User login
SAN FRANCISCO – An umbilical artery systolic-to-diastolic ratio of less than 3 as measured on weekly Doppler ultrasounds in a fetus with 30 weeks’ or more gestation and suspected intrauterine growth restriction suggests that the fetus probably is doing okay, Dr. Vickie A. Feldstein said.
That "ballpark guideline" is most helpful if physicians at your institution have agreed to use the umbilical artery systolic/diastolic (S/D) ratio as the parameter for assessing fetuses with intrauterine growth restriction (IUGR) and have agreed on which anatomical location is preferred for the ultrasound interrogation, so that there is some uniformity in how results are presented and interpreted, she said.
The recent Practice Bulletin No. 134 from the American College of Obstetricians and Gynecologists recommended in May 2013 that if the ultrasonographically estimated fetal weight is below the 10th percentile for gestational age, further evaluation should be considered, such as Doppler blood flow studies of the umbilical artery (Obstet. Gynecol. 2013;121:1122-33).
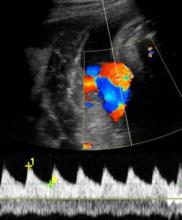
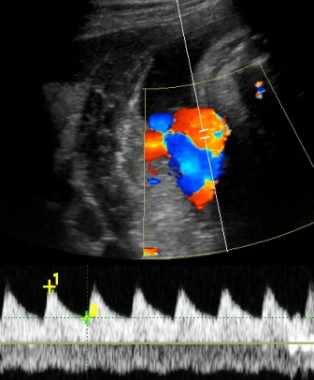
The medical literature describes several Doppler ultrasound parameters that could be used in suspected IUGR, including the umbilical artery S/D ratio, the resistance index, or the pulsatility index. They’re all about the same phenomenon, which is measuring resistance to perfusion in the placenta as reflected in the interrogation of the umbilical artery, Dr. Feldstein said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
"I think a report that includes all of them would make our heads spin," said Dr. Feldstein, professor of clinical radiology at the university. She and her colleagues use the S/D ratio, calculated by using calipers to measure the peak of systole on umbilical artery Doppler ultrasound and dividing that by the measure of end diastole.
"I don’t care how fast the flow actually is, I care about the character of the flow, the relative difference between systole and diastole," she said. The ratio reflects the status of placental circulation. It normally is high early in pregnancy and decreases as gestation advances, placental resistance decreases, and there is more forward flow during diastole.
If separate umbilical artery Doppler tracings yield discrepant S/D ratios, that may reflect normal variability or be due to changes in fetal heart rate. "A significant change in heart rate might change the S/D ratio quite a bit," she said. Or, an ultrasound filter set too low can produce noise in the tracing that might alter where you place the calipers.
The location along the umbilical cord that the sonographer samples also can affect measurements. The medical literature is full of suggestions about where to sample. Dr. Feldstein recommends sampling toward the placenta, if possible, which will reflect resistance to perfusion in the placenta.
"We’ve found the cord insertion, typically, so we know where to look," she said. "The farther away from the placenta you go, you’re adding resistance of the cord to your tracing."
She encouraged obstetricians to talk to the people who do Doppler at their institutions "to decide together how you want this done, how you want it reported, and what parameter you want used, so you don’t overwhelm yourselves with excess information."
If the S/D ratio is a bit above 3 in a third-trimester fetus with IUGR but there’s decent diastolic flow, "don’t sweat the small stuff," she suggested. As the S/D ratio goes higher and higher, however, placental insufficiency (and resistance) increases and forward flow decreases, and can become absent or even reversed end-diastolic flow.
An absence of diastolic flow is associated with a 60%-70% loss of vasculature, "a really significant abnormality in the placenta," she said. With reversed diastolic flow, the odds of perinatal death increase more than fivefold.
A recent study of 1,116 fetuses with IUGR showed that an abnormal umbilical artery Doppler ultrasound tracing (defined by pulsatility index or the absence or reversal of end-diastolic flow) was significantly associated with adverse outcomes irrespective of estimated fetal weight or abdominal circumference (Am. J. Obstet. Gynecol. 2013;208:e1-6 [doi: 10.1016/j.ajog.2013.02.007]).
When Dr. Feldstein sees an abnormal umbilical artery Doppler tracing, she samples the fetal middle cerebral artery by Doppler ultrasound. The middle cerebral artery S/D ratio should always be higher than the umbilical artery SD ratio, with a typical middle cerebral artery S/D ratio greater than 4 after 30 weeks’ gestation.
A fetus in trouble with IUGR will respond by lowering cerebral vascular resistance to maintain blood flow to its brain, decreasing the middle cerebral artery S/D ratio in what’s known as a "brain-sparing" wave form. Although there’s nothing that can be done for the fetus at this point, she said, it can be helpful to know that brain-sparing in growth-restricted fetuses was associated with increased risk for abnormal neurobehavioral outcomes in a controlled study of 126 preterm infants (Ultrasound Obstet. Gynecol. 2011;38:288-94).
"It’s a sign of distress," she said. Until recently, clinicians would follow that fetus carefully with various kinds of testing and watch for reverse diastolic flow in the umbilical artery, which is a sign of significant compromise, hypoxemia, and possible death. Today, a finding of brain-sparing next leads Dr. Feldstein to interrogate the ductus venosus in the liver, which is "the hardest to do, but it can be done," she said.
The ductus venosus flow should be phasic but continuous, in a pattern called the "a wave" reflecting forward, continuous flow even during right atrial contractions. If the flow reverses backward into the ductus venosus during right atrial contractions, that’s a sign of cardiac compromise, severe hypoxia, and right ventricular dysfunction, associated with high risk of morbidity and mortality.
Locating the ductus venosus for sampling can be tricky, in part because it is so close to hepatic veins, but if the ductus venosus flow is abnormal enough, there’s a shortcut that is easier to do: Sample the umbilical vein. Abnormal phasicity in umbilical vein pulsation may reflect ductus venosus flow reversal.
A previous study reported that the risk for perinatal mortality increased to nearly 6% with an elevated umbilical artery S/D ratio, to more than 11% with absent or reversed diastolic flow in the uterine artery, and to 39% with an abnormal ductus venosus wave form (Ultrasound Obstet. Gynecol. 2003;22:240-5). In a 2010 Cochrane Review of 18 studies that included more than 10,000 women with high-risk pregnancies, Doppler ultrasound was associated with a 29% reduction in the rate of perinatal deaths (1.2% with Doppler and 1.7% without); analysis showed that using Doppler on 203 high-risk pregnancies would avoid 1 perinatal death (Cochrane Database Syst. Rev. 2010 Jan. 20). "So, there’s a significant impact and not that much excess work," Dr. Feldstein said.
She reported having no financial disclosures.
sboschert@frontlinemedcom.com
On Twitter @sherryboschert
SAN FRANCISCO – An umbilical artery systolic-to-diastolic ratio of less than 3 as measured on weekly Doppler ultrasounds in a fetus with 30 weeks’ or more gestation and suspected intrauterine growth restriction suggests that the fetus probably is doing okay, Dr. Vickie A. Feldstein said.
That "ballpark guideline" is most helpful if physicians at your institution have agreed to use the umbilical artery systolic/diastolic (S/D) ratio as the parameter for assessing fetuses with intrauterine growth restriction (IUGR) and have agreed on which anatomical location is preferred for the ultrasound interrogation, so that there is some uniformity in how results are presented and interpreted, she said.
The recent Practice Bulletin No. 134 from the American College of Obstetricians and Gynecologists recommended in May 2013 that if the ultrasonographically estimated fetal weight is below the 10th percentile for gestational age, further evaluation should be considered, such as Doppler blood flow studies of the umbilical artery (Obstet. Gynecol. 2013;121:1122-33).
The medical literature describes several Doppler ultrasound parameters that could be used in suspected IUGR, including the umbilical artery S/D ratio, the resistance index, or the pulsatility index. They’re all about the same phenomenon, which is measuring resistance to perfusion in the placenta as reflected in the interrogation of the umbilical artery, Dr. Feldstein said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
"I think a report that includes all of them would make our heads spin," said Dr. Feldstein, professor of clinical radiology at the university. She and her colleagues use the S/D ratio, calculated by using calipers to measure the peak of systole on umbilical artery Doppler ultrasound and dividing that by the measure of end diastole.
"I don’t care how fast the flow actually is, I care about the character of the flow, the relative difference between systole and diastole," she said. The ratio reflects the status of placental circulation. It normally is high early in pregnancy and decreases as gestation advances, placental resistance decreases, and there is more forward flow during diastole.
If separate umbilical artery Doppler tracings yield discrepant S/D ratios, that may reflect normal variability or be due to changes in fetal heart rate. "A significant change in heart rate might change the S/D ratio quite a bit," she said. Or, an ultrasound filter set too low can produce noise in the tracing that might alter where you place the calipers.
The location along the umbilical cord that the sonographer samples also can affect measurements. The medical literature is full of suggestions about where to sample. Dr. Feldstein recommends sampling toward the placenta, if possible, which will reflect resistance to perfusion in the placenta.
"We’ve found the cord insertion, typically, so we know where to look," she said. "The farther away from the placenta you go, you’re adding resistance of the cord to your tracing."
She encouraged obstetricians to talk to the people who do Doppler at their institutions "to decide together how you want this done, how you want it reported, and what parameter you want used, so you don’t overwhelm yourselves with excess information."
If the S/D ratio is a bit above 3 in a third-trimester fetus with IUGR but there’s decent diastolic flow, "don’t sweat the small stuff," she suggested. As the S/D ratio goes higher and higher, however, placental insufficiency (and resistance) increases and forward flow decreases, and can become absent or even reversed end-diastolic flow.
An absence of diastolic flow is associated with a 60%-70% loss of vasculature, "a really significant abnormality in the placenta," she said. With reversed diastolic flow, the odds of perinatal death increase more than fivefold.
A recent study of 1,116 fetuses with IUGR showed that an abnormal umbilical artery Doppler ultrasound tracing (defined by pulsatility index or the absence or reversal of end-diastolic flow) was significantly associated with adverse outcomes irrespective of estimated fetal weight or abdominal circumference (Am. J. Obstet. Gynecol. 2013;208:e1-6 [doi: 10.1016/j.ajog.2013.02.007]).
When Dr. Feldstein sees an abnormal umbilical artery Doppler tracing, she samples the fetal middle cerebral artery by Doppler ultrasound. The middle cerebral artery S/D ratio should always be higher than the umbilical artery SD ratio, with a typical middle cerebral artery S/D ratio greater than 4 after 30 weeks’ gestation.
A fetus in trouble with IUGR will respond by lowering cerebral vascular resistance to maintain blood flow to its brain, decreasing the middle cerebral artery S/D ratio in what’s known as a "brain-sparing" wave form. Although there’s nothing that can be done for the fetus at this point, she said, it can be helpful to know that brain-sparing in growth-restricted fetuses was associated with increased risk for abnormal neurobehavioral outcomes in a controlled study of 126 preterm infants (Ultrasound Obstet. Gynecol. 2011;38:288-94).
"It’s a sign of distress," she said. Until recently, clinicians would follow that fetus carefully with various kinds of testing and watch for reverse diastolic flow in the umbilical artery, which is a sign of significant compromise, hypoxemia, and possible death. Today, a finding of brain-sparing next leads Dr. Feldstein to interrogate the ductus venosus in the liver, which is "the hardest to do, but it can be done," she said.
The ductus venosus flow should be phasic but continuous, in a pattern called the "a wave" reflecting forward, continuous flow even during right atrial contractions. If the flow reverses backward into the ductus venosus during right atrial contractions, that’s a sign of cardiac compromise, severe hypoxia, and right ventricular dysfunction, associated with high risk of morbidity and mortality.
Locating the ductus venosus for sampling can be tricky, in part because it is so close to hepatic veins, but if the ductus venosus flow is abnormal enough, there’s a shortcut that is easier to do: Sample the umbilical vein. Abnormal phasicity in umbilical vein pulsation may reflect ductus venosus flow reversal.
A previous study reported that the risk for perinatal mortality increased to nearly 6% with an elevated umbilical artery S/D ratio, to more than 11% with absent or reversed diastolic flow in the uterine artery, and to 39% with an abnormal ductus venosus wave form (Ultrasound Obstet. Gynecol. 2003;22:240-5). In a 2010 Cochrane Review of 18 studies that included more than 10,000 women with high-risk pregnancies, Doppler ultrasound was associated with a 29% reduction in the rate of perinatal deaths (1.2% with Doppler and 1.7% without); analysis showed that using Doppler on 203 high-risk pregnancies would avoid 1 perinatal death (Cochrane Database Syst. Rev. 2010 Jan. 20). "So, there’s a significant impact and not that much excess work," Dr. Feldstein said.
She reported having no financial disclosures.
sboschert@frontlinemedcom.com
On Twitter @sherryboschert
SAN FRANCISCO – An umbilical artery systolic-to-diastolic ratio of less than 3 as measured on weekly Doppler ultrasounds in a fetus with 30 weeks’ or more gestation and suspected intrauterine growth restriction suggests that the fetus probably is doing okay, Dr. Vickie A. Feldstein said.
That "ballpark guideline" is most helpful if physicians at your institution have agreed to use the umbilical artery systolic/diastolic (S/D) ratio as the parameter for assessing fetuses with intrauterine growth restriction (IUGR) and have agreed on which anatomical location is preferred for the ultrasound interrogation, so that there is some uniformity in how results are presented and interpreted, she said.
The recent Practice Bulletin No. 134 from the American College of Obstetricians and Gynecologists recommended in May 2013 that if the ultrasonographically estimated fetal weight is below the 10th percentile for gestational age, further evaluation should be considered, such as Doppler blood flow studies of the umbilical artery (Obstet. Gynecol. 2013;121:1122-33).
The medical literature describes several Doppler ultrasound parameters that could be used in suspected IUGR, including the umbilical artery S/D ratio, the resistance index, or the pulsatility index. They’re all about the same phenomenon, which is measuring resistance to perfusion in the placenta as reflected in the interrogation of the umbilical artery, Dr. Feldstein said at a meeting on antepartum and intrapartum management sponsored by the University of California, San Francisco.
"I think a report that includes all of them would make our heads spin," said Dr. Feldstein, professor of clinical radiology at the university. She and her colleagues use the S/D ratio, calculated by using calipers to measure the peak of systole on umbilical artery Doppler ultrasound and dividing that by the measure of end diastole.
"I don’t care how fast the flow actually is, I care about the character of the flow, the relative difference between systole and diastole," she said. The ratio reflects the status of placental circulation. It normally is high early in pregnancy and decreases as gestation advances, placental resistance decreases, and there is more forward flow during diastole.
If separate umbilical artery Doppler tracings yield discrepant S/D ratios, that may reflect normal variability or be due to changes in fetal heart rate. "A significant change in heart rate might change the S/D ratio quite a bit," she said. Or, an ultrasound filter set too low can produce noise in the tracing that might alter where you place the calipers.
The location along the umbilical cord that the sonographer samples also can affect measurements. The medical literature is full of suggestions about where to sample. Dr. Feldstein recommends sampling toward the placenta, if possible, which will reflect resistance to perfusion in the placenta.
"We’ve found the cord insertion, typically, so we know where to look," she said. "The farther away from the placenta you go, you’re adding resistance of the cord to your tracing."
She encouraged obstetricians to talk to the people who do Doppler at their institutions "to decide together how you want this done, how you want it reported, and what parameter you want used, so you don’t overwhelm yourselves with excess information."
If the S/D ratio is a bit above 3 in a third-trimester fetus with IUGR but there’s decent diastolic flow, "don’t sweat the small stuff," she suggested. As the S/D ratio goes higher and higher, however, placental insufficiency (and resistance) increases and forward flow decreases, and can become absent or even reversed end-diastolic flow.
An absence of diastolic flow is associated with a 60%-70% loss of vasculature, "a really significant abnormality in the placenta," she said. With reversed diastolic flow, the odds of perinatal death increase more than fivefold.
A recent study of 1,116 fetuses with IUGR showed that an abnormal umbilical artery Doppler ultrasound tracing (defined by pulsatility index or the absence or reversal of end-diastolic flow) was significantly associated with adverse outcomes irrespective of estimated fetal weight or abdominal circumference (Am. J. Obstet. Gynecol. 2013;208:e1-6 [doi: 10.1016/j.ajog.2013.02.007]).
When Dr. Feldstein sees an abnormal umbilical artery Doppler tracing, she samples the fetal middle cerebral artery by Doppler ultrasound. The middle cerebral artery S/D ratio should always be higher than the umbilical artery SD ratio, with a typical middle cerebral artery S/D ratio greater than 4 after 30 weeks’ gestation.
A fetus in trouble with IUGR will respond by lowering cerebral vascular resistance to maintain blood flow to its brain, decreasing the middle cerebral artery S/D ratio in what’s known as a "brain-sparing" wave form. Although there’s nothing that can be done for the fetus at this point, she said, it can be helpful to know that brain-sparing in growth-restricted fetuses was associated with increased risk for abnormal neurobehavioral outcomes in a controlled study of 126 preterm infants (Ultrasound Obstet. Gynecol. 2011;38:288-94).
"It’s a sign of distress," she said. Until recently, clinicians would follow that fetus carefully with various kinds of testing and watch for reverse diastolic flow in the umbilical artery, which is a sign of significant compromise, hypoxemia, and possible death. Today, a finding of brain-sparing next leads Dr. Feldstein to interrogate the ductus venosus in the liver, which is "the hardest to do, but it can be done," she said.
The ductus venosus flow should be phasic but continuous, in a pattern called the "a wave" reflecting forward, continuous flow even during right atrial contractions. If the flow reverses backward into the ductus venosus during right atrial contractions, that’s a sign of cardiac compromise, severe hypoxia, and right ventricular dysfunction, associated with high risk of morbidity and mortality.
Locating the ductus venosus for sampling can be tricky, in part because it is so close to hepatic veins, but if the ductus venosus flow is abnormal enough, there’s a shortcut that is easier to do: Sample the umbilical vein. Abnormal phasicity in umbilical vein pulsation may reflect ductus venosus flow reversal.
A previous study reported that the risk for perinatal mortality increased to nearly 6% with an elevated umbilical artery S/D ratio, to more than 11% with absent or reversed diastolic flow in the uterine artery, and to 39% with an abnormal ductus venosus wave form (Ultrasound Obstet. Gynecol. 2003;22:240-5). In a 2010 Cochrane Review of 18 studies that included more than 10,000 women with high-risk pregnancies, Doppler ultrasound was associated with a 29% reduction in the rate of perinatal deaths (1.2% with Doppler and 1.7% without); analysis showed that using Doppler on 203 high-risk pregnancies would avoid 1 perinatal death (Cochrane Database Syst. Rev. 2010 Jan. 20). "So, there’s a significant impact and not that much excess work," Dr. Feldstein said.
She reported having no financial disclosures.
sboschert@frontlinemedcom.com
On Twitter @sherryboschert
EXPERT ANALYSIS FROM A MEETING ON ANTEPARTUM AND INTRAPARTUM MANAGEMENT