User login
SAN DIEGO – A variety of factors, some of them modifiable, increase the risk of recurrence of Clostridium difficile infection among inpatients, researchers reported at IDWeek.
The team retrospectively studied 4,200 adult inpatients who had an initial C. difficile infection, defined as a positive toxin assay at hospital admission in the setting of unformed stools. Overall, 10% went on to experience a recurrence within 6 weeks.
Results showed that patients had a more than one-third increase in recurrence risk if they were started on a new gastric acid–suppressing agent during treatment of their initial infection, and a near tripling of the risk if they were started on a high-risk antibiotic after completing treatment.
"Recognizing both modifiable and nonmodifiable recurrent C. difficile infection risk factors may help clinicians tailor the therapy for the initial episode of C. difficile infection more precisely," presenting author Dr. Erik R. Dubberke commented.
"Some characteristics, such as age, were not modifiable, but there were several modifiable exposures, such as gastric acid suppression as well as antimicrobial exposures during as well as after the treatment for the initial C. difficile infection," he said. "Reducing these exposures may help decrease the risk of developing future episodes of C. difficile infection." Dr. Dubberke is with the department of medicine at the Washington University in St. Louis.
Audience members inquired about the finer points of the investigation.
One attendee was "curious" about the elevated risk seen after receipt of intravenous vancomycin, "since this is a drug that doesn’t get into the stool at all." He wondered if perhaps other antibiotics given with vancomycin were actually at play.
Dr. Dubberke noted that multivariate analysis took this into consideration, and receipt of vancomycin after completing treatment was still a risk factor. "There are data to suggest that even intravenous vancomycin – though you don’t get adequate levels to treat C. difficile in the colon – can potentially get into the colon and affect the microbiome. So it’s possible there may be some direct causation," he said. "Conversely ... people who receive intravenous vancomycin tend to get other antibiotics. They also tend to be sicker patients, patients at increased risk for having drug-resistant organisms. So it is possible this is just a marker for recurrent C. difficile based on the patient characteristics."
Regarding whether severity of the initial infection affected recurrence risk, the research did not find an association on multivariate analysis with white count, new-onset renal dysfunction, baseline renal dysfunction, being in the ICU or being transferred to the ICU, or initiation of vasopressors, Dr. Dubberke explained. He speculated that lack of association was due in part to the competing risk of death.
"If a patient is very sick from C. difficile, they may die. Our [group] has demonstrated that you have an increased risk of death even after that initial episode is treated. So maybe that is why were not seeing [severity] as a risk for recurrent C. difficile."
Another attendee asked about the finding of elevated risk associated with gastric acid–suppressing medications. "[Have you] taken any practical steps at your hospital or in your health system to try to modify that risk factor because it’s medication that we clearly use and prescribe, and it’s questionable as to whether these prescriptions actually meet the indications ... " she said.
"We have not done anything in regard to interventions at this point based on the data," Dr. Dubberke replied.
The investigators identified patients having an initial C. difficile infection on admission to Barnes-Jewish Hospital, St. Louis, between 2003 and 2009, and classified those infections according to standard definitions as health care–onset infections; community-onset, health care facility–associated infections; or community-associated infections.
They classified antibiotics received as high risk (clindamycin, cephalosporins, and aminopenicillins), intravenous vancomycin, fluoroquinolones, and low risk (all others).
Study results shows that, compared with their peers who did not have a recurrence, patients who did were older and more likely to have diabetes, had higher levels of comorbidity, were more likely to have a community-onset, health care facility–associated initial infection, and were more likely to have been hospitalized in the past 60 days, Dr. Dubberke reported at the meeting, which is a the combined annual meeting of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society..
In multivariate analyses, patients were significantly more likely to have a recurrence of C. difficile if their initial infection was a community-onset, health care facility–associated infection as compared with a health care–onset infection (hazard ratio, 1.80) or they had at least two hospitalizations in the 60 days before that infection (HR, 1.40). Additionally, risk increased with age (HR, 1.01).
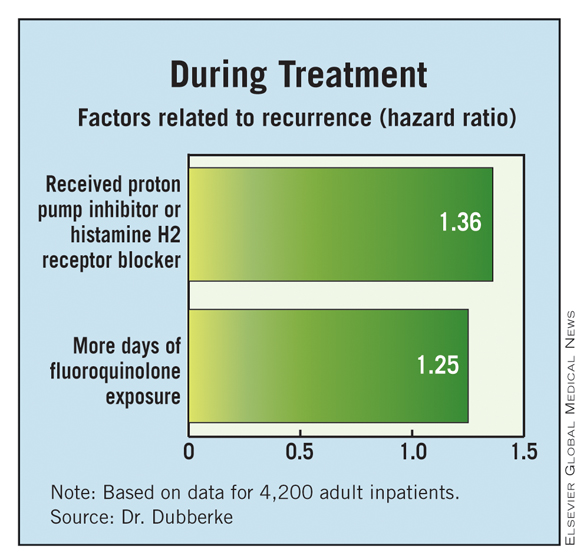
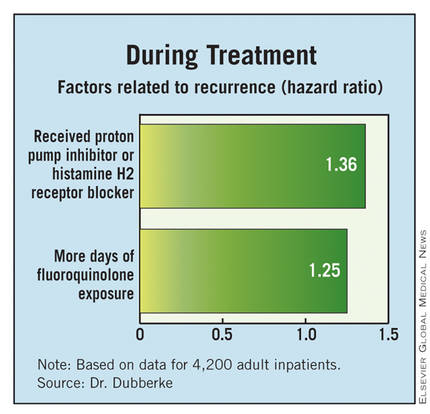
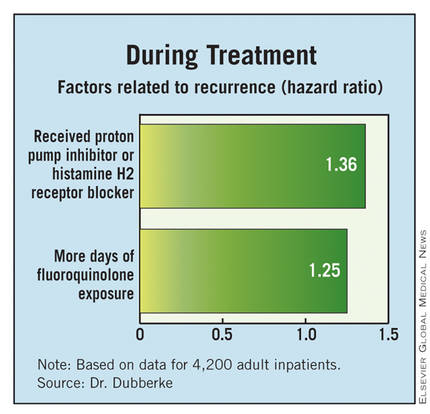
With respect to factors during the treatment of the initial infection, patients were more likely to have a recurrence if they received a new gastric acid–suppressing agent (a proton pump inhibitor or histamine H2 receptor blocker) (HR, 1.36) or had more days of fluoroquinolone exposure (1.24).
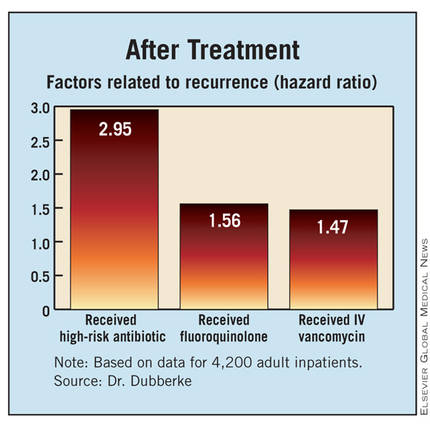
Finally, with respect to factors after completing treatment of the initial infection, patients were more likely to have a recurrence if they received a high-risk antibiotic (HR, 2.95), received a fluoroquinolone (HR, 1.56), or received intravenous vancomycin (HR, 1.45).
Discussing the study’s limitations, Dr. Dubberke noted that the investigators relied on the hospital database to identify cases of C. difficile recurrence. "We likely missed recurrences that were diagnosed and managed as outpatients," he acknowledged. "However, conversely, the recurrences that were identified were presumably more severe in that these patients ended up having another contact with our hospital, either in the emergency room" or through direct admission.
Dr. Dubberke disclosed that he has received research funding from Optimer Pharmaceuticals, ViroPharma, Merck, and Sanofi Pasteur, and that he has been a consultant to Optimer, Merck, Pfizer, and Sanofi Pasteur. The study was supported by Optimer.
SAN DIEGO – A variety of factors, some of them modifiable, increase the risk of recurrence of Clostridium difficile infection among inpatients, researchers reported at IDWeek.
The team retrospectively studied 4,200 adult inpatients who had an initial C. difficile infection, defined as a positive toxin assay at hospital admission in the setting of unformed stools. Overall, 10% went on to experience a recurrence within 6 weeks.
Results showed that patients had a more than one-third increase in recurrence risk if they were started on a new gastric acid–suppressing agent during treatment of their initial infection, and a near tripling of the risk if they were started on a high-risk antibiotic after completing treatment.
"Recognizing both modifiable and nonmodifiable recurrent C. difficile infection risk factors may help clinicians tailor the therapy for the initial episode of C. difficile infection more precisely," presenting author Dr. Erik R. Dubberke commented.
"Some characteristics, such as age, were not modifiable, but there were several modifiable exposures, such as gastric acid suppression as well as antimicrobial exposures during as well as after the treatment for the initial C. difficile infection," he said. "Reducing these exposures may help decrease the risk of developing future episodes of C. difficile infection." Dr. Dubberke is with the department of medicine at the Washington University in St. Louis.
Audience members inquired about the finer points of the investigation.
One attendee was "curious" about the elevated risk seen after receipt of intravenous vancomycin, "since this is a drug that doesn’t get into the stool at all." He wondered if perhaps other antibiotics given with vancomycin were actually at play.
Dr. Dubberke noted that multivariate analysis took this into consideration, and receipt of vancomycin after completing treatment was still a risk factor. "There are data to suggest that even intravenous vancomycin – though you don’t get adequate levels to treat C. difficile in the colon – can potentially get into the colon and affect the microbiome. So it’s possible there may be some direct causation," he said. "Conversely ... people who receive intravenous vancomycin tend to get other antibiotics. They also tend to be sicker patients, patients at increased risk for having drug-resistant organisms. So it is possible this is just a marker for recurrent C. difficile based on the patient characteristics."
Regarding whether severity of the initial infection affected recurrence risk, the research did not find an association on multivariate analysis with white count, new-onset renal dysfunction, baseline renal dysfunction, being in the ICU or being transferred to the ICU, or initiation of vasopressors, Dr. Dubberke explained. He speculated that lack of association was due in part to the competing risk of death.
"If a patient is very sick from C. difficile, they may die. Our [group] has demonstrated that you have an increased risk of death even after that initial episode is treated. So maybe that is why were not seeing [severity] as a risk for recurrent C. difficile."
Another attendee asked about the finding of elevated risk associated with gastric acid–suppressing medications. "[Have you] taken any practical steps at your hospital or in your health system to try to modify that risk factor because it’s medication that we clearly use and prescribe, and it’s questionable as to whether these prescriptions actually meet the indications ... " she said.
"We have not done anything in regard to interventions at this point based on the data," Dr. Dubberke replied.
The investigators identified patients having an initial C. difficile infection on admission to Barnes-Jewish Hospital, St. Louis, between 2003 and 2009, and classified those infections according to standard definitions as health care–onset infections; community-onset, health care facility–associated infections; or community-associated infections.
They classified antibiotics received as high risk (clindamycin, cephalosporins, and aminopenicillins), intravenous vancomycin, fluoroquinolones, and low risk (all others).
Study results shows that, compared with their peers who did not have a recurrence, patients who did were older and more likely to have diabetes, had higher levels of comorbidity, were more likely to have a community-onset, health care facility–associated initial infection, and were more likely to have been hospitalized in the past 60 days, Dr. Dubberke reported at the meeting, which is a the combined annual meeting of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society..
In multivariate analyses, patients were significantly more likely to have a recurrence of C. difficile if their initial infection was a community-onset, health care facility–associated infection as compared with a health care–onset infection (hazard ratio, 1.80) or they had at least two hospitalizations in the 60 days before that infection (HR, 1.40). Additionally, risk increased with age (HR, 1.01).
With respect to factors during the treatment of the initial infection, patients were more likely to have a recurrence if they received a new gastric acid–suppressing agent (a proton pump inhibitor or histamine H2 receptor blocker) (HR, 1.36) or had more days of fluoroquinolone exposure (1.24).
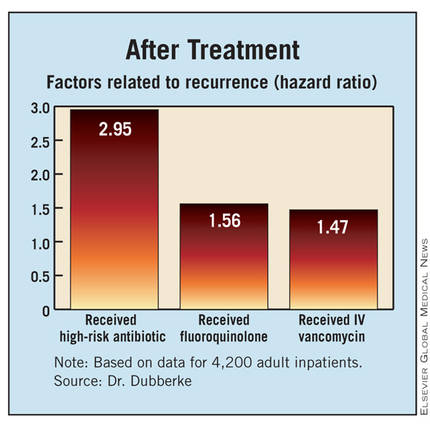
Finally, with respect to factors after completing treatment of the initial infection, patients were more likely to have a recurrence if they received a high-risk antibiotic (HR, 2.95), received a fluoroquinolone (HR, 1.56), or received intravenous vancomycin (HR, 1.45).
Discussing the study’s limitations, Dr. Dubberke noted that the investigators relied on the hospital database to identify cases of C. difficile recurrence. "We likely missed recurrences that were diagnosed and managed as outpatients," he acknowledged. "However, conversely, the recurrences that were identified were presumably more severe in that these patients ended up having another contact with our hospital, either in the emergency room" or through direct admission.
Dr. Dubberke disclosed that he has received research funding from Optimer Pharmaceuticals, ViroPharma, Merck, and Sanofi Pasteur, and that he has been a consultant to Optimer, Merck, Pfizer, and Sanofi Pasteur. The study was supported by Optimer.
SAN DIEGO – A variety of factors, some of them modifiable, increase the risk of recurrence of Clostridium difficile infection among inpatients, researchers reported at IDWeek.
The team retrospectively studied 4,200 adult inpatients who had an initial C. difficile infection, defined as a positive toxin assay at hospital admission in the setting of unformed stools. Overall, 10% went on to experience a recurrence within 6 weeks.
Results showed that patients had a more than one-third increase in recurrence risk if they were started on a new gastric acid–suppressing agent during treatment of their initial infection, and a near tripling of the risk if they were started on a high-risk antibiotic after completing treatment.
"Recognizing both modifiable and nonmodifiable recurrent C. difficile infection risk factors may help clinicians tailor the therapy for the initial episode of C. difficile infection more precisely," presenting author Dr. Erik R. Dubberke commented.
"Some characteristics, such as age, were not modifiable, but there were several modifiable exposures, such as gastric acid suppression as well as antimicrobial exposures during as well as after the treatment for the initial C. difficile infection," he said. "Reducing these exposures may help decrease the risk of developing future episodes of C. difficile infection." Dr. Dubberke is with the department of medicine at the Washington University in St. Louis.
Audience members inquired about the finer points of the investigation.
One attendee was "curious" about the elevated risk seen after receipt of intravenous vancomycin, "since this is a drug that doesn’t get into the stool at all." He wondered if perhaps other antibiotics given with vancomycin were actually at play.
Dr. Dubberke noted that multivariate analysis took this into consideration, and receipt of vancomycin after completing treatment was still a risk factor. "There are data to suggest that even intravenous vancomycin – though you don’t get adequate levels to treat C. difficile in the colon – can potentially get into the colon and affect the microbiome. So it’s possible there may be some direct causation," he said. "Conversely ... people who receive intravenous vancomycin tend to get other antibiotics. They also tend to be sicker patients, patients at increased risk for having drug-resistant organisms. So it is possible this is just a marker for recurrent C. difficile based on the patient characteristics."
Regarding whether severity of the initial infection affected recurrence risk, the research did not find an association on multivariate analysis with white count, new-onset renal dysfunction, baseline renal dysfunction, being in the ICU or being transferred to the ICU, or initiation of vasopressors, Dr. Dubberke explained. He speculated that lack of association was due in part to the competing risk of death.
"If a patient is very sick from C. difficile, they may die. Our [group] has demonstrated that you have an increased risk of death even after that initial episode is treated. So maybe that is why were not seeing [severity] as a risk for recurrent C. difficile."
Another attendee asked about the finding of elevated risk associated with gastric acid–suppressing medications. "[Have you] taken any practical steps at your hospital or in your health system to try to modify that risk factor because it’s medication that we clearly use and prescribe, and it’s questionable as to whether these prescriptions actually meet the indications ... " she said.
"We have not done anything in regard to interventions at this point based on the data," Dr. Dubberke replied.
The investigators identified patients having an initial C. difficile infection on admission to Barnes-Jewish Hospital, St. Louis, between 2003 and 2009, and classified those infections according to standard definitions as health care–onset infections; community-onset, health care facility–associated infections; or community-associated infections.
They classified antibiotics received as high risk (clindamycin, cephalosporins, and aminopenicillins), intravenous vancomycin, fluoroquinolones, and low risk (all others).
Study results shows that, compared with their peers who did not have a recurrence, patients who did were older and more likely to have diabetes, had higher levels of comorbidity, were more likely to have a community-onset, health care facility–associated initial infection, and were more likely to have been hospitalized in the past 60 days, Dr. Dubberke reported at the meeting, which is a the combined annual meeting of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society..
In multivariate analyses, patients were significantly more likely to have a recurrence of C. difficile if their initial infection was a community-onset, health care facility–associated infection as compared with a health care–onset infection (hazard ratio, 1.80) or they had at least two hospitalizations in the 60 days before that infection (HR, 1.40). Additionally, risk increased with age (HR, 1.01).
With respect to factors during the treatment of the initial infection, patients were more likely to have a recurrence if they received a new gastric acid–suppressing agent (a proton pump inhibitor or histamine H2 receptor blocker) (HR, 1.36) or had more days of fluoroquinolone exposure (1.24).
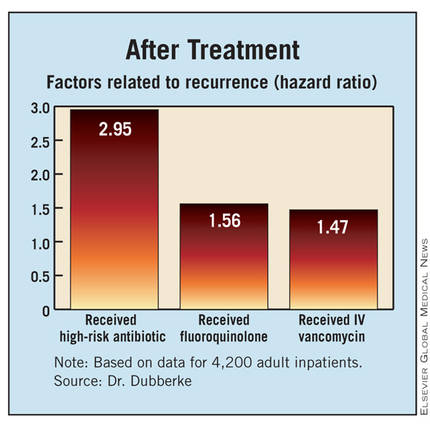
Finally, with respect to factors after completing treatment of the initial infection, patients were more likely to have a recurrence if they received a high-risk antibiotic (HR, 2.95), received a fluoroquinolone (HR, 1.56), or received intravenous vancomycin (HR, 1.45).
Discussing the study’s limitations, Dr. Dubberke noted that the investigators relied on the hospital database to identify cases of C. difficile recurrence. "We likely missed recurrences that were diagnosed and managed as outpatients," he acknowledged. "However, conversely, the recurrences that were identified were presumably more severe in that these patients ended up having another contact with our hospital, either in the emergency room" or through direct admission.
Dr. Dubberke disclosed that he has received research funding from Optimer Pharmaceuticals, ViroPharma, Merck, and Sanofi Pasteur, and that he has been a consultant to Optimer, Merck, Pfizer, and Sanofi Pasteur. The study was supported by Optimer.
AT IDWEEK
Major Finding: Risk factors for recurrence included starting gastric acid suppression during treatment of the initial infection (hazard ratio, 1.36) and receipt of a high-risk antibiotic after completing treatment (HR, 2.95).
Data Source: Results were taken from a retrospective cohort study of 4,200 adults having C. difficile infection on hospital admission
Disclosures: Dr. Dubberke disclosed that he has received research funding from and/or been a consultant for Optimer Pharmaceuticals, ViroPharma, Merck, Pfizer, and Sanofi Pasteur. The study was supported by Optimer.