User login
The introduction of amniocentesis in the 1960s brought to prenatal diagnosticians the ability to detect fetal chromosome abnormalities and certain structural defects (including neural tube defects). Since that time, a goal for these practitioners has been the development of effective screening algorithms to better identify women at high risk for detectable fetal abnormalities in concert with the advent of safer and more accessible diagnostic tests, with the eventual aim being the development of a noninvasive prenatal diagnostic test.
Postamniocentesis advancements have included the identification of maternal serum analytes as well as the incorporation of first-trimester ultrasonographic measurements of the fetal nuchal translucency (NT) and nasal bone, all associated with an improved ability to identify women at increased risk for fetal trisomies 21 and 18 as well as some other fetal abnormalities. In addition, targeted ultrasound has greatly improved the ability to detect fetal structural and growth abnormalities in women of all risk levels, although it remains a highly subjective process with considerable inter/intraoperator and equipment variability.
Related article: NIPT is expanding rapidly--but don't throw out that CVS kit just yet! (Update on Obstetrics; Jaimey M. Pauli, MD, and John T. Repke, MD; January 2014)
Noninvasive prenatal screening has the advantages of being noninvasive and carrying no increased risk for fetal loss compared with chorionic villus sampling (CVS) and amniocentesis, which are associated with a small increased risk for pregnancy loss (1/500 to 1/1,500 over baseline risk for loss). However, noninvasive screening is limited compared with diagnostic procedures because it provides only a risk adjustment rather than a definitive diagnostic outcome and is mostly limited to assessment for fetal trisomies 18 and 21.
Targeted ultrasound can identify structural abnormalities associated with other chromosomal, genetic, and genomic abnormalities, but again depends on operator experience, equipment used, maternal habitus, and fetal position. Accordingly, considerable interest has remained in developing a more effective approach for detecting fetal aneuploidy and other fetal abnormalities, including assays that eventually could serve to provide noninvasive prenatal diagnosis.
RECENT ADVANCES BRING US CLOSER TO OUR ULTIMATE GOAL
The recent introduction of circulating cell-free nucleic acids (ccfna) technologies for prenatal screening for common fetal aneuploidies, better known as noninvasive prenatal testing, or NIPT, has presented a far more effective prenatal screening protocol for certain groups of women compared with the aforementioned screening algorithms that rely on measurements of the fetal NT in the late first trimester and maternal serum measurements of analytes in the first and second trimesters.
Currently, four NIPT screening products are available commercially in the United States: MaterniT21 Plus (Sequenom, San Diego, California); Verifi (Illumina, San Diego, California); Harmony Prenatal Test (Ariosa Diagnostics, San Jose, California); and Panorama Prenatal Test (Natera, San Carlos, California). While the technologies and algorithms used by each of the companies differ, they all rely on the premise that 5% to 10% of ccfna in maternal blood are fetal in nature.1 Calculating the ratios of the expected amount of each chromosome-specific nucleic acid to that actually measured in the sample, a prediction of a normal or abnormal complement for that specific chromosome is then made. None of the commercially available tests specifically identify fetal DNA or differentiate fetal from maternal DNA.
Current validation studies have thus far limited the offering of NIPT to women at increased risk for fetal aneuploidy, including those:2–6
- of advanced maternal age
- with a positive conventional screening test
- with abnormal ultrasound results suggestive of aneuploidy, or
- who have had a prior pregnancy with a chromosome aneuploidy found in the NIPT panel.
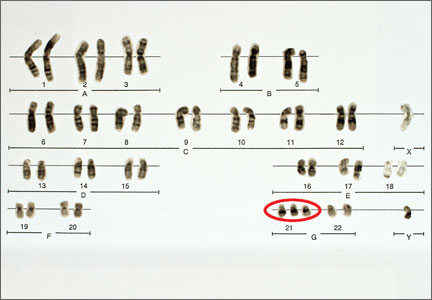
Studies of all available technologies tested on women at increased risk for fetal aneuploidy have thus far shown considerably higher sensitivities and specificities and detection rates for fetal trisomies 21, 18, and 13 than conventional screening algorithms, although detection rates for trisomy 13 are slightly lower than those observed for trisomies 21 and 18.
WE STILL HAVE MANY HURDLES TO LEAP
However, the groups of women at high risk for fetal aneuploidy just outlined represent only a small segment of the community of pregnant women. A multicenter study involving 1,914 women published February 2014 in the New England Journal of Medicine7 showed considerably and significantly lower false-positive rates and higher positive predictive values for the detection of trisomies 21 and 18 by NIPT compared with conventional fetal aneuploidy screening. This study incorporated women at low risk for fetal aneuploidies in the study cohort, although women at high risk (based on the stated range of maternal age) also were included in the cohort. Unfortunately, no information was provided in the report about the percentage of low-risk women among the study participants.
Related articles:
Noninvasive prenatal DNA testing: Who is using it, and how? Audiocast, June 2013
Noninvasive prenatal DNA tests are unproven and costly David A. Carpenter, MD (Comment & Controversy; September 2013)
Another concern about the published accuracy of NIPT clinical assays was recently sounded by Menutti and colleagues.8 The authors cited recent cases of positive NIPT outcomes for fetal trisomies 18 and 13 that were not confirmed by diagnostic testing of the pregnancies in question. The authors pondered whether such cases may reflect a limitation of the positive predictive values attributed to NIPT assays and that such limitations may carry profound inaccuracies in determining the accuracy of such protocols for rare aneuploidies.
While the improved detection rates for NIPT compared with conventional screening are not surprising, guidelines published by the American College of Obstetricians and Gynecologists still do not recommend the use of NIPT for the screening of low-risk women because of insufficient evaluation of ccfna technologies in the screening of such pregnancies.3 This also applies to twin pregnancies, despite preliminary studies showing comparable detection of trisomies 18 and 21 in such pregnancies compared with singleton pregnancies.3,9
There are no direct comparative studies of the four commercially available screening products, thus precluding a robust comparison and determination of the best existing method to use.
SO, WHERE ARE WE WITH NIPT EXACTLY?
The recent introduction of NIPT into routine obstetric care has left many clinicians with a wide range of questions, many of which cannot be answered because of little or no information, robust or otherwise, to formulate an accurate and cogent response. So let’s state what we know based on the available evidence, recognizing that this will likely change, perhaps considerably, in the weeks and months ahead.
NIPT is a far superior approach, compared with conventional screening approaches, to screening for fetal trisomies 21, 18, and 13 in women carrying singleton pregnancies who are at an increased risk for fetal chromosome abnormalities.
In our current understanding of prenatal screening and diagnosis, NIPT does not provide either the comprehensive approach or the diagnostic accuracy associated with CVS and amniocentesis. As such, NIPT is not a suitable replacement for prenatal diagnostic procedures.
However, its application to screening a low-risk population for the common fetal aneuploidies, as well as in twin pregnancies, has been supported by initial studies, and the inclusion of other clinical outcomes—including other chromosome abnormalities, such as X and Y aneuploidies, trisomy 16, and triploidy10,11 and certain genomic abnormalities (eg, 22q deletions)—in the screening algorithm will expand the future clinical applications of NIPT screening.
DOES NIPT CHANGE OUR CONCEPTS OF SCREENING AND DIAGNOSIS?
This question is simple but profound and is perhaps the most important to be asked and addressed. Is a screening algorithm that has a similar sensitivity and specificity to that of CVS and amniocentesis for the most common fetal trisomies in the first and second trimesters sufficient to replace invasive testing for most women? Does the ability to detect fetal genomic abnormalities with microarray analyses of fetal cells obtained by CVS or amniocentesis provide a far greater benefit than that possible with any screening algorithm?
With renewed interest in the cost of health-care screening and diagnosis, we need to consider how comprehensive and accurate our prenatal screening and diagnostic tests should be and whether such improvements are desired or even possible from a clinical or economic viewpoint. In addition, the development of new technologies, such as the capture and analysis of fetal cells in maternal blood, presents the potential for a direct diagnostic fetal assay without the risks of an invasive procedure.
BIAS-FREE COUNSELING CANNOT BE OVERLOOKED
That being said, the current role of NIPT and other screening protocols in obstetric care needs to be clearly communicated to women who are considering their fetal assessment options, with emphasis placed on the capabilities and limitations of prenatal screening (even the newer ccfna-based options), the actual risks associated with invasive testing, and the ability of invasive testing to provide expanded fetal information with the use of microarray analyses.
As it has been from the beginning of prenatal testing in the 1960s, counseling continues to be the most important part of the prenatal screening and diagnostic process and it is needed to facilitate clinical decisions made by women and couples. Counseling must include an accurate communication of the risks, benefits, and limitations of the aforementioned options and issues, and should be provided in a manner that strives to be free of bias, direction, and the personal opinions of the counselor.
In order to provide such counseling, we must remain informed of the ongoing work in the field of prenatal testing, a task that has become more challenging with the rapid release of a considerable amount of new information on prenatal screening technologies over the past 2 years. This will likely continue, and perhaps become even more frenetic, with the expected release of additional information on the clinical applications of ccfna technologies in the near future as well as the development of new technologies applicable for the screening and diagnosis of fetal abnormalities.
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article. Send your letter to: obg@frontlinemedcom.com Please include the city and state in which you practice.
- Lo YM, Corbetta N, Chamberlain PF, et al. Presence of fetal DNA in maternal plasma and serum. Lancet. 1997;350(9076):485–487.
- Ashoor G, Syngelaki A, Wagner M, Birdir C, Nicolaides KH. Chromosome-selective sequencing of maternal plasma cell–free DNA for first-trimester detection of trisomy 21 and trisomy 18. Am J Obstet Gynecol. 2012;206(4):322.e1–e5.
- American College of Obstetricians and Gynecologists Committee on Genetics. Committee Opinion No. 545: Noninvasive prenatal testing for fetal aneuploidy. Obstet Gynecol. 2012;120(6):1532–1534.
- Bianchi DW, Platt LD, Goldberg JD, et al; MatErnal Blood IS Source to Accurately diagnose fetal aneuploidy (MELISSA) Study Group. Genome-wide fetal aneuploidy detection by maternal plasma DNA-sequencing. Obstet Gynecol. 2012;119(5):890–901.
- Palomaki GE, Kloza EM, Lambert-Messerlian GM, et al. DNA sequencing of maternal plasma to detect Down syndrome: An international clinical validation study. Genet Med. 2011;13(11):913–920.
- Palomaki GE, Deciu C, Kloza EM, et al. DNA sequencing of maternal plasma reliably identifies trisomy 18 and trisomy 13 as well as Down syndrome: An international collaborative study. Genet Med. 2012;14(3):296–305.
- Bianchi DW, Parker RL, Wentworth J, et al; CARE Study Group. DNA sequencing versus standard prenatal aneuploidy screening. N Engl J Med. 2014;370(9):799–808.
- Menutti MT, Cherry AM, Morrissette JJ, Dugoff L. Is it time to sound an alarm about false-positive cell-free DNA testing for fetal aneuploidy. Am J Obstet Gynecol. 2013;209(5):415−419.
- Canick JA, Kloza EM, Lambert-Messerlian GM, et al. DNA sequencing of maternal plasma to identify Down syndrome and other trisomies in multiple gestations. Prenat Diagn. 2012;32(8):730–734.
- Nicolaides KH, Syngelaki A, Gil MM, Quezada MS, Zinevich Y. Prenatal detection of fetal triploidy from cell-free DNA testing in maternal blood [published online ahead of print October 10, 2013]. Fetal Diagn Ther.
- Semango-Sprouse C, Banjevic M, Ryan A, et al. SNP-based non-invasive prenatal testing detects sex chromosome aneuploidies with high accuracy. Prenat Diagn. 2013;33(7):643–649.
The introduction of amniocentesis in the 1960s brought to prenatal diagnosticians the ability to detect fetal chromosome abnormalities and certain structural defects (including neural tube defects). Since that time, a goal for these practitioners has been the development of effective screening algorithms to better identify women at high risk for detectable fetal abnormalities in concert with the advent of safer and more accessible diagnostic tests, with the eventual aim being the development of a noninvasive prenatal diagnostic test.
Postamniocentesis advancements have included the identification of maternal serum analytes as well as the incorporation of first-trimester ultrasonographic measurements of the fetal nuchal translucency (NT) and nasal bone, all associated with an improved ability to identify women at increased risk for fetal trisomies 21 and 18 as well as some other fetal abnormalities. In addition, targeted ultrasound has greatly improved the ability to detect fetal structural and growth abnormalities in women of all risk levels, although it remains a highly subjective process with considerable inter/intraoperator and equipment variability.
Related article: NIPT is expanding rapidly--but don't throw out that CVS kit just yet! (Update on Obstetrics; Jaimey M. Pauli, MD, and John T. Repke, MD; January 2014)
Noninvasive prenatal screening has the advantages of being noninvasive and carrying no increased risk for fetal loss compared with chorionic villus sampling (CVS) and amniocentesis, which are associated with a small increased risk for pregnancy loss (1/500 to 1/1,500 over baseline risk for loss). However, noninvasive screening is limited compared with diagnostic procedures because it provides only a risk adjustment rather than a definitive diagnostic outcome and is mostly limited to assessment for fetal trisomies 18 and 21.
Targeted ultrasound can identify structural abnormalities associated with other chromosomal, genetic, and genomic abnormalities, but again depends on operator experience, equipment used, maternal habitus, and fetal position. Accordingly, considerable interest has remained in developing a more effective approach for detecting fetal aneuploidy and other fetal abnormalities, including assays that eventually could serve to provide noninvasive prenatal diagnosis.
RECENT ADVANCES BRING US CLOSER TO OUR ULTIMATE GOAL
The recent introduction of circulating cell-free nucleic acids (ccfna) technologies for prenatal screening for common fetal aneuploidies, better known as noninvasive prenatal testing, or NIPT, has presented a far more effective prenatal screening protocol for certain groups of women compared with the aforementioned screening algorithms that rely on measurements of the fetal NT in the late first trimester and maternal serum measurements of analytes in the first and second trimesters.
Currently, four NIPT screening products are available commercially in the United States: MaterniT21 Plus (Sequenom, San Diego, California); Verifi (Illumina, San Diego, California); Harmony Prenatal Test (Ariosa Diagnostics, San Jose, California); and Panorama Prenatal Test (Natera, San Carlos, California). While the technologies and algorithms used by each of the companies differ, they all rely on the premise that 5% to 10% of ccfna in maternal blood are fetal in nature.1 Calculating the ratios of the expected amount of each chromosome-specific nucleic acid to that actually measured in the sample, a prediction of a normal or abnormal complement for that specific chromosome is then made. None of the commercially available tests specifically identify fetal DNA or differentiate fetal from maternal DNA.
Current validation studies have thus far limited the offering of NIPT to women at increased risk for fetal aneuploidy, including those:2–6
- of advanced maternal age
- with a positive conventional screening test
- with abnormal ultrasound results suggestive of aneuploidy, or
- who have had a prior pregnancy with a chromosome aneuploidy found in the NIPT panel.
Studies of all available technologies tested on women at increased risk for fetal aneuploidy have thus far shown considerably higher sensitivities and specificities and detection rates for fetal trisomies 21, 18, and 13 than conventional screening algorithms, although detection rates for trisomy 13 are slightly lower than those observed for trisomies 21 and 18.
WE STILL HAVE MANY HURDLES TO LEAP
However, the groups of women at high risk for fetal aneuploidy just outlined represent only a small segment of the community of pregnant women. A multicenter study involving 1,914 women published February 2014 in the New England Journal of Medicine7 showed considerably and significantly lower false-positive rates and higher positive predictive values for the detection of trisomies 21 and 18 by NIPT compared with conventional fetal aneuploidy screening. This study incorporated women at low risk for fetal aneuploidies in the study cohort, although women at high risk (based on the stated range of maternal age) also were included in the cohort. Unfortunately, no information was provided in the report about the percentage of low-risk women among the study participants.
Related articles:
Noninvasive prenatal DNA testing: Who is using it, and how? Audiocast, June 2013
Noninvasive prenatal DNA tests are unproven and costly David A. Carpenter, MD (Comment & Controversy; September 2013)
Another concern about the published accuracy of NIPT clinical assays was recently sounded by Menutti and colleagues.8 The authors cited recent cases of positive NIPT outcomes for fetal trisomies 18 and 13 that were not confirmed by diagnostic testing of the pregnancies in question. The authors pondered whether such cases may reflect a limitation of the positive predictive values attributed to NIPT assays and that such limitations may carry profound inaccuracies in determining the accuracy of such protocols for rare aneuploidies.
While the improved detection rates for NIPT compared with conventional screening are not surprising, guidelines published by the American College of Obstetricians and Gynecologists still do not recommend the use of NIPT for the screening of low-risk women because of insufficient evaluation of ccfna technologies in the screening of such pregnancies.3 This also applies to twin pregnancies, despite preliminary studies showing comparable detection of trisomies 18 and 21 in such pregnancies compared with singleton pregnancies.3,9
There are no direct comparative studies of the four commercially available screening products, thus precluding a robust comparison and determination of the best existing method to use.
SO, WHERE ARE WE WITH NIPT EXACTLY?
The recent introduction of NIPT into routine obstetric care has left many clinicians with a wide range of questions, many of which cannot be answered because of little or no information, robust or otherwise, to formulate an accurate and cogent response. So let’s state what we know based on the available evidence, recognizing that this will likely change, perhaps considerably, in the weeks and months ahead.
NIPT is a far superior approach, compared with conventional screening approaches, to screening for fetal trisomies 21, 18, and 13 in women carrying singleton pregnancies who are at an increased risk for fetal chromosome abnormalities.
In our current understanding of prenatal screening and diagnosis, NIPT does not provide either the comprehensive approach or the diagnostic accuracy associated with CVS and amniocentesis. As such, NIPT is not a suitable replacement for prenatal diagnostic procedures.
However, its application to screening a low-risk population for the common fetal aneuploidies, as well as in twin pregnancies, has been supported by initial studies, and the inclusion of other clinical outcomes—including other chromosome abnormalities, such as X and Y aneuploidies, trisomy 16, and triploidy10,11 and certain genomic abnormalities (eg, 22q deletions)—in the screening algorithm will expand the future clinical applications of NIPT screening.
DOES NIPT CHANGE OUR CONCEPTS OF SCREENING AND DIAGNOSIS?
This question is simple but profound and is perhaps the most important to be asked and addressed. Is a screening algorithm that has a similar sensitivity and specificity to that of CVS and amniocentesis for the most common fetal trisomies in the first and second trimesters sufficient to replace invasive testing for most women? Does the ability to detect fetal genomic abnormalities with microarray analyses of fetal cells obtained by CVS or amniocentesis provide a far greater benefit than that possible with any screening algorithm?
With renewed interest in the cost of health-care screening and diagnosis, we need to consider how comprehensive and accurate our prenatal screening and diagnostic tests should be and whether such improvements are desired or even possible from a clinical or economic viewpoint. In addition, the development of new technologies, such as the capture and analysis of fetal cells in maternal blood, presents the potential for a direct diagnostic fetal assay without the risks of an invasive procedure.
BIAS-FREE COUNSELING CANNOT BE OVERLOOKED
That being said, the current role of NIPT and other screening protocols in obstetric care needs to be clearly communicated to women who are considering their fetal assessment options, with emphasis placed on the capabilities and limitations of prenatal screening (even the newer ccfna-based options), the actual risks associated with invasive testing, and the ability of invasive testing to provide expanded fetal information with the use of microarray analyses.
As it has been from the beginning of prenatal testing in the 1960s, counseling continues to be the most important part of the prenatal screening and diagnostic process and it is needed to facilitate clinical decisions made by women and couples. Counseling must include an accurate communication of the risks, benefits, and limitations of the aforementioned options and issues, and should be provided in a manner that strives to be free of bias, direction, and the personal opinions of the counselor.
In order to provide such counseling, we must remain informed of the ongoing work in the field of prenatal testing, a task that has become more challenging with the rapid release of a considerable amount of new information on prenatal screening technologies over the past 2 years. This will likely continue, and perhaps become even more frenetic, with the expected release of additional information on the clinical applications of ccfna technologies in the near future as well as the development of new technologies applicable for the screening and diagnosis of fetal abnormalities.
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article. Send your letter to: obg@frontlinemedcom.com Please include the city and state in which you practice.
The introduction of amniocentesis in the 1960s brought to prenatal diagnosticians the ability to detect fetal chromosome abnormalities and certain structural defects (including neural tube defects). Since that time, a goal for these practitioners has been the development of effective screening algorithms to better identify women at high risk for detectable fetal abnormalities in concert with the advent of safer and more accessible diagnostic tests, with the eventual aim being the development of a noninvasive prenatal diagnostic test.
Postamniocentesis advancements have included the identification of maternal serum analytes as well as the incorporation of first-trimester ultrasonographic measurements of the fetal nuchal translucency (NT) and nasal bone, all associated with an improved ability to identify women at increased risk for fetal trisomies 21 and 18 as well as some other fetal abnormalities. In addition, targeted ultrasound has greatly improved the ability to detect fetal structural and growth abnormalities in women of all risk levels, although it remains a highly subjective process with considerable inter/intraoperator and equipment variability.
Related article: NIPT is expanding rapidly--but don't throw out that CVS kit just yet! (Update on Obstetrics; Jaimey M. Pauli, MD, and John T. Repke, MD; January 2014)
Noninvasive prenatal screening has the advantages of being noninvasive and carrying no increased risk for fetal loss compared with chorionic villus sampling (CVS) and amniocentesis, which are associated with a small increased risk for pregnancy loss (1/500 to 1/1,500 over baseline risk for loss). However, noninvasive screening is limited compared with diagnostic procedures because it provides only a risk adjustment rather than a definitive diagnostic outcome and is mostly limited to assessment for fetal trisomies 18 and 21.
Targeted ultrasound can identify structural abnormalities associated with other chromosomal, genetic, and genomic abnormalities, but again depends on operator experience, equipment used, maternal habitus, and fetal position. Accordingly, considerable interest has remained in developing a more effective approach for detecting fetal aneuploidy and other fetal abnormalities, including assays that eventually could serve to provide noninvasive prenatal diagnosis.
RECENT ADVANCES BRING US CLOSER TO OUR ULTIMATE GOAL
The recent introduction of circulating cell-free nucleic acids (ccfna) technologies for prenatal screening for common fetal aneuploidies, better known as noninvasive prenatal testing, or NIPT, has presented a far more effective prenatal screening protocol for certain groups of women compared with the aforementioned screening algorithms that rely on measurements of the fetal NT in the late first trimester and maternal serum measurements of analytes in the first and second trimesters.
Currently, four NIPT screening products are available commercially in the United States: MaterniT21 Plus (Sequenom, San Diego, California); Verifi (Illumina, San Diego, California); Harmony Prenatal Test (Ariosa Diagnostics, San Jose, California); and Panorama Prenatal Test (Natera, San Carlos, California). While the technologies and algorithms used by each of the companies differ, they all rely on the premise that 5% to 10% of ccfna in maternal blood are fetal in nature.1 Calculating the ratios of the expected amount of each chromosome-specific nucleic acid to that actually measured in the sample, a prediction of a normal or abnormal complement for that specific chromosome is then made. None of the commercially available tests specifically identify fetal DNA or differentiate fetal from maternal DNA.
Current validation studies have thus far limited the offering of NIPT to women at increased risk for fetal aneuploidy, including those:2–6
- of advanced maternal age
- with a positive conventional screening test
- with abnormal ultrasound results suggestive of aneuploidy, or
- who have had a prior pregnancy with a chromosome aneuploidy found in the NIPT panel.
Studies of all available technologies tested on women at increased risk for fetal aneuploidy have thus far shown considerably higher sensitivities and specificities and detection rates for fetal trisomies 21, 18, and 13 than conventional screening algorithms, although detection rates for trisomy 13 are slightly lower than those observed for trisomies 21 and 18.
WE STILL HAVE MANY HURDLES TO LEAP
However, the groups of women at high risk for fetal aneuploidy just outlined represent only a small segment of the community of pregnant women. A multicenter study involving 1,914 women published February 2014 in the New England Journal of Medicine7 showed considerably and significantly lower false-positive rates and higher positive predictive values for the detection of trisomies 21 and 18 by NIPT compared with conventional fetal aneuploidy screening. This study incorporated women at low risk for fetal aneuploidies in the study cohort, although women at high risk (based on the stated range of maternal age) also were included in the cohort. Unfortunately, no information was provided in the report about the percentage of low-risk women among the study participants.
Related articles:
Noninvasive prenatal DNA testing: Who is using it, and how? Audiocast, June 2013
Noninvasive prenatal DNA tests are unproven and costly David A. Carpenter, MD (Comment & Controversy; September 2013)
Another concern about the published accuracy of NIPT clinical assays was recently sounded by Menutti and colleagues.8 The authors cited recent cases of positive NIPT outcomes for fetal trisomies 18 and 13 that were not confirmed by diagnostic testing of the pregnancies in question. The authors pondered whether such cases may reflect a limitation of the positive predictive values attributed to NIPT assays and that such limitations may carry profound inaccuracies in determining the accuracy of such protocols for rare aneuploidies.
While the improved detection rates for NIPT compared with conventional screening are not surprising, guidelines published by the American College of Obstetricians and Gynecologists still do not recommend the use of NIPT for the screening of low-risk women because of insufficient evaluation of ccfna technologies in the screening of such pregnancies.3 This also applies to twin pregnancies, despite preliminary studies showing comparable detection of trisomies 18 and 21 in such pregnancies compared with singleton pregnancies.3,9
There are no direct comparative studies of the four commercially available screening products, thus precluding a robust comparison and determination of the best existing method to use.
SO, WHERE ARE WE WITH NIPT EXACTLY?
The recent introduction of NIPT into routine obstetric care has left many clinicians with a wide range of questions, many of which cannot be answered because of little or no information, robust or otherwise, to formulate an accurate and cogent response. So let’s state what we know based on the available evidence, recognizing that this will likely change, perhaps considerably, in the weeks and months ahead.
NIPT is a far superior approach, compared with conventional screening approaches, to screening for fetal trisomies 21, 18, and 13 in women carrying singleton pregnancies who are at an increased risk for fetal chromosome abnormalities.
In our current understanding of prenatal screening and diagnosis, NIPT does not provide either the comprehensive approach or the diagnostic accuracy associated with CVS and amniocentesis. As such, NIPT is not a suitable replacement for prenatal diagnostic procedures.
However, its application to screening a low-risk population for the common fetal aneuploidies, as well as in twin pregnancies, has been supported by initial studies, and the inclusion of other clinical outcomes—including other chromosome abnormalities, such as X and Y aneuploidies, trisomy 16, and triploidy10,11 and certain genomic abnormalities (eg, 22q deletions)—in the screening algorithm will expand the future clinical applications of NIPT screening.
DOES NIPT CHANGE OUR CONCEPTS OF SCREENING AND DIAGNOSIS?
This question is simple but profound and is perhaps the most important to be asked and addressed. Is a screening algorithm that has a similar sensitivity and specificity to that of CVS and amniocentesis for the most common fetal trisomies in the first and second trimesters sufficient to replace invasive testing for most women? Does the ability to detect fetal genomic abnormalities with microarray analyses of fetal cells obtained by CVS or amniocentesis provide a far greater benefit than that possible with any screening algorithm?
With renewed interest in the cost of health-care screening and diagnosis, we need to consider how comprehensive and accurate our prenatal screening and diagnostic tests should be and whether such improvements are desired or even possible from a clinical or economic viewpoint. In addition, the development of new technologies, such as the capture and analysis of fetal cells in maternal blood, presents the potential for a direct diagnostic fetal assay without the risks of an invasive procedure.
BIAS-FREE COUNSELING CANNOT BE OVERLOOKED
That being said, the current role of NIPT and other screening protocols in obstetric care needs to be clearly communicated to women who are considering their fetal assessment options, with emphasis placed on the capabilities and limitations of prenatal screening (even the newer ccfna-based options), the actual risks associated with invasive testing, and the ability of invasive testing to provide expanded fetal information with the use of microarray analyses.
As it has been from the beginning of prenatal testing in the 1960s, counseling continues to be the most important part of the prenatal screening and diagnostic process and it is needed to facilitate clinical decisions made by women and couples. Counseling must include an accurate communication of the risks, benefits, and limitations of the aforementioned options and issues, and should be provided in a manner that strives to be free of bias, direction, and the personal opinions of the counselor.
In order to provide such counseling, we must remain informed of the ongoing work in the field of prenatal testing, a task that has become more challenging with the rapid release of a considerable amount of new information on prenatal screening technologies over the past 2 years. This will likely continue, and perhaps become even more frenetic, with the expected release of additional information on the clinical applications of ccfna technologies in the near future as well as the development of new technologies applicable for the screening and diagnosis of fetal abnormalities.
WE WANT TO HEAR FROM YOU!
Share your thoughts on this article. Send your letter to: obg@frontlinemedcom.com Please include the city and state in which you practice.
- Lo YM, Corbetta N, Chamberlain PF, et al. Presence of fetal DNA in maternal plasma and serum. Lancet. 1997;350(9076):485–487.
- Ashoor G, Syngelaki A, Wagner M, Birdir C, Nicolaides KH. Chromosome-selective sequencing of maternal plasma cell–free DNA for first-trimester detection of trisomy 21 and trisomy 18. Am J Obstet Gynecol. 2012;206(4):322.e1–e5.
- American College of Obstetricians and Gynecologists Committee on Genetics. Committee Opinion No. 545: Noninvasive prenatal testing for fetal aneuploidy. Obstet Gynecol. 2012;120(6):1532–1534.
- Bianchi DW, Platt LD, Goldberg JD, et al; MatErnal Blood IS Source to Accurately diagnose fetal aneuploidy (MELISSA) Study Group. Genome-wide fetal aneuploidy detection by maternal plasma DNA-sequencing. Obstet Gynecol. 2012;119(5):890–901.
- Palomaki GE, Kloza EM, Lambert-Messerlian GM, et al. DNA sequencing of maternal plasma to detect Down syndrome: An international clinical validation study. Genet Med. 2011;13(11):913–920.
- Palomaki GE, Deciu C, Kloza EM, et al. DNA sequencing of maternal plasma reliably identifies trisomy 18 and trisomy 13 as well as Down syndrome: An international collaborative study. Genet Med. 2012;14(3):296–305.
- Bianchi DW, Parker RL, Wentworth J, et al; CARE Study Group. DNA sequencing versus standard prenatal aneuploidy screening. N Engl J Med. 2014;370(9):799–808.
- Menutti MT, Cherry AM, Morrissette JJ, Dugoff L. Is it time to sound an alarm about false-positive cell-free DNA testing for fetal aneuploidy. Am J Obstet Gynecol. 2013;209(5):415−419.
- Canick JA, Kloza EM, Lambert-Messerlian GM, et al. DNA sequencing of maternal plasma to identify Down syndrome and other trisomies in multiple gestations. Prenat Diagn. 2012;32(8):730–734.
- Nicolaides KH, Syngelaki A, Gil MM, Quezada MS, Zinevich Y. Prenatal detection of fetal triploidy from cell-free DNA testing in maternal blood [published online ahead of print October 10, 2013]. Fetal Diagn Ther.
- Semango-Sprouse C, Banjevic M, Ryan A, et al. SNP-based non-invasive prenatal testing detects sex chromosome aneuploidies with high accuracy. Prenat Diagn. 2013;33(7):643–649.
- Lo YM, Corbetta N, Chamberlain PF, et al. Presence of fetal DNA in maternal plasma and serum. Lancet. 1997;350(9076):485–487.
- Ashoor G, Syngelaki A, Wagner M, Birdir C, Nicolaides KH. Chromosome-selective sequencing of maternal plasma cell–free DNA for first-trimester detection of trisomy 21 and trisomy 18. Am J Obstet Gynecol. 2012;206(4):322.e1–e5.
- American College of Obstetricians and Gynecologists Committee on Genetics. Committee Opinion No. 545: Noninvasive prenatal testing for fetal aneuploidy. Obstet Gynecol. 2012;120(6):1532–1534.
- Bianchi DW, Platt LD, Goldberg JD, et al; MatErnal Blood IS Source to Accurately diagnose fetal aneuploidy (MELISSA) Study Group. Genome-wide fetal aneuploidy detection by maternal plasma DNA-sequencing. Obstet Gynecol. 2012;119(5):890–901.
- Palomaki GE, Kloza EM, Lambert-Messerlian GM, et al. DNA sequencing of maternal plasma to detect Down syndrome: An international clinical validation study. Genet Med. 2011;13(11):913–920.
- Palomaki GE, Deciu C, Kloza EM, et al. DNA sequencing of maternal plasma reliably identifies trisomy 18 and trisomy 13 as well as Down syndrome: An international collaborative study. Genet Med. 2012;14(3):296–305.
- Bianchi DW, Parker RL, Wentworth J, et al; CARE Study Group. DNA sequencing versus standard prenatal aneuploidy screening. N Engl J Med. 2014;370(9):799–808.
- Menutti MT, Cherry AM, Morrissette JJ, Dugoff L. Is it time to sound an alarm about false-positive cell-free DNA testing for fetal aneuploidy. Am J Obstet Gynecol. 2013;209(5):415−419.
- Canick JA, Kloza EM, Lambert-Messerlian GM, et al. DNA sequencing of maternal plasma to identify Down syndrome and other trisomies in multiple gestations. Prenat Diagn. 2012;32(8):730–734.
- Nicolaides KH, Syngelaki A, Gil MM, Quezada MS, Zinevich Y. Prenatal detection of fetal triploidy from cell-free DNA testing in maternal blood [published online ahead of print October 10, 2013]. Fetal Diagn Ther.
- Semango-Sprouse C, Banjevic M, Ryan A, et al. SNP-based non-invasive prenatal testing detects sex chromosome aneuploidies with high accuracy. Prenat Diagn. 2013;33(7):643–649.