User login
- The gynecologist’s role in managing menstrual migraine
Anne H. Calhoun, MD (April 2010)
Headaches are highly prevalent in women during their reproductive years. Most are a painful nuisance and do not present a risk of serious morbidity. Some, however, can be dangerous, and the addition of an estrogen-containing contraceptive can increase that risk.
Combination estrogen-progestin contraceptives are effective, popular, and easy to use—but are they safe for women who have headaches? This is a critical question. Some women who have preexisting headaches experience relief with hormonal contraception; others report stable or worsening symptoms; still others do not develop headaches until they begin hormonal contraception.
The differentiation between nuisance and true medical risk in this population depends on an accurate diagnosis of headache subtype. Taking a few moments to confirm whether a patient with headache has a true risk if she chooses hormonal contraception will prevent unnecessary restriction of a method and promote contraceptive success.
In this article, we present three cases that facilitate discussion of the safety, adverse effects, and benefits of various contraceptive strategies in women who have headaches.
Many women who report migraines don’t have them
Most women who report headaches to their gynecologist have not received a clinical diagnosis of headache subtype. They may say that they have “migraines” because that is the term used most commonly in the United States to indicate a severe level of distress with a headache. In actuality, although migraine is common in women, tension-type headaches are more prevalent.
The evaluation of a patient with headaches who is seeking contraception should begin with a simple diagnostic algorithm for headache type. Accurate diagnosis can be made using the International Headache Society (IHS) comprehensive guide for headache subtypes, last updated in 2004.1 TABLE 1, presents a simple classification of chronic headache syndromes, which account for more than 90% of headaches.
TABLE 1
Diagnostic criteria for headache subtypes
| Tension-type | |
| Infrequent episodic | |
| A. | At least 10 episodes <1 day per month on average (<12 days per year) and fulfilling criteria B–D below |
| Frequent episodic | |
| A. | At least 10 episodes occurring ≥1 but <15 days per month for at least 3 months (≥12 and <180 days per year) and fulfilling criteria B–D |
| B. | Headache lasting for 30 minutes to 7 days |
| C. | Headache has at least two of the following characteristics: |
| |
| D. | Both of the following: |
| |
| E. | Not attributable to another disorder |
| Cluster | |
| A. | At least 5 attacks fulfilling criteria B–D |
| B. | Severe or very severe unilateral orbital, supraorbital and/or temporal pain lasting 15–180 minutes if untreated |
| C. | Headache is accompanied by at least one of the following: |
| |
| D. | Attacks have a frequency from one every other day to 8 per day |
| E. | Not attributable to another disorder |
| Migraine without aura | |
| At least 5 attacks fulfilling criteria B–D | |
| A. | Headache attacks lasting 4–72 hours (untreated or successfully treated) |
| B. | Headache has at least two of the following characteristics: |
| |
| C. | During headache at least one of the following: |
| |
| D. | Not attributable to another disorder |
| Typical migraine with aura headache | |
| A. | At least 2 attacks fulfilling criteria B–D |
| B. | Aura consisting of at least one of the following, but no motor weakness: |
| |
| C. | At least two of the following: |
| |
| D. | Headache fulfilling criteria B–D for migraine without aura begins during the aura or follows aura within 60 minutes |
| E. | Not attributable to another disorder |
| Pure menstrual migraine without aura | |
| A. | Attacks, in a menstruating woman, fulfilling criteria for migraine without aura |
| B. | Attacks occur exclusively on Day 1 ±2 days (i.e., Days +2 to –3) of menstruation in at least two out of three menstrual cycles and at no other times of the cycle |
| Estrogen-withdrawal headache | |
| A. | Headache or migraine fulfilling criteria C and D |
| B. | Daily use of exogenous estrogen for >3 weeks, which is interrupted |
| C. | Headache or migraine develops within 5 days after last use of estrogen |
| D. | Headache or migraine resolves within 3 days |
| Exogenous hormone-induced headache | |
| A. | Headache or migraine fulfilling criteria C and D |
| B. | Regular use of exogenous hormones |
| C. | Headache or migraine develops or markedly worsens within 3 months of commencing exogenous hormones |
| D. | Headache or migraine resolves or reverts to its previous pattern within 3 months after total discontinuation of exogenous hormones |
| Source: International Headache Society1 | |
CASE 1: Patient reports a history of migraine
A 21-year-old nulliparous woman has severe dysmenorrhea that has been unresponsive to treatment with nonsteroidal anti-inflammatory drugs (NSAIDs). She also desires contraception. Her primary care provider has recommended combination oral contraceptives (OCs) as a solution to both problems. However, the patient has heard from friends that she should not use OCs because of her history of migraine headache, and she has come to see you for a second opinion.
She describes her headaches as bilateral and reports a “tightening” sensation. The headaches are associated with photophobia and are not aggravated by routine physical activity. They respond to NSAIDs.
She also reports that her mother and sister have been on a prescription medication for migraines for many years.
Is an OC appropriate for this patient?
This young woman’s history is consistent with tension-type headache, not migraine. Tension headache is the most common subtype, with prevalence as high as 59% in women of reproductive age.2 It is generally characterized by mild or moderate pain that is bilateral, pressing, or tightening in quality. The pain does not worsen with routine physical activity. There is no nausea, but photophobia or phonophobia may be present.1
A systematic review of the risk of stroke associated with combination OC use and headaches did not find any studies examining the association between nonmigraine headache and the risk of stroke among combination OC users.3 In contrast to some migraines, however, tension-type headache has not been associated with an increased risk of stroke in the general population. Nor is there evidence that hormonal fluctuations play a role in the pathogenesis or clinical course of tension headache.
In summary, there are no contraindications to combination hormonal contraceptives—including estrogen-progestin OCs, the contraceptive patch, and the contraceptive ring—in women who have tension headache.4
Explore any family history of migraine
The patient in Case 1 appears to have a family history of migraine. Some evidence suggests that such a family history increases the risk of new-onset migraine with use of a combination OC.5 Because the background prevalence of migraine is so high in the population of women likely to use a combination OC, it can be difficult to determine whether worsening headache or development of migraine with OC use is causal or coincidental.
Were this patient to express concern over even a theoretical risk of triggering migraine headache, then a combination OC would probably not be appropriate. In the absence of such concern, however, there is no reason to withhold hormonal contraception. Progestin-only options exist that will provide her with excellent contraceptive efficacy and help relieve her dysmenorrhea:
- the etonogestrel subdermal implant (Implanon)
- depot medroxyprogesterone acetate (DMPA) injection (Depo-Provera)
- the levonorgestrel-releasing intrauterine system (LNG-IUS; Mirena).
Although some women do develop headaches while using progestin-only contraceptives, there is no evidence that such use can trigger a new migraine syndrome in a woman with a family history of such. Again, however, the data are limited.
Progestin methods are safe
The use of progestin-only methods has been promoted in headache sufferers, especially those who have a specific diagnosis of migraine, because progestins do not add to the elevated risk of stroke that accompanies migraine with aura.
Because headache is common in women of reproductive age, it is not surprising that it is listed as a common adverse event for all contraceptives, including progestin-only methods. Evidence that progestin-only methods cause or worsen headaches is slim, however. Preliminary studies indicate that mid-luteal elevations of progesterone or its metabolites could prevent migraine, compared with other times in the cycle.6 Older studies report that a daily oral progestin could prevent migraine in premenopausal women, possibly secondary to induction of anovulation. At the same time, there are clinical reports that DMPA may trigger headache as a side effect in susceptible women.
Generally, then, although progestin-only methods are likely to be safe in all patients with headache, and ovulation suppression may improve the headaches, some patients may experience worsening symptoms.
CASE 2: OC user reports migraine with aura
A 26-year-old mother of one comes to your office for her annual exam. She has used combination OCs for 2 years. She also has a history of severe headaches, which occur four or five times a year. She says the headaches are unilateral, pulsating, and associated with photophobia. The symptoms worsen when she is active and are preceded by a flashing zigzag line that migrates from the center of her visual field to the lateral periphery. The headaches are not associated with her menstrual cycle and have not changed in character or frequency since she began using an OC. She does not smoke.
Should she continue taking an OC?
This patient’s history is consistent with migraine headache with aura. Migraine is a common, disabling primary headache disorder, with an estimated 1-year prevalence in adult women of 15% to 18% and a lifetime prevalence of about 30%.2 Approximately 10% to 20% of people who have migraine experience auras.7
Research on the association between combination OCs, migraine, and stroke has been limited by the rarity of the outcome in the population of concern. Most data come from case-controlled studies and are fettered by a lack of standardized criteria for the diagnosis of migraine (few studies use criteria from the IHS); by recall bias (such as self-reported OC use); and by survivorship bias. Many studies fail to differentiate by the presence of aura, which indicates a different effect on cerebral blood flow patterns than does migraine without aura.
Although most studies attempt to control for the confounding effect of smoking, some do not, and in others the prevalence of smoking is so high it can be difficult to remove from the equation. Some of the studies examining the association between migraine and stroke do not differentiate by gender.
Taking all these variables into account, migraine in women independently appears to carry a twofold to threefold increased risk of ischemic stroke, compared with the risk in similarly aged women who do not have migraine.8 Among women who have a history of migraine, those who use combination OCs are two times to four times more likely to experience ischemic stroke than nonusers are. Among women with the highest risk (combination OC users with migraine), the odds ratio for ischemic stroke ranges from 6 to almost 14, compared with women with the lowest risk (nonusers without migraine).3
To put all this in perspective, the absolute risk of stroke for a 26-year-old nonsmoker like our patient is 6 cases in every 100,000 woman-years.9 Multiplying this risk by a factor of 3 to account for her migraines, and by 3 again to account for her OC use, we can roughly estimate her absolute risk of stroke as about 54 cases for every 100,000 woman-years. Although this absolute risk is extremely low, the outcome can be catastrophic. It behooves us to proceed with caution.
A common misperception among health-care providers is that nausea, vomiting, photophobia, and phonophobia represent migraine aura, when in fact these symptoms are part of the associated diagnostic symptoms of all migraines.
About 20% of people who have migraine experience an aura. The aura begins before the headache and typically lasts 5 to 20 minutes—rarely does it last more than 60 minutes. The headache occurs soon after the aura stops.
The aura may include zigzag lines of light, flashing lights or bright spots, blurred or darkened spots, or focal neurologic symptoms such as numbness or tingling in the fingers of one hand, lips, tongue, or lower face. Auras may involve other senses, such as smell, and can occasionally cause temporary focal weakness or changes in speech.
Presence of aura likely confers greater risk
Many studies of migraine do not explore contraceptive use. They report a higher risk of stroke when aura is present.8,10-15 One of the few prospective studies found no increased risk of stroke in migraineurs who did not experience aura.12
No studies examining a link between combination OCs and ischemic stroke in migraineurs have been large enough to stratify the risk of stroke by the presence or absence of aura. The assumption has been that this risk is amplified by use of combination OCs. Consequently, migraine with aura is designated as an absolute contraindication to the use of combination OCs by the World Health Organization (WHO), ACOG, and the IHS.4,16Although no studies have included women using the contraceptive patch or ring, it is assumed that these methods carry a risk of ischemic stroke similar to that of combination OCs.17 The IHS recommendations on combination hormonal contraception in women with migraine are given in TABLE 2.18
TABLE 2
When combination OCs are appropriate for a woman who has migraine
|
| Source: International Headache Society18 |
Although the patient in Case 2 has been experiencing migraine with aura for some time without a change in headache pattern, combination hormonal contraception is contraindicated. Her history of migraine with aura may have been missed during previous evaluation if she did not consider it to be a “medical problem.” All candidates for combination OCs should be directly questioned about any history of migraine, thrombosis, cigarette smoking, and hypertension.
The patient described in Case 2 should be encouraged to switch to a progestin-only method of contraception or a highly effective nonhormonal method, such as a copper-containing IUD (Paragard). Because she had no change in her headache pattern on ovulation-suppression therapy (OCs), she likely will have no change with continued ovulation suppression (DMPA, subdermal implant) or without it (LNG-IUS, copper lUD).
Be sure to time the switch in methods so that contraception is maintained throughout the transition. This patient would also benefit from referral to a headache specialist for evaluation and treatment.
CASE 3 Perimenstrual headache in a smoker
A 32-year-old mother of two visits your office for contraceptive counseling. She reports that she smokes two to five cigarettes a day and has a history of migraine without aura. Her headaches occur exclusively during the two days just before her period, and they resolve within the first few days of bleeding. NSAIDs provide limited relief. Is hormonal contraception appropriate?
When a woman with perimenstrual headache is choosing a contraceptive method, we need to ensure that she is not exposed to undue risks and focus on improving her quality of life, if possible.
TABLE 1, reviews the diagnostic criteria for pure menstrual migraine, in which symptoms occur only in the perimenstrual period, as in this patient. Most practitioners use a broader definition of menstrual-related migraine, in which women may have other migraine triggers but still experience predictable headaches with menses. More than 50% of women who have migraine report an association between their headaches and menstruation, but only about 10% of women report migraine exclusively with menstruation.7
Hormonal manipulation is not first-line management for menstrual migraine.19 However, for the patient seeking contraception, it is appropriate to consider the effect of a given method on her headaches because that effect is sure to influence her satisfaction, quality of life, and compliance.
Menstrual migraine is rarely associated with aura, even in women who have migraine with aura at other times in the cycle.7However, the headaches experienced at the time of menstruation tend to be more severe and longer-lasting and less responsive to medication than are migraines experienced at other times of the month.20
Eliminate the placebo week
Research into the pathogenesis of menstrual migraine has focused on the withdrawal of estrogen in the luteal phase of the menstrual cycle. Ovulation is not a requisite for menstrual migraine attacks, which frequently occur during the hormone-free interval in combination hormonal contraceptive regimens. Several lines of evidence suggest that stabilizing estrogen fluctuations can prevent migraine (FIGURE).7
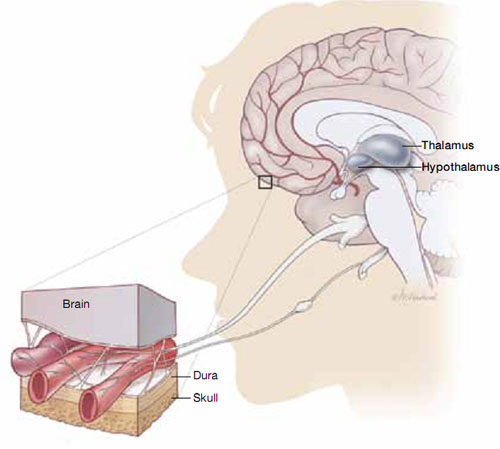
Hormonal fluctuations can trigger migraine
Fluctuations in estrogen during the menstrual cycle may trigger dilation and constriction of blood vessels in the brain, causing migraine.If a patient who has pure menstrual migraine desires to use an estrogen-containing contraceptive, she is likely to be as safe in that choice as a patient without migraine. However, she is not likely to experience improvement in her migraines if she uses a traditional 21/7 active-to-placebo pill regimen. It is necessary to maintain an adequate estrogen level during the placebo week, either through estrogen supplementation or extended-cycle dosing, to prevent the estrogen-withdrawal trigger for headaches.
A few OC regimens reduce the estrogen-free interval to 4 days or provide estrogen supplementation during the placebo week; these regimens may benefit women who have menstrual migraine, although data are scant. If most, or all, of the patient’s migraines are suppressed on combined hormonal contraception, continuous use with rare (e.g., yearly) withdrawals may be indicated.
Alternatives to estrogen-containing contraceptives
If the patient does not desire a combination OC or has other contraindications to estrogen, she may benefit from a progestin-only contraceptive that suppresses ovulation, such as DMPA or the etonogestrel implant. Even with ovulation suppression, however, estrogen fluctuations may occur, and the evidence supporting the use of these methods in the concurrent management of contraceptive needs and menstrual migraine is less clear. Although they are safe in women who have migraine, progestin-only pills and the LNG-IUS do not suppress ovulation reliably enough to be considered useful in managing menstrual migraine.
Take a careful history
Choosing a contraceptive for a woman who has headaches begins the same way as with any other patient: with careful assessment of her short-term and long-term family-planning goals, along with a history and physical to elicit any “red flags,” cultural preferences, and tolerance for specific side effects.
Once you become aware of a history of headache, careful history-taking can usually differentiate between the major headache subtypes and help you avoid limiting contraceptive options unnecessarily.
Women who start any contraceptive may report improvement, worsening, or new onset of headache symptoms. This change usually occurs within the first 3 months, and headaches associated with hormone use tend to improve with continued use.21
In women who have preexisting migraine, you should undertake prompt evaluation and consider a change of contraceptive method in response to 1) any increase in severity or frequency or 2) the onset of associated neurologic symptoms.
We want to hear from you! Tell us what you think.
1. International Headache Society. The international classification of headache disorders: 2nd edition. Cephalalgia. 2004;24(suppl 1):9-160.
2. Rasmussen BK. Epidemiology of headache. Cephalalgia. 2001;21(7):774-777.
3. Curtis KM, Mohllajee AP, Peterson HB. Use of combined oral contraceptives among women with migraine and nonmigrainous headaches: a systematic review. Contraception. 2006;73(2):189-194.
4. Harris M, Kaneshiro B. An evidence-based approach to hormonal contraception and headaches. Contraception. 2009;80(5):417-421.
5. Loder EW, Buse DC, Golub JR. Headache and combination estrogen-progestin oral contraceptives: integrating evidence, guidelines, and clinical practice. Headache. 2005;45(3):224.
6. Martin VT, Behbehani M. Ovarian hormones and migraine headache: understanding mechanisms and pathogenesis— part 2. Headache. 2006;46(3):365-386.
7. Macgregor EA. Menstrual migraine: a clinical review. J Fam Plann Reprod Health Care. 2007;33(1):36-47.
8. Etminan M, Takkouche B, Isorna FC, et al. Risk of ischaemic stroke in people with migraine: systematic review and metaanalysis of observational studies. BMJ. 2005;330(7482):63.-
9. Petitti DB, Sidney S, Quesenberry CP, Jr. Bernstein A. Incidence of stroke and myocardial infarction in women of reproductive age. Stroke. 1997;28(2):280-283.
10. Carolei A, Marini C, De Matteis G. History of migraine and risk of cerebral ischaemia in young adults. Lancet. 1996;347(9014):1503-1506.
11. Chang CL, Donaghy M, Poulter N. Migraine and stroke in young women: case-control study. BMJ. 1999;318(7175):13.
12. Kurth T, Slomke MA, Kase CS, et al. Migraine, headache, and the risk of stroke in women: a prospective study. Neurology. 2005;64(6):1020-1026.
13. MacClellan LR, Giles W, Cole J, et al. Probable migraine with visual aura and risk of ischemic stroke: the stroke prevention in young women study. Stroke. 2007;38(9):2438-2445.
14. Tzourio C, Kittner SJ, Bousser MG, Alperovitch A. Migraine and stroke in young women. Cephalalgia. 2000;20(3):190-199.
15. Tzourio C, Tehindrazanarivelo A, Iglesias S, et al. Case-control study of migraine and risk of ischaemic stroke in young women. BMJ. 1995;310(6983):830-833.
16. ACOG practice bulletin. No. 73: Use of hormonal contraception in women with coexisting medical conditions. Obstet Gynecol. 2006;107(6):1453-1472.
17. Department of Reproductive Health. Medical Eligibility Criteria for Contraceptive Use. 4th ed; 2009. Geneva, Switzerland: World Health Organization; 2010.
18. Bousser MG, Conard J, Kittner S, et al. Recommendations on the risk of ischaemic stroke associated with use of combined oral contraceptives and hormone replacement therapy in women with migraine. The International Headache Society Task Force on Combined Oral Contraceptives & Hormone Replacement Therapy. Cephalalgia. 2000;20(3):155-156.
19. Calhoun AH. The gynecologist’s role in managing menstrual migraine. OBG Manage. 2010;22(4):30-43.
20. Martin VT, Wernke S, Mandell K, et al. Defining the relationship between ovarian hormones and migraine headache. Headache. 2005;45(9):1190-1201.
21. Allais G, Gabellari IC, De Lorenzo C, C, Mana O, Benedetto C. Oral contraceptives in migraine. Expert Rev Neurother. 2009;9(3):381-393.
- The gynecologist’s role in managing menstrual migraine
Anne H. Calhoun, MD (April 2010)
Headaches are highly prevalent in women during their reproductive years. Most are a painful nuisance and do not present a risk of serious morbidity. Some, however, can be dangerous, and the addition of an estrogen-containing contraceptive can increase that risk.
Combination estrogen-progestin contraceptives are effective, popular, and easy to use—but are they safe for women who have headaches? This is a critical question. Some women who have preexisting headaches experience relief with hormonal contraception; others report stable or worsening symptoms; still others do not develop headaches until they begin hormonal contraception.
The differentiation between nuisance and true medical risk in this population depends on an accurate diagnosis of headache subtype. Taking a few moments to confirm whether a patient with headache has a true risk if she chooses hormonal contraception will prevent unnecessary restriction of a method and promote contraceptive success.
In this article, we present three cases that facilitate discussion of the safety, adverse effects, and benefits of various contraceptive strategies in women who have headaches.
Many women who report migraines don’t have them
Most women who report headaches to their gynecologist have not received a clinical diagnosis of headache subtype. They may say that they have “migraines” because that is the term used most commonly in the United States to indicate a severe level of distress with a headache. In actuality, although migraine is common in women, tension-type headaches are more prevalent.
The evaluation of a patient with headaches who is seeking contraception should begin with a simple diagnostic algorithm for headache type. Accurate diagnosis can be made using the International Headache Society (IHS) comprehensive guide for headache subtypes, last updated in 2004.1 TABLE 1, presents a simple classification of chronic headache syndromes, which account for more than 90% of headaches.
TABLE 1
Diagnostic criteria for headache subtypes
| Tension-type | |
| Infrequent episodic | |
| A. | At least 10 episodes <1 day per month on average (<12 days per year) and fulfilling criteria B–D below |
| Frequent episodic | |
| A. | At least 10 episodes occurring ≥1 but <15 days per month for at least 3 months (≥12 and <180 days per year) and fulfilling criteria B–D |
| B. | Headache lasting for 30 minutes to 7 days |
| C. | Headache has at least two of the following characteristics: |
| |
| D. | Both of the following: |
| |
| E. | Not attributable to another disorder |
| Cluster | |
| A. | At least 5 attacks fulfilling criteria B–D |
| B. | Severe or very severe unilateral orbital, supraorbital and/or temporal pain lasting 15–180 minutes if untreated |
| C. | Headache is accompanied by at least one of the following: |
| |
| D. | Attacks have a frequency from one every other day to 8 per day |
| E. | Not attributable to another disorder |
| Migraine without aura | |
| At least 5 attacks fulfilling criteria B–D | |
| A. | Headache attacks lasting 4–72 hours (untreated or successfully treated) |
| B. | Headache has at least two of the following characteristics: |
| |
| C. | During headache at least one of the following: |
| |
| D. | Not attributable to another disorder |
| Typical migraine with aura headache | |
| A. | At least 2 attacks fulfilling criteria B–D |
| B. | Aura consisting of at least one of the following, but no motor weakness: |
| |
| C. | At least two of the following: |
| |
| D. | Headache fulfilling criteria B–D for migraine without aura begins during the aura or follows aura within 60 minutes |
| E. | Not attributable to another disorder |
| Pure menstrual migraine without aura | |
| A. | Attacks, in a menstruating woman, fulfilling criteria for migraine without aura |
| B. | Attacks occur exclusively on Day 1 ±2 days (i.e., Days +2 to –3) of menstruation in at least two out of three menstrual cycles and at no other times of the cycle |
| Estrogen-withdrawal headache | |
| A. | Headache or migraine fulfilling criteria C and D |
| B. | Daily use of exogenous estrogen for >3 weeks, which is interrupted |
| C. | Headache or migraine develops within 5 days after last use of estrogen |
| D. | Headache or migraine resolves within 3 days |
| Exogenous hormone-induced headache | |
| A. | Headache or migraine fulfilling criteria C and D |
| B. | Regular use of exogenous hormones |
| C. | Headache or migraine develops or markedly worsens within 3 months of commencing exogenous hormones |
| D. | Headache or migraine resolves or reverts to its previous pattern within 3 months after total discontinuation of exogenous hormones |
| Source: International Headache Society1 | |
CASE 1: Patient reports a history of migraine
A 21-year-old nulliparous woman has severe dysmenorrhea that has been unresponsive to treatment with nonsteroidal anti-inflammatory drugs (NSAIDs). She also desires contraception. Her primary care provider has recommended combination oral contraceptives (OCs) as a solution to both problems. However, the patient has heard from friends that she should not use OCs because of her history of migraine headache, and she has come to see you for a second opinion.
She describes her headaches as bilateral and reports a “tightening” sensation. The headaches are associated with photophobia and are not aggravated by routine physical activity. They respond to NSAIDs.
She also reports that her mother and sister have been on a prescription medication for migraines for many years.
Is an OC appropriate for this patient?
This young woman’s history is consistent with tension-type headache, not migraine. Tension headache is the most common subtype, with prevalence as high as 59% in women of reproductive age.2 It is generally characterized by mild or moderate pain that is bilateral, pressing, or tightening in quality. The pain does not worsen with routine physical activity. There is no nausea, but photophobia or phonophobia may be present.1
A systematic review of the risk of stroke associated with combination OC use and headaches did not find any studies examining the association between nonmigraine headache and the risk of stroke among combination OC users.3 In contrast to some migraines, however, tension-type headache has not been associated with an increased risk of stroke in the general population. Nor is there evidence that hormonal fluctuations play a role in the pathogenesis or clinical course of tension headache.
In summary, there are no contraindications to combination hormonal contraceptives—including estrogen-progestin OCs, the contraceptive patch, and the contraceptive ring—in women who have tension headache.4
Explore any family history of migraine
The patient in Case 1 appears to have a family history of migraine. Some evidence suggests that such a family history increases the risk of new-onset migraine with use of a combination OC.5 Because the background prevalence of migraine is so high in the population of women likely to use a combination OC, it can be difficult to determine whether worsening headache or development of migraine with OC use is causal or coincidental.
Were this patient to express concern over even a theoretical risk of triggering migraine headache, then a combination OC would probably not be appropriate. In the absence of such concern, however, there is no reason to withhold hormonal contraception. Progestin-only options exist that will provide her with excellent contraceptive efficacy and help relieve her dysmenorrhea:
- the etonogestrel subdermal implant (Implanon)
- depot medroxyprogesterone acetate (DMPA) injection (Depo-Provera)
- the levonorgestrel-releasing intrauterine system (LNG-IUS; Mirena).
Although some women do develop headaches while using progestin-only contraceptives, there is no evidence that such use can trigger a new migraine syndrome in a woman with a family history of such. Again, however, the data are limited.
Progestin methods are safe
The use of progestin-only methods has been promoted in headache sufferers, especially those who have a specific diagnosis of migraine, because progestins do not add to the elevated risk of stroke that accompanies migraine with aura.
Because headache is common in women of reproductive age, it is not surprising that it is listed as a common adverse event for all contraceptives, including progestin-only methods. Evidence that progestin-only methods cause or worsen headaches is slim, however. Preliminary studies indicate that mid-luteal elevations of progesterone or its metabolites could prevent migraine, compared with other times in the cycle.6 Older studies report that a daily oral progestin could prevent migraine in premenopausal women, possibly secondary to induction of anovulation. At the same time, there are clinical reports that DMPA may trigger headache as a side effect in susceptible women.
Generally, then, although progestin-only methods are likely to be safe in all patients with headache, and ovulation suppression may improve the headaches, some patients may experience worsening symptoms.
CASE 2: OC user reports migraine with aura
A 26-year-old mother of one comes to your office for her annual exam. She has used combination OCs for 2 years. She also has a history of severe headaches, which occur four or five times a year. She says the headaches are unilateral, pulsating, and associated with photophobia. The symptoms worsen when she is active and are preceded by a flashing zigzag line that migrates from the center of her visual field to the lateral periphery. The headaches are not associated with her menstrual cycle and have not changed in character or frequency since she began using an OC. She does not smoke.
Should she continue taking an OC?
This patient’s history is consistent with migraine headache with aura. Migraine is a common, disabling primary headache disorder, with an estimated 1-year prevalence in adult women of 15% to 18% and a lifetime prevalence of about 30%.2 Approximately 10% to 20% of people who have migraine experience auras.7
Research on the association between combination OCs, migraine, and stroke has been limited by the rarity of the outcome in the population of concern. Most data come from case-controlled studies and are fettered by a lack of standardized criteria for the diagnosis of migraine (few studies use criteria from the IHS); by recall bias (such as self-reported OC use); and by survivorship bias. Many studies fail to differentiate by the presence of aura, which indicates a different effect on cerebral blood flow patterns than does migraine without aura.
Although most studies attempt to control for the confounding effect of smoking, some do not, and in others the prevalence of smoking is so high it can be difficult to remove from the equation. Some of the studies examining the association between migraine and stroke do not differentiate by gender.
Taking all these variables into account, migraine in women independently appears to carry a twofold to threefold increased risk of ischemic stroke, compared with the risk in similarly aged women who do not have migraine.8 Among women who have a history of migraine, those who use combination OCs are two times to four times more likely to experience ischemic stroke than nonusers are. Among women with the highest risk (combination OC users with migraine), the odds ratio for ischemic stroke ranges from 6 to almost 14, compared with women with the lowest risk (nonusers without migraine).3
To put all this in perspective, the absolute risk of stroke for a 26-year-old nonsmoker like our patient is 6 cases in every 100,000 woman-years.9 Multiplying this risk by a factor of 3 to account for her migraines, and by 3 again to account for her OC use, we can roughly estimate her absolute risk of stroke as about 54 cases for every 100,000 woman-years. Although this absolute risk is extremely low, the outcome can be catastrophic. It behooves us to proceed with caution.
A common misperception among health-care providers is that nausea, vomiting, photophobia, and phonophobia represent migraine aura, when in fact these symptoms are part of the associated diagnostic symptoms of all migraines.
About 20% of people who have migraine experience an aura. The aura begins before the headache and typically lasts 5 to 20 minutes—rarely does it last more than 60 minutes. The headache occurs soon after the aura stops.
The aura may include zigzag lines of light, flashing lights or bright spots, blurred or darkened spots, or focal neurologic symptoms such as numbness or tingling in the fingers of one hand, lips, tongue, or lower face. Auras may involve other senses, such as smell, and can occasionally cause temporary focal weakness or changes in speech.
Presence of aura likely confers greater risk
Many studies of migraine do not explore contraceptive use. They report a higher risk of stroke when aura is present.8,10-15 One of the few prospective studies found no increased risk of stroke in migraineurs who did not experience aura.12
No studies examining a link between combination OCs and ischemic stroke in migraineurs have been large enough to stratify the risk of stroke by the presence or absence of aura. The assumption has been that this risk is amplified by use of combination OCs. Consequently, migraine with aura is designated as an absolute contraindication to the use of combination OCs by the World Health Organization (WHO), ACOG, and the IHS.4,16Although no studies have included women using the contraceptive patch or ring, it is assumed that these methods carry a risk of ischemic stroke similar to that of combination OCs.17 The IHS recommendations on combination hormonal contraception in women with migraine are given in TABLE 2.18
TABLE 2
When combination OCs are appropriate for a woman who has migraine
|
| Source: International Headache Society18 |
Although the patient in Case 2 has been experiencing migraine with aura for some time without a change in headache pattern, combination hormonal contraception is contraindicated. Her history of migraine with aura may have been missed during previous evaluation if she did not consider it to be a “medical problem.” All candidates for combination OCs should be directly questioned about any history of migraine, thrombosis, cigarette smoking, and hypertension.
The patient described in Case 2 should be encouraged to switch to a progestin-only method of contraception or a highly effective nonhormonal method, such as a copper-containing IUD (Paragard). Because she had no change in her headache pattern on ovulation-suppression therapy (OCs), she likely will have no change with continued ovulation suppression (DMPA, subdermal implant) or without it (LNG-IUS, copper lUD).
Be sure to time the switch in methods so that contraception is maintained throughout the transition. This patient would also benefit from referral to a headache specialist for evaluation and treatment.
CASE 3 Perimenstrual headache in a smoker
A 32-year-old mother of two visits your office for contraceptive counseling. She reports that she smokes two to five cigarettes a day and has a history of migraine without aura. Her headaches occur exclusively during the two days just before her period, and they resolve within the first few days of bleeding. NSAIDs provide limited relief. Is hormonal contraception appropriate?
When a woman with perimenstrual headache is choosing a contraceptive method, we need to ensure that she is not exposed to undue risks and focus on improving her quality of life, if possible.
TABLE 1, reviews the diagnostic criteria for pure menstrual migraine, in which symptoms occur only in the perimenstrual period, as in this patient. Most practitioners use a broader definition of menstrual-related migraine, in which women may have other migraine triggers but still experience predictable headaches with menses. More than 50% of women who have migraine report an association between their headaches and menstruation, but only about 10% of women report migraine exclusively with menstruation.7
Hormonal manipulation is not first-line management for menstrual migraine.19 However, for the patient seeking contraception, it is appropriate to consider the effect of a given method on her headaches because that effect is sure to influence her satisfaction, quality of life, and compliance.
Menstrual migraine is rarely associated with aura, even in women who have migraine with aura at other times in the cycle.7However, the headaches experienced at the time of menstruation tend to be more severe and longer-lasting and less responsive to medication than are migraines experienced at other times of the month.20
Eliminate the placebo week
Research into the pathogenesis of menstrual migraine has focused on the withdrawal of estrogen in the luteal phase of the menstrual cycle. Ovulation is not a requisite for menstrual migraine attacks, which frequently occur during the hormone-free interval in combination hormonal contraceptive regimens. Several lines of evidence suggest that stabilizing estrogen fluctuations can prevent migraine (FIGURE).7
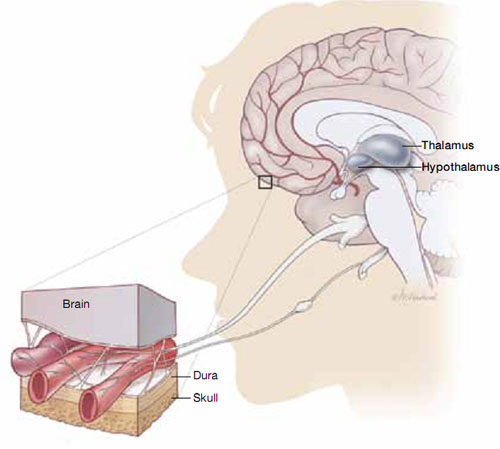
Hormonal fluctuations can trigger migraine
Fluctuations in estrogen during the menstrual cycle may trigger dilation and constriction of blood vessels in the brain, causing migraine.If a patient who has pure menstrual migraine desires to use an estrogen-containing contraceptive, she is likely to be as safe in that choice as a patient without migraine. However, she is not likely to experience improvement in her migraines if she uses a traditional 21/7 active-to-placebo pill regimen. It is necessary to maintain an adequate estrogen level during the placebo week, either through estrogen supplementation or extended-cycle dosing, to prevent the estrogen-withdrawal trigger for headaches.
A few OC regimens reduce the estrogen-free interval to 4 days or provide estrogen supplementation during the placebo week; these regimens may benefit women who have menstrual migraine, although data are scant. If most, or all, of the patient’s migraines are suppressed on combined hormonal contraception, continuous use with rare (e.g., yearly) withdrawals may be indicated.
Alternatives to estrogen-containing contraceptives
If the patient does not desire a combination OC or has other contraindications to estrogen, she may benefit from a progestin-only contraceptive that suppresses ovulation, such as DMPA or the etonogestrel implant. Even with ovulation suppression, however, estrogen fluctuations may occur, and the evidence supporting the use of these methods in the concurrent management of contraceptive needs and menstrual migraine is less clear. Although they are safe in women who have migraine, progestin-only pills and the LNG-IUS do not suppress ovulation reliably enough to be considered useful in managing menstrual migraine.
Take a careful history
Choosing a contraceptive for a woman who has headaches begins the same way as with any other patient: with careful assessment of her short-term and long-term family-planning goals, along with a history and physical to elicit any “red flags,” cultural preferences, and tolerance for specific side effects.
Once you become aware of a history of headache, careful history-taking can usually differentiate between the major headache subtypes and help you avoid limiting contraceptive options unnecessarily.
Women who start any contraceptive may report improvement, worsening, or new onset of headache symptoms. This change usually occurs within the first 3 months, and headaches associated with hormone use tend to improve with continued use.21
In women who have preexisting migraine, you should undertake prompt evaluation and consider a change of contraceptive method in response to 1) any increase in severity or frequency or 2) the onset of associated neurologic symptoms.
We want to hear from you! Tell us what you think.
- The gynecologist’s role in managing menstrual migraine
Anne H. Calhoun, MD (April 2010)
Headaches are highly prevalent in women during their reproductive years. Most are a painful nuisance and do not present a risk of serious morbidity. Some, however, can be dangerous, and the addition of an estrogen-containing contraceptive can increase that risk.
Combination estrogen-progestin contraceptives are effective, popular, and easy to use—but are they safe for women who have headaches? This is a critical question. Some women who have preexisting headaches experience relief with hormonal contraception; others report stable or worsening symptoms; still others do not develop headaches until they begin hormonal contraception.
The differentiation between nuisance and true medical risk in this population depends on an accurate diagnosis of headache subtype. Taking a few moments to confirm whether a patient with headache has a true risk if she chooses hormonal contraception will prevent unnecessary restriction of a method and promote contraceptive success.
In this article, we present three cases that facilitate discussion of the safety, adverse effects, and benefits of various contraceptive strategies in women who have headaches.
Many women who report migraines don’t have them
Most women who report headaches to their gynecologist have not received a clinical diagnosis of headache subtype. They may say that they have “migraines” because that is the term used most commonly in the United States to indicate a severe level of distress with a headache. In actuality, although migraine is common in women, tension-type headaches are more prevalent.
The evaluation of a patient with headaches who is seeking contraception should begin with a simple diagnostic algorithm for headache type. Accurate diagnosis can be made using the International Headache Society (IHS) comprehensive guide for headache subtypes, last updated in 2004.1 TABLE 1, presents a simple classification of chronic headache syndromes, which account for more than 90% of headaches.
TABLE 1
Diagnostic criteria for headache subtypes
| Tension-type | |
| Infrequent episodic | |
| A. | At least 10 episodes <1 day per month on average (<12 days per year) and fulfilling criteria B–D below |
| Frequent episodic | |
| A. | At least 10 episodes occurring ≥1 but <15 days per month for at least 3 months (≥12 and <180 days per year) and fulfilling criteria B–D |
| B. | Headache lasting for 30 minutes to 7 days |
| C. | Headache has at least two of the following characteristics: |
| |
| D. | Both of the following: |
| |
| E. | Not attributable to another disorder |
| Cluster | |
| A. | At least 5 attacks fulfilling criteria B–D |
| B. | Severe or very severe unilateral orbital, supraorbital and/or temporal pain lasting 15–180 minutes if untreated |
| C. | Headache is accompanied by at least one of the following: |
| |
| D. | Attacks have a frequency from one every other day to 8 per day |
| E. | Not attributable to another disorder |
| Migraine without aura | |
| At least 5 attacks fulfilling criteria B–D | |
| A. | Headache attacks lasting 4–72 hours (untreated or successfully treated) |
| B. | Headache has at least two of the following characteristics: |
| |
| C. | During headache at least one of the following: |
| |
| D. | Not attributable to another disorder |
| Typical migraine with aura headache | |
| A. | At least 2 attacks fulfilling criteria B–D |
| B. | Aura consisting of at least one of the following, but no motor weakness: |
| |
| C. | At least two of the following: |
| |
| D. | Headache fulfilling criteria B–D for migraine without aura begins during the aura or follows aura within 60 minutes |
| E. | Not attributable to another disorder |
| Pure menstrual migraine without aura | |
| A. | Attacks, in a menstruating woman, fulfilling criteria for migraine without aura |
| B. | Attacks occur exclusively on Day 1 ±2 days (i.e., Days +2 to –3) of menstruation in at least two out of three menstrual cycles and at no other times of the cycle |
| Estrogen-withdrawal headache | |
| A. | Headache or migraine fulfilling criteria C and D |
| B. | Daily use of exogenous estrogen for >3 weeks, which is interrupted |
| C. | Headache or migraine develops within 5 days after last use of estrogen |
| D. | Headache or migraine resolves within 3 days |
| Exogenous hormone-induced headache | |
| A. | Headache or migraine fulfilling criteria C and D |
| B. | Regular use of exogenous hormones |
| C. | Headache or migraine develops or markedly worsens within 3 months of commencing exogenous hormones |
| D. | Headache or migraine resolves or reverts to its previous pattern within 3 months after total discontinuation of exogenous hormones |
| Source: International Headache Society1 | |
CASE 1: Patient reports a history of migraine
A 21-year-old nulliparous woman has severe dysmenorrhea that has been unresponsive to treatment with nonsteroidal anti-inflammatory drugs (NSAIDs). She also desires contraception. Her primary care provider has recommended combination oral contraceptives (OCs) as a solution to both problems. However, the patient has heard from friends that she should not use OCs because of her history of migraine headache, and she has come to see you for a second opinion.
She describes her headaches as bilateral and reports a “tightening” sensation. The headaches are associated with photophobia and are not aggravated by routine physical activity. They respond to NSAIDs.
She also reports that her mother and sister have been on a prescription medication for migraines for many years.
Is an OC appropriate for this patient?
This young woman’s history is consistent with tension-type headache, not migraine. Tension headache is the most common subtype, with prevalence as high as 59% in women of reproductive age.2 It is generally characterized by mild or moderate pain that is bilateral, pressing, or tightening in quality. The pain does not worsen with routine physical activity. There is no nausea, but photophobia or phonophobia may be present.1
A systematic review of the risk of stroke associated with combination OC use and headaches did not find any studies examining the association between nonmigraine headache and the risk of stroke among combination OC users.3 In contrast to some migraines, however, tension-type headache has not been associated with an increased risk of stroke in the general population. Nor is there evidence that hormonal fluctuations play a role in the pathogenesis or clinical course of tension headache.
In summary, there are no contraindications to combination hormonal contraceptives—including estrogen-progestin OCs, the contraceptive patch, and the contraceptive ring—in women who have tension headache.4
Explore any family history of migraine
The patient in Case 1 appears to have a family history of migraine. Some evidence suggests that such a family history increases the risk of new-onset migraine with use of a combination OC.5 Because the background prevalence of migraine is so high in the population of women likely to use a combination OC, it can be difficult to determine whether worsening headache or development of migraine with OC use is causal or coincidental.
Were this patient to express concern over even a theoretical risk of triggering migraine headache, then a combination OC would probably not be appropriate. In the absence of such concern, however, there is no reason to withhold hormonal contraception. Progestin-only options exist that will provide her with excellent contraceptive efficacy and help relieve her dysmenorrhea:
- the etonogestrel subdermal implant (Implanon)
- depot medroxyprogesterone acetate (DMPA) injection (Depo-Provera)
- the levonorgestrel-releasing intrauterine system (LNG-IUS; Mirena).
Although some women do develop headaches while using progestin-only contraceptives, there is no evidence that such use can trigger a new migraine syndrome in a woman with a family history of such. Again, however, the data are limited.
Progestin methods are safe
The use of progestin-only methods has been promoted in headache sufferers, especially those who have a specific diagnosis of migraine, because progestins do not add to the elevated risk of stroke that accompanies migraine with aura.
Because headache is common in women of reproductive age, it is not surprising that it is listed as a common adverse event for all contraceptives, including progestin-only methods. Evidence that progestin-only methods cause or worsen headaches is slim, however. Preliminary studies indicate that mid-luteal elevations of progesterone or its metabolites could prevent migraine, compared with other times in the cycle.6 Older studies report that a daily oral progestin could prevent migraine in premenopausal women, possibly secondary to induction of anovulation. At the same time, there are clinical reports that DMPA may trigger headache as a side effect in susceptible women.
Generally, then, although progestin-only methods are likely to be safe in all patients with headache, and ovulation suppression may improve the headaches, some patients may experience worsening symptoms.
CASE 2: OC user reports migraine with aura
A 26-year-old mother of one comes to your office for her annual exam. She has used combination OCs for 2 years. She also has a history of severe headaches, which occur four or five times a year. She says the headaches are unilateral, pulsating, and associated with photophobia. The symptoms worsen when she is active and are preceded by a flashing zigzag line that migrates from the center of her visual field to the lateral periphery. The headaches are not associated with her menstrual cycle and have not changed in character or frequency since she began using an OC. She does not smoke.
Should she continue taking an OC?
This patient’s history is consistent with migraine headache with aura. Migraine is a common, disabling primary headache disorder, with an estimated 1-year prevalence in adult women of 15% to 18% and a lifetime prevalence of about 30%.2 Approximately 10% to 20% of people who have migraine experience auras.7
Research on the association between combination OCs, migraine, and stroke has been limited by the rarity of the outcome in the population of concern. Most data come from case-controlled studies and are fettered by a lack of standardized criteria for the diagnosis of migraine (few studies use criteria from the IHS); by recall bias (such as self-reported OC use); and by survivorship bias. Many studies fail to differentiate by the presence of aura, which indicates a different effect on cerebral blood flow patterns than does migraine without aura.
Although most studies attempt to control for the confounding effect of smoking, some do not, and in others the prevalence of smoking is so high it can be difficult to remove from the equation. Some of the studies examining the association between migraine and stroke do not differentiate by gender.
Taking all these variables into account, migraine in women independently appears to carry a twofold to threefold increased risk of ischemic stroke, compared with the risk in similarly aged women who do not have migraine.8 Among women who have a history of migraine, those who use combination OCs are two times to four times more likely to experience ischemic stroke than nonusers are. Among women with the highest risk (combination OC users with migraine), the odds ratio for ischemic stroke ranges from 6 to almost 14, compared with women with the lowest risk (nonusers without migraine).3
To put all this in perspective, the absolute risk of stroke for a 26-year-old nonsmoker like our patient is 6 cases in every 100,000 woman-years.9 Multiplying this risk by a factor of 3 to account for her migraines, and by 3 again to account for her OC use, we can roughly estimate her absolute risk of stroke as about 54 cases for every 100,000 woman-years. Although this absolute risk is extremely low, the outcome can be catastrophic. It behooves us to proceed with caution.
A common misperception among health-care providers is that nausea, vomiting, photophobia, and phonophobia represent migraine aura, when in fact these symptoms are part of the associated diagnostic symptoms of all migraines.
About 20% of people who have migraine experience an aura. The aura begins before the headache and typically lasts 5 to 20 minutes—rarely does it last more than 60 minutes. The headache occurs soon after the aura stops.
The aura may include zigzag lines of light, flashing lights or bright spots, blurred or darkened spots, or focal neurologic symptoms such as numbness or tingling in the fingers of one hand, lips, tongue, or lower face. Auras may involve other senses, such as smell, and can occasionally cause temporary focal weakness or changes in speech.
Presence of aura likely confers greater risk
Many studies of migraine do not explore contraceptive use. They report a higher risk of stroke when aura is present.8,10-15 One of the few prospective studies found no increased risk of stroke in migraineurs who did not experience aura.12
No studies examining a link between combination OCs and ischemic stroke in migraineurs have been large enough to stratify the risk of stroke by the presence or absence of aura. The assumption has been that this risk is amplified by use of combination OCs. Consequently, migraine with aura is designated as an absolute contraindication to the use of combination OCs by the World Health Organization (WHO), ACOG, and the IHS.4,16Although no studies have included women using the contraceptive patch or ring, it is assumed that these methods carry a risk of ischemic stroke similar to that of combination OCs.17 The IHS recommendations on combination hormonal contraception in women with migraine are given in TABLE 2.18
TABLE 2
When combination OCs are appropriate for a woman who has migraine
|
| Source: International Headache Society18 |
Although the patient in Case 2 has been experiencing migraine with aura for some time without a change in headache pattern, combination hormonal contraception is contraindicated. Her history of migraine with aura may have been missed during previous evaluation if she did not consider it to be a “medical problem.” All candidates for combination OCs should be directly questioned about any history of migraine, thrombosis, cigarette smoking, and hypertension.
The patient described in Case 2 should be encouraged to switch to a progestin-only method of contraception or a highly effective nonhormonal method, such as a copper-containing IUD (Paragard). Because she had no change in her headache pattern on ovulation-suppression therapy (OCs), she likely will have no change with continued ovulation suppression (DMPA, subdermal implant) or without it (LNG-IUS, copper lUD).
Be sure to time the switch in methods so that contraception is maintained throughout the transition. This patient would also benefit from referral to a headache specialist for evaluation and treatment.
CASE 3 Perimenstrual headache in a smoker
A 32-year-old mother of two visits your office for contraceptive counseling. She reports that she smokes two to five cigarettes a day and has a history of migraine without aura. Her headaches occur exclusively during the two days just before her period, and they resolve within the first few days of bleeding. NSAIDs provide limited relief. Is hormonal contraception appropriate?
When a woman with perimenstrual headache is choosing a contraceptive method, we need to ensure that she is not exposed to undue risks and focus on improving her quality of life, if possible.
TABLE 1, reviews the diagnostic criteria for pure menstrual migraine, in which symptoms occur only in the perimenstrual period, as in this patient. Most practitioners use a broader definition of menstrual-related migraine, in which women may have other migraine triggers but still experience predictable headaches with menses. More than 50% of women who have migraine report an association between their headaches and menstruation, but only about 10% of women report migraine exclusively with menstruation.7
Hormonal manipulation is not first-line management for menstrual migraine.19 However, for the patient seeking contraception, it is appropriate to consider the effect of a given method on her headaches because that effect is sure to influence her satisfaction, quality of life, and compliance.
Menstrual migraine is rarely associated with aura, even in women who have migraine with aura at other times in the cycle.7However, the headaches experienced at the time of menstruation tend to be more severe and longer-lasting and less responsive to medication than are migraines experienced at other times of the month.20
Eliminate the placebo week
Research into the pathogenesis of menstrual migraine has focused on the withdrawal of estrogen in the luteal phase of the menstrual cycle. Ovulation is not a requisite for menstrual migraine attacks, which frequently occur during the hormone-free interval in combination hormonal contraceptive regimens. Several lines of evidence suggest that stabilizing estrogen fluctuations can prevent migraine (FIGURE).7
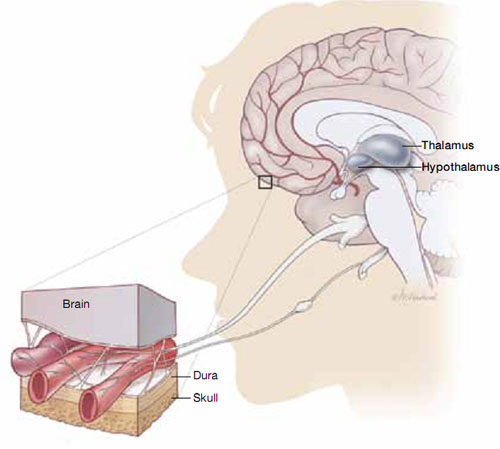
Hormonal fluctuations can trigger migraine
Fluctuations in estrogen during the menstrual cycle may trigger dilation and constriction of blood vessels in the brain, causing migraine.If a patient who has pure menstrual migraine desires to use an estrogen-containing contraceptive, she is likely to be as safe in that choice as a patient without migraine. However, she is not likely to experience improvement in her migraines if she uses a traditional 21/7 active-to-placebo pill regimen. It is necessary to maintain an adequate estrogen level during the placebo week, either through estrogen supplementation or extended-cycle dosing, to prevent the estrogen-withdrawal trigger for headaches.
A few OC regimens reduce the estrogen-free interval to 4 days or provide estrogen supplementation during the placebo week; these regimens may benefit women who have menstrual migraine, although data are scant. If most, or all, of the patient’s migraines are suppressed on combined hormonal contraception, continuous use with rare (e.g., yearly) withdrawals may be indicated.
Alternatives to estrogen-containing contraceptives
If the patient does not desire a combination OC or has other contraindications to estrogen, she may benefit from a progestin-only contraceptive that suppresses ovulation, such as DMPA or the etonogestrel implant. Even with ovulation suppression, however, estrogen fluctuations may occur, and the evidence supporting the use of these methods in the concurrent management of contraceptive needs and menstrual migraine is less clear. Although they are safe in women who have migraine, progestin-only pills and the LNG-IUS do not suppress ovulation reliably enough to be considered useful in managing menstrual migraine.
Take a careful history
Choosing a contraceptive for a woman who has headaches begins the same way as with any other patient: with careful assessment of her short-term and long-term family-planning goals, along with a history and physical to elicit any “red flags,” cultural preferences, and tolerance for specific side effects.
Once you become aware of a history of headache, careful history-taking can usually differentiate between the major headache subtypes and help you avoid limiting contraceptive options unnecessarily.
Women who start any contraceptive may report improvement, worsening, or new onset of headache symptoms. This change usually occurs within the first 3 months, and headaches associated with hormone use tend to improve with continued use.21
In women who have preexisting migraine, you should undertake prompt evaluation and consider a change of contraceptive method in response to 1) any increase in severity or frequency or 2) the onset of associated neurologic symptoms.
We want to hear from you! Tell us what you think.
1. International Headache Society. The international classification of headache disorders: 2nd edition. Cephalalgia. 2004;24(suppl 1):9-160.
2. Rasmussen BK. Epidemiology of headache. Cephalalgia. 2001;21(7):774-777.
3. Curtis KM, Mohllajee AP, Peterson HB. Use of combined oral contraceptives among women with migraine and nonmigrainous headaches: a systematic review. Contraception. 2006;73(2):189-194.
4. Harris M, Kaneshiro B. An evidence-based approach to hormonal contraception and headaches. Contraception. 2009;80(5):417-421.
5. Loder EW, Buse DC, Golub JR. Headache and combination estrogen-progestin oral contraceptives: integrating evidence, guidelines, and clinical practice. Headache. 2005;45(3):224.
6. Martin VT, Behbehani M. Ovarian hormones and migraine headache: understanding mechanisms and pathogenesis— part 2. Headache. 2006;46(3):365-386.
7. Macgregor EA. Menstrual migraine: a clinical review. J Fam Plann Reprod Health Care. 2007;33(1):36-47.
8. Etminan M, Takkouche B, Isorna FC, et al. Risk of ischaemic stroke in people with migraine: systematic review and metaanalysis of observational studies. BMJ. 2005;330(7482):63.-
9. Petitti DB, Sidney S, Quesenberry CP, Jr. Bernstein A. Incidence of stroke and myocardial infarction in women of reproductive age. Stroke. 1997;28(2):280-283.
10. Carolei A, Marini C, De Matteis G. History of migraine and risk of cerebral ischaemia in young adults. Lancet. 1996;347(9014):1503-1506.
11. Chang CL, Donaghy M, Poulter N. Migraine and stroke in young women: case-control study. BMJ. 1999;318(7175):13.
12. Kurth T, Slomke MA, Kase CS, et al. Migraine, headache, and the risk of stroke in women: a prospective study. Neurology. 2005;64(6):1020-1026.
13. MacClellan LR, Giles W, Cole J, et al. Probable migraine with visual aura and risk of ischemic stroke: the stroke prevention in young women study. Stroke. 2007;38(9):2438-2445.
14. Tzourio C, Kittner SJ, Bousser MG, Alperovitch A. Migraine and stroke in young women. Cephalalgia. 2000;20(3):190-199.
15. Tzourio C, Tehindrazanarivelo A, Iglesias S, et al. Case-control study of migraine and risk of ischaemic stroke in young women. BMJ. 1995;310(6983):830-833.
16. ACOG practice bulletin. No. 73: Use of hormonal contraception in women with coexisting medical conditions. Obstet Gynecol. 2006;107(6):1453-1472.
17. Department of Reproductive Health. Medical Eligibility Criteria for Contraceptive Use. 4th ed; 2009. Geneva, Switzerland: World Health Organization; 2010.
18. Bousser MG, Conard J, Kittner S, et al. Recommendations on the risk of ischaemic stroke associated with use of combined oral contraceptives and hormone replacement therapy in women with migraine. The International Headache Society Task Force on Combined Oral Contraceptives & Hormone Replacement Therapy. Cephalalgia. 2000;20(3):155-156.
19. Calhoun AH. The gynecologist’s role in managing menstrual migraine. OBG Manage. 2010;22(4):30-43.
20. Martin VT, Wernke S, Mandell K, et al. Defining the relationship between ovarian hormones and migraine headache. Headache. 2005;45(9):1190-1201.
21. Allais G, Gabellari IC, De Lorenzo C, C, Mana O, Benedetto C. Oral contraceptives in migraine. Expert Rev Neurother. 2009;9(3):381-393.
1. International Headache Society. The international classification of headache disorders: 2nd edition. Cephalalgia. 2004;24(suppl 1):9-160.
2. Rasmussen BK. Epidemiology of headache. Cephalalgia. 2001;21(7):774-777.
3. Curtis KM, Mohllajee AP, Peterson HB. Use of combined oral contraceptives among women with migraine and nonmigrainous headaches: a systematic review. Contraception. 2006;73(2):189-194.
4. Harris M, Kaneshiro B. An evidence-based approach to hormonal contraception and headaches. Contraception. 2009;80(5):417-421.
5. Loder EW, Buse DC, Golub JR. Headache and combination estrogen-progestin oral contraceptives: integrating evidence, guidelines, and clinical practice. Headache. 2005;45(3):224.
6. Martin VT, Behbehani M. Ovarian hormones and migraine headache: understanding mechanisms and pathogenesis— part 2. Headache. 2006;46(3):365-386.
7. Macgregor EA. Menstrual migraine: a clinical review. J Fam Plann Reprod Health Care. 2007;33(1):36-47.
8. Etminan M, Takkouche B, Isorna FC, et al. Risk of ischaemic stroke in people with migraine: systematic review and metaanalysis of observational studies. BMJ. 2005;330(7482):63.-
9. Petitti DB, Sidney S, Quesenberry CP, Jr. Bernstein A. Incidence of stroke and myocardial infarction in women of reproductive age. Stroke. 1997;28(2):280-283.
10. Carolei A, Marini C, De Matteis G. History of migraine and risk of cerebral ischaemia in young adults. Lancet. 1996;347(9014):1503-1506.
11. Chang CL, Donaghy M, Poulter N. Migraine and stroke in young women: case-control study. BMJ. 1999;318(7175):13.
12. Kurth T, Slomke MA, Kase CS, et al. Migraine, headache, and the risk of stroke in women: a prospective study. Neurology. 2005;64(6):1020-1026.
13. MacClellan LR, Giles W, Cole J, et al. Probable migraine with visual aura and risk of ischemic stroke: the stroke prevention in young women study. Stroke. 2007;38(9):2438-2445.
14. Tzourio C, Kittner SJ, Bousser MG, Alperovitch A. Migraine and stroke in young women. Cephalalgia. 2000;20(3):190-199.
15. Tzourio C, Tehindrazanarivelo A, Iglesias S, et al. Case-control study of migraine and risk of ischaemic stroke in young women. BMJ. 1995;310(6983):830-833.
16. ACOG practice bulletin. No. 73: Use of hormonal contraception in women with coexisting medical conditions. Obstet Gynecol. 2006;107(6):1453-1472.
17. Department of Reproductive Health. Medical Eligibility Criteria for Contraceptive Use. 4th ed; 2009. Geneva, Switzerland: World Health Organization; 2010.
18. Bousser MG, Conard J, Kittner S, et al. Recommendations on the risk of ischaemic stroke associated with use of combined oral contraceptives and hormone replacement therapy in women with migraine. The International Headache Society Task Force on Combined Oral Contraceptives & Hormone Replacement Therapy. Cephalalgia. 2000;20(3):155-156.
19. Calhoun AH. The gynecologist’s role in managing menstrual migraine. OBG Manage. 2010;22(4):30-43.
20. Martin VT, Wernke S, Mandell K, et al. Defining the relationship between ovarian hormones and migraine headache. Headache. 2005;45(9):1190-1201.
21. Allais G, Gabellari IC, De Lorenzo C, C, Mana O, Benedetto C. Oral contraceptives in migraine. Expert Rev Neurother. 2009;9(3):381-393.