User login
Adherence to positive airway pressure (PAP) therapy is a difficult patient management issue. Clinicians at the John D. Dingell VA Medical Center in Detroit (VAMC Detroit) developed the O’Brien criteria and extensive patient education materials to increase patient adherence. The importance of PAP therapy and the reasons veterans should sleep with a PAP machine for 7 to 9 hours each night are stressed (many sleep only 4 to 5 hours). Several recent studies have confirmed widely varying PAP therapy adherence rates (30%-84%).1-13 A majority of patients indicated that mask discomfort is the primary reason for nonadherence.1
Adherence is affected by many factors, including heated humidity, patient education, mask type, and type of PAP machine (eg, continuous PAP [CPAP] vs bilevel PAP [BPAP]; auto-PAP vs CPAP). Other factors, such as race and economic status, also affect adherence.14 The Wisconsin Sleep Cohort Study found that patients with moderate-to-severe untreated obstructive sleep apnea (OSA) were 4 to 5 times more likely to die of a cardiovascular event and 3 times more likely to die of any cause.15 The morbidity and mortality associated with severe untreated OSA led the clinicians to intensify treatment efforts.16In this article, the authors summarize the initiative at the VAMC Detroit to enhance PAP therapy adherence in patients with sleep apnea. The goal was to motivate patients to maximize PAP machine use. This article is a guide that federal health care providers and their civilian counterparts in the private sector can use to maximize PAP machine use. Working toward that goal, a set of PAP “super user” criteria was developed and used to create a 5-point method for encouraging patients to maximize adherence to PAP therapy.
Background
Positive airway pressure is the room air pressure, measured in centimeters of H2O, which splints open the airway to prevent snoring, apneas, and hypopneas. An apnea is a 90%-plus airway obstruction that lasts longer than 10 seconds and is seen with sleep study polysomnography. A hypopnea is a 30%-plus airway obstruction that lasts longer than 10 seconds and is accompanied by a 3% drop in pulse oximetry (SpO2).
A CPAP device delivers pressure continuously through a medical air compressor or flow generator called a PAP machine. The BPAP machine has separate inspiratory pressure and expiratory pressure. Auto-PAP machines give minimum pressure and maximum pressure usually between the range of 4 cm H2O to 20 cm H2O. This machine finds the user’s median pressure (90th percentile) and maximum pressure and averages pressure over a specified period of use. The auto-PAP can then be set to CPAP mode and the pressure fixed or set to the 90th percentile.
O’Brien Criteria
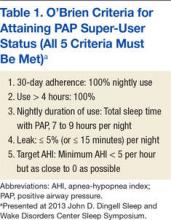
The O’Brien criteria for PAP super-user status (Table 1) were developed for maximizing PAP machine use and presented at the 2013 John D. Dingell Sleep and Wake Disorders Center Symposium. There is no other published reference or criteria proposed for maximizing PAP machine adherence. A recent study on sleep time criteria suggested that a higher percentage of patients achieved normal functioning with longer duration nightly CPAP therapy, which is in line with the authors’ recommended PAP machine use duration.17
Positive airway pressure therapy is eligible for insurance reimbursement by Medicare and third-party payers for adult patients who have OSA and achieve 4 hours of nightly use for 70% of nights over 30 days. Coverage for CPAP therapy is initially limited to 12 weeks during which beneficiaries with an OSA diagnosis can be identified and any therapy benefits documented. Subsequent CPAP therapy is covered only for those OSA patients who benefit during the 12-week period.18At VAMC Detroit, the data covering the previous 30 days of use is downloaded. Medicare allows for the best 30-day period out of the 12-week window. The hospital, along with Harper Hospital and the Detroit Medical Centers in conjunction with the Wayne State University sleep program, is an Academic Center of Distinction, which follows the sleep guidelines and practice parameters for Medicare, third-party insurance companies, and the American Academy of Sleep Medicine.
The sleep clinic clinicians follow the clinical guidelines for evaluation, management, and long-term care of adults with OSA.19,20 Follow-up visits are scheduled and made on a consultation basis up to 90 days for the required download or as necessary for PAP therapy. In this initiative, practitioners offer veteran-specific patient care with PAP therapy that exceeds Medicare guidelines. The success of this process yielded a growing cohort of PAP super users at VAMC Detroit. These patients exceed the Medicare criterion of 4 hours of nightly use for 70% of nights over 30 days. Thus, 4 hours of nightly use for 100% of nights over the same period was proposed as another criterion.
The super-user criteria, which provide motivation to reach the top, stimulate many patients to achieve the Medicare criteria. All 5 criteria must be satisfied to attain super-user status, and becoming a super user is not easy. In fact, the expectation is that, if an adherence data study is conducted, it will show that only a small percentage of all users meet the criteria. Maximum adherence is expected to be the tail (3%-4%) of a bell-shaped curve.
PAP Super-User Status
At the initial evaluation, practitioners create a self-fulfilling prophecy that, as first described by Merton, sets expectations.21 A self-fulfilling prophecy is a prediction that directly or indirectly causes the prediction to become true as a result of the positive feedback between belief and behavior.21 The personnel at VAMC Detroit sleep clinic set a tone that enables patients to meet and exceed the Medicare sleep guidelines and their expectations. Patients are encouraged to make it their personal mission to achieve the goal of becoming a PAP super user. The patients receive the O’Brien criteria for PAP super-user status—guidelines thought to contribute to higher quality of life.
The Medicare criterion emphasized is the minimum required for full adherence. The goal is to reduce sleepiness and increase well-being. The literature shows that increasing duration of sleep results in lower daytime sleepiness.22 Inadequate sleep has many detrimental effects. According to a recent study, insufficient sleep contributes to weight gain.22 Desired patient outcomes are increased sleep time without arousals, increased slow-wave sleep (SWS), consolidation of memories and rapid eye movement (REM), and improvement in emotional and procedural skill memories.23 Patients are informed that using a PAP machine for 7 to 9 hours can reduce excessive daytime sleepiness and allow for more SWS and REM sleep, which help improve memory, judgment, and concentration. Many other studies have shown how 7 to 9 hours of sleep benefit adults. Thus, 7 to 9 hours became the criterion for maximizing PAP sleep time.
Initial Evaluation and Sleep Study
A primary care provider can enroll a patient into the clinic for a sleep study by requesting an evaluation. The consultation is then triaged using the STOP-BANG (Snoring, Tiredness, Observed apnea, high blood Pressure–Body mass index > 35, Age > 50, Neck circumference > 40 cm, Gender male) questionnaire. The STOP-BANG has a high sensitivity for predicting moderate-to-severe (87.0%) and severe (70.4%) sleep-disordered breathing.24 More than 3 affirmative answers indicate a high risk for sleep-disordered breathing and is cause for ordering a sleep study.
CPAP Group Class
Patients with a diagnosis of sleep apnea subsequently receive their CPAP machines when they attend a 2-hour group class taught by a respiratory therapist. Group education sessions increase the chance of issuing more machines and providing better education.25 One study found that “attendance in a group clinic designed to encourage compliance with CPAP therapy provided a simple and effective means of improving treatment of OSA.”25
In class, the respiratory therapist briefly assesses each patient’s CPAP prescription, describes the patient’s type of sleep apnea and final diagnosis, and reviews the CPAP machine’s features. Veterans are then instructed to take their CPAP machines home to use all night, every night for 4 weeks. All night is defined as a period of 7.5 to 8 hours, as population-based study results have shown that sleep of this duration is associated with lowest cardiovascular morbidity and mortality. After the initial 4-plus weeks of machine use, patients with all their CPAP equipment are seen in the sleep clinic.
First Sleep Clinic Follow-Up Visit
At first follow-up, patients are asked for a subjective evaluation of their sleep. Most state they are “better” with PAP therapy. Each patient’s mask is checked and refitted with the patient’s prescribed pressure.
Patients are informed of their PAP settings and requirements from the sleep study and told their particular “magic pressure.” Patients understand that a person’s magic pressure, determined in the laboratory, is the pressure of room air blown into the nose, mouth, or both that eliminates not only snoring, but also partial and complete airway obstructions (hypopneas, apneas). Patients are asked to remember their particular magic pressure and their AHI and told their OSA status (mild, moderate, or severe) as assessed by the laboratory study.26 Extensive education on sleep apnea and treatment are also addressed. Education and training are among the most important tenets of PAP therapy, and these are incorporated into all encounters.25,26
PAP Data Report and Leak
The CPAP data are downloaded and printed. If adherence is suboptimal, clinician and patient discuss increasing adherence and possibly becoming a super user. The patient receives a copy of the report, which can be compared with the patient’s adherence statistics and with the adherence statistics of similar patients who are super users. A few blacked-out names are posted on the board in front of the provider’s computer station. Patients can thus easily see that attaining super-user status is very difficult but possible. Some patients maximize their therapy and are designated PAP super users. These patients are proud to receive this designation, and they strive to keep it.
Data downloads are crucial for adherence. In a recent study, the American Thoracic Society stated, “Providers need to be able to interpret adherence systems.”27
The clinic provides a summary report on each patient’s adherence. A provider interpretation is added, and the report is copied into the Computer Patient Record System.
After the report is downloaded, the provider checks for correct pressure and then for a large leak. A large leak is an unintentional leak (the total amount that leaks but not including leak from the mask) > 5% of the night. A leak of > 15 minutes was added to the super-user criteria, because some software provides the average time of a large leak per day in minutes.28 Many veterans sleep only 4 to 5 hours nightly (300 minutes × 5% = 15 minutes). Therefore, the leak should not be more than 5% or 15 minutes for a veteran sleeping 5 hours.
The machine indicates a percentage of leak on the patient self-check LED screen for adherence. There is no standardized leak criterion used by all flow-generator manufacturers. Every mask has venting designed to leak intentionally so that the patient does not rebreathe air CO2. The main concern is unintentional leaks above the intentional leak or venting threshold.
The ResMed CPAP (ResMed Corp, San Diego, CA) maximum intentional leak is 24 L/min.29 Above that level is large leak. The exact leak amount varies by interface (mask) based on pressure and mask type.2,12
The larger the interface surface area, the larger the leak. Unintentional leak is higher with the full-face mask than with the nasal mask, most likely because there is more opportunity for leakage with the larger surface area of the full-face mask. Nasal pillows seem to leak less because of their smaller surface area, but more studies on mask interfaces are needed to validate this finding.
Chin Strap
Adding a chin strap improved patient adherence, nightly duration of use, residual AHI, and leak in patients with sleep apnea.30 Other investigators reported reduced OSA, confirmed by polysomnography and nasopharyngolaryngoscopy, with use of only a chin strap.31 When a nasal mask with chin strap is used, the strap should be made to fit properly over the chin, not on the throat. Properly used chin straps significantly reduce leakage and residual AHI.30
A chin strap most likely reduces large leak and dry mouth.30 Dry mouth can result from mouth leak, which is commonly caused by nasal congestion or high pressure and mouth breathing. The nasal turbinates help humidify, warm, and cool the air. Heated humidification of PAP can help prevent dry mouth.
Asking the Right Questions
The clinician should ask several key questions at the first follow-up: How is it going with your PAP machine? Do you feel PAP therapy is helping you sleep? Do you feel better with PAP therapy? To a patient who states he or she is not doing well with therapy, the clinician should ask, What type of problems are you having? In many cases, poor adherence is attributable to a large leak from a poorly fitting mask. A large leak can also increase residual AHI and cause frequent arousals.30
Some machines cannot maintain the pressure of a large leak and will shut off and trigger an alarm that wakes the patient to readjust the mask. This situation causes some patients to discontinue CPAP/BPAP use. The mask leak must be adjusted. Another common complaint is morning dry mouth. This extreme dryness—a significant clue pointing to mouth leak caused in part by the mouth dropping open during sleep with PAP—should be addressed by fitting the patient with a chin strap.30 Dry mouth also can be caused by low humidity; increasing the humidity setting usually resolves the problem. However, as one study found, use of controlled heated humidification did not improve adherence or quality of life.32 In the same study, the nasopharyngeal dryness that resulted from CPAP therapy without humidification was reduced immediately and during the first weeks of treatment.All current PAP machines feature heated humidification.
Mouth breathing can also result from nasal congestion, allergic or vasomotor rhinitis, nasal turbinate hypertrophy, obstruction from a deviated septum, polyps, or air hunger/insufficient PAP pressure. Chronic rhinosinusitis is a problem that affects up to 12.5% of the U.S. population.33
Adherence is also increased with the elimination of leak and associated arousals. Patients are shown how to use their PAP machine’s heated humidity settings to obtain desired comfort levels. The clinician explains that the nasal turbinates heat and cool the air and that they can become swollen and irritated with PAP therapy. A heated hose may be prescribed to provide optimal humidification without condensation or water dripping into the hose (rainout).
A full-face mask is used only when the patient cannot breathe out the nose adequately or when PAP becomes too high. A 2013 study found no significant differences among ResMed, Respironics, and Fisher & Paykel CPAP interfaces (Fisher & Paykel Healthcare, Irvine, CA).34 The clinician determines which mask is comfortable for a patient and tries to stay with that mask for that patient.
Adherence Report
A therapy data summary is downloaded and reviewed with the patient.28 A pattern of use report that shows daily use with times over the month is also reviewed.28 The software’s sleep therapy long-term trend report lists important statistics. The adherence data summary and the CPAP summary are also reviewed (Table 2).28 This page is printed and given to patients to reieiw their progress. For some it represents a reward for using the CPAP/BPAP machine as well as a congratulatory note.
In the Example 1 summary download (Table 2), a patient used a PAP machine 4 hours or more on 93.3% of the 30 days the machine was used.28 Residual AHI was low, 2.1, and there was no appreciable leak. The PAP of 11.2 cm H2O was in the 90th percentile. The patient was fixed to 12 cm H2O with expiratory pressure relief (EPR) of 1. The EPR is a comfort feature that reduces pressure from 1 cm H2O to 3 cm H2O to make it easier for the patient to exhale. (A flow generator that produces EPR of > 3 cm H2O is a BPAP machine.)
This patient was not a super user. Overall use was low—5 hours, 28 minutes—which could indicate behaviorally insufficient sleep syndrome. Sleep time is controversial, but the National Sleep Foundation recommends 7 to 9 hours of sleep per night.
A different patient used a PAP machine 4 hours or more on 100% (28/28) of the days when the machine was used (Table 3).29 Residual AHI was low (0.6), median use was 8 hours, 47 minutes, and there was no appreciable leak. The patient was using autoset mode with a minimum pressure of 13 cm H2O and maximum pressure of 18 cm H2O. The 95th percentile pressure was 13.6 cm H2O. The patient’s pressure was changed to 14 cm H2O with EPR of 3. This patient was a super user.
Sleep Hygiene Discussion
Providers must discuss sleep hygiene (good sleep habits) with veterans. If needed, AASM pamphlets on sleep hygiene and other educational materials can be provided. The bedroom should be cool, comfortable, quiet, and dark and should not include a television or computer. Exposure to room light before bedtime suppresses melatonin onset and shortens melatonin duration and tells the brain it is time to wake up.34
Patients are asked about the number of arousals they have per night. At first follow-up, providers must determine what is causing a patient to arouse while on CPAP/BPAP therapy. Some causes are air leak resulting in unresolved OSA, nocturia (may be triggered by unresolved OSA), dry mouth (indicating need for chin strap), nightmares (suggestive of unresolved OSA in REM sleep), posttraumatic stress disorder (PTSD), environmental noise, and claustrophobia. The provider should have thought-out answers to these problems in advance.
Epworth Sleepiness Scale
The Epworth Sleepiness Scale (ESS) is administered as part of the baseline comprehensive examination and at every sleep clinic follow-up after issuing a CPAP/BPAP machine.35 The first evaluation after the machine is issued should show a reduction in ESS. No reduction in ESS indicates that a problem needs to be addressed. The most common reason for insufficient reduction in ESS is suboptimal PAP therapy adherence, usually because of a large leak. Some cases of poor adherence may be attributable to restless legs syndrome, periodic limb movement disorder, chronic musculoskeletal pain, and sleep fragmentation caused by alcohol, smoking, caffeine, or cocaine. Excessive daytime sleepiness may persist from use of pain medications or other sedating medications. One study found a correlation between sleep duration with CPAP therapy and reduction in ESS.36 In addition to administering the ESS, patients are asked how they doing with PAP therapy, and the answer is documented. Treatment changes are made if needed to reduce excessive daytime sleepiness.
Ear-Nose-Throat Examination
A quick look into the nose with a nasal speculum is a crucial component of a thorough examination. The clinician looks for a deviated septum, swollen turbinates, obstruction, polyps, bleeding, infection, septal perforation, and discharge. In addition, the patient is checked for airflow amount, nasal congestion, and obstruction; if necessary a nasal steroid spray or a nasal saline spray is prescribed. In some cases, saline spray can be added to the steroid spray to help reduce or eliminate nasal congestion.37
Treatment of congestion requires education, as many patients improperly use these sprays. The steroid spray is not an instant vasoconstrictor; a week of regular use is needed to reduce inflammation and congestion. Saline spray and saline irrigation can be used as a treatment adjunct for symptoms of chronic rhinosinusitis.37If the steroid and saline sprays fail after a 2-month trial, consider an ear-nose-throat (ENT) consultation. A recent study found that adherence rates increased after septoplasty in patients with nasal obstruction.38 The throat is examined for macroglossia or scalloping of the tongue.39 Macroglossic Mallampati IV tongues are platterlike. They are big, long, and wide and often have impressions or scalloping along the outside from a molding of the teeth. The patient is shown a Mallampati diagram and given a Mallampati score.
Creating a Sense of Mission
The sleep physician assistant (PA)at the Detroit VAMC is a retired U.S. Army colonel who ensures that the language the physician uses aligns with the language veterans use. Behavioral techniques are used to create a common culture that helps overcome obstacles—allowing patients to understand the benefits of and need for full CPAP/BPAP therapy adherence. One technique reinforces their sense of mission accomplishment, their military pride, and their interservice rivalry to increase adherence. The mission with each patient is to “work until success is achieved...but the patient can’t quit.” The mantra given to a patient with a difficult case is, “We will not let you fail with CPAP/BPAP therapy,” which echoes a familiar military motto, “We will not leave you behind.” Also, the goal of the physician is: Never give up on the patient.
Behavioral and Psychological Principles
The behavioral and psychological principles for success with PAP super users should be studied to validate better outcomes with longer duration PAP machine use. Patients who are motivated to succeed and to participate in their care can make great strides in changing their behavior to get more and better sleep. Obese patients can get referrals to the MOVE! weight loss program. Some veterans simply follow instructions, pay attention to detail, and do what they are told regarding sleep, PAP education, and good sleep hygiene. Many veterans have poor sleep hygiene and insomnia because they watch television or play games on electronic devices right before bedtime. Many patients develop behaviorally insufficient sleep syndrome. Their behavior prevents them from going to bed at a time that will allow sufficient sleep. Some veterans smoke or drink caffeinated beverages or al cohol immediately before sleep time and then wonder why they have insomnia.
Veterans with insomnia may be referred to the insomnia clinic psychologist for cognitive behavioral therapy for insomnia.40 Referral to this psychologist can be very helpful in the treatment of insomnia after the patient’s OSA has been treated. Veterans are encouraged to follow good sleep hygiene principles and permanently discontinue detrimental sleep behaviors.
For veterans with PTSD, imagery rehearsal before sleep has been effective in resolving disturbing nightmares and excluding their violent details.41 Clinicians recommend that these veterans rehearse a pleasant dream before sleep time. Cartwright and Lamberg performed extensive research on dreams and nightmares, and their book may provide insight into reducing nightmares for veterans with severe PTSD.42 Persistent nightmares associated with PTSD also can be reduced with use of prazosin. 43
Sleep Clinic Economics
The economic impact of OSA is substantial because of increased risk of cardiovascular disease and risk of motor vehicle accidents and decreased quality of life and productivity. Results of cost-effectiveness analyses support the value of diagnosing and treating OSA. Studies have provided estimates from a payer perspective, ranging from $2,000 to $11,000 per quality-adjusted life year over 5 years for treating moderate-to-severe OSA. The Sleep Heart Health Study showed that OSA was associated with an 18% increase in predicted health care utilization based on medication use.44,45 Moreover, CPAP therapy was found to be clinically more effective than no treatment: Therapy increased life expectancy in males and females, and effective treatment of OSA was associated with lower health care and disability costs and fewer missed workdays.
The authors’ initiatives to improve PAP therapy adherence required adding a PA and a registered respiratory therapist (RT) to the staff of 2 full-time equivalent (FTE) board-certified sleep physicians. The sleep physicians trained the PA to initiate and complete all the recommendations described, and the PA attended an AASM-sponsored review course for additional training. The PA is responsible for performing comprehensive face-to-face clinical evaluations in 4 half-day clinic sessions each week, as well as providing follow-up care in 4 additional half-day clinic sessions each week.
During these sessions, the PA provides education about sleep apnea and treatment. Thirty-minute follow-up clinic appointments are reserved for downloading CPAP data, providing interpretation, and educating patients to maximize PAP therapy and become super users. The remaining clinic sessions are run by 3 sleep fellows under the supervision of the sleep physicians. During all visits, providers encourage patients to maintain good sleep hygiene. Nonadherent patients are scheduled to be seen in a separate clinic session during which the RT troubleshoots and corrects PAP machine and mask-related problems.
Setting up the CPAP group classes and follow-up clinics required adding an FTE RT at a cost of $44,000 to $48,000 per year. By recruiting an FTE PA starting at GS-12 and $75,542 instead of another board-certified sleep physician, VAMC Detroit was able to provide increased access to patient care (8 clinics) at sizable financial savings (estimate, $75,000/y). A 0.5 FTE clinical psychologist provided cognitive behavioral therapy for insomnia and PAP therapy nonadherence and helped achieve the initiative’s goals.
The sleep center projects that the overall cost-effectiveness of these initiatives in terms of admission rates, life expectancy, and productivity would not be dissimilar to that reported in the peer-reviewed literature, as noted earlier. The center’s upcoming research projects will provide more data specific to its population. Educating patients requires that only motivated providers give patients instructions during a 30-minute follow-up clinic visit—there is no additional expense. This model of intensive care can be adopted at other VAMCs.
Conclusion
Maximizing PAP machine use is a unique approach that stimulates veterans to attain the highest level of adherence. This approach is based on clinical observation and patient encounters, and treatment recommendations over 8 years.
Showing enthusiasm with patients is crucial. Enthusiasm is contagious. Clinicians who are also PAP machine users should let patients know of their PAP super-user status and add that many others have attained this status, too. The benefits of optimal treatment are reviewed with patients: increased energy, lower risk of cardiovascular disease, lower blood pressure, better insulin sensitivity, and overall reduced mortality. Some patients have difficulty using the nasal mask and chin strap and understanding and adhering to PAP therapy. These impediments can be overcome with further education and follow-up. Sleep clinic clinicians take the time to show patients how to use the machine’s self-adherence check and leak functions. Patients can then monitor their progress daily.
To motivate patients, clinicians should set expectations early, invest time in providing education at follow-up; be diligent with respect to mask fitting and download evaluation. Sleep clinic providers should also speak the veterans’ language, create a self-fulfilling prophesy for success, and schedule a follow-up sleep clinic appointment if a patient is not fulfilling the Medicare adherence criterion of 4 hours’ nightly use for 70% of nights over 30 days.
PAP therapy coaching and persistent education with provider contact and enthusiasm can improve adherence. Encouragement and praise can help patients exceed Medicare’s minimum PAP therapy criterion and improve their overall PAP experience. The sleep team should tell patients they are proud of their accomplishments with such a difficult treatment. Being genuine and caring and showing concern about their evaluation, treatment, and follow-up is important. This helps reduce their OSA-related morbidity, lessen their depression, and improves their daily well-being and quality of life.
“The variation in responses to CPAP and acceptance of CPAP suggest that focused interventions, rather than one-size-fits-all interventions, may have a greater effect on the overall outcome of CPAP adherence,” wrote Weaver and Sawyer.46
Finally, one cannot equate spending on veteran care with spending in other areas of the national budget. The real cost of not giving veterans appropriate care will be a loss of trust, given that the overarching mission is “to care for him who shall have borne the battle and for his widow and his orphan.”
1. Boyaci H, Gacar K, Baris SA, Basyigit I, Yildiz F. Positive airway pressure device compliance of patients with obstructive sleep apnea syndrome. Adv Clin Exp Med. 2013;22(6):809-815.
2. Bachour A, Vitikainen P, Virkkula P, Maasilta P. CPAP interface: satisfaction and side effects. Sleep Breath. 2013;17(2):667-672.
3. Wimms AJ, Richards GN, Genjafield AV. Assessment of the impact on compliance of a new CPAP system in obstructive sleep apnea. Sleep Breath. 2013;17(1):69-76.
4. Smith I, Nadig V, Lasserson TJ. Educational, supportive and behavioral interventions to improve usage of continuous positive airway pressure machines for adults with obstructive sleep apnea. Cochrane Database Syst Rev. 2009;(2):CD007736.
5. Beecroft J, Zanon S, Lukic D, Hanly P. Oral continuous positive airway pressure for sleep apnea: effectiveness, patient preference, and adherence. Chest. 2003;124(6):2200-2208.
6. Chai CL, Pathinathan A, Smith B. Continuous positive airway pressure delivery interfaces for obstructive sleep apnoea. Cochrane Database Syst Rev. 2006;(4):CD005308.
7. Nilius G, Happel A, Domanski U, Ruhle KH. Pressure-relief continuous positive airway pressure vs constant continuous positive airway pressure: a comparison of efficacy and compliance. Chest. 2006;130(4):1018-1024.
8. Ballard RD, Gay PC, Strollo PJ. Interventions to improve compliance in sleep apnea patients previously non-compliant with continuous positive airway pressure. J Clin Sleep Med. 2007;3(7):706-712.
9. Sin DD, Mayers I, Man GC, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002;121(2):430-435.
10. Mortimore IL, Whittle AT, Douglas NJ. Comparison of nose and face mask CPAP therapy for sleep apnoea. Thorax. 1998;53(4):290-292.
11. Haniffa M, Lasserson TJ, Smith I. Interventions to improve compliance with continuous positive airway pressure for obstructive sleep apnoea. Cochrane Database Syst Rev. 2004;(4):CD003531.
12. Kushida CA, Berry RB, Blau, A, et al. Positive airway pressure initiation: a randomized controlled trial to assess the impact of therapy mode and titration process on efficacy, adherence, and outcomes. Sleep. 2011;34(8):1083-1092.
13. Gentina T, Fortin F, Douay B, et al. Auto bi-level with pressure relief during exhalation as a rescue therapy for optimally treated obstructive sleep apnoea patients with poor compliance to continuous positive airways pressure therapy--a pilot study. Sleep Breath. 2011;15(1):21-27.
14. Billings, ME, Auckley D, Benca R, et al. Race and residential socioeconomics as predictors of CPAP adherence. Sleep. 2011;34(12):1653-1658.
15. Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin Sleep Cohort. Sleep. 2008;31(8):1071-1078.
16. Centers for Disease Control and Prevention. Effect of short sleep duration on daily activities--United States, 2005-2008. MMWR Morb Mortal Wkly Rep. 2011;60(8):239-242.
17. Antic NA, Catcheside P, Buchan C, et al. The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep. 2011;34(1):111-119.
18. Phurrough S, Jacques L, Spencer F, Stiller J, Brechner R. Coverage decision memorandum for continuous positive airway pressure (CPAP) therapy for obstructive sleep apnea (OSA) (CAG-00093R2). Centers for Medicare & Medicaid Services Website. https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=204&fromdb=true. Accessed February 5, 2016.
19. Epstein LJ, Kristo D, Strollo PJ Jr, et al; Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2009;5(3):263-276.
20. Berry RB, Chediak A, Brown LK, et al; NPPV Titration Task Force of the American Academy of Sleep Medicine. Best clinical practices for the sleep center adjustment of noninvasive positive pressure ventilation (NPPV) in stable chronic alveolar hypoventilation syndromes. J Clin Sleep Med. 2010;6(5):491-509.
21. Merton RK. Social Theory and Social Structure. New York, NY: Free Press; 1968.
22. Chaput JP, McNeil J, Després JP, Bouchard C, Tremblay A. Seven to eight hours of sleep a night is associated with a lower prevalence of the metabolic syndrome and reduced overall cardiometabolic risk in adults. PLoS One. 2013;8(9):e72832.
23. Born J, Wagner U. Sleep, hormones, and memory. Obstet Gynecol Clin North Am. 2009;36(4):809-829, x.
24. Silva GE, Vana KD, Goodwin JL, Sherrill DL, Quan SF. Identification of patients with sleep disordered breathing: comparing the four-variable screening tool, STOP, STOP-Bang, and Epworth Sleepiness Scales. J Clin Sleep Med. 2011;7(5):467-472.
25. Soares Pires F, Drummond M, Marinho A, et al. Effectiveness of a group education session on adherence with APAP in obstructive sleep apnea--a randomized controlled study. Sleep Breath. 2013;17(3):993-1001.
26. Berry RB, Budhiraja R, Gottlieb DJ, et al; American Academy of Sleep Medicine. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8(5):597-619.
27. Schwab RJ, Badr SM, Epstein LJ, et al; ATS Subcommittee on CPAP Adherence Tracking Systems. An official American Thoracic Society statement: continuous positive airway pressure adherence tracking systems. The optimal monitoring strategies and outcome measures in adults. Am J Respir Crit Care Med. 2013;188(5):613-620.
28. Respironics Encore Pro and Encore Pro 2 [computer program]. Philips, Inc; May 12, 2013.
29. ResMed. Version 04.01.013. San Diego, CA.
30. Knowles SR, O'Brien DT, Zhang S, Devara A, Rowley JA. Effect of addition of chin strap on PAP compliance, nightly duration of use, and other factors. J Clin Sleep Med. 2014;10(4):377-383.
31. Vorona RD, Ware JC, Sinacori JT, Ford ML 3rd, Cross JP. Treatment of severe obstructive sleep apnea syndrome with a chinstrap. J Clin Sleep Med. 2007;3(7):729-730.
32. Ruhle KH, Franke KJ, Domanski U, Nilius G. Quality of life, compliance, sleep and nasopharyngeal side effects during CPAP therapy with and without controlled heated humidification. Sleep Breath. 2011;15(3):479-485.
33. Hamilos DL. Chronic rhinosinusitis: epidemiology and medical management. J Allergy Clin Immunol. 2011;128(4):693-707.
34. Gooley JJ, Chamberlain K, Smith KA, et al. Exposure to room light before bedtime suppresses melatonin onset and shortens melatonin duration in humans. J Clin Endocrinol Metab. 2011;96(3):E463-E472.
35. Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991;14(6):540-545.
36. Bednarek M, Zgierska A, Pływaczewski R, Zielinski J. The effect of CPAP treatment on excessive daytime somnolence in patients with obstructive sleep apnea [in Polish]. Pneumonol Alergol Pol. 1999;67(5-6):237-244.
37. Harvey R, Hannan SA, Badia L, Scadding G. Nasal saline irrigations for the symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev. 2007;(3):CD006394.
38. Poirier J, George C, Rotenberg B. The effect of nasal surgery on nasal continuous positive airway pressure compliance. Laryngoscope. 2014;124(1):317-319.
39. Law JA. From the journal archives: Mallampati in two millennia: its impact then and implications now. Can J Anaesth. 2014;61(5):480-484.
40. Hood HK, Rogojanski J, Moss TG. Cognitive-behavioral therapy for chronic insomnia. Curr Treat Options Neurol. 2014;16(12):321.
41. Harb GC, Thompson R, Ross RJ, Cook JM. Combat-related PTSD nightmares and imagery rehearsal: nightmare characteristics and relation to treatment outcome. J Trauma Stress. 2012;25(5):511-518.
42. Cartwright R, Lamberg L. Crisis Dreaming: Using Your Dreams to Solve Your Problems.. New York, NY: HarperCollins;1992.
43.Writer BW, Meyer EG, Schillerstrom JE. Prazosin for military combat-related PTSD nightmares: a critical review. J Neuropsychiatry Clin Neurosci. 2014;26(1):24-33.
44. Park JG, Ramar K, Olson EJ. Updates on definition, consequences, and management of obstructive sleep apnea. Mayo Clin Proc. 2011;86(6):549-554.
45. Kapur V, Blough DK, Sandblom RE, et al. The medical cost of undiagnosed sleep apnea. Sleep. 1999;22(6):749-755.
46. Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res. 2010;131:245-258.
Adherence to positive airway pressure (PAP) therapy is a difficult patient management issue. Clinicians at the John D. Dingell VA Medical Center in Detroit (VAMC Detroit) developed the O’Brien criteria and extensive patient education materials to increase patient adherence. The importance of PAP therapy and the reasons veterans should sleep with a PAP machine for 7 to 9 hours each night are stressed (many sleep only 4 to 5 hours). Several recent studies have confirmed widely varying PAP therapy adherence rates (30%-84%).1-13 A majority of patients indicated that mask discomfort is the primary reason for nonadherence.1
Adherence is affected by many factors, including heated humidity, patient education, mask type, and type of PAP machine (eg, continuous PAP [CPAP] vs bilevel PAP [BPAP]; auto-PAP vs CPAP). Other factors, such as race and economic status, also affect adherence.14 The Wisconsin Sleep Cohort Study found that patients with moderate-to-severe untreated obstructive sleep apnea (OSA) were 4 to 5 times more likely to die of a cardiovascular event and 3 times more likely to die of any cause.15 The morbidity and mortality associated with severe untreated OSA led the clinicians to intensify treatment efforts.16In this article, the authors summarize the initiative at the VAMC Detroit to enhance PAP therapy adherence in patients with sleep apnea. The goal was to motivate patients to maximize PAP machine use. This article is a guide that federal health care providers and their civilian counterparts in the private sector can use to maximize PAP machine use. Working toward that goal, a set of PAP “super user” criteria was developed and used to create a 5-point method for encouraging patients to maximize adherence to PAP therapy.
Background
Positive airway pressure is the room air pressure, measured in centimeters of H2O, which splints open the airway to prevent snoring, apneas, and hypopneas. An apnea is a 90%-plus airway obstruction that lasts longer than 10 seconds and is seen with sleep study polysomnography. A hypopnea is a 30%-plus airway obstruction that lasts longer than 10 seconds and is accompanied by a 3% drop in pulse oximetry (SpO2).
A CPAP device delivers pressure continuously through a medical air compressor or flow generator called a PAP machine. The BPAP machine has separate inspiratory pressure and expiratory pressure. Auto-PAP machines give minimum pressure and maximum pressure usually between the range of 4 cm H2O to 20 cm H2O. This machine finds the user’s median pressure (90th percentile) and maximum pressure and averages pressure over a specified period of use. The auto-PAP can then be set to CPAP mode and the pressure fixed or set to the 90th percentile.
O’Brien Criteria
The O’Brien criteria for PAP super-user status (Table 1) were developed for maximizing PAP machine use and presented at the 2013 John D. Dingell Sleep and Wake Disorders Center Symposium. There is no other published reference or criteria proposed for maximizing PAP machine adherence. A recent study on sleep time criteria suggested that a higher percentage of patients achieved normal functioning with longer duration nightly CPAP therapy, which is in line with the authors’ recommended PAP machine use duration.17
Positive airway pressure therapy is eligible for insurance reimbursement by Medicare and third-party payers for adult patients who have OSA and achieve 4 hours of nightly use for 70% of nights over 30 days. Coverage for CPAP therapy is initially limited to 12 weeks during which beneficiaries with an OSA diagnosis can be identified and any therapy benefits documented. Subsequent CPAP therapy is covered only for those OSA patients who benefit during the 12-week period.18At VAMC Detroit, the data covering the previous 30 days of use is downloaded. Medicare allows for the best 30-day period out of the 12-week window. The hospital, along with Harper Hospital and the Detroit Medical Centers in conjunction with the Wayne State University sleep program, is an Academic Center of Distinction, which follows the sleep guidelines and practice parameters for Medicare, third-party insurance companies, and the American Academy of Sleep Medicine.
The sleep clinic clinicians follow the clinical guidelines for evaluation, management, and long-term care of adults with OSA.19,20 Follow-up visits are scheduled and made on a consultation basis up to 90 days for the required download or as necessary for PAP therapy. In this initiative, practitioners offer veteran-specific patient care with PAP therapy that exceeds Medicare guidelines. The success of this process yielded a growing cohort of PAP super users at VAMC Detroit. These patients exceed the Medicare criterion of 4 hours of nightly use for 70% of nights over 30 days. Thus, 4 hours of nightly use for 100% of nights over the same period was proposed as another criterion.
The super-user criteria, which provide motivation to reach the top, stimulate many patients to achieve the Medicare criteria. All 5 criteria must be satisfied to attain super-user status, and becoming a super user is not easy. In fact, the expectation is that, if an adherence data study is conducted, it will show that only a small percentage of all users meet the criteria. Maximum adherence is expected to be the tail (3%-4%) of a bell-shaped curve.
PAP Super-User Status
At the initial evaluation, practitioners create a self-fulfilling prophecy that, as first described by Merton, sets expectations.21 A self-fulfilling prophecy is a prediction that directly or indirectly causes the prediction to become true as a result of the positive feedback between belief and behavior.21 The personnel at VAMC Detroit sleep clinic set a tone that enables patients to meet and exceed the Medicare sleep guidelines and their expectations. Patients are encouraged to make it their personal mission to achieve the goal of becoming a PAP super user. The patients receive the O’Brien criteria for PAP super-user status—guidelines thought to contribute to higher quality of life.
The Medicare criterion emphasized is the minimum required for full adherence. The goal is to reduce sleepiness and increase well-being. The literature shows that increasing duration of sleep results in lower daytime sleepiness.22 Inadequate sleep has many detrimental effects. According to a recent study, insufficient sleep contributes to weight gain.22 Desired patient outcomes are increased sleep time without arousals, increased slow-wave sleep (SWS), consolidation of memories and rapid eye movement (REM), and improvement in emotional and procedural skill memories.23 Patients are informed that using a PAP machine for 7 to 9 hours can reduce excessive daytime sleepiness and allow for more SWS and REM sleep, which help improve memory, judgment, and concentration. Many other studies have shown how 7 to 9 hours of sleep benefit adults. Thus, 7 to 9 hours became the criterion for maximizing PAP sleep time.
Initial Evaluation and Sleep Study
A primary care provider can enroll a patient into the clinic for a sleep study by requesting an evaluation. The consultation is then triaged using the STOP-BANG (Snoring, Tiredness, Observed apnea, high blood Pressure–Body mass index > 35, Age > 50, Neck circumference > 40 cm, Gender male) questionnaire. The STOP-BANG has a high sensitivity for predicting moderate-to-severe (87.0%) and severe (70.4%) sleep-disordered breathing.24 More than 3 affirmative answers indicate a high risk for sleep-disordered breathing and is cause for ordering a sleep study.
CPAP Group Class
Patients with a diagnosis of sleep apnea subsequently receive their CPAP machines when they attend a 2-hour group class taught by a respiratory therapist. Group education sessions increase the chance of issuing more machines and providing better education.25 One study found that “attendance in a group clinic designed to encourage compliance with CPAP therapy provided a simple and effective means of improving treatment of OSA.”25
In class, the respiratory therapist briefly assesses each patient’s CPAP prescription, describes the patient’s type of sleep apnea and final diagnosis, and reviews the CPAP machine’s features. Veterans are then instructed to take their CPAP machines home to use all night, every night for 4 weeks. All night is defined as a period of 7.5 to 8 hours, as population-based study results have shown that sleep of this duration is associated with lowest cardiovascular morbidity and mortality. After the initial 4-plus weeks of machine use, patients with all their CPAP equipment are seen in the sleep clinic.
First Sleep Clinic Follow-Up Visit
At first follow-up, patients are asked for a subjective evaluation of their sleep. Most state they are “better” with PAP therapy. Each patient’s mask is checked and refitted with the patient’s prescribed pressure.
Patients are informed of their PAP settings and requirements from the sleep study and told their particular “magic pressure.” Patients understand that a person’s magic pressure, determined in the laboratory, is the pressure of room air blown into the nose, mouth, or both that eliminates not only snoring, but also partial and complete airway obstructions (hypopneas, apneas). Patients are asked to remember their particular magic pressure and their AHI and told their OSA status (mild, moderate, or severe) as assessed by the laboratory study.26 Extensive education on sleep apnea and treatment are also addressed. Education and training are among the most important tenets of PAP therapy, and these are incorporated into all encounters.25,26
PAP Data Report and Leak
The CPAP data are downloaded and printed. If adherence is suboptimal, clinician and patient discuss increasing adherence and possibly becoming a super user. The patient receives a copy of the report, which can be compared with the patient’s adherence statistics and with the adherence statistics of similar patients who are super users. A few blacked-out names are posted on the board in front of the provider’s computer station. Patients can thus easily see that attaining super-user status is very difficult but possible. Some patients maximize their therapy and are designated PAP super users. These patients are proud to receive this designation, and they strive to keep it.
Data downloads are crucial for adherence. In a recent study, the American Thoracic Society stated, “Providers need to be able to interpret adherence systems.”27
The clinic provides a summary report on each patient’s adherence. A provider interpretation is added, and the report is copied into the Computer Patient Record System.
After the report is downloaded, the provider checks for correct pressure and then for a large leak. A large leak is an unintentional leak (the total amount that leaks but not including leak from the mask) > 5% of the night. A leak of > 15 minutes was added to the super-user criteria, because some software provides the average time of a large leak per day in minutes.28 Many veterans sleep only 4 to 5 hours nightly (300 minutes × 5% = 15 minutes). Therefore, the leak should not be more than 5% or 15 minutes for a veteran sleeping 5 hours.
The machine indicates a percentage of leak on the patient self-check LED screen for adherence. There is no standardized leak criterion used by all flow-generator manufacturers. Every mask has venting designed to leak intentionally so that the patient does not rebreathe air CO2. The main concern is unintentional leaks above the intentional leak or venting threshold.
The ResMed CPAP (ResMed Corp, San Diego, CA) maximum intentional leak is 24 L/min.29 Above that level is large leak. The exact leak amount varies by interface (mask) based on pressure and mask type.2,12
The larger the interface surface area, the larger the leak. Unintentional leak is higher with the full-face mask than with the nasal mask, most likely because there is more opportunity for leakage with the larger surface area of the full-face mask. Nasal pillows seem to leak less because of their smaller surface area, but more studies on mask interfaces are needed to validate this finding.
Chin Strap
Adding a chin strap improved patient adherence, nightly duration of use, residual AHI, and leak in patients with sleep apnea.30 Other investigators reported reduced OSA, confirmed by polysomnography and nasopharyngolaryngoscopy, with use of only a chin strap.31 When a nasal mask with chin strap is used, the strap should be made to fit properly over the chin, not on the throat. Properly used chin straps significantly reduce leakage and residual AHI.30
A chin strap most likely reduces large leak and dry mouth.30 Dry mouth can result from mouth leak, which is commonly caused by nasal congestion or high pressure and mouth breathing. The nasal turbinates help humidify, warm, and cool the air. Heated humidification of PAP can help prevent dry mouth.
Asking the Right Questions
The clinician should ask several key questions at the first follow-up: How is it going with your PAP machine? Do you feel PAP therapy is helping you sleep? Do you feel better with PAP therapy? To a patient who states he or she is not doing well with therapy, the clinician should ask, What type of problems are you having? In many cases, poor adherence is attributable to a large leak from a poorly fitting mask. A large leak can also increase residual AHI and cause frequent arousals.30
Some machines cannot maintain the pressure of a large leak and will shut off and trigger an alarm that wakes the patient to readjust the mask. This situation causes some patients to discontinue CPAP/BPAP use. The mask leak must be adjusted. Another common complaint is morning dry mouth. This extreme dryness—a significant clue pointing to mouth leak caused in part by the mouth dropping open during sleep with PAP—should be addressed by fitting the patient with a chin strap.30 Dry mouth also can be caused by low humidity; increasing the humidity setting usually resolves the problem. However, as one study found, use of controlled heated humidification did not improve adherence or quality of life.32 In the same study, the nasopharyngeal dryness that resulted from CPAP therapy without humidification was reduced immediately and during the first weeks of treatment.All current PAP machines feature heated humidification.
Mouth breathing can also result from nasal congestion, allergic or vasomotor rhinitis, nasal turbinate hypertrophy, obstruction from a deviated septum, polyps, or air hunger/insufficient PAP pressure. Chronic rhinosinusitis is a problem that affects up to 12.5% of the U.S. population.33
Adherence is also increased with the elimination of leak and associated arousals. Patients are shown how to use their PAP machine’s heated humidity settings to obtain desired comfort levels. The clinician explains that the nasal turbinates heat and cool the air and that they can become swollen and irritated with PAP therapy. A heated hose may be prescribed to provide optimal humidification without condensation or water dripping into the hose (rainout).
A full-face mask is used only when the patient cannot breathe out the nose adequately or when PAP becomes too high. A 2013 study found no significant differences among ResMed, Respironics, and Fisher & Paykel CPAP interfaces (Fisher & Paykel Healthcare, Irvine, CA).34 The clinician determines which mask is comfortable for a patient and tries to stay with that mask for that patient.
Adherence Report
A therapy data summary is downloaded and reviewed with the patient.28 A pattern of use report that shows daily use with times over the month is also reviewed.28 The software’s sleep therapy long-term trend report lists important statistics. The adherence data summary and the CPAP summary are also reviewed (Table 2).28 This page is printed and given to patients to reieiw their progress. For some it represents a reward for using the CPAP/BPAP machine as well as a congratulatory note.
In the Example 1 summary download (Table 2), a patient used a PAP machine 4 hours or more on 93.3% of the 30 days the machine was used.28 Residual AHI was low, 2.1, and there was no appreciable leak. The PAP of 11.2 cm H2O was in the 90th percentile. The patient was fixed to 12 cm H2O with expiratory pressure relief (EPR) of 1. The EPR is a comfort feature that reduces pressure from 1 cm H2O to 3 cm H2O to make it easier for the patient to exhale. (A flow generator that produces EPR of > 3 cm H2O is a BPAP machine.)
This patient was not a super user. Overall use was low—5 hours, 28 minutes—which could indicate behaviorally insufficient sleep syndrome. Sleep time is controversial, but the National Sleep Foundation recommends 7 to 9 hours of sleep per night.
A different patient used a PAP machine 4 hours or more on 100% (28/28) of the days when the machine was used (Table 3).29 Residual AHI was low (0.6), median use was 8 hours, 47 minutes, and there was no appreciable leak. The patient was using autoset mode with a minimum pressure of 13 cm H2O and maximum pressure of 18 cm H2O. The 95th percentile pressure was 13.6 cm H2O. The patient’s pressure was changed to 14 cm H2O with EPR of 3. This patient was a super user.
Sleep Hygiene Discussion
Providers must discuss sleep hygiene (good sleep habits) with veterans. If needed, AASM pamphlets on sleep hygiene and other educational materials can be provided. The bedroom should be cool, comfortable, quiet, and dark and should not include a television or computer. Exposure to room light before bedtime suppresses melatonin onset and shortens melatonin duration and tells the brain it is time to wake up.34
Patients are asked about the number of arousals they have per night. At first follow-up, providers must determine what is causing a patient to arouse while on CPAP/BPAP therapy. Some causes are air leak resulting in unresolved OSA, nocturia (may be triggered by unresolved OSA), dry mouth (indicating need for chin strap), nightmares (suggestive of unresolved OSA in REM sleep), posttraumatic stress disorder (PTSD), environmental noise, and claustrophobia. The provider should have thought-out answers to these problems in advance.
Epworth Sleepiness Scale
The Epworth Sleepiness Scale (ESS) is administered as part of the baseline comprehensive examination and at every sleep clinic follow-up after issuing a CPAP/BPAP machine.35 The first evaluation after the machine is issued should show a reduction in ESS. No reduction in ESS indicates that a problem needs to be addressed. The most common reason for insufficient reduction in ESS is suboptimal PAP therapy adherence, usually because of a large leak. Some cases of poor adherence may be attributable to restless legs syndrome, periodic limb movement disorder, chronic musculoskeletal pain, and sleep fragmentation caused by alcohol, smoking, caffeine, or cocaine. Excessive daytime sleepiness may persist from use of pain medications or other sedating medications. One study found a correlation between sleep duration with CPAP therapy and reduction in ESS.36 In addition to administering the ESS, patients are asked how they doing with PAP therapy, and the answer is documented. Treatment changes are made if needed to reduce excessive daytime sleepiness.
Ear-Nose-Throat Examination
A quick look into the nose with a nasal speculum is a crucial component of a thorough examination. The clinician looks for a deviated septum, swollen turbinates, obstruction, polyps, bleeding, infection, septal perforation, and discharge. In addition, the patient is checked for airflow amount, nasal congestion, and obstruction; if necessary a nasal steroid spray or a nasal saline spray is prescribed. In some cases, saline spray can be added to the steroid spray to help reduce or eliminate nasal congestion.37
Treatment of congestion requires education, as many patients improperly use these sprays. The steroid spray is not an instant vasoconstrictor; a week of regular use is needed to reduce inflammation and congestion. Saline spray and saline irrigation can be used as a treatment adjunct for symptoms of chronic rhinosinusitis.37If the steroid and saline sprays fail after a 2-month trial, consider an ear-nose-throat (ENT) consultation. A recent study found that adherence rates increased after septoplasty in patients with nasal obstruction.38 The throat is examined for macroglossia or scalloping of the tongue.39 Macroglossic Mallampati IV tongues are platterlike. They are big, long, and wide and often have impressions or scalloping along the outside from a molding of the teeth. The patient is shown a Mallampati diagram and given a Mallampati score.
Creating a Sense of Mission
The sleep physician assistant (PA)at the Detroit VAMC is a retired U.S. Army colonel who ensures that the language the physician uses aligns with the language veterans use. Behavioral techniques are used to create a common culture that helps overcome obstacles—allowing patients to understand the benefits of and need for full CPAP/BPAP therapy adherence. One technique reinforces their sense of mission accomplishment, their military pride, and their interservice rivalry to increase adherence. The mission with each patient is to “work until success is achieved...but the patient can’t quit.” The mantra given to a patient with a difficult case is, “We will not let you fail with CPAP/BPAP therapy,” which echoes a familiar military motto, “We will not leave you behind.” Also, the goal of the physician is: Never give up on the patient.
Behavioral and Psychological Principles
The behavioral and psychological principles for success with PAP super users should be studied to validate better outcomes with longer duration PAP machine use. Patients who are motivated to succeed and to participate in their care can make great strides in changing their behavior to get more and better sleep. Obese patients can get referrals to the MOVE! weight loss program. Some veterans simply follow instructions, pay attention to detail, and do what they are told regarding sleep, PAP education, and good sleep hygiene. Many veterans have poor sleep hygiene and insomnia because they watch television or play games on electronic devices right before bedtime. Many patients develop behaviorally insufficient sleep syndrome. Their behavior prevents them from going to bed at a time that will allow sufficient sleep. Some veterans smoke or drink caffeinated beverages or al cohol immediately before sleep time and then wonder why they have insomnia.
Veterans with insomnia may be referred to the insomnia clinic psychologist for cognitive behavioral therapy for insomnia.40 Referral to this psychologist can be very helpful in the treatment of insomnia after the patient’s OSA has been treated. Veterans are encouraged to follow good sleep hygiene principles and permanently discontinue detrimental sleep behaviors.
For veterans with PTSD, imagery rehearsal before sleep has been effective in resolving disturbing nightmares and excluding their violent details.41 Clinicians recommend that these veterans rehearse a pleasant dream before sleep time. Cartwright and Lamberg performed extensive research on dreams and nightmares, and their book may provide insight into reducing nightmares for veterans with severe PTSD.42 Persistent nightmares associated with PTSD also can be reduced with use of prazosin. 43
Sleep Clinic Economics
The economic impact of OSA is substantial because of increased risk of cardiovascular disease and risk of motor vehicle accidents and decreased quality of life and productivity. Results of cost-effectiveness analyses support the value of diagnosing and treating OSA. Studies have provided estimates from a payer perspective, ranging from $2,000 to $11,000 per quality-adjusted life year over 5 years for treating moderate-to-severe OSA. The Sleep Heart Health Study showed that OSA was associated with an 18% increase in predicted health care utilization based on medication use.44,45 Moreover, CPAP therapy was found to be clinically more effective than no treatment: Therapy increased life expectancy in males and females, and effective treatment of OSA was associated with lower health care and disability costs and fewer missed workdays.
The authors’ initiatives to improve PAP therapy adherence required adding a PA and a registered respiratory therapist (RT) to the staff of 2 full-time equivalent (FTE) board-certified sleep physicians. The sleep physicians trained the PA to initiate and complete all the recommendations described, and the PA attended an AASM-sponsored review course for additional training. The PA is responsible for performing comprehensive face-to-face clinical evaluations in 4 half-day clinic sessions each week, as well as providing follow-up care in 4 additional half-day clinic sessions each week.
During these sessions, the PA provides education about sleep apnea and treatment. Thirty-minute follow-up clinic appointments are reserved for downloading CPAP data, providing interpretation, and educating patients to maximize PAP therapy and become super users. The remaining clinic sessions are run by 3 sleep fellows under the supervision of the sleep physicians. During all visits, providers encourage patients to maintain good sleep hygiene. Nonadherent patients are scheduled to be seen in a separate clinic session during which the RT troubleshoots and corrects PAP machine and mask-related problems.
Setting up the CPAP group classes and follow-up clinics required adding an FTE RT at a cost of $44,000 to $48,000 per year. By recruiting an FTE PA starting at GS-12 and $75,542 instead of another board-certified sleep physician, VAMC Detroit was able to provide increased access to patient care (8 clinics) at sizable financial savings (estimate, $75,000/y). A 0.5 FTE clinical psychologist provided cognitive behavioral therapy for insomnia and PAP therapy nonadherence and helped achieve the initiative’s goals.
The sleep center projects that the overall cost-effectiveness of these initiatives in terms of admission rates, life expectancy, and productivity would not be dissimilar to that reported in the peer-reviewed literature, as noted earlier. The center’s upcoming research projects will provide more data specific to its population. Educating patients requires that only motivated providers give patients instructions during a 30-minute follow-up clinic visit—there is no additional expense. This model of intensive care can be adopted at other VAMCs.
Conclusion
Maximizing PAP machine use is a unique approach that stimulates veterans to attain the highest level of adherence. This approach is based on clinical observation and patient encounters, and treatment recommendations over 8 years.
Showing enthusiasm with patients is crucial. Enthusiasm is contagious. Clinicians who are also PAP machine users should let patients know of their PAP super-user status and add that many others have attained this status, too. The benefits of optimal treatment are reviewed with patients: increased energy, lower risk of cardiovascular disease, lower blood pressure, better insulin sensitivity, and overall reduced mortality. Some patients have difficulty using the nasal mask and chin strap and understanding and adhering to PAP therapy. These impediments can be overcome with further education and follow-up. Sleep clinic clinicians take the time to show patients how to use the machine’s self-adherence check and leak functions. Patients can then monitor their progress daily.
To motivate patients, clinicians should set expectations early, invest time in providing education at follow-up; be diligent with respect to mask fitting and download evaluation. Sleep clinic providers should also speak the veterans’ language, create a self-fulfilling prophesy for success, and schedule a follow-up sleep clinic appointment if a patient is not fulfilling the Medicare adherence criterion of 4 hours’ nightly use for 70% of nights over 30 days.
PAP therapy coaching and persistent education with provider contact and enthusiasm can improve adherence. Encouragement and praise can help patients exceed Medicare’s minimum PAP therapy criterion and improve their overall PAP experience. The sleep team should tell patients they are proud of their accomplishments with such a difficult treatment. Being genuine and caring and showing concern about their evaluation, treatment, and follow-up is important. This helps reduce their OSA-related morbidity, lessen their depression, and improves their daily well-being and quality of life.
“The variation in responses to CPAP and acceptance of CPAP suggest that focused interventions, rather than one-size-fits-all interventions, may have a greater effect on the overall outcome of CPAP adherence,” wrote Weaver and Sawyer.46
Finally, one cannot equate spending on veteran care with spending in other areas of the national budget. The real cost of not giving veterans appropriate care will be a loss of trust, given that the overarching mission is “to care for him who shall have borne the battle and for his widow and his orphan.”
Adherence to positive airway pressure (PAP) therapy is a difficult patient management issue. Clinicians at the John D. Dingell VA Medical Center in Detroit (VAMC Detroit) developed the O’Brien criteria and extensive patient education materials to increase patient adherence. The importance of PAP therapy and the reasons veterans should sleep with a PAP machine for 7 to 9 hours each night are stressed (many sleep only 4 to 5 hours). Several recent studies have confirmed widely varying PAP therapy adherence rates (30%-84%).1-13 A majority of patients indicated that mask discomfort is the primary reason for nonadherence.1
Adherence is affected by many factors, including heated humidity, patient education, mask type, and type of PAP machine (eg, continuous PAP [CPAP] vs bilevel PAP [BPAP]; auto-PAP vs CPAP). Other factors, such as race and economic status, also affect adherence.14 The Wisconsin Sleep Cohort Study found that patients with moderate-to-severe untreated obstructive sleep apnea (OSA) were 4 to 5 times more likely to die of a cardiovascular event and 3 times more likely to die of any cause.15 The morbidity and mortality associated with severe untreated OSA led the clinicians to intensify treatment efforts.16In this article, the authors summarize the initiative at the VAMC Detroit to enhance PAP therapy adherence in patients with sleep apnea. The goal was to motivate patients to maximize PAP machine use. This article is a guide that federal health care providers and their civilian counterparts in the private sector can use to maximize PAP machine use. Working toward that goal, a set of PAP “super user” criteria was developed and used to create a 5-point method for encouraging patients to maximize adherence to PAP therapy.
Background
Positive airway pressure is the room air pressure, measured in centimeters of H2O, which splints open the airway to prevent snoring, apneas, and hypopneas. An apnea is a 90%-plus airway obstruction that lasts longer than 10 seconds and is seen with sleep study polysomnography. A hypopnea is a 30%-plus airway obstruction that lasts longer than 10 seconds and is accompanied by a 3% drop in pulse oximetry (SpO2).
A CPAP device delivers pressure continuously through a medical air compressor or flow generator called a PAP machine. The BPAP machine has separate inspiratory pressure and expiratory pressure. Auto-PAP machines give minimum pressure and maximum pressure usually between the range of 4 cm H2O to 20 cm H2O. This machine finds the user’s median pressure (90th percentile) and maximum pressure and averages pressure over a specified period of use. The auto-PAP can then be set to CPAP mode and the pressure fixed or set to the 90th percentile.
O’Brien Criteria
The O’Brien criteria for PAP super-user status (Table 1) were developed for maximizing PAP machine use and presented at the 2013 John D. Dingell Sleep and Wake Disorders Center Symposium. There is no other published reference or criteria proposed for maximizing PAP machine adherence. A recent study on sleep time criteria suggested that a higher percentage of patients achieved normal functioning with longer duration nightly CPAP therapy, which is in line with the authors’ recommended PAP machine use duration.17
Positive airway pressure therapy is eligible for insurance reimbursement by Medicare and third-party payers for adult patients who have OSA and achieve 4 hours of nightly use for 70% of nights over 30 days. Coverage for CPAP therapy is initially limited to 12 weeks during which beneficiaries with an OSA diagnosis can be identified and any therapy benefits documented. Subsequent CPAP therapy is covered only for those OSA patients who benefit during the 12-week period.18At VAMC Detroit, the data covering the previous 30 days of use is downloaded. Medicare allows for the best 30-day period out of the 12-week window. The hospital, along with Harper Hospital and the Detroit Medical Centers in conjunction with the Wayne State University sleep program, is an Academic Center of Distinction, which follows the sleep guidelines and practice parameters for Medicare, third-party insurance companies, and the American Academy of Sleep Medicine.
The sleep clinic clinicians follow the clinical guidelines for evaluation, management, and long-term care of adults with OSA.19,20 Follow-up visits are scheduled and made on a consultation basis up to 90 days for the required download or as necessary for PAP therapy. In this initiative, practitioners offer veteran-specific patient care with PAP therapy that exceeds Medicare guidelines. The success of this process yielded a growing cohort of PAP super users at VAMC Detroit. These patients exceed the Medicare criterion of 4 hours of nightly use for 70% of nights over 30 days. Thus, 4 hours of nightly use for 100% of nights over the same period was proposed as another criterion.
The super-user criteria, which provide motivation to reach the top, stimulate many patients to achieve the Medicare criteria. All 5 criteria must be satisfied to attain super-user status, and becoming a super user is not easy. In fact, the expectation is that, if an adherence data study is conducted, it will show that only a small percentage of all users meet the criteria. Maximum adherence is expected to be the tail (3%-4%) of a bell-shaped curve.
PAP Super-User Status
At the initial evaluation, practitioners create a self-fulfilling prophecy that, as first described by Merton, sets expectations.21 A self-fulfilling prophecy is a prediction that directly or indirectly causes the prediction to become true as a result of the positive feedback between belief and behavior.21 The personnel at VAMC Detroit sleep clinic set a tone that enables patients to meet and exceed the Medicare sleep guidelines and their expectations. Patients are encouraged to make it their personal mission to achieve the goal of becoming a PAP super user. The patients receive the O’Brien criteria for PAP super-user status—guidelines thought to contribute to higher quality of life.
The Medicare criterion emphasized is the minimum required for full adherence. The goal is to reduce sleepiness and increase well-being. The literature shows that increasing duration of sleep results in lower daytime sleepiness.22 Inadequate sleep has many detrimental effects. According to a recent study, insufficient sleep contributes to weight gain.22 Desired patient outcomes are increased sleep time without arousals, increased slow-wave sleep (SWS), consolidation of memories and rapid eye movement (REM), and improvement in emotional and procedural skill memories.23 Patients are informed that using a PAP machine for 7 to 9 hours can reduce excessive daytime sleepiness and allow for more SWS and REM sleep, which help improve memory, judgment, and concentration. Many other studies have shown how 7 to 9 hours of sleep benefit adults. Thus, 7 to 9 hours became the criterion for maximizing PAP sleep time.
Initial Evaluation and Sleep Study
A primary care provider can enroll a patient into the clinic for a sleep study by requesting an evaluation. The consultation is then triaged using the STOP-BANG (Snoring, Tiredness, Observed apnea, high blood Pressure–Body mass index > 35, Age > 50, Neck circumference > 40 cm, Gender male) questionnaire. The STOP-BANG has a high sensitivity for predicting moderate-to-severe (87.0%) and severe (70.4%) sleep-disordered breathing.24 More than 3 affirmative answers indicate a high risk for sleep-disordered breathing and is cause for ordering a sleep study.
CPAP Group Class
Patients with a diagnosis of sleep apnea subsequently receive their CPAP machines when they attend a 2-hour group class taught by a respiratory therapist. Group education sessions increase the chance of issuing more machines and providing better education.25 One study found that “attendance in a group clinic designed to encourage compliance with CPAP therapy provided a simple and effective means of improving treatment of OSA.”25
In class, the respiratory therapist briefly assesses each patient’s CPAP prescription, describes the patient’s type of sleep apnea and final diagnosis, and reviews the CPAP machine’s features. Veterans are then instructed to take their CPAP machines home to use all night, every night for 4 weeks. All night is defined as a period of 7.5 to 8 hours, as population-based study results have shown that sleep of this duration is associated with lowest cardiovascular morbidity and mortality. After the initial 4-plus weeks of machine use, patients with all their CPAP equipment are seen in the sleep clinic.
First Sleep Clinic Follow-Up Visit
At first follow-up, patients are asked for a subjective evaluation of their sleep. Most state they are “better” with PAP therapy. Each patient’s mask is checked and refitted with the patient’s prescribed pressure.
Patients are informed of their PAP settings and requirements from the sleep study and told their particular “magic pressure.” Patients understand that a person’s magic pressure, determined in the laboratory, is the pressure of room air blown into the nose, mouth, or both that eliminates not only snoring, but also partial and complete airway obstructions (hypopneas, apneas). Patients are asked to remember their particular magic pressure and their AHI and told their OSA status (mild, moderate, or severe) as assessed by the laboratory study.26 Extensive education on sleep apnea and treatment are also addressed. Education and training are among the most important tenets of PAP therapy, and these are incorporated into all encounters.25,26
PAP Data Report and Leak
The CPAP data are downloaded and printed. If adherence is suboptimal, clinician and patient discuss increasing adherence and possibly becoming a super user. The patient receives a copy of the report, which can be compared with the patient’s adherence statistics and with the adherence statistics of similar patients who are super users. A few blacked-out names are posted on the board in front of the provider’s computer station. Patients can thus easily see that attaining super-user status is very difficult but possible. Some patients maximize their therapy and are designated PAP super users. These patients are proud to receive this designation, and they strive to keep it.
Data downloads are crucial for adherence. In a recent study, the American Thoracic Society stated, “Providers need to be able to interpret adherence systems.”27
The clinic provides a summary report on each patient’s adherence. A provider interpretation is added, and the report is copied into the Computer Patient Record System.
After the report is downloaded, the provider checks for correct pressure and then for a large leak. A large leak is an unintentional leak (the total amount that leaks but not including leak from the mask) > 5% of the night. A leak of > 15 minutes was added to the super-user criteria, because some software provides the average time of a large leak per day in minutes.28 Many veterans sleep only 4 to 5 hours nightly (300 minutes × 5% = 15 minutes). Therefore, the leak should not be more than 5% or 15 minutes for a veteran sleeping 5 hours.
The machine indicates a percentage of leak on the patient self-check LED screen for adherence. There is no standardized leak criterion used by all flow-generator manufacturers. Every mask has venting designed to leak intentionally so that the patient does not rebreathe air CO2. The main concern is unintentional leaks above the intentional leak or venting threshold.
The ResMed CPAP (ResMed Corp, San Diego, CA) maximum intentional leak is 24 L/min.29 Above that level is large leak. The exact leak amount varies by interface (mask) based on pressure and mask type.2,12
The larger the interface surface area, the larger the leak. Unintentional leak is higher with the full-face mask than with the nasal mask, most likely because there is more opportunity for leakage with the larger surface area of the full-face mask. Nasal pillows seem to leak less because of their smaller surface area, but more studies on mask interfaces are needed to validate this finding.
Chin Strap
Adding a chin strap improved patient adherence, nightly duration of use, residual AHI, and leak in patients with sleep apnea.30 Other investigators reported reduced OSA, confirmed by polysomnography and nasopharyngolaryngoscopy, with use of only a chin strap.31 When a nasal mask with chin strap is used, the strap should be made to fit properly over the chin, not on the throat. Properly used chin straps significantly reduce leakage and residual AHI.30
A chin strap most likely reduces large leak and dry mouth.30 Dry mouth can result from mouth leak, which is commonly caused by nasal congestion or high pressure and mouth breathing. The nasal turbinates help humidify, warm, and cool the air. Heated humidification of PAP can help prevent dry mouth.
Asking the Right Questions
The clinician should ask several key questions at the first follow-up: How is it going with your PAP machine? Do you feel PAP therapy is helping you sleep? Do you feel better with PAP therapy? To a patient who states he or she is not doing well with therapy, the clinician should ask, What type of problems are you having? In many cases, poor adherence is attributable to a large leak from a poorly fitting mask. A large leak can also increase residual AHI and cause frequent arousals.30
Some machines cannot maintain the pressure of a large leak and will shut off and trigger an alarm that wakes the patient to readjust the mask. This situation causes some patients to discontinue CPAP/BPAP use. The mask leak must be adjusted. Another common complaint is morning dry mouth. This extreme dryness—a significant clue pointing to mouth leak caused in part by the mouth dropping open during sleep with PAP—should be addressed by fitting the patient with a chin strap.30 Dry mouth also can be caused by low humidity; increasing the humidity setting usually resolves the problem. However, as one study found, use of controlled heated humidification did not improve adherence or quality of life.32 In the same study, the nasopharyngeal dryness that resulted from CPAP therapy without humidification was reduced immediately and during the first weeks of treatment.All current PAP machines feature heated humidification.
Mouth breathing can also result from nasal congestion, allergic or vasomotor rhinitis, nasal turbinate hypertrophy, obstruction from a deviated septum, polyps, or air hunger/insufficient PAP pressure. Chronic rhinosinusitis is a problem that affects up to 12.5% of the U.S. population.33
Adherence is also increased with the elimination of leak and associated arousals. Patients are shown how to use their PAP machine’s heated humidity settings to obtain desired comfort levels. The clinician explains that the nasal turbinates heat and cool the air and that they can become swollen and irritated with PAP therapy. A heated hose may be prescribed to provide optimal humidification without condensation or water dripping into the hose (rainout).
A full-face mask is used only when the patient cannot breathe out the nose adequately or when PAP becomes too high. A 2013 study found no significant differences among ResMed, Respironics, and Fisher & Paykel CPAP interfaces (Fisher & Paykel Healthcare, Irvine, CA).34 The clinician determines which mask is comfortable for a patient and tries to stay with that mask for that patient.
Adherence Report
A therapy data summary is downloaded and reviewed with the patient.28 A pattern of use report that shows daily use with times over the month is also reviewed.28 The software’s sleep therapy long-term trend report lists important statistics. The adherence data summary and the CPAP summary are also reviewed (Table 2).28 This page is printed and given to patients to reieiw their progress. For some it represents a reward for using the CPAP/BPAP machine as well as a congratulatory note.
In the Example 1 summary download (Table 2), a patient used a PAP machine 4 hours or more on 93.3% of the 30 days the machine was used.28 Residual AHI was low, 2.1, and there was no appreciable leak. The PAP of 11.2 cm H2O was in the 90th percentile. The patient was fixed to 12 cm H2O with expiratory pressure relief (EPR) of 1. The EPR is a comfort feature that reduces pressure from 1 cm H2O to 3 cm H2O to make it easier for the patient to exhale. (A flow generator that produces EPR of > 3 cm H2O is a BPAP machine.)
This patient was not a super user. Overall use was low—5 hours, 28 minutes—which could indicate behaviorally insufficient sleep syndrome. Sleep time is controversial, but the National Sleep Foundation recommends 7 to 9 hours of sleep per night.
A different patient used a PAP machine 4 hours or more on 100% (28/28) of the days when the machine was used (Table 3).29 Residual AHI was low (0.6), median use was 8 hours, 47 minutes, and there was no appreciable leak. The patient was using autoset mode with a minimum pressure of 13 cm H2O and maximum pressure of 18 cm H2O. The 95th percentile pressure was 13.6 cm H2O. The patient’s pressure was changed to 14 cm H2O with EPR of 3. This patient was a super user.
Sleep Hygiene Discussion
Providers must discuss sleep hygiene (good sleep habits) with veterans. If needed, AASM pamphlets on sleep hygiene and other educational materials can be provided. The bedroom should be cool, comfortable, quiet, and dark and should not include a television or computer. Exposure to room light before bedtime suppresses melatonin onset and shortens melatonin duration and tells the brain it is time to wake up.34
Patients are asked about the number of arousals they have per night. At first follow-up, providers must determine what is causing a patient to arouse while on CPAP/BPAP therapy. Some causes are air leak resulting in unresolved OSA, nocturia (may be triggered by unresolved OSA), dry mouth (indicating need for chin strap), nightmares (suggestive of unresolved OSA in REM sleep), posttraumatic stress disorder (PTSD), environmental noise, and claustrophobia. The provider should have thought-out answers to these problems in advance.
Epworth Sleepiness Scale
The Epworth Sleepiness Scale (ESS) is administered as part of the baseline comprehensive examination and at every sleep clinic follow-up after issuing a CPAP/BPAP machine.35 The first evaluation after the machine is issued should show a reduction in ESS. No reduction in ESS indicates that a problem needs to be addressed. The most common reason for insufficient reduction in ESS is suboptimal PAP therapy adherence, usually because of a large leak. Some cases of poor adherence may be attributable to restless legs syndrome, periodic limb movement disorder, chronic musculoskeletal pain, and sleep fragmentation caused by alcohol, smoking, caffeine, or cocaine. Excessive daytime sleepiness may persist from use of pain medications or other sedating medications. One study found a correlation between sleep duration with CPAP therapy and reduction in ESS.36 In addition to administering the ESS, patients are asked how they doing with PAP therapy, and the answer is documented. Treatment changes are made if needed to reduce excessive daytime sleepiness.
Ear-Nose-Throat Examination
A quick look into the nose with a nasal speculum is a crucial component of a thorough examination. The clinician looks for a deviated septum, swollen turbinates, obstruction, polyps, bleeding, infection, septal perforation, and discharge. In addition, the patient is checked for airflow amount, nasal congestion, and obstruction; if necessary a nasal steroid spray or a nasal saline spray is prescribed. In some cases, saline spray can be added to the steroid spray to help reduce or eliminate nasal congestion.37
Treatment of congestion requires education, as many patients improperly use these sprays. The steroid spray is not an instant vasoconstrictor; a week of regular use is needed to reduce inflammation and congestion. Saline spray and saline irrigation can be used as a treatment adjunct for symptoms of chronic rhinosinusitis.37If the steroid and saline sprays fail after a 2-month trial, consider an ear-nose-throat (ENT) consultation. A recent study found that adherence rates increased after septoplasty in patients with nasal obstruction.38 The throat is examined for macroglossia or scalloping of the tongue.39 Macroglossic Mallampati IV tongues are platterlike. They are big, long, and wide and often have impressions or scalloping along the outside from a molding of the teeth. The patient is shown a Mallampati diagram and given a Mallampati score.
Creating a Sense of Mission
The sleep physician assistant (PA)at the Detroit VAMC is a retired U.S. Army colonel who ensures that the language the physician uses aligns with the language veterans use. Behavioral techniques are used to create a common culture that helps overcome obstacles—allowing patients to understand the benefits of and need for full CPAP/BPAP therapy adherence. One technique reinforces their sense of mission accomplishment, their military pride, and their interservice rivalry to increase adherence. The mission with each patient is to “work until success is achieved...but the patient can’t quit.” The mantra given to a patient with a difficult case is, “We will not let you fail with CPAP/BPAP therapy,” which echoes a familiar military motto, “We will not leave you behind.” Also, the goal of the physician is: Never give up on the patient.
Behavioral and Psychological Principles
The behavioral and psychological principles for success with PAP super users should be studied to validate better outcomes with longer duration PAP machine use. Patients who are motivated to succeed and to participate in their care can make great strides in changing their behavior to get more and better sleep. Obese patients can get referrals to the MOVE! weight loss program. Some veterans simply follow instructions, pay attention to detail, and do what they are told regarding sleep, PAP education, and good sleep hygiene. Many veterans have poor sleep hygiene and insomnia because they watch television or play games on electronic devices right before bedtime. Many patients develop behaviorally insufficient sleep syndrome. Their behavior prevents them from going to bed at a time that will allow sufficient sleep. Some veterans smoke or drink caffeinated beverages or al cohol immediately before sleep time and then wonder why they have insomnia.
Veterans with insomnia may be referred to the insomnia clinic psychologist for cognitive behavioral therapy for insomnia.40 Referral to this psychologist can be very helpful in the treatment of insomnia after the patient’s OSA has been treated. Veterans are encouraged to follow good sleep hygiene principles and permanently discontinue detrimental sleep behaviors.
For veterans with PTSD, imagery rehearsal before sleep has been effective in resolving disturbing nightmares and excluding their violent details.41 Clinicians recommend that these veterans rehearse a pleasant dream before sleep time. Cartwright and Lamberg performed extensive research on dreams and nightmares, and their book may provide insight into reducing nightmares for veterans with severe PTSD.42 Persistent nightmares associated with PTSD also can be reduced with use of prazosin. 43
Sleep Clinic Economics
The economic impact of OSA is substantial because of increased risk of cardiovascular disease and risk of motor vehicle accidents and decreased quality of life and productivity. Results of cost-effectiveness analyses support the value of diagnosing and treating OSA. Studies have provided estimates from a payer perspective, ranging from $2,000 to $11,000 per quality-adjusted life year over 5 years for treating moderate-to-severe OSA. The Sleep Heart Health Study showed that OSA was associated with an 18% increase in predicted health care utilization based on medication use.44,45 Moreover, CPAP therapy was found to be clinically more effective than no treatment: Therapy increased life expectancy in males and females, and effective treatment of OSA was associated with lower health care and disability costs and fewer missed workdays.
The authors’ initiatives to improve PAP therapy adherence required adding a PA and a registered respiratory therapist (RT) to the staff of 2 full-time equivalent (FTE) board-certified sleep physicians. The sleep physicians trained the PA to initiate and complete all the recommendations described, and the PA attended an AASM-sponsored review course for additional training. The PA is responsible for performing comprehensive face-to-face clinical evaluations in 4 half-day clinic sessions each week, as well as providing follow-up care in 4 additional half-day clinic sessions each week.
During these sessions, the PA provides education about sleep apnea and treatment. Thirty-minute follow-up clinic appointments are reserved for downloading CPAP data, providing interpretation, and educating patients to maximize PAP therapy and become super users. The remaining clinic sessions are run by 3 sleep fellows under the supervision of the sleep physicians. During all visits, providers encourage patients to maintain good sleep hygiene. Nonadherent patients are scheduled to be seen in a separate clinic session during which the RT troubleshoots and corrects PAP machine and mask-related problems.
Setting up the CPAP group classes and follow-up clinics required adding an FTE RT at a cost of $44,000 to $48,000 per year. By recruiting an FTE PA starting at GS-12 and $75,542 instead of another board-certified sleep physician, VAMC Detroit was able to provide increased access to patient care (8 clinics) at sizable financial savings (estimate, $75,000/y). A 0.5 FTE clinical psychologist provided cognitive behavioral therapy for insomnia and PAP therapy nonadherence and helped achieve the initiative’s goals.
The sleep center projects that the overall cost-effectiveness of these initiatives in terms of admission rates, life expectancy, and productivity would not be dissimilar to that reported in the peer-reviewed literature, as noted earlier. The center’s upcoming research projects will provide more data specific to its population. Educating patients requires that only motivated providers give patients instructions during a 30-minute follow-up clinic visit—there is no additional expense. This model of intensive care can be adopted at other VAMCs.
Conclusion
Maximizing PAP machine use is a unique approach that stimulates veterans to attain the highest level of adherence. This approach is based on clinical observation and patient encounters, and treatment recommendations over 8 years.
Showing enthusiasm with patients is crucial. Enthusiasm is contagious. Clinicians who are also PAP machine users should let patients know of their PAP super-user status and add that many others have attained this status, too. The benefits of optimal treatment are reviewed with patients: increased energy, lower risk of cardiovascular disease, lower blood pressure, better insulin sensitivity, and overall reduced mortality. Some patients have difficulty using the nasal mask and chin strap and understanding and adhering to PAP therapy. These impediments can be overcome with further education and follow-up. Sleep clinic clinicians take the time to show patients how to use the machine’s self-adherence check and leak functions. Patients can then monitor their progress daily.
To motivate patients, clinicians should set expectations early, invest time in providing education at follow-up; be diligent with respect to mask fitting and download evaluation. Sleep clinic providers should also speak the veterans’ language, create a self-fulfilling prophesy for success, and schedule a follow-up sleep clinic appointment if a patient is not fulfilling the Medicare adherence criterion of 4 hours’ nightly use for 70% of nights over 30 days.
PAP therapy coaching and persistent education with provider contact and enthusiasm can improve adherence. Encouragement and praise can help patients exceed Medicare’s minimum PAP therapy criterion and improve their overall PAP experience. The sleep team should tell patients they are proud of their accomplishments with such a difficult treatment. Being genuine and caring and showing concern about their evaluation, treatment, and follow-up is important. This helps reduce their OSA-related morbidity, lessen their depression, and improves their daily well-being and quality of life.
“The variation in responses to CPAP and acceptance of CPAP suggest that focused interventions, rather than one-size-fits-all interventions, may have a greater effect on the overall outcome of CPAP adherence,” wrote Weaver and Sawyer.46
Finally, one cannot equate spending on veteran care with spending in other areas of the national budget. The real cost of not giving veterans appropriate care will be a loss of trust, given that the overarching mission is “to care for him who shall have borne the battle and for his widow and his orphan.”
1. Boyaci H, Gacar K, Baris SA, Basyigit I, Yildiz F. Positive airway pressure device compliance of patients with obstructive sleep apnea syndrome. Adv Clin Exp Med. 2013;22(6):809-815.
2. Bachour A, Vitikainen P, Virkkula P, Maasilta P. CPAP interface: satisfaction and side effects. Sleep Breath. 2013;17(2):667-672.
3. Wimms AJ, Richards GN, Genjafield AV. Assessment of the impact on compliance of a new CPAP system in obstructive sleep apnea. Sleep Breath. 2013;17(1):69-76.
4. Smith I, Nadig V, Lasserson TJ. Educational, supportive and behavioral interventions to improve usage of continuous positive airway pressure machines for adults with obstructive sleep apnea. Cochrane Database Syst Rev. 2009;(2):CD007736.
5. Beecroft J, Zanon S, Lukic D, Hanly P. Oral continuous positive airway pressure for sleep apnea: effectiveness, patient preference, and adherence. Chest. 2003;124(6):2200-2208.
6. Chai CL, Pathinathan A, Smith B. Continuous positive airway pressure delivery interfaces for obstructive sleep apnoea. Cochrane Database Syst Rev. 2006;(4):CD005308.
7. Nilius G, Happel A, Domanski U, Ruhle KH. Pressure-relief continuous positive airway pressure vs constant continuous positive airway pressure: a comparison of efficacy and compliance. Chest. 2006;130(4):1018-1024.
8. Ballard RD, Gay PC, Strollo PJ. Interventions to improve compliance in sleep apnea patients previously non-compliant with continuous positive airway pressure. J Clin Sleep Med. 2007;3(7):706-712.
9. Sin DD, Mayers I, Man GC, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002;121(2):430-435.
10. Mortimore IL, Whittle AT, Douglas NJ. Comparison of nose and face mask CPAP therapy for sleep apnoea. Thorax. 1998;53(4):290-292.
11. Haniffa M, Lasserson TJ, Smith I. Interventions to improve compliance with continuous positive airway pressure for obstructive sleep apnoea. Cochrane Database Syst Rev. 2004;(4):CD003531.
12. Kushida CA, Berry RB, Blau, A, et al. Positive airway pressure initiation: a randomized controlled trial to assess the impact of therapy mode and titration process on efficacy, adherence, and outcomes. Sleep. 2011;34(8):1083-1092.
13. Gentina T, Fortin F, Douay B, et al. Auto bi-level with pressure relief during exhalation as a rescue therapy for optimally treated obstructive sleep apnoea patients with poor compliance to continuous positive airways pressure therapy--a pilot study. Sleep Breath. 2011;15(1):21-27.
14. Billings, ME, Auckley D, Benca R, et al. Race and residential socioeconomics as predictors of CPAP adherence. Sleep. 2011;34(12):1653-1658.
15. Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin Sleep Cohort. Sleep. 2008;31(8):1071-1078.
16. Centers for Disease Control and Prevention. Effect of short sleep duration on daily activities--United States, 2005-2008. MMWR Morb Mortal Wkly Rep. 2011;60(8):239-242.
17. Antic NA, Catcheside P, Buchan C, et al. The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep. 2011;34(1):111-119.
18. Phurrough S, Jacques L, Spencer F, Stiller J, Brechner R. Coverage decision memorandum for continuous positive airway pressure (CPAP) therapy for obstructive sleep apnea (OSA) (CAG-00093R2). Centers for Medicare & Medicaid Services Website. https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=204&fromdb=true. Accessed February 5, 2016.
19. Epstein LJ, Kristo D, Strollo PJ Jr, et al; Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2009;5(3):263-276.
20. Berry RB, Chediak A, Brown LK, et al; NPPV Titration Task Force of the American Academy of Sleep Medicine. Best clinical practices for the sleep center adjustment of noninvasive positive pressure ventilation (NPPV) in stable chronic alveolar hypoventilation syndromes. J Clin Sleep Med. 2010;6(5):491-509.
21. Merton RK. Social Theory and Social Structure. New York, NY: Free Press; 1968.
22. Chaput JP, McNeil J, Després JP, Bouchard C, Tremblay A. Seven to eight hours of sleep a night is associated with a lower prevalence of the metabolic syndrome and reduced overall cardiometabolic risk in adults. PLoS One. 2013;8(9):e72832.
23. Born J, Wagner U. Sleep, hormones, and memory. Obstet Gynecol Clin North Am. 2009;36(4):809-829, x.
24. Silva GE, Vana KD, Goodwin JL, Sherrill DL, Quan SF. Identification of patients with sleep disordered breathing: comparing the four-variable screening tool, STOP, STOP-Bang, and Epworth Sleepiness Scales. J Clin Sleep Med. 2011;7(5):467-472.
25. Soares Pires F, Drummond M, Marinho A, et al. Effectiveness of a group education session on adherence with APAP in obstructive sleep apnea--a randomized controlled study. Sleep Breath. 2013;17(3):993-1001.
26. Berry RB, Budhiraja R, Gottlieb DJ, et al; American Academy of Sleep Medicine. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8(5):597-619.
27. Schwab RJ, Badr SM, Epstein LJ, et al; ATS Subcommittee on CPAP Adherence Tracking Systems. An official American Thoracic Society statement: continuous positive airway pressure adherence tracking systems. The optimal monitoring strategies and outcome measures in adults. Am J Respir Crit Care Med. 2013;188(5):613-620.
28. Respironics Encore Pro and Encore Pro 2 [computer program]. Philips, Inc; May 12, 2013.
29. ResMed. Version 04.01.013. San Diego, CA.
30. Knowles SR, O'Brien DT, Zhang S, Devara A, Rowley JA. Effect of addition of chin strap on PAP compliance, nightly duration of use, and other factors. J Clin Sleep Med. 2014;10(4):377-383.
31. Vorona RD, Ware JC, Sinacori JT, Ford ML 3rd, Cross JP. Treatment of severe obstructive sleep apnea syndrome with a chinstrap. J Clin Sleep Med. 2007;3(7):729-730.
32. Ruhle KH, Franke KJ, Domanski U, Nilius G. Quality of life, compliance, sleep and nasopharyngeal side effects during CPAP therapy with and without controlled heated humidification. Sleep Breath. 2011;15(3):479-485.
33. Hamilos DL. Chronic rhinosinusitis: epidemiology and medical management. J Allergy Clin Immunol. 2011;128(4):693-707.
34. Gooley JJ, Chamberlain K, Smith KA, et al. Exposure to room light before bedtime suppresses melatonin onset and shortens melatonin duration in humans. J Clin Endocrinol Metab. 2011;96(3):E463-E472.
35. Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991;14(6):540-545.
36. Bednarek M, Zgierska A, Pływaczewski R, Zielinski J. The effect of CPAP treatment on excessive daytime somnolence in patients with obstructive sleep apnea [in Polish]. Pneumonol Alergol Pol. 1999;67(5-6):237-244.
37. Harvey R, Hannan SA, Badia L, Scadding G. Nasal saline irrigations for the symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev. 2007;(3):CD006394.
38. Poirier J, George C, Rotenberg B. The effect of nasal surgery on nasal continuous positive airway pressure compliance. Laryngoscope. 2014;124(1):317-319.
39. Law JA. From the journal archives: Mallampati in two millennia: its impact then and implications now. Can J Anaesth. 2014;61(5):480-484.
40. Hood HK, Rogojanski J, Moss TG. Cognitive-behavioral therapy for chronic insomnia. Curr Treat Options Neurol. 2014;16(12):321.
41. Harb GC, Thompson R, Ross RJ, Cook JM. Combat-related PTSD nightmares and imagery rehearsal: nightmare characteristics and relation to treatment outcome. J Trauma Stress. 2012;25(5):511-518.
42. Cartwright R, Lamberg L. Crisis Dreaming: Using Your Dreams to Solve Your Problems.. New York, NY: HarperCollins;1992.
43.Writer BW, Meyer EG, Schillerstrom JE. Prazosin for military combat-related PTSD nightmares: a critical review. J Neuropsychiatry Clin Neurosci. 2014;26(1):24-33.
44. Park JG, Ramar K, Olson EJ. Updates on definition, consequences, and management of obstructive sleep apnea. Mayo Clin Proc. 2011;86(6):549-554.
45. Kapur V, Blough DK, Sandblom RE, et al. The medical cost of undiagnosed sleep apnea. Sleep. 1999;22(6):749-755.
46. Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res. 2010;131:245-258.
1. Boyaci H, Gacar K, Baris SA, Basyigit I, Yildiz F. Positive airway pressure device compliance of patients with obstructive sleep apnea syndrome. Adv Clin Exp Med. 2013;22(6):809-815.
2. Bachour A, Vitikainen P, Virkkula P, Maasilta P. CPAP interface: satisfaction and side effects. Sleep Breath. 2013;17(2):667-672.
3. Wimms AJ, Richards GN, Genjafield AV. Assessment of the impact on compliance of a new CPAP system in obstructive sleep apnea. Sleep Breath. 2013;17(1):69-76.
4. Smith I, Nadig V, Lasserson TJ. Educational, supportive and behavioral interventions to improve usage of continuous positive airway pressure machines for adults with obstructive sleep apnea. Cochrane Database Syst Rev. 2009;(2):CD007736.
5. Beecroft J, Zanon S, Lukic D, Hanly P. Oral continuous positive airway pressure for sleep apnea: effectiveness, patient preference, and adherence. Chest. 2003;124(6):2200-2208.
6. Chai CL, Pathinathan A, Smith B. Continuous positive airway pressure delivery interfaces for obstructive sleep apnoea. Cochrane Database Syst Rev. 2006;(4):CD005308.
7. Nilius G, Happel A, Domanski U, Ruhle KH. Pressure-relief continuous positive airway pressure vs constant continuous positive airway pressure: a comparison of efficacy and compliance. Chest. 2006;130(4):1018-1024.
8. Ballard RD, Gay PC, Strollo PJ. Interventions to improve compliance in sleep apnea patients previously non-compliant with continuous positive airway pressure. J Clin Sleep Med. 2007;3(7):706-712.
9. Sin DD, Mayers I, Man GC, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002;121(2):430-435.
10. Mortimore IL, Whittle AT, Douglas NJ. Comparison of nose and face mask CPAP therapy for sleep apnoea. Thorax. 1998;53(4):290-292.
11. Haniffa M, Lasserson TJ, Smith I. Interventions to improve compliance with continuous positive airway pressure for obstructive sleep apnoea. Cochrane Database Syst Rev. 2004;(4):CD003531.
12. Kushida CA, Berry RB, Blau, A, et al. Positive airway pressure initiation: a randomized controlled trial to assess the impact of therapy mode and titration process on efficacy, adherence, and outcomes. Sleep. 2011;34(8):1083-1092.
13. Gentina T, Fortin F, Douay B, et al. Auto bi-level with pressure relief during exhalation as a rescue therapy for optimally treated obstructive sleep apnoea patients with poor compliance to continuous positive airways pressure therapy--a pilot study. Sleep Breath. 2011;15(1):21-27.
14. Billings, ME, Auckley D, Benca R, et al. Race and residential socioeconomics as predictors of CPAP adherence. Sleep. 2011;34(12):1653-1658.
15. Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin Sleep Cohort. Sleep. 2008;31(8):1071-1078.
16. Centers for Disease Control and Prevention. Effect of short sleep duration on daily activities--United States, 2005-2008. MMWR Morb Mortal Wkly Rep. 2011;60(8):239-242.
17. Antic NA, Catcheside P, Buchan C, et al. The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep. 2011;34(1):111-119.
18. Phurrough S, Jacques L, Spencer F, Stiller J, Brechner R. Coverage decision memorandum for continuous positive airway pressure (CPAP) therapy for obstructive sleep apnea (OSA) (CAG-00093R2). Centers for Medicare & Medicaid Services Website. https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=204&fromdb=true. Accessed February 5, 2016.
19. Epstein LJ, Kristo D, Strollo PJ Jr, et al; Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2009;5(3):263-276.
20. Berry RB, Chediak A, Brown LK, et al; NPPV Titration Task Force of the American Academy of Sleep Medicine. Best clinical practices for the sleep center adjustment of noninvasive positive pressure ventilation (NPPV) in stable chronic alveolar hypoventilation syndromes. J Clin Sleep Med. 2010;6(5):491-509.
21. Merton RK. Social Theory and Social Structure. New York, NY: Free Press; 1968.
22. Chaput JP, McNeil J, Després JP, Bouchard C, Tremblay A. Seven to eight hours of sleep a night is associated with a lower prevalence of the metabolic syndrome and reduced overall cardiometabolic risk in adults. PLoS One. 2013;8(9):e72832.
23. Born J, Wagner U. Sleep, hormones, and memory. Obstet Gynecol Clin North Am. 2009;36(4):809-829, x.
24. Silva GE, Vana KD, Goodwin JL, Sherrill DL, Quan SF. Identification of patients with sleep disordered breathing: comparing the four-variable screening tool, STOP, STOP-Bang, and Epworth Sleepiness Scales. J Clin Sleep Med. 2011;7(5):467-472.
25. Soares Pires F, Drummond M, Marinho A, et al. Effectiveness of a group education session on adherence with APAP in obstructive sleep apnea--a randomized controlled study. Sleep Breath. 2013;17(3):993-1001.
26. Berry RB, Budhiraja R, Gottlieb DJ, et al; American Academy of Sleep Medicine. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8(5):597-619.
27. Schwab RJ, Badr SM, Epstein LJ, et al; ATS Subcommittee on CPAP Adherence Tracking Systems. An official American Thoracic Society statement: continuous positive airway pressure adherence tracking systems. The optimal monitoring strategies and outcome measures in adults. Am J Respir Crit Care Med. 2013;188(5):613-620.
28. Respironics Encore Pro and Encore Pro 2 [computer program]. Philips, Inc; May 12, 2013.
29. ResMed. Version 04.01.013. San Diego, CA.
30. Knowles SR, O'Brien DT, Zhang S, Devara A, Rowley JA. Effect of addition of chin strap on PAP compliance, nightly duration of use, and other factors. J Clin Sleep Med. 2014;10(4):377-383.
31. Vorona RD, Ware JC, Sinacori JT, Ford ML 3rd, Cross JP. Treatment of severe obstructive sleep apnea syndrome with a chinstrap. J Clin Sleep Med. 2007;3(7):729-730.
32. Ruhle KH, Franke KJ, Domanski U, Nilius G. Quality of life, compliance, sleep and nasopharyngeal side effects during CPAP therapy with and without controlled heated humidification. Sleep Breath. 2011;15(3):479-485.
33. Hamilos DL. Chronic rhinosinusitis: epidemiology and medical management. J Allergy Clin Immunol. 2011;128(4):693-707.
34. Gooley JJ, Chamberlain K, Smith KA, et al. Exposure to room light before bedtime suppresses melatonin onset and shortens melatonin duration in humans. J Clin Endocrinol Metab. 2011;96(3):E463-E472.
35. Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991;14(6):540-545.
36. Bednarek M, Zgierska A, Pływaczewski R, Zielinski J. The effect of CPAP treatment on excessive daytime somnolence in patients with obstructive sleep apnea [in Polish]. Pneumonol Alergol Pol. 1999;67(5-6):237-244.
37. Harvey R, Hannan SA, Badia L, Scadding G. Nasal saline irrigations for the symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev. 2007;(3):CD006394.
38. Poirier J, George C, Rotenberg B. The effect of nasal surgery on nasal continuous positive airway pressure compliance. Laryngoscope. 2014;124(1):317-319.
39. Law JA. From the journal archives: Mallampati in two millennia: its impact then and implications now. Can J Anaesth. 2014;61(5):480-484.
40. Hood HK, Rogojanski J, Moss TG. Cognitive-behavioral therapy for chronic insomnia. Curr Treat Options Neurol. 2014;16(12):321.
41. Harb GC, Thompson R, Ross RJ, Cook JM. Combat-related PTSD nightmares and imagery rehearsal: nightmare characteristics and relation to treatment outcome. J Trauma Stress. 2012;25(5):511-518.
42. Cartwright R, Lamberg L. Crisis Dreaming: Using Your Dreams to Solve Your Problems.. New York, NY: HarperCollins;1992.
43.Writer BW, Meyer EG, Schillerstrom JE. Prazosin for military combat-related PTSD nightmares: a critical review. J Neuropsychiatry Clin Neurosci. 2014;26(1):24-33.
44. Park JG, Ramar K, Olson EJ. Updates on definition, consequences, and management of obstructive sleep apnea. Mayo Clin Proc. 2011;86(6):549-554.
45. Kapur V, Blough DK, Sandblom RE, et al. The medical cost of undiagnosed sleep apnea. Sleep. 1999;22(6):749-755.
46. Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res. 2010;131:245-258.