User login
CE/CME No: CR-1310
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Describe the pathophysiology of Ménière’s disease, as it is currently understood.
• Discuss the triad of symptoms that should prompt suspicion for Ménière’s disease in a primary care patient.
• List the diagnostic criteria for “definite” Ménière’s disease, as defined by the American Academy of Otolaryngology–Head and Neck Surgery.
• Review pharmacologic management, intratympanic injection and other nonoperative therapies, and surgical treatment for Ménière’s disease.
FACULTY
Tamera Pearson is an Associate Professor in the School of Nursing at Western Carolina University.
The author has no significant financial relationships to disclose.
ACCREDITATION STATEMENT
Article begins on next page >>
Ménière’s disease is a complex disorder of intermittent vertigo, tinnitus, and hearing loss whose symptoms usually manifest between ages 20 and 60. Although this disorder is uncommon, its impact on a person’s quality of life can be significant. Here are the symptoms, criteria for diagnosis, and appropriate treatment or referrals for Ménière’s disease.
Ménière’s disease can significantly affect a person’s quality of life and is a challenge to diagnose and treat effectively. The French physician Prosper Ménière first described this disorder approximately 150 years ago. Yet, researchers are still uncertain of its exact etiology and underlying pathophysiology.1,2
Ménière’s disease is defined as a chronic condition with recurrent episodes of vertigo that are associated with sensorineural hearing loss, tinnitus, and/or a sensation of aural fullness.3,4 Thanks to researchers’ evolving knowledge of Ménière’s disease, a new definition has been proposed: a degenerating inner ear leading to impaired homoeostasis, hearing loss, and vertigo.5
In the United States, the prevalence of Ménière’s disease is estimated at 15 to 150 cases per 100,000 persons. (This wide variation in prevalence reflects a lack of standard diagnostic criteria, as well as differences based on geographic area.6,7) Many affected individuals experience symptoms significant enough to lead to disability.6,7 Patients with Ménière’s disease usually present between ages 20 and 60, with a peak incidence occurring between ages 40 and 50.1,4,6,8 This disease affects both genders, but is slightly more common in women.1,4,6,8
Diagnosis of Ménière’s disease is based on recognition of the clinical symptoms that characterize the disorder, and management is centered on heuristic treatment options. Thus, a person may experience mild to severe symptoms of Ménière’s disease for months to years before receiving either the diagnosis or first-line treatment. This article reviews the current understanding of the underlying physiologic mechanisms that cause Ménière’s disease and discusses the criteria for diagnosis and various treatment options.
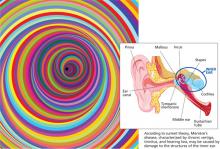
ETIOLOGY AND PATHOPHYSIOLOGY
The cause of Ménière’s disease and the subsequent mechanical, physiologic, and biochemical changes that occur are poorly understood, but several theories have been proposed. According to the current central theory, a buildup of fluid (endolymph) within the cochlear and saccular ducts in the inner ear causes distention of these structures into the endolymphatic space, resulting in the development of endolymphatic hydrops.4 Pressure from endolymphatic hydrops may cause damage to hair follicles and to the vestibular epithelium, resulting in symptoms of vertigo, tinnitus, and hearing loss.1,4 Researchers previously attributed the symptoms of Ménière’s disease completely to hydrops and focused on identifying anatomic abnormalities.7,9 However, studies now suggest that a range of pathophysiologic processes resulting from intrinsic and/or extrinsic factors may be responsible.7,9 While hydrops may develop, it is not always the definitive or only cause of Meniere’s disease symptoms.9
Recently recognized factors that contribute to the development of Meniere’s disease include autoimmune reactions, genetic irregularities, vascular abnormalities, and viral influences. Approximately one-third of Ménière’s disease cases can be attributed to an autoimmune origin.1,6 Researchers hypothesize that several immunologic processes may contribute to Ménière’s disease:
• Antibodies may cause inner ear damage,
• Injury to the inner ear may result in the release of cytokines which provoke immune reactions, and
• Certain genes may affect a person’s immune system and increase the probability of Ménière’s disease.1
The probability of a genetic influence is supported by the fact that one in 20 people with Ménière’s disease reports a positive family history of the disorder.4
Many patients with Ménière’s disease experience migraine headaches, and thus vascular abnormalities are another area of consideration among the etiologies of this disease.10 Researchers are also studying a potential viral cause in the development of Ménière’s disease.1,6
Regardless of the specific cause or physiologic changes that occur, the one common finding in patients with Ménière’s disease is a dysfunction of fluid homeostasis within the inner ear.
On the next page: Diagnosis >>
DIAGNOSIS
Establishing the diagnosis of Ménière’s disease can be difficult and time-consuming because the symptoms of the disorder are nonspecific and variable. Ménière’s disease is a clinical diagnosis, and thus the clinician must conduct a thorough physical exam and elicit a very specific history, including a detailed description of vertigo incidents and associated symptoms. Often, the greatest challenge is encouraging patients to articulate the details of their episodes. Patients may not keep a record of the variations of episodes, nor do they always know what information is needed. Thus, the provider needs to elicit specific information by asking questions regarding frequency and duration of episodes, as well as fluctuation of hearing loss, nausea, and tinnitus. Symptoms associated with vertigo during a Ménière’s episode may include nausea, vomiting, gait imbalance, and tinnitus. Most vertigo attacks from Ménière’s disease occur in clusters, but they may also occur sporadically.6
An additional challenge for clinicians is that other potential diagnoses related to vertigo must be excluded before the diagnosis of Ménière’s disease can be made. Also, it is important to note that specialists may differentiate Ménière’s disease, an idiopathic condition, from Ménière’s syndrome, which results from known causes of damage to the inner ear. In the literature, however, this distinction in terminology is not always clear.7
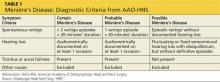
Specific diagnostic criteria for Ménière’s disease, defined in 1995 by the American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS), remain the gold standard for diagnosis.3 A “definite” diagnosis of Ménière’s disease is based on:
• A history of two or more episodes of spontaneous vertigo lasting 20 minutes or longer,
• Hearing loss documented by audiometry at least once,
• Presence of tinnitus, and/or
• A sensation of aural fullness.2,6,7
The AAO-HNS diagnostic criteria also define categories of “probable” and “possible” Ménière’s disease based on the frequency of vertigo episodes or the presence of a combination of associated symptoms (see Table 1).3,7
Patients with Ménière’s disease may experience different patterns of symptoms. “Auditory dominant” Ménière’s disease produces more hearing loss changes than vertigo, while “vestibular dominant” causes frequent episodes of severe vertigo and less severe hearing changes. A “mixed” pattern of Ménière’s disease manifests with both hearing fluctuations and vertigo.5
Unilateral symptoms are most common; however, bilateral disorder occurs in approximately 25% of patients, either at onset or with changing symptomatology over time.5,8,9
On the next page: History and examination >>
HISTORY AND EXAMINATION
Obtaining a detailed history from the patient and completing thorough neurologic and otologic examinations are essential components of the diagnostic process. Audiometry should be completed to evaluate neurosensory hearing loss, as audiometrically documented hearing loss is part of the AAO-HSN diagnostic criteria for Ménière’s disease.6
Based on findings from the patient’s history, physical exam, and audiometric testing, a tentative diagnosis can be made. The role and inclusion of adjunctive tests in the diagnostic process varies considerably by region in the US. While not required for the diagnosis of Ménière’s disease, electrical vestibular stimulation and videonystagmography are useful tests to assess abnormalities in vestibular function and monitor disease progression, which may help determine intervention options.6 Additional diagnostic tests may be suggested due to the essential need to exclude other potential causes of vertigo prior to determining the final diagnosis of Ménière’s disease.
Triggers of Vertigo
Selected triggers of vertigo that must be considered are benign paroxysmal positional vertigo (BPPV), labyrinthitis, acoustic neuroma, migraine with vertigo, and cerebral vascular events.6 Diagnostic tests are indicated to rule out certain problems, such as MRI to exclude a tumor or an acoustic neuroma. Distinct differences noted during a complete assessment may help eliminate certain disorders. BPPV is triggered by a change in physical position and usually lasts less than one minute; the diagnosis can be confirmed by the Dix-Hallpike maneuver.4 Labyrinthitis is characterized by acute vertigo associated with continuing imbalance, while instability with walking resolves completely between vertigo episodes in Ménière’s disease.4 If abnormal neurologic manifestations are noted during the exam or reported in a patient’s account of a vertigo episode, then a transient ischemic attack or stroke must be ruled out by more detailed diagnostic testing.
TREATMENT OPTIONS
Presently, no evidence-based guidelines exist for the treatment of Ménière’s disease, and the evidence supporting the efficacy of currently used therapies is inconsistent. However, several medicines and treatments are useful in relieving symptoms and improving a patient’s quality of life.
Primary care clinicians can initiate treatment for Ménière’s disease through lifestyle recommendations and prescription of specific medications. Everyday adjustments that incorporate dietary changes, stress reduction, adequate sleep, and regular exercise have been shown to improve vertigo symptoms in 60% of patients with Ménière’s disease.5,9
On the next page: Lifestyle changes >>
Lifestyle Changes
Dietary changes. Patients diagnosed with Ménière’s disease may benefit from following a low-sodium diet, limiting their daily sodium intake to between 1,000 and 2,000 mg.2,7,11 A low-sodium diet is believed to have a positive impact on inner ear fluid homeostasis by decreasing fluid retention and reducing the endolymphatic hydrops.2,7,11 Decreasing alcohol and caffeine consumption is also routinely recommended as part of the treatment of Ménière’s disease.2,5
Researchers have recently suggested a different approach to dietary changes for Ménière’s disease that reflects the underlying loss of ability to regulate fluid in the inner ear. This alternate method of dietary regulation aims to maintain fluid homeostasis by avoiding variations in the daily intake of sodium, caffeine, or alcohol, rather than limiting daily consumption.5
The goal of any proposed dietary changes is to limit fluid and electrolyte shifts that could disrupt the delicate fluid balance in the inner ear.9 When caring for patients with Ménière’s disease, clinicians need to keep in mind that dietary changes may be difficult and will probably require ongoing encouragement.
Stress reduction. Stress is associated with the occurrence of Ménière’s disease and often is the trigger for an acute episode of symptom exacerbation.5 Thus, clinicians should encourage stress management as a way to reduce the impact of Ménière’s disease on a patient’s life. Stress reduction techniques that can be recommended include progressive relaxation, meditation with deep breathing, yoga, and exercise.
Although studies of the effect of stress reduction methods on Ménière’s disease are not available in the current literature, the association of stress with Ménière’s disease is well documented.5 By avoiding stress, it is hoped, patients may experience a reduction in the frequency and severity of Ménière’s disease–associated episodes of vertigo. Researchers also suggest that stress reduction and patient education may help alleviate patients’ feelings of frustration resulting from misinformation about their condition.2,11
Oral Medications for Acute Relief
Acute attacks of vertigo associated with Ménière’s disease can be treated with benzodiazepines, antiemetics, or anticholinergic medications.4,6 Alleviation of symptoms is achieved through different physiologic pathways, based on the drug category prescribed. If a patient reports typical symptoms of Ménière’s disease but has not undergone audiometry, the plausible diagnosis may lead to tentative treatment for acute episodes if other causes of vertigo have been ruled out.
Antihistamines, such as meclizine or dimenhydrinate, may help reduce vertigo symptoms and associated nausea by blocking the effects of histamine.4,6 One of the most common side effects of antihistamines is drowsiness, so patients must be cautioned to avoid certain activities while taking this medication. Antihistamines should not be given to patients with glaucoma or prostate disease due to the potentially strong anticholinergic effects of these drugs.4,6
Scopolamineis a belladonna alkaloid that can be applied topically on the tissue just behind the ear to help reduce nausea and vomiting related to vertigo.11
Another option for treatment of acute vertigo is a benzodiazepine, such as alprazolam, to suppress active cerebellar responses; this agent may also reduce anxiety associated with an acute episode of vertigo.6,11 Benzodiazepines should be started at the lowest dose and increased as needed to the maximum recommended for individual medications based on symptom relief and side effects.6 Although caution needs to be used when prescribing benzodiazepines, studies show that they can be effective for persons with Meniere’s disease.11
Other antiemetic medications, such as promethazine or ondansetron, may be needed to treat severe nausea, but these agents should be used cautiously with other medications due a potential side effect of sedation.
Long-Term Oral Medication
Medication for long-term management of Ménière’s disease can promote improvement in symptoms and reduce the frequency of vertigo episodes. A mild diuretic, such as hydrochlorothiazide with or without triamterene, taken on a regular basis reduces extracellular fluids and may decrease pressure from endolymphatic hydrops.2,7 While strong evidence regarding the efficacy of diuretics is lacking, the majority of patients with Ménière’s disease who are treated with diuretics do experience improvement in vertigo.2,5
Betahistine hydrochloride, a vasodilator and histamine receptor antagonist, is another medication to consider for management of Ménière’s disease.1 This agent is not approved by the FDA; however, the FDA classifies betahistine as an inert chemical, so it is available in compounding pharmacies in the United States. The efficacy of betahistine has not been clearly or consistently established in research studies, but it has been and continues to be widely used to treat Ménière’s disease in Europe, with good results. Betahistine affects the microcirculation in the inner ear and inhibits the vestibular nuclei, which may reduce the frequency of vertigo episodes and improve tinnitus associated with Ménière’s disease.2,8,11
On the next page: Intratympanic medication >>
Intratympanic Medication
Patients who do not respond well to the previously described management should be referred to a specialist for additional treatment options. An otolaryngology specialist may administer intratympanic medications to patients with Ménière’s disease who have not responded to primary medical therapy.
Patients in the US who have not responded positively to lifestyle or diuretic medication are commonly offered treatment with intratympanic dexamethasone. The primary goal of this therapy is to improve vertigo without affecting a patient’s hearing; an added effect may be a potential positive impact on the immune system.11 Studies show that intratympanic steroid injection results in control of vertigo in patients with Ménière’s disease, but up to four injection treatments may be required for optimal effectiveness.2,7 Improvement of vertigo is achieved in more than 80% of patients who undergo intratympanic steroid injections.9
An option reserved for patients with severe, frequent vertigo related to Ménière’s disease is a type of chemical ablation of the labyrinth induced by injecting gentamicin into the middle ear.2 Gentamicin has a toxic effect on the vestibular hair cells in the inner ear, resulting in elimination of vestibular function.2 Intratympanic gentamicin is reported to reduce symptoms from Ménière’s disease, but this treatment is only recommended for patients with unilateral disease because it may induce permanent hearing loss.11
The primary care clinician needs to be aware of these intratympanic procedures and encourage patients to follow up with the specialist if additional treatments are indicated.
Portable Pressure Device
Use of the Meniett device is a minimally invasive treatment for Ménière’s disease based on the principle of using alternating pressure to stimulate the flow of endolymph.11 This handheld device delivers low-pressure pulses within the inner ear through a standard ventilation tube in order to increase exchange of fluids and improve homeostasis.8 The Meniett device should be used for five-minute intervals three times per day.12
Several studies have shown excellent results in patients who use the Meniett device routinely for several weeks.2,12 As noted, the use of this device, which is obtained by prescription from an otolaryngologist, requires placement of ventilation tubes.
Acupuncture
A traditional Chinese medical approach, acupuncture is one complementary and alternative medicine therapy that has been studied as a treatment option for Ménière’s disease. Studies on the use of acupuncture to treat vertigo demonstrate a beneficial effect for persons with this disease. While the optimal number and frequency of treatments has not been determined, all types of acupuncture studied showed benefit. Acupuncture has a positive effect in both acute episodes of vertigo in those without Ménière’s disease and in patients who have had Ménière’s disease for many years.13
Vestibular Rehabilitation
An additional adjunctive treatment option to consider for patients with residual disequilibrium is vestibular rehabilitation. Vestibular rehabilitation is designed to desensitize or retrain the balance system response through a series of exercises and activities supervised by a physical or occupational therapist. This rehabilitation may improve balance in patients with Ménière’s disease who have undergone medical or surgical intervention used to treat vertigo. Patients who have significant balance problems occurring between acute vertigo episodes may also benefit from vestibular rehabilitation.6
Surgical Treatment
Surgical intervention should be the last resort to treat Ménière’s disease due to the higher risk involved with any surgical procedure and the potential adverse effect on hearing. Endolymphatic sac decompression surgery involves removing a portion of the mastoid bone, resulting in decompression of the sac adjacent to the sigmoid sinus. This procedure has been used for more than 40 years to control vertigo and has the advantage of preserving hearing.7,9 However, the benefit of this procedure is now somewhat controversial and possibly related to a placebo effect.6 Researchers also report positive results with the use of tenotomy surgery, which involves severing tendons to the stapedius and tensor tympani muscles in the middle ear.14
No surgical procedure should be considered without the recommendation of an otolaryngology specialist. The decision should be made based on the severity of the disease and its effect on the patient, weighed against the risks involved in such an invasive treatment option.
On the next page: Conclusion >>
CONCLUSION
Ménière’s disease is a complex disorder that can significantly alter a person’s quality of life. While neither the exact cause nor pathophysiology underlying Ménière’s disease is well understood, several solid theories are being investigated and contribute to the current understanding of treatment options. Primary care clinicians can help determine this clinical diagnosis based on a detailed history and comprehensive assessment of recurrent vertigo with tinnitus, hearing loss, and possibly a sensation of aural fullness. Establishing the diagnosis of Ménière’s disease requires ruling out other possible causes of vertigo.
Lifestyle changes that improve the consistency of dietary intake of sodium, caffeine, and alcohol as well as reduction of stress are ongoing recommendations for patients with Ménière’s disease. Oral medications from a range of drug categories may be used to improve acute and chronic symptoms, including antiemetics, anticholinergics, antihistamines, benzodiazepines, and mild diuretics. Additionally, a compounded substance with vasodilator and histamine- receptor–antagonist properties (betahistine) can be used for treatment of Meniere’s.
Patients who do not respond well to conservative therapy should be referred to an otolaryngologist for possible intratympanic medications, ventilation tube placement with a prescription for pulse pressure therapy (ie, Meniett device), or surgical intervention. Primary care clinicians can initiate treatment for Ménière’s disease by recommending lifestyle changes, prescribing oral medications, providing patient education, and recognizing indications for referral.
1. Greco A, Gallo A, Fusconi M, et al. Ménière’s disease might be an autoimmune condition? Autoimmun Rev. 2012;11:731-738.
2. Greenberg SL, Nedzelski JM. Medical and noninvasive therapy for Ménière’s disease. Otolaryngol Clin North Am. 2010;43:1081-1090.
3. American Academy of Otolaryngology–Head and Neck Foundation, Inc. Committee on Hearing and Equilibrium guidelines for the diagnosis and evaluation of therapy in Ménière’s disease. Otolaryngol Head Neck Surg. 1995;113:181-185.
4. Syed I, Aldren C. Ménière’s disease: an evidence based approach to assessment and management. Int J Clin Pract. 2012;66:166-170.
5. Rauch SD. Clinical hints and precipitating factors in patients suffering from Ménière’s disease. Otolaryngol Clin North Am. 2010;43:1011-1017.
6. Dinces EA, Rauch SS. Ménière’s disease. In: UpToDate. Deschler DG, Lin FH, eds. 2012:November 27,2012.
7. Semaan MT, Megerian CA. Ménière’s disease: a challenging and relentless disorder. Otolaryngol Clin North Am. 2011;44:383-403.
8. Martin González C, González FM, Trinidad A, et al. Medical management of Ménière’s disease: a 10-year case series and review of literature. Eur Arch Otorhinolaryngol. 2010;267:1371-1376.
9. Berlinger NT. Ménière’s disease: new concepts, new treatments. Minn Med. 2011;94:33-36.
10. von Brevern M, Neuhauser H. Epidemiological evidence for a link between vertigo and migraine. J Vestib Res. 2011;21:299-304.
11. Coelho DH, Lalwani AK. Medical management of Ménière’s disease. Laryngoscope. 2008;118:1099-1108.
12. Gates GA, Green JD Jr, Tucci DL, Telian SA. The effects of transtympanic micropressure treatment in people with unilateral Ménière’s disease. Arch Otolaryngol Head Neck Surg. 2004;130:718-725.
13. Long A, Xing M, Morgan K, Brettle A. Exploring the evidence base for acupuncture in the treatment of Ménière’s syndrome-a systematic review. Evid Based Complement Alternat Med. 2011;2011:1-13.
14. Loader B, Beicht D, Hamzavi JS, Franz P. Tenotomy of the middle ear muscles causes a dramatic reduction in vertigo attacks and improves audiological function in definite Ménière’s disease. Acta Otolaryngol. 2012;132:491-497.
CE/CME No: CR-1310
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Describe the pathophysiology of Ménière’s disease, as it is currently understood.
• Discuss the triad of symptoms that should prompt suspicion for Ménière’s disease in a primary care patient.
• List the diagnostic criteria for “definite” Ménière’s disease, as defined by the American Academy of Otolaryngology–Head and Neck Surgery.
• Review pharmacologic management, intratympanic injection and other nonoperative therapies, and surgical treatment for Ménière’s disease.
FACULTY
Tamera Pearson is an Associate Professor in the School of Nursing at Western Carolina University.
The author has no significant financial relationships to disclose.
ACCREDITATION STATEMENT
Article begins on next page >>
Ménière’s disease is a complex disorder of intermittent vertigo, tinnitus, and hearing loss whose symptoms usually manifest between ages 20 and 60. Although this disorder is uncommon, its impact on a person’s quality of life can be significant. Here are the symptoms, criteria for diagnosis, and appropriate treatment or referrals for Ménière’s disease.
Ménière’s disease can significantly affect a person’s quality of life and is a challenge to diagnose and treat effectively. The French physician Prosper Ménière first described this disorder approximately 150 years ago. Yet, researchers are still uncertain of its exact etiology and underlying pathophysiology.1,2
Ménière’s disease is defined as a chronic condition with recurrent episodes of vertigo that are associated with sensorineural hearing loss, tinnitus, and/or a sensation of aural fullness.3,4 Thanks to researchers’ evolving knowledge of Ménière’s disease, a new definition has been proposed: a degenerating inner ear leading to impaired homoeostasis, hearing loss, and vertigo.5
In the United States, the prevalence of Ménière’s disease is estimated at 15 to 150 cases per 100,000 persons. (This wide variation in prevalence reflects a lack of standard diagnostic criteria, as well as differences based on geographic area.6,7) Many affected individuals experience symptoms significant enough to lead to disability.6,7 Patients with Ménière’s disease usually present between ages 20 and 60, with a peak incidence occurring between ages 40 and 50.1,4,6,8 This disease affects both genders, but is slightly more common in women.1,4,6,8
Diagnosis of Ménière’s disease is based on recognition of the clinical symptoms that characterize the disorder, and management is centered on heuristic treatment options. Thus, a person may experience mild to severe symptoms of Ménière’s disease for months to years before receiving either the diagnosis or first-line treatment. This article reviews the current understanding of the underlying physiologic mechanisms that cause Ménière’s disease and discusses the criteria for diagnosis and various treatment options.
ETIOLOGY AND PATHOPHYSIOLOGY
The cause of Ménière’s disease and the subsequent mechanical, physiologic, and biochemical changes that occur are poorly understood, but several theories have been proposed. According to the current central theory, a buildup of fluid (endolymph) within the cochlear and saccular ducts in the inner ear causes distention of these structures into the endolymphatic space, resulting in the development of endolymphatic hydrops.4 Pressure from endolymphatic hydrops may cause damage to hair follicles and to the vestibular epithelium, resulting in symptoms of vertigo, tinnitus, and hearing loss.1,4 Researchers previously attributed the symptoms of Ménière’s disease completely to hydrops and focused on identifying anatomic abnormalities.7,9 However, studies now suggest that a range of pathophysiologic processes resulting from intrinsic and/or extrinsic factors may be responsible.7,9 While hydrops may develop, it is not always the definitive or only cause of Meniere’s disease symptoms.9
Recently recognized factors that contribute to the development of Meniere’s disease include autoimmune reactions, genetic irregularities, vascular abnormalities, and viral influences. Approximately one-third of Ménière’s disease cases can be attributed to an autoimmune origin.1,6 Researchers hypothesize that several immunologic processes may contribute to Ménière’s disease:
• Antibodies may cause inner ear damage,
• Injury to the inner ear may result in the release of cytokines which provoke immune reactions, and
• Certain genes may affect a person’s immune system and increase the probability of Ménière’s disease.1
The probability of a genetic influence is supported by the fact that one in 20 people with Ménière’s disease reports a positive family history of the disorder.4
Many patients with Ménière’s disease experience migraine headaches, and thus vascular abnormalities are another area of consideration among the etiologies of this disease.10 Researchers are also studying a potential viral cause in the development of Ménière’s disease.1,6
Regardless of the specific cause or physiologic changes that occur, the one common finding in patients with Ménière’s disease is a dysfunction of fluid homeostasis within the inner ear.
On the next page: Diagnosis >>
DIAGNOSIS
Establishing the diagnosis of Ménière’s disease can be difficult and time-consuming because the symptoms of the disorder are nonspecific and variable. Ménière’s disease is a clinical diagnosis, and thus the clinician must conduct a thorough physical exam and elicit a very specific history, including a detailed description of vertigo incidents and associated symptoms. Often, the greatest challenge is encouraging patients to articulate the details of their episodes. Patients may not keep a record of the variations of episodes, nor do they always know what information is needed. Thus, the provider needs to elicit specific information by asking questions regarding frequency and duration of episodes, as well as fluctuation of hearing loss, nausea, and tinnitus. Symptoms associated with vertigo during a Ménière’s episode may include nausea, vomiting, gait imbalance, and tinnitus. Most vertigo attacks from Ménière’s disease occur in clusters, but they may also occur sporadically.6
An additional challenge for clinicians is that other potential diagnoses related to vertigo must be excluded before the diagnosis of Ménière’s disease can be made. Also, it is important to note that specialists may differentiate Ménière’s disease, an idiopathic condition, from Ménière’s syndrome, which results from known causes of damage to the inner ear. In the literature, however, this distinction in terminology is not always clear.7
Specific diagnostic criteria for Ménière’s disease, defined in 1995 by the American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS), remain the gold standard for diagnosis.3 A “definite” diagnosis of Ménière’s disease is based on:
• A history of two or more episodes of spontaneous vertigo lasting 20 minutes or longer,
• Hearing loss documented by audiometry at least once,
• Presence of tinnitus, and/or
• A sensation of aural fullness.2,6,7
The AAO-HNS diagnostic criteria also define categories of “probable” and “possible” Ménière’s disease based on the frequency of vertigo episodes or the presence of a combination of associated symptoms (see Table 1).3,7
Patients with Ménière’s disease may experience different patterns of symptoms. “Auditory dominant” Ménière’s disease produces more hearing loss changes than vertigo, while “vestibular dominant” causes frequent episodes of severe vertigo and less severe hearing changes. A “mixed” pattern of Ménière’s disease manifests with both hearing fluctuations and vertigo.5
Unilateral symptoms are most common; however, bilateral disorder occurs in approximately 25% of patients, either at onset or with changing symptomatology over time.5,8,9
On the next page: History and examination >>
HISTORY AND EXAMINATION
Obtaining a detailed history from the patient and completing thorough neurologic and otologic examinations are essential components of the diagnostic process. Audiometry should be completed to evaluate neurosensory hearing loss, as audiometrically documented hearing loss is part of the AAO-HSN diagnostic criteria for Ménière’s disease.6
Based on findings from the patient’s history, physical exam, and audiometric testing, a tentative diagnosis can be made. The role and inclusion of adjunctive tests in the diagnostic process varies considerably by region in the US. While not required for the diagnosis of Ménière’s disease, electrical vestibular stimulation and videonystagmography are useful tests to assess abnormalities in vestibular function and monitor disease progression, which may help determine intervention options.6 Additional diagnostic tests may be suggested due to the essential need to exclude other potential causes of vertigo prior to determining the final diagnosis of Ménière’s disease.
Triggers of Vertigo
Selected triggers of vertigo that must be considered are benign paroxysmal positional vertigo (BPPV), labyrinthitis, acoustic neuroma, migraine with vertigo, and cerebral vascular events.6 Diagnostic tests are indicated to rule out certain problems, such as MRI to exclude a tumor or an acoustic neuroma. Distinct differences noted during a complete assessment may help eliminate certain disorders. BPPV is triggered by a change in physical position and usually lasts less than one minute; the diagnosis can be confirmed by the Dix-Hallpike maneuver.4 Labyrinthitis is characterized by acute vertigo associated with continuing imbalance, while instability with walking resolves completely between vertigo episodes in Ménière’s disease.4 If abnormal neurologic manifestations are noted during the exam or reported in a patient’s account of a vertigo episode, then a transient ischemic attack or stroke must be ruled out by more detailed diagnostic testing.
TREATMENT OPTIONS
Presently, no evidence-based guidelines exist for the treatment of Ménière’s disease, and the evidence supporting the efficacy of currently used therapies is inconsistent. However, several medicines and treatments are useful in relieving symptoms and improving a patient’s quality of life.
Primary care clinicians can initiate treatment for Ménière’s disease through lifestyle recommendations and prescription of specific medications. Everyday adjustments that incorporate dietary changes, stress reduction, adequate sleep, and regular exercise have been shown to improve vertigo symptoms in 60% of patients with Ménière’s disease.5,9
On the next page: Lifestyle changes >>
Lifestyle Changes
Dietary changes. Patients diagnosed with Ménière’s disease may benefit from following a low-sodium diet, limiting their daily sodium intake to between 1,000 and 2,000 mg.2,7,11 A low-sodium diet is believed to have a positive impact on inner ear fluid homeostasis by decreasing fluid retention and reducing the endolymphatic hydrops.2,7,11 Decreasing alcohol and caffeine consumption is also routinely recommended as part of the treatment of Ménière’s disease.2,5
Researchers have recently suggested a different approach to dietary changes for Ménière’s disease that reflects the underlying loss of ability to regulate fluid in the inner ear. This alternate method of dietary regulation aims to maintain fluid homeostasis by avoiding variations in the daily intake of sodium, caffeine, or alcohol, rather than limiting daily consumption.5
The goal of any proposed dietary changes is to limit fluid and electrolyte shifts that could disrupt the delicate fluid balance in the inner ear.9 When caring for patients with Ménière’s disease, clinicians need to keep in mind that dietary changes may be difficult and will probably require ongoing encouragement.
Stress reduction. Stress is associated with the occurrence of Ménière’s disease and often is the trigger for an acute episode of symptom exacerbation.5 Thus, clinicians should encourage stress management as a way to reduce the impact of Ménière’s disease on a patient’s life. Stress reduction techniques that can be recommended include progressive relaxation, meditation with deep breathing, yoga, and exercise.
Although studies of the effect of stress reduction methods on Ménière’s disease are not available in the current literature, the association of stress with Ménière’s disease is well documented.5 By avoiding stress, it is hoped, patients may experience a reduction in the frequency and severity of Ménière’s disease–associated episodes of vertigo. Researchers also suggest that stress reduction and patient education may help alleviate patients’ feelings of frustration resulting from misinformation about their condition.2,11
Oral Medications for Acute Relief
Acute attacks of vertigo associated with Ménière’s disease can be treated with benzodiazepines, antiemetics, or anticholinergic medications.4,6 Alleviation of symptoms is achieved through different physiologic pathways, based on the drug category prescribed. If a patient reports typical symptoms of Ménière’s disease but has not undergone audiometry, the plausible diagnosis may lead to tentative treatment for acute episodes if other causes of vertigo have been ruled out.
Antihistamines, such as meclizine or dimenhydrinate, may help reduce vertigo symptoms and associated nausea by blocking the effects of histamine.4,6 One of the most common side effects of antihistamines is drowsiness, so patients must be cautioned to avoid certain activities while taking this medication. Antihistamines should not be given to patients with glaucoma or prostate disease due to the potentially strong anticholinergic effects of these drugs.4,6
Scopolamineis a belladonna alkaloid that can be applied topically on the tissue just behind the ear to help reduce nausea and vomiting related to vertigo.11
Another option for treatment of acute vertigo is a benzodiazepine, such as alprazolam, to suppress active cerebellar responses; this agent may also reduce anxiety associated with an acute episode of vertigo.6,11 Benzodiazepines should be started at the lowest dose and increased as needed to the maximum recommended for individual medications based on symptom relief and side effects.6 Although caution needs to be used when prescribing benzodiazepines, studies show that they can be effective for persons with Meniere’s disease.11
Other antiemetic medications, such as promethazine or ondansetron, may be needed to treat severe nausea, but these agents should be used cautiously with other medications due a potential side effect of sedation.
Long-Term Oral Medication
Medication for long-term management of Ménière’s disease can promote improvement in symptoms and reduce the frequency of vertigo episodes. A mild diuretic, such as hydrochlorothiazide with or without triamterene, taken on a regular basis reduces extracellular fluids and may decrease pressure from endolymphatic hydrops.2,7 While strong evidence regarding the efficacy of diuretics is lacking, the majority of patients with Ménière’s disease who are treated with diuretics do experience improvement in vertigo.2,5
Betahistine hydrochloride, a vasodilator and histamine receptor antagonist, is another medication to consider for management of Ménière’s disease.1 This agent is not approved by the FDA; however, the FDA classifies betahistine as an inert chemical, so it is available in compounding pharmacies in the United States. The efficacy of betahistine has not been clearly or consistently established in research studies, but it has been and continues to be widely used to treat Ménière’s disease in Europe, with good results. Betahistine affects the microcirculation in the inner ear and inhibits the vestibular nuclei, which may reduce the frequency of vertigo episodes and improve tinnitus associated with Ménière’s disease.2,8,11
On the next page: Intratympanic medication >>
Intratympanic Medication
Patients who do not respond well to the previously described management should be referred to a specialist for additional treatment options. An otolaryngology specialist may administer intratympanic medications to patients with Ménière’s disease who have not responded to primary medical therapy.
Patients in the US who have not responded positively to lifestyle or diuretic medication are commonly offered treatment with intratympanic dexamethasone. The primary goal of this therapy is to improve vertigo without affecting a patient’s hearing; an added effect may be a potential positive impact on the immune system.11 Studies show that intratympanic steroid injection results in control of vertigo in patients with Ménière’s disease, but up to four injection treatments may be required for optimal effectiveness.2,7 Improvement of vertigo is achieved in more than 80% of patients who undergo intratympanic steroid injections.9
An option reserved for patients with severe, frequent vertigo related to Ménière’s disease is a type of chemical ablation of the labyrinth induced by injecting gentamicin into the middle ear.2 Gentamicin has a toxic effect on the vestibular hair cells in the inner ear, resulting in elimination of vestibular function.2 Intratympanic gentamicin is reported to reduce symptoms from Ménière’s disease, but this treatment is only recommended for patients with unilateral disease because it may induce permanent hearing loss.11
The primary care clinician needs to be aware of these intratympanic procedures and encourage patients to follow up with the specialist if additional treatments are indicated.
Portable Pressure Device
Use of the Meniett device is a minimally invasive treatment for Ménière’s disease based on the principle of using alternating pressure to stimulate the flow of endolymph.11 This handheld device delivers low-pressure pulses within the inner ear through a standard ventilation tube in order to increase exchange of fluids and improve homeostasis.8 The Meniett device should be used for five-minute intervals three times per day.12
Several studies have shown excellent results in patients who use the Meniett device routinely for several weeks.2,12 As noted, the use of this device, which is obtained by prescription from an otolaryngologist, requires placement of ventilation tubes.
Acupuncture
A traditional Chinese medical approach, acupuncture is one complementary and alternative medicine therapy that has been studied as a treatment option for Ménière’s disease. Studies on the use of acupuncture to treat vertigo demonstrate a beneficial effect for persons with this disease. While the optimal number and frequency of treatments has not been determined, all types of acupuncture studied showed benefit. Acupuncture has a positive effect in both acute episodes of vertigo in those without Ménière’s disease and in patients who have had Ménière’s disease for many years.13
Vestibular Rehabilitation
An additional adjunctive treatment option to consider for patients with residual disequilibrium is vestibular rehabilitation. Vestibular rehabilitation is designed to desensitize or retrain the balance system response through a series of exercises and activities supervised by a physical or occupational therapist. This rehabilitation may improve balance in patients with Ménière’s disease who have undergone medical or surgical intervention used to treat vertigo. Patients who have significant balance problems occurring between acute vertigo episodes may also benefit from vestibular rehabilitation.6
Surgical Treatment
Surgical intervention should be the last resort to treat Ménière’s disease due to the higher risk involved with any surgical procedure and the potential adverse effect on hearing. Endolymphatic sac decompression surgery involves removing a portion of the mastoid bone, resulting in decompression of the sac adjacent to the sigmoid sinus. This procedure has been used for more than 40 years to control vertigo and has the advantage of preserving hearing.7,9 However, the benefit of this procedure is now somewhat controversial and possibly related to a placebo effect.6 Researchers also report positive results with the use of tenotomy surgery, which involves severing tendons to the stapedius and tensor tympani muscles in the middle ear.14
No surgical procedure should be considered without the recommendation of an otolaryngology specialist. The decision should be made based on the severity of the disease and its effect on the patient, weighed against the risks involved in such an invasive treatment option.
On the next page: Conclusion >>
CONCLUSION
Ménière’s disease is a complex disorder that can significantly alter a person’s quality of life. While neither the exact cause nor pathophysiology underlying Ménière’s disease is well understood, several solid theories are being investigated and contribute to the current understanding of treatment options. Primary care clinicians can help determine this clinical diagnosis based on a detailed history and comprehensive assessment of recurrent vertigo with tinnitus, hearing loss, and possibly a sensation of aural fullness. Establishing the diagnosis of Ménière’s disease requires ruling out other possible causes of vertigo.
Lifestyle changes that improve the consistency of dietary intake of sodium, caffeine, and alcohol as well as reduction of stress are ongoing recommendations for patients with Ménière’s disease. Oral medications from a range of drug categories may be used to improve acute and chronic symptoms, including antiemetics, anticholinergics, antihistamines, benzodiazepines, and mild diuretics. Additionally, a compounded substance with vasodilator and histamine- receptor–antagonist properties (betahistine) can be used for treatment of Meniere’s.
Patients who do not respond well to conservative therapy should be referred to an otolaryngologist for possible intratympanic medications, ventilation tube placement with a prescription for pulse pressure therapy (ie, Meniett device), or surgical intervention. Primary care clinicians can initiate treatment for Ménière’s disease by recommending lifestyle changes, prescribing oral medications, providing patient education, and recognizing indications for referral.
CE/CME No: CR-1310
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Describe the pathophysiology of Ménière’s disease, as it is currently understood.
• Discuss the triad of symptoms that should prompt suspicion for Ménière’s disease in a primary care patient.
• List the diagnostic criteria for “definite” Ménière’s disease, as defined by the American Academy of Otolaryngology–Head and Neck Surgery.
• Review pharmacologic management, intratympanic injection and other nonoperative therapies, and surgical treatment for Ménière’s disease.
FACULTY
Tamera Pearson is an Associate Professor in the School of Nursing at Western Carolina University.
The author has no significant financial relationships to disclose.
ACCREDITATION STATEMENT
Article begins on next page >>
Ménière’s disease is a complex disorder of intermittent vertigo, tinnitus, and hearing loss whose symptoms usually manifest between ages 20 and 60. Although this disorder is uncommon, its impact on a person’s quality of life can be significant. Here are the symptoms, criteria for diagnosis, and appropriate treatment or referrals for Ménière’s disease.
Ménière’s disease can significantly affect a person’s quality of life and is a challenge to diagnose and treat effectively. The French physician Prosper Ménière first described this disorder approximately 150 years ago. Yet, researchers are still uncertain of its exact etiology and underlying pathophysiology.1,2
Ménière’s disease is defined as a chronic condition with recurrent episodes of vertigo that are associated with sensorineural hearing loss, tinnitus, and/or a sensation of aural fullness.3,4 Thanks to researchers’ evolving knowledge of Ménière’s disease, a new definition has been proposed: a degenerating inner ear leading to impaired homoeostasis, hearing loss, and vertigo.5
In the United States, the prevalence of Ménière’s disease is estimated at 15 to 150 cases per 100,000 persons. (This wide variation in prevalence reflects a lack of standard diagnostic criteria, as well as differences based on geographic area.6,7) Many affected individuals experience symptoms significant enough to lead to disability.6,7 Patients with Ménière’s disease usually present between ages 20 and 60, with a peak incidence occurring between ages 40 and 50.1,4,6,8 This disease affects both genders, but is slightly more common in women.1,4,6,8
Diagnosis of Ménière’s disease is based on recognition of the clinical symptoms that characterize the disorder, and management is centered on heuristic treatment options. Thus, a person may experience mild to severe symptoms of Ménière’s disease for months to years before receiving either the diagnosis or first-line treatment. This article reviews the current understanding of the underlying physiologic mechanisms that cause Ménière’s disease and discusses the criteria for diagnosis and various treatment options.
ETIOLOGY AND PATHOPHYSIOLOGY
The cause of Ménière’s disease and the subsequent mechanical, physiologic, and biochemical changes that occur are poorly understood, but several theories have been proposed. According to the current central theory, a buildup of fluid (endolymph) within the cochlear and saccular ducts in the inner ear causes distention of these structures into the endolymphatic space, resulting in the development of endolymphatic hydrops.4 Pressure from endolymphatic hydrops may cause damage to hair follicles and to the vestibular epithelium, resulting in symptoms of vertigo, tinnitus, and hearing loss.1,4 Researchers previously attributed the symptoms of Ménière’s disease completely to hydrops and focused on identifying anatomic abnormalities.7,9 However, studies now suggest that a range of pathophysiologic processes resulting from intrinsic and/or extrinsic factors may be responsible.7,9 While hydrops may develop, it is not always the definitive or only cause of Meniere’s disease symptoms.9
Recently recognized factors that contribute to the development of Meniere’s disease include autoimmune reactions, genetic irregularities, vascular abnormalities, and viral influences. Approximately one-third of Ménière’s disease cases can be attributed to an autoimmune origin.1,6 Researchers hypothesize that several immunologic processes may contribute to Ménière’s disease:
• Antibodies may cause inner ear damage,
• Injury to the inner ear may result in the release of cytokines which provoke immune reactions, and
• Certain genes may affect a person’s immune system and increase the probability of Ménière’s disease.1
The probability of a genetic influence is supported by the fact that one in 20 people with Ménière’s disease reports a positive family history of the disorder.4
Many patients with Ménière’s disease experience migraine headaches, and thus vascular abnormalities are another area of consideration among the etiologies of this disease.10 Researchers are also studying a potential viral cause in the development of Ménière’s disease.1,6
Regardless of the specific cause or physiologic changes that occur, the one common finding in patients with Ménière’s disease is a dysfunction of fluid homeostasis within the inner ear.
On the next page: Diagnosis >>
DIAGNOSIS
Establishing the diagnosis of Ménière’s disease can be difficult and time-consuming because the symptoms of the disorder are nonspecific and variable. Ménière’s disease is a clinical diagnosis, and thus the clinician must conduct a thorough physical exam and elicit a very specific history, including a detailed description of vertigo incidents and associated symptoms. Often, the greatest challenge is encouraging patients to articulate the details of their episodes. Patients may not keep a record of the variations of episodes, nor do they always know what information is needed. Thus, the provider needs to elicit specific information by asking questions regarding frequency and duration of episodes, as well as fluctuation of hearing loss, nausea, and tinnitus. Symptoms associated with vertigo during a Ménière’s episode may include nausea, vomiting, gait imbalance, and tinnitus. Most vertigo attacks from Ménière’s disease occur in clusters, but they may also occur sporadically.6
An additional challenge for clinicians is that other potential diagnoses related to vertigo must be excluded before the diagnosis of Ménière’s disease can be made. Also, it is important to note that specialists may differentiate Ménière’s disease, an idiopathic condition, from Ménière’s syndrome, which results from known causes of damage to the inner ear. In the literature, however, this distinction in terminology is not always clear.7
Specific diagnostic criteria for Ménière’s disease, defined in 1995 by the American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS), remain the gold standard for diagnosis.3 A “definite” diagnosis of Ménière’s disease is based on:
• A history of two or more episodes of spontaneous vertigo lasting 20 minutes or longer,
• Hearing loss documented by audiometry at least once,
• Presence of tinnitus, and/or
• A sensation of aural fullness.2,6,7
The AAO-HNS diagnostic criteria also define categories of “probable” and “possible” Ménière’s disease based on the frequency of vertigo episodes or the presence of a combination of associated symptoms (see Table 1).3,7
Patients with Ménière’s disease may experience different patterns of symptoms. “Auditory dominant” Ménière’s disease produces more hearing loss changes than vertigo, while “vestibular dominant” causes frequent episodes of severe vertigo and less severe hearing changes. A “mixed” pattern of Ménière’s disease manifests with both hearing fluctuations and vertigo.5
Unilateral symptoms are most common; however, bilateral disorder occurs in approximately 25% of patients, either at onset or with changing symptomatology over time.5,8,9
On the next page: History and examination >>
HISTORY AND EXAMINATION
Obtaining a detailed history from the patient and completing thorough neurologic and otologic examinations are essential components of the diagnostic process. Audiometry should be completed to evaluate neurosensory hearing loss, as audiometrically documented hearing loss is part of the AAO-HSN diagnostic criteria for Ménière’s disease.6
Based on findings from the patient’s history, physical exam, and audiometric testing, a tentative diagnosis can be made. The role and inclusion of adjunctive tests in the diagnostic process varies considerably by region in the US. While not required for the diagnosis of Ménière’s disease, electrical vestibular stimulation and videonystagmography are useful tests to assess abnormalities in vestibular function and monitor disease progression, which may help determine intervention options.6 Additional diagnostic tests may be suggested due to the essential need to exclude other potential causes of vertigo prior to determining the final diagnosis of Ménière’s disease.
Triggers of Vertigo
Selected triggers of vertigo that must be considered are benign paroxysmal positional vertigo (BPPV), labyrinthitis, acoustic neuroma, migraine with vertigo, and cerebral vascular events.6 Diagnostic tests are indicated to rule out certain problems, such as MRI to exclude a tumor or an acoustic neuroma. Distinct differences noted during a complete assessment may help eliminate certain disorders. BPPV is triggered by a change in physical position and usually lasts less than one minute; the diagnosis can be confirmed by the Dix-Hallpike maneuver.4 Labyrinthitis is characterized by acute vertigo associated with continuing imbalance, while instability with walking resolves completely between vertigo episodes in Ménière’s disease.4 If abnormal neurologic manifestations are noted during the exam or reported in a patient’s account of a vertigo episode, then a transient ischemic attack or stroke must be ruled out by more detailed diagnostic testing.
TREATMENT OPTIONS
Presently, no evidence-based guidelines exist for the treatment of Ménière’s disease, and the evidence supporting the efficacy of currently used therapies is inconsistent. However, several medicines and treatments are useful in relieving symptoms and improving a patient’s quality of life.
Primary care clinicians can initiate treatment for Ménière’s disease through lifestyle recommendations and prescription of specific medications. Everyday adjustments that incorporate dietary changes, stress reduction, adequate sleep, and regular exercise have been shown to improve vertigo symptoms in 60% of patients with Ménière’s disease.5,9
On the next page: Lifestyle changes >>
Lifestyle Changes
Dietary changes. Patients diagnosed with Ménière’s disease may benefit from following a low-sodium diet, limiting their daily sodium intake to between 1,000 and 2,000 mg.2,7,11 A low-sodium diet is believed to have a positive impact on inner ear fluid homeostasis by decreasing fluid retention and reducing the endolymphatic hydrops.2,7,11 Decreasing alcohol and caffeine consumption is also routinely recommended as part of the treatment of Ménière’s disease.2,5
Researchers have recently suggested a different approach to dietary changes for Ménière’s disease that reflects the underlying loss of ability to regulate fluid in the inner ear. This alternate method of dietary regulation aims to maintain fluid homeostasis by avoiding variations in the daily intake of sodium, caffeine, or alcohol, rather than limiting daily consumption.5
The goal of any proposed dietary changes is to limit fluid and electrolyte shifts that could disrupt the delicate fluid balance in the inner ear.9 When caring for patients with Ménière’s disease, clinicians need to keep in mind that dietary changes may be difficult and will probably require ongoing encouragement.
Stress reduction. Stress is associated with the occurrence of Ménière’s disease and often is the trigger for an acute episode of symptom exacerbation.5 Thus, clinicians should encourage stress management as a way to reduce the impact of Ménière’s disease on a patient’s life. Stress reduction techniques that can be recommended include progressive relaxation, meditation with deep breathing, yoga, and exercise.
Although studies of the effect of stress reduction methods on Ménière’s disease are not available in the current literature, the association of stress with Ménière’s disease is well documented.5 By avoiding stress, it is hoped, patients may experience a reduction in the frequency and severity of Ménière’s disease–associated episodes of vertigo. Researchers also suggest that stress reduction and patient education may help alleviate patients’ feelings of frustration resulting from misinformation about their condition.2,11
Oral Medications for Acute Relief
Acute attacks of vertigo associated with Ménière’s disease can be treated with benzodiazepines, antiemetics, or anticholinergic medications.4,6 Alleviation of symptoms is achieved through different physiologic pathways, based on the drug category prescribed. If a patient reports typical symptoms of Ménière’s disease but has not undergone audiometry, the plausible diagnosis may lead to tentative treatment for acute episodes if other causes of vertigo have been ruled out.
Antihistamines, such as meclizine or dimenhydrinate, may help reduce vertigo symptoms and associated nausea by blocking the effects of histamine.4,6 One of the most common side effects of antihistamines is drowsiness, so patients must be cautioned to avoid certain activities while taking this medication. Antihistamines should not be given to patients with glaucoma or prostate disease due to the potentially strong anticholinergic effects of these drugs.4,6
Scopolamineis a belladonna alkaloid that can be applied topically on the tissue just behind the ear to help reduce nausea and vomiting related to vertigo.11
Another option for treatment of acute vertigo is a benzodiazepine, such as alprazolam, to suppress active cerebellar responses; this agent may also reduce anxiety associated with an acute episode of vertigo.6,11 Benzodiazepines should be started at the lowest dose and increased as needed to the maximum recommended for individual medications based on symptom relief and side effects.6 Although caution needs to be used when prescribing benzodiazepines, studies show that they can be effective for persons with Meniere’s disease.11
Other antiemetic medications, such as promethazine or ondansetron, may be needed to treat severe nausea, but these agents should be used cautiously with other medications due a potential side effect of sedation.
Long-Term Oral Medication
Medication for long-term management of Ménière’s disease can promote improvement in symptoms and reduce the frequency of vertigo episodes. A mild diuretic, such as hydrochlorothiazide with or without triamterene, taken on a regular basis reduces extracellular fluids and may decrease pressure from endolymphatic hydrops.2,7 While strong evidence regarding the efficacy of diuretics is lacking, the majority of patients with Ménière’s disease who are treated with diuretics do experience improvement in vertigo.2,5
Betahistine hydrochloride, a vasodilator and histamine receptor antagonist, is another medication to consider for management of Ménière’s disease.1 This agent is not approved by the FDA; however, the FDA classifies betahistine as an inert chemical, so it is available in compounding pharmacies in the United States. The efficacy of betahistine has not been clearly or consistently established in research studies, but it has been and continues to be widely used to treat Ménière’s disease in Europe, with good results. Betahistine affects the microcirculation in the inner ear and inhibits the vestibular nuclei, which may reduce the frequency of vertigo episodes and improve tinnitus associated with Ménière’s disease.2,8,11
On the next page: Intratympanic medication >>
Intratympanic Medication
Patients who do not respond well to the previously described management should be referred to a specialist for additional treatment options. An otolaryngology specialist may administer intratympanic medications to patients with Ménière’s disease who have not responded to primary medical therapy.
Patients in the US who have not responded positively to lifestyle or diuretic medication are commonly offered treatment with intratympanic dexamethasone. The primary goal of this therapy is to improve vertigo without affecting a patient’s hearing; an added effect may be a potential positive impact on the immune system.11 Studies show that intratympanic steroid injection results in control of vertigo in patients with Ménière’s disease, but up to four injection treatments may be required for optimal effectiveness.2,7 Improvement of vertigo is achieved in more than 80% of patients who undergo intratympanic steroid injections.9
An option reserved for patients with severe, frequent vertigo related to Ménière’s disease is a type of chemical ablation of the labyrinth induced by injecting gentamicin into the middle ear.2 Gentamicin has a toxic effect on the vestibular hair cells in the inner ear, resulting in elimination of vestibular function.2 Intratympanic gentamicin is reported to reduce symptoms from Ménière’s disease, but this treatment is only recommended for patients with unilateral disease because it may induce permanent hearing loss.11
The primary care clinician needs to be aware of these intratympanic procedures and encourage patients to follow up with the specialist if additional treatments are indicated.
Portable Pressure Device
Use of the Meniett device is a minimally invasive treatment for Ménière’s disease based on the principle of using alternating pressure to stimulate the flow of endolymph.11 This handheld device delivers low-pressure pulses within the inner ear through a standard ventilation tube in order to increase exchange of fluids and improve homeostasis.8 The Meniett device should be used for five-minute intervals three times per day.12
Several studies have shown excellent results in patients who use the Meniett device routinely for several weeks.2,12 As noted, the use of this device, which is obtained by prescription from an otolaryngologist, requires placement of ventilation tubes.
Acupuncture
A traditional Chinese medical approach, acupuncture is one complementary and alternative medicine therapy that has been studied as a treatment option for Ménière’s disease. Studies on the use of acupuncture to treat vertigo demonstrate a beneficial effect for persons with this disease. While the optimal number and frequency of treatments has not been determined, all types of acupuncture studied showed benefit. Acupuncture has a positive effect in both acute episodes of vertigo in those without Ménière’s disease and in patients who have had Ménière’s disease for many years.13
Vestibular Rehabilitation
An additional adjunctive treatment option to consider for patients with residual disequilibrium is vestibular rehabilitation. Vestibular rehabilitation is designed to desensitize or retrain the balance system response through a series of exercises and activities supervised by a physical or occupational therapist. This rehabilitation may improve balance in patients with Ménière’s disease who have undergone medical or surgical intervention used to treat vertigo. Patients who have significant balance problems occurring between acute vertigo episodes may also benefit from vestibular rehabilitation.6
Surgical Treatment
Surgical intervention should be the last resort to treat Ménière’s disease due to the higher risk involved with any surgical procedure and the potential adverse effect on hearing. Endolymphatic sac decompression surgery involves removing a portion of the mastoid bone, resulting in decompression of the sac adjacent to the sigmoid sinus. This procedure has been used for more than 40 years to control vertigo and has the advantage of preserving hearing.7,9 However, the benefit of this procedure is now somewhat controversial and possibly related to a placebo effect.6 Researchers also report positive results with the use of tenotomy surgery, which involves severing tendons to the stapedius and tensor tympani muscles in the middle ear.14
No surgical procedure should be considered without the recommendation of an otolaryngology specialist. The decision should be made based on the severity of the disease and its effect on the patient, weighed against the risks involved in such an invasive treatment option.
On the next page: Conclusion >>
CONCLUSION
Ménière’s disease is a complex disorder that can significantly alter a person’s quality of life. While neither the exact cause nor pathophysiology underlying Ménière’s disease is well understood, several solid theories are being investigated and contribute to the current understanding of treatment options. Primary care clinicians can help determine this clinical diagnosis based on a detailed history and comprehensive assessment of recurrent vertigo with tinnitus, hearing loss, and possibly a sensation of aural fullness. Establishing the diagnosis of Ménière’s disease requires ruling out other possible causes of vertigo.
Lifestyle changes that improve the consistency of dietary intake of sodium, caffeine, and alcohol as well as reduction of stress are ongoing recommendations for patients with Ménière’s disease. Oral medications from a range of drug categories may be used to improve acute and chronic symptoms, including antiemetics, anticholinergics, antihistamines, benzodiazepines, and mild diuretics. Additionally, a compounded substance with vasodilator and histamine- receptor–antagonist properties (betahistine) can be used for treatment of Meniere’s.
Patients who do not respond well to conservative therapy should be referred to an otolaryngologist for possible intratympanic medications, ventilation tube placement with a prescription for pulse pressure therapy (ie, Meniett device), or surgical intervention. Primary care clinicians can initiate treatment for Ménière’s disease by recommending lifestyle changes, prescribing oral medications, providing patient education, and recognizing indications for referral.
1. Greco A, Gallo A, Fusconi M, et al. Ménière’s disease might be an autoimmune condition? Autoimmun Rev. 2012;11:731-738.
2. Greenberg SL, Nedzelski JM. Medical and noninvasive therapy for Ménière’s disease. Otolaryngol Clin North Am. 2010;43:1081-1090.
3. American Academy of Otolaryngology–Head and Neck Foundation, Inc. Committee on Hearing and Equilibrium guidelines for the diagnosis and evaluation of therapy in Ménière’s disease. Otolaryngol Head Neck Surg. 1995;113:181-185.
4. Syed I, Aldren C. Ménière’s disease: an evidence based approach to assessment and management. Int J Clin Pract. 2012;66:166-170.
5. Rauch SD. Clinical hints and precipitating factors in patients suffering from Ménière’s disease. Otolaryngol Clin North Am. 2010;43:1011-1017.
6. Dinces EA, Rauch SS. Ménière’s disease. In: UpToDate. Deschler DG, Lin FH, eds. 2012:November 27,2012.
7. Semaan MT, Megerian CA. Ménière’s disease: a challenging and relentless disorder. Otolaryngol Clin North Am. 2011;44:383-403.
8. Martin González C, González FM, Trinidad A, et al. Medical management of Ménière’s disease: a 10-year case series and review of literature. Eur Arch Otorhinolaryngol. 2010;267:1371-1376.
9. Berlinger NT. Ménière’s disease: new concepts, new treatments. Minn Med. 2011;94:33-36.
10. von Brevern M, Neuhauser H. Epidemiological evidence for a link between vertigo and migraine. J Vestib Res. 2011;21:299-304.
11. Coelho DH, Lalwani AK. Medical management of Ménière’s disease. Laryngoscope. 2008;118:1099-1108.
12. Gates GA, Green JD Jr, Tucci DL, Telian SA. The effects of transtympanic micropressure treatment in people with unilateral Ménière’s disease. Arch Otolaryngol Head Neck Surg. 2004;130:718-725.
13. Long A, Xing M, Morgan K, Brettle A. Exploring the evidence base for acupuncture in the treatment of Ménière’s syndrome-a systematic review. Evid Based Complement Alternat Med. 2011;2011:1-13.
14. Loader B, Beicht D, Hamzavi JS, Franz P. Tenotomy of the middle ear muscles causes a dramatic reduction in vertigo attacks and improves audiological function in definite Ménière’s disease. Acta Otolaryngol. 2012;132:491-497.
1. Greco A, Gallo A, Fusconi M, et al. Ménière’s disease might be an autoimmune condition? Autoimmun Rev. 2012;11:731-738.
2. Greenberg SL, Nedzelski JM. Medical and noninvasive therapy for Ménière’s disease. Otolaryngol Clin North Am. 2010;43:1081-1090.
3. American Academy of Otolaryngology–Head and Neck Foundation, Inc. Committee on Hearing and Equilibrium guidelines for the diagnosis and evaluation of therapy in Ménière’s disease. Otolaryngol Head Neck Surg. 1995;113:181-185.
4. Syed I, Aldren C. Ménière’s disease: an evidence based approach to assessment and management. Int J Clin Pract. 2012;66:166-170.
5. Rauch SD. Clinical hints and precipitating factors in patients suffering from Ménière’s disease. Otolaryngol Clin North Am. 2010;43:1011-1017.
6. Dinces EA, Rauch SS. Ménière’s disease. In: UpToDate. Deschler DG, Lin FH, eds. 2012:November 27,2012.
7. Semaan MT, Megerian CA. Ménière’s disease: a challenging and relentless disorder. Otolaryngol Clin North Am. 2011;44:383-403.
8. Martin González C, González FM, Trinidad A, et al. Medical management of Ménière’s disease: a 10-year case series and review of literature. Eur Arch Otorhinolaryngol. 2010;267:1371-1376.
9. Berlinger NT. Ménière’s disease: new concepts, new treatments. Minn Med. 2011;94:33-36.
10. von Brevern M, Neuhauser H. Epidemiological evidence for a link between vertigo and migraine. J Vestib Res. 2011;21:299-304.
11. Coelho DH, Lalwani AK. Medical management of Ménière’s disease. Laryngoscope. 2008;118:1099-1108.
12. Gates GA, Green JD Jr, Tucci DL, Telian SA. The effects of transtympanic micropressure treatment in people with unilateral Ménière’s disease. Arch Otolaryngol Head Neck Surg. 2004;130:718-725.
13. Long A, Xing M, Morgan K, Brettle A. Exploring the evidence base for acupuncture in the treatment of Ménière’s syndrome-a systematic review. Evid Based Complement Alternat Med. 2011;2011:1-13.
14. Loader B, Beicht D, Hamzavi JS, Franz P. Tenotomy of the middle ear muscles causes a dramatic reduction in vertigo attacks and improves audiological function in definite Ménière’s disease. Acta Otolaryngol. 2012;132:491-497.