User login
Psychiatric partial hospitalization programs (PHPs), previously known as “day hospitals,” serve to bridge the gap between inpatient and outpatient facilities by providing intensive, highly structured outpatient behavioral health services (typically several hours of psychotherapy each weekday for most days of the week). The concept of PHPs has existed since at least the 1950s, but such programs started to become more common in the United States as the result of legislation passed in 1963 (Box1-3). In this article, I provide a brief introductory review of PHPs, while acknowledging that most research on PHPs was conducted years ago and is rather limited.
Box
The concept of partial hospitalization programs (PHPs) was developed before the 1950s.1 However, in the United States, PHPs did not take hold until Congress passed the Community Mental Health Act of 1963, which required that PHPs must be a core component of Community Mental Health Centers (CMHCs). The Omnibus Budget Reconciliation Acts of 1987 and 1990 required Medicare to pay for PHPs affiliated with or based in CMHCs and psychiatric hospitals, which resulted in a proliferation of PHPs across the country. The number of CMHCbased PHPs grew from 296 in 1993 to 769 in 1997.2 By 2016, more than one-third (38.7%) of all metropolitan hospitals and 11.4% of nonmetropolitan hospitals in the United States provided PHP services.3 This growth was also partially the result of private health insurance companies and the managed care industry clamping down on inpatient hospital stays and approving PHP care to reduce costs. In recent years, freestanding PHPs that are not affiliated with a CMHC or hospital have opened to serve high-functioning patients who do not want inpatient hospitalization or the stigma associated with it.
PHPs: What they are, and how they work
The term “partial hospitalization” is fraught with confusion because initially it was used to contrast such services from full hospitalization. Historically, it was used to describe services for patients who had been discharged home from a state hospital and attended a program on the hospital grounds during the day as outpatients. In reality, today’s PHPs are “day treatment” programs, but the terminology has stuck.
PHPs are neither an inpatient service nor a strict outpatient service, but rather a midground along the continuum of treatment intensity between the 2 traditional types of psychiatric services for patients with a range of mental illness of varying severity. The Association for Ambulatory Behavioral Healthcare, which has set standards and guidelines for PHPs, defines a PHP as “an ambulatory treatment program that includes the major diagnostic, medical, psychiatric, psychosocial, and prevocational treatment modalities designed for patients with serious mental disorders who require coordinated intensive, comprehensive, and multidisciplinary treatment not provided in an outpatient clinical setting.”4 PHPs can render acute care as an alternative to inpatient treatment, provide transitional stabilization treatment between an inpatient stay and traditional outpatient treatment (once a week or less frequent), and function as a supplement to traditional outpatient treatment.
Medicare has established criteria that PHPs must meet to qualify for reimbursement5; these criteria are now widely accepted as standards of care by the insurance industry. To meet the Medicare criteria, PHP treatment must be active and structured to provide an individualized treatment plan that incorporates coordination of services to meet the particular needs of the patient.5 It must include a multidisciplinary team approach to patient care under the direction of a physician, and the treatment goals must be measurable, functional, time-framed, medically necessary, and directly related to the reason for admission.5 The physician must certify the medical necessity for admission by documenting that the patient has a diagnosis of an acute Axis I mental disorder, a level of functioning that includes severe impairments in multiple areas of daily life, and a “reasonable expectation” that the disorder and level of functioning will improve as a result of the treatment.5
The Joint Commission (formerly JCAHO) lumps day treatment, intensive outpatient, partial hospitalization, and adult day care services into a single category of an ambulatory health care environment offering an organized day or night program of assessment, treatment, care, services, habilitation, or rehabilitation for individuals who do not require 24-hour care.6 For behavioral health, this may be a structured, ongoing program that typically meets 2 to 5 times a week for 2 to 5 hours per day.6
Most PHPs for adult patients provide services during the day 5 days per week and average 5 to 6 hours of programming per day. Night or evening programming may be a good option for patients who work during the day. Typically, treatment is provided in a group therapy format, with individual therapy at least once a week. Group therapy may include cognitive-behavioral therapy, coping with grief and loss, trauma recovery, conflict resolution, stress management, anger control, and behavioral modification. Family therapy is provided as needed, but usually is mandatory for children and adolescents. Many PHPs offer intensive outpatient programs (IOPs) as a step down to further facilitate a patient’s adjustment to psychosocial and family functioning while returning to work on a part-time basis. IOPs typically provide 3 to 4 hours of service per day 3 days per week. While not evidence-based, the typical duration of PHP treatment is 4 to 6 weeks, followed by an additional 2 to 4 weeks of IOP.
Continue to: Advantages and disadvantages...
Advantages and disadvantages
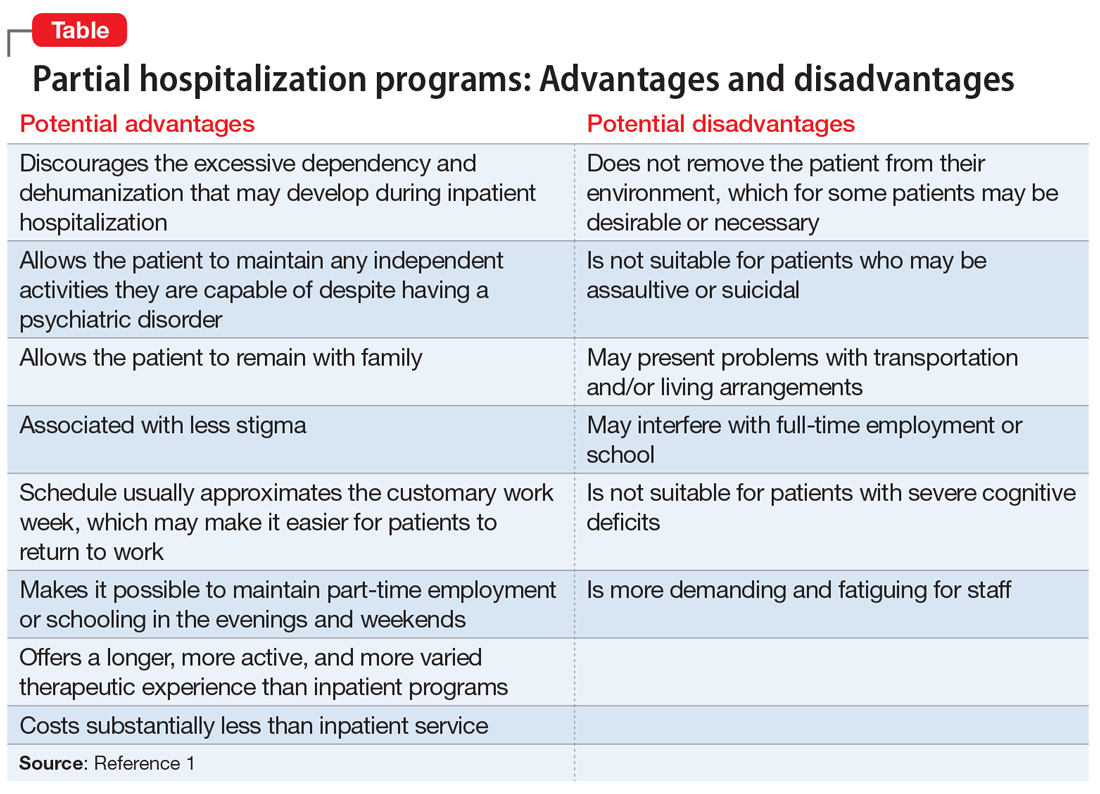
Based on a qualitative literature review, Neffinger1 outlined potential advantages and disadvantages of PHPs vs inpatient hospitalization (Table1). While these have not been empirically studied, they may be useful to consider when determining if a PHP would be beneficial for a specific patient.
Which factors are most therapeutic?
Research on which factors of PHPs are of therapeutic value is quite limited and primarily consists of surveys of small numbers of participants. Hoge et al7 explored the active therapeutic factors responsible for change in the Connecticut Mental Health Center PHP by comparing responses of 20 patients with those of their clinicians. Ninety-five percent of patients rated structure as the top therapeutic factor, followed by interpersonal contact, medication, and altruism. Other factors that were rated as important by 40% or fewer participants were catharsis, learning, mobilization of family support, connection to community, universality, patient autonomy, successful completion, security, feedback on behavior, and practice at home. In a British study8 that used a similar method, patients reported that counseling was the most helpful aspect of treatment, followed by medical treatment, while staff picked groups followed by a planned approach.
Evidence supports PHPs’ effectiveness
Some research has suggested that PHPs can be effective, both clinically and in terms of cost. Marshall et al9 conducted a systematic review of the effectiveness of an acute day hospital vs inpatient admission vs outpatient care that included 9 trials. They concluded that psychiatric inpatient admissions could be reduced by at least 23% if patients were diverted to an acute day hospital. They also found some evidence that day treatment programs may be superior to outpatient care in improving symptoms in nonpsychotic patients who are refractory to outpatient treatment. In a systematic review of 18 studies, high rates of satisfaction with PHP services suggested PHPs have an advantage over inpatient treatment within 1 year of discharge; patients and families were more satisfied with PHPs.10 In a study of 197 urban, socioeconomically disadvantaged, severely ill patients, Sledge et al11 compared the clinical outcomes of those who participated in day hospital programs with those of patients who received inpatient care. They found that while overall the 2 approaches produced similar outcomes, there were slightly more positive effects for day hospital programs in measures of symptoms, overall functioning, and social functioning. In terms of cost effectiveness, a 1978 study found that even after correcting for differences in treatment days between inpatient and PHP services, there was a significant financial advantage with PHP (costs were one-third less), primarily because of lower costs per day.12 In another study, PHP cost savings were 20%, and potential savings were higher for nonpsychotic patients.13
Are PHPs appropriate for children and adolescents?
Studies of PHPs for adolescents found that patients made gains in peer relationships, behavioral and academic performance, and control of their emotions.14,15 A review of PHPs’ effectiveness for children suggested that 66% to 99% of treated patients demonstrated improvement and successful return to community-based schools, and family functioning was a major factor in improvement.14 In a follow-up study that surveyed patients via telephone >1 year after discharge from a PHP, almost 80% of the children and adolescents were either “doing OK” or were “well-adjusted.”14 Only 22.5% required inpatient or residential treatment; the majority were doing well in school, with only 7% failing.14 In addition, 60% of parents reported satisfaction with treatment, and 85% reported functional improvement in their children.
Factors that predict PHP success or failure
In an analysis of a day treatment program that provided 4 months of intensive psychodynamic, group-oriented milieu treatment for patients with long-standing personality disorders, Rosie et al16 found 3 factors that contributed to the success of the PHP:
- optimal treatment-patient matching
- judicious use of authority in milieu therapy
- maintaining close relationships with referral sources.
In a study that compared 58 patients who completed an Ottawa hospital PHP and 44 who did not complete the program, psychological mindedness and chronicity of psychiatric illness were found to predict completion.17 However, a study of 59 females with anorexia nervosa who were transferred from inpatient care to an eating disorder day hospital program found that a longer duration of illness, amenorrhea, and a lower body mass index were associated with PHP treatment failure and inpatient rehospitalization.18 One study found that for individuals who were referred to a PHP from inpatient care, suicidal ideation and greater psychotic symptoms were associated with acute inpatient rehospitalization.19 Other factors associated with PHP nonattendance and treatment failure include limited personal and economic resources, high rates of substance abuse disorders, multiple admissions, and disability.20 In a study of 103 alcohol-dependent patients who completed IOP treatment, 64% were abstinent at 6 months follow-up; relapse was associated with a longer duration of alcohol dependence and a higher number of prior treatments, while favorable outcomes were associated with a lower degree of depression, anxiety, and craving.21 Patients with cocaine dependence who completed an IOP showed significant improvements in addiction scores and had more favorable outcomes in employment status and psychological problems if they stayed longer in treatment.22
Bottom Line
Psychiatric partial hospitalization programs (PHPs) provide a transition from inpatient hospitalization to outpatient treatment for patients who need further stabilization, or serve as an alternative to inpatient treatment for patients who don’t need or want inpatient hospitalization. PHPs can be as effective as inpatient treatment for all but the most seriously ill patients, and are more cost-effective than inpatient treatment.
1. Neffinger GG. Partial hospitalization: an overview. J Community Psychol. 1981;9(3):262-269.
2. Leung MY, Drozd EM, Healy DA, et al. Impacts associated with the Medicare Psychiatric PPS: a study of partial hospitalization programs. February 2009. Accessed January 8, 2022. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Reports/downloads/Leung_PHP_PPS_2010.pdf
3. Williams T, Borders TF, Jasinski L. Partial Psychiatric Hospitalization Program Availability in Non-Metropolitan and Non-Metropolitan Hospitals Nationally. Rural and Underserved Health Research Center; 2019.
4. Rosser J, Michael S, eds. Standards and guidelines for partial hospital programs and intensive outpatient programs. Association for Ambulatory Behavioral Healthcare. 2018. Accessed January 8, 2022. https://aabh.org/wp-content/uploads/2021/05/2021-SandG-Final.pdf
5. CMS Manual System PUB. 100-02 Medicare Benefit Policy: Partial Hospitalization Services, Department of Health and Human Services. Centers for Medicare & Medicaid Services; 2004:6-9.
6. Joint Commission. Guide to Joint Commission Behavioral Healthcare Accreditation. Joint Commission; 2007:36.
7. Hoge MA, Farrell SP, Munchel ME, et al. Therapeutic factors in partial hospitalization. Psychiatry. 1988;51(2):199-210.
8. Ricketts T, Kirshbaum MN. Helpfulness of mental health day care: client and staff views. J Adv Nurs. 1994;20(2):297-306.
9. Marshall M, Crowther R, Almaraz-Serrano A, et al. Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) acute day hospital versus admission; (2) vocational rehabilitation; (3) day hospital versus outpatient care. Health Technol Assess. 2001;5(21):1-75.
10. Horvitz-Lennon M, Normand SL, Gaccione P, et al. Partial versus full hospitalization for adults in psychiatric distress: a systematic review of the published literature (1957-1997). Am J Psychiatry. 2001;158(5):676-685.
11. Sledge WH, Tebes J, Rakfeldt J, et al. Day hospital/crisis respite care versus inpatient care, Part I: Clinical outcomes. Am J Psychiatry. 1996;153(8):1065-1073.
12. Fink EB, Longabaugh R, Stout R. The paradoxical underutilization of partial hospitalization. Am J Psychiatry. 1978;135(6):713-716.
13. Sledge WH, Tebes J, Wolff N, et al. Day hospital/crisis respite care versus inpatient care, Part II: service utilization and costs. Am J Psychiatry. 1996;153(8):1074-1083.
14. Kiser LJ. Treatment-effectiveness research in child and adolescent partial hospitalization. Psychiatr Hosp. 1991;22(2):51-8.
15. Milin R, Coupland K, Walker S, et al. Outcome and follow-up study of an adolescent psychiatric day treatment school program. J Am Acad Child Adolesc Psychiatry. 2000;39(3):320-328.
16. Rosie JS, Azim HF, Piper WE, et al. Effective psychiatric day treatment: historical lessons. Psychiatr Serv. 1995;46(10):1019-1026.
17. Tasca GA, Balfour L, Bissada H, et al. Treatment completion and outcome in a partial hospitalization program: interactions among patient variables. Psychotherapy Res. 1999;9(2):232-247.
18. Howard WT, Evans KK, Quintero-Howard CV, et al. Predictors of success or failure of transition to day hospital treatment for inpatients with anorexia nervosa. Am J Psychiatry. 1999;156(11):1697-1702.
19. Beard C, Hearon BA, Lee J, et al. When partial hospitalization fails: risk factors for inpatient hospitalization. J Nerv Ment Dis. 2016;204(6):431-436.
20. Lieberman PB, Guggenheim FG. Reasons for patient nonattendance during acute partial hospitalization. Psychiatr Serv. 2016;67(6):684-687.
21. Bottlender M, Soyka M. Efficacy of an intensive outpatient rehabilitation program in alcoholism: predictors of outcome 6 months after treatment. Eur Addict Res. 2005;11(3):132-137.
22. Gottheil E, Weinstein SP, Sterling RC, et al. A randomized controlled study of the effectiveness of intensive outpatient treatment for cocaine dependence. Psychiatr Serv. 1998;49(6):782-787.
Psychiatric partial hospitalization programs (PHPs), previously known as “day hospitals,” serve to bridge the gap between inpatient and outpatient facilities by providing intensive, highly structured outpatient behavioral health services (typically several hours of psychotherapy each weekday for most days of the week). The concept of PHPs has existed since at least the 1950s, but such programs started to become more common in the United States as the result of legislation passed in 1963 (Box1-3). In this article, I provide a brief introductory review of PHPs, while acknowledging that most research on PHPs was conducted years ago and is rather limited.
Box
The concept of partial hospitalization programs (PHPs) was developed before the 1950s.1 However, in the United States, PHPs did not take hold until Congress passed the Community Mental Health Act of 1963, which required that PHPs must be a core component of Community Mental Health Centers (CMHCs). The Omnibus Budget Reconciliation Acts of 1987 and 1990 required Medicare to pay for PHPs affiliated with or based in CMHCs and psychiatric hospitals, which resulted in a proliferation of PHPs across the country. The number of CMHCbased PHPs grew from 296 in 1993 to 769 in 1997.2 By 2016, more than one-third (38.7%) of all metropolitan hospitals and 11.4% of nonmetropolitan hospitals in the United States provided PHP services.3 This growth was also partially the result of private health insurance companies and the managed care industry clamping down on inpatient hospital stays and approving PHP care to reduce costs. In recent years, freestanding PHPs that are not affiliated with a CMHC or hospital have opened to serve high-functioning patients who do not want inpatient hospitalization or the stigma associated with it.
PHPs: What they are, and how they work
The term “partial hospitalization” is fraught with confusion because initially it was used to contrast such services from full hospitalization. Historically, it was used to describe services for patients who had been discharged home from a state hospital and attended a program on the hospital grounds during the day as outpatients. In reality, today’s PHPs are “day treatment” programs, but the terminology has stuck.
PHPs are neither an inpatient service nor a strict outpatient service, but rather a midground along the continuum of treatment intensity between the 2 traditional types of psychiatric services for patients with a range of mental illness of varying severity. The Association for Ambulatory Behavioral Healthcare, which has set standards and guidelines for PHPs, defines a PHP as “an ambulatory treatment program that includes the major diagnostic, medical, psychiatric, psychosocial, and prevocational treatment modalities designed for patients with serious mental disorders who require coordinated intensive, comprehensive, and multidisciplinary treatment not provided in an outpatient clinical setting.”4 PHPs can render acute care as an alternative to inpatient treatment, provide transitional stabilization treatment between an inpatient stay and traditional outpatient treatment (once a week or less frequent), and function as a supplement to traditional outpatient treatment.
Medicare has established criteria that PHPs must meet to qualify for reimbursement5; these criteria are now widely accepted as standards of care by the insurance industry. To meet the Medicare criteria, PHP treatment must be active and structured to provide an individualized treatment plan that incorporates coordination of services to meet the particular needs of the patient.5 It must include a multidisciplinary team approach to patient care under the direction of a physician, and the treatment goals must be measurable, functional, time-framed, medically necessary, and directly related to the reason for admission.5 The physician must certify the medical necessity for admission by documenting that the patient has a diagnosis of an acute Axis I mental disorder, a level of functioning that includes severe impairments in multiple areas of daily life, and a “reasonable expectation” that the disorder and level of functioning will improve as a result of the treatment.5
The Joint Commission (formerly JCAHO) lumps day treatment, intensive outpatient, partial hospitalization, and adult day care services into a single category of an ambulatory health care environment offering an organized day or night program of assessment, treatment, care, services, habilitation, or rehabilitation for individuals who do not require 24-hour care.6 For behavioral health, this may be a structured, ongoing program that typically meets 2 to 5 times a week for 2 to 5 hours per day.6
Most PHPs for adult patients provide services during the day 5 days per week and average 5 to 6 hours of programming per day. Night or evening programming may be a good option for patients who work during the day. Typically, treatment is provided in a group therapy format, with individual therapy at least once a week. Group therapy may include cognitive-behavioral therapy, coping with grief and loss, trauma recovery, conflict resolution, stress management, anger control, and behavioral modification. Family therapy is provided as needed, but usually is mandatory for children and adolescents. Many PHPs offer intensive outpatient programs (IOPs) as a step down to further facilitate a patient’s adjustment to psychosocial and family functioning while returning to work on a part-time basis. IOPs typically provide 3 to 4 hours of service per day 3 days per week. While not evidence-based, the typical duration of PHP treatment is 4 to 6 weeks, followed by an additional 2 to 4 weeks of IOP.
Continue to: Advantages and disadvantages...
Advantages and disadvantages
Based on a qualitative literature review, Neffinger1 outlined potential advantages and disadvantages of PHPs vs inpatient hospitalization (Table1). While these have not been empirically studied, they may be useful to consider when determining if a PHP would be beneficial for a specific patient.
Which factors are most therapeutic?
Research on which factors of PHPs are of therapeutic value is quite limited and primarily consists of surveys of small numbers of participants. Hoge et al7 explored the active therapeutic factors responsible for change in the Connecticut Mental Health Center PHP by comparing responses of 20 patients with those of their clinicians. Ninety-five percent of patients rated structure as the top therapeutic factor, followed by interpersonal contact, medication, and altruism. Other factors that were rated as important by 40% or fewer participants were catharsis, learning, mobilization of family support, connection to community, universality, patient autonomy, successful completion, security, feedback on behavior, and practice at home. In a British study8 that used a similar method, patients reported that counseling was the most helpful aspect of treatment, followed by medical treatment, while staff picked groups followed by a planned approach.
Evidence supports PHPs’ effectiveness
Some research has suggested that PHPs can be effective, both clinically and in terms of cost. Marshall et al9 conducted a systematic review of the effectiveness of an acute day hospital vs inpatient admission vs outpatient care that included 9 trials. They concluded that psychiatric inpatient admissions could be reduced by at least 23% if patients were diverted to an acute day hospital. They also found some evidence that day treatment programs may be superior to outpatient care in improving symptoms in nonpsychotic patients who are refractory to outpatient treatment. In a systematic review of 18 studies, high rates of satisfaction with PHP services suggested PHPs have an advantage over inpatient treatment within 1 year of discharge; patients and families were more satisfied with PHPs.10 In a study of 197 urban, socioeconomically disadvantaged, severely ill patients, Sledge et al11 compared the clinical outcomes of those who participated in day hospital programs with those of patients who received inpatient care. They found that while overall the 2 approaches produced similar outcomes, there were slightly more positive effects for day hospital programs in measures of symptoms, overall functioning, and social functioning. In terms of cost effectiveness, a 1978 study found that even after correcting for differences in treatment days between inpatient and PHP services, there was a significant financial advantage with PHP (costs were one-third less), primarily because of lower costs per day.12 In another study, PHP cost savings were 20%, and potential savings were higher for nonpsychotic patients.13
Are PHPs appropriate for children and adolescents?
Studies of PHPs for adolescents found that patients made gains in peer relationships, behavioral and academic performance, and control of their emotions.14,15 A review of PHPs’ effectiveness for children suggested that 66% to 99% of treated patients demonstrated improvement and successful return to community-based schools, and family functioning was a major factor in improvement.14 In a follow-up study that surveyed patients via telephone >1 year after discharge from a PHP, almost 80% of the children and adolescents were either “doing OK” or were “well-adjusted.”14 Only 22.5% required inpatient or residential treatment; the majority were doing well in school, with only 7% failing.14 In addition, 60% of parents reported satisfaction with treatment, and 85% reported functional improvement in their children.
Factors that predict PHP success or failure
In an analysis of a day treatment program that provided 4 months of intensive psychodynamic, group-oriented milieu treatment for patients with long-standing personality disorders, Rosie et al16 found 3 factors that contributed to the success of the PHP:
- optimal treatment-patient matching
- judicious use of authority in milieu therapy
- maintaining close relationships with referral sources.
In a study that compared 58 patients who completed an Ottawa hospital PHP and 44 who did not complete the program, psychological mindedness and chronicity of psychiatric illness were found to predict completion.17 However, a study of 59 females with anorexia nervosa who were transferred from inpatient care to an eating disorder day hospital program found that a longer duration of illness, amenorrhea, and a lower body mass index were associated with PHP treatment failure and inpatient rehospitalization.18 One study found that for individuals who were referred to a PHP from inpatient care, suicidal ideation and greater psychotic symptoms were associated with acute inpatient rehospitalization.19 Other factors associated with PHP nonattendance and treatment failure include limited personal and economic resources, high rates of substance abuse disorders, multiple admissions, and disability.20 In a study of 103 alcohol-dependent patients who completed IOP treatment, 64% were abstinent at 6 months follow-up; relapse was associated with a longer duration of alcohol dependence and a higher number of prior treatments, while favorable outcomes were associated with a lower degree of depression, anxiety, and craving.21 Patients with cocaine dependence who completed an IOP showed significant improvements in addiction scores and had more favorable outcomes in employment status and psychological problems if they stayed longer in treatment.22
Bottom Line
Psychiatric partial hospitalization programs (PHPs) provide a transition from inpatient hospitalization to outpatient treatment for patients who need further stabilization, or serve as an alternative to inpatient treatment for patients who don’t need or want inpatient hospitalization. PHPs can be as effective as inpatient treatment for all but the most seriously ill patients, and are more cost-effective than inpatient treatment.
Psychiatric partial hospitalization programs (PHPs), previously known as “day hospitals,” serve to bridge the gap between inpatient and outpatient facilities by providing intensive, highly structured outpatient behavioral health services (typically several hours of psychotherapy each weekday for most days of the week). The concept of PHPs has existed since at least the 1950s, but such programs started to become more common in the United States as the result of legislation passed in 1963 (Box1-3). In this article, I provide a brief introductory review of PHPs, while acknowledging that most research on PHPs was conducted years ago and is rather limited.
Box
The concept of partial hospitalization programs (PHPs) was developed before the 1950s.1 However, in the United States, PHPs did not take hold until Congress passed the Community Mental Health Act of 1963, which required that PHPs must be a core component of Community Mental Health Centers (CMHCs). The Omnibus Budget Reconciliation Acts of 1987 and 1990 required Medicare to pay for PHPs affiliated with or based in CMHCs and psychiatric hospitals, which resulted in a proliferation of PHPs across the country. The number of CMHCbased PHPs grew from 296 in 1993 to 769 in 1997.2 By 2016, more than one-third (38.7%) of all metropolitan hospitals and 11.4% of nonmetropolitan hospitals in the United States provided PHP services.3 This growth was also partially the result of private health insurance companies and the managed care industry clamping down on inpatient hospital stays and approving PHP care to reduce costs. In recent years, freestanding PHPs that are not affiliated with a CMHC or hospital have opened to serve high-functioning patients who do not want inpatient hospitalization or the stigma associated with it.
PHPs: What they are, and how they work
The term “partial hospitalization” is fraught with confusion because initially it was used to contrast such services from full hospitalization. Historically, it was used to describe services for patients who had been discharged home from a state hospital and attended a program on the hospital grounds during the day as outpatients. In reality, today’s PHPs are “day treatment” programs, but the terminology has stuck.
PHPs are neither an inpatient service nor a strict outpatient service, but rather a midground along the continuum of treatment intensity between the 2 traditional types of psychiatric services for patients with a range of mental illness of varying severity. The Association for Ambulatory Behavioral Healthcare, which has set standards and guidelines for PHPs, defines a PHP as “an ambulatory treatment program that includes the major diagnostic, medical, psychiatric, psychosocial, and prevocational treatment modalities designed for patients with serious mental disorders who require coordinated intensive, comprehensive, and multidisciplinary treatment not provided in an outpatient clinical setting.”4 PHPs can render acute care as an alternative to inpatient treatment, provide transitional stabilization treatment between an inpatient stay and traditional outpatient treatment (once a week or less frequent), and function as a supplement to traditional outpatient treatment.
Medicare has established criteria that PHPs must meet to qualify for reimbursement5; these criteria are now widely accepted as standards of care by the insurance industry. To meet the Medicare criteria, PHP treatment must be active and structured to provide an individualized treatment plan that incorporates coordination of services to meet the particular needs of the patient.5 It must include a multidisciplinary team approach to patient care under the direction of a physician, and the treatment goals must be measurable, functional, time-framed, medically necessary, and directly related to the reason for admission.5 The physician must certify the medical necessity for admission by documenting that the patient has a diagnosis of an acute Axis I mental disorder, a level of functioning that includes severe impairments in multiple areas of daily life, and a “reasonable expectation” that the disorder and level of functioning will improve as a result of the treatment.5
The Joint Commission (formerly JCAHO) lumps day treatment, intensive outpatient, partial hospitalization, and adult day care services into a single category of an ambulatory health care environment offering an organized day or night program of assessment, treatment, care, services, habilitation, or rehabilitation for individuals who do not require 24-hour care.6 For behavioral health, this may be a structured, ongoing program that typically meets 2 to 5 times a week for 2 to 5 hours per day.6
Most PHPs for adult patients provide services during the day 5 days per week and average 5 to 6 hours of programming per day. Night or evening programming may be a good option for patients who work during the day. Typically, treatment is provided in a group therapy format, with individual therapy at least once a week. Group therapy may include cognitive-behavioral therapy, coping with grief and loss, trauma recovery, conflict resolution, stress management, anger control, and behavioral modification. Family therapy is provided as needed, but usually is mandatory for children and adolescents. Many PHPs offer intensive outpatient programs (IOPs) as a step down to further facilitate a patient’s adjustment to psychosocial and family functioning while returning to work on a part-time basis. IOPs typically provide 3 to 4 hours of service per day 3 days per week. While not evidence-based, the typical duration of PHP treatment is 4 to 6 weeks, followed by an additional 2 to 4 weeks of IOP.
Continue to: Advantages and disadvantages...
Advantages and disadvantages
Based on a qualitative literature review, Neffinger1 outlined potential advantages and disadvantages of PHPs vs inpatient hospitalization (Table1). While these have not been empirically studied, they may be useful to consider when determining if a PHP would be beneficial for a specific patient.
Which factors are most therapeutic?
Research on which factors of PHPs are of therapeutic value is quite limited and primarily consists of surveys of small numbers of participants. Hoge et al7 explored the active therapeutic factors responsible for change in the Connecticut Mental Health Center PHP by comparing responses of 20 patients with those of their clinicians. Ninety-five percent of patients rated structure as the top therapeutic factor, followed by interpersonal contact, medication, and altruism. Other factors that were rated as important by 40% or fewer participants were catharsis, learning, mobilization of family support, connection to community, universality, patient autonomy, successful completion, security, feedback on behavior, and practice at home. In a British study8 that used a similar method, patients reported that counseling was the most helpful aspect of treatment, followed by medical treatment, while staff picked groups followed by a planned approach.
Evidence supports PHPs’ effectiveness
Some research has suggested that PHPs can be effective, both clinically and in terms of cost. Marshall et al9 conducted a systematic review of the effectiveness of an acute day hospital vs inpatient admission vs outpatient care that included 9 trials. They concluded that psychiatric inpatient admissions could be reduced by at least 23% if patients were diverted to an acute day hospital. They also found some evidence that day treatment programs may be superior to outpatient care in improving symptoms in nonpsychotic patients who are refractory to outpatient treatment. In a systematic review of 18 studies, high rates of satisfaction with PHP services suggested PHPs have an advantage over inpatient treatment within 1 year of discharge; patients and families were more satisfied with PHPs.10 In a study of 197 urban, socioeconomically disadvantaged, severely ill patients, Sledge et al11 compared the clinical outcomes of those who participated in day hospital programs with those of patients who received inpatient care. They found that while overall the 2 approaches produced similar outcomes, there were slightly more positive effects for day hospital programs in measures of symptoms, overall functioning, and social functioning. In terms of cost effectiveness, a 1978 study found that even after correcting for differences in treatment days between inpatient and PHP services, there was a significant financial advantage with PHP (costs were one-third less), primarily because of lower costs per day.12 In another study, PHP cost savings were 20%, and potential savings were higher for nonpsychotic patients.13
Are PHPs appropriate for children and adolescents?
Studies of PHPs for adolescents found that patients made gains in peer relationships, behavioral and academic performance, and control of their emotions.14,15 A review of PHPs’ effectiveness for children suggested that 66% to 99% of treated patients demonstrated improvement and successful return to community-based schools, and family functioning was a major factor in improvement.14 In a follow-up study that surveyed patients via telephone >1 year after discharge from a PHP, almost 80% of the children and adolescents were either “doing OK” or were “well-adjusted.”14 Only 22.5% required inpatient or residential treatment; the majority were doing well in school, with only 7% failing.14 In addition, 60% of parents reported satisfaction with treatment, and 85% reported functional improvement in their children.
Factors that predict PHP success or failure
In an analysis of a day treatment program that provided 4 months of intensive psychodynamic, group-oriented milieu treatment for patients with long-standing personality disorders, Rosie et al16 found 3 factors that contributed to the success of the PHP:
- optimal treatment-patient matching
- judicious use of authority in milieu therapy
- maintaining close relationships with referral sources.
In a study that compared 58 patients who completed an Ottawa hospital PHP and 44 who did not complete the program, psychological mindedness and chronicity of psychiatric illness were found to predict completion.17 However, a study of 59 females with anorexia nervosa who were transferred from inpatient care to an eating disorder day hospital program found that a longer duration of illness, amenorrhea, and a lower body mass index were associated with PHP treatment failure and inpatient rehospitalization.18 One study found that for individuals who were referred to a PHP from inpatient care, suicidal ideation and greater psychotic symptoms were associated with acute inpatient rehospitalization.19 Other factors associated with PHP nonattendance and treatment failure include limited personal and economic resources, high rates of substance abuse disorders, multiple admissions, and disability.20 In a study of 103 alcohol-dependent patients who completed IOP treatment, 64% were abstinent at 6 months follow-up; relapse was associated with a longer duration of alcohol dependence and a higher number of prior treatments, while favorable outcomes were associated with a lower degree of depression, anxiety, and craving.21 Patients with cocaine dependence who completed an IOP showed significant improvements in addiction scores and had more favorable outcomes in employment status and psychological problems if they stayed longer in treatment.22
Bottom Line
Psychiatric partial hospitalization programs (PHPs) provide a transition from inpatient hospitalization to outpatient treatment for patients who need further stabilization, or serve as an alternative to inpatient treatment for patients who don’t need or want inpatient hospitalization. PHPs can be as effective as inpatient treatment for all but the most seriously ill patients, and are more cost-effective than inpatient treatment.
1. Neffinger GG. Partial hospitalization: an overview. J Community Psychol. 1981;9(3):262-269.
2. Leung MY, Drozd EM, Healy DA, et al. Impacts associated with the Medicare Psychiatric PPS: a study of partial hospitalization programs. February 2009. Accessed January 8, 2022. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Reports/downloads/Leung_PHP_PPS_2010.pdf
3. Williams T, Borders TF, Jasinski L. Partial Psychiatric Hospitalization Program Availability in Non-Metropolitan and Non-Metropolitan Hospitals Nationally. Rural and Underserved Health Research Center; 2019.
4. Rosser J, Michael S, eds. Standards and guidelines for partial hospital programs and intensive outpatient programs. Association for Ambulatory Behavioral Healthcare. 2018. Accessed January 8, 2022. https://aabh.org/wp-content/uploads/2021/05/2021-SandG-Final.pdf
5. CMS Manual System PUB. 100-02 Medicare Benefit Policy: Partial Hospitalization Services, Department of Health and Human Services. Centers for Medicare & Medicaid Services; 2004:6-9.
6. Joint Commission. Guide to Joint Commission Behavioral Healthcare Accreditation. Joint Commission; 2007:36.
7. Hoge MA, Farrell SP, Munchel ME, et al. Therapeutic factors in partial hospitalization. Psychiatry. 1988;51(2):199-210.
8. Ricketts T, Kirshbaum MN. Helpfulness of mental health day care: client and staff views. J Adv Nurs. 1994;20(2):297-306.
9. Marshall M, Crowther R, Almaraz-Serrano A, et al. Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) acute day hospital versus admission; (2) vocational rehabilitation; (3) day hospital versus outpatient care. Health Technol Assess. 2001;5(21):1-75.
10. Horvitz-Lennon M, Normand SL, Gaccione P, et al. Partial versus full hospitalization for adults in psychiatric distress: a systematic review of the published literature (1957-1997). Am J Psychiatry. 2001;158(5):676-685.
11. Sledge WH, Tebes J, Rakfeldt J, et al. Day hospital/crisis respite care versus inpatient care, Part I: Clinical outcomes. Am J Psychiatry. 1996;153(8):1065-1073.
12. Fink EB, Longabaugh R, Stout R. The paradoxical underutilization of partial hospitalization. Am J Psychiatry. 1978;135(6):713-716.
13. Sledge WH, Tebes J, Wolff N, et al. Day hospital/crisis respite care versus inpatient care, Part II: service utilization and costs. Am J Psychiatry. 1996;153(8):1074-1083.
14. Kiser LJ. Treatment-effectiveness research in child and adolescent partial hospitalization. Psychiatr Hosp. 1991;22(2):51-8.
15. Milin R, Coupland K, Walker S, et al. Outcome and follow-up study of an adolescent psychiatric day treatment school program. J Am Acad Child Adolesc Psychiatry. 2000;39(3):320-328.
16. Rosie JS, Azim HF, Piper WE, et al. Effective psychiatric day treatment: historical lessons. Psychiatr Serv. 1995;46(10):1019-1026.
17. Tasca GA, Balfour L, Bissada H, et al. Treatment completion and outcome in a partial hospitalization program: interactions among patient variables. Psychotherapy Res. 1999;9(2):232-247.
18. Howard WT, Evans KK, Quintero-Howard CV, et al. Predictors of success or failure of transition to day hospital treatment for inpatients with anorexia nervosa. Am J Psychiatry. 1999;156(11):1697-1702.
19. Beard C, Hearon BA, Lee J, et al. When partial hospitalization fails: risk factors for inpatient hospitalization. J Nerv Ment Dis. 2016;204(6):431-436.
20. Lieberman PB, Guggenheim FG. Reasons for patient nonattendance during acute partial hospitalization. Psychiatr Serv. 2016;67(6):684-687.
21. Bottlender M, Soyka M. Efficacy of an intensive outpatient rehabilitation program in alcoholism: predictors of outcome 6 months after treatment. Eur Addict Res. 2005;11(3):132-137.
22. Gottheil E, Weinstein SP, Sterling RC, et al. A randomized controlled study of the effectiveness of intensive outpatient treatment for cocaine dependence. Psychiatr Serv. 1998;49(6):782-787.
1. Neffinger GG. Partial hospitalization: an overview. J Community Psychol. 1981;9(3):262-269.
2. Leung MY, Drozd EM, Healy DA, et al. Impacts associated with the Medicare Psychiatric PPS: a study of partial hospitalization programs. February 2009. Accessed January 8, 2022. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Reports/downloads/Leung_PHP_PPS_2010.pdf
3. Williams T, Borders TF, Jasinski L. Partial Psychiatric Hospitalization Program Availability in Non-Metropolitan and Non-Metropolitan Hospitals Nationally. Rural and Underserved Health Research Center; 2019.
4. Rosser J, Michael S, eds. Standards and guidelines for partial hospital programs and intensive outpatient programs. Association for Ambulatory Behavioral Healthcare. 2018. Accessed January 8, 2022. https://aabh.org/wp-content/uploads/2021/05/2021-SandG-Final.pdf
5. CMS Manual System PUB. 100-02 Medicare Benefit Policy: Partial Hospitalization Services, Department of Health and Human Services. Centers for Medicare & Medicaid Services; 2004:6-9.
6. Joint Commission. Guide to Joint Commission Behavioral Healthcare Accreditation. Joint Commission; 2007:36.
7. Hoge MA, Farrell SP, Munchel ME, et al. Therapeutic factors in partial hospitalization. Psychiatry. 1988;51(2):199-210.
8. Ricketts T, Kirshbaum MN. Helpfulness of mental health day care: client and staff views. J Adv Nurs. 1994;20(2):297-306.
9. Marshall M, Crowther R, Almaraz-Serrano A, et al. Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) acute day hospital versus admission; (2) vocational rehabilitation; (3) day hospital versus outpatient care. Health Technol Assess. 2001;5(21):1-75.
10. Horvitz-Lennon M, Normand SL, Gaccione P, et al. Partial versus full hospitalization for adults in psychiatric distress: a systematic review of the published literature (1957-1997). Am J Psychiatry. 2001;158(5):676-685.
11. Sledge WH, Tebes J, Rakfeldt J, et al. Day hospital/crisis respite care versus inpatient care, Part I: Clinical outcomes. Am J Psychiatry. 1996;153(8):1065-1073.
12. Fink EB, Longabaugh R, Stout R. The paradoxical underutilization of partial hospitalization. Am J Psychiatry. 1978;135(6):713-716.
13. Sledge WH, Tebes J, Wolff N, et al. Day hospital/crisis respite care versus inpatient care, Part II: service utilization and costs. Am J Psychiatry. 1996;153(8):1074-1083.
14. Kiser LJ. Treatment-effectiveness research in child and adolescent partial hospitalization. Psychiatr Hosp. 1991;22(2):51-8.
15. Milin R, Coupland K, Walker S, et al. Outcome and follow-up study of an adolescent psychiatric day treatment school program. J Am Acad Child Adolesc Psychiatry. 2000;39(3):320-328.
16. Rosie JS, Azim HF, Piper WE, et al. Effective psychiatric day treatment: historical lessons. Psychiatr Serv. 1995;46(10):1019-1026.
17. Tasca GA, Balfour L, Bissada H, et al. Treatment completion and outcome in a partial hospitalization program: interactions among patient variables. Psychotherapy Res. 1999;9(2):232-247.
18. Howard WT, Evans KK, Quintero-Howard CV, et al. Predictors of success or failure of transition to day hospital treatment for inpatients with anorexia nervosa. Am J Psychiatry. 1999;156(11):1697-1702.
19. Beard C, Hearon BA, Lee J, et al. When partial hospitalization fails: risk factors for inpatient hospitalization. J Nerv Ment Dis. 2016;204(6):431-436.
20. Lieberman PB, Guggenheim FG. Reasons for patient nonattendance during acute partial hospitalization. Psychiatr Serv. 2016;67(6):684-687.
21. Bottlender M, Soyka M. Efficacy of an intensive outpatient rehabilitation program in alcoholism: predictors of outcome 6 months after treatment. Eur Addict Res. 2005;11(3):132-137.
22. Gottheil E, Weinstein SP, Sterling RC, et al. A randomized controlled study of the effectiveness of intensive outpatient treatment for cocaine dependence. Psychiatr Serv. 1998;49(6):782-787.