User login
HISTORY
A 64 year-old man is referred to dermatology for investigation of a non-healing asymptomatic lesion present on his left ear for slightly less than a year. His history included his having had a number of basal cell carcinomas removed from his face over the years, and, of course, a history of excessive sun exposure as a young man.
Additional history-taking revealed his having had a kidney transplant 5 years previously, for which he was still under the care of the transplant team, including taking immunosuppressive medications. He had been warned by his transplant providers of the increased risk of skin cancers associated with these medications.
EXAMINATION
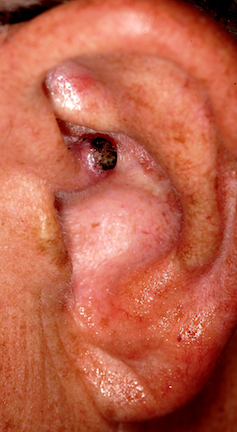
A 1 cm friable nodule on the left helical crus could readily be seen, covered by thin eschar, with a faintly red base. Abundant evidence of ancient sun damage could be seen on the ear and face, including telangiectasias and solar lentigines. No nodes or other masses could be detected on palpation of the periauricular and neck regions. A generous shave biopsy of this lesion showed clear evidence of a moderately well-differentiated squamous cell carcinoma.
DISCUSSION
Squamous cell carcinoma (SCC) is the second-most common skin cancer, after basal cell carcinoma (BCC), but unlike the latter, SCC has a very real chance of leading to metastasis and death. 8,000 cases of nodal involvement occur in this country every year, 3,000 of which result in death from metastasis to the brain and/or lung. In general, the more well-differentiated the cancer (similar-appearing cells), the better the prognosis, but the more poorly differentiated the cells are (dissimilar appearance), the greater the chance for invasion and spread.
But several other factors determine the prognosis for any given SCC. Each anatomic site has its own pattern of spread and prognosis. In this particular case, the proximity of the cancer to the external auditory meatus predicts an increased potential for local or nodal spread. Moreover, the patient’s suppressed immune system increases the risk even further.
Approximately 15% of all SCCs occur on upper extremities, but these tend to be relatively safe, especially when sun-caused. Non-solar causation of SCC, such as from HPV, chronic arsenic exposure, or over-exposure to ionizing radiation, tends to have a worse prognosis, especially if it occurs near orifices such as the ear, vagina, mouth or in anogential regions. The size of the tumor matters as well, with tumors greater than 2 cm being increasingly prone to local invasion and metastasis compared to smaller lesions. Beyond these factors, variations in the biologic activity of individual SCCs can be unpredictable, making all SCCs considerably more worrisome than BCCs.
Relatively safe forms of SCC are common, and include intraepidermal SCC in situ, also known as Bowen’s disease, which presents as a slowly growing, fixed papulosquamous plaque on sun-exposed skin. As with all forms of sun-caused SCC, Bowen’s in more common in older, chronically sun-damaged patients.
The lateral and vertical dimensions of this man’s SCC were determined by the Mohs surgeon who excised the lesion, examining the margins of the excised tissue to insure complete removal and to detect any deeper involvement of cartilage or potential perineural involvement. Fortunately, these were not seen in his case, but the operative site was treated with radiation of the site because of the uncertainty caused by his immunosuppressive state.
Obviously, SCCs are not confined to the skin, occurring in a wide variety of areas such as the cervix, lung and oral cavity. The comments made above regarding SCC of the skin have little if any bearing on the diagnosis and treatment of internal squamous cell carcinoma, a subject far beyond the scope of this article.
LEARNING POINTS
1) Any cell in human skin can undergo malignant transformation
2) The tendency to develop SCC is held in check in part by an intact immune system.
3) Non-solar causes of SCC include HPV, chronic exposure to arsenic, and ionizing radiation exposure.
4) SCC, because of its potential for metastasis, is considered more dangerous than BCC.
5) Transplant patients are especially prone to SCC.
HISTORY
A 64 year-old man is referred to dermatology for investigation of a non-healing asymptomatic lesion present on his left ear for slightly less than a year. His history included his having had a number of basal cell carcinomas removed from his face over the years, and, of course, a history of excessive sun exposure as a young man.
Additional history-taking revealed his having had a kidney transplant 5 years previously, for which he was still under the care of the transplant team, including taking immunosuppressive medications. He had been warned by his transplant providers of the increased risk of skin cancers associated with these medications.
EXAMINATION
A 1 cm friable nodule on the left helical crus could readily be seen, covered by thin eschar, with a faintly red base. Abundant evidence of ancient sun damage could be seen on the ear and face, including telangiectasias and solar lentigines. No nodes or other masses could be detected on palpation of the periauricular and neck regions. A generous shave biopsy of this lesion showed clear evidence of a moderately well-differentiated squamous cell carcinoma.
DISCUSSION
Squamous cell carcinoma (SCC) is the second-most common skin cancer, after basal cell carcinoma (BCC), but unlike the latter, SCC has a very real chance of leading to metastasis and death. 8,000 cases of nodal involvement occur in this country every year, 3,000 of which result in death from metastasis to the brain and/or lung. In general, the more well-differentiated the cancer (similar-appearing cells), the better the prognosis, but the more poorly differentiated the cells are (dissimilar appearance), the greater the chance for invasion and spread.
But several other factors determine the prognosis for any given SCC. Each anatomic site has its own pattern of spread and prognosis. In this particular case, the proximity of the cancer to the external auditory meatus predicts an increased potential for local or nodal spread. Moreover, the patient’s suppressed immune system increases the risk even further.
Approximately 15% of all SCCs occur on upper extremities, but these tend to be relatively safe, especially when sun-caused. Non-solar causation of SCC, such as from HPV, chronic arsenic exposure, or over-exposure to ionizing radiation, tends to have a worse prognosis, especially if it occurs near orifices such as the ear, vagina, mouth or in anogential regions. The size of the tumor matters as well, with tumors greater than 2 cm being increasingly prone to local invasion and metastasis compared to smaller lesions. Beyond these factors, variations in the biologic activity of individual SCCs can be unpredictable, making all SCCs considerably more worrisome than BCCs.
Relatively safe forms of SCC are common, and include intraepidermal SCC in situ, also known as Bowen’s disease, which presents as a slowly growing, fixed papulosquamous plaque on sun-exposed skin. As with all forms of sun-caused SCC, Bowen’s in more common in older, chronically sun-damaged patients.
The lateral and vertical dimensions of this man’s SCC were determined by the Mohs surgeon who excised the lesion, examining the margins of the excised tissue to insure complete removal and to detect any deeper involvement of cartilage or potential perineural involvement. Fortunately, these were not seen in his case, but the operative site was treated with radiation of the site because of the uncertainty caused by his immunosuppressive state.
Obviously, SCCs are not confined to the skin, occurring in a wide variety of areas such as the cervix, lung and oral cavity. The comments made above regarding SCC of the skin have little if any bearing on the diagnosis and treatment of internal squamous cell carcinoma, a subject far beyond the scope of this article.
LEARNING POINTS
1) Any cell in human skin can undergo malignant transformation
2) The tendency to develop SCC is held in check in part by an intact immune system.
3) Non-solar causes of SCC include HPV, chronic exposure to arsenic, and ionizing radiation exposure.
4) SCC, because of its potential for metastasis, is considered more dangerous than BCC.
5) Transplant patients are especially prone to SCC.
HISTORY
A 64 year-old man is referred to dermatology for investigation of a non-healing asymptomatic lesion present on his left ear for slightly less than a year. His history included his having had a number of basal cell carcinomas removed from his face over the years, and, of course, a history of excessive sun exposure as a young man.
Additional history-taking revealed his having had a kidney transplant 5 years previously, for which he was still under the care of the transplant team, including taking immunosuppressive medications. He had been warned by his transplant providers of the increased risk of skin cancers associated with these medications.
EXAMINATION
A 1 cm friable nodule on the left helical crus could readily be seen, covered by thin eschar, with a faintly red base. Abundant evidence of ancient sun damage could be seen on the ear and face, including telangiectasias and solar lentigines. No nodes or other masses could be detected on palpation of the periauricular and neck regions. A generous shave biopsy of this lesion showed clear evidence of a moderately well-differentiated squamous cell carcinoma.
DISCUSSION
Squamous cell carcinoma (SCC) is the second-most common skin cancer, after basal cell carcinoma (BCC), but unlike the latter, SCC has a very real chance of leading to metastasis and death. 8,000 cases of nodal involvement occur in this country every year, 3,000 of which result in death from metastasis to the brain and/or lung. In general, the more well-differentiated the cancer (similar-appearing cells), the better the prognosis, but the more poorly differentiated the cells are (dissimilar appearance), the greater the chance for invasion and spread.
But several other factors determine the prognosis for any given SCC. Each anatomic site has its own pattern of spread and prognosis. In this particular case, the proximity of the cancer to the external auditory meatus predicts an increased potential for local or nodal spread. Moreover, the patient’s suppressed immune system increases the risk even further.
Approximately 15% of all SCCs occur on upper extremities, but these tend to be relatively safe, especially when sun-caused. Non-solar causation of SCC, such as from HPV, chronic arsenic exposure, or over-exposure to ionizing radiation, tends to have a worse prognosis, especially if it occurs near orifices such as the ear, vagina, mouth or in anogential regions. The size of the tumor matters as well, with tumors greater than 2 cm being increasingly prone to local invasion and metastasis compared to smaller lesions. Beyond these factors, variations in the biologic activity of individual SCCs can be unpredictable, making all SCCs considerably more worrisome than BCCs.
Relatively safe forms of SCC are common, and include intraepidermal SCC in situ, also known as Bowen’s disease, which presents as a slowly growing, fixed papulosquamous plaque on sun-exposed skin. As with all forms of sun-caused SCC, Bowen’s in more common in older, chronically sun-damaged patients.
The lateral and vertical dimensions of this man’s SCC were determined by the Mohs surgeon who excised the lesion, examining the margins of the excised tissue to insure complete removal and to detect any deeper involvement of cartilage or potential perineural involvement. Fortunately, these were not seen in his case, but the operative site was treated with radiation of the site because of the uncertainty caused by his immunosuppressive state.
Obviously, SCCs are not confined to the skin, occurring in a wide variety of areas such as the cervix, lung and oral cavity. The comments made above regarding SCC of the skin have little if any bearing on the diagnosis and treatment of internal squamous cell carcinoma, a subject far beyond the scope of this article.
LEARNING POINTS
1) Any cell in human skin can undergo malignant transformation
2) The tendency to develop SCC is held in check in part by an intact immune system.
3) Non-solar causes of SCC include HPV, chronic exposure to arsenic, and ionizing radiation exposure.
4) SCC, because of its potential for metastasis, is considered more dangerous than BCC.
5) Transplant patients are especially prone to SCC.