User login
Assessing patients with liver disease for surgery is one of the most common reasons for hepatology consultation in the hospital. This review focuses on practical aspects of evaluating patients with known or suspected liver disease and provides guidance for determining whether it is safe to proceed with surgery in such patients. I begin with a case study to introduce some common clinical challenges and then revisit the case—with relevant teaching points—at the end.
CASE: A MIDDLE-AGED MAN WITH LIVER DISEASE SCHEDULED FOR CARDIAC SURGERY
A 57-year-old man with a history of liver disease is referred for preoperative assessment. It is 6:30 pm, and the patient has just arrived in the hospital; he is scheduled for coronary artery bypass graft surgery (CABG) early tomorrow morning for ischemic heart disease. Ten years ago, he was diagnosed with hepatitis C virus infection; 2 years later, he had a cholecystectomy. He has a remote history of intravenous drug use.
The sub-intern asks for an assessment of operative risk as well as advice on the type of anesthesia to be used.
HEPATIC EFFECTS OF ANESTHESIA
Anesthesiologists are keenly aware of the hepatic effects of anesthesia and that they must carefully choose anesthetics for patients with liver disease. There are a number of at least theoretical concerns about using particular anesthetics:
- Inhaled anesthetics, such as isoflurane, cause systemic vasodilation and depress cardiac output. These effects are of concern since many patients with advanced liver disease already have a hyperdynamic circulation because of peripheral vasodilation.
- Spinal or epidural anesthetics may reduce mean arterial pressure, which is of concern for similar reasons.
- Nitrous oxide has less of a depressive effect unless the patient has concomitant hypercapnia.
Another consideration is the hepatic metabolism of anesthetic agents. Use of halothane, which is 20% metabolized by the liver, is now uncommon, particularly if there is any concern about liver disease. In contrast, enflurane is only 4% metabolized by the liver. Numerous other anesthetics—including isoflurane, desflurane, and sevoflurane—have only minimal hepatic metabolism (< 0.2%), which makes them, along with nitrous oxide, the best anesthetic choices for patients with liver disease.
ASSESSING OPERATIVE RISK
The more important issue in the consultation for our patient is the degree of operative risk associated with his underlying liver disease. A number of factors are pertinent, including the etiology and severity of the liver disease and the type of surgery planned.
Acute liver disease has higher operative risk
Literature dating back 40 years has associated acute viral and alcoholic hepatitis with poor outcomes in surgical patients. Major elective surgery for a patient with suspected acute hepatitis A, for example, should be deferred until the patient has recovered, barring some compelling reason for greater urgency, such as a perforated viscus.
In chronic liver disease, hepatocellular function predicts outcome
When a patient with liver disease is evaluated for surgery, evidence should be sought to determine whether an index complication has already occurred. Because the patient in our case study had a cholecystectomy several years before, I would also ask, “What did the surgeon say your liver looked like? Did you have any bleeding problems afterwards? Did you develop ascites?”
It is also important to determine whether portal hypertension is present. For a patient with liver disease, otherwise unexplained thrombocytopenia is a useful indicator of portal hypertension.
Systems for scoring liver disease severity
Even a surgical patient with well-compensated liver disease is at risk for developing complications postoperatively, particularly if abdominal surgery is planned. Risk should be assessed in all patients with liver disease using either the Child-Pugh scoring system or the Model for End-Stage Liver Disease (MELD) scoring system.
The Child-Pugh score, which assigns 1 to 3 points according to the presence/absence and levels of each of five simple factors (bilirubin, albumin, prothrombin time/international normalized ratio [INR], ascites, and encephalopathy stage), has been used for decades to assess the severity of liver disease. Patients with Child-Pugh class A disease (score of 5–6) have well-compensated cirrhosis and good synthetic function, and therefore have essentially no restrictions for undergoing surgery. For patients in Child-Pugh class B (score of 7–9), the risk of perioperative complications and mortality is higher and any major hepatic surgery (such as hepatic resection) should be avoided. Patients with class C cirrhosis (score of 10–15) are not candidates for any major elective surgery and should be considered for liver transplantation referral.
The MELD scoring system was developed more recently and is used to prioritize eligibility for liver transplantation. Calculated using a mathematical formula that incorporates three objective patient variables—
creatinine, bilirubin, and INR—the MELD score correlates very well with prognosis. The score can be calculated by an online MELD calculator such as the one at www.unos.org/resources.2 A patient with a high MELD score is unlikely to survive for more than a few months without liver transplantation; a patient with a low MELD score is likely to survive for at least 12 months. Calculating the MELD score is now one of the first assessments in any patient suspected of having cirrhosis.
Risk factors for complications and death
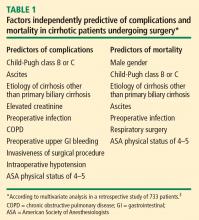
In a retrospective study to identify factors associated with complications and mortality in surgical patients with cirrhosis, Ziser et al reviewed the records of 733 patients with cirrhosis who underwent surgical procedures (except liver transplantation) at the Mayo Clinic over an 11-year period (1980–1991).3 The mortality rate within 30 days of surgery was 11.6%. Long-term follow-up showed that most deaths occurred within the first few months after surgery, when many patients succumbed to pneumonia or renal insufficiency.
Risk factors have strong cumulative power
The study by Ziser et al also underscored the cumulative effect of risk factors, as the probability of developing a perioperative complication increased dramatically with the number of risk factors (as identified by multiavariate analysis) that a patient had, as follows3:
- 9.3% risk of complications with 1 risk factor
- 14.5% risk with 2 factors
- 33.5% risk with 3 factors
- 63.0% risk with 4 or 5 factors
- 73.3% risk with 6 factors
- 100% risk with 7 or 8 factors.
Postoperative complications: Beware hepatorenal syndrome
The most common postoperative complications in the study by Ziser et al were pneumonia, other infections, ventilation dependency, and ascites.3
Possibly the most ominous perioperative complication in a patient with liver disease is the onset of renal insufficiency, which may be precipitated by a number of factors, including nephrotoxic drugs and intraoperative hypotension. Renal insufficiency is usually a predictor of markedly reduced survival and a sign that hepatorenal syndrome may have developed.
Hepatorenal syndrome, which occurred in 3.3% of patients in the analysis by Ziser et al,3 is the presence of renal failure in a patient with cirrhosis. It is characterized by advanced liver failure and severe sinusoidal portal hypertension. The renal failure is said to be “functional” because significant histological changes are absent on kidney biopsy. Marked arteriolar vasodilation occurs in the extrarenal circulation with renal vasoconstriction leading to reduced glomerular filtration.
IMPORTANCE OF SURGICAL PROCEDURE TYPE
In addition to the patient-specific risk factors discussed above, certain surgical procedures deserve special consideration in patients with liver disease.
Cholecystectomy: Open vs closed
Patients with liver disease have the same indication for cholecystectomy as anyone else does: symptomatic gallstone disease. Patients with cirrhosis who are found to have incidental gallstones on ultrasonography should not undergo cholecystectomy unless the gallstones are symptomatic, as liver function may deteriorate after surgery.
For a patient with liver disease undergoing cholecystectomy, a common concern is whether an open or closed procedure should be done. Conventional wisdom had been that a patient with underlying liver disease (particularly cirrhosis) should have an open procedure so that the surgeon could more easily control bleeding, but that notion has changed in recent years with evidence supporting the safety of a laparoscopic approach in patients with liver disease.
One study supporting this new strategy is a retrospective review of 50 patients who had undergone cholecystectomy for symptomatic gallstone disease at the Mayo Clinic between 1990 and 1997.4 The procedure was open in half of the patients and laparoscopic in the other half. All patients had Child-Pugh class A or B cirrhosis. The indications for surgery were acute cholecystitis, biliary colic, or pancreatitis, and the number of patients with each of these indications was comparable between the open-surgery and laparoscopy groups. Three patients who initially underwent laparoscopy were converted to open cholecystectomy: two for bleeding and one for poor access. The study found that laparoscopic cholecystectomy was associated with statistically significant reductions in operating room time, blood loss, and length of hospital stay. No deaths occurred in either group. The authors concluded that laparoscopic cholecystectomy is safe in patients with cirrhosis and offers several advantages over an open surgical approach.
In light of these findings and other recent evidence, laparoscopic cholecystectomy should be recommended for patients with liver disease unless they have ascites or other evidence of overt hepatic decompensation, in which case cholecystectomy itself is contraindicated.
Cardiac surgery with bypass poses extra risk
Patients with liver disease undergoing open heart surgery with cardiopulmonary bypass are at especially high risk because of the effect on hepatic hemodynamics. This risk was demonstrated in a retrospective review of all patients with cirrhosis who underwent cardiac surgery with cardiopulmonary bypass at the Cleveland Clinic from 1992 to 2002.5 Of the 44 patients identified, 12 (27%) developed hepatic decompensation and 7 (16%) died. Hepatic decompensation was a major factor in all the deaths.
The MELD and Child-Pugh scores correlated well with one another in this study and were highly associated with hepatic decompensation and death. The best cutoff values for predicting mortality and hepatic decompensation were found to be a score greater than 7 in the Child-Pugh system and a score greater than 13 in the MELD system. (For context, receipt of a donor liver via a transplant list in the United States requires a MELD score of at least 15.) The study confirmed that the Child-Pugh score, which is easy to determine at the bedside, remains a reliable predictor of poor outcomes.5
CASE REVISITED: POSTOPERATIVE LIVER FUNCTION DECLINE―HOW SERIOUS IS IT?
Our patient undergoes the CABG procedure, and 3 days later you are asked to see him. According to the sub-intern, although the surgery was successful, the patient is now “in liver failure.” After hearing this news, the family is anxious to discuss liver transplantation.
On examination, the patient is alert and extubated, so he is clearly not encephalopathic. His wound is clean and shows no sign of infection. He appears to be mildly icteric, and he may have some ascites, based on mild flank dullness.
His laboratory test results are as follows:
- Bilirubin, 3.1 mg/dL (normal range, 0.3–1.2)
- INR, 1.2 (0.9–1.2)
- Alanine aminotransferase (ALT), 300 U/L (10–40)
- Creatinine, 0.9 mg/dL (0.6–1.2).
Although the bilirubin and ALT are elevated, it is notable that the creatinine is normal. This pattern is not uncommon after elective surgery in a patient with underlying cirrhosis. Renal dysfunction is the biggest concern in the perioperative management of a patient with liver disease, as it is an indicator that the patient may develop overt hepatic decompensation. Likely reasons for the patient’s ALT elevation are the effects of cardiopulmonary bypass and possible intraoperative hypotension.
The family needs to be told that the patient is not in liver failure and that it is best to wait with the expectation that he will do fine unless other complications supervene.
You advise cautious diuresis, and the ALT falls over the next few days. The bilirubin declines to 2.0 mg/dL. At this point, you advise discharge planning.
One need not wait for the bilirubin to return to normal: after an acute hepatic insult such as ischemic hepatitis or intraoperative hypotension, bilirubin is the last indicator to improve. Bilirubin is in part albumin-bound, and the half-life of albumin is 18 days, so a patient can remain icteric for some time after the rest of the liver function tests have returned to normal.
DISCUSSION
Question from the audience: What are your recommendations regarding platelet transfusion if the platelet count is less than 50,000 in a patient with liver disease?
Dr. Martin: For patients with thrombocytopenia, it is prudent to get the platelet count above 60,000 before any procedure. We will not even do a blind liver biopsy in a patient with a platelet count of less than 60,000.
Question from the audience: A study from the Annals of Surgery concludes that patients with liver disease do poorly with a hemoglobin of less than 10 g/dL. Would you transfuse aggressively before surgery?
Dr. Martin: For a patient with anemia, I don’t like to use aggressive transfusion if cirrhosis is present because the portal pressure may go up and increase the risk of variceal hemorrhage. If there is adequate time for a work-up, one can screen for varices by endoscopy. If there is evidence of overt hepatic decompensation and portal hypertension (esophageal varices, a palpable spleen, and thrombocytopenia), I wouldn’t try to get the hemoglobin much above 10 g/dL.
Question from the audience: How would you modify prophylaxis for deep vein thrombosis following hip or knee replacement surgery in patients with liver disease?
Dr. Martin: I would base it on the INR. Patients who are already mildly coagulopathic tend to be very sensitive to warfarin in the long term. For immediate perioperative prophylaxis, I would not administer anything if the patient had a platelet count below 60,000; otherwise I would probably proceed as usual.
Question from the audience: You said that we shouldn’t operate on patients with acute hepatitis, but we frequently encounter patients with drug-induced hepatitis, such as from anticholesterol drugs. These patients’ ALT and aspartate aminotransferase (AST) levels can remain elevated for 2 or 3 months. How long should we delay surgery? For example, is it dangerous to proceed with a mastectomy a month after discontinuing the drug if the liver enzymes are still around 100 U/L?
Dr. Martin: It’s worth noting that much of the literature on surgery in patients with acute viral hepatitis is 30 or 40 years old. If such a patient had a compelling reason to have surgery, you might wait until the liver enzymes were trending downward and you were confident that the patient was recovering.
Question from the audience: How do you manage patients who have varices or have had variceal bleeding in the past? Many of them are on beta-blockers, such as propranolol, which can cause hypotension intraoperatively.
Dr. Martin: The standard of care is to prescribe beta-blockers for a patient with large varices, or to ablate the varices by endoscopy, which is my practice. In general, I would discontinue propranolol on the morning of surgery. If possible, however, I would have the patient undergo endoscopy before surgery to assess the likelihood of short-term variceal bleeding. If the varices look to be at low risk of bleeding, the beta-blocker can safely be stopped. If they look to be at high risk of bleeding, the surgery should be delayed for a few weeks, if possible, so that the varices can be ablated, which usually takes two or three sessions.
Question from the audience: I deal with many referrals, and I struggle with how aggressive a work-up I should do for patients undergoing elective surgery when a new abnormality is found in one of their liver function tests.
Dr. Martin: I would try to establish whether the abnormality is a chronic problem. Has the patient been told about an abnormal liver test in the past? Ask if the patient has been a blood donor, as measurement of ALT and some hepatitis serologies would have been required. Also ask if he or she has ever taken out a big life insurance policy, which also would have required liver function testing. If the abnormality is chronic, you may proceed with surgery if the bilirubin and INR are normal. In the absence of chronicity, surgery should be delayed for further work-up only in patients with indicators of significant liver disease—either markedly abnormal liver tests, thrombocytopenia, or coagulopathy.
Follow-up question: But patients rarely know whether they’ve had elevated liver enzymes in the past. You said not to worry about enzyme abnormalities unless they are markedly elevated, but how high is that?
Dr. Martin: AST and ALT are indicators of liver injury rather than of synthetic function. The true liver function tests are really albumin, bilirubin, and prothrombin time. Paradoxically, one of the best liver function tests is the platelet count. For me, a red flag for a patient with newly recognized liver disease is any degree of thrombocytopenia or coagulopathy or an elevation of bilirubin above the upper limit of normal. A patient with a platelet count of 90,000 and an INR above 1.2 has significant underlying liver disease, and I would be very concerned. Unless it’s a dire emergency, such a patient would need further evaluation before proceeding with surgery. In contrast, a patient with an ALT of 89, an AST of 65, and normal prothrombin time and platelet count should be safe to proceed to surgery. But such a patient needs an evaluation for liver disease afterward.
Question from the audience: My institution performs many liver resections for metastases or primary liver cancers. Our liver surgeons routinely discontinue statins 2 to 3 weeks before liver surgery, but it has been said at this summit that is not necessary. What’s your opinion?
Dr. Martin: I think that statins get a very bad rap in terms of hepatotoxity. Most patients with metabolic syndrome have hyperlipidemia, which can cause fatty liver disease and hepatic dysfunction. Statins help bring the lipid levels down. Hepatologists do not regard statins as major culprits in causing liver problems. I don’t believe there’s any particular indication to stop them before a patient undergoes hepatic surgery.
Question from the audience: I assess patients 1 or 2 weeks before surgery. For a patient with coagulopathy whom you suspect has underlying liver disease, is there any value in trying to treat the coagulopathy with vitamin K?
Dr. Martin: It can be worthwhile to try 10 mg subcutaneously for 3 days to see whether the situation improves, but if the patient has severe parenchymal liver disease, the vitamin K won’t help much.
- Ginés P, Quintero E, Arroyo V, et al. Compensated cirrhosis: natural history and prognostic factors. Hepatology 1987; 7:122–128.
- MELD/PELD calculator. United Network for Organ Sharing Web site. http://www.unos.org/resources/MeldPeldCalculator.asp?index=98. Accessed May 8, 2009.
- Ziser A, Plevak DJ, Wiesner RH, Rakela J, Offord KP, Brown DL. Morbidity and mortality in cirrhotic patients undergoing anesthesia and surgery. Anesthesiology 1999; 90:42–53.
- Poggio JL, Rowland CM, Gores GJ, et al. A comparison of laparoscopic and open cholecystectomy in patients with compensated cirrhosis and symptomatic gallstone disease. Surgery 2000; 127:405–411.
- Suman A, Barnes DS, Zein NN, et al. Predicting outcome after cardiac surgery in patients with cirrhosis: a comparison of Child-Pugh and MELD scores. Clin Gastroenterol Hepatol 2004; 2:719–723.
Assessing patients with liver disease for surgery is one of the most common reasons for hepatology consultation in the hospital. This review focuses on practical aspects of evaluating patients with known or suspected liver disease and provides guidance for determining whether it is safe to proceed with surgery in such patients. I begin with a case study to introduce some common clinical challenges and then revisit the case—with relevant teaching points—at the end.
CASE: A MIDDLE-AGED MAN WITH LIVER DISEASE SCHEDULED FOR CARDIAC SURGERY
A 57-year-old man with a history of liver disease is referred for preoperative assessment. It is 6:30 pm, and the patient has just arrived in the hospital; he is scheduled for coronary artery bypass graft surgery (CABG) early tomorrow morning for ischemic heart disease. Ten years ago, he was diagnosed with hepatitis C virus infection; 2 years later, he had a cholecystectomy. He has a remote history of intravenous drug use.
The sub-intern asks for an assessment of operative risk as well as advice on the type of anesthesia to be used.
HEPATIC EFFECTS OF ANESTHESIA
Anesthesiologists are keenly aware of the hepatic effects of anesthesia and that they must carefully choose anesthetics for patients with liver disease. There are a number of at least theoretical concerns about using particular anesthetics:
- Inhaled anesthetics, such as isoflurane, cause systemic vasodilation and depress cardiac output. These effects are of concern since many patients with advanced liver disease already have a hyperdynamic circulation because of peripheral vasodilation.
- Spinal or epidural anesthetics may reduce mean arterial pressure, which is of concern for similar reasons.
- Nitrous oxide has less of a depressive effect unless the patient has concomitant hypercapnia.
Another consideration is the hepatic metabolism of anesthetic agents. Use of halothane, which is 20% metabolized by the liver, is now uncommon, particularly if there is any concern about liver disease. In contrast, enflurane is only 4% metabolized by the liver. Numerous other anesthetics—including isoflurane, desflurane, and sevoflurane—have only minimal hepatic metabolism (< 0.2%), which makes them, along with nitrous oxide, the best anesthetic choices for patients with liver disease.
ASSESSING OPERATIVE RISK
The more important issue in the consultation for our patient is the degree of operative risk associated with his underlying liver disease. A number of factors are pertinent, including the etiology and severity of the liver disease and the type of surgery planned.
Acute liver disease has higher operative risk
Literature dating back 40 years has associated acute viral and alcoholic hepatitis with poor outcomes in surgical patients. Major elective surgery for a patient with suspected acute hepatitis A, for example, should be deferred until the patient has recovered, barring some compelling reason for greater urgency, such as a perforated viscus.
In chronic liver disease, hepatocellular function predicts outcome
When a patient with liver disease is evaluated for surgery, evidence should be sought to determine whether an index complication has already occurred. Because the patient in our case study had a cholecystectomy several years before, I would also ask, “What did the surgeon say your liver looked like? Did you have any bleeding problems afterwards? Did you develop ascites?”
It is also important to determine whether portal hypertension is present. For a patient with liver disease, otherwise unexplained thrombocytopenia is a useful indicator of portal hypertension.
Systems for scoring liver disease severity
Even a surgical patient with well-compensated liver disease is at risk for developing complications postoperatively, particularly if abdominal surgery is planned. Risk should be assessed in all patients with liver disease using either the Child-Pugh scoring system or the Model for End-Stage Liver Disease (MELD) scoring system.
The Child-Pugh score, which assigns 1 to 3 points according to the presence/absence and levels of each of five simple factors (bilirubin, albumin, prothrombin time/international normalized ratio [INR], ascites, and encephalopathy stage), has been used for decades to assess the severity of liver disease. Patients with Child-Pugh class A disease (score of 5–6) have well-compensated cirrhosis and good synthetic function, and therefore have essentially no restrictions for undergoing surgery. For patients in Child-Pugh class B (score of 7–9), the risk of perioperative complications and mortality is higher and any major hepatic surgery (such as hepatic resection) should be avoided. Patients with class C cirrhosis (score of 10–15) are not candidates for any major elective surgery and should be considered for liver transplantation referral.
The MELD scoring system was developed more recently and is used to prioritize eligibility for liver transplantation. Calculated using a mathematical formula that incorporates three objective patient variables—
creatinine, bilirubin, and INR—the MELD score correlates very well with prognosis. The score can be calculated by an online MELD calculator such as the one at www.unos.org/resources.2 A patient with a high MELD score is unlikely to survive for more than a few months without liver transplantation; a patient with a low MELD score is likely to survive for at least 12 months. Calculating the MELD score is now one of the first assessments in any patient suspected of having cirrhosis.
Risk factors for complications and death
In a retrospective study to identify factors associated with complications and mortality in surgical patients with cirrhosis, Ziser et al reviewed the records of 733 patients with cirrhosis who underwent surgical procedures (except liver transplantation) at the Mayo Clinic over an 11-year period (1980–1991).3 The mortality rate within 30 days of surgery was 11.6%. Long-term follow-up showed that most deaths occurred within the first few months after surgery, when many patients succumbed to pneumonia or renal insufficiency.
Risk factors have strong cumulative power
The study by Ziser et al also underscored the cumulative effect of risk factors, as the probability of developing a perioperative complication increased dramatically with the number of risk factors (as identified by multiavariate analysis) that a patient had, as follows3:
- 9.3% risk of complications with 1 risk factor
- 14.5% risk with 2 factors
- 33.5% risk with 3 factors
- 63.0% risk with 4 or 5 factors
- 73.3% risk with 6 factors
- 100% risk with 7 or 8 factors.
Postoperative complications: Beware hepatorenal syndrome
The most common postoperative complications in the study by Ziser et al were pneumonia, other infections, ventilation dependency, and ascites.3
Possibly the most ominous perioperative complication in a patient with liver disease is the onset of renal insufficiency, which may be precipitated by a number of factors, including nephrotoxic drugs and intraoperative hypotension. Renal insufficiency is usually a predictor of markedly reduced survival and a sign that hepatorenal syndrome may have developed.
Hepatorenal syndrome, which occurred in 3.3% of patients in the analysis by Ziser et al,3 is the presence of renal failure in a patient with cirrhosis. It is characterized by advanced liver failure and severe sinusoidal portal hypertension. The renal failure is said to be “functional” because significant histological changes are absent on kidney biopsy. Marked arteriolar vasodilation occurs in the extrarenal circulation with renal vasoconstriction leading to reduced glomerular filtration.
IMPORTANCE OF SURGICAL PROCEDURE TYPE
In addition to the patient-specific risk factors discussed above, certain surgical procedures deserve special consideration in patients with liver disease.
Cholecystectomy: Open vs closed
Patients with liver disease have the same indication for cholecystectomy as anyone else does: symptomatic gallstone disease. Patients with cirrhosis who are found to have incidental gallstones on ultrasonography should not undergo cholecystectomy unless the gallstones are symptomatic, as liver function may deteriorate after surgery.
For a patient with liver disease undergoing cholecystectomy, a common concern is whether an open or closed procedure should be done. Conventional wisdom had been that a patient with underlying liver disease (particularly cirrhosis) should have an open procedure so that the surgeon could more easily control bleeding, but that notion has changed in recent years with evidence supporting the safety of a laparoscopic approach in patients with liver disease.
One study supporting this new strategy is a retrospective review of 50 patients who had undergone cholecystectomy for symptomatic gallstone disease at the Mayo Clinic between 1990 and 1997.4 The procedure was open in half of the patients and laparoscopic in the other half. All patients had Child-Pugh class A or B cirrhosis. The indications for surgery were acute cholecystitis, biliary colic, or pancreatitis, and the number of patients with each of these indications was comparable between the open-surgery and laparoscopy groups. Three patients who initially underwent laparoscopy were converted to open cholecystectomy: two for bleeding and one for poor access. The study found that laparoscopic cholecystectomy was associated with statistically significant reductions in operating room time, blood loss, and length of hospital stay. No deaths occurred in either group. The authors concluded that laparoscopic cholecystectomy is safe in patients with cirrhosis and offers several advantages over an open surgical approach.
In light of these findings and other recent evidence, laparoscopic cholecystectomy should be recommended for patients with liver disease unless they have ascites or other evidence of overt hepatic decompensation, in which case cholecystectomy itself is contraindicated.
Cardiac surgery with bypass poses extra risk
Patients with liver disease undergoing open heart surgery with cardiopulmonary bypass are at especially high risk because of the effect on hepatic hemodynamics. This risk was demonstrated in a retrospective review of all patients with cirrhosis who underwent cardiac surgery with cardiopulmonary bypass at the Cleveland Clinic from 1992 to 2002.5 Of the 44 patients identified, 12 (27%) developed hepatic decompensation and 7 (16%) died. Hepatic decompensation was a major factor in all the deaths.
The MELD and Child-Pugh scores correlated well with one another in this study and were highly associated with hepatic decompensation and death. The best cutoff values for predicting mortality and hepatic decompensation were found to be a score greater than 7 in the Child-Pugh system and a score greater than 13 in the MELD system. (For context, receipt of a donor liver via a transplant list in the United States requires a MELD score of at least 15.) The study confirmed that the Child-Pugh score, which is easy to determine at the bedside, remains a reliable predictor of poor outcomes.5
CASE REVISITED: POSTOPERATIVE LIVER FUNCTION DECLINE―HOW SERIOUS IS IT?
Our patient undergoes the CABG procedure, and 3 days later you are asked to see him. According to the sub-intern, although the surgery was successful, the patient is now “in liver failure.” After hearing this news, the family is anxious to discuss liver transplantation.
On examination, the patient is alert and extubated, so he is clearly not encephalopathic. His wound is clean and shows no sign of infection. He appears to be mildly icteric, and he may have some ascites, based on mild flank dullness.
His laboratory test results are as follows:
- Bilirubin, 3.1 mg/dL (normal range, 0.3–1.2)
- INR, 1.2 (0.9–1.2)
- Alanine aminotransferase (ALT), 300 U/L (10–40)
- Creatinine, 0.9 mg/dL (0.6–1.2).
Although the bilirubin and ALT are elevated, it is notable that the creatinine is normal. This pattern is not uncommon after elective surgery in a patient with underlying cirrhosis. Renal dysfunction is the biggest concern in the perioperative management of a patient with liver disease, as it is an indicator that the patient may develop overt hepatic decompensation. Likely reasons for the patient’s ALT elevation are the effects of cardiopulmonary bypass and possible intraoperative hypotension.
The family needs to be told that the patient is not in liver failure and that it is best to wait with the expectation that he will do fine unless other complications supervene.
You advise cautious diuresis, and the ALT falls over the next few days. The bilirubin declines to 2.0 mg/dL. At this point, you advise discharge planning.
One need not wait for the bilirubin to return to normal: after an acute hepatic insult such as ischemic hepatitis or intraoperative hypotension, bilirubin is the last indicator to improve. Bilirubin is in part albumin-bound, and the half-life of albumin is 18 days, so a patient can remain icteric for some time after the rest of the liver function tests have returned to normal.
DISCUSSION
Question from the audience: What are your recommendations regarding platelet transfusion if the platelet count is less than 50,000 in a patient with liver disease?
Dr. Martin: For patients with thrombocytopenia, it is prudent to get the platelet count above 60,000 before any procedure. We will not even do a blind liver biopsy in a patient with a platelet count of less than 60,000.
Question from the audience: A study from the Annals of Surgery concludes that patients with liver disease do poorly with a hemoglobin of less than 10 g/dL. Would you transfuse aggressively before surgery?
Dr. Martin: For a patient with anemia, I don’t like to use aggressive transfusion if cirrhosis is present because the portal pressure may go up and increase the risk of variceal hemorrhage. If there is adequate time for a work-up, one can screen for varices by endoscopy. If there is evidence of overt hepatic decompensation and portal hypertension (esophageal varices, a palpable spleen, and thrombocytopenia), I wouldn’t try to get the hemoglobin much above 10 g/dL.
Question from the audience: How would you modify prophylaxis for deep vein thrombosis following hip or knee replacement surgery in patients with liver disease?
Dr. Martin: I would base it on the INR. Patients who are already mildly coagulopathic tend to be very sensitive to warfarin in the long term. For immediate perioperative prophylaxis, I would not administer anything if the patient had a platelet count below 60,000; otherwise I would probably proceed as usual.
Question from the audience: You said that we shouldn’t operate on patients with acute hepatitis, but we frequently encounter patients with drug-induced hepatitis, such as from anticholesterol drugs. These patients’ ALT and aspartate aminotransferase (AST) levels can remain elevated for 2 or 3 months. How long should we delay surgery? For example, is it dangerous to proceed with a mastectomy a month after discontinuing the drug if the liver enzymes are still around 100 U/L?
Dr. Martin: It’s worth noting that much of the literature on surgery in patients with acute viral hepatitis is 30 or 40 years old. If such a patient had a compelling reason to have surgery, you might wait until the liver enzymes were trending downward and you were confident that the patient was recovering.
Question from the audience: How do you manage patients who have varices or have had variceal bleeding in the past? Many of them are on beta-blockers, such as propranolol, which can cause hypotension intraoperatively.
Dr. Martin: The standard of care is to prescribe beta-blockers for a patient with large varices, or to ablate the varices by endoscopy, which is my practice. In general, I would discontinue propranolol on the morning of surgery. If possible, however, I would have the patient undergo endoscopy before surgery to assess the likelihood of short-term variceal bleeding. If the varices look to be at low risk of bleeding, the beta-blocker can safely be stopped. If they look to be at high risk of bleeding, the surgery should be delayed for a few weeks, if possible, so that the varices can be ablated, which usually takes two or three sessions.
Question from the audience: I deal with many referrals, and I struggle with how aggressive a work-up I should do for patients undergoing elective surgery when a new abnormality is found in one of their liver function tests.
Dr. Martin: I would try to establish whether the abnormality is a chronic problem. Has the patient been told about an abnormal liver test in the past? Ask if the patient has been a blood donor, as measurement of ALT and some hepatitis serologies would have been required. Also ask if he or she has ever taken out a big life insurance policy, which also would have required liver function testing. If the abnormality is chronic, you may proceed with surgery if the bilirubin and INR are normal. In the absence of chronicity, surgery should be delayed for further work-up only in patients with indicators of significant liver disease—either markedly abnormal liver tests, thrombocytopenia, or coagulopathy.
Follow-up question: But patients rarely know whether they’ve had elevated liver enzymes in the past. You said not to worry about enzyme abnormalities unless they are markedly elevated, but how high is that?
Dr. Martin: AST and ALT are indicators of liver injury rather than of synthetic function. The true liver function tests are really albumin, bilirubin, and prothrombin time. Paradoxically, one of the best liver function tests is the platelet count. For me, a red flag for a patient with newly recognized liver disease is any degree of thrombocytopenia or coagulopathy or an elevation of bilirubin above the upper limit of normal. A patient with a platelet count of 90,000 and an INR above 1.2 has significant underlying liver disease, and I would be very concerned. Unless it’s a dire emergency, such a patient would need further evaluation before proceeding with surgery. In contrast, a patient with an ALT of 89, an AST of 65, and normal prothrombin time and platelet count should be safe to proceed to surgery. But such a patient needs an evaluation for liver disease afterward.
Question from the audience: My institution performs many liver resections for metastases or primary liver cancers. Our liver surgeons routinely discontinue statins 2 to 3 weeks before liver surgery, but it has been said at this summit that is not necessary. What’s your opinion?
Dr. Martin: I think that statins get a very bad rap in terms of hepatotoxity. Most patients with metabolic syndrome have hyperlipidemia, which can cause fatty liver disease and hepatic dysfunction. Statins help bring the lipid levels down. Hepatologists do not regard statins as major culprits in causing liver problems. I don’t believe there’s any particular indication to stop them before a patient undergoes hepatic surgery.
Question from the audience: I assess patients 1 or 2 weeks before surgery. For a patient with coagulopathy whom you suspect has underlying liver disease, is there any value in trying to treat the coagulopathy with vitamin K?
Dr. Martin: It can be worthwhile to try 10 mg subcutaneously for 3 days to see whether the situation improves, but if the patient has severe parenchymal liver disease, the vitamin K won’t help much.
Assessing patients with liver disease for surgery is one of the most common reasons for hepatology consultation in the hospital. This review focuses on practical aspects of evaluating patients with known or suspected liver disease and provides guidance for determining whether it is safe to proceed with surgery in such patients. I begin with a case study to introduce some common clinical challenges and then revisit the case—with relevant teaching points—at the end.
CASE: A MIDDLE-AGED MAN WITH LIVER DISEASE SCHEDULED FOR CARDIAC SURGERY
A 57-year-old man with a history of liver disease is referred for preoperative assessment. It is 6:30 pm, and the patient has just arrived in the hospital; he is scheduled for coronary artery bypass graft surgery (CABG) early tomorrow morning for ischemic heart disease. Ten years ago, he was diagnosed with hepatitis C virus infection; 2 years later, he had a cholecystectomy. He has a remote history of intravenous drug use.
The sub-intern asks for an assessment of operative risk as well as advice on the type of anesthesia to be used.
HEPATIC EFFECTS OF ANESTHESIA
Anesthesiologists are keenly aware of the hepatic effects of anesthesia and that they must carefully choose anesthetics for patients with liver disease. There are a number of at least theoretical concerns about using particular anesthetics:
- Inhaled anesthetics, such as isoflurane, cause systemic vasodilation and depress cardiac output. These effects are of concern since many patients with advanced liver disease already have a hyperdynamic circulation because of peripheral vasodilation.
- Spinal or epidural anesthetics may reduce mean arterial pressure, which is of concern for similar reasons.
- Nitrous oxide has less of a depressive effect unless the patient has concomitant hypercapnia.
Another consideration is the hepatic metabolism of anesthetic agents. Use of halothane, which is 20% metabolized by the liver, is now uncommon, particularly if there is any concern about liver disease. In contrast, enflurane is only 4% metabolized by the liver. Numerous other anesthetics—including isoflurane, desflurane, and sevoflurane—have only minimal hepatic metabolism (< 0.2%), which makes them, along with nitrous oxide, the best anesthetic choices for patients with liver disease.
ASSESSING OPERATIVE RISK
The more important issue in the consultation for our patient is the degree of operative risk associated with his underlying liver disease. A number of factors are pertinent, including the etiology and severity of the liver disease and the type of surgery planned.
Acute liver disease has higher operative risk
Literature dating back 40 years has associated acute viral and alcoholic hepatitis with poor outcomes in surgical patients. Major elective surgery for a patient with suspected acute hepatitis A, for example, should be deferred until the patient has recovered, barring some compelling reason for greater urgency, such as a perforated viscus.
In chronic liver disease, hepatocellular function predicts outcome
When a patient with liver disease is evaluated for surgery, evidence should be sought to determine whether an index complication has already occurred. Because the patient in our case study had a cholecystectomy several years before, I would also ask, “What did the surgeon say your liver looked like? Did you have any bleeding problems afterwards? Did you develop ascites?”
It is also important to determine whether portal hypertension is present. For a patient with liver disease, otherwise unexplained thrombocytopenia is a useful indicator of portal hypertension.
Systems for scoring liver disease severity
Even a surgical patient with well-compensated liver disease is at risk for developing complications postoperatively, particularly if abdominal surgery is planned. Risk should be assessed in all patients with liver disease using either the Child-Pugh scoring system or the Model for End-Stage Liver Disease (MELD) scoring system.
The Child-Pugh score, which assigns 1 to 3 points according to the presence/absence and levels of each of five simple factors (bilirubin, albumin, prothrombin time/international normalized ratio [INR], ascites, and encephalopathy stage), has been used for decades to assess the severity of liver disease. Patients with Child-Pugh class A disease (score of 5–6) have well-compensated cirrhosis and good synthetic function, and therefore have essentially no restrictions for undergoing surgery. For patients in Child-Pugh class B (score of 7–9), the risk of perioperative complications and mortality is higher and any major hepatic surgery (such as hepatic resection) should be avoided. Patients with class C cirrhosis (score of 10–15) are not candidates for any major elective surgery and should be considered for liver transplantation referral.
The MELD scoring system was developed more recently and is used to prioritize eligibility for liver transplantation. Calculated using a mathematical formula that incorporates three objective patient variables—
creatinine, bilirubin, and INR—the MELD score correlates very well with prognosis. The score can be calculated by an online MELD calculator such as the one at www.unos.org/resources.2 A patient with a high MELD score is unlikely to survive for more than a few months without liver transplantation; a patient with a low MELD score is likely to survive for at least 12 months. Calculating the MELD score is now one of the first assessments in any patient suspected of having cirrhosis.
Risk factors for complications and death
In a retrospective study to identify factors associated with complications and mortality in surgical patients with cirrhosis, Ziser et al reviewed the records of 733 patients with cirrhosis who underwent surgical procedures (except liver transplantation) at the Mayo Clinic over an 11-year period (1980–1991).3 The mortality rate within 30 days of surgery was 11.6%. Long-term follow-up showed that most deaths occurred within the first few months after surgery, when many patients succumbed to pneumonia or renal insufficiency.
Risk factors have strong cumulative power
The study by Ziser et al also underscored the cumulative effect of risk factors, as the probability of developing a perioperative complication increased dramatically with the number of risk factors (as identified by multiavariate analysis) that a patient had, as follows3:
- 9.3% risk of complications with 1 risk factor
- 14.5% risk with 2 factors
- 33.5% risk with 3 factors
- 63.0% risk with 4 or 5 factors
- 73.3% risk with 6 factors
- 100% risk with 7 or 8 factors.
Postoperative complications: Beware hepatorenal syndrome
The most common postoperative complications in the study by Ziser et al were pneumonia, other infections, ventilation dependency, and ascites.3
Possibly the most ominous perioperative complication in a patient with liver disease is the onset of renal insufficiency, which may be precipitated by a number of factors, including nephrotoxic drugs and intraoperative hypotension. Renal insufficiency is usually a predictor of markedly reduced survival and a sign that hepatorenal syndrome may have developed.
Hepatorenal syndrome, which occurred in 3.3% of patients in the analysis by Ziser et al,3 is the presence of renal failure in a patient with cirrhosis. It is characterized by advanced liver failure and severe sinusoidal portal hypertension. The renal failure is said to be “functional” because significant histological changes are absent on kidney biopsy. Marked arteriolar vasodilation occurs in the extrarenal circulation with renal vasoconstriction leading to reduced glomerular filtration.
IMPORTANCE OF SURGICAL PROCEDURE TYPE
In addition to the patient-specific risk factors discussed above, certain surgical procedures deserve special consideration in patients with liver disease.
Cholecystectomy: Open vs closed
Patients with liver disease have the same indication for cholecystectomy as anyone else does: symptomatic gallstone disease. Patients with cirrhosis who are found to have incidental gallstones on ultrasonography should not undergo cholecystectomy unless the gallstones are symptomatic, as liver function may deteriorate after surgery.
For a patient with liver disease undergoing cholecystectomy, a common concern is whether an open or closed procedure should be done. Conventional wisdom had been that a patient with underlying liver disease (particularly cirrhosis) should have an open procedure so that the surgeon could more easily control bleeding, but that notion has changed in recent years with evidence supporting the safety of a laparoscopic approach in patients with liver disease.
One study supporting this new strategy is a retrospective review of 50 patients who had undergone cholecystectomy for symptomatic gallstone disease at the Mayo Clinic between 1990 and 1997.4 The procedure was open in half of the patients and laparoscopic in the other half. All patients had Child-Pugh class A or B cirrhosis. The indications for surgery were acute cholecystitis, biliary colic, or pancreatitis, and the number of patients with each of these indications was comparable between the open-surgery and laparoscopy groups. Three patients who initially underwent laparoscopy were converted to open cholecystectomy: two for bleeding and one for poor access. The study found that laparoscopic cholecystectomy was associated with statistically significant reductions in operating room time, blood loss, and length of hospital stay. No deaths occurred in either group. The authors concluded that laparoscopic cholecystectomy is safe in patients with cirrhosis and offers several advantages over an open surgical approach.
In light of these findings and other recent evidence, laparoscopic cholecystectomy should be recommended for patients with liver disease unless they have ascites or other evidence of overt hepatic decompensation, in which case cholecystectomy itself is contraindicated.
Cardiac surgery with bypass poses extra risk
Patients with liver disease undergoing open heart surgery with cardiopulmonary bypass are at especially high risk because of the effect on hepatic hemodynamics. This risk was demonstrated in a retrospective review of all patients with cirrhosis who underwent cardiac surgery with cardiopulmonary bypass at the Cleveland Clinic from 1992 to 2002.5 Of the 44 patients identified, 12 (27%) developed hepatic decompensation and 7 (16%) died. Hepatic decompensation was a major factor in all the deaths.
The MELD and Child-Pugh scores correlated well with one another in this study and were highly associated with hepatic decompensation and death. The best cutoff values for predicting mortality and hepatic decompensation were found to be a score greater than 7 in the Child-Pugh system and a score greater than 13 in the MELD system. (For context, receipt of a donor liver via a transplant list in the United States requires a MELD score of at least 15.) The study confirmed that the Child-Pugh score, which is easy to determine at the bedside, remains a reliable predictor of poor outcomes.5
CASE REVISITED: POSTOPERATIVE LIVER FUNCTION DECLINE―HOW SERIOUS IS IT?
Our patient undergoes the CABG procedure, and 3 days later you are asked to see him. According to the sub-intern, although the surgery was successful, the patient is now “in liver failure.” After hearing this news, the family is anxious to discuss liver transplantation.
On examination, the patient is alert and extubated, so he is clearly not encephalopathic. His wound is clean and shows no sign of infection. He appears to be mildly icteric, and he may have some ascites, based on mild flank dullness.
His laboratory test results are as follows:
- Bilirubin, 3.1 mg/dL (normal range, 0.3–1.2)
- INR, 1.2 (0.9–1.2)
- Alanine aminotransferase (ALT), 300 U/L (10–40)
- Creatinine, 0.9 mg/dL (0.6–1.2).
Although the bilirubin and ALT are elevated, it is notable that the creatinine is normal. This pattern is not uncommon after elective surgery in a patient with underlying cirrhosis. Renal dysfunction is the biggest concern in the perioperative management of a patient with liver disease, as it is an indicator that the patient may develop overt hepatic decompensation. Likely reasons for the patient’s ALT elevation are the effects of cardiopulmonary bypass and possible intraoperative hypotension.
The family needs to be told that the patient is not in liver failure and that it is best to wait with the expectation that he will do fine unless other complications supervene.
You advise cautious diuresis, and the ALT falls over the next few days. The bilirubin declines to 2.0 mg/dL. At this point, you advise discharge planning.
One need not wait for the bilirubin to return to normal: after an acute hepatic insult such as ischemic hepatitis or intraoperative hypotension, bilirubin is the last indicator to improve. Bilirubin is in part albumin-bound, and the half-life of albumin is 18 days, so a patient can remain icteric for some time after the rest of the liver function tests have returned to normal.
DISCUSSION
Question from the audience: What are your recommendations regarding platelet transfusion if the platelet count is less than 50,000 in a patient with liver disease?
Dr. Martin: For patients with thrombocytopenia, it is prudent to get the platelet count above 60,000 before any procedure. We will not even do a blind liver biopsy in a patient with a platelet count of less than 60,000.
Question from the audience: A study from the Annals of Surgery concludes that patients with liver disease do poorly with a hemoglobin of less than 10 g/dL. Would you transfuse aggressively before surgery?
Dr. Martin: For a patient with anemia, I don’t like to use aggressive transfusion if cirrhosis is present because the portal pressure may go up and increase the risk of variceal hemorrhage. If there is adequate time for a work-up, one can screen for varices by endoscopy. If there is evidence of overt hepatic decompensation and portal hypertension (esophageal varices, a palpable spleen, and thrombocytopenia), I wouldn’t try to get the hemoglobin much above 10 g/dL.
Question from the audience: How would you modify prophylaxis for deep vein thrombosis following hip or knee replacement surgery in patients with liver disease?
Dr. Martin: I would base it on the INR. Patients who are already mildly coagulopathic tend to be very sensitive to warfarin in the long term. For immediate perioperative prophylaxis, I would not administer anything if the patient had a platelet count below 60,000; otherwise I would probably proceed as usual.
Question from the audience: You said that we shouldn’t operate on patients with acute hepatitis, but we frequently encounter patients with drug-induced hepatitis, such as from anticholesterol drugs. These patients’ ALT and aspartate aminotransferase (AST) levels can remain elevated for 2 or 3 months. How long should we delay surgery? For example, is it dangerous to proceed with a mastectomy a month after discontinuing the drug if the liver enzymes are still around 100 U/L?
Dr. Martin: It’s worth noting that much of the literature on surgery in patients with acute viral hepatitis is 30 or 40 years old. If such a patient had a compelling reason to have surgery, you might wait until the liver enzymes were trending downward and you were confident that the patient was recovering.
Question from the audience: How do you manage patients who have varices or have had variceal bleeding in the past? Many of them are on beta-blockers, such as propranolol, which can cause hypotension intraoperatively.
Dr. Martin: The standard of care is to prescribe beta-blockers for a patient with large varices, or to ablate the varices by endoscopy, which is my practice. In general, I would discontinue propranolol on the morning of surgery. If possible, however, I would have the patient undergo endoscopy before surgery to assess the likelihood of short-term variceal bleeding. If the varices look to be at low risk of bleeding, the beta-blocker can safely be stopped. If they look to be at high risk of bleeding, the surgery should be delayed for a few weeks, if possible, so that the varices can be ablated, which usually takes two or three sessions.
Question from the audience: I deal with many referrals, and I struggle with how aggressive a work-up I should do for patients undergoing elective surgery when a new abnormality is found in one of their liver function tests.
Dr. Martin: I would try to establish whether the abnormality is a chronic problem. Has the patient been told about an abnormal liver test in the past? Ask if the patient has been a blood donor, as measurement of ALT and some hepatitis serologies would have been required. Also ask if he or she has ever taken out a big life insurance policy, which also would have required liver function testing. If the abnormality is chronic, you may proceed with surgery if the bilirubin and INR are normal. In the absence of chronicity, surgery should be delayed for further work-up only in patients with indicators of significant liver disease—either markedly abnormal liver tests, thrombocytopenia, or coagulopathy.
Follow-up question: But patients rarely know whether they’ve had elevated liver enzymes in the past. You said not to worry about enzyme abnormalities unless they are markedly elevated, but how high is that?
Dr. Martin: AST and ALT are indicators of liver injury rather than of synthetic function. The true liver function tests are really albumin, bilirubin, and prothrombin time. Paradoxically, one of the best liver function tests is the platelet count. For me, a red flag for a patient with newly recognized liver disease is any degree of thrombocytopenia or coagulopathy or an elevation of bilirubin above the upper limit of normal. A patient with a platelet count of 90,000 and an INR above 1.2 has significant underlying liver disease, and I would be very concerned. Unless it’s a dire emergency, such a patient would need further evaluation before proceeding with surgery. In contrast, a patient with an ALT of 89, an AST of 65, and normal prothrombin time and platelet count should be safe to proceed to surgery. But such a patient needs an evaluation for liver disease afterward.
Question from the audience: My institution performs many liver resections for metastases or primary liver cancers. Our liver surgeons routinely discontinue statins 2 to 3 weeks before liver surgery, but it has been said at this summit that is not necessary. What’s your opinion?
Dr. Martin: I think that statins get a very bad rap in terms of hepatotoxity. Most patients with metabolic syndrome have hyperlipidemia, which can cause fatty liver disease and hepatic dysfunction. Statins help bring the lipid levels down. Hepatologists do not regard statins as major culprits in causing liver problems. I don’t believe there’s any particular indication to stop them before a patient undergoes hepatic surgery.
Question from the audience: I assess patients 1 or 2 weeks before surgery. For a patient with coagulopathy whom you suspect has underlying liver disease, is there any value in trying to treat the coagulopathy with vitamin K?
Dr. Martin: It can be worthwhile to try 10 mg subcutaneously for 3 days to see whether the situation improves, but if the patient has severe parenchymal liver disease, the vitamin K won’t help much.
- Ginés P, Quintero E, Arroyo V, et al. Compensated cirrhosis: natural history and prognostic factors. Hepatology 1987; 7:122–128.
- MELD/PELD calculator. United Network for Organ Sharing Web site. http://www.unos.org/resources/MeldPeldCalculator.asp?index=98. Accessed May 8, 2009.
- Ziser A, Plevak DJ, Wiesner RH, Rakela J, Offord KP, Brown DL. Morbidity and mortality in cirrhotic patients undergoing anesthesia and surgery. Anesthesiology 1999; 90:42–53.
- Poggio JL, Rowland CM, Gores GJ, et al. A comparison of laparoscopic and open cholecystectomy in patients with compensated cirrhosis and symptomatic gallstone disease. Surgery 2000; 127:405–411.
- Suman A, Barnes DS, Zein NN, et al. Predicting outcome after cardiac surgery in patients with cirrhosis: a comparison of Child-Pugh and MELD scores. Clin Gastroenterol Hepatol 2004; 2:719–723.
- Ginés P, Quintero E, Arroyo V, et al. Compensated cirrhosis: natural history and prognostic factors. Hepatology 1987; 7:122–128.
- MELD/PELD calculator. United Network for Organ Sharing Web site. http://www.unos.org/resources/MeldPeldCalculator.asp?index=98. Accessed May 8, 2009.
- Ziser A, Plevak DJ, Wiesner RH, Rakela J, Offord KP, Brown DL. Morbidity and mortality in cirrhotic patients undergoing anesthesia and surgery. Anesthesiology 1999; 90:42–53.
- Poggio JL, Rowland CM, Gores GJ, et al. A comparison of laparoscopic and open cholecystectomy in patients with compensated cirrhosis and symptomatic gallstone disease. Surgery 2000; 127:405–411.
- Suman A, Barnes DS, Zein NN, et al. Predicting outcome after cardiac surgery in patients with cirrhosis: a comparison of Child-Pugh and MELD scores. Clin Gastroenterol Hepatol 2004; 2:719–723.
KEY POINTS
- Patients with acute hepatitis should delay elective surgery until after their hepatitis resolves.
- Patients with chronic liver disease who have developed any index complication—variceal hemorrhage, ascites, hepatic encephalopathy, or jaundice—are at increased risk for postoperative complications and death.
- The Child-Pugh and MELD scores appear to be comparably effective in predicting surgical outcomes in patients with liver disease.
- Cardiac surgery with cardiopulmonary bypass and abdominal surgery are particularly high-risk procedures in patients with liver disease.
- If cholecystectomy is indicated in a patient with compensated liver disease, laparoscopy should be the initial approach, with conversion to an open procedure only if necessary.