
These results should also reassure breastfeeding women and their providers regarding the use of bottles. Bottle-feeding after 3 weeks does not appear to jeopardize breastfeeding success up to 12 weeks and may even improve it.
* Table W1 appears on the JFP Web site at www.jfponline.com.
Acknowledgments
This study was supported by National Institutes of Health grant #30866.
1. American Academy of Family Physicians. Policies on Health Issues: Infant Health. URL: http://aafp.org/policy/issues/i3.html
2. Beaudry M, Dufour R, Marcoux S. Relation between infant feeding and infections during the first six months of life. J Pediatr 1995;126:696-702.
3. Dewey K, Heinig M, Nommsen-Rivers LA. Differences in morbidity between breast-fed and formula-fed infants. J Pediatr 1995;126:191-7.
4. Duncan B, Ey J, Holberg CJ, Wright AL, Martinez FD, Taussig LM. Exclusive breast-feeding for at least 4 months protects against otitis media. Pediatrics 1993;91:867-72.
5. Raisler J, Alexander C, O’Campo P. Breast-feeding and infant illness: a dose-reponse relationship? Am J Public Health 2000;90:1478-9.
6. Hanson LA. Breastfeeding provides passive and likely long-lasting active immunity. Ann Allergy Asthma Immunol 1998;81:523-33.
7. Newcomb P, Storer B, Longnecker M, et al. Lactation and a reduced risk of premenopausal breast cancer. N Engl J Med 1994;330:81-7.
8. Cumming RG, Klinieberg RJ. Breastfeeding and other reproductive factors and the risk of hip fractures in elderly women. Int J Epidemiol 1993;22:884-91.
9. Mother’s Survey, Ross Products Division, Abbot Laboratories, Inc. Columbus OH, 1998.
10. U.S. Department of Health and Human Services. Healthy People 2010. (Conference edition in 2 volumes.) Washington, DC: January 2000.
11. Gielen AC, Faden RR, O’Campo P, Brown CH, Paige DM. Maternal employment during the early postpartum period: effects on initiation and continuation of breastfeeding. Pediatrics 1991;87:298-305.
12. Fein SB, Roe B. The effect of work status on initiation and duration of breast-feeding. Am J Public Health 1998;88:1042-6.
13. Kurinij N, Shiono PH, Ezrine SF, Rhoads GG. Does maternal employment affect breast-feeding? Am J Public Health 1989;79:1247-50.
14. Kearney MH, Cronenwett L. Breastfeeding and employment. J Obstet Gynecol Neonatal Nurs 1991;20:471-80.
15. Feinstein JM, Berkelhamer JE, Gruszka ME, Wong CA, Carey AE. Factors related to early termination of breast-feeding in an urban population. Pediatrics 1986;78:210-5.
16. Ryan AS, Wysong JL, Martinez GA, Simon SD. Duration of breast-feeding patterns established in the hospital. Clin Pediatr 1990;29:99-107.
17. Cronenwett L, Strukel T, Kearney M, et al. Single daily bottle use in the early weeks postpartum and breast-feeding outcomes. Pediatrics 1992;90:760-6.
18. Gray-Donald K, Kramer MS, Munday S, Leduc DG. Effect of formula supplementation in the hospital on the duration of breast-feeding; a controlled clinical trial. Pediatrics 1985;75:514-8.
19. Hill PD, Humenick SS, Brennan ML, Woolley D. Does early supplementation affect long-term breastfeeding? Clin Pediatr 1997;June:345-350.
20. Wright HJ, Walker PC. Prediction of duration of breast feeding in primiparas. J Epidemiol Comm Health 1983;37:89-94.
21. Hawkins LM, Nichols FH, Tanner JL. Predictors of the duration of breastfeeding in low-income women. Birth 1987;14:204-9.
22. Hill PD, Aldag JC. Insufficient milk supply among black and white breast-feeding mothers. Res Nurs Health 1993;16:203-11.
23. Kurinij N, Shiono PH, Rhoads GG. Breast-feeding incidence and duration in black and white women. Pediatrics 1988;81:365-71.
24. Cooper PJ, Murray L, Stein A. Psychosocial factors associated with the early termination of breast-feeding. J Psychosom Res 1993;37:171-6.
25. Statistical Package for the Social Sciences. Chicago, IL: SPSS Inc; 1998.
26. Marshall B, Hepper J. Zirbel. Sporadic mastitis: an infection that need not interrupt lactation. JAMA 1975;233:1377-9.
27. Lawrence R. Mastitis. In: Breastfeeding: a guide for the medical profession. 4th ed. St. Louis: Mosby; 1994.
28. Hill PD, Humenick SS, Argubright T, Aldag JC. Effects of parity and weaning practices on breastfeeding duration. Public Health Nurs 1997;14:227-34.
29. Hill PD, Aldag JC. Smoking and breastfeeding status. Res Nurs Health 1996;19:125-32.
30. Woodward A, Hand K. Smoking and reduced duration of breast-feeding. Med J Australia 1988;148:477-8.
31. Victora CG, Behague DP, Barros FC, Olinto MT, Weiderpass E. Pacifier use and short breastfeeding duration: cause, consequence, or coincidence. Pediatrics 1997;99:445-3.
32. Howard CR, Howard FM, Lanphear B, deBlieck EA, Eberly S, Lawrence RA. The effects of early pacifier use on breastfeeding duration? Pediatrics 1999;103:E33.-
1. American Academy of Family Physicians. Policies on Health Issues: Infant Health. URL: http://aafp.org/policy/issues/i3.html
2. Beaudry M, Dufour R, Marcoux S. Relation between infant feeding and infections during the first six months of life. J Pediatr 1995;126:696-702.
3. Dewey K, Heinig M, Nommsen-Rivers LA. Differences in morbidity between breast-fed and formula-fed infants. J Pediatr 1995;126:191-7.
4. Duncan B, Ey J, Holberg CJ, Wright AL, Martinez FD, Taussig LM. Exclusive breast-feeding for at least 4 months protects against otitis media. Pediatrics 1993;91:867-72.
5. Raisler J, Alexander C, O’Campo P. Breast-feeding and infant illness: a dose-reponse relationship? Am J Public Health 2000;90:1478-9.
6. Hanson LA. Breastfeeding provides passive and likely long-lasting active immunity. Ann Allergy Asthma Immunol 1998;81:523-33.
7. Newcomb P, Storer B, Longnecker M, et al. Lactation and a reduced risk of premenopausal breast cancer. N Engl J Med 1994;330:81-7.
8. Cumming RG, Klinieberg RJ. Breastfeeding and other reproductive factors and the risk of hip fractures in elderly women. Int J Epidemiol 1993;22:884-91.
9. Mother’s Survey, Ross Products Division, Abbot Laboratories, Inc. Columbus OH, 1998.
10. U.S. Department of Health and Human Services. Healthy People 2010. (Conference edition in 2 volumes.) Washington, DC: January 2000.
11. Gielen AC, Faden RR, O’Campo P, Brown CH, Paige DM. Maternal employment during the early postpartum period: effects on initiation and continuation of breastfeeding. Pediatrics 1991;87:298-305.
12. Fein SB, Roe B. The effect of work status on initiation and duration of breast-feeding. Am J Public Health 1998;88:1042-6.
13. Kurinij N, Shiono PH, Ezrine SF, Rhoads GG. Does maternal employment affect breast-feeding? Am J Public Health 1989;79:1247-50.
14. Kearney MH, Cronenwett L. Breastfeeding and employment. J Obstet Gynecol Neonatal Nurs 1991;20:471-80.
15. Feinstein JM, Berkelhamer JE, Gruszka ME, Wong CA, Carey AE. Factors related to early termination of breast-feeding in an urban population. Pediatrics 1986;78:210-5.
16. Ryan AS, Wysong JL, Martinez GA, Simon SD. Duration of breast-feeding patterns established in the hospital. Clin Pediatr 1990;29:99-107.
17. Cronenwett L, Strukel T, Kearney M, et al. Single daily bottle use in the early weeks postpartum and breast-feeding outcomes. Pediatrics 1992;90:760-6.
18. Gray-Donald K, Kramer MS, Munday S, Leduc DG. Effect of formula supplementation in the hospital on the duration of breast-feeding; a controlled clinical trial. Pediatrics 1985;75:514-8.
19. Hill PD, Humenick SS, Brennan ML, Woolley D. Does early supplementation affect long-term breastfeeding? Clin Pediatr 1997;June:345-350.
20. Wright HJ, Walker PC. Prediction of duration of breast feeding in primiparas. J Epidemiol Comm Health 1983;37:89-94.
21. Hawkins LM, Nichols FH, Tanner JL. Predictors of the duration of breastfeeding in low-income women. Birth 1987;14:204-9.
22. Hill PD, Aldag JC. Insufficient milk supply among black and white breast-feeding mothers. Res Nurs Health 1993;16:203-11.
23. Kurinij N, Shiono PH, Rhoads GG. Breast-feeding incidence and duration in black and white women. Pediatrics 1988;81:365-71.
24. Cooper PJ, Murray L, Stein A. Psychosocial factors associated with the early termination of breast-feeding. J Psychosom Res 1993;37:171-6.
25. Statistical Package for the Social Sciences. Chicago, IL: SPSS Inc; 1998.
26. Marshall B, Hepper J. Zirbel. Sporadic mastitis: an infection that need not interrupt lactation. JAMA 1975;233:1377-9.
27. Lawrence R. Mastitis. In: Breastfeeding: a guide for the medical profession. 4th ed. St. Louis: Mosby; 1994.
28. Hill PD, Humenick SS, Argubright T, Aldag JC. Effects of parity and weaning practices on breastfeeding duration. Public Health Nurs 1997;14:227-34.
29. Hill PD, Aldag JC. Smoking and breastfeeding status. Res Nurs Health 1996;19:125-32.
30. Woodward A, Hand K. Smoking and reduced duration of breast-feeding. Med J Australia 1988;148:477-8.
31. Victora CG, Behague DP, Barros FC, Olinto MT, Weiderpass E. Pacifier use and short breastfeeding duration: cause, consequence, or coincidence. Pediatrics 1997;99:445-3.
32. Howard CR, Howard FM, Lanphear B, deBlieck EA, Eberly S, Lawrence RA. The effects of early pacifier use on breastfeeding duration? Pediatrics 1999;103:E33.-