User login
Clinical pharmacists have expanded their role over the past few decades in both outpatient and inpatient settings and are now members of an interdisciplinary health care team that includes nutritionists, physical therapists, physicians, and nurses.1,2 The emergency department (ED), however, has lagged behind in the inclusion of pharmacists.3 Despite well documented financial and ED operational benefits of pharmacists and the recommendation of their inclusion by the Institute of Medicine, only about 30% of academic EDs in a 2009 survey employed a pharmacist.4-8 A larger 2005 survey of 510 hospital pharmacy directors revealed that only 3.5% of hospitals sampled (academic and nonacademic) provided clinical pharmacy services in the ED.9
About 3.8 million annual preventable medical errors occur in the ED, giving the ED the highest rate of medication errors among all hospital departments.4 In 2000, Schenkel found that 3% of all inpatient medication errors were initiated in the ED.10 Similarly, Chin and colleagues found that 3.6% of elderly patients were administered an inappropriate medication in the ED with 5.6% receiving an inappropriate prescription at discharge.11
In a 2008 study conducted at the Durham VAMC in North Carolina, Hastings and colleagues found that suboptimal pharmacy was common among elderly veterans discharged from the ED (11%) and that potentially inappropriate medication use was associated with a 32% greater risk of repeat ED visits, hospitalization, or death (P = .10).12 In 2010, Rothschild and colleagues found 7.8 medication errors per 100 ED patients or 2.9 errors per 100 prescribed medications.13 Despite this unacceptably high rate of medication errors, most EDs do not employ pharmacy specialists or have a pharmacist easily available for consultation—options that could not only streamline ED operations, but also reduce patient risk.
The pharmacist role in the ED has changed considerably. In the 1970s, ED pharmacists were used mainly to dispense medicine, maintain inventories, and participate in cardiopulmonary resuscitation.3,14,15 Today, following the guidelines set by the American Society for Health-System Pharmacists, emergency pharmacists have an expanded, more direct role in patient care and evaluation and support of the physicians and other ED staff who work alongside them.4,14,16,17 Pharmacists gather accurate and complete medication histories, review and reconcile medication lists, and screen ED medication orders for errors or anticipated drug interactions.13,18-23 They adjust medication doses on a patient-by-patient basis, accounting for renal and hepatic clearance and closely monitor patients for treatment response. They also provide one-on-one patient education on medication dosing, administration, adverse drug events (ADEs), and interactions, increasing patients’ drug knowledge and adherence.17,24 Pharmacists provide information to patients on vaccinations and medication assistance programs, which is unlikely to be shared by other providers.3,19,20 Pharmacists in the ED reduce medication delays and omissions that occur in admitted patients staying in the ED.25,26
Aside from patient education, clinical pharmacists have an important role in providing education and consultation to ED physicians, midlevel providers, and house staff on topics that include availability of new medications and local antibiotic resistance patterns.14,27-29 Additionally, pharmacists monitor drug supplies and restock medications to avoid shortages during critical moments, offer the ED perspective in hospital formulary reviews, and increase efficiency and throughput in the ED while decreasing costs by evaluating and treating patients who present simply for prescription refills alongside a supervising physician.14
With this in mind, the ED of the Atlanta VAMC in Decatur, Georgia, conducted a pilot study to assess the financial and logistic feasibility of a full-time pharmacist in the ED setting with the hope that a pharmacist would integrate well into the health care team, reducing overall departmental expense and the risk of medication error associated with patient harm and simultaneously improving patient satisfaction and departmental efficiency.
Methodology
The ED of the Atlanta VAMC is part of a tertiary care teaching hospital affiliated with both the Emory and Morehouse schools of medicine. At the time of the pilot, the facility had 128 acute care medical/surgical beds, 12 inpatient palliative care beds, 40 acute care psychiatric beds, 24 medical surgical intensive care unit beds, and 60 inpatient nursing home beds. The ED provides care to > 37,000 veterans annually, and in December 2011 when this study was conducted, 3,195 veterans were seen in the ED.
The ED was divided into the main ED and the urgent care. Patient intake occurred through a centralized triage, and based on acuity, patients were sent to the appropriate setting for treatment. The ED used a 5-tier triage system. Patients with triage levels 1, 2, and 3 were sent to the main ED, and patients with triage levels 4 and 5 were sent to the urgent care.
Pharmacists
Pharmacy services were provided by 5 residency-trained doctors of pharmacy employed by the medical center working as clinical pharmacists with the inpatient medical teams at the time of the pilot. The pilot was conducted over a 2-week period in December 2011, Monday through Friday, for a total of 10 days. The clinical pharmacists divided the days among themselves. Each pharmacist provided services for a total of 2 days, 3 hours per day, from about 3 pm to 6 pm. The pharmacists were given a room previously used as a physician workroom in which to evaluate patients.
Patient Selection
Patients to be seen by the clinical pharmacist were chosen by the triage nurse, the charge nurse, the ED physician, the urgent care provider (physician or midlevel provider), or by the pharmacists. The triage nurse or charge nurse, based on chief medical problem and acuity, chose patients directly out of triage. Only patients with triage acuity level 4 or 5 were taken directly from triage without first seeing a physician or midlevel provider. These patients presented with the chief problem of medication refill or coumadin/International Normalized Ratio check. Once chosen as appropriate for the clinical pharmacist, the charge nurse helped with patient flow, and if the pharmacist was occupied with other patients, the nurse redirected the patient to urgent care.
Additional patients were chosen to see the clinical pharmacist after an evaluation of their initial problem was completed by a physician or midlevel practitioner in the urgent care or main ED. Patients whom the provider felt could benefit from any of the following services were directed to the clinical pharmacist: anticoagulation consult, diabetic education, pharmacokinetic consult, medication history, medication reconciliation, formulary management, medication refills, therapeutic interchange, screening for drug interactions, allergy review, and nonformulary or restricted medications requests. Additionally, the clinical pharmacist reviewed the charts of patients in the main ED whom they were not asked to see. They offered assistance when needed in all the aforementioned areas and for order clarification, assuring IV compatibility, reporting medication errors and ADEs, promotion of safe medical practices, and elimination of duplicate/redundant medications.
Data Collection
The pharmacists developed a log to record their activities. The log included the date and time of the intervention, number of minutes spent with the patient, the reason for intervention, and recommendations, if applicable. They categorized their interventions into 16 categories: anticoagulation, pharmacokinetics, drug information, order clarification, medication reconciliation, therapeutic interchange, formulary management, medication history, IV compatibility, screening for drug interactions, patient education, allergy documentation, promotion of safe medical practices, reporting of medication error/ADEs, nonformulary and restricted medication requests, and prescription refills. Patients could receive more than 1 intervention.
Though not a focus of this pilot, all patients seen by a pharmacist received a postencounter survey seeking their opinion on whether the pharmacist improved the value of their visit.
Review Process
At the conclusion of the pilot, 2 independent reviewers, both physicians, reviewed the logs, and each task was reassigned to 1 of 8 categories. These categories included either medication refills or 1 of 7 other areas that had established cost avoidance estimates from 2 other well accepted studies (Lee and colleagues and Ling and colleagues).30,31 These 7 categories included adjusting dose or frequency of medication, elimination of duplication of therapy, education/information inquiry, formulary management, prevention and management of ADEs, prevention or management of allergies, and therapeutic interchange. If the independent reviewers did not have initial concordance of classification of the intervention, they discussed the intervention and came to an agreement.
Cost Analysis
Cost avoidance estimates for 7 individual interventions were made, using data from Lee and colleagues and Ling and colleagues.30,31 Four of these came from the study by Lee and colleagues: prevent or manage drug allergy, adjust dosage or frequency, prevent or manage ADEs, and eliminate duplication of therapy.30 Lee and colleagues’ “drug interaction” group was not clearly defined, thus this was included with the “prevent or manage ADE” group. Ling and colleagues provided data for the 3 additional groups of interventions that pharmacists performed: education and information inquiry, formulary management, and therapeutic interchange.31
Financial estimates of cost avoidance were adjusted for inflation, using the consumer price index (CPI) of the U.S. Bureau of Labor Statistics.32 The Lee study was conducted in 2002, and estimates for cost avoidance using their model were adjusted to 2011 values using the CPI inflation rate of 25%. The Ling study was conducted in 2005, and estimates for cost avoidance using their model were adjusted for 2011 values using the CPI rate of inflation of 15.2%.32
For the remaining intervention, prescription refill, cost savings was determined by calculating the average times spent by the ED pharmacist on each intervention and then using the difference between hourly physician and pharmacist pay (about $50/h difference based on VA wage tables).
RESULTS
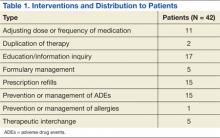
During the 30-hour total time in which a pharmacist was present in the ED, a total of 42 patients were assisted through 71 interventions (Table 1).
Pharmacists provided a diverse range of services to patients in the ED. The most common intervention was education and/or information inquiry. Tasks in this category included patient education about medication dosing, administration, AEs, interactions and warnings, as well as diabetes management. In several instances, education was provided to attending physicians or house staff, though it should be noted that this provider education was not counted as an intervention for this study unless it was associated with a patient (of which there were 3 total instances, eg, instruction on how to choose the proper insulin syringe).
Interventions, when a medication list was screened by the ED pharmacist for interactions or when drug choices were recommended to the physician or midlevel providers, were counted as prevention and management of ADEs. For example, the pharmacist noted a patient with a new diagnosis of gout who was prescribed hydrochlorothiazide; this was brought to the attention of the provider and alternative antihypertensives were suggested. In another instance, a patient was found to be on both ibuprofen and enoxaparin; the treating physician was alerted of this potential interaction. There were 15 such events in total.
Several other interventions arose from the screenings for ADEs, including adjusting dose or frequency of medication (11); therapeutic interchange (5); eliminating duplication of therapy (2); and prevention or management of allergies (1). Cases included hepatic and/or renal dose changes, substituting equivalent medications for better treatment outcome or adherence, or discontinuing 2 or more medications in a patient’s medication profile that were considered duplication.
During the pharmacist screening, one patient who had piperacillin/tazobactam ordered in the ED had a penicillin allergy. This intervention was categorized as prevention and management of an ADE as well as prevention and management of allergies. Interventions not accompanied by the “prevention of ADE” category included those in which the change did not provide a clear risk reduction. For example, one therapeutic interchange was from levofloxacin to moxifloxacin for a better-anticipated therapy. Another was a metformin dose increase, presumably for improved glycemic control.
Prescription refills occurred with the same frequency as prevention of ADEs.15 This intervention led in some cases to switching to pharmaceutical equivalents when a drug prescribed at another facility was not on the formulary. Other drugs that were not on the preferred list but available with nonformulary medication requests were ordered or approved with the assistance of the pharmacist. The pharmacist’s direct involvement significantly reduced the initial contact-to-approval time for these patients.
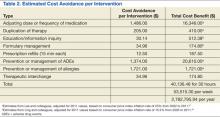
After tallying the total number of interventions, the potential financial cost savings to the ED were determined (Table 2). As mentioned previously, the Lee and Ling studies provided the categories for classification of 7 pharmacist interactions. The estimated cost avoidance for the 4 applicable groups from the Lee study had inflation-corrected values of $1,486 per adjusted dose or frequency of medication, $205 per elimination of duplication of therapy, $1,374 per prevention or management of ADEs, and $1,721 per prevention or management of allergies.30
The estimated cost avoidance for the 3 applicable groups from the Ling study had inflation-corrected values of $512.38 per education/information inquiry, $174.80 per formulary management, and $174.80 per therapeutic interchange.31 The eighth group, prescription refills, was valued at $12.50 each, using the difference between physician and pharmacist salary for an average of 15 minutes per interaction.
When multiplied by the number of interventions in each of these groups, the total potential cost avoidance in the study period was about $40,136.48. Extrapolated into a yearly amount, that is a $2,782,795.94 potential cost savings for the medical center.
Seventeen of the 42 (40.5%) postencounter surveys from the patients seen by the pharmacists were received. Of these veterans, 100% reported that they were “extremely satisfied” with the treatment they had received during their visit to the ED.
DISCUSSION
There is the potential for significant cost avoidance by adding a single full-time pharmacist to the ED: Annually, more than $2.7 million in potential savings for the medical center. Though surprising, this figure is actually in line with the much larger study by Lada and colleagues in which an estimated $3 million was avoided.15 At the same hospital 12 years earlier, Levy noted about $1 million in cost avoidance (not inflation-adjusted).33 The Ling study, however, did not have as high a figure, with annual cost avoidance estimated at $600,000.31 All these figures are based on estimates and, therefore, imprecise, but it is clear even using the most conservative model that the cost to employ a clinical pharmacist is justified.
The final value of cost savings is likely significantly underestimated relative to non-VA hospitals due to the decision to correct for inflation, using the total market inflation rate rather than the medical sector inflation rate over the same time period. The Lee study values were increased by 25.0% and the Ling study values by 15.2%, to bring them to 2011 amounts. Using the medical inflation rate instead (42.3% and 25.2%, respectively), an additional $378,000 in annual savings would have been realized. The lower CPI inflation rate rather than the higher rate in the medical sector was chosen to make the cost avoidance outcomes more conservative.
The true value of a clinical pharmacist comes from the services they provide to patients. In this pilot, as well as in several others, it has been shown that education is a commonly performed and highly valued task. Education was a service lacking in this ED prior to this intervention due to financial and logistical constraints. It is unclear how much instruction patients receive at the outpatient pharmacy while picking up medications after leaving the ED, but it is likely limited, given the large volumes and long lines often found at the in-house pharmacy. Education has a demonstrated effect on prevention and management of ADEs and was the most interactive of the interventions the pharmacist provided during this study. This type of intervention was most likely the source of increased patient satisfaction that was noted in the postencounter surveys.17,24
Prevention of ADEs, which was a frequent intervention in this pilot, has been noted by many sources to be the single most beneficial task performed by a clinical pharmacist both from financial and risk reduction standpoints.13,21-23 Although not able to assess patient outcomes after this limited pilot, the authors anticipate such an evaluation when a full-time ED pharmacist joins the department.
The Joint Commission recommends that a pharmacist review all medication orders before administration, though there is an exception for the emergency setting.34 The Joint Commission also recommends medication reconciliation at every visit, including those in the ED setting. The addition of a clinical pharmacist would increase compliance with this and other standards and bring ED operations up to the same benchmark as other practice settings.
LIMITATIONS
The most significant limitation of this study was sample size. The volunteered time of the pharmacists in the ED totaled only 30 hours over 2 weeks. In that limited time, however, the pharmacists had more patient interactions than were anticipated. Had the pilot been conducted over a longer period, it is unclear whether this would have been sustained or whether this was a coincidental overestimate of the effect that a full-time pharmacist would have on the department. Likely, it is an underestimate of their potential, as the availability of the pharmacist was novel and likely underused by other providers. Given more time with the ED staff, pharmacists would be more frequently called on for their expertise, because their skills and knowledge set would be better understood. During this pilot, the pharmacist was located in a separate room in the ED where not all ED staff knew they were available for consultation.
The other major limitation of the pilot was the inherent imprecision of cost avoidance estimates. The dollar amounts attributed to the duties fulfilled by the pharmacists relied on 2 studies. The first, by Lee and colleagues, provided cost avoidance estimates of certain pharmacist actions based on a combination of 4 to 5 clinicians’ estimates of risk reduction, combined with their individual location’s costs for hospitalization, laboratory tests, diagnostic procedures, medications, telephone care, clinic visits, and emergency department visits.30 The numbers are based not only on a small number of individual estimations of risk, but also on facility costs that are highly variable. Despite this, the authors believe the estimates are actually on the conservative side, since they do not account for costs of lost productivity and/or litigation.
The current pilot was performed in a different type of setting than the one by Lee. That study was conducted in a similar VAMC setting, but their study data were obtained from other areas of the medical center. Of 600 pharmacist interventions, 250 were in an outpatient clinic, 250 were in an inpatient setting, and 100 were in a nursing home.30 Despite this, the estimates are likely still relevant to this study, given that drugs used in the ED are often a mix of inpatient and outpatient ones, with the same risks to an individual regardless of where they are initiated, changed, or discontinued.
The study by Ling and colleagues was performed in an ED setting more closely matching this study’s setting and was a larger, well powered study. As with the Lee study, it was difficult if not impossible to obtain exact numbers on the expenses each pharmacist recommendation spared the hospital and/or patients.31 Not all drug interactions avoided would have led to symptoms, reevaluation, or hospitalization.35 Not all drug “allergies” avoided are true allergies (as seen dramatically by Raja and colleagues), and thus this action may not have spared any cost at all.36 In the end, however, the estimates provided by both studies are averaged over many patients and thus provided the best numbers available.
Unlike the Lee study, this pilot did not evaluate the medication cost differences between original treatment and the new recommended treatment. Given the small number of patients with whom significant changes were made in this study, evaluating the cost differences between the treatments would likely be insignificant. A larger study, such as Lee, was much more sufficiently powered to evaluate such a figure.30
Of note, in this pilot there were no cases seen in which there was any change in route of delivery, ie, IV to equivalent po treatments. This is typically a large source of cost savings secondary to reduction in equipment and nursing time. The Lada study found 66 such changes among 2,150 pharmacist interventions in the ED.15 The authors hypothesize that had their pilot been conducted over a longer period, significant cost savings would have resulted from similar interventions.
In this pilot, a significant number of patients presented for prescription refills. Veterans often prefer to fill medications at the VA pharmacy because of reduced cost and often bring prescriptions written by private sector physicians. These veterans are required to have a primary care physician assigned within the VA, but until they have their initial intake appointment, they use the ED for these prescriptions. Additionally, veterans from other VA locations presenting as visitors to the area or relocating to the city and not yet assigned to a primary care physician require their medication lists from other location(s) be accessed and reentered into intrafacility computerized ordering systems. Given these particulars of VA operation, the authors’ facility assuredly sees more patients presenting for prescription refill than nongovernment facilities. Thus our savings with this particular task may not be generalizable to settings outside the VA, at least in as high a number of encounters.
CONCLUSIONS
About 37,000 veterans received care at the ED of the Atlanta VAMC in 2011. Given these numbers and the evidence that EDs have some of the highest rates of preventable ADEs of any clinical environment, the presence of a clinical pharmacist in the ED is a necessary intervention, based on safety considerations alone. In addition to providing a needed layer of safety in the vulnerable ED environment, a clinical pharmacist likely provides a cost saving benefit to the ED, as demonstrated by this pilot and other studies. Further, the overwhelmingly positive response to this pilot by the veterans who participated shows that they want and need this service. Adding a clinical pharmacist to the ED is integral to the VA mission of providing patient-centered care. A larger study to obtain a more precise cost savings benefit within the VA system should be considered.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Schumock GT, Butler MG, Meek PD, et al. Evidence of the economic benefit of clinical pharmacy services: 1996-2000. Pharmacotherapy. 2003;23(1):113-132.
2. Pedersen CA, Schneider PJ, Scheckelhoff DJ. ASHP national survey of pharmacy practice in hospital settings: Prescribing and transcribing—2010. Am J Health Syst Pharm. 2011;68(8):669-688.
3. Rudis MI, Attwood RJ. Emergency medicine pharmacy practice. J Pharm Pract. 2011; 4(2):135-145.
4. Clancy CM. Evidence shows cost and patient safety benefits of emergency pharmacists. Am J Med Qual. 2008;23(3):231-233.
5. Fairbanks RJ, Hays DP, Webster DF, et al. Clinical pharmacy services in an emergency department. Am J Health Syst Pharm. 2004;61(9):934-937.
6. Abu-Ramaileh AM, Shane R, Churchill W, Steffenhagen A, Patka J, Rothschild JM. Evaluating and classifying pharmacists’ quality interventions in the emergency department. Am J Health Syst Pharm. 2011;68(23):2271-2275.
7. Committee on the Future of Emergency Care in the United States Health System. Hospital-Based Emergency Care: At the Breaking Point. Washington, DC: National Academies Press; 2006.
8. Szczesiul JM, Fairbanks RJ, Hildebrand JM, Hays DP, Shah MN. Survey of physicians regarding clinical pharmacy services in academic emergency departments. Am J Health Syst Pharm. 2009;66(6):576-579.
9. Pedersen CA, Schneider PJ, Scheckelhoff DJ. ASHP national survey of pharmacy practice in hospital settings: Dispensing and Administration—2005. Am J Health Syst Pharm. 2006;63(4):327-345.
10. Schenkel S. Promoting patient safety and preventing medical error in emergency departments. Acad Emerg Med. 2000;7(11):1204-1222.
11. Chin MH, Wang LC, Jin L, et al. Appropriateness of medication selection for older persons in an urban academic emergency department. Acad Emerg Med. 1999;6(12):1232-1242.
12. Hastings SN, Schmader KE, Sloane RJ, et al. Quality of pharmacotherapy and outcomes for older veterans discharged from the emergency department. J Am Geriatr Soc. 2008;56(5):875-880.
13. Rothschild JM, Churchill W, Erickson A, et al. Medication errors recovered by emergency department pharmacists. Ann Emerg Med. 2010;55(6):513-521.
14. Eppert HD, Reznek AJ; American Society of Health-System Pharmacists. ASHP guidelines on emergency medicine pharmacist services. Am J Health Syst Pharm. 2011;68(23):e81-95.
15. Lada P, Delgado G Jr. Documentation of pharmacists’ interventions in an emergency department and associated cost avoidance. Am J Health Syst Pharm. 2007;64(1):63-68.
16. Cohen V, Jellineck SP, Hatch A, Motov S. Effect of clinical pharmacists on care in the emergency department: A systematic review. Am J Health Syst Pharm. 2009;66(15):1353-1361.
17. Randolph TC. Expansion of pharmacists’ responsibilities in an emergency department. Am J Health Syst Pharm. 2009;66(16):1484-1487.
18. Hayes BD, Donovan JL, Smith BS, Hartman CA. Pharmacist-conducted medication reconciliation in an emergency department. Am J Health Syst Pharm. 2007;64(16):1720-1723.
19. DeWinter S, Spriet I, Indevuyst C, et al. Pharmacist-versus physician-acquired medication history: A prospective study at the emergency department. Qual Saf Health Care. 2010; 19(5):371-375.
20. American Society of Health-System Pharmacists. ASHP statement on pharmacy services to the emergency department. Am J Health Syst Pharm. 2008;65(24):2380-2383.
21. Ernst AA, Weiss SJ, Sullivan A IV, et al. On-site pharmacists in the ED improve medical errors. Am J Emerg Med. 2011;30(5):717-725.
22. Weant KA, Humphries RL, Hite K, Armitstead JA. Effect of emergency medicine pharmacists on medication-error reporting in an emergency department. Am J Health Syst Pharm. 2010;67(21):1851-1855.
23. Brown JN, Barnes CL, Beasley B, et al. Effect of pharmacists on medication errors in an emergency department. Am J Health Syst Pharm. 2008;65(4):330-333.
24. Holland R, Desborough J, Goodyer L, Hall S, Wright D, Loke YK. Does pharmacist-led medication review help to reduce hospital admissions and deaths in older people? A systematic review and meta-analysis. Br J Clin Pharmacol. 2008;65(3):303-316.
25. Marconi GP, Claudius I. Impact of an emergency department pharmacy on medication omission and delay. Pediatr Emerg Care. 2012;28(1):30-33.
26. Jellinek SP, Cohen V, Fancher LB, et al. Pharmacist improves timely administration of medications to boarded patients in the emergency department. J Emerg Nurs. 2010;36(2):105-110.
27. Pantanwala AE, Sanders AB, Thomas MC, et al. A prospective, multicenter study of pharmacist activities resulting in medication error interception in the emergency department. Ann Emerg Med. 2012;59(5)369-373.
28. Fairbanks RJ, Hildebrand JM, Kolstee KE, Schneider SM, Shah MN. Medical and nursing staff highly value clinical pharmacists in the emergency department. Emerg Med J. 2007;24(10):716-718.
29. Randolph TC, Parker A, Meyer L, Zeina R. Effect of pharmacist-managed culture review process on antimicrobial therapy in an emergency department. Am J Health Syst Pharm. 2011; 68(10):916-919.
30. Lee AJ, Boro MS, Knapp KK, Meier JL, Kirman NE. Clinical and economic outcomes of pharmacist recommendations in a veterans affairs medical center. Am J Health Syst Pharm. 2002;59(21):2070-2077.
31. Ling JM, Mike LA, Rubin J, et al. Documentation of pharmacist interventions in the emergency department. Am J Health Syst Pharm. 2005;62(17):1793-1797.
32. U.S. Bureau of Labor Statistics. Database, tools and calculators by subject. CPI inflation calculator. U.S. Bureau of Labor Statistics Website. http://www.bls.gov/data/inflation_calculator.htm. Accessed August 05, 2014.
33. Levy DB. Documentation of clinical and cost-saving pharmacy interventions in the emergency room. Hosp Pharm. 1993;28(7):624-627, 630-634, 653.
34. Uselton JP, Kienle P, Murdaugh LB, eds. Assuring Continuous Compliance With Joint Commission Standards: A Pharmacy Guide. 8th ed. Bethesda, MD: American Society of Health-System Pharmacists; 2010.
35. Pantanwala AE, Hays DP, Sanders AB, Erstad BL. Severity and probability of harm of medication errors intercepted by an emergency pharmacist. Int J Pharm Pract. 2011;19(5):358-362.
36. Raja AS, Lindsell CJ, Bernstein JA, Codispoti CD Moellman JJ. The use of penicillin skin testing to assess the prevalence of penicillin allergy in an emergency department setting. Ann Emerg Med. 2009;54(1):72-77.
Clinical pharmacists have expanded their role over the past few decades in both outpatient and inpatient settings and are now members of an interdisciplinary health care team that includes nutritionists, physical therapists, physicians, and nurses.1,2 The emergency department (ED), however, has lagged behind in the inclusion of pharmacists.3 Despite well documented financial and ED operational benefits of pharmacists and the recommendation of their inclusion by the Institute of Medicine, only about 30% of academic EDs in a 2009 survey employed a pharmacist.4-8 A larger 2005 survey of 510 hospital pharmacy directors revealed that only 3.5% of hospitals sampled (academic and nonacademic) provided clinical pharmacy services in the ED.9
About 3.8 million annual preventable medical errors occur in the ED, giving the ED the highest rate of medication errors among all hospital departments.4 In 2000, Schenkel found that 3% of all inpatient medication errors were initiated in the ED.10 Similarly, Chin and colleagues found that 3.6% of elderly patients were administered an inappropriate medication in the ED with 5.6% receiving an inappropriate prescription at discharge.11
In a 2008 study conducted at the Durham VAMC in North Carolina, Hastings and colleagues found that suboptimal pharmacy was common among elderly veterans discharged from the ED (11%) and that potentially inappropriate medication use was associated with a 32% greater risk of repeat ED visits, hospitalization, or death (P = .10).12 In 2010, Rothschild and colleagues found 7.8 medication errors per 100 ED patients or 2.9 errors per 100 prescribed medications.13 Despite this unacceptably high rate of medication errors, most EDs do not employ pharmacy specialists or have a pharmacist easily available for consultation—options that could not only streamline ED operations, but also reduce patient risk.
The pharmacist role in the ED has changed considerably. In the 1970s, ED pharmacists were used mainly to dispense medicine, maintain inventories, and participate in cardiopulmonary resuscitation.3,14,15 Today, following the guidelines set by the American Society for Health-System Pharmacists, emergency pharmacists have an expanded, more direct role in patient care and evaluation and support of the physicians and other ED staff who work alongside them.4,14,16,17 Pharmacists gather accurate and complete medication histories, review and reconcile medication lists, and screen ED medication orders for errors or anticipated drug interactions.13,18-23 They adjust medication doses on a patient-by-patient basis, accounting for renal and hepatic clearance and closely monitor patients for treatment response. They also provide one-on-one patient education on medication dosing, administration, adverse drug events (ADEs), and interactions, increasing patients’ drug knowledge and adherence.17,24 Pharmacists provide information to patients on vaccinations and medication assistance programs, which is unlikely to be shared by other providers.3,19,20 Pharmacists in the ED reduce medication delays and omissions that occur in admitted patients staying in the ED.25,26
Aside from patient education, clinical pharmacists have an important role in providing education and consultation to ED physicians, midlevel providers, and house staff on topics that include availability of new medications and local antibiotic resistance patterns.14,27-29 Additionally, pharmacists monitor drug supplies and restock medications to avoid shortages during critical moments, offer the ED perspective in hospital formulary reviews, and increase efficiency and throughput in the ED while decreasing costs by evaluating and treating patients who present simply for prescription refills alongside a supervising physician.14
With this in mind, the ED of the Atlanta VAMC in Decatur, Georgia, conducted a pilot study to assess the financial and logistic feasibility of a full-time pharmacist in the ED setting with the hope that a pharmacist would integrate well into the health care team, reducing overall departmental expense and the risk of medication error associated with patient harm and simultaneously improving patient satisfaction and departmental efficiency.
Methodology
The ED of the Atlanta VAMC is part of a tertiary care teaching hospital affiliated with both the Emory and Morehouse schools of medicine. At the time of the pilot, the facility had 128 acute care medical/surgical beds, 12 inpatient palliative care beds, 40 acute care psychiatric beds, 24 medical surgical intensive care unit beds, and 60 inpatient nursing home beds. The ED provides care to > 37,000 veterans annually, and in December 2011 when this study was conducted, 3,195 veterans were seen in the ED.
The ED was divided into the main ED and the urgent care. Patient intake occurred through a centralized triage, and based on acuity, patients were sent to the appropriate setting for treatment. The ED used a 5-tier triage system. Patients with triage levels 1, 2, and 3 were sent to the main ED, and patients with triage levels 4 and 5 were sent to the urgent care.
Pharmacists
Pharmacy services were provided by 5 residency-trained doctors of pharmacy employed by the medical center working as clinical pharmacists with the inpatient medical teams at the time of the pilot. The pilot was conducted over a 2-week period in December 2011, Monday through Friday, for a total of 10 days. The clinical pharmacists divided the days among themselves. Each pharmacist provided services for a total of 2 days, 3 hours per day, from about 3 pm to 6 pm. The pharmacists were given a room previously used as a physician workroom in which to evaluate patients.
Patient Selection
Patients to be seen by the clinical pharmacist were chosen by the triage nurse, the charge nurse, the ED physician, the urgent care provider (physician or midlevel provider), or by the pharmacists. The triage nurse or charge nurse, based on chief medical problem and acuity, chose patients directly out of triage. Only patients with triage acuity level 4 or 5 were taken directly from triage without first seeing a physician or midlevel provider. These patients presented with the chief problem of medication refill or coumadin/International Normalized Ratio check. Once chosen as appropriate for the clinical pharmacist, the charge nurse helped with patient flow, and if the pharmacist was occupied with other patients, the nurse redirected the patient to urgent care.
Additional patients were chosen to see the clinical pharmacist after an evaluation of their initial problem was completed by a physician or midlevel practitioner in the urgent care or main ED. Patients whom the provider felt could benefit from any of the following services were directed to the clinical pharmacist: anticoagulation consult, diabetic education, pharmacokinetic consult, medication history, medication reconciliation, formulary management, medication refills, therapeutic interchange, screening for drug interactions, allergy review, and nonformulary or restricted medications requests. Additionally, the clinical pharmacist reviewed the charts of patients in the main ED whom they were not asked to see. They offered assistance when needed in all the aforementioned areas and for order clarification, assuring IV compatibility, reporting medication errors and ADEs, promotion of safe medical practices, and elimination of duplicate/redundant medications.
Data Collection
The pharmacists developed a log to record their activities. The log included the date and time of the intervention, number of minutes spent with the patient, the reason for intervention, and recommendations, if applicable. They categorized their interventions into 16 categories: anticoagulation, pharmacokinetics, drug information, order clarification, medication reconciliation, therapeutic interchange, formulary management, medication history, IV compatibility, screening for drug interactions, patient education, allergy documentation, promotion of safe medical practices, reporting of medication error/ADEs, nonformulary and restricted medication requests, and prescription refills. Patients could receive more than 1 intervention.
Though not a focus of this pilot, all patients seen by a pharmacist received a postencounter survey seeking their opinion on whether the pharmacist improved the value of their visit.
Review Process
At the conclusion of the pilot, 2 independent reviewers, both physicians, reviewed the logs, and each task was reassigned to 1 of 8 categories. These categories included either medication refills or 1 of 7 other areas that had established cost avoidance estimates from 2 other well accepted studies (Lee and colleagues and Ling and colleagues).30,31 These 7 categories included adjusting dose or frequency of medication, elimination of duplication of therapy, education/information inquiry, formulary management, prevention and management of ADEs, prevention or management of allergies, and therapeutic interchange. If the independent reviewers did not have initial concordance of classification of the intervention, they discussed the intervention and came to an agreement.
Cost Analysis
Cost avoidance estimates for 7 individual interventions were made, using data from Lee and colleagues and Ling and colleagues.30,31 Four of these came from the study by Lee and colleagues: prevent or manage drug allergy, adjust dosage or frequency, prevent or manage ADEs, and eliminate duplication of therapy.30 Lee and colleagues’ “drug interaction” group was not clearly defined, thus this was included with the “prevent or manage ADE” group. Ling and colleagues provided data for the 3 additional groups of interventions that pharmacists performed: education and information inquiry, formulary management, and therapeutic interchange.31
Financial estimates of cost avoidance were adjusted for inflation, using the consumer price index (CPI) of the U.S. Bureau of Labor Statistics.32 The Lee study was conducted in 2002, and estimates for cost avoidance using their model were adjusted to 2011 values using the CPI inflation rate of 25%. The Ling study was conducted in 2005, and estimates for cost avoidance using their model were adjusted for 2011 values using the CPI rate of inflation of 15.2%.32
For the remaining intervention, prescription refill, cost savings was determined by calculating the average times spent by the ED pharmacist on each intervention and then using the difference between hourly physician and pharmacist pay (about $50/h difference based on VA wage tables).
RESULTS
During the 30-hour total time in which a pharmacist was present in the ED, a total of 42 patients were assisted through 71 interventions (Table 1).
Pharmacists provided a diverse range of services to patients in the ED. The most common intervention was education and/or information inquiry. Tasks in this category included patient education about medication dosing, administration, AEs, interactions and warnings, as well as diabetes management. In several instances, education was provided to attending physicians or house staff, though it should be noted that this provider education was not counted as an intervention for this study unless it was associated with a patient (of which there were 3 total instances, eg, instruction on how to choose the proper insulin syringe).
Interventions, when a medication list was screened by the ED pharmacist for interactions or when drug choices were recommended to the physician or midlevel providers, were counted as prevention and management of ADEs. For example, the pharmacist noted a patient with a new diagnosis of gout who was prescribed hydrochlorothiazide; this was brought to the attention of the provider and alternative antihypertensives were suggested. In another instance, a patient was found to be on both ibuprofen and enoxaparin; the treating physician was alerted of this potential interaction. There were 15 such events in total.
Several other interventions arose from the screenings for ADEs, including adjusting dose or frequency of medication (11); therapeutic interchange (5); eliminating duplication of therapy (2); and prevention or management of allergies (1). Cases included hepatic and/or renal dose changes, substituting equivalent medications for better treatment outcome or adherence, or discontinuing 2 or more medications in a patient’s medication profile that were considered duplication.
During the pharmacist screening, one patient who had piperacillin/tazobactam ordered in the ED had a penicillin allergy. This intervention was categorized as prevention and management of an ADE as well as prevention and management of allergies. Interventions not accompanied by the “prevention of ADE” category included those in which the change did not provide a clear risk reduction. For example, one therapeutic interchange was from levofloxacin to moxifloxacin for a better-anticipated therapy. Another was a metformin dose increase, presumably for improved glycemic control.
Prescription refills occurred with the same frequency as prevention of ADEs.15 This intervention led in some cases to switching to pharmaceutical equivalents when a drug prescribed at another facility was not on the formulary. Other drugs that were not on the preferred list but available with nonformulary medication requests were ordered or approved with the assistance of the pharmacist. The pharmacist’s direct involvement significantly reduced the initial contact-to-approval time for these patients.
After tallying the total number of interventions, the potential financial cost savings to the ED were determined (Table 2). As mentioned previously, the Lee and Ling studies provided the categories for classification of 7 pharmacist interactions. The estimated cost avoidance for the 4 applicable groups from the Lee study had inflation-corrected values of $1,486 per adjusted dose or frequency of medication, $205 per elimination of duplication of therapy, $1,374 per prevention or management of ADEs, and $1,721 per prevention or management of allergies.30
The estimated cost avoidance for the 3 applicable groups from the Ling study had inflation-corrected values of $512.38 per education/information inquiry, $174.80 per formulary management, and $174.80 per therapeutic interchange.31 The eighth group, prescription refills, was valued at $12.50 each, using the difference between physician and pharmacist salary for an average of 15 minutes per interaction.
When multiplied by the number of interventions in each of these groups, the total potential cost avoidance in the study period was about $40,136.48. Extrapolated into a yearly amount, that is a $2,782,795.94 potential cost savings for the medical center.
Seventeen of the 42 (40.5%) postencounter surveys from the patients seen by the pharmacists were received. Of these veterans, 100% reported that they were “extremely satisfied” with the treatment they had received during their visit to the ED.
DISCUSSION
There is the potential for significant cost avoidance by adding a single full-time pharmacist to the ED: Annually, more than $2.7 million in potential savings for the medical center. Though surprising, this figure is actually in line with the much larger study by Lada and colleagues in which an estimated $3 million was avoided.15 At the same hospital 12 years earlier, Levy noted about $1 million in cost avoidance (not inflation-adjusted).33 The Ling study, however, did not have as high a figure, with annual cost avoidance estimated at $600,000.31 All these figures are based on estimates and, therefore, imprecise, but it is clear even using the most conservative model that the cost to employ a clinical pharmacist is justified.
The final value of cost savings is likely significantly underestimated relative to non-VA hospitals due to the decision to correct for inflation, using the total market inflation rate rather than the medical sector inflation rate over the same time period. The Lee study values were increased by 25.0% and the Ling study values by 15.2%, to bring them to 2011 amounts. Using the medical inflation rate instead (42.3% and 25.2%, respectively), an additional $378,000 in annual savings would have been realized. The lower CPI inflation rate rather than the higher rate in the medical sector was chosen to make the cost avoidance outcomes more conservative.
The true value of a clinical pharmacist comes from the services they provide to patients. In this pilot, as well as in several others, it has been shown that education is a commonly performed and highly valued task. Education was a service lacking in this ED prior to this intervention due to financial and logistical constraints. It is unclear how much instruction patients receive at the outpatient pharmacy while picking up medications after leaving the ED, but it is likely limited, given the large volumes and long lines often found at the in-house pharmacy. Education has a demonstrated effect on prevention and management of ADEs and was the most interactive of the interventions the pharmacist provided during this study. This type of intervention was most likely the source of increased patient satisfaction that was noted in the postencounter surveys.17,24
Prevention of ADEs, which was a frequent intervention in this pilot, has been noted by many sources to be the single most beneficial task performed by a clinical pharmacist both from financial and risk reduction standpoints.13,21-23 Although not able to assess patient outcomes after this limited pilot, the authors anticipate such an evaluation when a full-time ED pharmacist joins the department.
The Joint Commission recommends that a pharmacist review all medication orders before administration, though there is an exception for the emergency setting.34 The Joint Commission also recommends medication reconciliation at every visit, including those in the ED setting. The addition of a clinical pharmacist would increase compliance with this and other standards and bring ED operations up to the same benchmark as other practice settings.
LIMITATIONS
The most significant limitation of this study was sample size. The volunteered time of the pharmacists in the ED totaled only 30 hours over 2 weeks. In that limited time, however, the pharmacists had more patient interactions than were anticipated. Had the pilot been conducted over a longer period, it is unclear whether this would have been sustained or whether this was a coincidental overestimate of the effect that a full-time pharmacist would have on the department. Likely, it is an underestimate of their potential, as the availability of the pharmacist was novel and likely underused by other providers. Given more time with the ED staff, pharmacists would be more frequently called on for their expertise, because their skills and knowledge set would be better understood. During this pilot, the pharmacist was located in a separate room in the ED where not all ED staff knew they were available for consultation.
The other major limitation of the pilot was the inherent imprecision of cost avoidance estimates. The dollar amounts attributed to the duties fulfilled by the pharmacists relied on 2 studies. The first, by Lee and colleagues, provided cost avoidance estimates of certain pharmacist actions based on a combination of 4 to 5 clinicians’ estimates of risk reduction, combined with their individual location’s costs for hospitalization, laboratory tests, diagnostic procedures, medications, telephone care, clinic visits, and emergency department visits.30 The numbers are based not only on a small number of individual estimations of risk, but also on facility costs that are highly variable. Despite this, the authors believe the estimates are actually on the conservative side, since they do not account for costs of lost productivity and/or litigation.
The current pilot was performed in a different type of setting than the one by Lee. That study was conducted in a similar VAMC setting, but their study data were obtained from other areas of the medical center. Of 600 pharmacist interventions, 250 were in an outpatient clinic, 250 were in an inpatient setting, and 100 were in a nursing home.30 Despite this, the estimates are likely still relevant to this study, given that drugs used in the ED are often a mix of inpatient and outpatient ones, with the same risks to an individual regardless of where they are initiated, changed, or discontinued.
The study by Ling and colleagues was performed in an ED setting more closely matching this study’s setting and was a larger, well powered study. As with the Lee study, it was difficult if not impossible to obtain exact numbers on the expenses each pharmacist recommendation spared the hospital and/or patients.31 Not all drug interactions avoided would have led to symptoms, reevaluation, or hospitalization.35 Not all drug “allergies” avoided are true allergies (as seen dramatically by Raja and colleagues), and thus this action may not have spared any cost at all.36 In the end, however, the estimates provided by both studies are averaged over many patients and thus provided the best numbers available.
Unlike the Lee study, this pilot did not evaluate the medication cost differences between original treatment and the new recommended treatment. Given the small number of patients with whom significant changes were made in this study, evaluating the cost differences between the treatments would likely be insignificant. A larger study, such as Lee, was much more sufficiently powered to evaluate such a figure.30
Of note, in this pilot there were no cases seen in which there was any change in route of delivery, ie, IV to equivalent po treatments. This is typically a large source of cost savings secondary to reduction in equipment and nursing time. The Lada study found 66 such changes among 2,150 pharmacist interventions in the ED.15 The authors hypothesize that had their pilot been conducted over a longer period, significant cost savings would have resulted from similar interventions.
In this pilot, a significant number of patients presented for prescription refills. Veterans often prefer to fill medications at the VA pharmacy because of reduced cost and often bring prescriptions written by private sector physicians. These veterans are required to have a primary care physician assigned within the VA, but until they have their initial intake appointment, they use the ED for these prescriptions. Additionally, veterans from other VA locations presenting as visitors to the area or relocating to the city and not yet assigned to a primary care physician require their medication lists from other location(s) be accessed and reentered into intrafacility computerized ordering systems. Given these particulars of VA operation, the authors’ facility assuredly sees more patients presenting for prescription refill than nongovernment facilities. Thus our savings with this particular task may not be generalizable to settings outside the VA, at least in as high a number of encounters.
CONCLUSIONS
About 37,000 veterans received care at the ED of the Atlanta VAMC in 2011. Given these numbers and the evidence that EDs have some of the highest rates of preventable ADEs of any clinical environment, the presence of a clinical pharmacist in the ED is a necessary intervention, based on safety considerations alone. In addition to providing a needed layer of safety in the vulnerable ED environment, a clinical pharmacist likely provides a cost saving benefit to the ED, as demonstrated by this pilot and other studies. Further, the overwhelmingly positive response to this pilot by the veterans who participated shows that they want and need this service. Adding a clinical pharmacist to the ED is integral to the VA mission of providing patient-centered care. A larger study to obtain a more precise cost savings benefit within the VA system should be considered.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Clinical pharmacists have expanded their role over the past few decades in both outpatient and inpatient settings and are now members of an interdisciplinary health care team that includes nutritionists, physical therapists, physicians, and nurses.1,2 The emergency department (ED), however, has lagged behind in the inclusion of pharmacists.3 Despite well documented financial and ED operational benefits of pharmacists and the recommendation of their inclusion by the Institute of Medicine, only about 30% of academic EDs in a 2009 survey employed a pharmacist.4-8 A larger 2005 survey of 510 hospital pharmacy directors revealed that only 3.5% of hospitals sampled (academic and nonacademic) provided clinical pharmacy services in the ED.9
About 3.8 million annual preventable medical errors occur in the ED, giving the ED the highest rate of medication errors among all hospital departments.4 In 2000, Schenkel found that 3% of all inpatient medication errors were initiated in the ED.10 Similarly, Chin and colleagues found that 3.6% of elderly patients were administered an inappropriate medication in the ED with 5.6% receiving an inappropriate prescription at discharge.11
In a 2008 study conducted at the Durham VAMC in North Carolina, Hastings and colleagues found that suboptimal pharmacy was common among elderly veterans discharged from the ED (11%) and that potentially inappropriate medication use was associated with a 32% greater risk of repeat ED visits, hospitalization, or death (P = .10).12 In 2010, Rothschild and colleagues found 7.8 medication errors per 100 ED patients or 2.9 errors per 100 prescribed medications.13 Despite this unacceptably high rate of medication errors, most EDs do not employ pharmacy specialists or have a pharmacist easily available for consultation—options that could not only streamline ED operations, but also reduce patient risk.
The pharmacist role in the ED has changed considerably. In the 1970s, ED pharmacists were used mainly to dispense medicine, maintain inventories, and participate in cardiopulmonary resuscitation.3,14,15 Today, following the guidelines set by the American Society for Health-System Pharmacists, emergency pharmacists have an expanded, more direct role in patient care and evaluation and support of the physicians and other ED staff who work alongside them.4,14,16,17 Pharmacists gather accurate and complete medication histories, review and reconcile medication lists, and screen ED medication orders for errors or anticipated drug interactions.13,18-23 They adjust medication doses on a patient-by-patient basis, accounting for renal and hepatic clearance and closely monitor patients for treatment response. They also provide one-on-one patient education on medication dosing, administration, adverse drug events (ADEs), and interactions, increasing patients’ drug knowledge and adherence.17,24 Pharmacists provide information to patients on vaccinations and medication assistance programs, which is unlikely to be shared by other providers.3,19,20 Pharmacists in the ED reduce medication delays and omissions that occur in admitted patients staying in the ED.25,26
Aside from patient education, clinical pharmacists have an important role in providing education and consultation to ED physicians, midlevel providers, and house staff on topics that include availability of new medications and local antibiotic resistance patterns.14,27-29 Additionally, pharmacists monitor drug supplies and restock medications to avoid shortages during critical moments, offer the ED perspective in hospital formulary reviews, and increase efficiency and throughput in the ED while decreasing costs by evaluating and treating patients who present simply for prescription refills alongside a supervising physician.14
With this in mind, the ED of the Atlanta VAMC in Decatur, Georgia, conducted a pilot study to assess the financial and logistic feasibility of a full-time pharmacist in the ED setting with the hope that a pharmacist would integrate well into the health care team, reducing overall departmental expense and the risk of medication error associated with patient harm and simultaneously improving patient satisfaction and departmental efficiency.
Methodology
The ED of the Atlanta VAMC is part of a tertiary care teaching hospital affiliated with both the Emory and Morehouse schools of medicine. At the time of the pilot, the facility had 128 acute care medical/surgical beds, 12 inpatient palliative care beds, 40 acute care psychiatric beds, 24 medical surgical intensive care unit beds, and 60 inpatient nursing home beds. The ED provides care to > 37,000 veterans annually, and in December 2011 when this study was conducted, 3,195 veterans were seen in the ED.
The ED was divided into the main ED and the urgent care. Patient intake occurred through a centralized triage, and based on acuity, patients were sent to the appropriate setting for treatment. The ED used a 5-tier triage system. Patients with triage levels 1, 2, and 3 were sent to the main ED, and patients with triage levels 4 and 5 were sent to the urgent care.
Pharmacists
Pharmacy services were provided by 5 residency-trained doctors of pharmacy employed by the medical center working as clinical pharmacists with the inpatient medical teams at the time of the pilot. The pilot was conducted over a 2-week period in December 2011, Monday through Friday, for a total of 10 days. The clinical pharmacists divided the days among themselves. Each pharmacist provided services for a total of 2 days, 3 hours per day, from about 3 pm to 6 pm. The pharmacists were given a room previously used as a physician workroom in which to evaluate patients.
Patient Selection
Patients to be seen by the clinical pharmacist were chosen by the triage nurse, the charge nurse, the ED physician, the urgent care provider (physician or midlevel provider), or by the pharmacists. The triage nurse or charge nurse, based on chief medical problem and acuity, chose patients directly out of triage. Only patients with triage acuity level 4 or 5 were taken directly from triage without first seeing a physician or midlevel provider. These patients presented with the chief problem of medication refill or coumadin/International Normalized Ratio check. Once chosen as appropriate for the clinical pharmacist, the charge nurse helped with patient flow, and if the pharmacist was occupied with other patients, the nurse redirected the patient to urgent care.
Additional patients were chosen to see the clinical pharmacist after an evaluation of their initial problem was completed by a physician or midlevel practitioner in the urgent care or main ED. Patients whom the provider felt could benefit from any of the following services were directed to the clinical pharmacist: anticoagulation consult, diabetic education, pharmacokinetic consult, medication history, medication reconciliation, formulary management, medication refills, therapeutic interchange, screening for drug interactions, allergy review, and nonformulary or restricted medications requests. Additionally, the clinical pharmacist reviewed the charts of patients in the main ED whom they were not asked to see. They offered assistance when needed in all the aforementioned areas and for order clarification, assuring IV compatibility, reporting medication errors and ADEs, promotion of safe medical practices, and elimination of duplicate/redundant medications.
Data Collection
The pharmacists developed a log to record their activities. The log included the date and time of the intervention, number of minutes spent with the patient, the reason for intervention, and recommendations, if applicable. They categorized their interventions into 16 categories: anticoagulation, pharmacokinetics, drug information, order clarification, medication reconciliation, therapeutic interchange, formulary management, medication history, IV compatibility, screening for drug interactions, patient education, allergy documentation, promotion of safe medical practices, reporting of medication error/ADEs, nonformulary and restricted medication requests, and prescription refills. Patients could receive more than 1 intervention.
Though not a focus of this pilot, all patients seen by a pharmacist received a postencounter survey seeking their opinion on whether the pharmacist improved the value of their visit.
Review Process
At the conclusion of the pilot, 2 independent reviewers, both physicians, reviewed the logs, and each task was reassigned to 1 of 8 categories. These categories included either medication refills or 1 of 7 other areas that had established cost avoidance estimates from 2 other well accepted studies (Lee and colleagues and Ling and colleagues).30,31 These 7 categories included adjusting dose or frequency of medication, elimination of duplication of therapy, education/information inquiry, formulary management, prevention and management of ADEs, prevention or management of allergies, and therapeutic interchange. If the independent reviewers did not have initial concordance of classification of the intervention, they discussed the intervention and came to an agreement.
Cost Analysis
Cost avoidance estimates for 7 individual interventions were made, using data from Lee and colleagues and Ling and colleagues.30,31 Four of these came from the study by Lee and colleagues: prevent or manage drug allergy, adjust dosage or frequency, prevent or manage ADEs, and eliminate duplication of therapy.30 Lee and colleagues’ “drug interaction” group was not clearly defined, thus this was included with the “prevent or manage ADE” group. Ling and colleagues provided data for the 3 additional groups of interventions that pharmacists performed: education and information inquiry, formulary management, and therapeutic interchange.31
Financial estimates of cost avoidance were adjusted for inflation, using the consumer price index (CPI) of the U.S. Bureau of Labor Statistics.32 The Lee study was conducted in 2002, and estimates for cost avoidance using their model were adjusted to 2011 values using the CPI inflation rate of 25%. The Ling study was conducted in 2005, and estimates for cost avoidance using their model were adjusted for 2011 values using the CPI rate of inflation of 15.2%.32
For the remaining intervention, prescription refill, cost savings was determined by calculating the average times spent by the ED pharmacist on each intervention and then using the difference between hourly physician and pharmacist pay (about $50/h difference based on VA wage tables).
RESULTS
During the 30-hour total time in which a pharmacist was present in the ED, a total of 42 patients were assisted through 71 interventions (Table 1).
Pharmacists provided a diverse range of services to patients in the ED. The most common intervention was education and/or information inquiry. Tasks in this category included patient education about medication dosing, administration, AEs, interactions and warnings, as well as diabetes management. In several instances, education was provided to attending physicians or house staff, though it should be noted that this provider education was not counted as an intervention for this study unless it was associated with a patient (of which there were 3 total instances, eg, instruction on how to choose the proper insulin syringe).
Interventions, when a medication list was screened by the ED pharmacist for interactions or when drug choices were recommended to the physician or midlevel providers, were counted as prevention and management of ADEs. For example, the pharmacist noted a patient with a new diagnosis of gout who was prescribed hydrochlorothiazide; this was brought to the attention of the provider and alternative antihypertensives were suggested. In another instance, a patient was found to be on both ibuprofen and enoxaparin; the treating physician was alerted of this potential interaction. There were 15 such events in total.
Several other interventions arose from the screenings for ADEs, including adjusting dose or frequency of medication (11); therapeutic interchange (5); eliminating duplication of therapy (2); and prevention or management of allergies (1). Cases included hepatic and/or renal dose changes, substituting equivalent medications for better treatment outcome or adherence, or discontinuing 2 or more medications in a patient’s medication profile that were considered duplication.
During the pharmacist screening, one patient who had piperacillin/tazobactam ordered in the ED had a penicillin allergy. This intervention was categorized as prevention and management of an ADE as well as prevention and management of allergies. Interventions not accompanied by the “prevention of ADE” category included those in which the change did not provide a clear risk reduction. For example, one therapeutic interchange was from levofloxacin to moxifloxacin for a better-anticipated therapy. Another was a metformin dose increase, presumably for improved glycemic control.
Prescription refills occurred with the same frequency as prevention of ADEs.15 This intervention led in some cases to switching to pharmaceutical equivalents when a drug prescribed at another facility was not on the formulary. Other drugs that were not on the preferred list but available with nonformulary medication requests were ordered or approved with the assistance of the pharmacist. The pharmacist’s direct involvement significantly reduced the initial contact-to-approval time for these patients.
After tallying the total number of interventions, the potential financial cost savings to the ED were determined (Table 2). As mentioned previously, the Lee and Ling studies provided the categories for classification of 7 pharmacist interactions. The estimated cost avoidance for the 4 applicable groups from the Lee study had inflation-corrected values of $1,486 per adjusted dose or frequency of medication, $205 per elimination of duplication of therapy, $1,374 per prevention or management of ADEs, and $1,721 per prevention or management of allergies.30
The estimated cost avoidance for the 3 applicable groups from the Ling study had inflation-corrected values of $512.38 per education/information inquiry, $174.80 per formulary management, and $174.80 per therapeutic interchange.31 The eighth group, prescription refills, was valued at $12.50 each, using the difference between physician and pharmacist salary for an average of 15 minutes per interaction.
When multiplied by the number of interventions in each of these groups, the total potential cost avoidance in the study period was about $40,136.48. Extrapolated into a yearly amount, that is a $2,782,795.94 potential cost savings for the medical center.
Seventeen of the 42 (40.5%) postencounter surveys from the patients seen by the pharmacists were received. Of these veterans, 100% reported that they were “extremely satisfied” with the treatment they had received during their visit to the ED.
DISCUSSION
There is the potential for significant cost avoidance by adding a single full-time pharmacist to the ED: Annually, more than $2.7 million in potential savings for the medical center. Though surprising, this figure is actually in line with the much larger study by Lada and colleagues in which an estimated $3 million was avoided.15 At the same hospital 12 years earlier, Levy noted about $1 million in cost avoidance (not inflation-adjusted).33 The Ling study, however, did not have as high a figure, with annual cost avoidance estimated at $600,000.31 All these figures are based on estimates and, therefore, imprecise, but it is clear even using the most conservative model that the cost to employ a clinical pharmacist is justified.
The final value of cost savings is likely significantly underestimated relative to non-VA hospitals due to the decision to correct for inflation, using the total market inflation rate rather than the medical sector inflation rate over the same time period. The Lee study values were increased by 25.0% and the Ling study values by 15.2%, to bring them to 2011 amounts. Using the medical inflation rate instead (42.3% and 25.2%, respectively), an additional $378,000 in annual savings would have been realized. The lower CPI inflation rate rather than the higher rate in the medical sector was chosen to make the cost avoidance outcomes more conservative.
The true value of a clinical pharmacist comes from the services they provide to patients. In this pilot, as well as in several others, it has been shown that education is a commonly performed and highly valued task. Education was a service lacking in this ED prior to this intervention due to financial and logistical constraints. It is unclear how much instruction patients receive at the outpatient pharmacy while picking up medications after leaving the ED, but it is likely limited, given the large volumes and long lines often found at the in-house pharmacy. Education has a demonstrated effect on prevention and management of ADEs and was the most interactive of the interventions the pharmacist provided during this study. This type of intervention was most likely the source of increased patient satisfaction that was noted in the postencounter surveys.17,24
Prevention of ADEs, which was a frequent intervention in this pilot, has been noted by many sources to be the single most beneficial task performed by a clinical pharmacist both from financial and risk reduction standpoints.13,21-23 Although not able to assess patient outcomes after this limited pilot, the authors anticipate such an evaluation when a full-time ED pharmacist joins the department.
The Joint Commission recommends that a pharmacist review all medication orders before administration, though there is an exception for the emergency setting.34 The Joint Commission also recommends medication reconciliation at every visit, including those in the ED setting. The addition of a clinical pharmacist would increase compliance with this and other standards and bring ED operations up to the same benchmark as other practice settings.
LIMITATIONS
The most significant limitation of this study was sample size. The volunteered time of the pharmacists in the ED totaled only 30 hours over 2 weeks. In that limited time, however, the pharmacists had more patient interactions than were anticipated. Had the pilot been conducted over a longer period, it is unclear whether this would have been sustained or whether this was a coincidental overestimate of the effect that a full-time pharmacist would have on the department. Likely, it is an underestimate of their potential, as the availability of the pharmacist was novel and likely underused by other providers. Given more time with the ED staff, pharmacists would be more frequently called on for their expertise, because their skills and knowledge set would be better understood. During this pilot, the pharmacist was located in a separate room in the ED where not all ED staff knew they were available for consultation.
The other major limitation of the pilot was the inherent imprecision of cost avoidance estimates. The dollar amounts attributed to the duties fulfilled by the pharmacists relied on 2 studies. The first, by Lee and colleagues, provided cost avoidance estimates of certain pharmacist actions based on a combination of 4 to 5 clinicians’ estimates of risk reduction, combined with their individual location’s costs for hospitalization, laboratory tests, diagnostic procedures, medications, telephone care, clinic visits, and emergency department visits.30 The numbers are based not only on a small number of individual estimations of risk, but also on facility costs that are highly variable. Despite this, the authors believe the estimates are actually on the conservative side, since they do not account for costs of lost productivity and/or litigation.
The current pilot was performed in a different type of setting than the one by Lee. That study was conducted in a similar VAMC setting, but their study data were obtained from other areas of the medical center. Of 600 pharmacist interventions, 250 were in an outpatient clinic, 250 were in an inpatient setting, and 100 were in a nursing home.30 Despite this, the estimates are likely still relevant to this study, given that drugs used in the ED are often a mix of inpatient and outpatient ones, with the same risks to an individual regardless of where they are initiated, changed, or discontinued.
The study by Ling and colleagues was performed in an ED setting more closely matching this study’s setting and was a larger, well powered study. As with the Lee study, it was difficult if not impossible to obtain exact numbers on the expenses each pharmacist recommendation spared the hospital and/or patients.31 Not all drug interactions avoided would have led to symptoms, reevaluation, or hospitalization.35 Not all drug “allergies” avoided are true allergies (as seen dramatically by Raja and colleagues), and thus this action may not have spared any cost at all.36 In the end, however, the estimates provided by both studies are averaged over many patients and thus provided the best numbers available.
Unlike the Lee study, this pilot did not evaluate the medication cost differences between original treatment and the new recommended treatment. Given the small number of patients with whom significant changes were made in this study, evaluating the cost differences between the treatments would likely be insignificant. A larger study, such as Lee, was much more sufficiently powered to evaluate such a figure.30
Of note, in this pilot there were no cases seen in which there was any change in route of delivery, ie, IV to equivalent po treatments. This is typically a large source of cost savings secondary to reduction in equipment and nursing time. The Lada study found 66 such changes among 2,150 pharmacist interventions in the ED.15 The authors hypothesize that had their pilot been conducted over a longer period, significant cost savings would have resulted from similar interventions.
In this pilot, a significant number of patients presented for prescription refills. Veterans often prefer to fill medications at the VA pharmacy because of reduced cost and often bring prescriptions written by private sector physicians. These veterans are required to have a primary care physician assigned within the VA, but until they have their initial intake appointment, they use the ED for these prescriptions. Additionally, veterans from other VA locations presenting as visitors to the area or relocating to the city and not yet assigned to a primary care physician require their medication lists from other location(s) be accessed and reentered into intrafacility computerized ordering systems. Given these particulars of VA operation, the authors’ facility assuredly sees more patients presenting for prescription refill than nongovernment facilities. Thus our savings with this particular task may not be generalizable to settings outside the VA, at least in as high a number of encounters.
CONCLUSIONS
About 37,000 veterans received care at the ED of the Atlanta VAMC in 2011. Given these numbers and the evidence that EDs have some of the highest rates of preventable ADEs of any clinical environment, the presence of a clinical pharmacist in the ED is a necessary intervention, based on safety considerations alone. In addition to providing a needed layer of safety in the vulnerable ED environment, a clinical pharmacist likely provides a cost saving benefit to the ED, as demonstrated by this pilot and other studies. Further, the overwhelmingly positive response to this pilot by the veterans who participated shows that they want and need this service. Adding a clinical pharmacist to the ED is integral to the VA mission of providing patient-centered care. A larger study to obtain a more precise cost savings benefit within the VA system should be considered.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Schumock GT, Butler MG, Meek PD, et al. Evidence of the economic benefit of clinical pharmacy services: 1996-2000. Pharmacotherapy. 2003;23(1):113-132.
2. Pedersen CA, Schneider PJ, Scheckelhoff DJ. ASHP national survey of pharmacy practice in hospital settings: Prescribing and transcribing—2010. Am J Health Syst Pharm. 2011;68(8):669-688.
3. Rudis MI, Attwood RJ. Emergency medicine pharmacy practice. J Pharm Pract. 2011; 4(2):135-145.
4. Clancy CM. Evidence shows cost and patient safety benefits of emergency pharmacists. Am J Med Qual. 2008;23(3):231-233.
5. Fairbanks RJ, Hays DP, Webster DF, et al. Clinical pharmacy services in an emergency department. Am J Health Syst Pharm. 2004;61(9):934-937.
6. Abu-Ramaileh AM, Shane R, Churchill W, Steffenhagen A, Patka J, Rothschild JM. Evaluating and classifying pharmacists’ quality interventions in the emergency department. Am J Health Syst Pharm. 2011;68(23):2271-2275.
7. Committee on the Future of Emergency Care in the United States Health System. Hospital-Based Emergency Care: At the Breaking Point. Washington, DC: National Academies Press; 2006.
8. Szczesiul JM, Fairbanks RJ, Hildebrand JM, Hays DP, Shah MN. Survey of physicians regarding clinical pharmacy services in academic emergency departments. Am J Health Syst Pharm. 2009;66(6):576-579.
9. Pedersen CA, Schneider PJ, Scheckelhoff DJ. ASHP national survey of pharmacy practice in hospital settings: Dispensing and Administration—2005. Am J Health Syst Pharm. 2006;63(4):327-345.
10. Schenkel S. Promoting patient safety and preventing medical error in emergency departments. Acad Emerg Med. 2000;7(11):1204-1222.
11. Chin MH, Wang LC, Jin L, et al. Appropriateness of medication selection for older persons in an urban academic emergency department. Acad Emerg Med. 1999;6(12):1232-1242.
12. Hastings SN, Schmader KE, Sloane RJ, et al. Quality of pharmacotherapy and outcomes for older veterans discharged from the emergency department. J Am Geriatr Soc. 2008;56(5):875-880.
13. Rothschild JM, Churchill W, Erickson A, et al. Medication errors recovered by emergency department pharmacists. Ann Emerg Med. 2010;55(6):513-521.
14. Eppert HD, Reznek AJ; American Society of Health-System Pharmacists. ASHP guidelines on emergency medicine pharmacist services. Am J Health Syst Pharm. 2011;68(23):e81-95.
15. Lada P, Delgado G Jr. Documentation of pharmacists’ interventions in an emergency department and associated cost avoidance. Am J Health Syst Pharm. 2007;64(1):63-68.
16. Cohen V, Jellineck SP, Hatch A, Motov S. Effect of clinical pharmacists on care in the emergency department: A systematic review. Am J Health Syst Pharm. 2009;66(15):1353-1361.
17. Randolph TC. Expansion of pharmacists’ responsibilities in an emergency department. Am J Health Syst Pharm. 2009;66(16):1484-1487.
18. Hayes BD, Donovan JL, Smith BS, Hartman CA. Pharmacist-conducted medication reconciliation in an emergency department. Am J Health Syst Pharm. 2007;64(16):1720-1723.
19. DeWinter S, Spriet I, Indevuyst C, et al. Pharmacist-versus physician-acquired medication history: A prospective study at the emergency department. Qual Saf Health Care. 2010; 19(5):371-375.
20. American Society of Health-System Pharmacists. ASHP statement on pharmacy services to the emergency department. Am J Health Syst Pharm. 2008;65(24):2380-2383.
21. Ernst AA, Weiss SJ, Sullivan A IV, et al. On-site pharmacists in the ED improve medical errors. Am J Emerg Med. 2011;30(5):717-725.
22. Weant KA, Humphries RL, Hite K, Armitstead JA. Effect of emergency medicine pharmacists on medication-error reporting in an emergency department. Am J Health Syst Pharm. 2010;67(21):1851-1855.
23. Brown JN, Barnes CL, Beasley B, et al. Effect of pharmacists on medication errors in an emergency department. Am J Health Syst Pharm. 2008;65(4):330-333.
24. Holland R, Desborough J, Goodyer L, Hall S, Wright D, Loke YK. Does pharmacist-led medication review help to reduce hospital admissions and deaths in older people? A systematic review and meta-analysis. Br J Clin Pharmacol. 2008;65(3):303-316.
25. Marconi GP, Claudius I. Impact of an emergency department pharmacy on medication omission and delay. Pediatr Emerg Care. 2012;28(1):30-33.
26. Jellinek SP, Cohen V, Fancher LB, et al. Pharmacist improves timely administration of medications to boarded patients in the emergency department. J Emerg Nurs. 2010;36(2):105-110.
27. Pantanwala AE, Sanders AB, Thomas MC, et al. A prospective, multicenter study of pharmacist activities resulting in medication error interception in the emergency department. Ann Emerg Med. 2012;59(5)369-373.
28. Fairbanks RJ, Hildebrand JM, Kolstee KE, Schneider SM, Shah MN. Medical and nursing staff highly value clinical pharmacists in the emergency department. Emerg Med J. 2007;24(10):716-718.
29. Randolph TC, Parker A, Meyer L, Zeina R. Effect of pharmacist-managed culture review process on antimicrobial therapy in an emergency department. Am J Health Syst Pharm. 2011; 68(10):916-919.
30. Lee AJ, Boro MS, Knapp KK, Meier JL, Kirman NE. Clinical and economic outcomes of pharmacist recommendations in a veterans affairs medical center. Am J Health Syst Pharm. 2002;59(21):2070-2077.
31. Ling JM, Mike LA, Rubin J, et al. Documentation of pharmacist interventions in the emergency department. Am J Health Syst Pharm. 2005;62(17):1793-1797.
32. U.S. Bureau of Labor Statistics. Database, tools and calculators by subject. CPI inflation calculator. U.S. Bureau of Labor Statistics Website. http://www.bls.gov/data/inflation_calculator.htm. Accessed August 05, 2014.
33. Levy DB. Documentation of clinical and cost-saving pharmacy interventions in the emergency room. Hosp Pharm. 1993;28(7):624-627, 630-634, 653.
34. Uselton JP, Kienle P, Murdaugh LB, eds. Assuring Continuous Compliance With Joint Commission Standards: A Pharmacy Guide. 8th ed. Bethesda, MD: American Society of Health-System Pharmacists; 2010.
35. Pantanwala AE, Hays DP, Sanders AB, Erstad BL. Severity and probability of harm of medication errors intercepted by an emergency pharmacist. Int J Pharm Pract. 2011;19(5):358-362.
36. Raja AS, Lindsell CJ, Bernstein JA, Codispoti CD Moellman JJ. The use of penicillin skin testing to assess the prevalence of penicillin allergy in an emergency department setting. Ann Emerg Med. 2009;54(1):72-77.
1. Schumock GT, Butler MG, Meek PD, et al. Evidence of the economic benefit of clinical pharmacy services: 1996-2000. Pharmacotherapy. 2003;23(1):113-132.
2. Pedersen CA, Schneider PJ, Scheckelhoff DJ. ASHP national survey of pharmacy practice in hospital settings: Prescribing and transcribing—2010. Am J Health Syst Pharm. 2011;68(8):669-688.
3. Rudis MI, Attwood RJ. Emergency medicine pharmacy practice. J Pharm Pract. 2011; 4(2):135-145.
4. Clancy CM. Evidence shows cost and patient safety benefits of emergency pharmacists. Am J Med Qual. 2008;23(3):231-233.
5. Fairbanks RJ, Hays DP, Webster DF, et al. Clinical pharmacy services in an emergency department. Am J Health Syst Pharm. 2004;61(9):934-937.
6. Abu-Ramaileh AM, Shane R, Churchill W, Steffenhagen A, Patka J, Rothschild JM. Evaluating and classifying pharmacists’ quality interventions in the emergency department. Am J Health Syst Pharm. 2011;68(23):2271-2275.
7. Committee on the Future of Emergency Care in the United States Health System. Hospital-Based Emergency Care: At the Breaking Point. Washington, DC: National Academies Press; 2006.
8. Szczesiul JM, Fairbanks RJ, Hildebrand JM, Hays DP, Shah MN. Survey of physicians regarding clinical pharmacy services in academic emergency departments. Am J Health Syst Pharm. 2009;66(6):576-579.
9. Pedersen CA, Schneider PJ, Scheckelhoff DJ. ASHP national survey of pharmacy practice in hospital settings: Dispensing and Administration—2005. Am J Health Syst Pharm. 2006;63(4):327-345.
10. Schenkel S. Promoting patient safety and preventing medical error in emergency departments. Acad Emerg Med. 2000;7(11):1204-1222.
11. Chin MH, Wang LC, Jin L, et al. Appropriateness of medication selection for older persons in an urban academic emergency department. Acad Emerg Med. 1999;6(12):1232-1242.
12. Hastings SN, Schmader KE, Sloane RJ, et al. Quality of pharmacotherapy and outcomes for older veterans discharged from the emergency department. J Am Geriatr Soc. 2008;56(5):875-880.
13. Rothschild JM, Churchill W, Erickson A, et al. Medication errors recovered by emergency department pharmacists. Ann Emerg Med. 2010;55(6):513-521.
14. Eppert HD, Reznek AJ; American Society of Health-System Pharmacists. ASHP guidelines on emergency medicine pharmacist services. Am J Health Syst Pharm. 2011;68(23):e81-95.
15. Lada P, Delgado G Jr. Documentation of pharmacists’ interventions in an emergency department and associated cost avoidance. Am J Health Syst Pharm. 2007;64(1):63-68.
16. Cohen V, Jellineck SP, Hatch A, Motov S. Effect of clinical pharmacists on care in the emergency department: A systematic review. Am J Health Syst Pharm. 2009;66(15):1353-1361.
17. Randolph TC. Expansion of pharmacists’ responsibilities in an emergency department. Am J Health Syst Pharm. 2009;66(16):1484-1487.
18. Hayes BD, Donovan JL, Smith BS, Hartman CA. Pharmacist-conducted medication reconciliation in an emergency department. Am J Health Syst Pharm. 2007;64(16):1720-1723.
19. DeWinter S, Spriet I, Indevuyst C, et al. Pharmacist-versus physician-acquired medication history: A prospective study at the emergency department. Qual Saf Health Care. 2010; 19(5):371-375.
20. American Society of Health-System Pharmacists. ASHP statement on pharmacy services to the emergency department. Am J Health Syst Pharm. 2008;65(24):2380-2383.
21. Ernst AA, Weiss SJ, Sullivan A IV, et al. On-site pharmacists in the ED improve medical errors. Am J Emerg Med. 2011;30(5):717-725.
22. Weant KA, Humphries RL, Hite K, Armitstead JA. Effect of emergency medicine pharmacists on medication-error reporting in an emergency department. Am J Health Syst Pharm. 2010;67(21):1851-1855.
23. Brown JN, Barnes CL, Beasley B, et al. Effect of pharmacists on medication errors in an emergency department. Am J Health Syst Pharm. 2008;65(4):330-333.
24. Holland R, Desborough J, Goodyer L, Hall S, Wright D, Loke YK. Does pharmacist-led medication review help to reduce hospital admissions and deaths in older people? A systematic review and meta-analysis. Br J Clin Pharmacol. 2008;65(3):303-316.
25. Marconi GP, Claudius I. Impact of an emergency department pharmacy on medication omission and delay. Pediatr Emerg Care. 2012;28(1):30-33.
26. Jellinek SP, Cohen V, Fancher LB, et al. Pharmacist improves timely administration of medications to boarded patients in the emergency department. J Emerg Nurs. 2010;36(2):105-110.
27. Pantanwala AE, Sanders AB, Thomas MC, et al. A prospective, multicenter study of pharmacist activities resulting in medication error interception in the emergency department. Ann Emerg Med. 2012;59(5)369-373.
28. Fairbanks RJ, Hildebrand JM, Kolstee KE, Schneider SM, Shah MN. Medical and nursing staff highly value clinical pharmacists in the emergency department. Emerg Med J. 2007;24(10):716-718.
29. Randolph TC, Parker A, Meyer L, Zeina R. Effect of pharmacist-managed culture review process on antimicrobial therapy in an emergency department. Am J Health Syst Pharm. 2011; 68(10):916-919.
30. Lee AJ, Boro MS, Knapp KK, Meier JL, Kirman NE. Clinical and economic outcomes of pharmacist recommendations in a veterans affairs medical center. Am J Health Syst Pharm. 2002;59(21):2070-2077.
31. Ling JM, Mike LA, Rubin J, et al. Documentation of pharmacist interventions in the emergency department. Am J Health Syst Pharm. 2005;62(17):1793-1797.
32. U.S. Bureau of Labor Statistics. Database, tools and calculators by subject. CPI inflation calculator. U.S. Bureau of Labor Statistics Website. http://www.bls.gov/data/inflation_calculator.htm. Accessed August 05, 2014.
33. Levy DB. Documentation of clinical and cost-saving pharmacy interventions in the emergency room. Hosp Pharm. 1993;28(7):624-627, 630-634, 653.
34. Uselton JP, Kienle P, Murdaugh LB, eds. Assuring Continuous Compliance With Joint Commission Standards: A Pharmacy Guide. 8th ed. Bethesda, MD: American Society of Health-System Pharmacists; 2010.
35. Pantanwala AE, Hays DP, Sanders AB, Erstad BL. Severity and probability of harm of medication errors intercepted by an emergency pharmacist. Int J Pharm Pract. 2011;19(5):358-362.
36. Raja AS, Lindsell CJ, Bernstein JA, Codispoti CD Moellman JJ. The use of penicillin skin testing to assess the prevalence of penicillin allergy in an emergency department setting. Ann Emerg Med. 2009;54(1):72-77.