User login
PARIS – Fewer than half of commercial drivers who received implantable cardioverter-defibrillators (ICDs) recalled being told they should never drive professionally again, according to a recent Danish survey. Further, about a third of patients overall reported that they began driving soon after they received an ICD, during the period when guidelines recommend refraining from driving.
“These devices, they save lives – so what’s not to like?” lead investigator Jenny Bjerre, MD, asked at the annual congress of the European Society of Cardiology. “Well, if you are a patient qualifying for an ICD, you also automatically qualify for some driving restrictions.” These are put in place because of the concern for an arrhythmia causing a loss of consciousness behind the wheel, she said.
A European consensus statement calls for a 3-month driving moratorium when an ICD is implanted for secondary prevention or after an appropriate ICD shock, and a 4-week restriction when an ICD is placed for primary prevention. All these restrictions apply to personal driver’s licenses; anyone with an ICD is permanently restricted from commercial driving according to the consensus statement, said Dr. Bjerre, of the University Hospital, Copenhagen.
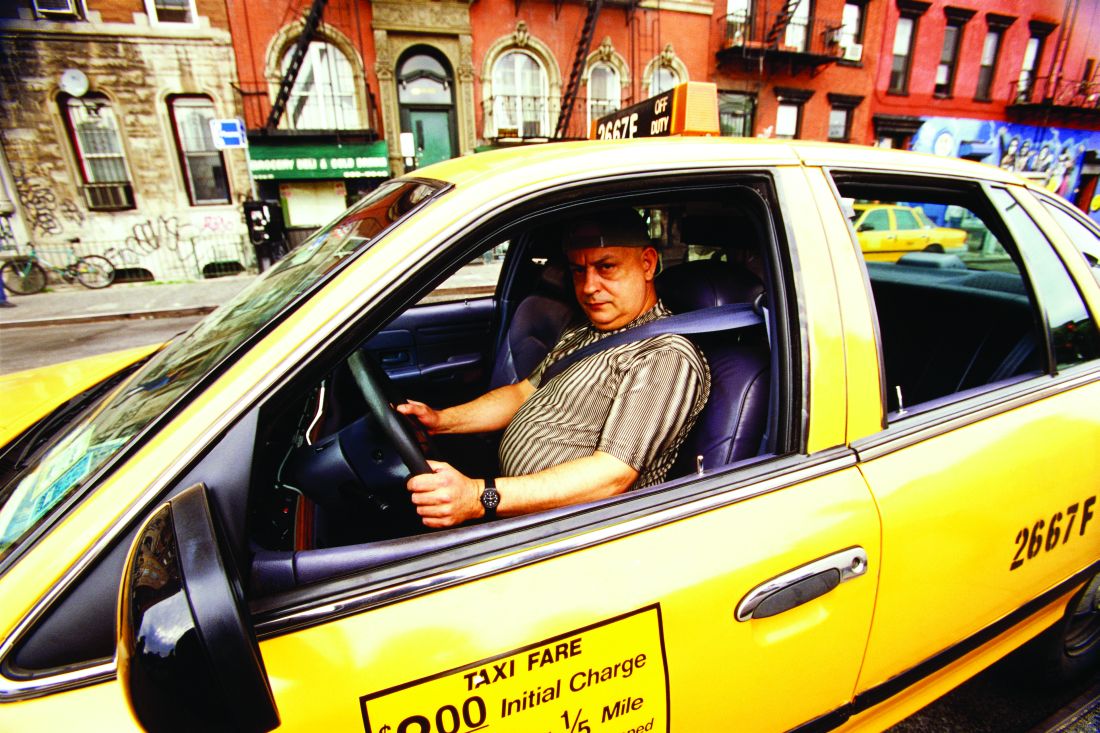
“As you can imagine, these restrictions are not that popular with the patients,” she said. She related the story of a patient, a taxi driver who had returned to a full range of physically taxing activities after his ICD implantation, but whose livelihood had been taken away from him.
Dr. Bjerre said she sought to understand the perspective of this patient, who said, “Sometimes I wish I hadn’t been resuscitated!” She saw that the loss of freedom and a meaningful occupation had profoundly affected the daily life of this patient, and she became curious about adherence to driving restrictions in patients with ICDs.
Using the nationwide Danish medical record database, Dr. Bjerre and her colleagues looked at a nationwide cohort of ICD patients to see they remembered hearing about restrictions on personal and commercial driving activities after ICD implantation. They also investigated adherence to restrictions, and sought to identify what factors were associated with nonadherence.
The questionnaire developed by Dr. Bjerre and her colleagues was made available to the ICD cohort both electronically and in a paper version. Questionnaires received were linked with a variety of nationwide registries through each participant’s unique national identification number, she explained. They obtained information about comorbidities, pharmacotherapies, and socioeconomic status. Not only did this linkage give more precise and complete data than would a questionnaire alone, but it also allowed the investigators to see how responders differed from nonresponders – important in questionnaire research, said Dr. Bjerre.
The investigators were able to locate and distribute questionnaires to a total of 3,913 living adults who had received first-time ICDs during the 3-year study period. In the end, even after excluding 31 responses for missing data, 2,741 responses were used for analysis – a response rate of over 70%.
The median age of respondents was 67, and 83% were male. About half – 46% – of respondents had an ICD implanted for primary prevention. Compared with those who did respond, said Dr. Bjerre, the nonresponders “were younger, sicker, more likely to be female, had lower socioeconomic status, and were less likely to be on guideline-directed therapy.”
Over 90% of respondents held a private driver’s license at the time of their ICD implantation, and just 7% were actively using a commercial license prior to implantation. Participants had a variety of commercial driving occupations, including driving trucks, buses, and taxis.
“Only 43% of primary prevention patients and 64% of secondary prevention patients stated that they had been informed about any driving restrictions,” said Dr. Bjerre. The figure was slightly better for patients after an ICD shock was delivered – 72% of these patients recalled hearing about driving restrictions.
“Among professional drivers – who are never supposed to drive again – only 45% said they had been informed about any professional driving restrictions,” she added.
What did patients report about their actual driving behaviors? Of patients receiving an ICD for primary prevention, 34% resumed driving within one week of ICD implantation. For those receiving an ICD for secondary prevention and those who had received an appropriate ICD shock, 43% and 30%, respectively, began driving before the recommended 3 months had elapsed.
The driving behavior of those with commercial licenses didn’t differ from the cohort as a whole: 35% of this group had resumed commercial driving.
In all the study’s subgroups, nonadherence to driving restrictions was more likely if the participant didn’t recall having been informed of the restrictions, with an odds ratio (OR) of 3.34 for nonadherence. However, noted Dr. Bjerre, at least 20% of patients in all subgroups who said they’d been told not to drive still resumed driving in contravention of restrictions. “So it seems that information can’t explain everything,” she said.
Additional predictors of nonadherence included male sex, with an OR of 1.53, being the only driver in the household (OR 1.29), and being at least 60 years old (OR, 1.20). Those receiving an ICD for secondary prevention had an OR of 2.20 for nonadherence, as well.
The study had a large cohort of real-life ICD patients and the response rate was high, said Dr. Bjerre. However, there was a risk of recall bias; additionally, nonresponders differed from responders, limiting full generalizability of the data. Finally, she observed that participants may have given the answers they thought were socially desirable.
“I want to get back to our friend the taxi driver,” who was adherent to restrictions, but who kept wanting to know what the actual chances were that he’d harm someone if he resumed driving. Realizing she couldn’t give him a very precise answer, Dr. Bjerre concluded, “I do think we owe it to our patients to provide more evidence on the absolute risk of traffic accidents in these patients.”
Dr. Bjerre reported that she had no conflicts of interest.
koakes@mdedge.com
PARIS – Fewer than half of commercial drivers who received implantable cardioverter-defibrillators (ICDs) recalled being told they should never drive professionally again, according to a recent Danish survey. Further, about a third of patients overall reported that they began driving soon after they received an ICD, during the period when guidelines recommend refraining from driving.
“These devices, they save lives – so what’s not to like?” lead investigator Jenny Bjerre, MD, asked at the annual congress of the European Society of Cardiology. “Well, if you are a patient qualifying for an ICD, you also automatically qualify for some driving restrictions.” These are put in place because of the concern for an arrhythmia causing a loss of consciousness behind the wheel, she said.
A European consensus statement calls for a 3-month driving moratorium when an ICD is implanted for secondary prevention or after an appropriate ICD shock, and a 4-week restriction when an ICD is placed for primary prevention. All these restrictions apply to personal driver’s licenses; anyone with an ICD is permanently restricted from commercial driving according to the consensus statement, said Dr. Bjerre, of the University Hospital, Copenhagen.
“As you can imagine, these restrictions are not that popular with the patients,” she said. She related the story of a patient, a taxi driver who had returned to a full range of physically taxing activities after his ICD implantation, but whose livelihood had been taken away from him.
Dr. Bjerre said she sought to understand the perspective of this patient, who said, “Sometimes I wish I hadn’t been resuscitated!” She saw that the loss of freedom and a meaningful occupation had profoundly affected the daily life of this patient, and she became curious about adherence to driving restrictions in patients with ICDs.
Using the nationwide Danish medical record database, Dr. Bjerre and her colleagues looked at a nationwide cohort of ICD patients to see they remembered hearing about restrictions on personal and commercial driving activities after ICD implantation. They also investigated adherence to restrictions, and sought to identify what factors were associated with nonadherence.
The questionnaire developed by Dr. Bjerre and her colleagues was made available to the ICD cohort both electronically and in a paper version. Questionnaires received were linked with a variety of nationwide registries through each participant’s unique national identification number, she explained. They obtained information about comorbidities, pharmacotherapies, and socioeconomic status. Not only did this linkage give more precise and complete data than would a questionnaire alone, but it also allowed the investigators to see how responders differed from nonresponders – important in questionnaire research, said Dr. Bjerre.
The investigators were able to locate and distribute questionnaires to a total of 3,913 living adults who had received first-time ICDs during the 3-year study period. In the end, even after excluding 31 responses for missing data, 2,741 responses were used for analysis – a response rate of over 70%.
The median age of respondents was 67, and 83% were male. About half – 46% – of respondents had an ICD implanted for primary prevention. Compared with those who did respond, said Dr. Bjerre, the nonresponders “were younger, sicker, more likely to be female, had lower socioeconomic status, and were less likely to be on guideline-directed therapy.”
Over 90% of respondents held a private driver’s license at the time of their ICD implantation, and just 7% were actively using a commercial license prior to implantation. Participants had a variety of commercial driving occupations, including driving trucks, buses, and taxis.
“Only 43% of primary prevention patients and 64% of secondary prevention patients stated that they had been informed about any driving restrictions,” said Dr. Bjerre. The figure was slightly better for patients after an ICD shock was delivered – 72% of these patients recalled hearing about driving restrictions.
“Among professional drivers – who are never supposed to drive again – only 45% said they had been informed about any professional driving restrictions,” she added.
What did patients report about their actual driving behaviors? Of patients receiving an ICD for primary prevention, 34% resumed driving within one week of ICD implantation. For those receiving an ICD for secondary prevention and those who had received an appropriate ICD shock, 43% and 30%, respectively, began driving before the recommended 3 months had elapsed.
The driving behavior of those with commercial licenses didn’t differ from the cohort as a whole: 35% of this group had resumed commercial driving.
In all the study’s subgroups, nonadherence to driving restrictions was more likely if the participant didn’t recall having been informed of the restrictions, with an odds ratio (OR) of 3.34 for nonadherence. However, noted Dr. Bjerre, at least 20% of patients in all subgroups who said they’d been told not to drive still resumed driving in contravention of restrictions. “So it seems that information can’t explain everything,” she said.
Additional predictors of nonadherence included male sex, with an OR of 1.53, being the only driver in the household (OR 1.29), and being at least 60 years old (OR, 1.20). Those receiving an ICD for secondary prevention had an OR of 2.20 for nonadherence, as well.
The study had a large cohort of real-life ICD patients and the response rate was high, said Dr. Bjerre. However, there was a risk of recall bias; additionally, nonresponders differed from responders, limiting full generalizability of the data. Finally, she observed that participants may have given the answers they thought were socially desirable.
“I want to get back to our friend the taxi driver,” who was adherent to restrictions, but who kept wanting to know what the actual chances were that he’d harm someone if he resumed driving. Realizing she couldn’t give him a very precise answer, Dr. Bjerre concluded, “I do think we owe it to our patients to provide more evidence on the absolute risk of traffic accidents in these patients.”
Dr. Bjerre reported that she had no conflicts of interest.
koakes@mdedge.com
PARIS – Fewer than half of commercial drivers who received implantable cardioverter-defibrillators (ICDs) recalled being told they should never drive professionally again, according to a recent Danish survey. Further, about a third of patients overall reported that they began driving soon after they received an ICD, during the period when guidelines recommend refraining from driving.
“These devices, they save lives – so what’s not to like?” lead investigator Jenny Bjerre, MD, asked at the annual congress of the European Society of Cardiology. “Well, if you are a patient qualifying for an ICD, you also automatically qualify for some driving restrictions.” These are put in place because of the concern for an arrhythmia causing a loss of consciousness behind the wheel, she said.
A European consensus statement calls for a 3-month driving moratorium when an ICD is implanted for secondary prevention or after an appropriate ICD shock, and a 4-week restriction when an ICD is placed for primary prevention. All these restrictions apply to personal driver’s licenses; anyone with an ICD is permanently restricted from commercial driving according to the consensus statement, said Dr. Bjerre, of the University Hospital, Copenhagen.
“As you can imagine, these restrictions are not that popular with the patients,” she said. She related the story of a patient, a taxi driver who had returned to a full range of physically taxing activities after his ICD implantation, but whose livelihood had been taken away from him.
Dr. Bjerre said she sought to understand the perspective of this patient, who said, “Sometimes I wish I hadn’t been resuscitated!” She saw that the loss of freedom and a meaningful occupation had profoundly affected the daily life of this patient, and she became curious about adherence to driving restrictions in patients with ICDs.
Using the nationwide Danish medical record database, Dr. Bjerre and her colleagues looked at a nationwide cohort of ICD patients to see they remembered hearing about restrictions on personal and commercial driving activities after ICD implantation. They also investigated adherence to restrictions, and sought to identify what factors were associated with nonadherence.
The questionnaire developed by Dr. Bjerre and her colleagues was made available to the ICD cohort both electronically and in a paper version. Questionnaires received were linked with a variety of nationwide registries through each participant’s unique national identification number, she explained. They obtained information about comorbidities, pharmacotherapies, and socioeconomic status. Not only did this linkage give more precise and complete data than would a questionnaire alone, but it also allowed the investigators to see how responders differed from nonresponders – important in questionnaire research, said Dr. Bjerre.
The investigators were able to locate and distribute questionnaires to a total of 3,913 living adults who had received first-time ICDs during the 3-year study period. In the end, even after excluding 31 responses for missing data, 2,741 responses were used for analysis – a response rate of over 70%.
The median age of respondents was 67, and 83% were male. About half – 46% – of respondents had an ICD implanted for primary prevention. Compared with those who did respond, said Dr. Bjerre, the nonresponders “were younger, sicker, more likely to be female, had lower socioeconomic status, and were less likely to be on guideline-directed therapy.”
Over 90% of respondents held a private driver’s license at the time of their ICD implantation, and just 7% were actively using a commercial license prior to implantation. Participants had a variety of commercial driving occupations, including driving trucks, buses, and taxis.
“Only 43% of primary prevention patients and 64% of secondary prevention patients stated that they had been informed about any driving restrictions,” said Dr. Bjerre. The figure was slightly better for patients after an ICD shock was delivered – 72% of these patients recalled hearing about driving restrictions.
“Among professional drivers – who are never supposed to drive again – only 45% said they had been informed about any professional driving restrictions,” she added.
What did patients report about their actual driving behaviors? Of patients receiving an ICD for primary prevention, 34% resumed driving within one week of ICD implantation. For those receiving an ICD for secondary prevention and those who had received an appropriate ICD shock, 43% and 30%, respectively, began driving before the recommended 3 months had elapsed.
The driving behavior of those with commercial licenses didn’t differ from the cohort as a whole: 35% of this group had resumed commercial driving.
In all the study’s subgroups, nonadherence to driving restrictions was more likely if the participant didn’t recall having been informed of the restrictions, with an odds ratio (OR) of 3.34 for nonadherence. However, noted Dr. Bjerre, at least 20% of patients in all subgroups who said they’d been told not to drive still resumed driving in contravention of restrictions. “So it seems that information can’t explain everything,” she said.
Additional predictors of nonadherence included male sex, with an OR of 1.53, being the only driver in the household (OR 1.29), and being at least 60 years old (OR, 1.20). Those receiving an ICD for secondary prevention had an OR of 2.20 for nonadherence, as well.
The study had a large cohort of real-life ICD patients and the response rate was high, said Dr. Bjerre. However, there was a risk of recall bias; additionally, nonresponders differed from responders, limiting full generalizability of the data. Finally, she observed that participants may have given the answers they thought were socially desirable.
“I want to get back to our friend the taxi driver,” who was adherent to restrictions, but who kept wanting to know what the actual chances were that he’d harm someone if he resumed driving. Realizing she couldn’t give him a very precise answer, Dr. Bjerre concluded, “I do think we owe it to our patients to provide more evidence on the absolute risk of traffic accidents in these patients.”
Dr. Bjerre reported that she had no conflicts of interest.
koakes@mdedge.com
REPORTING FROM ESC CONGRESS 2019