User login
From the Maine Medical Center, Portland, ME (Dr. Kramer, Ms. Palmeri, Dr. Robich, Mr. Groom, Dr. Hayes, Ms. Janoushek, Dr. Rappold, Dr. Swarz, and Dr. Quinn), and the Center for Outcomes Research and Evaluation, Maine Medical Center Research Institute, Portland, ME (Dr. Lucas).
Abstract
- Objective. To determine the accuracy of the glucometer currently used for point-of-care testing (POCT) of blood glucose in our cardiothoracic surgery intensive care unit (CTICU).
- Design. Prospective cohort study.
- Setting. Tertiary care community hospital affiliated with a school of medicine.
- Participants. Coronary artery bypass graft (CABG) surgery patients.
- Measurements. Blood glucose levels obtained via POCT with a glucometer using fingerstick and radial artery blood samples were compared with values obtained via central laboratory testing of radial artery blood samples (gold standard) in 106 CABG patients on continuous insulin infusions (CII) upon arrival to the CTICU from the operating room and 102 CABG patients on CII in the CTICU 6 hours later.
- Results. Fingerstick POCT and central lab blood glucose values correlated well (r = 0.83 for admission and 0.86 for 6-hour values), but the mean values were significantly different as determined by paired t-tests. Upon arrival, the fingerstick POCT mean value was 120.9 mg/dL, while the central laboratory value was 127.9 mg/dL (P value = 0.03). At the 6-hour time point, the mean value for fingerstick POCT was 129.7 mg/dL compared to a central laboratory value of 137.3 (P value = 0.02).
- Conclusion. The blood glucose POCT values correlated well with central laboratory values, but the values were statistically significantly different. Nevertheless, accurate clinical decisions were made despite the inaccuracies of POCT glucose testing, as experienced bedside nurses were able to use the glucometer successfully and safely. The device’s results informed them when the blood glucose was out of a prescibed range and the direction of the change, and they were able to adjust the CII accordingly.
Keywords: quality improvement; glucose management; point-of-care testing; critical care.
Achieving glycemic control in patients with and without diabetes during coronary artery bypass graft (CABG) surgery is associated with reduced perioperative morbidity and mortality and improved long-term survival.1 Hyperglycemia has detrimental effects on the cardiovascular system and insulin has beneficial effects on the ischemic myocardium.2 The current recommendations of the Society of Thoracic Surgery regarding blood glucose management include the use of continuous insulin infusions (CII) during and after surgery in the critical care unit,3 keeping blood glucose in a moderate range. Glucometers are commonly used in the critical care perioperative setting for point-of-care testing (POCT) for timely determinations of blood glucose levels for patients on CII.
POCT for glucose monitoring is a valuable tool for managing patients with diabetes in the outpatient setting. Evolving from urinary test strips that depended on a colorimetric model, glucometers now incoroporate digital technology that allows patients to determine their blood glucose using a drop of blood from a fingerstick. The US Food and Drug Administration’s approval for most glucose POCT technology includes home use by diabetic patients and use in the hospital setting, with the exception of critically ill patients, who may be affected by hypoxemia, poor capillary perfusion, tissue edema, severe anemia4 or other pathophysiologic states that could impact the accuracy of the devices. For example, poor peripheral perfusion related to shock or vasoconstrictors and interstitial edema are variables that could contribute to an erroneous reading. Therefore, many glucometers used in the critical care setting are being used off-label. Because much of the current POCT technology for glucose monitoring may provide erroneous results in certain ranges and in some clinical settings, the safety of most glucometers has been called into question.5,6
Given the concern regarding the potential inaccuracies of commonly used glucometers in the critical care setting, we undertook a quality improvement project to analyze the clinical performance of the glucometer currently used in our critically ill postoperative cardiac surgery population. The cardiac surgery division policy at our institution is to place all patients, both diabetic and nondiabetic, on a CII intraoperatively and to continue the infusion for at least 24 to 48 hours postoperatively. The CII start rate is determined utilizing the division’s Insulin Start Chart, and then the CII is adjusted according to the nomogram through the postoperative course. Both the Insulin Start Chart and nomogram have been previously described by Kramer et al.7
Currently, POCT of glucose in all post cardiac surgery patients is done hourly or more frequently in the first 24 to 48 hours after surgery in order to adjust the CII. In patients undergoing the stress of cardiac surgery, the action of insulin is counter-regulated by glucagon, epinephrine, norepinephrine, cortisol, and growth hormone. The resulting varying degrees of insulin resistance in this population of patients requires close monitoring of blood glucose, keeping it in a prescribed range, which in our center is 110 to 150 mg/dL, both in diabetic and nondiabetic patients. Frequent laboratory and POCT determinations of glucose are made. Providers and bedside nurses adjust the CII according to central laboratory values, POCT values, and trends, as previously described.7
Methods
Setting
Maine Medical Center is a 600-bed tertiary care teaching hospital. It is a level 1 trauma center where 1000 cardiac surgical operations are performed annually. POCT glucose monitoring is relied upon to monitor blood glucose and adjust the CII accordingly. This project, which did not require any additional procedures outside of the standard of care for this population of patients, was reviewed by the Institutional Review Board, who determined that this activity does not meet either the definition of research as specified under 45 CFR 46.102 (d) or the definition of clinical investigation as specified in 21 CFR 56.102 (c).
Patients
Using central laboratory glucose values drawn from the radial artery as the gold standard, we created a registry of consecutive postoperative cardiac surgery patients who had undergone CABG surgery and had blood glucose determinations from both POCT (fingerstick and radial artery samples) and central laboratory testing (radial artery sample) during a 7-month period (May 2016 through February 2017). To be included in the registry, patients had to (1) be postoperative following isolated CABG or CABG plus Maze procedure; (2) have been on cardiopulmonary bypass (CPB); (3) have radial arterial lines; and (4) be on a CII. A total of 116 patients qualified according to the inclusion criteria. Patients missing glucose results in 1 or more of the variables were excluded from data analysis.
Measurements and Variables
Using a POCT glucometer (FreeStyle Precision Pro, Abbott Laboratories, Abbott Park, IL), blood glucose conentrations were measured on samples obtained from both fingerstick and radial artery. Concurrently, radial arterial blood was sent to the central laboratory for glucose measurement. Blood glucose values were compared in CABG patients on CII upon arrival to the cardiothoracic surgery intensive care unit (CTICU) from the operating room and CABG patients on CII 6 hours after arrival in the CTICU. During the 6-hour interval, blood glucose levels were tested hourly or more frequently, allowing nurses to identify trends in blood glucose changes in order to keep blood glucose in the prescribed goal range of 110 to 150 mg/dL. At each of these 2 time points, on arrival to CTICU and 6 hours later, blood glucose values obtained with radial artery POCT and fingerstick POCT were compared with values obtained with central laboratory testing of radial artery samples. The amount of blood required was 1 drop each for POCT fingerstick and POCT radial artery and 2 mL for central lab testing.
Patient characteristics were identified from the electronic medical record. The variables recorded were type of operation, time on CPB, time of CTICU arrival, temperature, vasoconstrictor infusions (norepinephrine, vasopressin, phenylephrine), preoperative diagnosis of diabetes mellitus, preoperative HbA1c, and hemoglobin/hematocrit. Hemoglobin/hematocrit was only available at the time of the patient’s arrival to CTICU. The study was completed within the confines of our center’s standard of care protocol for postoperative cardiac surgical patients.
Analysis
We used standard statistical techniques to describe the study population, including proportions for categorical variables and means (standard deviations) for continuous variables. Correlation and regression techniques were used to describe the relationship between POCT and laboratory (gold standard) tests, both measured as continuous variables, and paired t-tests with Bonferroni correction were used to compare the central tendency and range of these comparisons. We calculated the differences between the gold standard measure and the POCT measure as an indication of outliers (ie, cases in which the 2 tests gave markedly different results). We examined plots to ascertain at which levels of the gold standard test these outliers occurred. An interim analysis was done at the halfway point and submitted to the Institutional Review Board, but no correction to the P value was done based on this analysis, which was largely qualitative. We used Bonferroni correction to declare a P value of 0.025 statistically significant with the 2-way comparisons of both fingerstick and radial artery values to central laboratory values. When the data was stratified by a clinical characteristic creating a 4-way comparison, we used Bonferroni correction to declare a P value of 0.0125 to be statistically significant when comparing both fingerstick and radial artery values to central laboratory values.
Results
Glucose POCT evaluations were carried out on 116 consecutive patients who underwent CABG surgery with or without a Maze procedure on CPB with a CII and an arterial line. Due to missing glucose results in 1 or more of the variables, 10 patients were excluded from data analysis for the time point of arrival in the CTICU and 14 patients were excluded from data analysis for the time point of 6 hours post CTICU arrival. This gave a final count of 106 CABG patients for CTICU arrival data analysis and 102 CABG patients for the 6 hours after CTICU arrival data analysis.
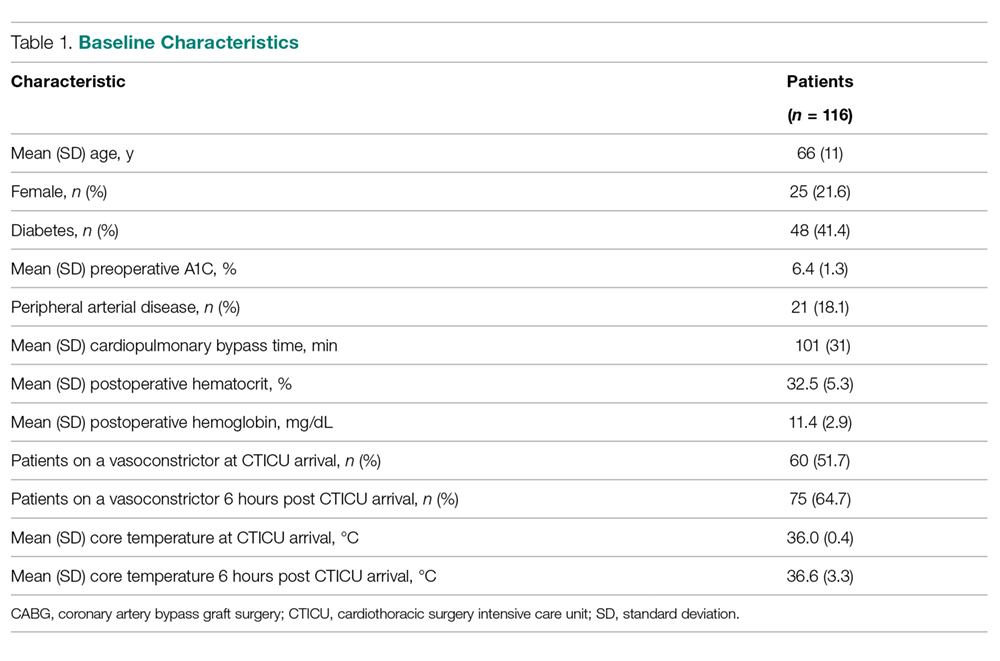
Patients ranged in age from 43 to 85 years, with a mean of age of 66 years, 22% were were women, 41% were diabetic, and 18% had peripheral vascular disease (Table 1). The average preoperative HbA1c was 6.4% ± 1.3% (range, 4.6% to 11.1%). Mean time on CBP for the group was 101 ± 31 minutes (range, 43 to 233 minutes). Postoperative mean hematocrit and hemoglobin were 32.5% and 11.4 g/dL, respectively. The average core temperature of patients on arrival was 36.0°C, which rose to an average of 36.6°C 6 hours later. A vasoconstrictor drip was infusing on 52% of patients upon CTICU arrival; 65% had a vasoconstrictor drip infusing 6 hours after arrival to the CTICU. Hemoglobin results were available only upon CTICU arrival as they are not routinely checked at 6 hours; 74 (64%) patients had a hemoglobin < 12 g/dL.
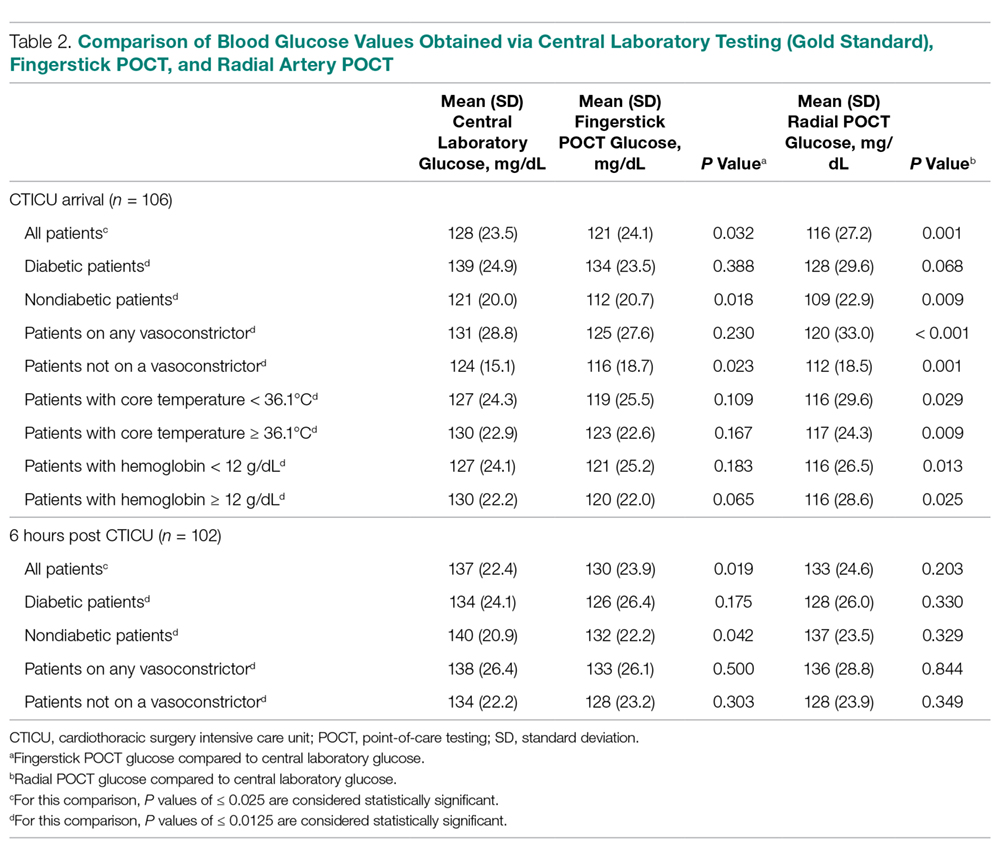
Compared to central laboratory testing, which we are defining as the gold standard, fingerstick POCT performed better on arrival, while radial artery POCT performed better at 6 hours (Table 2). At CTICU arrival, the mean blood glucose value for fingerstick POCT was 121 ± 24.1 mg/dL, 116 ± 27.2 mg/dL for radial artery POCT, and 128 ± 23.5 mg/dL for central lab testing. The difference in mean blood glucose between the fingerstick POCT and central lab testing was not statistically significant (P = 0.032), while the difference in mean blood glucose between radial artery POCT and central lab testing was statistically significant (P = 0.001). At 6 hours post arrival to the CTICU, the mean fingerstick POCT blood glucose value was 130 ± 23.9 mg/dL, compared to the mean central lab testing value of 137 ± 22.4 mg/dL; this difference was statistically significant (P = 0.019), while the radial artery POCT blood glucose value (133 ± 24.6 mg/dL) was not significantly different from the central lab testing value.
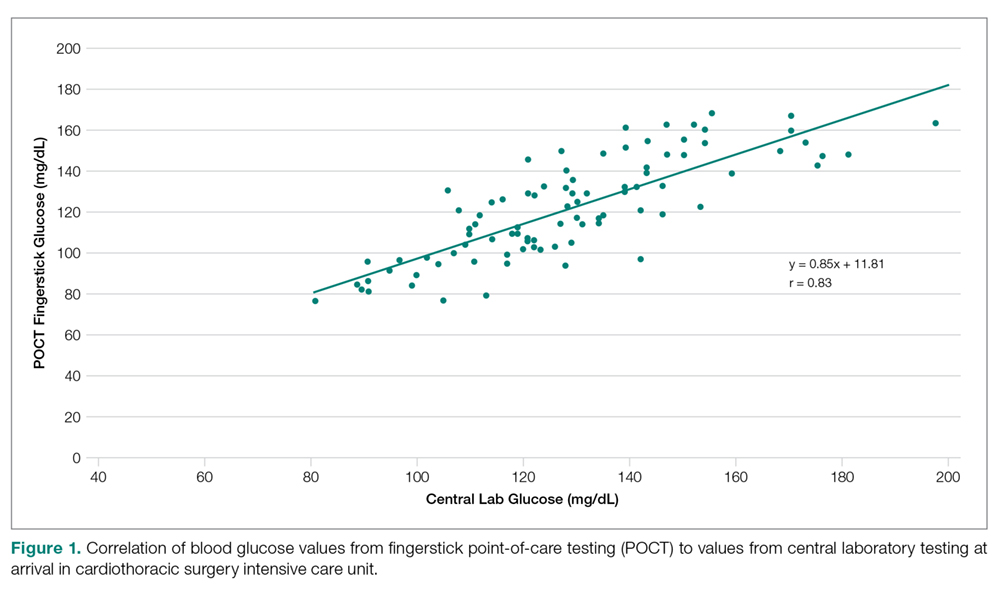
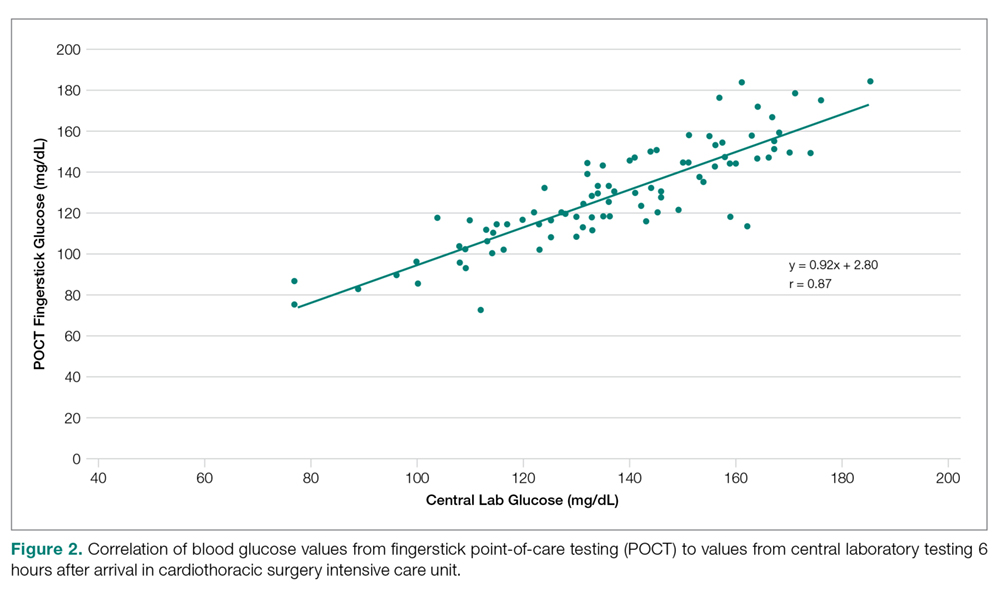
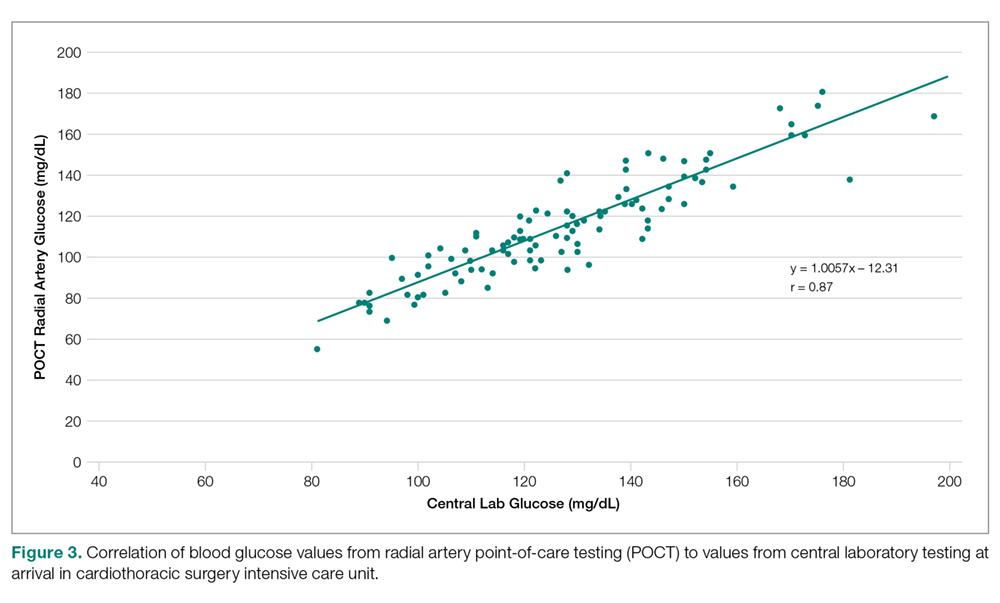
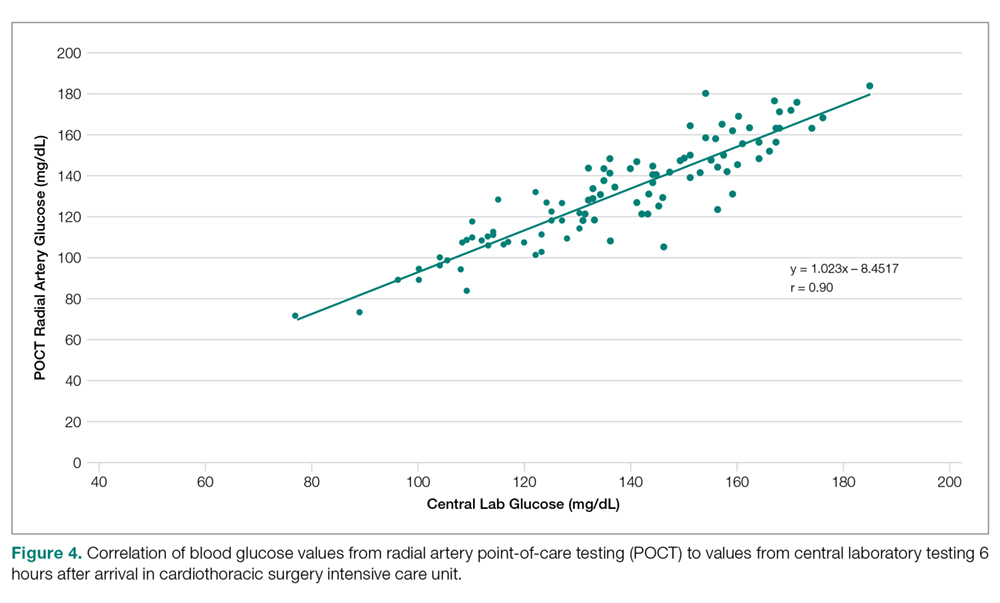
Blood glucose values from fingerstick POCT and central laboratory testing correlated well (r = 0.83 for admission and 0.86 for 6-hour values), as did radial artery POCT and central lab values (r = 0.87 for admission and 0.90 for 6-hour values) (Figures 1, 2, 3, and 4). Comparing individual values for fingerstick POCT and central lab testing, within-person differences between the 2 values ranged from –45 to 25 mg/dL, with 21% of pairs discrepant by 20 mg/dL or more (Figure 1); results were similar at 6 hours (Figure 2), with slightly less discrepancy.
The differences between radial artery POCT and central lab testing values at CTICU arrival ranged from –43 to 80 mg/dL, with 24% of pairs discrepant by 20 mg/dL or more (Figure 3). At 6 hours post CTICU arrival, the difference between radial artery POCT and central lab testing values ranged from –130 to 27 mg/dL, with 11% of pairs discrepant by 20 mg/dL or more (Figure 4). Ninety-two percent of central laboratory values were either close to (± 20) or within the moderate glycemic control target range (110–150 mg/dL).
When the patient cohort was stratified by anemia, diabetes, body temperature, and receipt of vasoconstrictor, there were no significant differences between mean fingerstick POCT and central lab testing values for any strata on CTICU arrival, while there were significant differences between radial artery POCT and central lab testing means for both vasoconstrictor strata as well as for patients with core temperature > 36.1°C (Table 2). At 6 hours, there were no statistically significant differences when stratified for receipt of vasoconstrictor or presence of diabetes. Stratification for anemia or core body temperature was not done for patients at the 6-hour post CTICU arrival time because no hemoglobin value was available and all patients except 1 reached a core temperature of 36.1°C.
Although we measured POCT values obtained using 2 different blood sample sources, fingerstick POCT performed better than radial artery POCT testing with regard to the mean values when compared with the central lab. However, radial artery POCT performed better with regard to correlation with the central lab value. In other words, fingerstick POCT values were less significantly different than radial artery POCT values when compared with the central lab, while radial artery POCT values correlated better with values from the central lab. In spite of this unexplained variability in differences and correlation, the blood glucose values stayed in the target goal range (Figures 1-4).
Discussion
The accuracy of glucose POCT in the critical care setting has been called into question.4,5 The clinical demands of glucose management using CII include timely and accurate guidance in postoperaptive cardiac surgery, in this case, CABG. A previous study compared POCT and central laboratory blood glucose values in medical intensive care unit patients,8 but not in patients who have had CABG surgery. Another study has reviewed the difference in glucose values from POCT and central lab analysis in the critically ill population, but not in the post cardiac surgical population.9 We have shown that the POCT blood glucose values correlate well with the clinical lab values, but the values are statistically different. Our study adds an additional observation in that, although the POCT inconsistencies were statistically significant, they were not clinically significant. That is, POCT of blood glucose was inaccurate, but it still helped guide care by providing enough information to keep the blood glucose in range (most of the time) and allowing the bedside nurse to detect trends and make appropriate adjustments to the infusion. However, given these inconsistencies, we recommend a low threshold for sending additional samples to the central lab to double-check the glucose values, especially when they are outside the prescribed range. Our analysis provides some measure of reassurance with regard to current postoperative CABG glucose management by showing that the limitations of the blood glucose meter do not jeopardize the safety of patients. Nonetheless, we look forward to advances in the accuracy of POCT blood glucose technology so that critical care patients can be better managed when blood glucose is outside the prescribed range.
This analysis of 116 CABG patients points out both the inaccuracy and the utility of a representative POCT glucometer (in this case, the FreeStyle Precision Pro) used at the bedside to manage CIIs in postoperative CABG patients, keeping the blood glucose level in the moderate control range (110-150 mg/dL). The correlation plot shows that in this population the bedside nurses were able to keep blood glucose in range most of the time, in spite of the inaccuracy of POCT of blood glucose, given that the error of the test fits in the wide margin of 40 mg/dL. The fact that the 6-hour values were slightly less variable than the admission values indicates that sequential determinations of blood glucose over the 6-hour period to detect trends allowed good clinical management even in the face of such inaccuracy. The correlation allows the inaccurate number (blood glucose value) to indicate direction, and frequent determinations allow the bedside nurse to keep that number in the prescribed range most of the time in this population of patients.
Conclusion
We have found that glucometer blood glucose determinations in our center used on a homogenous population (CABG surgery) utilizing a single type of glucometer correlated well with those of the central lab, but were not always accurate. In spite of the inaccuracies, experienced bedside nurses were able to use the instrument successfully and safely, as it informed them if the blood glucose was in or out of a predetermined range and in which direction it was going.
Acknowledgment: The authors are indebted to the nurses of the Cardiothoracic Surgery Intensive Care Unit at Maine Medical Center for their support and assistance, without which this analysis would not have been possible.
Corresponding author: Robert S. Kramer, MD, Division of Cardiothoracic Surgery, Maine Medical Center Cardiovascular Institute, 22 Bramhall St., Portland ME 04102; kramer@mmc.org.
Financial disclosures: None.
1. Furnary AP, Gao G, Grunkemeier GL, et al. Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003;125:1007-1021.
2. Lazar H. Glycemic control during coronary artery bypass graft surgery. ISRN Cardiol. 2012;2012:292490.
3. Lazar HL, McDonnell M, Chipkin SR, et al; Society of Thoracic Surgeons Blood Glucose Guideline Task Force. The Society of Thoracic Surgeons Practice Guideline Series: blood glucose management during adult cardiac surgery. Ann Thorac Surg. 2009;87:663-669.
4. US Food and Drug Administration. Blood Glucose Monitoring Test Systems for Prescription Point of Care Use. Guidance for Industry and Food and Drug Administration Staff,.www.fda.gov/downloads/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/UCM380325.pdf. Accessed March 8, 2019.
5. Finkielman JD, Oyen LJ, Afess B. Agreement between bedside blood and plasma glucose measurement in the ICU Setting. Chest. 2005;127:1749-1511.
6. Pidcoke HF, Wade CE, Mann EA, et al. Anemia causes hypoglycemia in ICU patients due to error in single-channel glucometers: methods of reducing patient risk. Crit Care Med. 2010;38:471-476.
7. Kramer R, Groom R, Weldner D, et al. Glycemic control reduces deep sternal wound infection: a multidisciplinary approach. Arch Surg. 2008;143:451-456.
8. Peterson JR, Graves DF, Tacker DH, et al. Comparison of POCT and central laboratory blood glucose results using arterial, capillary, and venous samples from MICU patients on a tight glycemic protocol. Clinica Chimica Acta. 2008;396:10-13.
9. Cook A, Laughlin D, Moore M, et al. Differences in glucose values obtained from point-of-care glucose meters and laboratory analysis in critically ill patients. Am J Crit Care. 2009;18:65-72.
From the Maine Medical Center, Portland, ME (Dr. Kramer, Ms. Palmeri, Dr. Robich, Mr. Groom, Dr. Hayes, Ms. Janoushek, Dr. Rappold, Dr. Swarz, and Dr. Quinn), and the Center for Outcomes Research and Evaluation, Maine Medical Center Research Institute, Portland, ME (Dr. Lucas).
Abstract
- Objective. To determine the accuracy of the glucometer currently used for point-of-care testing (POCT) of blood glucose in our cardiothoracic surgery intensive care unit (CTICU).
- Design. Prospective cohort study.
- Setting. Tertiary care community hospital affiliated with a school of medicine.
- Participants. Coronary artery bypass graft (CABG) surgery patients.
- Measurements. Blood glucose levels obtained via POCT with a glucometer using fingerstick and radial artery blood samples were compared with values obtained via central laboratory testing of radial artery blood samples (gold standard) in 106 CABG patients on continuous insulin infusions (CII) upon arrival to the CTICU from the operating room and 102 CABG patients on CII in the CTICU 6 hours later.
- Results. Fingerstick POCT and central lab blood glucose values correlated well (r = 0.83 for admission and 0.86 for 6-hour values), but the mean values were significantly different as determined by paired t-tests. Upon arrival, the fingerstick POCT mean value was 120.9 mg/dL, while the central laboratory value was 127.9 mg/dL (P value = 0.03). At the 6-hour time point, the mean value for fingerstick POCT was 129.7 mg/dL compared to a central laboratory value of 137.3 (P value = 0.02).
- Conclusion. The blood glucose POCT values correlated well with central laboratory values, but the values were statistically significantly different. Nevertheless, accurate clinical decisions were made despite the inaccuracies of POCT glucose testing, as experienced bedside nurses were able to use the glucometer successfully and safely. The device’s results informed them when the blood glucose was out of a prescibed range and the direction of the change, and they were able to adjust the CII accordingly.
Keywords: quality improvement; glucose management; point-of-care testing; critical care.
Achieving glycemic control in patients with and without diabetes during coronary artery bypass graft (CABG) surgery is associated with reduced perioperative morbidity and mortality and improved long-term survival.1 Hyperglycemia has detrimental effects on the cardiovascular system and insulin has beneficial effects on the ischemic myocardium.2 The current recommendations of the Society of Thoracic Surgery regarding blood glucose management include the use of continuous insulin infusions (CII) during and after surgery in the critical care unit,3 keeping blood glucose in a moderate range. Glucometers are commonly used in the critical care perioperative setting for point-of-care testing (POCT) for timely determinations of blood glucose levels for patients on CII.
POCT for glucose monitoring is a valuable tool for managing patients with diabetes in the outpatient setting. Evolving from urinary test strips that depended on a colorimetric model, glucometers now incoroporate digital technology that allows patients to determine their blood glucose using a drop of blood from a fingerstick. The US Food and Drug Administration’s approval for most glucose POCT technology includes home use by diabetic patients and use in the hospital setting, with the exception of critically ill patients, who may be affected by hypoxemia, poor capillary perfusion, tissue edema, severe anemia4 or other pathophysiologic states that could impact the accuracy of the devices. For example, poor peripheral perfusion related to shock or vasoconstrictors and interstitial edema are variables that could contribute to an erroneous reading. Therefore, many glucometers used in the critical care setting are being used off-label. Because much of the current POCT technology for glucose monitoring may provide erroneous results in certain ranges and in some clinical settings, the safety of most glucometers has been called into question.5,6
Given the concern regarding the potential inaccuracies of commonly used glucometers in the critical care setting, we undertook a quality improvement project to analyze the clinical performance of the glucometer currently used in our critically ill postoperative cardiac surgery population. The cardiac surgery division policy at our institution is to place all patients, both diabetic and nondiabetic, on a CII intraoperatively and to continue the infusion for at least 24 to 48 hours postoperatively. The CII start rate is determined utilizing the division’s Insulin Start Chart, and then the CII is adjusted according to the nomogram through the postoperative course. Both the Insulin Start Chart and nomogram have been previously described by Kramer et al.7
Currently, POCT of glucose in all post cardiac surgery patients is done hourly or more frequently in the first 24 to 48 hours after surgery in order to adjust the CII. In patients undergoing the stress of cardiac surgery, the action of insulin is counter-regulated by glucagon, epinephrine, norepinephrine, cortisol, and growth hormone. The resulting varying degrees of insulin resistance in this population of patients requires close monitoring of blood glucose, keeping it in a prescribed range, which in our center is 110 to 150 mg/dL, both in diabetic and nondiabetic patients. Frequent laboratory and POCT determinations of glucose are made. Providers and bedside nurses adjust the CII according to central laboratory values, POCT values, and trends, as previously described.7
Methods
Setting
Maine Medical Center is a 600-bed tertiary care teaching hospital. It is a level 1 trauma center where 1000 cardiac surgical operations are performed annually. POCT glucose monitoring is relied upon to monitor blood glucose and adjust the CII accordingly. This project, which did not require any additional procedures outside of the standard of care for this population of patients, was reviewed by the Institutional Review Board, who determined that this activity does not meet either the definition of research as specified under 45 CFR 46.102 (d) or the definition of clinical investigation as specified in 21 CFR 56.102 (c).
Patients
Using central laboratory glucose values drawn from the radial artery as the gold standard, we created a registry of consecutive postoperative cardiac surgery patients who had undergone CABG surgery and had blood glucose determinations from both POCT (fingerstick and radial artery samples) and central laboratory testing (radial artery sample) during a 7-month period (May 2016 through February 2017). To be included in the registry, patients had to (1) be postoperative following isolated CABG or CABG plus Maze procedure; (2) have been on cardiopulmonary bypass (CPB); (3) have radial arterial lines; and (4) be on a CII. A total of 116 patients qualified according to the inclusion criteria. Patients missing glucose results in 1 or more of the variables were excluded from data analysis.
Measurements and Variables
Using a POCT glucometer (FreeStyle Precision Pro, Abbott Laboratories, Abbott Park, IL), blood glucose conentrations were measured on samples obtained from both fingerstick and radial artery. Concurrently, radial arterial blood was sent to the central laboratory for glucose measurement. Blood glucose values were compared in CABG patients on CII upon arrival to the cardiothoracic surgery intensive care unit (CTICU) from the operating room and CABG patients on CII 6 hours after arrival in the CTICU. During the 6-hour interval, blood glucose levels were tested hourly or more frequently, allowing nurses to identify trends in blood glucose changes in order to keep blood glucose in the prescribed goal range of 110 to 150 mg/dL. At each of these 2 time points, on arrival to CTICU and 6 hours later, blood glucose values obtained with radial artery POCT and fingerstick POCT were compared with values obtained with central laboratory testing of radial artery samples. The amount of blood required was 1 drop each for POCT fingerstick and POCT radial artery and 2 mL for central lab testing.
Patient characteristics were identified from the electronic medical record. The variables recorded were type of operation, time on CPB, time of CTICU arrival, temperature, vasoconstrictor infusions (norepinephrine, vasopressin, phenylephrine), preoperative diagnosis of diabetes mellitus, preoperative HbA1c, and hemoglobin/hematocrit. Hemoglobin/hematocrit was only available at the time of the patient’s arrival to CTICU. The study was completed within the confines of our center’s standard of care protocol for postoperative cardiac surgical patients.
Analysis
We used standard statistical techniques to describe the study population, including proportions for categorical variables and means (standard deviations) for continuous variables. Correlation and regression techniques were used to describe the relationship between POCT and laboratory (gold standard) tests, both measured as continuous variables, and paired t-tests with Bonferroni correction were used to compare the central tendency and range of these comparisons. We calculated the differences between the gold standard measure and the POCT measure as an indication of outliers (ie, cases in which the 2 tests gave markedly different results). We examined plots to ascertain at which levels of the gold standard test these outliers occurred. An interim analysis was done at the halfway point and submitted to the Institutional Review Board, but no correction to the P value was done based on this analysis, which was largely qualitative. We used Bonferroni correction to declare a P value of 0.025 statistically significant with the 2-way comparisons of both fingerstick and radial artery values to central laboratory values. When the data was stratified by a clinical characteristic creating a 4-way comparison, we used Bonferroni correction to declare a P value of 0.0125 to be statistically significant when comparing both fingerstick and radial artery values to central laboratory values.
Results
Glucose POCT evaluations were carried out on 116 consecutive patients who underwent CABG surgery with or without a Maze procedure on CPB with a CII and an arterial line. Due to missing glucose results in 1 or more of the variables, 10 patients were excluded from data analysis for the time point of arrival in the CTICU and 14 patients were excluded from data analysis for the time point of 6 hours post CTICU arrival. This gave a final count of 106 CABG patients for CTICU arrival data analysis and 102 CABG patients for the 6 hours after CTICU arrival data analysis.
Patients ranged in age from 43 to 85 years, with a mean of age of 66 years, 22% were were women, 41% were diabetic, and 18% had peripheral vascular disease (Table 1). The average preoperative HbA1c was 6.4% ± 1.3% (range, 4.6% to 11.1%). Mean time on CBP for the group was 101 ± 31 minutes (range, 43 to 233 minutes). Postoperative mean hematocrit and hemoglobin were 32.5% and 11.4 g/dL, respectively. The average core temperature of patients on arrival was 36.0°C, which rose to an average of 36.6°C 6 hours later. A vasoconstrictor drip was infusing on 52% of patients upon CTICU arrival; 65% had a vasoconstrictor drip infusing 6 hours after arrival to the CTICU. Hemoglobin results were available only upon CTICU arrival as they are not routinely checked at 6 hours; 74 (64%) patients had a hemoglobin < 12 g/dL.
Compared to central laboratory testing, which we are defining as the gold standard, fingerstick POCT performed better on arrival, while radial artery POCT performed better at 6 hours (Table 2). At CTICU arrival, the mean blood glucose value for fingerstick POCT was 121 ± 24.1 mg/dL, 116 ± 27.2 mg/dL for radial artery POCT, and 128 ± 23.5 mg/dL for central lab testing. The difference in mean blood glucose between the fingerstick POCT and central lab testing was not statistically significant (P = 0.032), while the difference in mean blood glucose between radial artery POCT and central lab testing was statistically significant (P = 0.001). At 6 hours post arrival to the CTICU, the mean fingerstick POCT blood glucose value was 130 ± 23.9 mg/dL, compared to the mean central lab testing value of 137 ± 22.4 mg/dL; this difference was statistically significant (P = 0.019), while the radial artery POCT blood glucose value (133 ± 24.6 mg/dL) was not significantly different from the central lab testing value.
Blood glucose values from fingerstick POCT and central laboratory testing correlated well (r = 0.83 for admission and 0.86 for 6-hour values), as did radial artery POCT and central lab values (r = 0.87 for admission and 0.90 for 6-hour values) (Figures 1, 2, 3, and 4). Comparing individual values for fingerstick POCT and central lab testing, within-person differences between the 2 values ranged from –45 to 25 mg/dL, with 21% of pairs discrepant by 20 mg/dL or more (Figure 1); results were similar at 6 hours (Figure 2), with slightly less discrepancy.
The differences between radial artery POCT and central lab testing values at CTICU arrival ranged from –43 to 80 mg/dL, with 24% of pairs discrepant by 20 mg/dL or more (Figure 3). At 6 hours post CTICU arrival, the difference between radial artery POCT and central lab testing values ranged from –130 to 27 mg/dL, with 11% of pairs discrepant by 20 mg/dL or more (Figure 4). Ninety-two percent of central laboratory values were either close to (± 20) or within the moderate glycemic control target range (110–150 mg/dL).
When the patient cohort was stratified by anemia, diabetes, body temperature, and receipt of vasoconstrictor, there were no significant differences between mean fingerstick POCT and central lab testing values for any strata on CTICU arrival, while there were significant differences between radial artery POCT and central lab testing means for both vasoconstrictor strata as well as for patients with core temperature > 36.1°C (Table 2). At 6 hours, there were no statistically significant differences when stratified for receipt of vasoconstrictor or presence of diabetes. Stratification for anemia or core body temperature was not done for patients at the 6-hour post CTICU arrival time because no hemoglobin value was available and all patients except 1 reached a core temperature of 36.1°C.
Although we measured POCT values obtained using 2 different blood sample sources, fingerstick POCT performed better than radial artery POCT testing with regard to the mean values when compared with the central lab. However, radial artery POCT performed better with regard to correlation with the central lab value. In other words, fingerstick POCT values were less significantly different than radial artery POCT values when compared with the central lab, while radial artery POCT values correlated better with values from the central lab. In spite of this unexplained variability in differences and correlation, the blood glucose values stayed in the target goal range (Figures 1-4).
Discussion
The accuracy of glucose POCT in the critical care setting has been called into question.4,5 The clinical demands of glucose management using CII include timely and accurate guidance in postoperaptive cardiac surgery, in this case, CABG. A previous study compared POCT and central laboratory blood glucose values in medical intensive care unit patients,8 but not in patients who have had CABG surgery. Another study has reviewed the difference in glucose values from POCT and central lab analysis in the critically ill population, but not in the post cardiac surgical population.9 We have shown that the POCT blood glucose values correlate well with the clinical lab values, but the values are statistically different. Our study adds an additional observation in that, although the POCT inconsistencies were statistically significant, they were not clinically significant. That is, POCT of blood glucose was inaccurate, but it still helped guide care by providing enough information to keep the blood glucose in range (most of the time) and allowing the bedside nurse to detect trends and make appropriate adjustments to the infusion. However, given these inconsistencies, we recommend a low threshold for sending additional samples to the central lab to double-check the glucose values, especially when they are outside the prescribed range. Our analysis provides some measure of reassurance with regard to current postoperative CABG glucose management by showing that the limitations of the blood glucose meter do not jeopardize the safety of patients. Nonetheless, we look forward to advances in the accuracy of POCT blood glucose technology so that critical care patients can be better managed when blood glucose is outside the prescribed range.
This analysis of 116 CABG patients points out both the inaccuracy and the utility of a representative POCT glucometer (in this case, the FreeStyle Precision Pro) used at the bedside to manage CIIs in postoperative CABG patients, keeping the blood glucose level in the moderate control range (110-150 mg/dL). The correlation plot shows that in this population the bedside nurses were able to keep blood glucose in range most of the time, in spite of the inaccuracy of POCT of blood glucose, given that the error of the test fits in the wide margin of 40 mg/dL. The fact that the 6-hour values were slightly less variable than the admission values indicates that sequential determinations of blood glucose over the 6-hour period to detect trends allowed good clinical management even in the face of such inaccuracy. The correlation allows the inaccurate number (blood glucose value) to indicate direction, and frequent determinations allow the bedside nurse to keep that number in the prescribed range most of the time in this population of patients.
Conclusion
We have found that glucometer blood glucose determinations in our center used on a homogenous population (CABG surgery) utilizing a single type of glucometer correlated well with those of the central lab, but were not always accurate. In spite of the inaccuracies, experienced bedside nurses were able to use the instrument successfully and safely, as it informed them if the blood glucose was in or out of a predetermined range and in which direction it was going.
Acknowledgment: The authors are indebted to the nurses of the Cardiothoracic Surgery Intensive Care Unit at Maine Medical Center for their support and assistance, without which this analysis would not have been possible.
Corresponding author: Robert S. Kramer, MD, Division of Cardiothoracic Surgery, Maine Medical Center Cardiovascular Institute, 22 Bramhall St., Portland ME 04102; kramer@mmc.org.
Financial disclosures: None.
From the Maine Medical Center, Portland, ME (Dr. Kramer, Ms. Palmeri, Dr. Robich, Mr. Groom, Dr. Hayes, Ms. Janoushek, Dr. Rappold, Dr. Swarz, and Dr. Quinn), and the Center for Outcomes Research and Evaluation, Maine Medical Center Research Institute, Portland, ME (Dr. Lucas).
Abstract
- Objective. To determine the accuracy of the glucometer currently used for point-of-care testing (POCT) of blood glucose in our cardiothoracic surgery intensive care unit (CTICU).
- Design. Prospective cohort study.
- Setting. Tertiary care community hospital affiliated with a school of medicine.
- Participants. Coronary artery bypass graft (CABG) surgery patients.
- Measurements. Blood glucose levels obtained via POCT with a glucometer using fingerstick and radial artery blood samples were compared with values obtained via central laboratory testing of radial artery blood samples (gold standard) in 106 CABG patients on continuous insulin infusions (CII) upon arrival to the CTICU from the operating room and 102 CABG patients on CII in the CTICU 6 hours later.
- Results. Fingerstick POCT and central lab blood glucose values correlated well (r = 0.83 for admission and 0.86 for 6-hour values), but the mean values were significantly different as determined by paired t-tests. Upon arrival, the fingerstick POCT mean value was 120.9 mg/dL, while the central laboratory value was 127.9 mg/dL (P value = 0.03). At the 6-hour time point, the mean value for fingerstick POCT was 129.7 mg/dL compared to a central laboratory value of 137.3 (P value = 0.02).
- Conclusion. The blood glucose POCT values correlated well with central laboratory values, but the values were statistically significantly different. Nevertheless, accurate clinical decisions were made despite the inaccuracies of POCT glucose testing, as experienced bedside nurses were able to use the glucometer successfully and safely. The device’s results informed them when the blood glucose was out of a prescibed range and the direction of the change, and they were able to adjust the CII accordingly.
Keywords: quality improvement; glucose management; point-of-care testing; critical care.
Achieving glycemic control in patients with and without diabetes during coronary artery bypass graft (CABG) surgery is associated with reduced perioperative morbidity and mortality and improved long-term survival.1 Hyperglycemia has detrimental effects on the cardiovascular system and insulin has beneficial effects on the ischemic myocardium.2 The current recommendations of the Society of Thoracic Surgery regarding blood glucose management include the use of continuous insulin infusions (CII) during and after surgery in the critical care unit,3 keeping blood glucose in a moderate range. Glucometers are commonly used in the critical care perioperative setting for point-of-care testing (POCT) for timely determinations of blood glucose levels for patients on CII.
POCT for glucose monitoring is a valuable tool for managing patients with diabetes in the outpatient setting. Evolving from urinary test strips that depended on a colorimetric model, glucometers now incoroporate digital technology that allows patients to determine their blood glucose using a drop of blood from a fingerstick. The US Food and Drug Administration’s approval for most glucose POCT technology includes home use by diabetic patients and use in the hospital setting, with the exception of critically ill patients, who may be affected by hypoxemia, poor capillary perfusion, tissue edema, severe anemia4 or other pathophysiologic states that could impact the accuracy of the devices. For example, poor peripheral perfusion related to shock or vasoconstrictors and interstitial edema are variables that could contribute to an erroneous reading. Therefore, many glucometers used in the critical care setting are being used off-label. Because much of the current POCT technology for glucose monitoring may provide erroneous results in certain ranges and in some clinical settings, the safety of most glucometers has been called into question.5,6
Given the concern regarding the potential inaccuracies of commonly used glucometers in the critical care setting, we undertook a quality improvement project to analyze the clinical performance of the glucometer currently used in our critically ill postoperative cardiac surgery population. The cardiac surgery division policy at our institution is to place all patients, both diabetic and nondiabetic, on a CII intraoperatively and to continue the infusion for at least 24 to 48 hours postoperatively. The CII start rate is determined utilizing the division’s Insulin Start Chart, and then the CII is adjusted according to the nomogram through the postoperative course. Both the Insulin Start Chart and nomogram have been previously described by Kramer et al.7
Currently, POCT of glucose in all post cardiac surgery patients is done hourly or more frequently in the first 24 to 48 hours after surgery in order to adjust the CII. In patients undergoing the stress of cardiac surgery, the action of insulin is counter-regulated by glucagon, epinephrine, norepinephrine, cortisol, and growth hormone. The resulting varying degrees of insulin resistance in this population of patients requires close monitoring of blood glucose, keeping it in a prescribed range, which in our center is 110 to 150 mg/dL, both in diabetic and nondiabetic patients. Frequent laboratory and POCT determinations of glucose are made. Providers and bedside nurses adjust the CII according to central laboratory values, POCT values, and trends, as previously described.7
Methods
Setting
Maine Medical Center is a 600-bed tertiary care teaching hospital. It is a level 1 trauma center where 1000 cardiac surgical operations are performed annually. POCT glucose monitoring is relied upon to monitor blood glucose and adjust the CII accordingly. This project, which did not require any additional procedures outside of the standard of care for this population of patients, was reviewed by the Institutional Review Board, who determined that this activity does not meet either the definition of research as specified under 45 CFR 46.102 (d) or the definition of clinical investigation as specified in 21 CFR 56.102 (c).
Patients
Using central laboratory glucose values drawn from the radial artery as the gold standard, we created a registry of consecutive postoperative cardiac surgery patients who had undergone CABG surgery and had blood glucose determinations from both POCT (fingerstick and radial artery samples) and central laboratory testing (radial artery sample) during a 7-month period (May 2016 through February 2017). To be included in the registry, patients had to (1) be postoperative following isolated CABG or CABG plus Maze procedure; (2) have been on cardiopulmonary bypass (CPB); (3) have radial arterial lines; and (4) be on a CII. A total of 116 patients qualified according to the inclusion criteria. Patients missing glucose results in 1 or more of the variables were excluded from data analysis.
Measurements and Variables
Using a POCT glucometer (FreeStyle Precision Pro, Abbott Laboratories, Abbott Park, IL), blood glucose conentrations were measured on samples obtained from both fingerstick and radial artery. Concurrently, radial arterial blood was sent to the central laboratory for glucose measurement. Blood glucose values were compared in CABG patients on CII upon arrival to the cardiothoracic surgery intensive care unit (CTICU) from the operating room and CABG patients on CII 6 hours after arrival in the CTICU. During the 6-hour interval, blood glucose levels were tested hourly or more frequently, allowing nurses to identify trends in blood glucose changes in order to keep blood glucose in the prescribed goal range of 110 to 150 mg/dL. At each of these 2 time points, on arrival to CTICU and 6 hours later, blood glucose values obtained with radial artery POCT and fingerstick POCT were compared with values obtained with central laboratory testing of radial artery samples. The amount of blood required was 1 drop each for POCT fingerstick and POCT radial artery and 2 mL for central lab testing.
Patient characteristics were identified from the electronic medical record. The variables recorded were type of operation, time on CPB, time of CTICU arrival, temperature, vasoconstrictor infusions (norepinephrine, vasopressin, phenylephrine), preoperative diagnosis of diabetes mellitus, preoperative HbA1c, and hemoglobin/hematocrit. Hemoglobin/hematocrit was only available at the time of the patient’s arrival to CTICU. The study was completed within the confines of our center’s standard of care protocol for postoperative cardiac surgical patients.
Analysis
We used standard statistical techniques to describe the study population, including proportions for categorical variables and means (standard deviations) for continuous variables. Correlation and regression techniques were used to describe the relationship between POCT and laboratory (gold standard) tests, both measured as continuous variables, and paired t-tests with Bonferroni correction were used to compare the central tendency and range of these comparisons. We calculated the differences between the gold standard measure and the POCT measure as an indication of outliers (ie, cases in which the 2 tests gave markedly different results). We examined plots to ascertain at which levels of the gold standard test these outliers occurred. An interim analysis was done at the halfway point and submitted to the Institutional Review Board, but no correction to the P value was done based on this analysis, which was largely qualitative. We used Bonferroni correction to declare a P value of 0.025 statistically significant with the 2-way comparisons of both fingerstick and radial artery values to central laboratory values. When the data was stratified by a clinical characteristic creating a 4-way comparison, we used Bonferroni correction to declare a P value of 0.0125 to be statistically significant when comparing both fingerstick and radial artery values to central laboratory values.
Results
Glucose POCT evaluations were carried out on 116 consecutive patients who underwent CABG surgery with or without a Maze procedure on CPB with a CII and an arterial line. Due to missing glucose results in 1 or more of the variables, 10 patients were excluded from data analysis for the time point of arrival in the CTICU and 14 patients were excluded from data analysis for the time point of 6 hours post CTICU arrival. This gave a final count of 106 CABG patients for CTICU arrival data analysis and 102 CABG patients for the 6 hours after CTICU arrival data analysis.
Patients ranged in age from 43 to 85 years, with a mean of age of 66 years, 22% were were women, 41% were diabetic, and 18% had peripheral vascular disease (Table 1). The average preoperative HbA1c was 6.4% ± 1.3% (range, 4.6% to 11.1%). Mean time on CBP for the group was 101 ± 31 minutes (range, 43 to 233 minutes). Postoperative mean hematocrit and hemoglobin were 32.5% and 11.4 g/dL, respectively. The average core temperature of patients on arrival was 36.0°C, which rose to an average of 36.6°C 6 hours later. A vasoconstrictor drip was infusing on 52% of patients upon CTICU arrival; 65% had a vasoconstrictor drip infusing 6 hours after arrival to the CTICU. Hemoglobin results were available only upon CTICU arrival as they are not routinely checked at 6 hours; 74 (64%) patients had a hemoglobin < 12 g/dL.
Compared to central laboratory testing, which we are defining as the gold standard, fingerstick POCT performed better on arrival, while radial artery POCT performed better at 6 hours (Table 2). At CTICU arrival, the mean blood glucose value for fingerstick POCT was 121 ± 24.1 mg/dL, 116 ± 27.2 mg/dL for radial artery POCT, and 128 ± 23.5 mg/dL for central lab testing. The difference in mean blood glucose between the fingerstick POCT and central lab testing was not statistically significant (P = 0.032), while the difference in mean blood glucose between radial artery POCT and central lab testing was statistically significant (P = 0.001). At 6 hours post arrival to the CTICU, the mean fingerstick POCT blood glucose value was 130 ± 23.9 mg/dL, compared to the mean central lab testing value of 137 ± 22.4 mg/dL; this difference was statistically significant (P = 0.019), while the radial artery POCT blood glucose value (133 ± 24.6 mg/dL) was not significantly different from the central lab testing value.
Blood glucose values from fingerstick POCT and central laboratory testing correlated well (r = 0.83 for admission and 0.86 for 6-hour values), as did radial artery POCT and central lab values (r = 0.87 for admission and 0.90 for 6-hour values) (Figures 1, 2, 3, and 4). Comparing individual values for fingerstick POCT and central lab testing, within-person differences between the 2 values ranged from –45 to 25 mg/dL, with 21% of pairs discrepant by 20 mg/dL or more (Figure 1); results were similar at 6 hours (Figure 2), with slightly less discrepancy.
The differences between radial artery POCT and central lab testing values at CTICU arrival ranged from –43 to 80 mg/dL, with 24% of pairs discrepant by 20 mg/dL or more (Figure 3). At 6 hours post CTICU arrival, the difference between radial artery POCT and central lab testing values ranged from –130 to 27 mg/dL, with 11% of pairs discrepant by 20 mg/dL or more (Figure 4). Ninety-two percent of central laboratory values were either close to (± 20) or within the moderate glycemic control target range (110–150 mg/dL).
When the patient cohort was stratified by anemia, diabetes, body temperature, and receipt of vasoconstrictor, there were no significant differences between mean fingerstick POCT and central lab testing values for any strata on CTICU arrival, while there were significant differences between radial artery POCT and central lab testing means for both vasoconstrictor strata as well as for patients with core temperature > 36.1°C (Table 2). At 6 hours, there were no statistically significant differences when stratified for receipt of vasoconstrictor or presence of diabetes. Stratification for anemia or core body temperature was not done for patients at the 6-hour post CTICU arrival time because no hemoglobin value was available and all patients except 1 reached a core temperature of 36.1°C.
Although we measured POCT values obtained using 2 different blood sample sources, fingerstick POCT performed better than radial artery POCT testing with regard to the mean values when compared with the central lab. However, radial artery POCT performed better with regard to correlation with the central lab value. In other words, fingerstick POCT values were less significantly different than radial artery POCT values when compared with the central lab, while radial artery POCT values correlated better with values from the central lab. In spite of this unexplained variability in differences and correlation, the blood glucose values stayed in the target goal range (Figures 1-4).
Discussion
The accuracy of glucose POCT in the critical care setting has been called into question.4,5 The clinical demands of glucose management using CII include timely and accurate guidance in postoperaptive cardiac surgery, in this case, CABG. A previous study compared POCT and central laboratory blood glucose values in medical intensive care unit patients,8 but not in patients who have had CABG surgery. Another study has reviewed the difference in glucose values from POCT and central lab analysis in the critically ill population, but not in the post cardiac surgical population.9 We have shown that the POCT blood glucose values correlate well with the clinical lab values, but the values are statistically different. Our study adds an additional observation in that, although the POCT inconsistencies were statistically significant, they were not clinically significant. That is, POCT of blood glucose was inaccurate, but it still helped guide care by providing enough information to keep the blood glucose in range (most of the time) and allowing the bedside nurse to detect trends and make appropriate adjustments to the infusion. However, given these inconsistencies, we recommend a low threshold for sending additional samples to the central lab to double-check the glucose values, especially when they are outside the prescribed range. Our analysis provides some measure of reassurance with regard to current postoperative CABG glucose management by showing that the limitations of the blood glucose meter do not jeopardize the safety of patients. Nonetheless, we look forward to advances in the accuracy of POCT blood glucose technology so that critical care patients can be better managed when blood glucose is outside the prescribed range.
This analysis of 116 CABG patients points out both the inaccuracy and the utility of a representative POCT glucometer (in this case, the FreeStyle Precision Pro) used at the bedside to manage CIIs in postoperative CABG patients, keeping the blood glucose level in the moderate control range (110-150 mg/dL). The correlation plot shows that in this population the bedside nurses were able to keep blood glucose in range most of the time, in spite of the inaccuracy of POCT of blood glucose, given that the error of the test fits in the wide margin of 40 mg/dL. The fact that the 6-hour values were slightly less variable than the admission values indicates that sequential determinations of blood glucose over the 6-hour period to detect trends allowed good clinical management even in the face of such inaccuracy. The correlation allows the inaccurate number (blood glucose value) to indicate direction, and frequent determinations allow the bedside nurse to keep that number in the prescribed range most of the time in this population of patients.
Conclusion
We have found that glucometer blood glucose determinations in our center used on a homogenous population (CABG surgery) utilizing a single type of glucometer correlated well with those of the central lab, but were not always accurate. In spite of the inaccuracies, experienced bedside nurses were able to use the instrument successfully and safely, as it informed them if the blood glucose was in or out of a predetermined range and in which direction it was going.
Acknowledgment: The authors are indebted to the nurses of the Cardiothoracic Surgery Intensive Care Unit at Maine Medical Center for their support and assistance, without which this analysis would not have been possible.
Corresponding author: Robert S. Kramer, MD, Division of Cardiothoracic Surgery, Maine Medical Center Cardiovascular Institute, 22 Bramhall St., Portland ME 04102; kramer@mmc.org.
Financial disclosures: None.
1. Furnary AP, Gao G, Grunkemeier GL, et al. Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003;125:1007-1021.
2. Lazar H. Glycemic control during coronary artery bypass graft surgery. ISRN Cardiol. 2012;2012:292490.
3. Lazar HL, McDonnell M, Chipkin SR, et al; Society of Thoracic Surgeons Blood Glucose Guideline Task Force. The Society of Thoracic Surgeons Practice Guideline Series: blood glucose management during adult cardiac surgery. Ann Thorac Surg. 2009;87:663-669.
4. US Food and Drug Administration. Blood Glucose Monitoring Test Systems for Prescription Point of Care Use. Guidance for Industry and Food and Drug Administration Staff,.www.fda.gov/downloads/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/UCM380325.pdf. Accessed March 8, 2019.
5. Finkielman JD, Oyen LJ, Afess B. Agreement between bedside blood and plasma glucose measurement in the ICU Setting. Chest. 2005;127:1749-1511.
6. Pidcoke HF, Wade CE, Mann EA, et al. Anemia causes hypoglycemia in ICU patients due to error in single-channel glucometers: methods of reducing patient risk. Crit Care Med. 2010;38:471-476.
7. Kramer R, Groom R, Weldner D, et al. Glycemic control reduces deep sternal wound infection: a multidisciplinary approach. Arch Surg. 2008;143:451-456.
8. Peterson JR, Graves DF, Tacker DH, et al. Comparison of POCT and central laboratory blood glucose results using arterial, capillary, and venous samples from MICU patients on a tight glycemic protocol. Clinica Chimica Acta. 2008;396:10-13.
9. Cook A, Laughlin D, Moore M, et al. Differences in glucose values obtained from point-of-care glucose meters and laboratory analysis in critically ill patients. Am J Crit Care. 2009;18:65-72.
1. Furnary AP, Gao G, Grunkemeier GL, et al. Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003;125:1007-1021.
2. Lazar H. Glycemic control during coronary artery bypass graft surgery. ISRN Cardiol. 2012;2012:292490.
3. Lazar HL, McDonnell M, Chipkin SR, et al; Society of Thoracic Surgeons Blood Glucose Guideline Task Force. The Society of Thoracic Surgeons Practice Guideline Series: blood glucose management during adult cardiac surgery. Ann Thorac Surg. 2009;87:663-669.
4. US Food and Drug Administration. Blood Glucose Monitoring Test Systems for Prescription Point of Care Use. Guidance for Industry and Food and Drug Administration Staff,.www.fda.gov/downloads/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/UCM380325.pdf. Accessed March 8, 2019.
5. Finkielman JD, Oyen LJ, Afess B. Agreement between bedside blood and plasma glucose measurement in the ICU Setting. Chest. 2005;127:1749-1511.
6. Pidcoke HF, Wade CE, Mann EA, et al. Anemia causes hypoglycemia in ICU patients due to error in single-channel glucometers: methods of reducing patient risk. Crit Care Med. 2010;38:471-476.
7. Kramer R, Groom R, Weldner D, et al. Glycemic control reduces deep sternal wound infection: a multidisciplinary approach. Arch Surg. 2008;143:451-456.
8. Peterson JR, Graves DF, Tacker DH, et al. Comparison of POCT and central laboratory blood glucose results using arterial, capillary, and venous samples from MICU patients on a tight glycemic protocol. Clinica Chimica Acta. 2008;396:10-13.
9. Cook A, Laughlin D, Moore M, et al. Differences in glucose values obtained from point-of-care glucose meters and laboratory analysis in critically ill patients. Am J Crit Care. 2009;18:65-72.