User login
“How to prepare your patient for the many nuances of postpartum sexuality”
Roya Rezaee, MD; Sheryl Kingsberg, PhD (January 2012)
“Not all contraceptives are suitable immediately postpartum”
Robert L. Barbieri, MD (Editorial, September 2011)
What’s a vital aspect of the care we provide to postpartum patients?
Optimal timing of evaluation for contraception.
Good timing minimizes the likelihood that postpartum contraception will be initiated too early or too late to be effective.
The choice of a contraceptive method for a postpartum woman also requires a careful balancing act. On one side: the risks of contraception to the mother and her new-born. On the other: the risks of unintended pregnancy. Among the concerns that need to be addressed in contraceptive decision-making are:
- whether the woman has resumed sexual intercourse
- infant feeding practices
- risk of venous thromboembolism (VTE)
- logistics of various long-acting reversible contraceptives and tubal sterilization.
In this article, we outline the components of effective contraceptive counseling and decision-making. We also summarize recent recommendations from the Centers for Disease Control and Prevention (CDC) on the use of various contraceptive methods during the postpartum period.
First: Start at 3 weeks
The traditional 6-week postpartum visit was timed to take place after complete involution of the uterus following vaginal delivery. However, involution occurs too late to prevent unintended pregnancy because ovulation can—and often does—occur as early as the fourth postpartum week among nonbreastfeeding women.
In the past, when it was more common to fit a contraceptive diaphragm after pregnancy, 6 weeks may have been the best timing for the visit. Today, given the high safety and efficacy of modern contraceptive methods (even when initiated before complete involution), as well as the importance of safe birth spacing, the routine postpartum visit is more appropriately scheduled at 3 weeks for women who have had an uneventful delivery.
In some cases, of course, it may be appropriate to schedule a visit even earlier, depending on the medical needs of the mother, which may include staple removal after cesarean delivery, follow-up blood pressure assessment for patients who have gestational hypertension, and so on. That said, the first postpartum visit should be routinely scheduled for no later than 3 weeks for healthy women who have had an uncomplicated delivery.1
The data support this approach. In one study, 57% of women reported the resumption of intercourse by the sixth postpartum week.2 A routine 3-week postpartum visit instead of a visit at 6 weeks would reduce unmet contraceptive need among this group of women.
How infant feeding practices come into play
Both the American Congress of Obstetricians and Gynecologists (ACOG) and the American Academy of Pediatrics recommend 6 months of exclusive breastfeeding because of recognized health benefits for both the mother and her infant. Exclusive breastfeeding is also a requirement if a woman desires to use breastfeeding as a contraceptive method.
Healthy People 2010 is a set of US health objectives that includes goals for breastfeeding rates. Although the percentage of infants who were ever breastfed has reached the 75% target of Healthy People 2010, according to data from the National Health and Nutrition Examination Survey (NHANES), the percentage of infants who were breastfed at 6 months of age has changed only minimally.3 For Mexican-American infants, that rate is 40%, compared with 35% for non-Hispanic whites and 20% for non-Hispanic black infants.3 Rates of exclusive breastfeeding are even lower, highlighting the importance of early breastfeeding support and contraceptive guidance during the postpartum period—support and guidance that can be offered at a 3-week postpartum visit.
Extent of breastfeeding needs to be assessed
Full or nearly full breastfeeding should be encouraged, along with frequent feeding of the infant. In addition, the contraceptive effect of lactation during the first 6 months of breastfeeding should be emphasized (see the sidebar on the lactational amenorrhea method [LAM] of contraception). Keep in mind, however, that a substantial number of nursing mothers who are not breastfeeding exclusively will ovulate before the 6-week postpartum visit. Data suggest that approximately 50% of all nonbreastfeeding women will ovulate before the 6-week visit, with some ovulating as early as postpartum day 25.4
For this reason, you need to determine the extent of breastfeeding at the 3-week visit to determine whether LAM is a contraceptive option for your patient. “Full or nearly full” breastfeeding means that the vast majority of feeding is breastfeeding and that breastfeeding is not replaced by any other kind of feeding. “Frequent feeding” means that the infant is breastfed when hungry, be it day or night, which implies at least one night-time feeding. If evaluation at the 3-week visit indicates that breastfeeding is no longer full or nearly full and frequent, another form of contraception should be initiated.5
For most women, the benefits of initiating a progestin-only or nonhormonal method of contraception at this time outweigh the risks, regardless of breastfeeding status, according to the CDC’s medical eligibility criteria for contraceptive use.6
the patient knows how to use it
The lactational amenorrhea method (LAM) of contraception requires fertility awareness, exclusive breastfeeding, and an ability to recognize the physiologic signs and circumstances that suggest that ovulation is resuming.
How does it work?
Elevated prolactin levels in breastfeeding women inhibit the normal pulsatile secretion of gonadotropin-releasing hormone (GnRH), suppressing the secretion of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the pituitary, thereby inhibiting ovulation (FIGURE).9
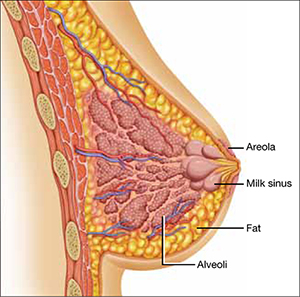
Nipple stimulation from breastfeeding causes the pituitary gland to release prolactin—the hormone that acts at the alveolar secretory cells of the breast to stimulate lactogenesis and at the hypothalamus to decrease the pulsatile release of GnRH. Suckling increases the plasma level of prolactin markedly within 10 minutes of its initiation.
There are three rules for effective use of LAM:
- The infant must be fully or nearly fully breastfed. Prolactin remains elevated for approximately 3 hours, which is about the time it takes for hunger to resume after a feeding of breast milk. Clearly, this level of breastfeeding requires at least one night-time feeding. If cow’s milk formula is given to supplement breastfeeding, its greater fat content slows transit time and prolongs the feeding interval. The result is a decreased prolactin level that may allow FSH and LH to rise and eventually trigger ovulation.
- The woman should be alert for vaginal bleeding after postpartum day 56, which could signal the return of menstruation. The duration of lochia is variable and can make it difficult to detect the onset of menstrual bleeding. In a study by the World Health Organization (WHO), postpartum lochia was present from a minimum of 2 days to a maximum of 90 days, with an average duration of 27 days.10 Most women with LAM will not experience true menstrual bleeding before postpartum day 56 (8 weeks). The frequency of breastfeeding has no effect on the duration of postpartum lochia.
- LAM should be used as contraception only during the first 6 months postpartum. After 6 months, even fully breastfeeding mothers begin to ovulate.
Breast pumping might not maintain an adequate prolactin level
When a woman is separated from her infant, breast pumping has been shown to stimulate the release of prolactin at a level comparable to actual breastfeeding.11 However, women separated from their infant tend to pump less often than they would breastfeed, which can lead to an increased frequency of ovulation and conception.11 Because it is difficult for women to pump at a sufficient frequency to reliably suppress ovulation, the increased risk of pregnancy should be anticipated, and another form of contraception should be encouraged.
What the data show
The WHO conducted a large prospective study examining the relationship between infant feeding and amenorrhea, as well as the rate of pregnancy during LAM. Women who were still breastfeeding and remained amenorrheic had a pregnancy rate of 0.8% at 6 months.10
How the risk of VTE affects the choice of contraceptive
The hematologic changes of normal pregnancy shift coagulability and fibrinolytic systems toward a state of hypercoagulability. This physiologic process reduces the risk of puerperal hemorrhage; however, it also predisposes women to VTE during pregnancy and into the postpartum period. Studies assessing the risk of VTE in postpartum women indicate that it increases by a factor of 22 to 84 during the first 6 weeks, compared with the risk in nonpregnant, nonpostpartum women of reproductive age.7 This heightened risk is most pronounced immediately after delivery, declining rapidly over the first 21 days after delivery and returning to a near-baseline level by 42 days postpartum.
By the time of the recommended 3-week postpartum visit, the period of highest VTE risk has passed. For women who are no longer breastfeeding, the benefits of all hormonal contraceptive methods, including those that contain estrogen, outweigh their risks, according to a newly released update to recommendations from the CDC (TABLE).6 Although combined oral contraceptives are known to increase the risk of VTE by a factor of 3 to 7, data suggest that healthy women who do not have additional risk factors for VTE (e.g., thrombophilia, obesity, smoking, or age of 35 years or older) can use them safely.6
The updated recommendations discourage the use of estrogen-containing contraceptives before 21 days postpartum because they present an unacceptable level of risk (regardless of breastfeeding status), but they allow the use of combined hormonal contraceptives among otherwise healthy breastfeeding women after 30 days postpartum. For women who have additional risk factors for VTE, the risks of combined hormonal contraceptives outweigh the benefits until 6 weeks postpartum, regardless of breastfeeding status.6
In contrast, progestin-only and nonhormonal contraceptive methods can be safely initiated by both breastfeeding and nonbreastfeeding women before 21 days postpartum, which means that women can begin using them before discharge from the hospital.
Updated recommendations for use of combined hormonal contraceptives during the postpartum period*
| Time since delivery | Recommendation | Clarification |
|---|---|---|
| Nonbreastfeeding women | ||
| <21 days | Combined hormonal contraception not recommended | Presents an unacceptable health risk |
| 21–42 days | Not recommended for women who have other risk factors for VTE (e.g., age ≥35 years, previous VTE, thrombophilia, immobility, transfusion at delivery, BMI ≥30, postpartum hemorrhage, cesarean delivery, preeclampsia or smoking) Acceptable for women who do not have other risk factors for VTE | Theoretical or proven risks usually outweigh advantages in women who have risk factors for VTE Advantages generally outweigh the theoretical or proven risks in women who do not have other risk factors for VTE |
| >42 days | Recommended | No restrictions |
| Breastfeeding women | ||
| <21 days | Not recommended | Presents an unacceptable health risk |
| 21–29 days | Not recommended for women who have other risk factors for VTE (e.g., age ≥35 years, previous VTE, thrombophilia, immobility, transfusion at delivery, BMI ≥30, postpartum hemorrhage, cesarean delivery, preeclampsia or smoking) Not recommended for women who do not have other risk factors for VTE | Theoretical or proven risks usually outweigh advantages |
| 30–42 days | Not recommended for women who have other risk factors for VTE (e.g., age ≥35 years, previous VTE, thrombophilia, immobility, transfusion at delivery, BMI ≥30, postpartum hemorrhage, cesarean delivery, preeclampsia or smoking) Acceptable for women who do not have other risk factors for VTE | Theoretical or proven risks usually outweigh advantages in women who have risk factors for VTE Advantages generally outweigh the theoretical or proven risks in women who do not have other risk factors for VTE |
| >42 days | Acceptable | Advantages generally outweigh the theoretical or proven risks |
| VTE = venous thromboembolism, BMI = body mass index * Includes combined oral contraceptives, combined hormonal patch, and combined vaginal ring SOURCE: Adapted from CDC6 | ||
When to consider LARC or sterilization
Long-acting reversible contraceptives (LARC) are an important postpartum contraceptive option because they offer highly effective protection against pregnancy that can begin as soon as the placenta is delivered. LARC methods include contraceptive implants and intrauterine devices (IUDs).
According to the CDC’s medical eligibility criteria for contraceptive use, contraceptive implants can be placed immediately after delivery of the placenta without restriction.8
The copper IUD can be placed within 10 minutes after delivery of the placenta without restriction. If this window is missed, the benefits of inserting the IUD still outweigh the risks. Because 4 weeks postpartum is another time when the copper IUD can be inserted without restriction, the 3-week visit is a reasonable time to screen and schedule a patient for insertion.
The benefits of insertion of the levonorgestrel-releasing intrauterine system (LNG-IUS) are also believed to outweigh the risks before 4 weeks postpartum. Like the copper IUD, the LNG-IUS can be inserted without restriction at 4 weeks postpartum or later.
There is no need for a pelvic exam at the 3-week postpartum visit among women who undergo immediate postplacental insertion of the copper IUD or LNG-IUS. In fact, women can delay the exam until involution is complete.
Sterilization is best after complete involution
Interval tubal sterilization by laparoscopic, bilateral tubal fulguration or hysteroscopic microinsert placement is one of the most effective ways to prevent pregnancy. Both methods are best performed after the completion of involution and the return of normal coagulation; scheduling can take place at the 3-week postpartum visit.
Given the benefit of depot medroxyprogesterone acetate (DMPA) in endometrial suppression before hysteroscopic sterilization, it is reasonable to consider administering DMPA at the 3-week postpartum visit in anticipation of surgery after involution is complete.
The bottom line
Because most contraceptive methods can be safely initiated at or shortly after a 3-weeks’ postpartum visit, there is no longer any reason to time the routine postpartum visit to coincide with the completion of involution. For healthy women who have had an uneventful delivery, the routine postpartum visit should occur at 3 weeks.
We want to hear from you! Tell us what you think.
1. Speroff L, Mishell DR. The postpartum visit: it’s time for a change in order to optimally initiate contraception. Contraception. 2008;78(2):90-98.
2. Connolly A, Thorp J, Pahel L. Effects of pregnancy and childbirth on postpartum sexual function: a longitudinal prospective study. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(4):263-267.
3. McDowell MA, Wang C-Y, Kennedy-Stephenson J. Breastfeeding in the United States: Findings from the National Health and Nutrition Examination Surveys 1999–2006. NCHS Data Briefs. 2008;5:1-8.
4. Jackson E, Glasier A. Return of ovulation and menses in postpartum nonlactatinglactating women: a systematic review. Obstet Gynecol. 2011;117(3):657-662.
5. Kennedy K, Rivera R, McNeilly A. Consensus statement on the use of breastfeeding as a family planning method. Contraception. 1988;39(5):477-496.
6. Centers for Disease Control and Prevention. Update to CDC’s US Medical Eligibility Criteria for Contraceptive Use 2010: Revised recommendations for the use of contraceptive methods during the postpartum period. MMWR. 2011;60(26):878-883.
7. Jackson E, Curtis K, Gaffield M. Risk of venous thromboembolism during the postpartum period: a systematic review. Obstet Gynecol. 2011;117(3):691-703.
8. Centers for Disease Control and Prevention. US Medical Eligibility Criteria for Contraceptive Use 2010. MMWR. 2010;59(No. RR-4):1-86.
9. Kletzky OA, Marrs RP, Howard WF, McCormick W, Mishell DR Jr. Prolactin synthesis and release during pregnancy and puerperium. Am J Obstet Gynecol. 1980;136(4):545-550.
10. Labbok MH, Hight-Laukaran V, Peterson AE, Fletcher V, von Hertzen H, Van Look PF. Multicenter study of the Lactional Amenorrhea Method (LAM): I. Efficacy duration, and implications for clinical application. Contraception. 1997;55(6):327-336.
11. Valdes V, Labbok MH, Pugin E, Perez A. The efficacy of the Lactational Amenorrhea Method (LAM) among working women. Contraception. 2000;62(5):217-219.
“How to prepare your patient for the many nuances of postpartum sexuality”
Roya Rezaee, MD; Sheryl Kingsberg, PhD (January 2012)
“Not all contraceptives are suitable immediately postpartum”
Robert L. Barbieri, MD (Editorial, September 2011)
What’s a vital aspect of the care we provide to postpartum patients?
Optimal timing of evaluation for contraception.
Good timing minimizes the likelihood that postpartum contraception will be initiated too early or too late to be effective.
The choice of a contraceptive method for a postpartum woman also requires a careful balancing act. On one side: the risks of contraception to the mother and her new-born. On the other: the risks of unintended pregnancy. Among the concerns that need to be addressed in contraceptive decision-making are:
- whether the woman has resumed sexual intercourse
- infant feeding practices
- risk of venous thromboembolism (VTE)
- logistics of various long-acting reversible contraceptives and tubal sterilization.
In this article, we outline the components of effective contraceptive counseling and decision-making. We also summarize recent recommendations from the Centers for Disease Control and Prevention (CDC) on the use of various contraceptive methods during the postpartum period.
First: Start at 3 weeks
The traditional 6-week postpartum visit was timed to take place after complete involution of the uterus following vaginal delivery. However, involution occurs too late to prevent unintended pregnancy because ovulation can—and often does—occur as early as the fourth postpartum week among nonbreastfeeding women.
In the past, when it was more common to fit a contraceptive diaphragm after pregnancy, 6 weeks may have been the best timing for the visit. Today, given the high safety and efficacy of modern contraceptive methods (even when initiated before complete involution), as well as the importance of safe birth spacing, the routine postpartum visit is more appropriately scheduled at 3 weeks for women who have had an uneventful delivery.
In some cases, of course, it may be appropriate to schedule a visit even earlier, depending on the medical needs of the mother, which may include staple removal after cesarean delivery, follow-up blood pressure assessment for patients who have gestational hypertension, and so on. That said, the first postpartum visit should be routinely scheduled for no later than 3 weeks for healthy women who have had an uncomplicated delivery.1
The data support this approach. In one study, 57% of women reported the resumption of intercourse by the sixth postpartum week.2 A routine 3-week postpartum visit instead of a visit at 6 weeks would reduce unmet contraceptive need among this group of women.
How infant feeding practices come into play
Both the American Congress of Obstetricians and Gynecologists (ACOG) and the American Academy of Pediatrics recommend 6 months of exclusive breastfeeding because of recognized health benefits for both the mother and her infant. Exclusive breastfeeding is also a requirement if a woman desires to use breastfeeding as a contraceptive method.
Healthy People 2010 is a set of US health objectives that includes goals for breastfeeding rates. Although the percentage of infants who were ever breastfed has reached the 75% target of Healthy People 2010, according to data from the National Health and Nutrition Examination Survey (NHANES), the percentage of infants who were breastfed at 6 months of age has changed only minimally.3 For Mexican-American infants, that rate is 40%, compared with 35% for non-Hispanic whites and 20% for non-Hispanic black infants.3 Rates of exclusive breastfeeding are even lower, highlighting the importance of early breastfeeding support and contraceptive guidance during the postpartum period—support and guidance that can be offered at a 3-week postpartum visit.
Extent of breastfeeding needs to be assessed
Full or nearly full breastfeeding should be encouraged, along with frequent feeding of the infant. In addition, the contraceptive effect of lactation during the first 6 months of breastfeeding should be emphasized (see the sidebar on the lactational amenorrhea method [LAM] of contraception). Keep in mind, however, that a substantial number of nursing mothers who are not breastfeeding exclusively will ovulate before the 6-week postpartum visit. Data suggest that approximately 50% of all nonbreastfeeding women will ovulate before the 6-week visit, with some ovulating as early as postpartum day 25.4
For this reason, you need to determine the extent of breastfeeding at the 3-week visit to determine whether LAM is a contraceptive option for your patient. “Full or nearly full” breastfeeding means that the vast majority of feeding is breastfeeding and that breastfeeding is not replaced by any other kind of feeding. “Frequent feeding” means that the infant is breastfed when hungry, be it day or night, which implies at least one night-time feeding. If evaluation at the 3-week visit indicates that breastfeeding is no longer full or nearly full and frequent, another form of contraception should be initiated.5
For most women, the benefits of initiating a progestin-only or nonhormonal method of contraception at this time outweigh the risks, regardless of breastfeeding status, according to the CDC’s medical eligibility criteria for contraceptive use.6
the patient knows how to use it
The lactational amenorrhea method (LAM) of contraception requires fertility awareness, exclusive breastfeeding, and an ability to recognize the physiologic signs and circumstances that suggest that ovulation is resuming.
How does it work?
Elevated prolactin levels in breastfeeding women inhibit the normal pulsatile secretion of gonadotropin-releasing hormone (GnRH), suppressing the secretion of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the pituitary, thereby inhibiting ovulation (FIGURE).9
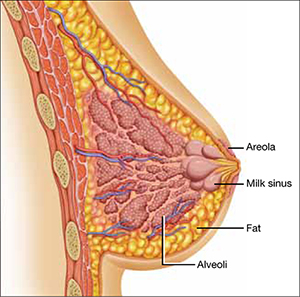
Nipple stimulation from breastfeeding causes the pituitary gland to release prolactin—the hormone that acts at the alveolar secretory cells of the breast to stimulate lactogenesis and at the hypothalamus to decrease the pulsatile release of GnRH. Suckling increases the plasma level of prolactin markedly within 10 minutes of its initiation.
There are three rules for effective use of LAM:
- The infant must be fully or nearly fully breastfed. Prolactin remains elevated for approximately 3 hours, which is about the time it takes for hunger to resume after a feeding of breast milk. Clearly, this level of breastfeeding requires at least one night-time feeding. If cow’s milk formula is given to supplement breastfeeding, its greater fat content slows transit time and prolongs the feeding interval. The result is a decreased prolactin level that may allow FSH and LH to rise and eventually trigger ovulation.
- The woman should be alert for vaginal bleeding after postpartum day 56, which could signal the return of menstruation. The duration of lochia is variable and can make it difficult to detect the onset of menstrual bleeding. In a study by the World Health Organization (WHO), postpartum lochia was present from a minimum of 2 days to a maximum of 90 days, with an average duration of 27 days.10 Most women with LAM will not experience true menstrual bleeding before postpartum day 56 (8 weeks). The frequency of breastfeeding has no effect on the duration of postpartum lochia.
- LAM should be used as contraception only during the first 6 months postpartum. After 6 months, even fully breastfeeding mothers begin to ovulate.
Breast pumping might not maintain an adequate prolactin level
When a woman is separated from her infant, breast pumping has been shown to stimulate the release of prolactin at a level comparable to actual breastfeeding.11 However, women separated from their infant tend to pump less often than they would breastfeed, which can lead to an increased frequency of ovulation and conception.11 Because it is difficult for women to pump at a sufficient frequency to reliably suppress ovulation, the increased risk of pregnancy should be anticipated, and another form of contraception should be encouraged.
What the data show
The WHO conducted a large prospective study examining the relationship between infant feeding and amenorrhea, as well as the rate of pregnancy during LAM. Women who were still breastfeeding and remained amenorrheic had a pregnancy rate of 0.8% at 6 months.10
How the risk of VTE affects the choice of contraceptive
The hematologic changes of normal pregnancy shift coagulability and fibrinolytic systems toward a state of hypercoagulability. This physiologic process reduces the risk of puerperal hemorrhage; however, it also predisposes women to VTE during pregnancy and into the postpartum period. Studies assessing the risk of VTE in postpartum women indicate that it increases by a factor of 22 to 84 during the first 6 weeks, compared with the risk in nonpregnant, nonpostpartum women of reproductive age.7 This heightened risk is most pronounced immediately after delivery, declining rapidly over the first 21 days after delivery and returning to a near-baseline level by 42 days postpartum.
By the time of the recommended 3-week postpartum visit, the period of highest VTE risk has passed. For women who are no longer breastfeeding, the benefits of all hormonal contraceptive methods, including those that contain estrogen, outweigh their risks, according to a newly released update to recommendations from the CDC (TABLE).6 Although combined oral contraceptives are known to increase the risk of VTE by a factor of 3 to 7, data suggest that healthy women who do not have additional risk factors for VTE (e.g., thrombophilia, obesity, smoking, or age of 35 years or older) can use them safely.6
The updated recommendations discourage the use of estrogen-containing contraceptives before 21 days postpartum because they present an unacceptable level of risk (regardless of breastfeeding status), but they allow the use of combined hormonal contraceptives among otherwise healthy breastfeeding women after 30 days postpartum. For women who have additional risk factors for VTE, the risks of combined hormonal contraceptives outweigh the benefits until 6 weeks postpartum, regardless of breastfeeding status.6
In contrast, progestin-only and nonhormonal contraceptive methods can be safely initiated by both breastfeeding and nonbreastfeeding women before 21 days postpartum, which means that women can begin using them before discharge from the hospital.
Updated recommendations for use of combined hormonal contraceptives during the postpartum period*
| Time since delivery | Recommendation | Clarification |
|---|---|---|
| Nonbreastfeeding women | ||
| <21 days | Combined hormonal contraception not recommended | Presents an unacceptable health risk |
| 21–42 days | Not recommended for women who have other risk factors for VTE (e.g., age ≥35 years, previous VTE, thrombophilia, immobility, transfusion at delivery, BMI ≥30, postpartum hemorrhage, cesarean delivery, preeclampsia or smoking) Acceptable for women who do not have other risk factors for VTE | Theoretical or proven risks usually outweigh advantages in women who have risk factors for VTE Advantages generally outweigh the theoretical or proven risks in women who do not have other risk factors for VTE |
| >42 days | Recommended | No restrictions |
| Breastfeeding women | ||
| <21 days | Not recommended | Presents an unacceptable health risk |
| 21–29 days | Not recommended for women who have other risk factors for VTE (e.g., age ≥35 years, previous VTE, thrombophilia, immobility, transfusion at delivery, BMI ≥30, postpartum hemorrhage, cesarean delivery, preeclampsia or smoking) Not recommended for women who do not have other risk factors for VTE | Theoretical or proven risks usually outweigh advantages |
| 30–42 days | Not recommended for women who have other risk factors for VTE (e.g., age ≥35 years, previous VTE, thrombophilia, immobility, transfusion at delivery, BMI ≥30, postpartum hemorrhage, cesarean delivery, preeclampsia or smoking) Acceptable for women who do not have other risk factors for VTE | Theoretical or proven risks usually outweigh advantages in women who have risk factors for VTE Advantages generally outweigh the theoretical or proven risks in women who do not have other risk factors for VTE |
| >42 days | Acceptable | Advantages generally outweigh the theoretical or proven risks |
| VTE = venous thromboembolism, BMI = body mass index * Includes combined oral contraceptives, combined hormonal patch, and combined vaginal ring SOURCE: Adapted from CDC6 | ||
When to consider LARC or sterilization
Long-acting reversible contraceptives (LARC) are an important postpartum contraceptive option because they offer highly effective protection against pregnancy that can begin as soon as the placenta is delivered. LARC methods include contraceptive implants and intrauterine devices (IUDs).
According to the CDC’s medical eligibility criteria for contraceptive use, contraceptive implants can be placed immediately after delivery of the placenta without restriction.8
The copper IUD can be placed within 10 minutes after delivery of the placenta without restriction. If this window is missed, the benefits of inserting the IUD still outweigh the risks. Because 4 weeks postpartum is another time when the copper IUD can be inserted without restriction, the 3-week visit is a reasonable time to screen and schedule a patient for insertion.
The benefits of insertion of the levonorgestrel-releasing intrauterine system (LNG-IUS) are also believed to outweigh the risks before 4 weeks postpartum. Like the copper IUD, the LNG-IUS can be inserted without restriction at 4 weeks postpartum or later.
There is no need for a pelvic exam at the 3-week postpartum visit among women who undergo immediate postplacental insertion of the copper IUD or LNG-IUS. In fact, women can delay the exam until involution is complete.
Sterilization is best after complete involution
Interval tubal sterilization by laparoscopic, bilateral tubal fulguration or hysteroscopic microinsert placement is one of the most effective ways to prevent pregnancy. Both methods are best performed after the completion of involution and the return of normal coagulation; scheduling can take place at the 3-week postpartum visit.
Given the benefit of depot medroxyprogesterone acetate (DMPA) in endometrial suppression before hysteroscopic sterilization, it is reasonable to consider administering DMPA at the 3-week postpartum visit in anticipation of surgery after involution is complete.
The bottom line
Because most contraceptive methods can be safely initiated at or shortly after a 3-weeks’ postpartum visit, there is no longer any reason to time the routine postpartum visit to coincide with the completion of involution. For healthy women who have had an uneventful delivery, the routine postpartum visit should occur at 3 weeks.
We want to hear from you! Tell us what you think.
“How to prepare your patient for the many nuances of postpartum sexuality”
Roya Rezaee, MD; Sheryl Kingsberg, PhD (January 2012)
“Not all contraceptives are suitable immediately postpartum”
Robert L. Barbieri, MD (Editorial, September 2011)
What’s a vital aspect of the care we provide to postpartum patients?
Optimal timing of evaluation for contraception.
Good timing minimizes the likelihood that postpartum contraception will be initiated too early or too late to be effective.
The choice of a contraceptive method for a postpartum woman also requires a careful balancing act. On one side: the risks of contraception to the mother and her new-born. On the other: the risks of unintended pregnancy. Among the concerns that need to be addressed in contraceptive decision-making are:
- whether the woman has resumed sexual intercourse
- infant feeding practices
- risk of venous thromboembolism (VTE)
- logistics of various long-acting reversible contraceptives and tubal sterilization.
In this article, we outline the components of effective contraceptive counseling and decision-making. We also summarize recent recommendations from the Centers for Disease Control and Prevention (CDC) on the use of various contraceptive methods during the postpartum period.
First: Start at 3 weeks
The traditional 6-week postpartum visit was timed to take place after complete involution of the uterus following vaginal delivery. However, involution occurs too late to prevent unintended pregnancy because ovulation can—and often does—occur as early as the fourth postpartum week among nonbreastfeeding women.
In the past, when it was more common to fit a contraceptive diaphragm after pregnancy, 6 weeks may have been the best timing for the visit. Today, given the high safety and efficacy of modern contraceptive methods (even when initiated before complete involution), as well as the importance of safe birth spacing, the routine postpartum visit is more appropriately scheduled at 3 weeks for women who have had an uneventful delivery.
In some cases, of course, it may be appropriate to schedule a visit even earlier, depending on the medical needs of the mother, which may include staple removal after cesarean delivery, follow-up blood pressure assessment for patients who have gestational hypertension, and so on. That said, the first postpartum visit should be routinely scheduled for no later than 3 weeks for healthy women who have had an uncomplicated delivery.1
The data support this approach. In one study, 57% of women reported the resumption of intercourse by the sixth postpartum week.2 A routine 3-week postpartum visit instead of a visit at 6 weeks would reduce unmet contraceptive need among this group of women.
How infant feeding practices come into play
Both the American Congress of Obstetricians and Gynecologists (ACOG) and the American Academy of Pediatrics recommend 6 months of exclusive breastfeeding because of recognized health benefits for both the mother and her infant. Exclusive breastfeeding is also a requirement if a woman desires to use breastfeeding as a contraceptive method.
Healthy People 2010 is a set of US health objectives that includes goals for breastfeeding rates. Although the percentage of infants who were ever breastfed has reached the 75% target of Healthy People 2010, according to data from the National Health and Nutrition Examination Survey (NHANES), the percentage of infants who were breastfed at 6 months of age has changed only minimally.3 For Mexican-American infants, that rate is 40%, compared with 35% for non-Hispanic whites and 20% for non-Hispanic black infants.3 Rates of exclusive breastfeeding are even lower, highlighting the importance of early breastfeeding support and contraceptive guidance during the postpartum period—support and guidance that can be offered at a 3-week postpartum visit.
Extent of breastfeeding needs to be assessed
Full or nearly full breastfeeding should be encouraged, along with frequent feeding of the infant. In addition, the contraceptive effect of lactation during the first 6 months of breastfeeding should be emphasized (see the sidebar on the lactational amenorrhea method [LAM] of contraception). Keep in mind, however, that a substantial number of nursing mothers who are not breastfeeding exclusively will ovulate before the 6-week postpartum visit. Data suggest that approximately 50% of all nonbreastfeeding women will ovulate before the 6-week visit, with some ovulating as early as postpartum day 25.4
For this reason, you need to determine the extent of breastfeeding at the 3-week visit to determine whether LAM is a contraceptive option for your patient. “Full or nearly full” breastfeeding means that the vast majority of feeding is breastfeeding and that breastfeeding is not replaced by any other kind of feeding. “Frequent feeding” means that the infant is breastfed when hungry, be it day or night, which implies at least one night-time feeding. If evaluation at the 3-week visit indicates that breastfeeding is no longer full or nearly full and frequent, another form of contraception should be initiated.5
For most women, the benefits of initiating a progestin-only or nonhormonal method of contraception at this time outweigh the risks, regardless of breastfeeding status, according to the CDC’s medical eligibility criteria for contraceptive use.6
the patient knows how to use it
The lactational amenorrhea method (LAM) of contraception requires fertility awareness, exclusive breastfeeding, and an ability to recognize the physiologic signs and circumstances that suggest that ovulation is resuming.
How does it work?
Elevated prolactin levels in breastfeeding women inhibit the normal pulsatile secretion of gonadotropin-releasing hormone (GnRH), suppressing the secretion of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the pituitary, thereby inhibiting ovulation (FIGURE).9
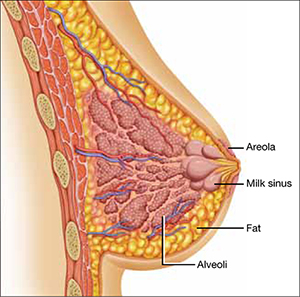
Nipple stimulation from breastfeeding causes the pituitary gland to release prolactin—the hormone that acts at the alveolar secretory cells of the breast to stimulate lactogenesis and at the hypothalamus to decrease the pulsatile release of GnRH. Suckling increases the plasma level of prolactin markedly within 10 minutes of its initiation.
There are three rules for effective use of LAM:
- The infant must be fully or nearly fully breastfed. Prolactin remains elevated for approximately 3 hours, which is about the time it takes for hunger to resume after a feeding of breast milk. Clearly, this level of breastfeeding requires at least one night-time feeding. If cow’s milk formula is given to supplement breastfeeding, its greater fat content slows transit time and prolongs the feeding interval. The result is a decreased prolactin level that may allow FSH and LH to rise and eventually trigger ovulation.
- The woman should be alert for vaginal bleeding after postpartum day 56, which could signal the return of menstruation. The duration of lochia is variable and can make it difficult to detect the onset of menstrual bleeding. In a study by the World Health Organization (WHO), postpartum lochia was present from a minimum of 2 days to a maximum of 90 days, with an average duration of 27 days.10 Most women with LAM will not experience true menstrual bleeding before postpartum day 56 (8 weeks). The frequency of breastfeeding has no effect on the duration of postpartum lochia.
- LAM should be used as contraception only during the first 6 months postpartum. After 6 months, even fully breastfeeding mothers begin to ovulate.
Breast pumping might not maintain an adequate prolactin level
When a woman is separated from her infant, breast pumping has been shown to stimulate the release of prolactin at a level comparable to actual breastfeeding.11 However, women separated from their infant tend to pump less often than they would breastfeed, which can lead to an increased frequency of ovulation and conception.11 Because it is difficult for women to pump at a sufficient frequency to reliably suppress ovulation, the increased risk of pregnancy should be anticipated, and another form of contraception should be encouraged.
What the data show
The WHO conducted a large prospective study examining the relationship between infant feeding and amenorrhea, as well as the rate of pregnancy during LAM. Women who were still breastfeeding and remained amenorrheic had a pregnancy rate of 0.8% at 6 months.10
How the risk of VTE affects the choice of contraceptive
The hematologic changes of normal pregnancy shift coagulability and fibrinolytic systems toward a state of hypercoagulability. This physiologic process reduces the risk of puerperal hemorrhage; however, it also predisposes women to VTE during pregnancy and into the postpartum period. Studies assessing the risk of VTE in postpartum women indicate that it increases by a factor of 22 to 84 during the first 6 weeks, compared with the risk in nonpregnant, nonpostpartum women of reproductive age.7 This heightened risk is most pronounced immediately after delivery, declining rapidly over the first 21 days after delivery and returning to a near-baseline level by 42 days postpartum.
By the time of the recommended 3-week postpartum visit, the period of highest VTE risk has passed. For women who are no longer breastfeeding, the benefits of all hormonal contraceptive methods, including those that contain estrogen, outweigh their risks, according to a newly released update to recommendations from the CDC (TABLE).6 Although combined oral contraceptives are known to increase the risk of VTE by a factor of 3 to 7, data suggest that healthy women who do not have additional risk factors for VTE (e.g., thrombophilia, obesity, smoking, or age of 35 years or older) can use them safely.6
The updated recommendations discourage the use of estrogen-containing contraceptives before 21 days postpartum because they present an unacceptable level of risk (regardless of breastfeeding status), but they allow the use of combined hormonal contraceptives among otherwise healthy breastfeeding women after 30 days postpartum. For women who have additional risk factors for VTE, the risks of combined hormonal contraceptives outweigh the benefits until 6 weeks postpartum, regardless of breastfeeding status.6
In contrast, progestin-only and nonhormonal contraceptive methods can be safely initiated by both breastfeeding and nonbreastfeeding women before 21 days postpartum, which means that women can begin using them before discharge from the hospital.
Updated recommendations for use of combined hormonal contraceptives during the postpartum period*
| Time since delivery | Recommendation | Clarification |
|---|---|---|
| Nonbreastfeeding women | ||
| <21 days | Combined hormonal contraception not recommended | Presents an unacceptable health risk |
| 21–42 days | Not recommended for women who have other risk factors for VTE (e.g., age ≥35 years, previous VTE, thrombophilia, immobility, transfusion at delivery, BMI ≥30, postpartum hemorrhage, cesarean delivery, preeclampsia or smoking) Acceptable for women who do not have other risk factors for VTE | Theoretical or proven risks usually outweigh advantages in women who have risk factors for VTE Advantages generally outweigh the theoretical or proven risks in women who do not have other risk factors for VTE |
| >42 days | Recommended | No restrictions |
| Breastfeeding women | ||
| <21 days | Not recommended | Presents an unacceptable health risk |
| 21–29 days | Not recommended for women who have other risk factors for VTE (e.g., age ≥35 years, previous VTE, thrombophilia, immobility, transfusion at delivery, BMI ≥30, postpartum hemorrhage, cesarean delivery, preeclampsia or smoking) Not recommended for women who do not have other risk factors for VTE | Theoretical or proven risks usually outweigh advantages |
| 30–42 days | Not recommended for women who have other risk factors for VTE (e.g., age ≥35 years, previous VTE, thrombophilia, immobility, transfusion at delivery, BMI ≥30, postpartum hemorrhage, cesarean delivery, preeclampsia or smoking) Acceptable for women who do not have other risk factors for VTE | Theoretical or proven risks usually outweigh advantages in women who have risk factors for VTE Advantages generally outweigh the theoretical or proven risks in women who do not have other risk factors for VTE |
| >42 days | Acceptable | Advantages generally outweigh the theoretical or proven risks |
| VTE = venous thromboembolism, BMI = body mass index * Includes combined oral contraceptives, combined hormonal patch, and combined vaginal ring SOURCE: Adapted from CDC6 | ||
When to consider LARC or sterilization
Long-acting reversible contraceptives (LARC) are an important postpartum contraceptive option because they offer highly effective protection against pregnancy that can begin as soon as the placenta is delivered. LARC methods include contraceptive implants and intrauterine devices (IUDs).
According to the CDC’s medical eligibility criteria for contraceptive use, contraceptive implants can be placed immediately after delivery of the placenta without restriction.8
The copper IUD can be placed within 10 minutes after delivery of the placenta without restriction. If this window is missed, the benefits of inserting the IUD still outweigh the risks. Because 4 weeks postpartum is another time when the copper IUD can be inserted without restriction, the 3-week visit is a reasonable time to screen and schedule a patient for insertion.
The benefits of insertion of the levonorgestrel-releasing intrauterine system (LNG-IUS) are also believed to outweigh the risks before 4 weeks postpartum. Like the copper IUD, the LNG-IUS can be inserted without restriction at 4 weeks postpartum or later.
There is no need for a pelvic exam at the 3-week postpartum visit among women who undergo immediate postplacental insertion of the copper IUD or LNG-IUS. In fact, women can delay the exam until involution is complete.
Sterilization is best after complete involution
Interval tubal sterilization by laparoscopic, bilateral tubal fulguration or hysteroscopic microinsert placement is one of the most effective ways to prevent pregnancy. Both methods are best performed after the completion of involution and the return of normal coagulation; scheduling can take place at the 3-week postpartum visit.
Given the benefit of depot medroxyprogesterone acetate (DMPA) in endometrial suppression before hysteroscopic sterilization, it is reasonable to consider administering DMPA at the 3-week postpartum visit in anticipation of surgery after involution is complete.
The bottom line
Because most contraceptive methods can be safely initiated at or shortly after a 3-weeks’ postpartum visit, there is no longer any reason to time the routine postpartum visit to coincide with the completion of involution. For healthy women who have had an uneventful delivery, the routine postpartum visit should occur at 3 weeks.
We want to hear from you! Tell us what you think.
1. Speroff L, Mishell DR. The postpartum visit: it’s time for a change in order to optimally initiate contraception. Contraception. 2008;78(2):90-98.
2. Connolly A, Thorp J, Pahel L. Effects of pregnancy and childbirth on postpartum sexual function: a longitudinal prospective study. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(4):263-267.
3. McDowell MA, Wang C-Y, Kennedy-Stephenson J. Breastfeeding in the United States: Findings from the National Health and Nutrition Examination Surveys 1999–2006. NCHS Data Briefs. 2008;5:1-8.
4. Jackson E, Glasier A. Return of ovulation and menses in postpartum nonlactatinglactating women: a systematic review. Obstet Gynecol. 2011;117(3):657-662.
5. Kennedy K, Rivera R, McNeilly A. Consensus statement on the use of breastfeeding as a family planning method. Contraception. 1988;39(5):477-496.
6. Centers for Disease Control and Prevention. Update to CDC’s US Medical Eligibility Criteria for Contraceptive Use 2010: Revised recommendations for the use of contraceptive methods during the postpartum period. MMWR. 2011;60(26):878-883.
7. Jackson E, Curtis K, Gaffield M. Risk of venous thromboembolism during the postpartum period: a systematic review. Obstet Gynecol. 2011;117(3):691-703.
8. Centers for Disease Control and Prevention. US Medical Eligibility Criteria for Contraceptive Use 2010. MMWR. 2010;59(No. RR-4):1-86.
9. Kletzky OA, Marrs RP, Howard WF, McCormick W, Mishell DR Jr. Prolactin synthesis and release during pregnancy and puerperium. Am J Obstet Gynecol. 1980;136(4):545-550.
10. Labbok MH, Hight-Laukaran V, Peterson AE, Fletcher V, von Hertzen H, Van Look PF. Multicenter study of the Lactional Amenorrhea Method (LAM): I. Efficacy duration, and implications for clinical application. Contraception. 1997;55(6):327-336.
11. Valdes V, Labbok MH, Pugin E, Perez A. The efficacy of the Lactational Amenorrhea Method (LAM) among working women. Contraception. 2000;62(5):217-219.
1. Speroff L, Mishell DR. The postpartum visit: it’s time for a change in order to optimally initiate contraception. Contraception. 2008;78(2):90-98.
2. Connolly A, Thorp J, Pahel L. Effects of pregnancy and childbirth on postpartum sexual function: a longitudinal prospective study. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(4):263-267.
3. McDowell MA, Wang C-Y, Kennedy-Stephenson J. Breastfeeding in the United States: Findings from the National Health and Nutrition Examination Surveys 1999–2006. NCHS Data Briefs. 2008;5:1-8.
4. Jackson E, Glasier A. Return of ovulation and menses in postpartum nonlactatinglactating women: a systematic review. Obstet Gynecol. 2011;117(3):657-662.
5. Kennedy K, Rivera R, McNeilly A. Consensus statement on the use of breastfeeding as a family planning method. Contraception. 1988;39(5):477-496.
6. Centers for Disease Control and Prevention. Update to CDC’s US Medical Eligibility Criteria for Contraceptive Use 2010: Revised recommendations for the use of contraceptive methods during the postpartum period. MMWR. 2011;60(26):878-883.
7. Jackson E, Curtis K, Gaffield M. Risk of venous thromboembolism during the postpartum period: a systematic review. Obstet Gynecol. 2011;117(3):691-703.
8. Centers for Disease Control and Prevention. US Medical Eligibility Criteria for Contraceptive Use 2010. MMWR. 2010;59(No. RR-4):1-86.
9. Kletzky OA, Marrs RP, Howard WF, McCormick W, Mishell DR Jr. Prolactin synthesis and release during pregnancy and puerperium. Am J Obstet Gynecol. 1980;136(4):545-550.
10. Labbok MH, Hight-Laukaran V, Peterson AE, Fletcher V, von Hertzen H, Van Look PF. Multicenter study of the Lactional Amenorrhea Method (LAM): I. Efficacy duration, and implications for clinical application. Contraception. 1997;55(6):327-336.
11. Valdes V, Labbok MH, Pugin E, Perez A. The efficacy of the Lactational Amenorrhea Method (LAM) among working women. Contraception. 2000;62(5):217-219.