User login
Division of Infectious Diseases, Department of Internal Medicine, VA Ann Arbor Healthcare System and University of Michigan Health System, Ann Arbor, MI.
Abstract
- Objective: To review prevention of central line–associated bloodstream infection (CLABSI).
- Method: Review of the literature.
- Results: Evidence-based prevention practices include ensuring hand hygiene before the procedure, using maximal sterile barrier precautions, cleaning the skin with alcoholic chlorhexidine before central line insertion, avoiding the femoral site for insertion, and removing unneeded catheters.
- Conclusion: For continued success in CLABSI prevention, best practices should be followed and patient safety should be emphasized.
Health care–associated infections (HAIs) are a preventable cause of morbidity and mortality in the United States and internationally. A Centers for Disease Control and Prevention (CDC) report estimates that in acute care hospitals, 1 in 25 patients end up with at least one HAI during their hospital stay [1]. HAIs can also be costly; in the United States, the indirect and direct cost has been estimated to be between $96 to $147 billion dollars [2]. National initiatives to prevent these types of infections have included efforts from the Department of Health and Human Services (HHS), the Institute of Medicine (IOM), the Institute for Healthcare Improvement (IHI) and the Centers for Medicare and Medicaid Services (CMS). This work has led to particular success in preventing central line–associated bloodstream infection (CLABSI).
CLABSI can lead to considerable mortality, morbidity, and cost. An estimated 250,000 CLABSIs occur in patients yearly, and about 80,000 of those are estimated to occur in the intensive care unit (ICU) setting [3]. Since central venous catheters (CVCs), or central lines, are most often used in the ICU setting, much of the work on prevention and management of CLABSI has been within the ICU population [4,5]. The increased use of peripherally inserted central catheters (PICCs) in the non-ICU setting and recognition of CLABSI in non-ICU settings has led to new efforts to understand the best way to prevent CLABSI in the non-ICU setting [4,6]. Regardless of setting, the annual cost of these infections has been estimated to be as high as $2.3 billion [7]. One episode is estimated to cost a hospital up to $46,485 per episode with components of excess length of stay, antibiotic cost, and cost of care [8]. In this review, selected best practices in CLABSI prevention are identified and described.
Elements of CLABSI Prevention
One of the key papers in the CLABSI literature was the Keystone ICU project in Michigan [9]. This state-wide effort grew out of a successful pilot patient-safety program that was trialed at Johns Hopkins Medical Institutions to reduce CLABSI in the ICU setting. In 2003, the Agency for Healthcare Research and Quality (AHRQ) funded a study to examine the intervention in ICUs in the state of Michigan. A total of 108 ICUs from 67 individual hospitals participated in the pre-intervention/post-intervention study [9]. A combination of technical and socio-adaptive interventions to prevent CLABSI included clinician education on best practices in insertion of central lines, having a central-line cart in each ICU, an insertion checklist of best practices, empowering nursing staff to stop the procedure if best practices were not being followed, discussing removal of catheters daily, and providing feedback to units regarding rates of CLABSI [10]. Executive administration of each hospital was also involved and there were monthly phone calls for hospital teams to share successes and barriers.
In the pre-intervention phase, the median catheter- related bloodstream infection rate was 2.7 infections per 1000 catheter days for the sum of hospitals. After the interventions were put in place, the median rate of catheter related bloodstream infections was down to 0.34 at 18 months. The study showed that results from a relatively inexpensive and straightforward intervention could be effective and could last in the long term. This study led to many other single center and multicenter studies, nationally and internationally, to replicate results in efforts to decrease CLABSI in ICU populations [5]. The CDC and AHRQ have continued to partner with regional, state and national efforts to focus on CLABSI prevention.
The Bundle Approach
A number of interventions have been proven to be effective at preventing CLABSI. Combining more than one intervention can often have additive effects. This effect has been recognized in numerous quality improvement studies on CLABSI and has been termed using the “bundle” approach.
Hand Hygiene
Poor hand hygiene by health care workers is generally thought to be the most common cause of HAIs [12]. Guidelines recommend an alcohol-based waterless product or antiseptic soap and water prior to catheter insertion [13]. The most common underlying etiology of CLABSI is through microorganisms introduced at time of insertion of catheter. This can be extraluminally mediated via skin flora of the patient, or due to lack of hand washing on the inserter’s part and can lead to CLABSI [14]. While a randomized controlled trial would be unethical, several studies have shown when targeted hand hygiene campaigns are held, CLABSI rates tend to decrease [15–17].
Maximal Barrier Precautions
The use of maximal sterile barrier precautions has been associated with less mortality, decreasing catheter colonization, incidence of HAI and cost savings [18–20]. Like most components of the bundle, maximal sterile barrier precautions have rarely been studied alone, but are often a part of a “bundle” or number of interventions [21]. Like hand hygiene, while regularly a part of many hospital’s checklist or bundle process, compliance with this key part of infection prevention can be deficient; one study noted measured maximal sterile barriers compliance to be 44% [22].
Chlorhexidine Skin Antisepsis
Chlorhexidine skin preparation decreases bacterial burden at site of insertion and is thought to reduce infection from this mechanism. Chlorhexidine-alcohol skin preparation has been proven in randomized controlled trials to outperform povidone iodine-alcohol in preventing CLABSI [23,24]. Chlorhexidine skin preparation is considered a technical element of checklists and is thought to be a straightforward and easily implementable action [25]. If a hospital supplies only alcoholic chlorhexidine and doesn’t provide povidone-iodine for skin preparation, then clinicians can be “nudged” towards performing this part of the bundle.
Optimal Catheter Site Selection
For all sites of insertion of CVC, the risk of mechanical and infectious complications depends on the skill and proficiency of operators, the clinical situation, and the availability of ultrasound to help guide placement. These factors are important in determining which anatomical site is best for each patient [26]. The femoral site has been associated with a greater risk of catheter-related infection and catheter-related thrombosis and is not recommended as the initial choice for non-emergent CVC insertion according to national guidelines [13,27]. The internal jugular vein site is associated with a lower risk of severe mechanical complications such as pneumothorax when compared to subclavian vein site [27]. The subclavian vein site is associated with a lower risk of catheter-related blood stream infection and lower rate of thrombosis, but this greatly depends on experience of operator. Experts have proposed that the subclavian site has a lower burden of colonization by bacteria than other sites and is anatomically more protected by catheter dressing; also the subcutaneous course of the central line itself is longer for the subclavian site than other sites and these reasons could contribute to the lower risk of infection [28]. The subclavian site is, however, associated with a higher risk of mechanical complications that can be serious for ICU patients. In general, the femoral vein site should be avoided in non-emergent line placement situations, particularly if the patient is an obese adult [13]. Using ultrasound as a guidance for catheter insertion has also been shown to reduce risk of CLABSI and other mechanical complications and is recommended [29,30].
Daily Review of Line Necessity
Removing unnecessary catheters as soon as possible decreases catheter dwell time and risk of infection. Few studies have concentrated on this step alone in CLABSI prevention, but the studies that have focused on catheter removal usually implement electronic reminders or multidisciplinary catheter rounds (where need for catheter is incorporated into daily rounds or discussed separately by a multidisciplinary group) [5,31].
Additional Considerations
Other basic practices that all hospitals should adopt include the above strategies and providing all inclusive catheter carts or kits, disinfecting hubs in maintenance care of catheters, covering the CVC site with sterile dressings, having recurrent educational interventions and using checklists to assure adherence to the evidence-based bundle (Table) [4,13]. As prevalence of non-ICU central lines has also grown, maintenance care is particularly important in reducing CLABSI. Maintenance bundles that highlight best practices such as aseptic technique, correct hand hygiene, chlorhexidine skin disinfection scrub, antimicrobial bandage application, and catheter hub disinfection have been used with success [32]. Specialized CVC insertion teams with trained personnel have also been recommended [4]. When these basic evidence-based practices are still unable to bring down CLABSI rates for select populations or during an outbreak, supplemental strategies can be tried to reduce CLABSI. These include antimicrobial-impregnated catheters, chlorhexidine-impregnated dressings, and chlorhexidine bathing, which is increasingly being used in the ICU setting [5,13,33].
Epidemiology/Risk Factors
At-risk Populations
ICU patients are at risk for CLABSI because of frequent use of multiple catheters, and the comorbidities and acuity of care that these patients have. ICU patients also tend to have lots of manipulation of their catheters and often these catheters are placed in emergent situations [13]. Patients in the non-ICU and outpatient setting are also at risk for CLABSI when they have a central venous catheter. Long courses of antibiotics for disease states such as osteomyelitis and endocarditis often entail central venous catheters. Recent work has shown that PICCs carry as high of a CLABSI risk as short-term CVCs in hospitalized patients [34]. Patients with end-stage renal disease, especially those undergoing maintenance hemodialysis via a tunneled dialysis catheter are particularly vulnerable to CLABSI [13,35].
Risk Factors for CLABSI
A number of studies have reviewed risk factors and epidemiology of CLABSI in the adult and pediatric population. Factors that have been associated with risk of CLABSI in more than one study include prolonged hospitalization before placement of the central line, prolonged duration of the central line, heavy microbial colonization at the site of insertion, heavy microbial colonization of the catheter hub, multiple lumens, internal jugular site catheterization, femoral vein site catheterization, neutropenia of the patient, a reduced nurse to patient ratio in the ICU setting, presence of total parenteral nutrition, and poor maintenance care of the catheter [4,13,36–40]. One study [41] that calculated a score to help predict risk of PICC-CLABSI found that previous CLABSI (within 3 months of PICC insertion) significantly increases risk of repeat CLABSI.
Conclusion
CLABSI is an important cause of morbidity, mortality and cost. There has been remarkable success in prevention of these infections in recent years due to focused efforts on patient safety. As efforts have multiplied to put into place interventions to decrease CLABSI nationally, the CDC published a Vital Signs report discussing the impact of these efforts [42]. It was estimated that over one decade, infection prevention efforts had avoided 25,000 CLABSIs in U.S. ICUs, a 58% reduction in this infection [42]. CLABSI has served as the best example of using evidence-based interventions through an infection prevention bundle or framework to reduce HAIs. Similar approaches are being used to try to reduce catheter-associated urinary tract infection, Clostridium difficile infection, surgical site infection, and ventilator-associated pneumonia, but there have been less distinct successes nationally and internationally for these other HAIs.
The literature emphasizes that there are several evidence-based measures that can prevent CLABSI. These include hand hygiene, using alcoholic chlorhexidine for skin preparation prior to insertion, maximal sterile barrier precautions, avoiding the femoral site for CVC insertion, and removing unnecessary catheters as soon as possible. Support from administration in emphasizing patient safety and HAI prevention along with following evidence-based practice could lead to long-term improvement in CLABSI prevention across hospital systems.
Corresponding author: Payal K. Patel, MD, MPH, Div of Infectious Diseases, Dept of Internal Medicine, VA Ann Arbor Healthcare System, 2215 Fuller Rd, Ann Arbor, MI 48105, payalkp@umich.edu.
Financial disclosures: None.
1. Magill SS, Edwards JR, Bamberg W, et al; Emerging Infections Program Healthcare-Associated Infections and Antimicrobial Use Prevalence Survey Team. Multistate point-prevalence survey of health care-associated infections. N Engl J Med 2014;370:1198–208.
2. Marchetti A, Rossiter R. Economic burden of healthcare-associated infection in US acute care hospitals: societal perspective. J Med Econ 2013;16:1399–404.
3. O’Neil C, Ball K, Wood H, et al. A central line care maintenance bundle for the prevention of central line-associated bloodstream infection in non-intensive care unit settings. Infect Control Hosp Epidemiol 2016;37:1–7.
4. Shekelle PG, Wachter RM, Pronovost PJ, et al. Making health care safer II: an updated critical analysis of the evidence for patient safety practices. Evid Rep Technol Assess (Full Rep) 2013:1–945.
5. Patel PK, Gupta A, Vaughn VM, Mann JD, Ameling JM, Meddings J. Review of strategies to reduce central line-associated bloodstream infection (CLABSI) and catheter-associated urinary tract infection (CAUTI) in adult ICUs. J Hosp Med 2018;13:105–16.
6. Chopra V, Ratz D, Kuhn L, et al. PICC-associated bloodstream infections: prevalence, patterns, and predictors. Am J Med 2014;127:319–28.
7. Sagana R, Hyzy RC. Achieving zero central line-associated bloodstream infection rates in your intensive care unit. Crit Care Clin 2013;29:1–9.
8. Nelson RE, Angelovic AW, Nelson SD, Gleed JR, Drews FA. An economic analysis of adherence engineering to improve use of best practices during central line maintenance procedures. Infect Control Hosp Epidemiol 2015;36:550–6.
9. Pronovost P, Needham D, Berenholtz S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med 2006;355:2725–32.
10. Dumyati G, Concannon C, van Wijngaarden E, et al. Sustained reduction of central line-associated bloodstream infections outside the intensive care unit with a multimodal intervention focusing on central line maintenance. Am J Infect Control 2014;42:723–30.
11. Sacks GD, Diggs BS, Hadjizacharia P, et al. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement Central Line Bundle. Am J Surg 2014;207:817–23.
12. Boyce JM, Pittet D; Healthcare Infection Control Practices Advisory Committee; HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Guideline for hand hygiene in health-care settings: recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Society for Healthcare Epidemiology of America/Association for Professionals in Infection Control/Infectious Diseases Society of America. MMWR Recomm Rep 2002; 51:1-45, quiz CE1–4.
13. Marschall J, Mermel LA, et al; Society for Healthcare Epidemiology of America. Strategies to prevent central line-associated bloodstream infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol 2014;35:753–71.
14. Safdar N, Maki DG. The pathogenesis of catheter-related bloodstream infection with noncuffed short-term central venous catheters. Intensive Care Med 2004;30:62–7.
15. Shabot MM, Chassin MR, France AC, et al. Using the targeted solutions tool(R) to improve hand hygiene compliance is associated with decreased health care-associated infections. Jt Comm J Qual Patient Saf 2016;42:6–17.
16. Johnson L, Grueber S, Schlotzhauer C, et al. A multifactorial action plan improves hand hygiene adherence and significantly reduces central line-associated bloodstream infections. Am J Infect Control 2014;42:1146–51.
17. Barrera L, Zingg W, Mendez F, Pittet D. Effectiveness of a hand hygiene promotion strategy using alcohol-based handrub in 6 intensive care units in Colombia. Am J Infect Control 2011;39:633–9.
18. Hu KK, Lipsky BA, Veenstra DL, Saint S. Using maximal sterile barriers to prevent central venous catheter-related infection: a systematic evidence-based review. Am J Infect Control 2004;32:142–6.
19. Hu KK, Veenstra DL, Lipsky BA, Saint S. Use of maximal sterile barriers during central venous catheter insertion: clinical and economic outcomes. Clin Infect Dis 2004;39:1441–5.
20. Raad II, Hohn DC, Gilbreath BJ, et al. Prevention of central venous catheter-related infections by using maximal sterile barrier precautions during insertion. Infect Control Hosp Epidemiol 1994;15:231–8.
21. Furuya EY, Dick AW, Herzig CT, Pogorzelska-Maziarz M, Larson EL, Stone PW. Central line-associated bloodstream infection reduction and bundle compliance in intensive care units: a national study. Infect Control Hosp Epidemiol 2016;37:805–10.
22. Sherertz RJ, Ely EW, Westbrook DM, et al. Education of physicians-in-training can decrease the risk for vascular catheter infection. Ann Intern Med 2000;132:641–8.
23. Mimoz O, Lucet JC, Kerforne T, Pascal J, et al. Skin antisepsis with chlorhexidine-alcohol versus povidone iodine-alcohol, with and without skin scrubbing, for prevention of intravascular-catheter-related infection (CLEAN): an open-label, multicentre, randomised, controlled, two-by-two factorial trial. Lancet 2015;386:2069–77.
24. Lai NM, Lai NA, O’Riordan E, et al. Skin antisepsis for reducing central venous catheter-related infections. Cochrane Database Syst Rev 2016;7:CD010140.
25. Chopra V, Shojania KG. Recipes for checklists and bundles: one part active ingredient, two parts measurement. BMJ Qual Saf 2013;22:93–6.
26. Marik PE, Flemmer M, Harrison W. The risk of catheter-related bloodstream infection with femoral venous catheters as compared to subclavian and internal jugular venous catheters: a systematic review of the literature and meta-analysis. Crit Care Med 2012;40:2479–85.
27. Timsit JF. What is the best site for central venous catheter insertion in critically ill patients? Crit Care 2003;7:397–99.
28. Parienti JJ, Mongardon N, Megarbane B, et al; 3SITES Study Group. Intravascular complications of central venous catheterization by insertion site. N Engl J Med 2015;373:1220–9.
29. Hind D, Calvert N, McWilliams R, et al. Ultrasonic locating devices for central venous cannulation: meta-analysis. BMJ 2003;327:361.
30. Fragou M, Gravvanis A, Dimitriou V, et al. Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: a prospective randomized study. Crit Care Med 2011;39:1607–12.
31. Pageler NM, Longhurst CA, Wood M, et al. Use of electronic medical record-enhanced checklist and electronic dashboard to decrease CLABSIs. Pediatrics 2014;133:e738–46.
32. Drews FA, Bakdash JZ, Gleed JR. Improving central line maintenance to reduce central line-associated bloodstream infections. Am J Infect Control 2017;45:1224–30.
33. Frost SA, Alogso MC, Metcalfe L, et al. Chlorhexidine bathing and health care-associated infections among adult intensive care patients: a systematic review and meta-analysis. Crit Care 2016;20:379.
34. Chopra V, O’Horo JC, Rogers MA, et al. The risk of bloodstream infection associated with peripherally inserted central catheters compared with central venous catheters in adults: a systematic review and meta-analysis. Infect Control Hosp Epidemiol 2013;34:908–18.
35. Xue H, Ix JH, Wang W, et al. Hemodialysis access usage patterns in the incident dialysis year and associated catheter-related complications. Am J Kidney Dis 2013;61:123–30.
36. Almuneef MA, Memish ZA, Balkhy HH, et al. Rate, risk factors and outcomes of catheter-related bloodstream infection in a paediatric intensive care unit in Saudi Arabia. J Hosp Infect 2006;62:207–13.
37. Alonso-Echanove J, Edwards JR, Richards MJ, et al. Effect of nurse staffing and antimicrobial-impregnated central venous catheters on the risk for bloodstream infections in intensive care units. Infect Control Hosp Epidemiol 2003;24:916–25.
38. Lorente L, Henry C, Martin MM, et al. Central venous catheter-related infection in a prospective and observational study of 2,595 catheters. Crit Care 2005;9:R631–5.
39. Rey C, Alvarez F, De-La-Rua V, et al. Intervention to reduce catheter-related bloodstream infections in a pediatric intensive care unit. Intensive Care Med 2011;37:678–85.
40. O’Brien J, Paquet F, Lindsay R, Valenti D. Insertion of PICCs with minimum number of lumens reduces complications and costs. J Am Coll Radiol. 2013;10:864–8.
41. Herc E, Patel P, Washer LL, et al. A model to predict central-line-associated bloodstream infection among patients with peripherally inserted central catheters: the MPC score. Infect Control Hosp Epidemiol 2017;38:1155–66.
42. Centers for Disease Control and Prevention. Vital signs: central line-associated blood stream infections--United States, 2001, 2008, and 2009. MMWR Morb Mortal Wkly Rep 2011;60:243–8.
Division of Infectious Diseases, Department of Internal Medicine, VA Ann Arbor Healthcare System and University of Michigan Health System, Ann Arbor, MI.
Abstract
- Objective: To review prevention of central line–associated bloodstream infection (CLABSI).
- Method: Review of the literature.
- Results: Evidence-based prevention practices include ensuring hand hygiene before the procedure, using maximal sterile barrier precautions, cleaning the skin with alcoholic chlorhexidine before central line insertion, avoiding the femoral site for insertion, and removing unneeded catheters.
- Conclusion: For continued success in CLABSI prevention, best practices should be followed and patient safety should be emphasized.
Health care–associated infections (HAIs) are a preventable cause of morbidity and mortality in the United States and internationally. A Centers for Disease Control and Prevention (CDC) report estimates that in acute care hospitals, 1 in 25 patients end up with at least one HAI during their hospital stay [1]. HAIs can also be costly; in the United States, the indirect and direct cost has been estimated to be between $96 to $147 billion dollars [2]. National initiatives to prevent these types of infections have included efforts from the Department of Health and Human Services (HHS), the Institute of Medicine (IOM), the Institute for Healthcare Improvement (IHI) and the Centers for Medicare and Medicaid Services (CMS). This work has led to particular success in preventing central line–associated bloodstream infection (CLABSI).
CLABSI can lead to considerable mortality, morbidity, and cost. An estimated 250,000 CLABSIs occur in patients yearly, and about 80,000 of those are estimated to occur in the intensive care unit (ICU) setting [3]. Since central venous catheters (CVCs), or central lines, are most often used in the ICU setting, much of the work on prevention and management of CLABSI has been within the ICU population [4,5]. The increased use of peripherally inserted central catheters (PICCs) in the non-ICU setting and recognition of CLABSI in non-ICU settings has led to new efforts to understand the best way to prevent CLABSI in the non-ICU setting [4,6]. Regardless of setting, the annual cost of these infections has been estimated to be as high as $2.3 billion [7]. One episode is estimated to cost a hospital up to $46,485 per episode with components of excess length of stay, antibiotic cost, and cost of care [8]. In this review, selected best practices in CLABSI prevention are identified and described.
Elements of CLABSI Prevention
One of the key papers in the CLABSI literature was the Keystone ICU project in Michigan [9]. This state-wide effort grew out of a successful pilot patient-safety program that was trialed at Johns Hopkins Medical Institutions to reduce CLABSI in the ICU setting. In 2003, the Agency for Healthcare Research and Quality (AHRQ) funded a study to examine the intervention in ICUs in the state of Michigan. A total of 108 ICUs from 67 individual hospitals participated in the pre-intervention/post-intervention study [9]. A combination of technical and socio-adaptive interventions to prevent CLABSI included clinician education on best practices in insertion of central lines, having a central-line cart in each ICU, an insertion checklist of best practices, empowering nursing staff to stop the procedure if best practices were not being followed, discussing removal of catheters daily, and providing feedback to units regarding rates of CLABSI [10]. Executive administration of each hospital was also involved and there were monthly phone calls for hospital teams to share successes and barriers.
In the pre-intervention phase, the median catheter- related bloodstream infection rate was 2.7 infections per 1000 catheter days for the sum of hospitals. After the interventions were put in place, the median rate of catheter related bloodstream infections was down to 0.34 at 18 months. The study showed that results from a relatively inexpensive and straightforward intervention could be effective and could last in the long term. This study led to many other single center and multicenter studies, nationally and internationally, to replicate results in efforts to decrease CLABSI in ICU populations [5]. The CDC and AHRQ have continued to partner with regional, state and national efforts to focus on CLABSI prevention.
The Bundle Approach
A number of interventions have been proven to be effective at preventing CLABSI. Combining more than one intervention can often have additive effects. This effect has been recognized in numerous quality improvement studies on CLABSI and has been termed using the “bundle” approach.
Hand Hygiene
Poor hand hygiene by health care workers is generally thought to be the most common cause of HAIs [12]. Guidelines recommend an alcohol-based waterless product or antiseptic soap and water prior to catheter insertion [13]. The most common underlying etiology of CLABSI is through microorganisms introduced at time of insertion of catheter. This can be extraluminally mediated via skin flora of the patient, or due to lack of hand washing on the inserter’s part and can lead to CLABSI [14]. While a randomized controlled trial would be unethical, several studies have shown when targeted hand hygiene campaigns are held, CLABSI rates tend to decrease [15–17].
Maximal Barrier Precautions
The use of maximal sterile barrier precautions has been associated with less mortality, decreasing catheter colonization, incidence of HAI and cost savings [18–20]. Like most components of the bundle, maximal sterile barrier precautions have rarely been studied alone, but are often a part of a “bundle” or number of interventions [21]. Like hand hygiene, while regularly a part of many hospital’s checklist or bundle process, compliance with this key part of infection prevention can be deficient; one study noted measured maximal sterile barriers compliance to be 44% [22].
Chlorhexidine Skin Antisepsis
Chlorhexidine skin preparation decreases bacterial burden at site of insertion and is thought to reduce infection from this mechanism. Chlorhexidine-alcohol skin preparation has been proven in randomized controlled trials to outperform povidone iodine-alcohol in preventing CLABSI [23,24]. Chlorhexidine skin preparation is considered a technical element of checklists and is thought to be a straightforward and easily implementable action [25]. If a hospital supplies only alcoholic chlorhexidine and doesn’t provide povidone-iodine for skin preparation, then clinicians can be “nudged” towards performing this part of the bundle.
Optimal Catheter Site Selection
For all sites of insertion of CVC, the risk of mechanical and infectious complications depends on the skill and proficiency of operators, the clinical situation, and the availability of ultrasound to help guide placement. These factors are important in determining which anatomical site is best for each patient [26]. The femoral site has been associated with a greater risk of catheter-related infection and catheter-related thrombosis and is not recommended as the initial choice for non-emergent CVC insertion according to national guidelines [13,27]. The internal jugular vein site is associated with a lower risk of severe mechanical complications such as pneumothorax when compared to subclavian vein site [27]. The subclavian vein site is associated with a lower risk of catheter-related blood stream infection and lower rate of thrombosis, but this greatly depends on experience of operator. Experts have proposed that the subclavian site has a lower burden of colonization by bacteria than other sites and is anatomically more protected by catheter dressing; also the subcutaneous course of the central line itself is longer for the subclavian site than other sites and these reasons could contribute to the lower risk of infection [28]. The subclavian site is, however, associated with a higher risk of mechanical complications that can be serious for ICU patients. In general, the femoral vein site should be avoided in non-emergent line placement situations, particularly if the patient is an obese adult [13]. Using ultrasound as a guidance for catheter insertion has also been shown to reduce risk of CLABSI and other mechanical complications and is recommended [29,30].
Daily Review of Line Necessity
Removing unnecessary catheters as soon as possible decreases catheter dwell time and risk of infection. Few studies have concentrated on this step alone in CLABSI prevention, but the studies that have focused on catheter removal usually implement electronic reminders or multidisciplinary catheter rounds (where need for catheter is incorporated into daily rounds or discussed separately by a multidisciplinary group) [5,31].
Additional Considerations
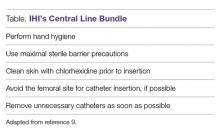
Other basic practices that all hospitals should adopt include the above strategies and providing all inclusive catheter carts or kits, disinfecting hubs in maintenance care of catheters, covering the CVC site with sterile dressings, having recurrent educational interventions and using checklists to assure adherence to the evidence-based bundle (Table) [4,13]. As prevalence of non-ICU central lines has also grown, maintenance care is particularly important in reducing CLABSI. Maintenance bundles that highlight best practices such as aseptic technique, correct hand hygiene, chlorhexidine skin disinfection scrub, antimicrobial bandage application, and catheter hub disinfection have been used with success [32]. Specialized CVC insertion teams with trained personnel have also been recommended [4]. When these basic evidence-based practices are still unable to bring down CLABSI rates for select populations or during an outbreak, supplemental strategies can be tried to reduce CLABSI. These include antimicrobial-impregnated catheters, chlorhexidine-impregnated dressings, and chlorhexidine bathing, which is increasingly being used in the ICU setting [5,13,33].
Epidemiology/Risk Factors
At-risk Populations
ICU patients are at risk for CLABSI because of frequent use of multiple catheters, and the comorbidities and acuity of care that these patients have. ICU patients also tend to have lots of manipulation of their catheters and often these catheters are placed in emergent situations [13]. Patients in the non-ICU and outpatient setting are also at risk for CLABSI when they have a central venous catheter. Long courses of antibiotics for disease states such as osteomyelitis and endocarditis often entail central venous catheters. Recent work has shown that PICCs carry as high of a CLABSI risk as short-term CVCs in hospitalized patients [34]. Patients with end-stage renal disease, especially those undergoing maintenance hemodialysis via a tunneled dialysis catheter are particularly vulnerable to CLABSI [13,35].
Risk Factors for CLABSI
A number of studies have reviewed risk factors and epidemiology of CLABSI in the adult and pediatric population. Factors that have been associated with risk of CLABSI in more than one study include prolonged hospitalization before placement of the central line, prolonged duration of the central line, heavy microbial colonization at the site of insertion, heavy microbial colonization of the catheter hub, multiple lumens, internal jugular site catheterization, femoral vein site catheterization, neutropenia of the patient, a reduced nurse to patient ratio in the ICU setting, presence of total parenteral nutrition, and poor maintenance care of the catheter [4,13,36–40]. One study [41] that calculated a score to help predict risk of PICC-CLABSI found that previous CLABSI (within 3 months of PICC insertion) significantly increases risk of repeat CLABSI.
Conclusion
CLABSI is an important cause of morbidity, mortality and cost. There has been remarkable success in prevention of these infections in recent years due to focused efforts on patient safety. As efforts have multiplied to put into place interventions to decrease CLABSI nationally, the CDC published a Vital Signs report discussing the impact of these efforts [42]. It was estimated that over one decade, infection prevention efforts had avoided 25,000 CLABSIs in U.S. ICUs, a 58% reduction in this infection [42]. CLABSI has served as the best example of using evidence-based interventions through an infection prevention bundle or framework to reduce HAIs. Similar approaches are being used to try to reduce catheter-associated urinary tract infection, Clostridium difficile infection, surgical site infection, and ventilator-associated pneumonia, but there have been less distinct successes nationally and internationally for these other HAIs.
The literature emphasizes that there are several evidence-based measures that can prevent CLABSI. These include hand hygiene, using alcoholic chlorhexidine for skin preparation prior to insertion, maximal sterile barrier precautions, avoiding the femoral site for CVC insertion, and removing unnecessary catheters as soon as possible. Support from administration in emphasizing patient safety and HAI prevention along with following evidence-based practice could lead to long-term improvement in CLABSI prevention across hospital systems.
Corresponding author: Payal K. Patel, MD, MPH, Div of Infectious Diseases, Dept of Internal Medicine, VA Ann Arbor Healthcare System, 2215 Fuller Rd, Ann Arbor, MI 48105, payalkp@umich.edu.
Financial disclosures: None.
Division of Infectious Diseases, Department of Internal Medicine, VA Ann Arbor Healthcare System and University of Michigan Health System, Ann Arbor, MI.
Abstract
- Objective: To review prevention of central line–associated bloodstream infection (CLABSI).
- Method: Review of the literature.
- Results: Evidence-based prevention practices include ensuring hand hygiene before the procedure, using maximal sterile barrier precautions, cleaning the skin with alcoholic chlorhexidine before central line insertion, avoiding the femoral site for insertion, and removing unneeded catheters.
- Conclusion: For continued success in CLABSI prevention, best practices should be followed and patient safety should be emphasized.
Health care–associated infections (HAIs) are a preventable cause of morbidity and mortality in the United States and internationally. A Centers for Disease Control and Prevention (CDC) report estimates that in acute care hospitals, 1 in 25 patients end up with at least one HAI during their hospital stay [1]. HAIs can also be costly; in the United States, the indirect and direct cost has been estimated to be between $96 to $147 billion dollars [2]. National initiatives to prevent these types of infections have included efforts from the Department of Health and Human Services (HHS), the Institute of Medicine (IOM), the Institute for Healthcare Improvement (IHI) and the Centers for Medicare and Medicaid Services (CMS). This work has led to particular success in preventing central line–associated bloodstream infection (CLABSI).
CLABSI can lead to considerable mortality, morbidity, and cost. An estimated 250,000 CLABSIs occur in patients yearly, and about 80,000 of those are estimated to occur in the intensive care unit (ICU) setting [3]. Since central venous catheters (CVCs), or central lines, are most often used in the ICU setting, much of the work on prevention and management of CLABSI has been within the ICU population [4,5]. The increased use of peripherally inserted central catheters (PICCs) in the non-ICU setting and recognition of CLABSI in non-ICU settings has led to new efforts to understand the best way to prevent CLABSI in the non-ICU setting [4,6]. Regardless of setting, the annual cost of these infections has been estimated to be as high as $2.3 billion [7]. One episode is estimated to cost a hospital up to $46,485 per episode with components of excess length of stay, antibiotic cost, and cost of care [8]. In this review, selected best practices in CLABSI prevention are identified and described.
Elements of CLABSI Prevention
One of the key papers in the CLABSI literature was the Keystone ICU project in Michigan [9]. This state-wide effort grew out of a successful pilot patient-safety program that was trialed at Johns Hopkins Medical Institutions to reduce CLABSI in the ICU setting. In 2003, the Agency for Healthcare Research and Quality (AHRQ) funded a study to examine the intervention in ICUs in the state of Michigan. A total of 108 ICUs from 67 individual hospitals participated in the pre-intervention/post-intervention study [9]. A combination of technical and socio-adaptive interventions to prevent CLABSI included clinician education on best practices in insertion of central lines, having a central-line cart in each ICU, an insertion checklist of best practices, empowering nursing staff to stop the procedure if best practices were not being followed, discussing removal of catheters daily, and providing feedback to units regarding rates of CLABSI [10]. Executive administration of each hospital was also involved and there were monthly phone calls for hospital teams to share successes and barriers.
In the pre-intervention phase, the median catheter- related bloodstream infection rate was 2.7 infections per 1000 catheter days for the sum of hospitals. After the interventions were put in place, the median rate of catheter related bloodstream infections was down to 0.34 at 18 months. The study showed that results from a relatively inexpensive and straightforward intervention could be effective and could last in the long term. This study led to many other single center and multicenter studies, nationally and internationally, to replicate results in efforts to decrease CLABSI in ICU populations [5]. The CDC and AHRQ have continued to partner with regional, state and national efforts to focus on CLABSI prevention.
The Bundle Approach
A number of interventions have been proven to be effective at preventing CLABSI. Combining more than one intervention can often have additive effects. This effect has been recognized in numerous quality improvement studies on CLABSI and has been termed using the “bundle” approach.
Hand Hygiene
Poor hand hygiene by health care workers is generally thought to be the most common cause of HAIs [12]. Guidelines recommend an alcohol-based waterless product or antiseptic soap and water prior to catheter insertion [13]. The most common underlying etiology of CLABSI is through microorganisms introduced at time of insertion of catheter. This can be extraluminally mediated via skin flora of the patient, or due to lack of hand washing on the inserter’s part and can lead to CLABSI [14]. While a randomized controlled trial would be unethical, several studies have shown when targeted hand hygiene campaigns are held, CLABSI rates tend to decrease [15–17].
Maximal Barrier Precautions
The use of maximal sterile barrier precautions has been associated with less mortality, decreasing catheter colonization, incidence of HAI and cost savings [18–20]. Like most components of the bundle, maximal sterile barrier precautions have rarely been studied alone, but are often a part of a “bundle” or number of interventions [21]. Like hand hygiene, while regularly a part of many hospital’s checklist or bundle process, compliance with this key part of infection prevention can be deficient; one study noted measured maximal sterile barriers compliance to be 44% [22].
Chlorhexidine Skin Antisepsis
Chlorhexidine skin preparation decreases bacterial burden at site of insertion and is thought to reduce infection from this mechanism. Chlorhexidine-alcohol skin preparation has been proven in randomized controlled trials to outperform povidone iodine-alcohol in preventing CLABSI [23,24]. Chlorhexidine skin preparation is considered a technical element of checklists and is thought to be a straightforward and easily implementable action [25]. If a hospital supplies only alcoholic chlorhexidine and doesn’t provide povidone-iodine for skin preparation, then clinicians can be “nudged” towards performing this part of the bundle.
Optimal Catheter Site Selection
For all sites of insertion of CVC, the risk of mechanical and infectious complications depends on the skill and proficiency of operators, the clinical situation, and the availability of ultrasound to help guide placement. These factors are important in determining which anatomical site is best for each patient [26]. The femoral site has been associated with a greater risk of catheter-related infection and catheter-related thrombosis and is not recommended as the initial choice for non-emergent CVC insertion according to national guidelines [13,27]. The internal jugular vein site is associated with a lower risk of severe mechanical complications such as pneumothorax when compared to subclavian vein site [27]. The subclavian vein site is associated with a lower risk of catheter-related blood stream infection and lower rate of thrombosis, but this greatly depends on experience of operator. Experts have proposed that the subclavian site has a lower burden of colonization by bacteria than other sites and is anatomically more protected by catheter dressing; also the subcutaneous course of the central line itself is longer for the subclavian site than other sites and these reasons could contribute to the lower risk of infection [28]. The subclavian site is, however, associated with a higher risk of mechanical complications that can be serious for ICU patients. In general, the femoral vein site should be avoided in non-emergent line placement situations, particularly if the patient is an obese adult [13]. Using ultrasound as a guidance for catheter insertion has also been shown to reduce risk of CLABSI and other mechanical complications and is recommended [29,30].
Daily Review of Line Necessity
Removing unnecessary catheters as soon as possible decreases catheter dwell time and risk of infection. Few studies have concentrated on this step alone in CLABSI prevention, but the studies that have focused on catheter removal usually implement electronic reminders or multidisciplinary catheter rounds (where need for catheter is incorporated into daily rounds or discussed separately by a multidisciplinary group) [5,31].
Additional Considerations
Other basic practices that all hospitals should adopt include the above strategies and providing all inclusive catheter carts or kits, disinfecting hubs in maintenance care of catheters, covering the CVC site with sterile dressings, having recurrent educational interventions and using checklists to assure adherence to the evidence-based bundle (Table) [4,13]. As prevalence of non-ICU central lines has also grown, maintenance care is particularly important in reducing CLABSI. Maintenance bundles that highlight best practices such as aseptic technique, correct hand hygiene, chlorhexidine skin disinfection scrub, antimicrobial bandage application, and catheter hub disinfection have been used with success [32]. Specialized CVC insertion teams with trained personnel have also been recommended [4]. When these basic evidence-based practices are still unable to bring down CLABSI rates for select populations or during an outbreak, supplemental strategies can be tried to reduce CLABSI. These include antimicrobial-impregnated catheters, chlorhexidine-impregnated dressings, and chlorhexidine bathing, which is increasingly being used in the ICU setting [5,13,33].
Epidemiology/Risk Factors
At-risk Populations
ICU patients are at risk for CLABSI because of frequent use of multiple catheters, and the comorbidities and acuity of care that these patients have. ICU patients also tend to have lots of manipulation of their catheters and often these catheters are placed in emergent situations [13]. Patients in the non-ICU and outpatient setting are also at risk for CLABSI when they have a central venous catheter. Long courses of antibiotics for disease states such as osteomyelitis and endocarditis often entail central venous catheters. Recent work has shown that PICCs carry as high of a CLABSI risk as short-term CVCs in hospitalized patients [34]. Patients with end-stage renal disease, especially those undergoing maintenance hemodialysis via a tunneled dialysis catheter are particularly vulnerable to CLABSI [13,35].
Risk Factors for CLABSI
A number of studies have reviewed risk factors and epidemiology of CLABSI in the adult and pediatric population. Factors that have been associated with risk of CLABSI in more than one study include prolonged hospitalization before placement of the central line, prolonged duration of the central line, heavy microbial colonization at the site of insertion, heavy microbial colonization of the catheter hub, multiple lumens, internal jugular site catheterization, femoral vein site catheterization, neutropenia of the patient, a reduced nurse to patient ratio in the ICU setting, presence of total parenteral nutrition, and poor maintenance care of the catheter [4,13,36–40]. One study [41] that calculated a score to help predict risk of PICC-CLABSI found that previous CLABSI (within 3 months of PICC insertion) significantly increases risk of repeat CLABSI.
Conclusion
CLABSI is an important cause of morbidity, mortality and cost. There has been remarkable success in prevention of these infections in recent years due to focused efforts on patient safety. As efforts have multiplied to put into place interventions to decrease CLABSI nationally, the CDC published a Vital Signs report discussing the impact of these efforts [42]. It was estimated that over one decade, infection prevention efforts had avoided 25,000 CLABSIs in U.S. ICUs, a 58% reduction in this infection [42]. CLABSI has served as the best example of using evidence-based interventions through an infection prevention bundle or framework to reduce HAIs. Similar approaches are being used to try to reduce catheter-associated urinary tract infection, Clostridium difficile infection, surgical site infection, and ventilator-associated pneumonia, but there have been less distinct successes nationally and internationally for these other HAIs.
The literature emphasizes that there are several evidence-based measures that can prevent CLABSI. These include hand hygiene, using alcoholic chlorhexidine for skin preparation prior to insertion, maximal sterile barrier precautions, avoiding the femoral site for CVC insertion, and removing unnecessary catheters as soon as possible. Support from administration in emphasizing patient safety and HAI prevention along with following evidence-based practice could lead to long-term improvement in CLABSI prevention across hospital systems.
Corresponding author: Payal K. Patel, MD, MPH, Div of Infectious Diseases, Dept of Internal Medicine, VA Ann Arbor Healthcare System, 2215 Fuller Rd, Ann Arbor, MI 48105, payalkp@umich.edu.
Financial disclosures: None.
1. Magill SS, Edwards JR, Bamberg W, et al; Emerging Infections Program Healthcare-Associated Infections and Antimicrobial Use Prevalence Survey Team. Multistate point-prevalence survey of health care-associated infections. N Engl J Med 2014;370:1198–208.
2. Marchetti A, Rossiter R. Economic burden of healthcare-associated infection in US acute care hospitals: societal perspective. J Med Econ 2013;16:1399–404.
3. O’Neil C, Ball K, Wood H, et al. A central line care maintenance bundle for the prevention of central line-associated bloodstream infection in non-intensive care unit settings. Infect Control Hosp Epidemiol 2016;37:1–7.
4. Shekelle PG, Wachter RM, Pronovost PJ, et al. Making health care safer II: an updated critical analysis of the evidence for patient safety practices. Evid Rep Technol Assess (Full Rep) 2013:1–945.
5. Patel PK, Gupta A, Vaughn VM, Mann JD, Ameling JM, Meddings J. Review of strategies to reduce central line-associated bloodstream infection (CLABSI) and catheter-associated urinary tract infection (CAUTI) in adult ICUs. J Hosp Med 2018;13:105–16.
6. Chopra V, Ratz D, Kuhn L, et al. PICC-associated bloodstream infections: prevalence, patterns, and predictors. Am J Med 2014;127:319–28.
7. Sagana R, Hyzy RC. Achieving zero central line-associated bloodstream infection rates in your intensive care unit. Crit Care Clin 2013;29:1–9.
8. Nelson RE, Angelovic AW, Nelson SD, Gleed JR, Drews FA. An economic analysis of adherence engineering to improve use of best practices during central line maintenance procedures. Infect Control Hosp Epidemiol 2015;36:550–6.
9. Pronovost P, Needham D, Berenholtz S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med 2006;355:2725–32.
10. Dumyati G, Concannon C, van Wijngaarden E, et al. Sustained reduction of central line-associated bloodstream infections outside the intensive care unit with a multimodal intervention focusing on central line maintenance. Am J Infect Control 2014;42:723–30.
11. Sacks GD, Diggs BS, Hadjizacharia P, et al. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement Central Line Bundle. Am J Surg 2014;207:817–23.
12. Boyce JM, Pittet D; Healthcare Infection Control Practices Advisory Committee; HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Guideline for hand hygiene in health-care settings: recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Society for Healthcare Epidemiology of America/Association for Professionals in Infection Control/Infectious Diseases Society of America. MMWR Recomm Rep 2002; 51:1-45, quiz CE1–4.
13. Marschall J, Mermel LA, et al; Society for Healthcare Epidemiology of America. Strategies to prevent central line-associated bloodstream infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol 2014;35:753–71.
14. Safdar N, Maki DG. The pathogenesis of catheter-related bloodstream infection with noncuffed short-term central venous catheters. Intensive Care Med 2004;30:62–7.
15. Shabot MM, Chassin MR, France AC, et al. Using the targeted solutions tool(R) to improve hand hygiene compliance is associated with decreased health care-associated infections. Jt Comm J Qual Patient Saf 2016;42:6–17.
16. Johnson L, Grueber S, Schlotzhauer C, et al. A multifactorial action plan improves hand hygiene adherence and significantly reduces central line-associated bloodstream infections. Am J Infect Control 2014;42:1146–51.
17. Barrera L, Zingg W, Mendez F, Pittet D. Effectiveness of a hand hygiene promotion strategy using alcohol-based handrub in 6 intensive care units in Colombia. Am J Infect Control 2011;39:633–9.
18. Hu KK, Lipsky BA, Veenstra DL, Saint S. Using maximal sterile barriers to prevent central venous catheter-related infection: a systematic evidence-based review. Am J Infect Control 2004;32:142–6.
19. Hu KK, Veenstra DL, Lipsky BA, Saint S. Use of maximal sterile barriers during central venous catheter insertion: clinical and economic outcomes. Clin Infect Dis 2004;39:1441–5.
20. Raad II, Hohn DC, Gilbreath BJ, et al. Prevention of central venous catheter-related infections by using maximal sterile barrier precautions during insertion. Infect Control Hosp Epidemiol 1994;15:231–8.
21. Furuya EY, Dick AW, Herzig CT, Pogorzelska-Maziarz M, Larson EL, Stone PW. Central line-associated bloodstream infection reduction and bundle compliance in intensive care units: a national study. Infect Control Hosp Epidemiol 2016;37:805–10.
22. Sherertz RJ, Ely EW, Westbrook DM, et al. Education of physicians-in-training can decrease the risk for vascular catheter infection. Ann Intern Med 2000;132:641–8.
23. Mimoz O, Lucet JC, Kerforne T, Pascal J, et al. Skin antisepsis with chlorhexidine-alcohol versus povidone iodine-alcohol, with and without skin scrubbing, for prevention of intravascular-catheter-related infection (CLEAN): an open-label, multicentre, randomised, controlled, two-by-two factorial trial. Lancet 2015;386:2069–77.
24. Lai NM, Lai NA, O’Riordan E, et al. Skin antisepsis for reducing central venous catheter-related infections. Cochrane Database Syst Rev 2016;7:CD010140.
25. Chopra V, Shojania KG. Recipes for checklists and bundles: one part active ingredient, two parts measurement. BMJ Qual Saf 2013;22:93–6.
26. Marik PE, Flemmer M, Harrison W. The risk of catheter-related bloodstream infection with femoral venous catheters as compared to subclavian and internal jugular venous catheters: a systematic review of the literature and meta-analysis. Crit Care Med 2012;40:2479–85.
27. Timsit JF. What is the best site for central venous catheter insertion in critically ill patients? Crit Care 2003;7:397–99.
28. Parienti JJ, Mongardon N, Megarbane B, et al; 3SITES Study Group. Intravascular complications of central venous catheterization by insertion site. N Engl J Med 2015;373:1220–9.
29. Hind D, Calvert N, McWilliams R, et al. Ultrasonic locating devices for central venous cannulation: meta-analysis. BMJ 2003;327:361.
30. Fragou M, Gravvanis A, Dimitriou V, et al. Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: a prospective randomized study. Crit Care Med 2011;39:1607–12.
31. Pageler NM, Longhurst CA, Wood M, et al. Use of electronic medical record-enhanced checklist and electronic dashboard to decrease CLABSIs. Pediatrics 2014;133:e738–46.
32. Drews FA, Bakdash JZ, Gleed JR. Improving central line maintenance to reduce central line-associated bloodstream infections. Am J Infect Control 2017;45:1224–30.
33. Frost SA, Alogso MC, Metcalfe L, et al. Chlorhexidine bathing and health care-associated infections among adult intensive care patients: a systematic review and meta-analysis. Crit Care 2016;20:379.
34. Chopra V, O’Horo JC, Rogers MA, et al. The risk of bloodstream infection associated with peripherally inserted central catheters compared with central venous catheters in adults: a systematic review and meta-analysis. Infect Control Hosp Epidemiol 2013;34:908–18.
35. Xue H, Ix JH, Wang W, et al. Hemodialysis access usage patterns in the incident dialysis year and associated catheter-related complications. Am J Kidney Dis 2013;61:123–30.
36. Almuneef MA, Memish ZA, Balkhy HH, et al. Rate, risk factors and outcomes of catheter-related bloodstream infection in a paediatric intensive care unit in Saudi Arabia. J Hosp Infect 2006;62:207–13.
37. Alonso-Echanove J, Edwards JR, Richards MJ, et al. Effect of nurse staffing and antimicrobial-impregnated central venous catheters on the risk for bloodstream infections in intensive care units. Infect Control Hosp Epidemiol 2003;24:916–25.
38. Lorente L, Henry C, Martin MM, et al. Central venous catheter-related infection in a prospective and observational study of 2,595 catheters. Crit Care 2005;9:R631–5.
39. Rey C, Alvarez F, De-La-Rua V, et al. Intervention to reduce catheter-related bloodstream infections in a pediatric intensive care unit. Intensive Care Med 2011;37:678–85.
40. O’Brien J, Paquet F, Lindsay R, Valenti D. Insertion of PICCs with minimum number of lumens reduces complications and costs. J Am Coll Radiol. 2013;10:864–8.
41. Herc E, Patel P, Washer LL, et al. A model to predict central-line-associated bloodstream infection among patients with peripherally inserted central catheters: the MPC score. Infect Control Hosp Epidemiol 2017;38:1155–66.
42. Centers for Disease Control and Prevention. Vital signs: central line-associated blood stream infections--United States, 2001, 2008, and 2009. MMWR Morb Mortal Wkly Rep 2011;60:243–8.
1. Magill SS, Edwards JR, Bamberg W, et al; Emerging Infections Program Healthcare-Associated Infections and Antimicrobial Use Prevalence Survey Team. Multistate point-prevalence survey of health care-associated infections. N Engl J Med 2014;370:1198–208.
2. Marchetti A, Rossiter R. Economic burden of healthcare-associated infection in US acute care hospitals: societal perspective. J Med Econ 2013;16:1399–404.
3. O’Neil C, Ball K, Wood H, et al. A central line care maintenance bundle for the prevention of central line-associated bloodstream infection in non-intensive care unit settings. Infect Control Hosp Epidemiol 2016;37:1–7.
4. Shekelle PG, Wachter RM, Pronovost PJ, et al. Making health care safer II: an updated critical analysis of the evidence for patient safety practices. Evid Rep Technol Assess (Full Rep) 2013:1–945.
5. Patel PK, Gupta A, Vaughn VM, Mann JD, Ameling JM, Meddings J. Review of strategies to reduce central line-associated bloodstream infection (CLABSI) and catheter-associated urinary tract infection (CAUTI) in adult ICUs. J Hosp Med 2018;13:105–16.
6. Chopra V, Ratz D, Kuhn L, et al. PICC-associated bloodstream infections: prevalence, patterns, and predictors. Am J Med 2014;127:319–28.
7. Sagana R, Hyzy RC. Achieving zero central line-associated bloodstream infection rates in your intensive care unit. Crit Care Clin 2013;29:1–9.
8. Nelson RE, Angelovic AW, Nelson SD, Gleed JR, Drews FA. An economic analysis of adherence engineering to improve use of best practices during central line maintenance procedures. Infect Control Hosp Epidemiol 2015;36:550–6.
9. Pronovost P, Needham D, Berenholtz S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med 2006;355:2725–32.
10. Dumyati G, Concannon C, van Wijngaarden E, et al. Sustained reduction of central line-associated bloodstream infections outside the intensive care unit with a multimodal intervention focusing on central line maintenance. Am J Infect Control 2014;42:723–30.
11. Sacks GD, Diggs BS, Hadjizacharia P, et al. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement Central Line Bundle. Am J Surg 2014;207:817–23.
12. Boyce JM, Pittet D; Healthcare Infection Control Practices Advisory Committee; HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Guideline for hand hygiene in health-care settings: recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Society for Healthcare Epidemiology of America/Association for Professionals in Infection Control/Infectious Diseases Society of America. MMWR Recomm Rep 2002; 51:1-45, quiz CE1–4.
13. Marschall J, Mermel LA, et al; Society for Healthcare Epidemiology of America. Strategies to prevent central line-associated bloodstream infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol 2014;35:753–71.
14. Safdar N, Maki DG. The pathogenesis of catheter-related bloodstream infection with noncuffed short-term central venous catheters. Intensive Care Med 2004;30:62–7.
15. Shabot MM, Chassin MR, France AC, et al. Using the targeted solutions tool(R) to improve hand hygiene compliance is associated with decreased health care-associated infections. Jt Comm J Qual Patient Saf 2016;42:6–17.
16. Johnson L, Grueber S, Schlotzhauer C, et al. A multifactorial action plan improves hand hygiene adherence and significantly reduces central line-associated bloodstream infections. Am J Infect Control 2014;42:1146–51.
17. Barrera L, Zingg W, Mendez F, Pittet D. Effectiveness of a hand hygiene promotion strategy using alcohol-based handrub in 6 intensive care units in Colombia. Am J Infect Control 2011;39:633–9.
18. Hu KK, Lipsky BA, Veenstra DL, Saint S. Using maximal sterile barriers to prevent central venous catheter-related infection: a systematic evidence-based review. Am J Infect Control 2004;32:142–6.
19. Hu KK, Veenstra DL, Lipsky BA, Saint S. Use of maximal sterile barriers during central venous catheter insertion: clinical and economic outcomes. Clin Infect Dis 2004;39:1441–5.
20. Raad II, Hohn DC, Gilbreath BJ, et al. Prevention of central venous catheter-related infections by using maximal sterile barrier precautions during insertion. Infect Control Hosp Epidemiol 1994;15:231–8.
21. Furuya EY, Dick AW, Herzig CT, Pogorzelska-Maziarz M, Larson EL, Stone PW. Central line-associated bloodstream infection reduction and bundle compliance in intensive care units: a national study. Infect Control Hosp Epidemiol 2016;37:805–10.
22. Sherertz RJ, Ely EW, Westbrook DM, et al. Education of physicians-in-training can decrease the risk for vascular catheter infection. Ann Intern Med 2000;132:641–8.
23. Mimoz O, Lucet JC, Kerforne T, Pascal J, et al. Skin antisepsis with chlorhexidine-alcohol versus povidone iodine-alcohol, with and without skin scrubbing, for prevention of intravascular-catheter-related infection (CLEAN): an open-label, multicentre, randomised, controlled, two-by-two factorial trial. Lancet 2015;386:2069–77.
24. Lai NM, Lai NA, O’Riordan E, et al. Skin antisepsis for reducing central venous catheter-related infections. Cochrane Database Syst Rev 2016;7:CD010140.
25. Chopra V, Shojania KG. Recipes for checklists and bundles: one part active ingredient, two parts measurement. BMJ Qual Saf 2013;22:93–6.
26. Marik PE, Flemmer M, Harrison W. The risk of catheter-related bloodstream infection with femoral venous catheters as compared to subclavian and internal jugular venous catheters: a systematic review of the literature and meta-analysis. Crit Care Med 2012;40:2479–85.
27. Timsit JF. What is the best site for central venous catheter insertion in critically ill patients? Crit Care 2003;7:397–99.
28. Parienti JJ, Mongardon N, Megarbane B, et al; 3SITES Study Group. Intravascular complications of central venous catheterization by insertion site. N Engl J Med 2015;373:1220–9.
29. Hind D, Calvert N, McWilliams R, et al. Ultrasonic locating devices for central venous cannulation: meta-analysis. BMJ 2003;327:361.
30. Fragou M, Gravvanis A, Dimitriou V, et al. Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: a prospective randomized study. Crit Care Med 2011;39:1607–12.
31. Pageler NM, Longhurst CA, Wood M, et al. Use of electronic medical record-enhanced checklist and electronic dashboard to decrease CLABSIs. Pediatrics 2014;133:e738–46.
32. Drews FA, Bakdash JZ, Gleed JR. Improving central line maintenance to reduce central line-associated bloodstream infections. Am J Infect Control 2017;45:1224–30.
33. Frost SA, Alogso MC, Metcalfe L, et al. Chlorhexidine bathing and health care-associated infections among adult intensive care patients: a systematic review and meta-analysis. Crit Care 2016;20:379.
34. Chopra V, O’Horo JC, Rogers MA, et al. The risk of bloodstream infection associated with peripherally inserted central catheters compared with central venous catheters in adults: a systematic review and meta-analysis. Infect Control Hosp Epidemiol 2013;34:908–18.
35. Xue H, Ix JH, Wang W, et al. Hemodialysis access usage patterns in the incident dialysis year and associated catheter-related complications. Am J Kidney Dis 2013;61:123–30.
36. Almuneef MA, Memish ZA, Balkhy HH, et al. Rate, risk factors and outcomes of catheter-related bloodstream infection in a paediatric intensive care unit in Saudi Arabia. J Hosp Infect 2006;62:207–13.
37. Alonso-Echanove J, Edwards JR, Richards MJ, et al. Effect of nurse staffing and antimicrobial-impregnated central venous catheters on the risk for bloodstream infections in intensive care units. Infect Control Hosp Epidemiol 2003;24:916–25.
38. Lorente L, Henry C, Martin MM, et al. Central venous catheter-related infection in a prospective and observational study of 2,595 catheters. Crit Care 2005;9:R631–5.
39. Rey C, Alvarez F, De-La-Rua V, et al. Intervention to reduce catheter-related bloodstream infections in a pediatric intensive care unit. Intensive Care Med 2011;37:678–85.
40. O’Brien J, Paquet F, Lindsay R, Valenti D. Insertion of PICCs with minimum number of lumens reduces complications and costs. J Am Coll Radiol. 2013;10:864–8.
41. Herc E, Patel P, Washer LL, et al. A model to predict central-line-associated bloodstream infection among patients with peripherally inserted central catheters: the MPC score. Infect Control Hosp Epidemiol 2017;38:1155–66.
42. Centers for Disease Control and Prevention. Vital signs: central line-associated blood stream infections--United States, 2001, 2008, and 2009. MMWR Morb Mortal Wkly Rep 2011;60:243–8.