User login
Paid content by 
Treatment for relapsing forms of multiple sclerosis (MS) is critical to address the disease’s hallmark relapses and brain lesions.2 There are currently over a dozen approved disease-modifying medications, but no one treatment is right for every patient.2
In March 2020, the U.S. Food and Drug Administration (FDA) approved ZEPOSIA® (ozanimod) 0.92 mg, an oral medication taken once daily for the treatment of adults with relapsing forms of MS, including clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease.1
Patients may start ZEPOSIA as soon as the same day it is prescribed
Binding with high affinity to S1P receptors 1 and 5, ZEPOSIA blocks the capacity of lymphocytes to egress from lymph nodes, reducing the number of lymphocytes in peripheral blood.1 The mechanism by which ZEPOSIA exerts therapeutic effects in MS is unknown, but may involve the reduction of lymphocyte migration into the central nervous system.1
ZEPOSIA is the only S1P receptor modulator that offers relapsing forms of MS patients an initiation with no genetic test and no required label-based first-dose observation.1,3,4 An up-titration scheme should be used to reach the maintenance dosage of ZEPOSIA, as a transient decrease in heart rate and atrioventricular conduction delays may occur.1 Before initiation of treatment with ZEPOSIA, all patients require assessments including a recent complete blood count including lymphocyte count (within six months or after discontinuation of prior MS therapy), an ECG to determine whether preexisting conduction abnormalities are present, a recent liver function test (within six months), and consideration of current and prior medications, including vaccinations.1 For patients with a history of uveitis or macular edema, an ophthalmic assessment is required.1
ZEPOSIA is contraindicated in patients who in the last six months experienced myocardial infarction, unstable angina, stroke, transient ischemic attack (TIA), decompensated heart failure requiring hospitalization, or Class III/IV heart failure; patients who have a presence of Mobitz type II second or third-degree atrioventricular (AV) block, sick sinus syndrome, or sino-atrial, unless the patient has a functioning pacemaker; patients with severe untreated sleep apnea; and patients taking a monoamine oxidase inhibitor.1ZEPOSIA is associated with the following Warnings and Precautions: increased risk of infections, bradyarrhythmia and atrioventricular conduction delays, liver injury, fetal risk, increased blood pressure, respiratory effects, macular edema, posterior reversible encephalopathy syndrome, additive immunosuppressive effects from prior immune-modulating treatments, severe increase in disability after stopping ZEPOSIA, and immune system effects after stopping ZEPOSIA.1 Please see Important Safety Information for additional details. The most common adverse reactions (incidence ≥4%) were upper respiratory infection, hepatic transaminase elevation, orthostatic hypotension, urinary tract infection, back pain, and hypertension.1
“There is no one size fits all treatment for patients with relapsing forms of MS, and doctors and patients are still seeking additional therapies that can address the hallmarks of this devastating disease,” said Mary Beth Harler, M.D., senior vice president, head of immunology and fibrosis development, Bristol Myers Squibb. “ZEPOSIA has demonstrated clinical potential in safety and efficacy and may allow patients to begin treatment the same day it is prescribed.”1
Powerful efficacy demonstrated in clinical trials
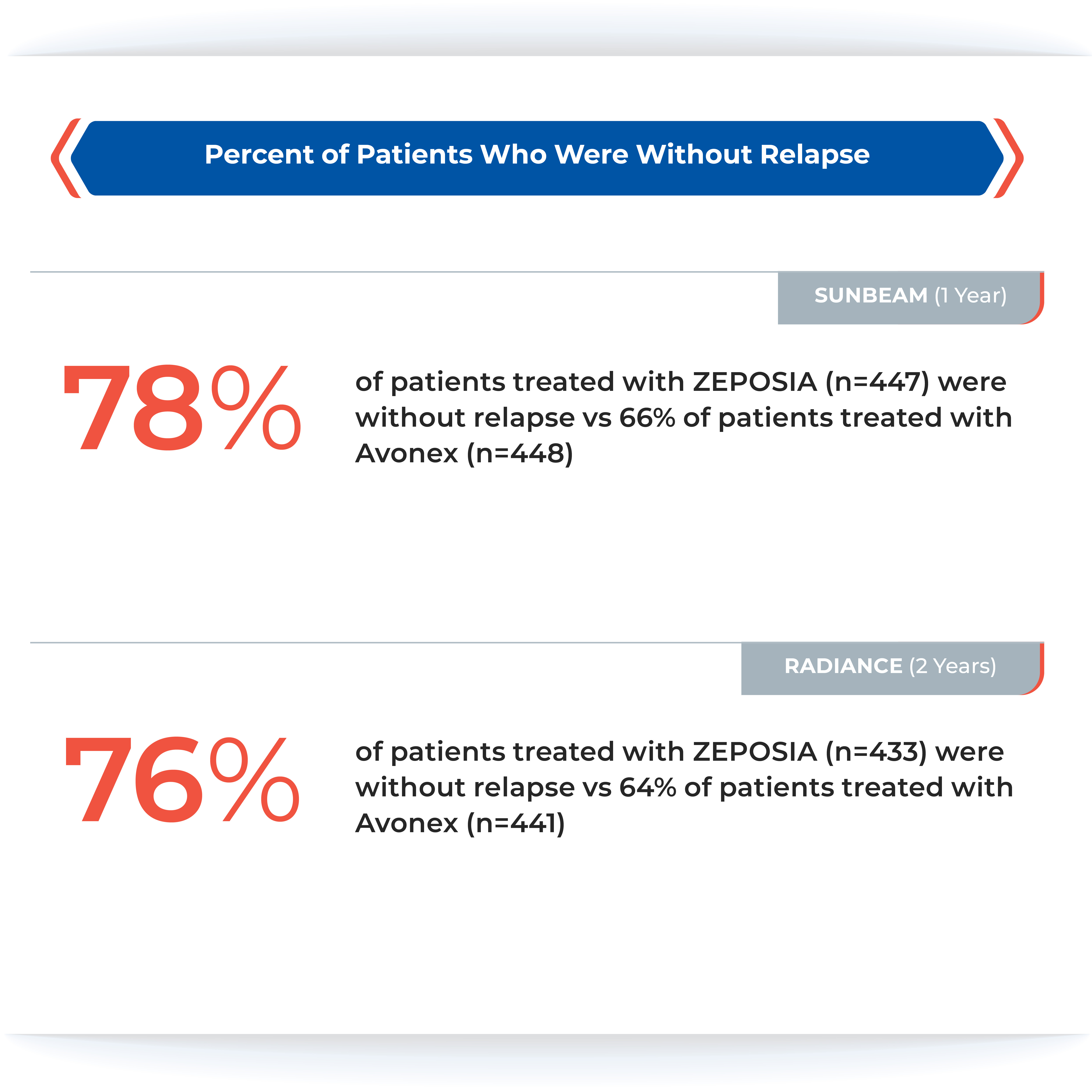
The ZEPOSIA approval was based on data from the largest, pivotal, head-to-head relapsing forms of MS studies with an active comparator to date: the randomized, Phase 3 SUNBEAM™ (safety and efficacy of ZEPOSIA versus interferon beta-1a in relapsing multiple sclerosis) and RADIANCE™ (safety and efficacy of the selective sphingosine 1-phosphate receptor modulator ZEPOSIA in relapsing multiple sclerosis) Part B clinical trials (N=2699).1,5,6,7 In both trials – as compared to AVONEX® (interferon beta-1a) – ZEPOSIA delivered powerful efficacy as measured by the primary endpoint of annualized relapse rate (ARR):
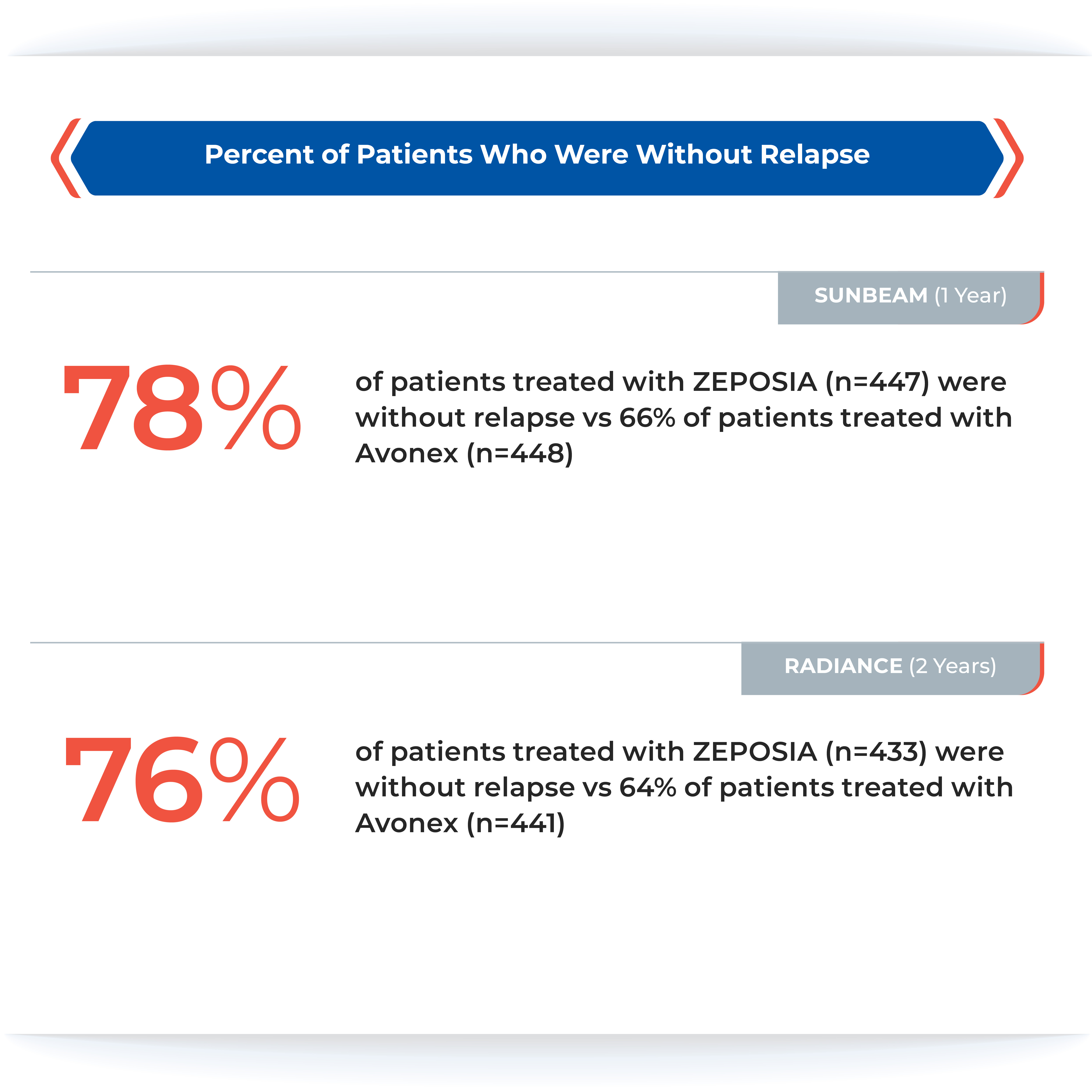
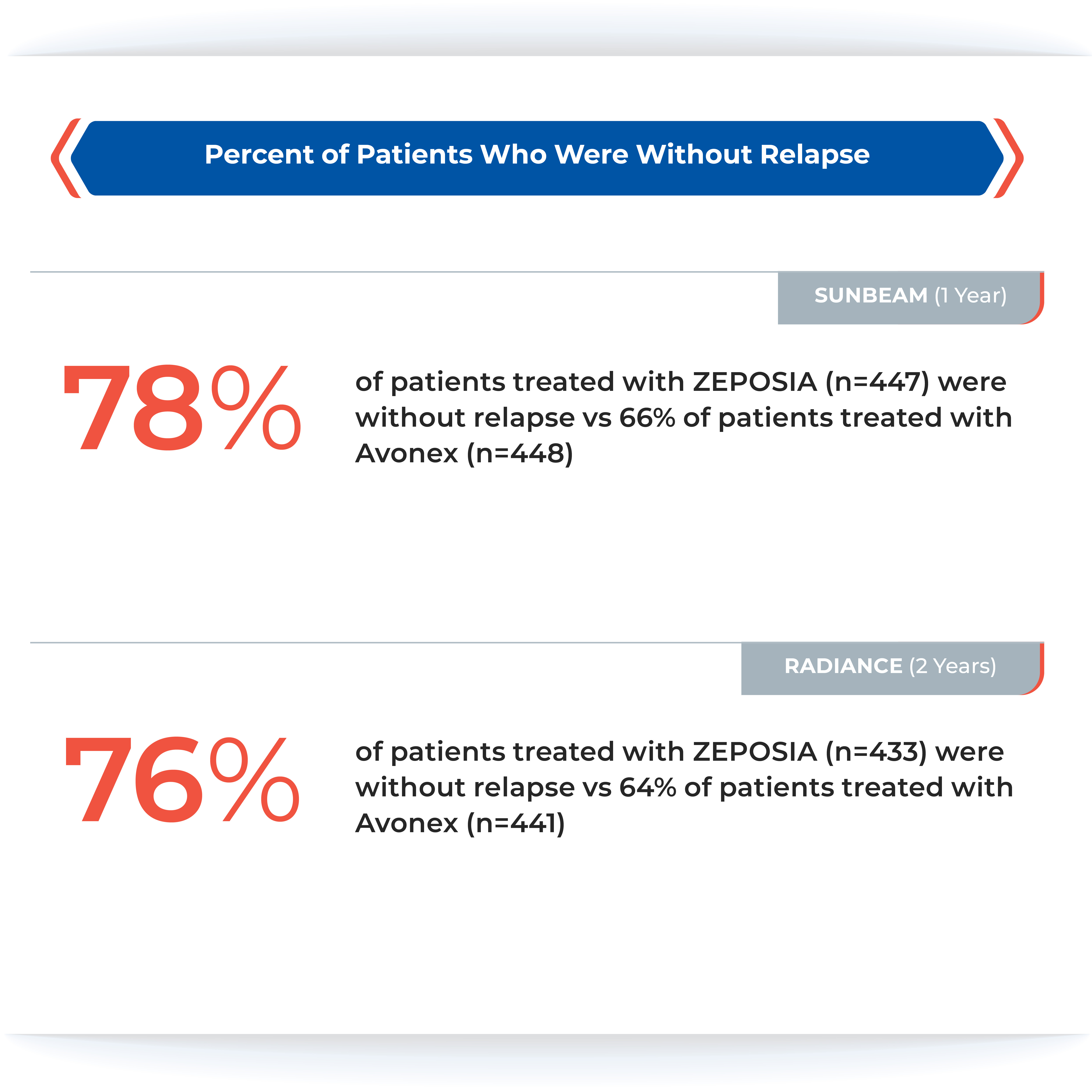
ZEPOSIA demonstrated a relative reduction in ARR versus AVONEX of 48% at one year and 38% at two years (absolute ARR of 0.18 versus 0.35 and 0.17 versus 0.28, respectively).1,5,6

The majority of patients in both groups experienced zero relapses.1
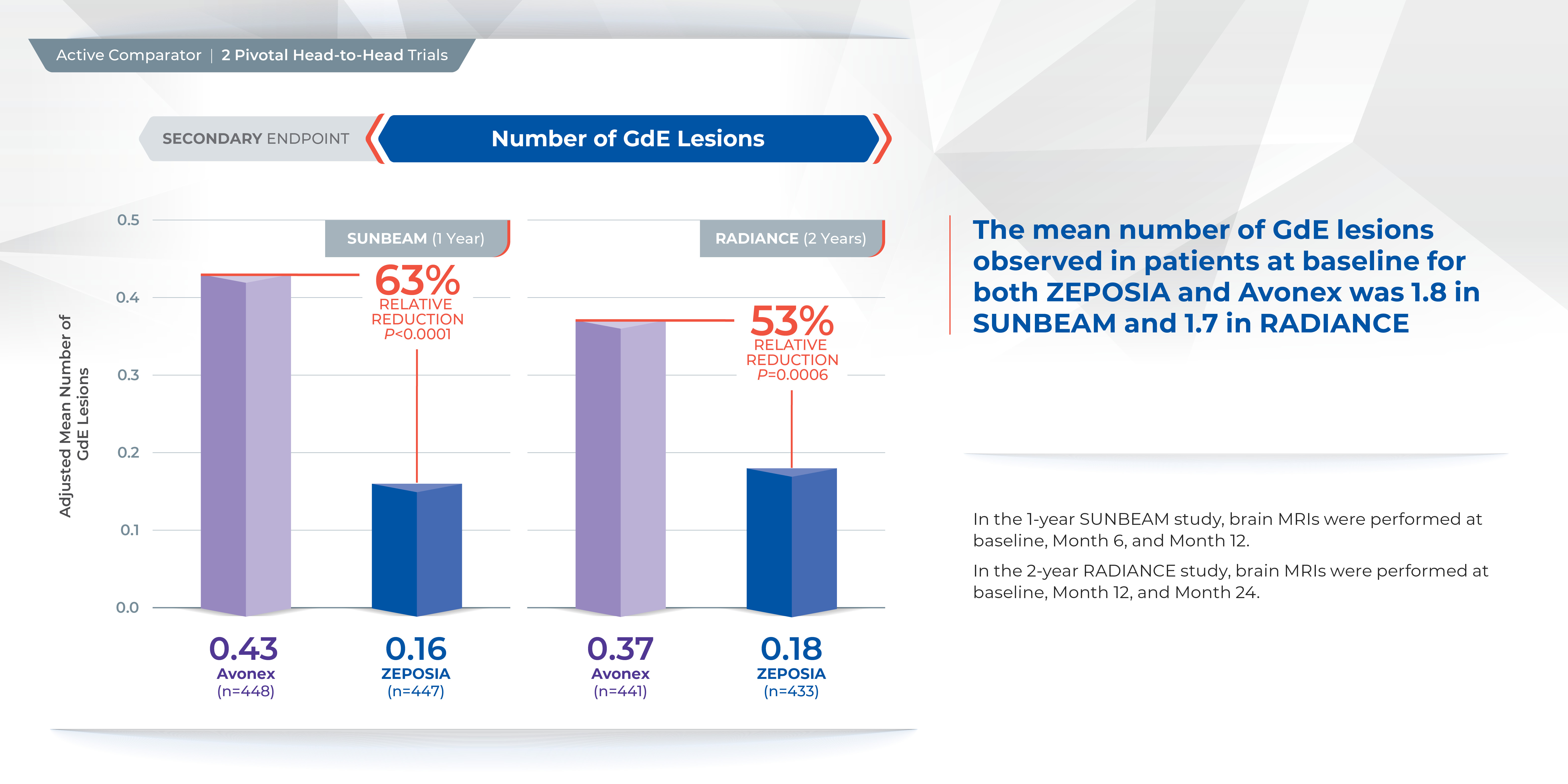
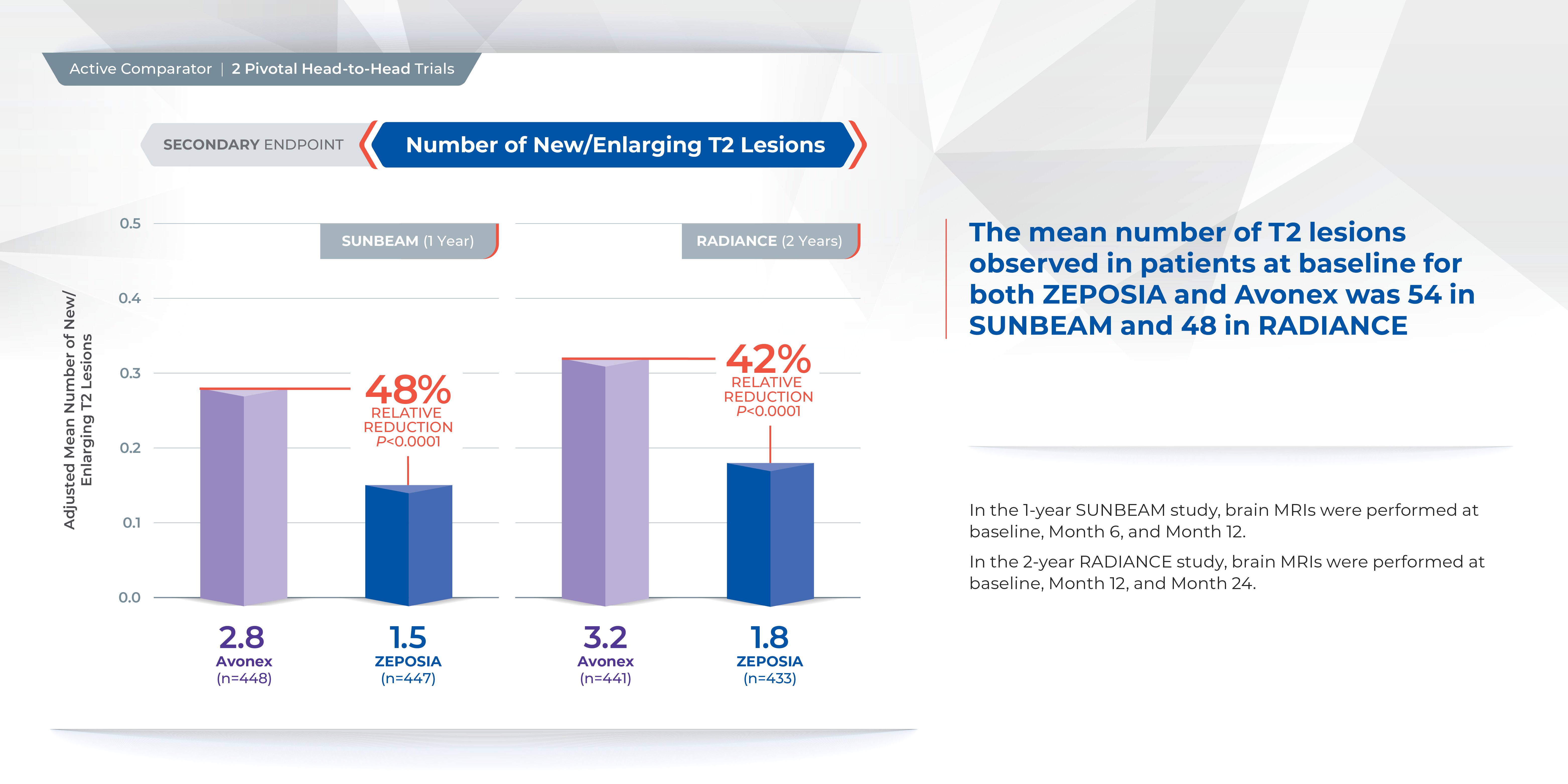
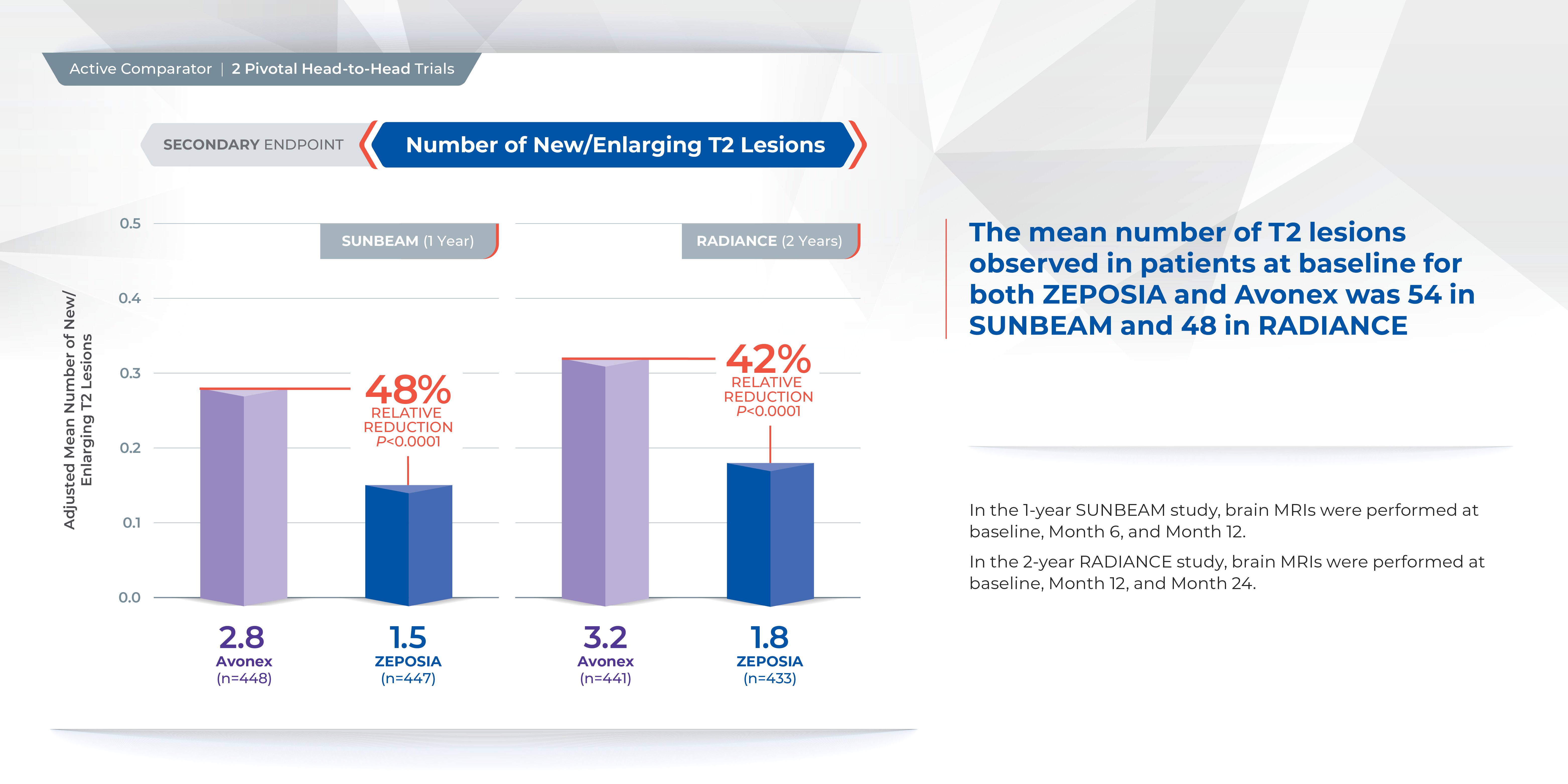
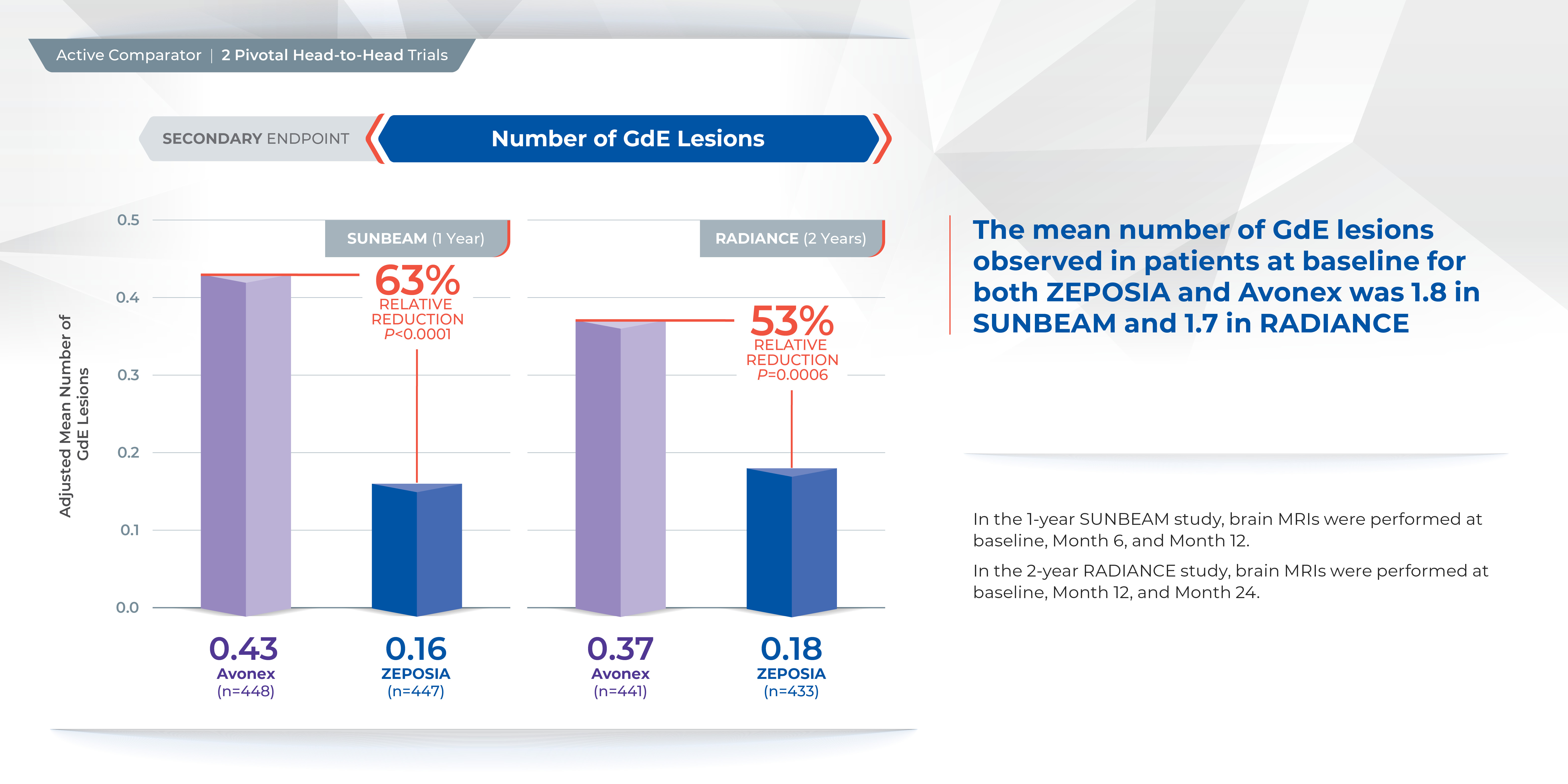
Proven superiority in reducing brain lesions
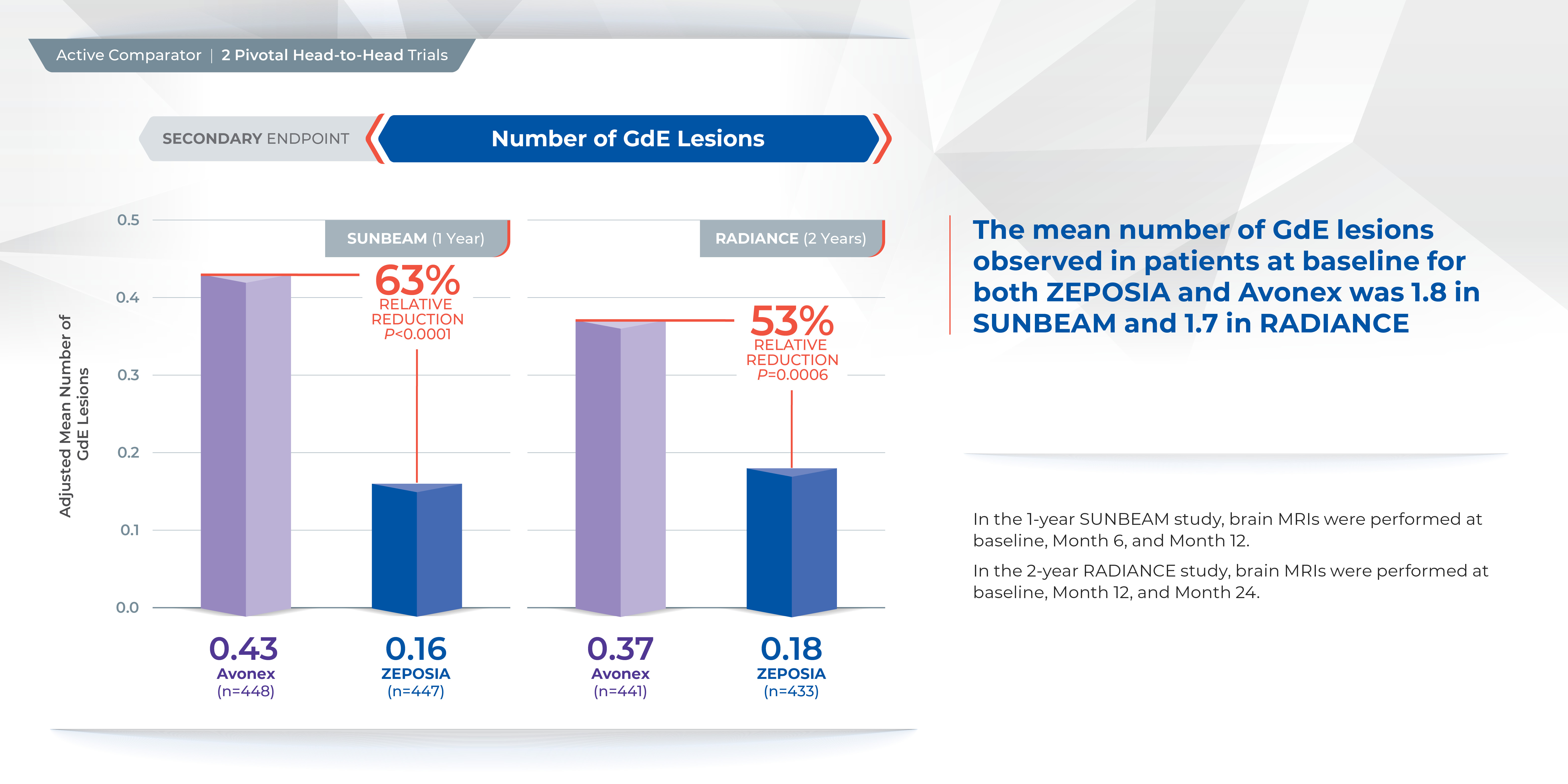
Treatment with ZEPOSIA reduced the number of T1-weighted gadolinium-enhanced (GdE) brain lesions more than AVONEX at one year (0.16 vs 0.43), a relative reduction of 63%, and at two years (0.18 vs 0.37), a relative reduction of 53%.1
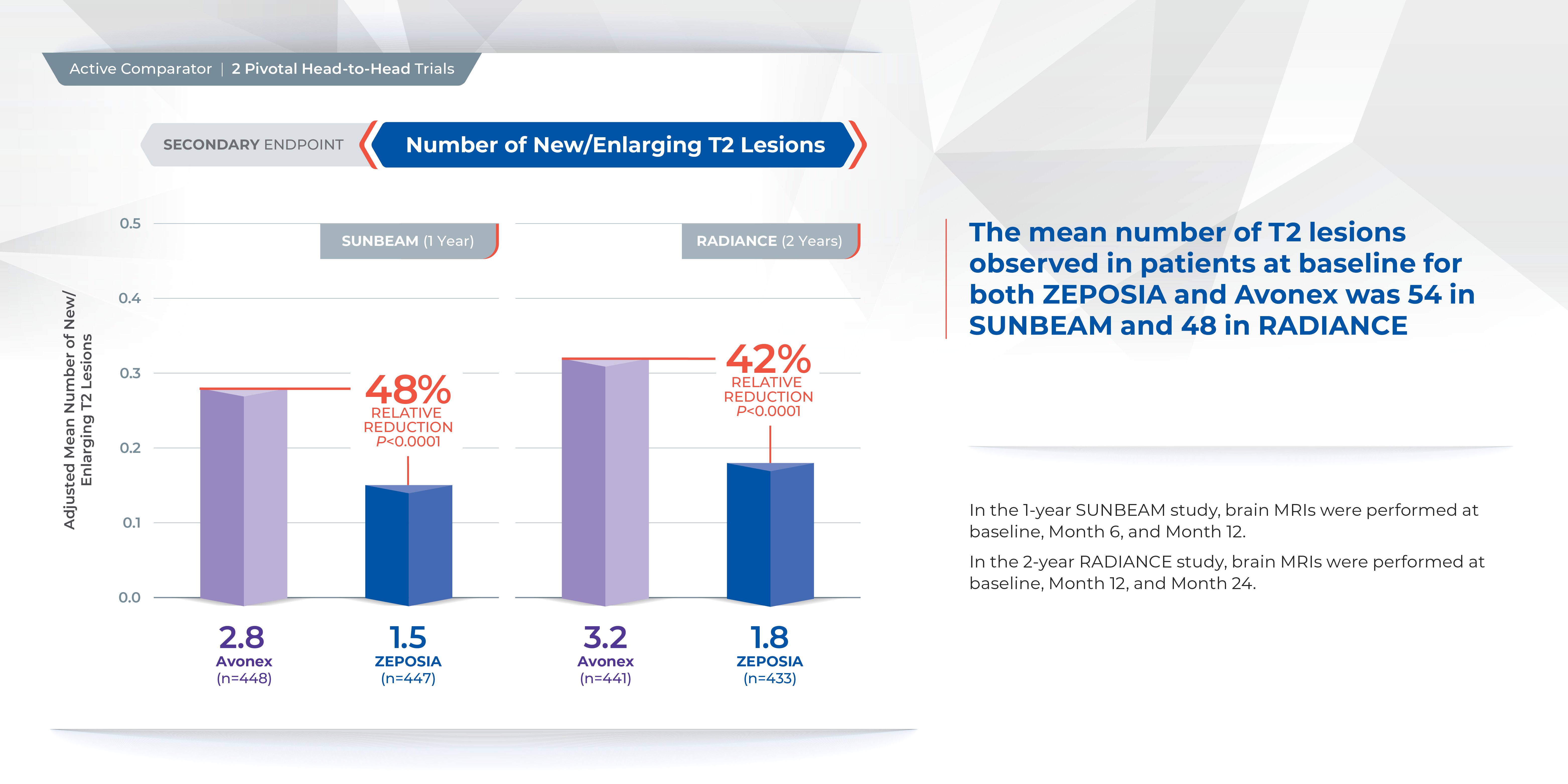
In addition, the number of new or enlarging T2 lesions was reduced at one year (1.47 vs. 2.84), a relative reduction of 48%, as well as at two years (1.84 versus 3.18), a relative reduction of 42%.1
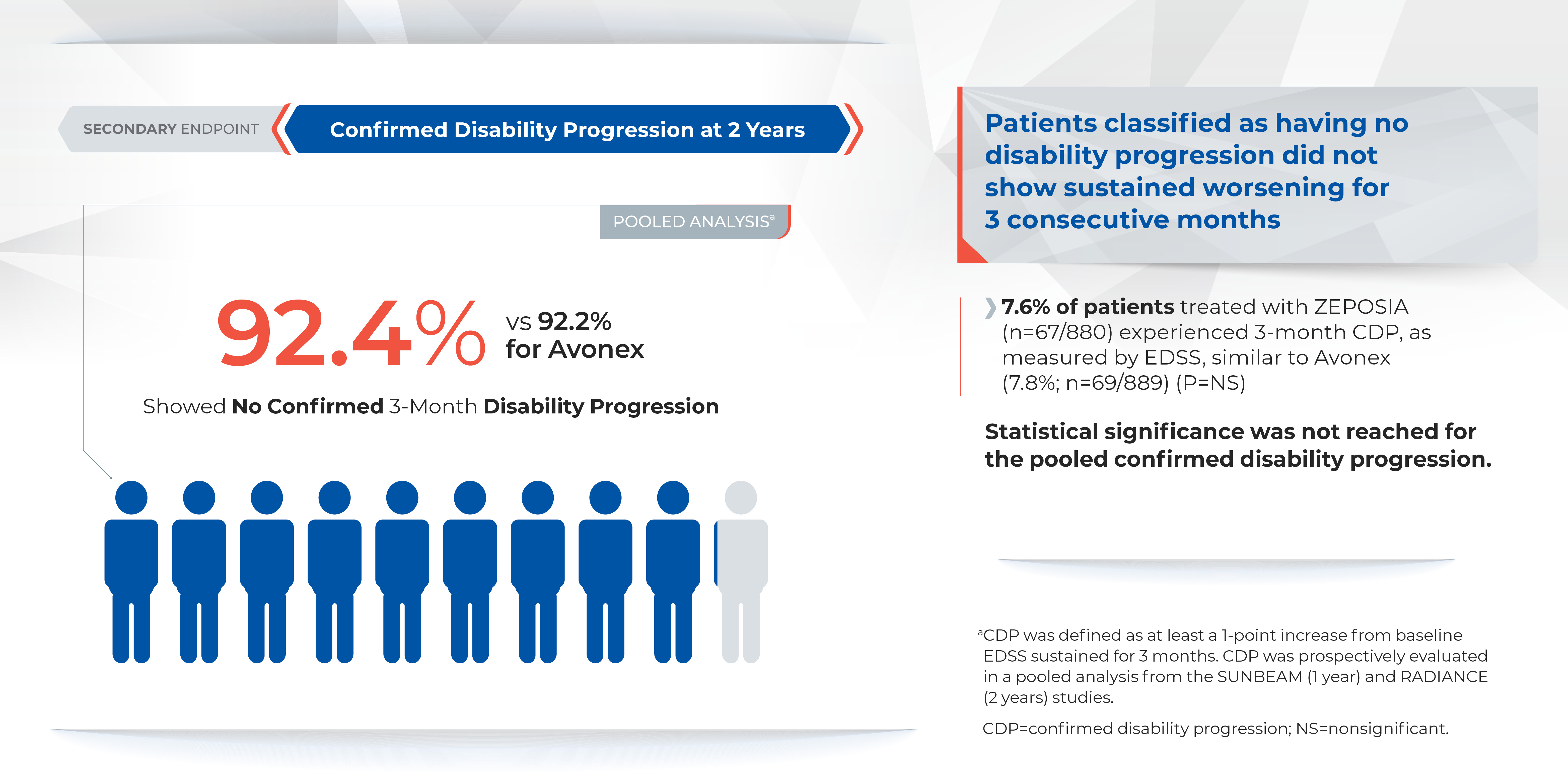
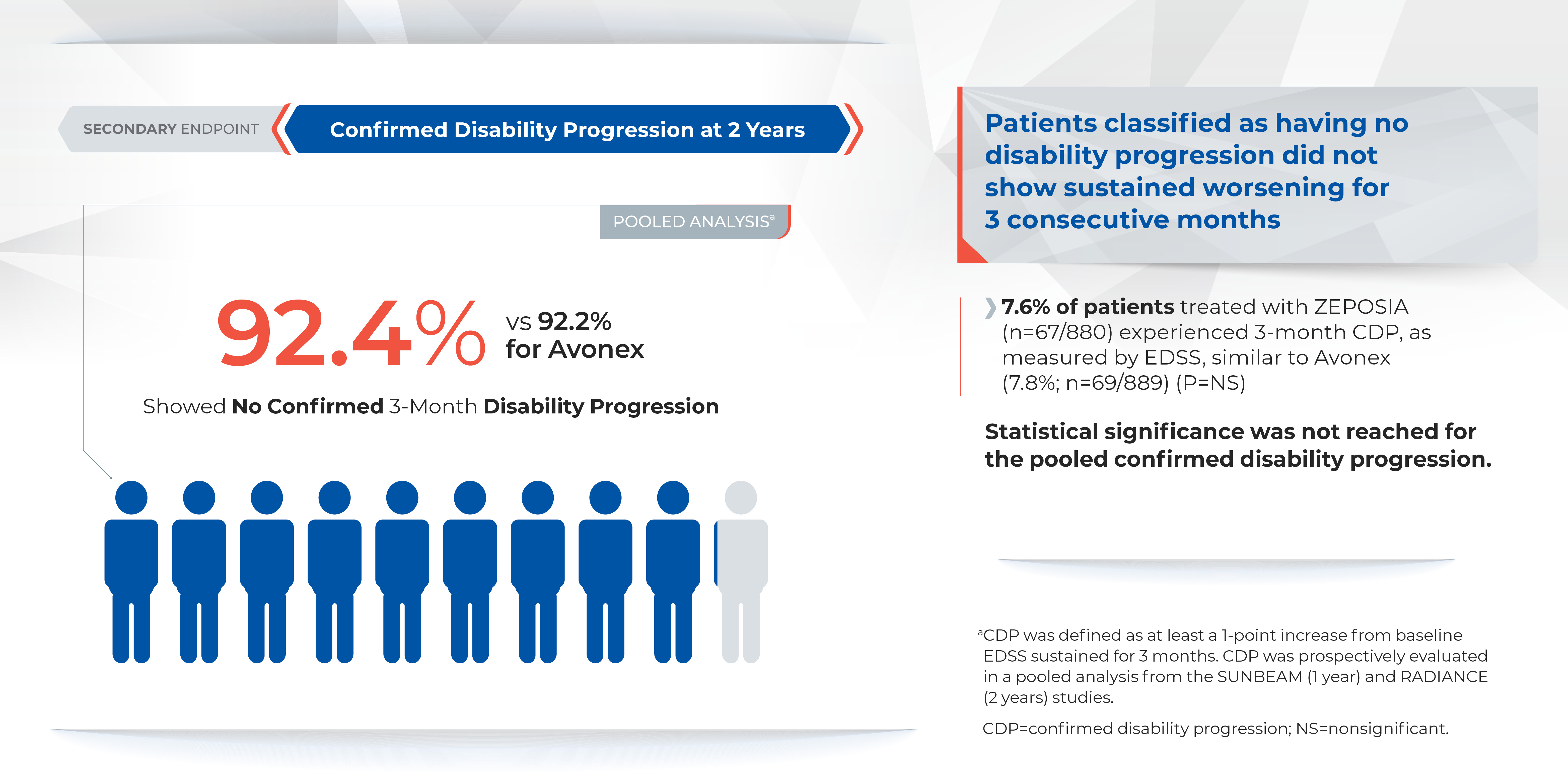
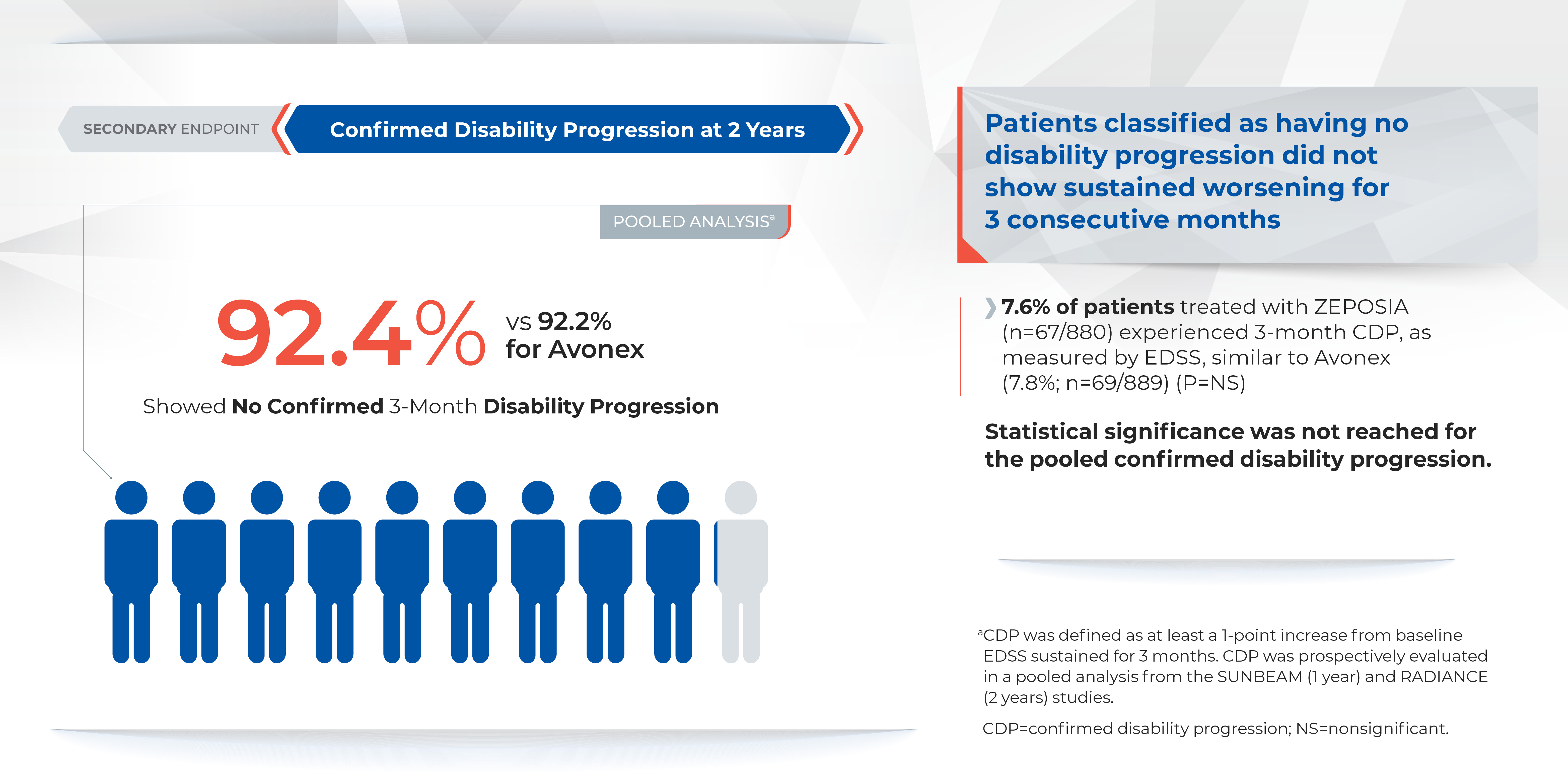
There was no statistically significant difference in the three-month and six-month confirmed disability progression between ZEPOSIA- and AVONEX- treated patients over two years.1
Comparable safety to AVONEX in overall incidence of adverse events
The overall incidence of adverse reactions experienced by patients for ZEPOSIA vs. AVONEX at one year were 59.8% and 75.5%, respectively, and at two years were 74.7% and 83.0%, respectively.1 ZEPOSIA demonstrated consistently low discontinuation rates due to adverse events versus AVONEX (<3%); at one year discontinuation rates due to adverse events for AVONEX were 3.6% and for ZEPOSIA were 2.9%, at two years discontinuation rates due to adverse events for AVONEX were 4.1% and for ZEPOSIA were 3.0%1 Overall discontinuation rates were <10% versus AVONEX across both trials. At one year discontinuation rates for AVONEX were 8% and for ZEPOSIA were 6%, at two years discontinuation rates for AVONEX were 15% and for ZEPOSIA were 10%.1
ZEPOSIA is contraindicated in patients who in the last six months experienced myocardial infarction, unstable angina, stroke, transient ischemic attack (TIA), decompensated heart failure requiring hospitalization, or Class III/IV heart failure; patients who have a presence of Mobitz type II second or third-degree atrioventricular (AV) block, sick sinus syndrome, or sino-atrial, unless the patient has a functioning pacemaker; patients with severe untreated sleep apnea; and patients taking a monoamine oxidase inhibitor.1 ZEPOSIA is associated with the following Warnings and Precautions: increased risk of infections, bradyarrhythmia and atrioventricular conduction delays, liver injury, fetal risk, increased blood pressure, respiratory effects, macular edema, posterior reversible encephalopathy syndrome, additive immunosuppressive effects from prior immune-modulating treatments, severe increase in disability after stopping ZEPOSIA, and immune system effects after stopping ZEPOSIA.1 Please see Important Safety Information for additional details.1 The most common adverse reactions (incidence ≥4%) were upper respiratory infection, hepatic transaminase elevation, orthostatic hypotension, urinary tract infection, back pain, and hypertension.1
Please visit www.ZEPOSIAHCP.com to learn more.
Indication
ZEPOSIA is indicated for the treatment of relapsing forms of multiple sclerosis (MS), to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults.
IMPORTANT SAFETY INFORMATION1
Contraindications:
- Patients who in the last 6 months, experienced myocardial infarction, unstable angina, stroke, transient ischemic attack (TIA), decompensated heart failure requiring hospitalization, or Class III/IV heart failure or have a presence of Mobitz type II second or third-degree atrioventricular (AV) block, sick sinus syndrome, or sino-atrial, unless the patient has a functioning pacemaker
- Patients with severe untreated sleep apnea
- Patients taking a monoamine oxidase (MAO) inhibitor
Infections: ZEPOSIA may increase the susceptibility to infections. Life-threatening and rare fatal infections have occurred in patients receiving ZEPOSIA. Obtain a recent (i.e., within 6 months or after discontinuation of prior MS therapy) complete blood count (CBC) including lymphocyte count before initiation of ZEPOSIA. Delay initiation of ZEPOSIA in patients with an active infection until the infection is resolved. Consider interruption of treatment with ZEPOSIA if a patient develops a serious infection. Continue monitoring for infections up to 3 months after discontinuing ZEPOSIA
- Herpes zoster was reported as an adverse reaction in ZEPOSIA-treated patients. Herpes simplex encephalitis and varicella zoster meningitis have been reported with sphingosine 1-phosphate (S1P) receptor modulators. Patients without a healthcare professional-confirmed history of varicella (chickenpox), or without documentation of a full course of vaccination against varicella zoster virus (VZV), should be tested for antibodies to VZV before initiating ZEPOSIA. A full course of vaccination for antibody-negative patients with varicella vaccine is recommended prior to commencing treatment with ZEPOSIA
- Cases of fatal cryptococcal meningitis (CM) were reported in patients treated with another S1P receptor modulator. If CM is suspected, ZEPOSIA should be suspended until cryptococcal infection has been excluded. If CM is diagnosed, appropriate treatment should be initiated.
- Progressive Multifocal Leukoencephalopathy (PML) is an opportunistic viral infection of the brain that typically occurs in patients who are immunocompromised, and that usually leads to death or severe disability. No cases of PML were identified in active-controlled MS clinical trials with ZEPOSIA. PML has been reported in patients treated with S1P receptor modulators and other MS therapies and has been associated with some risk factors. If PML is suspected, withhold ZEPOSIA and perform an appropriate diagnostic evaluation. If confirmed, treatment with ZEPOSIA should be discontinued
- In clinical studies, patients who received ZEPOSIA were not to receive concomitant treatment with antineoplastic, non-corticosteroid immunosuppressive, or immune-modulating therapies used for treatment of MS. Concomitant use of ZEPOSIA with any of these therapies would be expected to increase the risk of immunosuppression. When switching to ZEPOSIA from immunosuppressive medications, consider the duration of their effects and their mode of action to avoid unintended additive immunosuppressive effects
- Use of live attenuated vaccines should be avoided during and for 3 months after treatment with ZEPOSIA. If live attenuated vaccine immunizations are required, administer at least 1 month prior to initiation of ZEPOSIA
Bradyarrhythmia and Atrioventricular Conduction Delays: Since initiation of ZEPOSIA may result in a transient decrease in heart rate and atrioventricular conduction delays, dose titration is recommended to help reduce cardiac effects. Initiation of ZEPOSIA without dose escalation may result in greater decreases in heart rate. If treatment with ZEPOSIA is considered, advice from a cardiologist should be sought for those individuals:
- with significant QT prolongation
- with arrhythmias requiring treatment with Class 1a or III anti-arrhythmic drugs
- with ischemic heart disease, heart failure, history of cardiac arrest or myocardial infarction, cerebrovascular disease, and uncontrolled hypertension
- with a history of Mobitz type II second-degree or higher AV block, sick-sinus syndrome, or sinoatrial heart block
Liver Injury: Elevations of aminotransferases may occur in patients receiving ZEPOSIA. Obtain liver function tests, if not recently available (i.e., within 6 months), before initiation of ZEPOSIA. Patients who develop symptoms suggestive of hepatic dysfunction should have hepatic enzymes checked and ZEPOSIA should be discontinued if significant liver injury is confirmed. Caution should be exercised when using ZEPOSIA in patients with history of significant liver disease
Fetal Risk: There are no adequate and well-controlled studies in pregnant women. Based on animal studies, ZEPOSIA may cause fetal harm. Women of childbearing potential should use effective contraception to avoid pregnancy during treatment and for 3 months after stopping ZEPOSIA
Increased Blood Pressure: Increase in systolic pressure was observed after about 3 months of treatment and persisted throughout treatment. Blood pressure should be monitored during treatment and managed appropriately. Certain foods that may contain very high amounts of tyramine could cause severe hypertension in patients taking ZEPOSIA. Patients should be advised to avoid foods containing a very large amount of tyramine while taking ZEPOSIA
Respiratory Effects: ZEPOSIA may cause a decline in pulmonary function. Spirometric evaluation of respiratory function should be performed during therapy, if clinically indicated
Macular edema: S1P modulators have been associated with an increased risk of macular edema. Patients with a history of uveitis or diabetes mellitus are at increased risk. Patients with a history of these conditions should have an ophthalmic evaluation of the fundus, including the macula, prior to treatment initiation and regular follow-up examinations. An ophthalmic evaluation is recommended in all patients at any time if there is a change in vision. Continued use of ZEPOSIA in patients with macular edema has not been evaluated; potential benefits and risks for the individual patient should be considered if deciding whether ZEPOSIA should be discontinued
Posterior Reversible Encephalopathy Syndrome (PRES): Rare cases of PRES have been reported in patients receiving a S1P receptor modulator. If a ZEPOSIA-treated patient develops unexpected neurological or psychiatric symptoms or any symptom/sign suggestive of an increase in intracranial pressure, a complete physical and neurological examination should be conducted. Symptoms of PRES are usually reversible but may evolve into ischemic stroke or cerebral hemorrhage. Delay in diagnosis and treatment may lead to permanent neurological sequelae. If PRES is suspected, treatment with ZEPOSIA should be discontinued
Unintended Additive Immunosuppressive Effects From Prior Immunosuppressive or Immune-Modulating Drugs: When switching from drugs with prolonged immune effects, the half-life and mode of action of these drugs must be considered to avoid unintended additive immunosuppressive effects while at the same time minimizing risk of disease reactivation. Initiating treatment with ZEPOSIA after treatment with alemtuzumab is not recommended
Severe Increase in Disability After Stopping ZEPOSIA: Severe exacerbation of disease, including disease rebound, has been rarely reported after discontinuation of a S1P receptor modulator. The possibility of severe exacerbation of disease should be considered after stopping ZEPOSIA treatment so patients should be monitored upon discontinuation
Immune System Effects After Stopping ZEPOSIA: After discontinuing ZEPOSIA, the median time for lymphocyte counts to return to the normal range was 30 days with approximately 90% of patients in the normal range within 3 months. Use of immunosuppressants within this period may lead to an additive effect on the immune system, therefore caution should be applied when initiating other drugs 4 weeks after the last dose of ZEPOSIA
Most common Adverse Reactions (≥ 4%): upper respiratory infection, hepatic transaminase elevation, orthostatic hypotension, urinary tract infection, back pain, and hypertension.
For additional safety information, please see the full Prescribing Information and Medication Guide.
1. ZEPOSIA (ozanimod) capsules for oral use. Celgene Corporation. Full prescribing information. 3/2020.
2. National Multiple Sclerosis Society. Treating RMSS. www.nationalmssociety.org/What-is-MS/Types-of-MS/Relapsing-remitting-MS/Treatment. Accessed on April 24, 2020.
3. GILENYA (fingolimod) capsules for oral use. Novartis Pharmaceuticals Corporation. Full prescribing information. 8/2019.
4. MAYZENT (siponimod) tablets for oral use. Novartis Pharmaceuticals Corporation. Full prescribing information. 3/2019.
5. Cohen, JA, Comi, G, Selmaj, KW, et al. Safety and efficacy of ozanimod versus interferon beta-1a in relapsing multiple sclerosis (RADIANCE): a multicenter, randomized, 24-month, phase 3 trial. The Lancet: Neurology. DOI: 10.1016/S1474-4422(19)30238-8.
6. Comi, G, Kappos, L, Selmaj, KW, et at. Safety and efficacy of ozanimod versus interferon beta-1a in relapsing multiple sclerosis (SUNBEAM): a multicenter, randomized, minimum 12-month, phase 3 trial. The Lancet: Neurology. DOI: 10.1016/S1474-4422(19)30239-X.
7. McCann Agency. Pivotal Trials for MS Therapies: ZEPOSIA –2 head-to-head with Active Comparator Based on PIs. March 2020.
ZEPOSIA® is a trademark of Bristol-Myers Squibb Company.
© 2020 Bristol-Myers Squibb Company. All Rights Reserved.
US-ZEP-20-1095 10/20
Paid content by 
Treatment for relapsing forms of multiple sclerosis (MS) is critical to address the disease’s hallmark relapses and brain lesions.2 There are currently over a dozen approved disease-modifying medications, but no one treatment is right for every patient.2
In March 2020, the U.S. Food and Drug Administration (FDA) approved ZEPOSIA® (ozanimod) 0.92 mg, an oral medication taken once daily for the treatment of adults with relapsing forms of MS, including clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease.1
Patients may start ZEPOSIA as soon as the same day it is prescribed
Binding with high affinity to S1P receptors 1 and 5, ZEPOSIA blocks the capacity of lymphocytes to egress from lymph nodes, reducing the number of lymphocytes in peripheral blood.1 The mechanism by which ZEPOSIA exerts therapeutic effects in MS is unknown, but may involve the reduction of lymphocyte migration into the central nervous system.1
ZEPOSIA is the only S1P receptor modulator that offers relapsing forms of MS patients an initiation with no genetic test and no required label-based first-dose observation.1,3,4 An up-titration scheme should be used to reach the maintenance dosage of ZEPOSIA, as a transient decrease in heart rate and atrioventricular conduction delays may occur.1 Before initiation of treatment with ZEPOSIA, all patients require assessments including a recent complete blood count including lymphocyte count (within six months or after discontinuation of prior MS therapy), an ECG to determine whether preexisting conduction abnormalities are present, a recent liver function test (within six months), and consideration of current and prior medications, including vaccinations.1 For patients with a history of uveitis or macular edema, an ophthalmic assessment is required.1
ZEPOSIA is contraindicated in patients who in the last six months experienced myocardial infarction, unstable angina, stroke, transient ischemic attack (TIA), decompensated heart failure requiring hospitalization, or Class III/IV heart failure; patients who have a presence of Mobitz type II second or third-degree atrioventricular (AV) block, sick sinus syndrome, or sino-atrial, unless the patient has a functioning pacemaker; patients with severe untreated sleep apnea; and patients taking a monoamine oxidase inhibitor.1ZEPOSIA is associated with the following Warnings and Precautions: increased risk of infections, bradyarrhythmia and atrioventricular conduction delays, liver injury, fetal risk, increased blood pressure, respiratory effects, macular edema, posterior reversible encephalopathy syndrome, additive immunosuppressive effects from prior immune-modulating treatments, severe increase in disability after stopping ZEPOSIA, and immune system effects after stopping ZEPOSIA.1 Please see Important Safety Information for additional details. The most common adverse reactions (incidence ≥4%) were upper respiratory infection, hepatic transaminase elevation, orthostatic hypotension, urinary tract infection, back pain, and hypertension.1
“There is no one size fits all treatment for patients with relapsing forms of MS, and doctors and patients are still seeking additional therapies that can address the hallmarks of this devastating disease,” said Mary Beth Harler, M.D., senior vice president, head of immunology and fibrosis development, Bristol Myers Squibb. “ZEPOSIA has demonstrated clinical potential in safety and efficacy and may allow patients to begin treatment the same day it is prescribed.”1
Powerful efficacy demonstrated in clinical trials
The ZEPOSIA approval was based on data from the largest, pivotal, head-to-head relapsing forms of MS studies with an active comparator to date: the randomized, Phase 3 SUNBEAM™ (safety and efficacy of ZEPOSIA versus interferon beta-1a in relapsing multiple sclerosis) and RADIANCE™ (safety and efficacy of the selective sphingosine 1-phosphate receptor modulator ZEPOSIA in relapsing multiple sclerosis) Part B clinical trials (N=2699).1,5,6,7 In both trials – as compared to AVONEX® (interferon beta-1a) – ZEPOSIA delivered powerful efficacy as measured by the primary endpoint of annualized relapse rate (ARR):
ZEPOSIA demonstrated a relative reduction in ARR versus AVONEX of 48% at one year and 38% at two years (absolute ARR of 0.18 versus 0.35 and 0.17 versus 0.28, respectively).1,5,6

The majority of patients in both groups experienced zero relapses.1
Proven superiority in reducing brain lesions
Treatment with ZEPOSIA reduced the number of T1-weighted gadolinium-enhanced (GdE) brain lesions more than AVONEX at one year (0.16 vs 0.43), a relative reduction of 63%, and at two years (0.18 vs 0.37), a relative reduction of 53%.1
In addition, the number of new or enlarging T2 lesions was reduced at one year (1.47 vs. 2.84), a relative reduction of 48%, as well as at two years (1.84 versus 3.18), a relative reduction of 42%.1
There was no statistically significant difference in the three-month and six-month confirmed disability progression between ZEPOSIA- and AVONEX- treated patients over two years.1
Comparable safety to AVONEX in overall incidence of adverse events
The overall incidence of adverse reactions experienced by patients for ZEPOSIA vs. AVONEX at one year were 59.8% and 75.5%, respectively, and at two years were 74.7% and 83.0%, respectively.1 ZEPOSIA demonstrated consistently low discontinuation rates due to adverse events versus AVONEX (<3%); at one year discontinuation rates due to adverse events for AVONEX were 3.6% and for ZEPOSIA were 2.9%, at two years discontinuation rates due to adverse events for AVONEX were 4.1% and for ZEPOSIA were 3.0%1 Overall discontinuation rates were <10% versus AVONEX across both trials. At one year discontinuation rates for AVONEX were 8% and for ZEPOSIA were 6%, at two years discontinuation rates for AVONEX were 15% and for ZEPOSIA were 10%.1
ZEPOSIA is contraindicated in patients who in the last six months experienced myocardial infarction, unstable angina, stroke, transient ischemic attack (TIA), decompensated heart failure requiring hospitalization, or Class III/IV heart failure; patients who have a presence of Mobitz type II second or third-degree atrioventricular (AV) block, sick sinus syndrome, or sino-atrial, unless the patient has a functioning pacemaker; patients with severe untreated sleep apnea; and patients taking a monoamine oxidase inhibitor.1 ZEPOSIA is associated with the following Warnings and Precautions: increased risk of infections, bradyarrhythmia and atrioventricular conduction delays, liver injury, fetal risk, increased blood pressure, respiratory effects, macular edema, posterior reversible encephalopathy syndrome, additive immunosuppressive effects from prior immune-modulating treatments, severe increase in disability after stopping ZEPOSIA, and immune system effects after stopping ZEPOSIA.1 Please see Important Safety Information for additional details.1 The most common adverse reactions (incidence ≥4%) were upper respiratory infection, hepatic transaminase elevation, orthostatic hypotension, urinary tract infection, back pain, and hypertension.1
Please visit www.ZEPOSIAHCP.com to learn more.
Indication
ZEPOSIA is indicated for the treatment of relapsing forms of multiple sclerosis (MS), to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults.
IMPORTANT SAFETY INFORMATION1
Contraindications:
- Patients who in the last 6 months, experienced myocardial infarction, unstable angina, stroke, transient ischemic attack (TIA), decompensated heart failure requiring hospitalization, or Class III/IV heart failure or have a presence of Mobitz type II second or third-degree atrioventricular (AV) block, sick sinus syndrome, or sino-atrial, unless the patient has a functioning pacemaker
- Patients with severe untreated sleep apnea
- Patients taking a monoamine oxidase (MAO) inhibitor
Infections: ZEPOSIA may increase the susceptibility to infections. Life-threatening and rare fatal infections have occurred in patients receiving ZEPOSIA. Obtain a recent (i.e., within 6 months or after discontinuation of prior MS therapy) complete blood count (CBC) including lymphocyte count before initiation of ZEPOSIA. Delay initiation of ZEPOSIA in patients with an active infection until the infection is resolved. Consider interruption of treatment with ZEPOSIA if a patient develops a serious infection. Continue monitoring for infections up to 3 months after discontinuing ZEPOSIA
- Herpes zoster was reported as an adverse reaction in ZEPOSIA-treated patients. Herpes simplex encephalitis and varicella zoster meningitis have been reported with sphingosine 1-phosphate (S1P) receptor modulators. Patients without a healthcare professional-confirmed history of varicella (chickenpox), or without documentation of a full course of vaccination against varicella zoster virus (VZV), should be tested for antibodies to VZV before initiating ZEPOSIA. A full course of vaccination for antibody-negative patients with varicella vaccine is recommended prior to commencing treatment with ZEPOSIA
- Cases of fatal cryptococcal meningitis (CM) were reported in patients treated with another S1P receptor modulator. If CM is suspected, ZEPOSIA should be suspended until cryptococcal infection has been excluded. If CM is diagnosed, appropriate treatment should be initiated.
- Progressive Multifocal Leukoencephalopathy (PML) is an opportunistic viral infection of the brain that typically occurs in patients who are immunocompromised, and that usually leads to death or severe disability. No cases of PML were identified in active-controlled MS clinical trials with ZEPOSIA. PML has been reported in patients treated with S1P receptor modulators and other MS therapies and has been associated with some risk factors. If PML is suspected, withhold ZEPOSIA and perform an appropriate diagnostic evaluation. If confirmed, treatment with ZEPOSIA should be discontinued
- In clinical studies, patients who received ZEPOSIA were not to receive concomitant treatment with antineoplastic, non-corticosteroid immunosuppressive, or immune-modulating therapies used for treatment of MS. Concomitant use of ZEPOSIA with any of these therapies would be expected to increase the risk of immunosuppression. When switching to ZEPOSIA from immunosuppressive medications, consider the duration of their effects and their mode of action to avoid unintended additive immunosuppressive effects
- Use of live attenuated vaccines should be avoided during and for 3 months after treatment with ZEPOSIA. If live attenuated vaccine immunizations are required, administer at least 1 month prior to initiation of ZEPOSIA
Bradyarrhythmia and Atrioventricular Conduction Delays: Since initiation of ZEPOSIA may result in a transient decrease in heart rate and atrioventricular conduction delays, dose titration is recommended to help reduce cardiac effects. Initiation of ZEPOSIA without dose escalation may result in greater decreases in heart rate. If treatment with ZEPOSIA is considered, advice from a cardiologist should be sought for those individuals:
- with significant QT prolongation
- with arrhythmias requiring treatment with Class 1a or III anti-arrhythmic drugs
- with ischemic heart disease, heart failure, history of cardiac arrest or myocardial infarction, cerebrovascular disease, and uncontrolled hypertension
- with a history of Mobitz type II second-degree or higher AV block, sick-sinus syndrome, or sinoatrial heart block
Liver Injury: Elevations of aminotransferases may occur in patients receiving ZEPOSIA. Obtain liver function tests, if not recently available (i.e., within 6 months), before initiation of ZEPOSIA. Patients who develop symptoms suggestive of hepatic dysfunction should have hepatic enzymes checked and ZEPOSIA should be discontinued if significant liver injury is confirmed. Caution should be exercised when using ZEPOSIA in patients with history of significant liver disease
Fetal Risk: There are no adequate and well-controlled studies in pregnant women. Based on animal studies, ZEPOSIA may cause fetal harm. Women of childbearing potential should use effective contraception to avoid pregnancy during treatment and for 3 months after stopping ZEPOSIA
Increased Blood Pressure: Increase in systolic pressure was observed after about 3 months of treatment and persisted throughout treatment. Blood pressure should be monitored during treatment and managed appropriately. Certain foods that may contain very high amounts of tyramine could cause severe hypertension in patients taking ZEPOSIA. Patients should be advised to avoid foods containing a very large amount of tyramine while taking ZEPOSIA
Respiratory Effects: ZEPOSIA may cause a decline in pulmonary function. Spirometric evaluation of respiratory function should be performed during therapy, if clinically indicated
Macular edema: S1P modulators have been associated with an increased risk of macular edema. Patients with a history of uveitis or diabetes mellitus are at increased risk. Patients with a history of these conditions should have an ophthalmic evaluation of the fundus, including the macula, prior to treatment initiation and regular follow-up examinations. An ophthalmic evaluation is recommended in all patients at any time if there is a change in vision. Continued use of ZEPOSIA in patients with macular edema has not been evaluated; potential benefits and risks for the individual patient should be considered if deciding whether ZEPOSIA should be discontinued
Posterior Reversible Encephalopathy Syndrome (PRES): Rare cases of PRES have been reported in patients receiving a S1P receptor modulator. If a ZEPOSIA-treated patient develops unexpected neurological or psychiatric symptoms or any symptom/sign suggestive of an increase in intracranial pressure, a complete physical and neurological examination should be conducted. Symptoms of PRES are usually reversible but may evolve into ischemic stroke or cerebral hemorrhage. Delay in diagnosis and treatment may lead to permanent neurological sequelae. If PRES is suspected, treatment with ZEPOSIA should be discontinued
Unintended Additive Immunosuppressive Effects From Prior Immunosuppressive or Immune-Modulating Drugs: When switching from drugs with prolonged immune effects, the half-life and mode of action of these drugs must be considered to avoid unintended additive immunosuppressive effects while at the same time minimizing risk of disease reactivation. Initiating treatment with ZEPOSIA after treatment with alemtuzumab is not recommended
Severe Increase in Disability After Stopping ZEPOSIA: Severe exacerbation of disease, including disease rebound, has been rarely reported after discontinuation of a S1P receptor modulator. The possibility of severe exacerbation of disease should be considered after stopping ZEPOSIA treatment so patients should be monitored upon discontinuation
Immune System Effects After Stopping ZEPOSIA: After discontinuing ZEPOSIA, the median time for lymphocyte counts to return to the normal range was 30 days with approximately 90% of patients in the normal range within 3 months. Use of immunosuppressants within this period may lead to an additive effect on the immune system, therefore caution should be applied when initiating other drugs 4 weeks after the last dose of ZEPOSIA
Most common Adverse Reactions (≥ 4%): upper respiratory infection, hepatic transaminase elevation, orthostatic hypotension, urinary tract infection, back pain, and hypertension.
For additional safety information, please see the full Prescribing Information and Medication Guide.
1. ZEPOSIA (ozanimod) capsules for oral use. Celgene Corporation. Full prescribing information. 3/2020.
2. National Multiple Sclerosis Society. Treating RMSS. www.nationalmssociety.org/What-is-MS/Types-of-MS/Relapsing-remitting-MS/Treatment. Accessed on April 24, 2020.
3. GILENYA (fingolimod) capsules for oral use. Novartis Pharmaceuticals Corporation. Full prescribing information. 8/2019.
4. MAYZENT (siponimod) tablets for oral use. Novartis Pharmaceuticals Corporation. Full prescribing information. 3/2019.
5. Cohen, JA, Comi, G, Selmaj, KW, et al. Safety and efficacy of ozanimod versus interferon beta-1a in relapsing multiple sclerosis (RADIANCE): a multicenter, randomized, 24-month, phase 3 trial. The Lancet: Neurology. DOI: 10.1016/S1474-4422(19)30238-8.
6. Comi, G, Kappos, L, Selmaj, KW, et at. Safety and efficacy of ozanimod versus interferon beta-1a in relapsing multiple sclerosis (SUNBEAM): a multicenter, randomized, minimum 12-month, phase 3 trial. The Lancet: Neurology. DOI: 10.1016/S1474-4422(19)30239-X.
7. McCann Agency. Pivotal Trials for MS Therapies: ZEPOSIA –2 head-to-head with Active Comparator Based on PIs. March 2020.
ZEPOSIA® is a trademark of Bristol-Myers Squibb Company.
© 2020 Bristol-Myers Squibb Company. All Rights Reserved.
US-ZEP-20-1095 10/20
Paid content by 
Treatment for relapsing forms of multiple sclerosis (MS) is critical to address the disease’s hallmark relapses and brain lesions.2 There are currently over a dozen approved disease-modifying medications, but no one treatment is right for every patient.2
In March 2020, the U.S. Food and Drug Administration (FDA) approved ZEPOSIA® (ozanimod) 0.92 mg, an oral medication taken once daily for the treatment of adults with relapsing forms of MS, including clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease.1
Patients may start ZEPOSIA as soon as the same day it is prescribed
Binding with high affinity to S1P receptors 1 and 5, ZEPOSIA blocks the capacity of lymphocytes to egress from lymph nodes, reducing the number of lymphocytes in peripheral blood.1 The mechanism by which ZEPOSIA exerts therapeutic effects in MS is unknown, but may involve the reduction of lymphocyte migration into the central nervous system.1
ZEPOSIA is the only S1P receptor modulator that offers relapsing forms of MS patients an initiation with no genetic test and no required label-based first-dose observation.1,3,4 An up-titration scheme should be used to reach the maintenance dosage of ZEPOSIA, as a transient decrease in heart rate and atrioventricular conduction delays may occur.1 Before initiation of treatment with ZEPOSIA, all patients require assessments including a recent complete blood count including lymphocyte count (within six months or after discontinuation of prior MS therapy), an ECG to determine whether preexisting conduction abnormalities are present, a recent liver function test (within six months), and consideration of current and prior medications, including vaccinations.1 For patients with a history of uveitis or macular edema, an ophthalmic assessment is required.1
ZEPOSIA is contraindicated in patients who in the last six months experienced myocardial infarction, unstable angina, stroke, transient ischemic attack (TIA), decompensated heart failure requiring hospitalization, or Class III/IV heart failure; patients who have a presence of Mobitz type II second or third-degree atrioventricular (AV) block, sick sinus syndrome, or sino-atrial, unless the patient has a functioning pacemaker; patients with severe untreated sleep apnea; and patients taking a monoamine oxidase inhibitor.1ZEPOSIA is associated with the following Warnings and Precautions: increased risk of infections, bradyarrhythmia and atrioventricular conduction delays, liver injury, fetal risk, increased blood pressure, respiratory effects, macular edema, posterior reversible encephalopathy syndrome, additive immunosuppressive effects from prior immune-modulating treatments, severe increase in disability after stopping ZEPOSIA, and immune system effects after stopping ZEPOSIA.1 Please see Important Safety Information for additional details. The most common adverse reactions (incidence ≥4%) were upper respiratory infection, hepatic transaminase elevation, orthostatic hypotension, urinary tract infection, back pain, and hypertension.1
“There is no one size fits all treatment for patients with relapsing forms of MS, and doctors and patients are still seeking additional therapies that can address the hallmarks of this devastating disease,” said Mary Beth Harler, M.D., senior vice president, head of immunology and fibrosis development, Bristol Myers Squibb. “ZEPOSIA has demonstrated clinical potential in safety and efficacy and may allow patients to begin treatment the same day it is prescribed.”1
Powerful efficacy demonstrated in clinical trials
The ZEPOSIA approval was based on data from the largest, pivotal, head-to-head relapsing forms of MS studies with an active comparator to date: the randomized, Phase 3 SUNBEAM™ (safety and efficacy of ZEPOSIA versus interferon beta-1a in relapsing multiple sclerosis) and RADIANCE™ (safety and efficacy of the selective sphingosine 1-phosphate receptor modulator ZEPOSIA in relapsing multiple sclerosis) Part B clinical trials (N=2699).1,5,6,7 In both trials – as compared to AVONEX® (interferon beta-1a) – ZEPOSIA delivered powerful efficacy as measured by the primary endpoint of annualized relapse rate (ARR):
ZEPOSIA demonstrated a relative reduction in ARR versus AVONEX of 48% at one year and 38% at two years (absolute ARR of 0.18 versus 0.35 and 0.17 versus 0.28, respectively).1,5,6

The majority of patients in both groups experienced zero relapses.1
Proven superiority in reducing brain lesions
Treatment with ZEPOSIA reduced the number of T1-weighted gadolinium-enhanced (GdE) brain lesions more than AVONEX at one year (0.16 vs 0.43), a relative reduction of 63%, and at two years (0.18 vs 0.37), a relative reduction of 53%.1
In addition, the number of new or enlarging T2 lesions was reduced at one year (1.47 vs. 2.84), a relative reduction of 48%, as well as at two years (1.84 versus 3.18), a relative reduction of 42%.1
There was no statistically significant difference in the three-month and six-month confirmed disability progression between ZEPOSIA- and AVONEX- treated patients over two years.1
Comparable safety to AVONEX in overall incidence of adverse events
The overall incidence of adverse reactions experienced by patients for ZEPOSIA vs. AVONEX at one year were 59.8% and 75.5%, respectively, and at two years were 74.7% and 83.0%, respectively.1 ZEPOSIA demonstrated consistently low discontinuation rates due to adverse events versus AVONEX (<3%); at one year discontinuation rates due to adverse events for AVONEX were 3.6% and for ZEPOSIA were 2.9%, at two years discontinuation rates due to adverse events for AVONEX were 4.1% and for ZEPOSIA were 3.0%1 Overall discontinuation rates were <10% versus AVONEX across both trials. At one year discontinuation rates for AVONEX were 8% and for ZEPOSIA were 6%, at two years discontinuation rates for AVONEX were 15% and for ZEPOSIA were 10%.1
ZEPOSIA is contraindicated in patients who in the last six months experienced myocardial infarction, unstable angina, stroke, transient ischemic attack (TIA), decompensated heart failure requiring hospitalization, or Class III/IV heart failure; patients who have a presence of Mobitz type II second or third-degree atrioventricular (AV) block, sick sinus syndrome, or sino-atrial, unless the patient has a functioning pacemaker; patients with severe untreated sleep apnea; and patients taking a monoamine oxidase inhibitor.1 ZEPOSIA is associated with the following Warnings and Precautions: increased risk of infections, bradyarrhythmia and atrioventricular conduction delays, liver injury, fetal risk, increased blood pressure, respiratory effects, macular edema, posterior reversible encephalopathy syndrome, additive immunosuppressive effects from prior immune-modulating treatments, severe increase in disability after stopping ZEPOSIA, and immune system effects after stopping ZEPOSIA.1 Please see Important Safety Information for additional details.1 The most common adverse reactions (incidence ≥4%) were upper respiratory infection, hepatic transaminase elevation, orthostatic hypotension, urinary tract infection, back pain, and hypertension.1
Please visit www.ZEPOSIAHCP.com to learn more.
Indication
ZEPOSIA is indicated for the treatment of relapsing forms of multiple sclerosis (MS), to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults.
IMPORTANT SAFETY INFORMATION1
Contraindications:
- Patients who in the last 6 months, experienced myocardial infarction, unstable angina, stroke, transient ischemic attack (TIA), decompensated heart failure requiring hospitalization, or Class III/IV heart failure or have a presence of Mobitz type II second or third-degree atrioventricular (AV) block, sick sinus syndrome, or sino-atrial, unless the patient has a functioning pacemaker
- Patients with severe untreated sleep apnea
- Patients taking a monoamine oxidase (MAO) inhibitor
Infections: ZEPOSIA may increase the susceptibility to infections. Life-threatening and rare fatal infections have occurred in patients receiving ZEPOSIA. Obtain a recent (i.e., within 6 months or after discontinuation of prior MS therapy) complete blood count (CBC) including lymphocyte count before initiation of ZEPOSIA. Delay initiation of ZEPOSIA in patients with an active infection until the infection is resolved. Consider interruption of treatment with ZEPOSIA if a patient develops a serious infection. Continue monitoring for infections up to 3 months after discontinuing ZEPOSIA
- Herpes zoster was reported as an adverse reaction in ZEPOSIA-treated patients. Herpes simplex encephalitis and varicella zoster meningitis have been reported with sphingosine 1-phosphate (S1P) receptor modulators. Patients without a healthcare professional-confirmed history of varicella (chickenpox), or without documentation of a full course of vaccination against varicella zoster virus (VZV), should be tested for antibodies to VZV before initiating ZEPOSIA. A full course of vaccination for antibody-negative patients with varicella vaccine is recommended prior to commencing treatment with ZEPOSIA
- Cases of fatal cryptococcal meningitis (CM) were reported in patients treated with another S1P receptor modulator. If CM is suspected, ZEPOSIA should be suspended until cryptococcal infection has been excluded. If CM is diagnosed, appropriate treatment should be initiated.
- Progressive Multifocal Leukoencephalopathy (PML) is an opportunistic viral infection of the brain that typically occurs in patients who are immunocompromised, and that usually leads to death or severe disability. No cases of PML were identified in active-controlled MS clinical trials with ZEPOSIA. PML has been reported in patients treated with S1P receptor modulators and other MS therapies and has been associated with some risk factors. If PML is suspected, withhold ZEPOSIA and perform an appropriate diagnostic evaluation. If confirmed, treatment with ZEPOSIA should be discontinued
- In clinical studies, patients who received ZEPOSIA were not to receive concomitant treatment with antineoplastic, non-corticosteroid immunosuppressive, or immune-modulating therapies used for treatment of MS. Concomitant use of ZEPOSIA with any of these therapies would be expected to increase the risk of immunosuppression. When switching to ZEPOSIA from immunosuppressive medications, consider the duration of their effects and their mode of action to avoid unintended additive immunosuppressive effects
- Use of live attenuated vaccines should be avoided during and for 3 months after treatment with ZEPOSIA. If live attenuated vaccine immunizations are required, administer at least 1 month prior to initiation of ZEPOSIA
Bradyarrhythmia and Atrioventricular Conduction Delays: Since initiation of ZEPOSIA may result in a transient decrease in heart rate and atrioventricular conduction delays, dose titration is recommended to help reduce cardiac effects. Initiation of ZEPOSIA without dose escalation may result in greater decreases in heart rate. If treatment with ZEPOSIA is considered, advice from a cardiologist should be sought for those individuals:
- with significant QT prolongation
- with arrhythmias requiring treatment with Class 1a or III anti-arrhythmic drugs
- with ischemic heart disease, heart failure, history of cardiac arrest or myocardial infarction, cerebrovascular disease, and uncontrolled hypertension
- with a history of Mobitz type II second-degree or higher AV block, sick-sinus syndrome, or sinoatrial heart block
Liver Injury: Elevations of aminotransferases may occur in patients receiving ZEPOSIA. Obtain liver function tests, if not recently available (i.e., within 6 months), before initiation of ZEPOSIA. Patients who develop symptoms suggestive of hepatic dysfunction should have hepatic enzymes checked and ZEPOSIA should be discontinued if significant liver injury is confirmed. Caution should be exercised when using ZEPOSIA in patients with history of significant liver disease
Fetal Risk: There are no adequate and well-controlled studies in pregnant women. Based on animal studies, ZEPOSIA may cause fetal harm. Women of childbearing potential should use effective contraception to avoid pregnancy during treatment and for 3 months after stopping ZEPOSIA
Increased Blood Pressure: Increase in systolic pressure was observed after about 3 months of treatment and persisted throughout treatment. Blood pressure should be monitored during treatment and managed appropriately. Certain foods that may contain very high amounts of tyramine could cause severe hypertension in patients taking ZEPOSIA. Patients should be advised to avoid foods containing a very large amount of tyramine while taking ZEPOSIA
Respiratory Effects: ZEPOSIA may cause a decline in pulmonary function. Spirometric evaluation of respiratory function should be performed during therapy, if clinically indicated
Macular edema: S1P modulators have been associated with an increased risk of macular edema. Patients with a history of uveitis or diabetes mellitus are at increased risk. Patients with a history of these conditions should have an ophthalmic evaluation of the fundus, including the macula, prior to treatment initiation and regular follow-up examinations. An ophthalmic evaluation is recommended in all patients at any time if there is a change in vision. Continued use of ZEPOSIA in patients with macular edema has not been evaluated; potential benefits and risks for the individual patient should be considered if deciding whether ZEPOSIA should be discontinued
Posterior Reversible Encephalopathy Syndrome (PRES): Rare cases of PRES have been reported in patients receiving a S1P receptor modulator. If a ZEPOSIA-treated patient develops unexpected neurological or psychiatric symptoms or any symptom/sign suggestive of an increase in intracranial pressure, a complete physical and neurological examination should be conducted. Symptoms of PRES are usually reversible but may evolve into ischemic stroke or cerebral hemorrhage. Delay in diagnosis and treatment may lead to permanent neurological sequelae. If PRES is suspected, treatment with ZEPOSIA should be discontinued
Unintended Additive Immunosuppressive Effects From Prior Immunosuppressive or Immune-Modulating Drugs: When switching from drugs with prolonged immune effects, the half-life and mode of action of these drugs must be considered to avoid unintended additive immunosuppressive effects while at the same time minimizing risk of disease reactivation. Initiating treatment with ZEPOSIA after treatment with alemtuzumab is not recommended
Severe Increase in Disability After Stopping ZEPOSIA: Severe exacerbation of disease, including disease rebound, has been rarely reported after discontinuation of a S1P receptor modulator. The possibility of severe exacerbation of disease should be considered after stopping ZEPOSIA treatment so patients should be monitored upon discontinuation
Immune System Effects After Stopping ZEPOSIA: After discontinuing ZEPOSIA, the median time for lymphocyte counts to return to the normal range was 30 days with approximately 90% of patients in the normal range within 3 months. Use of immunosuppressants within this period may lead to an additive effect on the immune system, therefore caution should be applied when initiating other drugs 4 weeks after the last dose of ZEPOSIA
Most common Adverse Reactions (≥ 4%): upper respiratory infection, hepatic transaminase elevation, orthostatic hypotension, urinary tract infection, back pain, and hypertension.
For additional safety information, please see the full Prescribing Information and Medication Guide.
1. ZEPOSIA (ozanimod) capsules for oral use. Celgene Corporation. Full prescribing information. 3/2020.
2. National Multiple Sclerosis Society. Treating RMSS. www.nationalmssociety.org/What-is-MS/Types-of-MS/Relapsing-remitting-MS/Treatment. Accessed on April 24, 2020.
3. GILENYA (fingolimod) capsules for oral use. Novartis Pharmaceuticals Corporation. Full prescribing information. 8/2019.
4. MAYZENT (siponimod) tablets for oral use. Novartis Pharmaceuticals Corporation. Full prescribing information. 3/2019.
5. Cohen, JA, Comi, G, Selmaj, KW, et al. Safety and efficacy of ozanimod versus interferon beta-1a in relapsing multiple sclerosis (RADIANCE): a multicenter, randomized, 24-month, phase 3 trial. The Lancet: Neurology. DOI: 10.1016/S1474-4422(19)30238-8.
6. Comi, G, Kappos, L, Selmaj, KW, et at. Safety and efficacy of ozanimod versus interferon beta-1a in relapsing multiple sclerosis (SUNBEAM): a multicenter, randomized, minimum 12-month, phase 3 trial. The Lancet: Neurology. DOI: 10.1016/S1474-4422(19)30239-X.
7. McCann Agency. Pivotal Trials for MS Therapies: ZEPOSIA –2 head-to-head with Active Comparator Based on PIs. March 2020.
ZEPOSIA® is a trademark of Bristol-Myers Squibb Company.
© 2020 Bristol-Myers Squibb Company. All Rights Reserved.
US-ZEP-20-1095 10/20