User login
Last month the Food and Drug Administration approved the first vaccine (Gardisil) to prevent infection with specific types of human papillomavirus (HPV). The approval is the culmination of 2 decades of work in a variety of disciplines that have clearly demonstrated that infection with specific types of high-risk HPV is required for the development of cervical cancer—and that the development of HPV-associated disease can be prevented through vaccination.
How and when will HPV vaccine be put to use?
It is important to recognize that FDA approval does not mean the HPV vaccine will be widely used. Five components are necessary for successful introduction:
1. FDA approval
FDA approval is based solely on the safety and effectiveness of the vaccine.
Indications. The FDA determined that the quadrivalent HPV vaccine is indicated for prevention of HPV 6, 11, 16, and 18 associated cervical cancer, genital warts, CIN, AIS, and VIN 2,3 and VAIN 2,3.
The indication applies to girls and women 9 to 26 years of age. The indication in girls 9 to 15 years of age, who were not included in the Phase II and III trials, was based on immunological “bridging” studies that demonstrated better immune responses to vaccination in this group than in the older group enrolled in the trials.
2. Federal-level recommendations
The second component of a successful vaccine introduction is the support of the Advisory Committee on Immunization Practices (ACIP),2 a congressionally mandated federal advisory committee coordinated by the Centers for Disease Control and Prevention (CDC). The ACIP advises the Secretary of Health and Human Services, as well as the Director of the CDC, on appropriate immunization practices for the United States.
Within several months of the June 2006 FDA approval, the ACIP will make a recommendation on the vaccine’s use. When making its recommendation, the ACIP takes into account the burden of disease in the population, safety and efficacy, and health economics of vaccination—will it be cost-effective?
Funding and insurance coverage at stake. The ACIP also determines whether the vaccine will be acceptable to physicians and consumers and what programmatic issues are associated with its introduction.
- Public funding. The ACIP recommendation strongly influences standard of practice, and is relied upon by the federal government and states for determining whether to include a vaccine in public funding programs.
- Insurers likewise look to the ACIP for guidance when setting reimbursement policy.
3. Achieving adequate funding
The third component of a successful vaccine introduction is achieving adequate funding. Federal and state programs such as the Vaccines for Children (VFC) program currently pay for more than half of all childhood vaccinations. Therefore it is important that these programs include the HPV vaccine in order to ensure it is widely available, especially among lower socio-economic groups.
4. Recommendations by professional societies
Societies such as the American Academy of Pediatrics, the American College of Obstetricians and Gynecologists, and the American Academy of Family Physicians, whose members provide most of the vaccinations in the US, have representatives who work directly with the ACIP. Many societies make their own vaccination recommendations, as well.
5. Advocacy and education
Other groups increase awareness of the need for vaccination among consumers, public health and government officials, and clinicians.
The quadrivalent vaccine consists of recombinant viral-like particles (VLPs) derived from the 4 different types of HPV (6, 11, 16, and 18) which, combined, account for approximately 70% of all invasive cervical cancers, 60% of high-grade CIN lesions, and more than 90% of genital warts, both in the United States and globally.
The biotechnology. The VLPs used in the HPV vaccines are produced by cloning the major viral capsid genes (L1) from the 4 different HPV types, inserting them into plasmids, and then producing large amounts of the L1 proteins of each of the HPV types separately in yeast. The recombinant L1 proteins are subsequently self-assembled into VLPs that structurally appear identical to HPV virions, but which lack both DNA and RNA.
Therefore, the VLPs are completely non-infectious and non-oncogenic. The purified VLPs are then mixed with an aluminum-containing adjuvant to produce the final vaccine.
Administration. It is administered intramuscularly as 3 injections over a 6-month period: at enrollment and at 2 and 6 months.
A bivalent vaccine for HPV 16 and 18 produced by GlaxoSmithKline is based on similar technology, and will most likely become available in 2007.
Clinical trials: 100% effective, well-accepted, safe
FDA approval of the quadrivalent HPV vaccine came approximately 18 months earlier than expected because, in the Phase III trials, the vaccine proved much more effective than originally predicted, thus shortening the length of follow-up needed to reach the endpoints.
Efficacy and safety studies. Generally, the vaccine appears to be well-accepted and safe. To date, the efficacy and safety of the quadrivalent vaccine have been evaluated in 4 Phase II and III studies that included 20,541 females aged 16 to 26 who were followed for a median of 2 to 4 years in the different studies.1 The endpoint for these trials was biopsy-confirmed high-grade cervical neoplasia, including CIN 2,3 and adenocarcinoma in-situ (AIS). The primary analyses of efficacy were conducted in the “per protocol population,” which consisted of women who received all 3 vaccinations and who were both DNA and serologically negative for the relevant HPV types during the 6-month vaccination period.
In each of the 4 trials, the quadrivalent vaccine was found to be 100% efficacious against HPV 16 and 18 associated CIN 2,3 and AIS. Similarly, the vaccine was also highly efficacious against HPV 6, 11, 16, or 18 associated genital warts.
Adverse events. Although injection site pain, swelling, erythema, and pruritus were increased in vaccine recipients compared to placebo, few subjects (0.1%) discontinued the study as a result of adverse experiences.
Varicella vaccine success story. Varicella vaccine was approved in the 1990s, but both physicians and the public were slow to accept it, in part because it was relatively expensive for physicians to buy, and insurance companies were slow to pay for vaccination. What brought about widespread adoption of varicella vaccination was education on the dangers of chicken pox, directed to clinicians, patients, and government officials. This led to appreciation of the benefits of vaccination. As a result, states changed their school entry requirements, and today, almost all children receive the varicella vaccine.
The unknowns
It is important to recognize that with all new vaccines there are unknowns when they are first introduced.
What will the ACIP recommend?
One of the biggest concerns about the HPV vaccines is that we do not yet know who the ACIP will recommend for vaccination. In the clinical trials, the HPV vaccine did not appear effective in women already exposed to HPV. Since the cumulative incidence of HPV infection in young women is approximately 40% within 2 years of initiating intercourse, we will need to target adolescents prior to onset of sexual activity.3 In the US, 7.4% of adolescents report having begun having sexual intercourse by 13 years of age, and about one third by the ninth grade.4 Therefore the most likely primary target population will be young girls 11 to 12 years of age. It is also likely that there will be a recommendation for “catch-up” vaccination of older girls and young women.
What is the duration of protection afforded by HPV vaccination?
We know that the vaccine appears to provide protection for at least 4 years, but if we vaccinate 11- to 12-year-old girls, will they require a booster later in life?5
How will HPV vaccination affect cervical screening?
Once vaccination is widespread, a significant reduction in CIN 2,3 will occur, necessitating changes in the age to start screening and screening frequency. However, it is unclear what percentage of the population will need to be vaccinated before we change screening policy.
Will HPV vaccine be efficacious in women over the age of 26 years?
Vaccine trials are currently underway in older women, but until these trials are completed, all we can tell our older, sexually active patients is that we simply don’t know if the vaccine will benefit them.
Will parents, adolescents, and the public at large accept the vaccine?
As with all issues relating to sexual behavior, it is likely that opinions will differ as to the acceptability of vaccinating young adolescents against a sexually transmitted disease.
1. Gardasil package insert. Released June 2006.
2. Orenstein S, Rodewald L, Hinman A. Immunization in the United States. In: Plotkin SA, Orenstein S, editors. Vaccines. 4th ed. Philadelphia: WB Saunders Company; 2004:1357-1386.
3. Winer RL, Lee SK, Hughes JP, Adam DE, Kiviat NB, Koutsky LA. Genital human papillomavirus infection: incidence and risk factors in a cohort of female university students. Am J Epidemiol. 2003;157:218-226.
4. Whalen L, Grunbaum J, Kinchen S, McManus T, Shanklin S, Kann L. Middle School: Youth Risk Behavior Survey 2003. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2005.
5. Mao C, Koutsky LA, Ault KA, Wheeler CM, Brown DR, Wiley DJ, et al. Efficacy of human papillomavirus-16 vaccine to prevent cervical intraepithelial neoplasia: a randomized controlled trial. Obstet Gynecol. 2006;107:18-27.
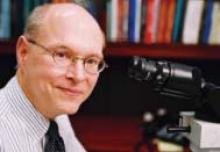
Dr. Wright is the chairman of the upcoming ASCCP (American Society for Colposcopy and Cervical Pathology) 2006 Consensus Conference. He is an author of the 2001 Consensus Guidelines on Managing Women with Cytological and Histological Abnormalities, the 2004 Interim Guidance for Use of HPV DNA testing for Primary Screening, and the 2001 Bethesda System. He is a Professor of Pathology, Columbia University, New York City.
Dr. Wright serves as a consultant to GlaxoSmithKline.
Last month the Food and Drug Administration approved the first vaccine (Gardisil) to prevent infection with specific types of human papillomavirus (HPV). The approval is the culmination of 2 decades of work in a variety of disciplines that have clearly demonstrated that infection with specific types of high-risk HPV is required for the development of cervical cancer—and that the development of HPV-associated disease can be prevented through vaccination.
How and when will HPV vaccine be put to use?
It is important to recognize that FDA approval does not mean the HPV vaccine will be widely used. Five components are necessary for successful introduction:
1. FDA approval
FDA approval is based solely on the safety and effectiveness of the vaccine.
Indications. The FDA determined that the quadrivalent HPV vaccine is indicated for prevention of HPV 6, 11, 16, and 18 associated cervical cancer, genital warts, CIN, AIS, and VIN 2,3 and VAIN 2,3.
The indication applies to girls and women 9 to 26 years of age. The indication in girls 9 to 15 years of age, who were not included in the Phase II and III trials, was based on immunological “bridging” studies that demonstrated better immune responses to vaccination in this group than in the older group enrolled in the trials.
2. Federal-level recommendations
The second component of a successful vaccine introduction is the support of the Advisory Committee on Immunization Practices (ACIP),2 a congressionally mandated federal advisory committee coordinated by the Centers for Disease Control and Prevention (CDC). The ACIP advises the Secretary of Health and Human Services, as well as the Director of the CDC, on appropriate immunization practices for the United States.
Within several months of the June 2006 FDA approval, the ACIP will make a recommendation on the vaccine’s use. When making its recommendation, the ACIP takes into account the burden of disease in the population, safety and efficacy, and health economics of vaccination—will it be cost-effective?
Funding and insurance coverage at stake. The ACIP also determines whether the vaccine will be acceptable to physicians and consumers and what programmatic issues are associated with its introduction.
- Public funding. The ACIP recommendation strongly influences standard of practice, and is relied upon by the federal government and states for determining whether to include a vaccine in public funding programs.
- Insurers likewise look to the ACIP for guidance when setting reimbursement policy.
3. Achieving adequate funding
The third component of a successful vaccine introduction is achieving adequate funding. Federal and state programs such as the Vaccines for Children (VFC) program currently pay for more than half of all childhood vaccinations. Therefore it is important that these programs include the HPV vaccine in order to ensure it is widely available, especially among lower socio-economic groups.
4. Recommendations by professional societies
Societies such as the American Academy of Pediatrics, the American College of Obstetricians and Gynecologists, and the American Academy of Family Physicians, whose members provide most of the vaccinations in the US, have representatives who work directly with the ACIP. Many societies make their own vaccination recommendations, as well.
5. Advocacy and education
Other groups increase awareness of the need for vaccination among consumers, public health and government officials, and clinicians.
The quadrivalent vaccine consists of recombinant viral-like particles (VLPs) derived from the 4 different types of HPV (6, 11, 16, and 18) which, combined, account for approximately 70% of all invasive cervical cancers, 60% of high-grade CIN lesions, and more than 90% of genital warts, both in the United States and globally.
The biotechnology. The VLPs used in the HPV vaccines are produced by cloning the major viral capsid genes (L1) from the 4 different HPV types, inserting them into plasmids, and then producing large amounts of the L1 proteins of each of the HPV types separately in yeast. The recombinant L1 proteins are subsequently self-assembled into VLPs that structurally appear identical to HPV virions, but which lack both DNA and RNA.
Therefore, the VLPs are completely non-infectious and non-oncogenic. The purified VLPs are then mixed with an aluminum-containing adjuvant to produce the final vaccine.
Administration. It is administered intramuscularly as 3 injections over a 6-month period: at enrollment and at 2 and 6 months.
A bivalent vaccine for HPV 16 and 18 produced by GlaxoSmithKline is based on similar technology, and will most likely become available in 2007.
Clinical trials: 100% effective, well-accepted, safe
FDA approval of the quadrivalent HPV vaccine came approximately 18 months earlier than expected because, in the Phase III trials, the vaccine proved much more effective than originally predicted, thus shortening the length of follow-up needed to reach the endpoints.
Efficacy and safety studies. Generally, the vaccine appears to be well-accepted and safe. To date, the efficacy and safety of the quadrivalent vaccine have been evaluated in 4 Phase II and III studies that included 20,541 females aged 16 to 26 who were followed for a median of 2 to 4 years in the different studies.1 The endpoint for these trials was biopsy-confirmed high-grade cervical neoplasia, including CIN 2,3 and adenocarcinoma in-situ (AIS). The primary analyses of efficacy were conducted in the “per protocol population,” which consisted of women who received all 3 vaccinations and who were both DNA and serologically negative for the relevant HPV types during the 6-month vaccination period.
In each of the 4 trials, the quadrivalent vaccine was found to be 100% efficacious against HPV 16 and 18 associated CIN 2,3 and AIS. Similarly, the vaccine was also highly efficacious against HPV 6, 11, 16, or 18 associated genital warts.
Adverse events. Although injection site pain, swelling, erythema, and pruritus were increased in vaccine recipients compared to placebo, few subjects (0.1%) discontinued the study as a result of adverse experiences.
Varicella vaccine success story. Varicella vaccine was approved in the 1990s, but both physicians and the public were slow to accept it, in part because it was relatively expensive for physicians to buy, and insurance companies were slow to pay for vaccination. What brought about widespread adoption of varicella vaccination was education on the dangers of chicken pox, directed to clinicians, patients, and government officials. This led to appreciation of the benefits of vaccination. As a result, states changed their school entry requirements, and today, almost all children receive the varicella vaccine.
The unknowns
It is important to recognize that with all new vaccines there are unknowns when they are first introduced.
What will the ACIP recommend?
One of the biggest concerns about the HPV vaccines is that we do not yet know who the ACIP will recommend for vaccination. In the clinical trials, the HPV vaccine did not appear effective in women already exposed to HPV. Since the cumulative incidence of HPV infection in young women is approximately 40% within 2 years of initiating intercourse, we will need to target adolescents prior to onset of sexual activity.3 In the US, 7.4% of adolescents report having begun having sexual intercourse by 13 years of age, and about one third by the ninth grade.4 Therefore the most likely primary target population will be young girls 11 to 12 years of age. It is also likely that there will be a recommendation for “catch-up” vaccination of older girls and young women.
What is the duration of protection afforded by HPV vaccination?
We know that the vaccine appears to provide protection for at least 4 years, but if we vaccinate 11- to 12-year-old girls, will they require a booster later in life?5
How will HPV vaccination affect cervical screening?
Once vaccination is widespread, a significant reduction in CIN 2,3 will occur, necessitating changes in the age to start screening and screening frequency. However, it is unclear what percentage of the population will need to be vaccinated before we change screening policy.
Will HPV vaccine be efficacious in women over the age of 26 years?
Vaccine trials are currently underway in older women, but until these trials are completed, all we can tell our older, sexually active patients is that we simply don’t know if the vaccine will benefit them.
Will parents, adolescents, and the public at large accept the vaccine?
As with all issues relating to sexual behavior, it is likely that opinions will differ as to the acceptability of vaccinating young adolescents against a sexually transmitted disease.
Last month the Food and Drug Administration approved the first vaccine (Gardisil) to prevent infection with specific types of human papillomavirus (HPV). The approval is the culmination of 2 decades of work in a variety of disciplines that have clearly demonstrated that infection with specific types of high-risk HPV is required for the development of cervical cancer—and that the development of HPV-associated disease can be prevented through vaccination.
How and when will HPV vaccine be put to use?
It is important to recognize that FDA approval does not mean the HPV vaccine will be widely used. Five components are necessary for successful introduction:
1. FDA approval
FDA approval is based solely on the safety and effectiveness of the vaccine.
Indications. The FDA determined that the quadrivalent HPV vaccine is indicated for prevention of HPV 6, 11, 16, and 18 associated cervical cancer, genital warts, CIN, AIS, and VIN 2,3 and VAIN 2,3.
The indication applies to girls and women 9 to 26 years of age. The indication in girls 9 to 15 years of age, who were not included in the Phase II and III trials, was based on immunological “bridging” studies that demonstrated better immune responses to vaccination in this group than in the older group enrolled in the trials.
2. Federal-level recommendations
The second component of a successful vaccine introduction is the support of the Advisory Committee on Immunization Practices (ACIP),2 a congressionally mandated federal advisory committee coordinated by the Centers for Disease Control and Prevention (CDC). The ACIP advises the Secretary of Health and Human Services, as well as the Director of the CDC, on appropriate immunization practices for the United States.
Within several months of the June 2006 FDA approval, the ACIP will make a recommendation on the vaccine’s use. When making its recommendation, the ACIP takes into account the burden of disease in the population, safety and efficacy, and health economics of vaccination—will it be cost-effective?
Funding and insurance coverage at stake. The ACIP also determines whether the vaccine will be acceptable to physicians and consumers and what programmatic issues are associated with its introduction.
- Public funding. The ACIP recommendation strongly influences standard of practice, and is relied upon by the federal government and states for determining whether to include a vaccine in public funding programs.
- Insurers likewise look to the ACIP for guidance when setting reimbursement policy.
3. Achieving adequate funding
The third component of a successful vaccine introduction is achieving adequate funding. Federal and state programs such as the Vaccines for Children (VFC) program currently pay for more than half of all childhood vaccinations. Therefore it is important that these programs include the HPV vaccine in order to ensure it is widely available, especially among lower socio-economic groups.
4. Recommendations by professional societies
Societies such as the American Academy of Pediatrics, the American College of Obstetricians and Gynecologists, and the American Academy of Family Physicians, whose members provide most of the vaccinations in the US, have representatives who work directly with the ACIP. Many societies make their own vaccination recommendations, as well.
5. Advocacy and education
Other groups increase awareness of the need for vaccination among consumers, public health and government officials, and clinicians.
The quadrivalent vaccine consists of recombinant viral-like particles (VLPs) derived from the 4 different types of HPV (6, 11, 16, and 18) which, combined, account for approximately 70% of all invasive cervical cancers, 60% of high-grade CIN lesions, and more than 90% of genital warts, both in the United States and globally.
The biotechnology. The VLPs used in the HPV vaccines are produced by cloning the major viral capsid genes (L1) from the 4 different HPV types, inserting them into plasmids, and then producing large amounts of the L1 proteins of each of the HPV types separately in yeast. The recombinant L1 proteins are subsequently self-assembled into VLPs that structurally appear identical to HPV virions, but which lack both DNA and RNA.
Therefore, the VLPs are completely non-infectious and non-oncogenic. The purified VLPs are then mixed with an aluminum-containing adjuvant to produce the final vaccine.
Administration. It is administered intramuscularly as 3 injections over a 6-month period: at enrollment and at 2 and 6 months.
A bivalent vaccine for HPV 16 and 18 produced by GlaxoSmithKline is based on similar technology, and will most likely become available in 2007.
Clinical trials: 100% effective, well-accepted, safe
FDA approval of the quadrivalent HPV vaccine came approximately 18 months earlier than expected because, in the Phase III trials, the vaccine proved much more effective than originally predicted, thus shortening the length of follow-up needed to reach the endpoints.
Efficacy and safety studies. Generally, the vaccine appears to be well-accepted and safe. To date, the efficacy and safety of the quadrivalent vaccine have been evaluated in 4 Phase II and III studies that included 20,541 females aged 16 to 26 who were followed for a median of 2 to 4 years in the different studies.1 The endpoint for these trials was biopsy-confirmed high-grade cervical neoplasia, including CIN 2,3 and adenocarcinoma in-situ (AIS). The primary analyses of efficacy were conducted in the “per protocol population,” which consisted of women who received all 3 vaccinations and who were both DNA and serologically negative for the relevant HPV types during the 6-month vaccination period.
In each of the 4 trials, the quadrivalent vaccine was found to be 100% efficacious against HPV 16 and 18 associated CIN 2,3 and AIS. Similarly, the vaccine was also highly efficacious against HPV 6, 11, 16, or 18 associated genital warts.
Adverse events. Although injection site pain, swelling, erythema, and pruritus were increased in vaccine recipients compared to placebo, few subjects (0.1%) discontinued the study as a result of adverse experiences.
Varicella vaccine success story. Varicella vaccine was approved in the 1990s, but both physicians and the public were slow to accept it, in part because it was relatively expensive for physicians to buy, and insurance companies were slow to pay for vaccination. What brought about widespread adoption of varicella vaccination was education on the dangers of chicken pox, directed to clinicians, patients, and government officials. This led to appreciation of the benefits of vaccination. As a result, states changed their school entry requirements, and today, almost all children receive the varicella vaccine.
The unknowns
It is important to recognize that with all new vaccines there are unknowns when they are first introduced.
What will the ACIP recommend?
One of the biggest concerns about the HPV vaccines is that we do not yet know who the ACIP will recommend for vaccination. In the clinical trials, the HPV vaccine did not appear effective in women already exposed to HPV. Since the cumulative incidence of HPV infection in young women is approximately 40% within 2 years of initiating intercourse, we will need to target adolescents prior to onset of sexual activity.3 In the US, 7.4% of adolescents report having begun having sexual intercourse by 13 years of age, and about one third by the ninth grade.4 Therefore the most likely primary target population will be young girls 11 to 12 years of age. It is also likely that there will be a recommendation for “catch-up” vaccination of older girls and young women.
What is the duration of protection afforded by HPV vaccination?
We know that the vaccine appears to provide protection for at least 4 years, but if we vaccinate 11- to 12-year-old girls, will they require a booster later in life?5
How will HPV vaccination affect cervical screening?
Once vaccination is widespread, a significant reduction in CIN 2,3 will occur, necessitating changes in the age to start screening and screening frequency. However, it is unclear what percentage of the population will need to be vaccinated before we change screening policy.
Will HPV vaccine be efficacious in women over the age of 26 years?
Vaccine trials are currently underway in older women, but until these trials are completed, all we can tell our older, sexually active patients is that we simply don’t know if the vaccine will benefit them.
Will parents, adolescents, and the public at large accept the vaccine?
As with all issues relating to sexual behavior, it is likely that opinions will differ as to the acceptability of vaccinating young adolescents against a sexually transmitted disease.
1. Gardasil package insert. Released June 2006.
2. Orenstein S, Rodewald L, Hinman A. Immunization in the United States. In: Plotkin SA, Orenstein S, editors. Vaccines. 4th ed. Philadelphia: WB Saunders Company; 2004:1357-1386.
3. Winer RL, Lee SK, Hughes JP, Adam DE, Kiviat NB, Koutsky LA. Genital human papillomavirus infection: incidence and risk factors in a cohort of female university students. Am J Epidemiol. 2003;157:218-226.
4. Whalen L, Grunbaum J, Kinchen S, McManus T, Shanklin S, Kann L. Middle School: Youth Risk Behavior Survey 2003. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2005.
5. Mao C, Koutsky LA, Ault KA, Wheeler CM, Brown DR, Wiley DJ, et al. Efficacy of human papillomavirus-16 vaccine to prevent cervical intraepithelial neoplasia: a randomized controlled trial. Obstet Gynecol. 2006;107:18-27.
Dr. Wright is the chairman of the upcoming ASCCP (American Society for Colposcopy and Cervical Pathology) 2006 Consensus Conference. He is an author of the 2001 Consensus Guidelines on Managing Women with Cytological and Histological Abnormalities, the 2004 Interim Guidance for Use of HPV DNA testing for Primary Screening, and the 2001 Bethesda System. He is a Professor of Pathology, Columbia University, New York City.
Dr. Wright serves as a consultant to GlaxoSmithKline.
1. Gardasil package insert. Released June 2006.
2. Orenstein S, Rodewald L, Hinman A. Immunization in the United States. In: Plotkin SA, Orenstein S, editors. Vaccines. 4th ed. Philadelphia: WB Saunders Company; 2004:1357-1386.
3. Winer RL, Lee SK, Hughes JP, Adam DE, Kiviat NB, Koutsky LA. Genital human papillomavirus infection: incidence and risk factors in a cohort of female university students. Am J Epidemiol. 2003;157:218-226.
4. Whalen L, Grunbaum J, Kinchen S, McManus T, Shanklin S, Kann L. Middle School: Youth Risk Behavior Survey 2003. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2005.
5. Mao C, Koutsky LA, Ault KA, Wheeler CM, Brown DR, Wiley DJ, et al. Efficacy of human papillomavirus-16 vaccine to prevent cervical intraepithelial neoplasia: a randomized controlled trial. Obstet Gynecol. 2006;107:18-27.
Dr. Wright is the chairman of the upcoming ASCCP (American Society for Colposcopy and Cervical Pathology) 2006 Consensus Conference. He is an author of the 2001 Consensus Guidelines on Managing Women with Cytological and Histological Abnormalities, the 2004 Interim Guidance for Use of HPV DNA testing for Primary Screening, and the 2001 Bethesda System. He is a Professor of Pathology, Columbia University, New York City.
Dr. Wright serves as a consultant to GlaxoSmithKline.
IN THIS ARTICLE