User login
VANCOUVER – Dimethyl fumarate and fingolimod appear to have an edge over other disease-modifying therapies for multiple sclerosis (MS) in real-world practice, according to a comparative effectiveness study reported at the annual meeting of the American Academy of Neurology.
Dr. Jacqueline A. Nicholas, a neuroimmunologist and MS specialist with the OhioHealth Multiple Sclerosis Center, Riverside Methodist Hospital, Columbus, and her colleagues analyzed claims data from 5,004 commercially insured adults with MS in the United States who started treatment with any of five oral and injectable disease-modifying therapies.
Findings reported at the meeting showed that dimethyl fumarate netted the greatest reduction in annualized relapse rate, at one-third, followed by fingolimod, at about one-fourth. The adjusted risk of relapse in the year after drug initiation was significantly higher for interferon-beta, glatiramer acetate, and teriflunomide, compared with dimethyl fumarate.
“Right now, a lot of the data that we have to use in the clinic is based on clinical trials data. That’s often not what we see in the real world, the MS centers, and even the outpatient neurology setting,” Dr. Nicholas said in an interview. “This study is nice just because it points out that when you look at real-world data, it shows, yes, that these drugs work, and that some of the initial benefit for the oral disease-modifying therapies is what we thought. Obviously, we don’t have cross-trial comparisons to make from the clinical trials, so this is real data that we can actually use in our clinic setting.”
The findings are also helpful given changing health care models and ongoing issues with reimbursement and obtaining insurance approval to use various drugs, she added. “These are things that we can show to those payers as to why it’s important that we have these therapies and that we be able to decide as MS specialists what’s going to be best for the patient.
“Right now, the biggest challenge in the MS world is that obviously, as an MS specialist, you have a lot of experience and knowledge. And based on poor prognostic factors, when somebody comes in, you may not want to go with an escalation model [of treatment], where you are starting with something that a payer may think we should start with, an injectable,” Dr. Nicholas added. “Somebody may have more aggressive disease, and maybe you are going to want to start with an oral or an IV drug. But the payers are the ones right now who have the say. So it’s a lot of time and a lot of work [getting insurance approval], and while you are fighting to get what you know your patient needs, your patient’s suffering, accumulating disability, and possibly having more relapses.”
For the study, the investigators analyzed administrative data from the Truven MarketScan Commercial Claims Databases for 2012 through 2014.
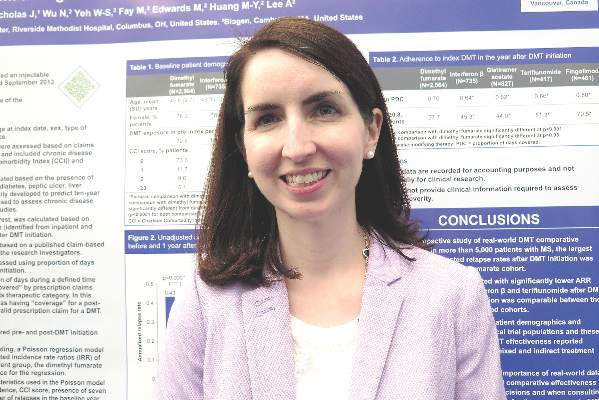
Analyses were based on 2,564 patients treated with dimethyl fumarate (brand name Tecfidera), 735 with interferon-beta (Rebif, Avonex, Betaseron, and Extavia), 827 with glatiramer acetate (Copaxone), 417 with teriflunomide (Aubagio), and 461 with fingolimod (Gilenya).
Comparing the year before and the year after drug initiation, only dimethyl fumarate and fingolimod were associated with significant reductions in the annualized relapse rate, according to findings reported in a poster session. The reductions were 33% and 27%, respectively.
In the postinitiation year and with dimethyl fumarate as the comparator, the adjusted incidence rate ratio for relapse was similar for fingolimod but significantly higher for glatiramer acetate (1.28), interferon-beta (1.25), and teriflunomide (1.28).
“I don’t think that these findings are surprising,” Dr. Nicholas said. “I work in a large MS center and I would say this is generally what I see clinically in terms of the effectiveness. So it’s more reassuring to me than anything.”
She acknowledged that safety and tolerability will also come into play when selecting among disease-modifying therapies. “Those data are incredibly important, and we certainly balance that. With a health care claims database, that’s hard data to pull unless you are looking at one specific [adverse effect], but that’s something that needs to be very carefully weighed with the efficacy data for the patient,” she said.
In a companion study also reported in the poster session, the investigators compared the impact of starting the same five drugs on health care costs and utilization.
Results of that study showed that total health care costs rose in the postinitiation year for all five drugs, with the increase ranging from $38,801 for dimethyl fumarate to $52,352 for fingolimod.
However, total nonprescription medical costs decreased across the board, apparently driven by both less use of outpatient services and fewer inpatient hospital stays, with the greatest reduction seen for dimethyl fumarate.
Dr. Nicholas disclosed that she has received research funding from Genzyme, Novartis, Teva, Biogen, and Alexion, and has received consulting and speaking honoraria from Genzyme, Novartis, Teva, Biogen, and Medtronic. The study was supported by Biogen.
VANCOUVER – Dimethyl fumarate and fingolimod appear to have an edge over other disease-modifying therapies for multiple sclerosis (MS) in real-world practice, according to a comparative effectiveness study reported at the annual meeting of the American Academy of Neurology.
Dr. Jacqueline A. Nicholas, a neuroimmunologist and MS specialist with the OhioHealth Multiple Sclerosis Center, Riverside Methodist Hospital, Columbus, and her colleagues analyzed claims data from 5,004 commercially insured adults with MS in the United States who started treatment with any of five oral and injectable disease-modifying therapies.
Findings reported at the meeting showed that dimethyl fumarate netted the greatest reduction in annualized relapse rate, at one-third, followed by fingolimod, at about one-fourth. The adjusted risk of relapse in the year after drug initiation was significantly higher for interferon-beta, glatiramer acetate, and teriflunomide, compared with dimethyl fumarate.
“Right now, a lot of the data that we have to use in the clinic is based on clinical trials data. That’s often not what we see in the real world, the MS centers, and even the outpatient neurology setting,” Dr. Nicholas said in an interview. “This study is nice just because it points out that when you look at real-world data, it shows, yes, that these drugs work, and that some of the initial benefit for the oral disease-modifying therapies is what we thought. Obviously, we don’t have cross-trial comparisons to make from the clinical trials, so this is real data that we can actually use in our clinic setting.”
The findings are also helpful given changing health care models and ongoing issues with reimbursement and obtaining insurance approval to use various drugs, she added. “These are things that we can show to those payers as to why it’s important that we have these therapies and that we be able to decide as MS specialists what’s going to be best for the patient.
“Right now, the biggest challenge in the MS world is that obviously, as an MS specialist, you have a lot of experience and knowledge. And based on poor prognostic factors, when somebody comes in, you may not want to go with an escalation model [of treatment], where you are starting with something that a payer may think we should start with, an injectable,” Dr. Nicholas added. “Somebody may have more aggressive disease, and maybe you are going to want to start with an oral or an IV drug. But the payers are the ones right now who have the say. So it’s a lot of time and a lot of work [getting insurance approval], and while you are fighting to get what you know your patient needs, your patient’s suffering, accumulating disability, and possibly having more relapses.”
For the study, the investigators analyzed administrative data from the Truven MarketScan Commercial Claims Databases for 2012 through 2014.
Analyses were based on 2,564 patients treated with dimethyl fumarate (brand name Tecfidera), 735 with interferon-beta (Rebif, Avonex, Betaseron, and Extavia), 827 with glatiramer acetate (Copaxone), 417 with teriflunomide (Aubagio), and 461 with fingolimod (Gilenya).
Comparing the year before and the year after drug initiation, only dimethyl fumarate and fingolimod were associated with significant reductions in the annualized relapse rate, according to findings reported in a poster session. The reductions were 33% and 27%, respectively.
In the postinitiation year and with dimethyl fumarate as the comparator, the adjusted incidence rate ratio for relapse was similar for fingolimod but significantly higher for glatiramer acetate (1.28), interferon-beta (1.25), and teriflunomide (1.28).
“I don’t think that these findings are surprising,” Dr. Nicholas said. “I work in a large MS center and I would say this is generally what I see clinically in terms of the effectiveness. So it’s more reassuring to me than anything.”
She acknowledged that safety and tolerability will also come into play when selecting among disease-modifying therapies. “Those data are incredibly important, and we certainly balance that. With a health care claims database, that’s hard data to pull unless you are looking at one specific [adverse effect], but that’s something that needs to be very carefully weighed with the efficacy data for the patient,” she said.
In a companion study also reported in the poster session, the investigators compared the impact of starting the same five drugs on health care costs and utilization.
Results of that study showed that total health care costs rose in the postinitiation year for all five drugs, with the increase ranging from $38,801 for dimethyl fumarate to $52,352 for fingolimod.
However, total nonprescription medical costs decreased across the board, apparently driven by both less use of outpatient services and fewer inpatient hospital stays, with the greatest reduction seen for dimethyl fumarate.
Dr. Nicholas disclosed that she has received research funding from Genzyme, Novartis, Teva, Biogen, and Alexion, and has received consulting and speaking honoraria from Genzyme, Novartis, Teva, Biogen, and Medtronic. The study was supported by Biogen.
VANCOUVER – Dimethyl fumarate and fingolimod appear to have an edge over other disease-modifying therapies for multiple sclerosis (MS) in real-world practice, according to a comparative effectiveness study reported at the annual meeting of the American Academy of Neurology.
Dr. Jacqueline A. Nicholas, a neuroimmunologist and MS specialist with the OhioHealth Multiple Sclerosis Center, Riverside Methodist Hospital, Columbus, and her colleagues analyzed claims data from 5,004 commercially insured adults with MS in the United States who started treatment with any of five oral and injectable disease-modifying therapies.
Findings reported at the meeting showed that dimethyl fumarate netted the greatest reduction in annualized relapse rate, at one-third, followed by fingolimod, at about one-fourth. The adjusted risk of relapse in the year after drug initiation was significantly higher for interferon-beta, glatiramer acetate, and teriflunomide, compared with dimethyl fumarate.
“Right now, a lot of the data that we have to use in the clinic is based on clinical trials data. That’s often not what we see in the real world, the MS centers, and even the outpatient neurology setting,” Dr. Nicholas said in an interview. “This study is nice just because it points out that when you look at real-world data, it shows, yes, that these drugs work, and that some of the initial benefit for the oral disease-modifying therapies is what we thought. Obviously, we don’t have cross-trial comparisons to make from the clinical trials, so this is real data that we can actually use in our clinic setting.”
The findings are also helpful given changing health care models and ongoing issues with reimbursement and obtaining insurance approval to use various drugs, she added. “These are things that we can show to those payers as to why it’s important that we have these therapies and that we be able to decide as MS specialists what’s going to be best for the patient.
“Right now, the biggest challenge in the MS world is that obviously, as an MS specialist, you have a lot of experience and knowledge. And based on poor prognostic factors, when somebody comes in, you may not want to go with an escalation model [of treatment], where you are starting with something that a payer may think we should start with, an injectable,” Dr. Nicholas added. “Somebody may have more aggressive disease, and maybe you are going to want to start with an oral or an IV drug. But the payers are the ones right now who have the say. So it’s a lot of time and a lot of work [getting insurance approval], and while you are fighting to get what you know your patient needs, your patient’s suffering, accumulating disability, and possibly having more relapses.”
For the study, the investigators analyzed administrative data from the Truven MarketScan Commercial Claims Databases for 2012 through 2014.
Analyses were based on 2,564 patients treated with dimethyl fumarate (brand name Tecfidera), 735 with interferon-beta (Rebif, Avonex, Betaseron, and Extavia), 827 with glatiramer acetate (Copaxone), 417 with teriflunomide (Aubagio), and 461 with fingolimod (Gilenya).
Comparing the year before and the year after drug initiation, only dimethyl fumarate and fingolimod were associated with significant reductions in the annualized relapse rate, according to findings reported in a poster session. The reductions were 33% and 27%, respectively.
In the postinitiation year and with dimethyl fumarate as the comparator, the adjusted incidence rate ratio for relapse was similar for fingolimod but significantly higher for glatiramer acetate (1.28), interferon-beta (1.25), and teriflunomide (1.28).
“I don’t think that these findings are surprising,” Dr. Nicholas said. “I work in a large MS center and I would say this is generally what I see clinically in terms of the effectiveness. So it’s more reassuring to me than anything.”
She acknowledged that safety and tolerability will also come into play when selecting among disease-modifying therapies. “Those data are incredibly important, and we certainly balance that. With a health care claims database, that’s hard data to pull unless you are looking at one specific [adverse effect], but that’s something that needs to be very carefully weighed with the efficacy data for the patient,” she said.
In a companion study also reported in the poster session, the investigators compared the impact of starting the same five drugs on health care costs and utilization.
Results of that study showed that total health care costs rose in the postinitiation year for all five drugs, with the increase ranging from $38,801 for dimethyl fumarate to $52,352 for fingolimod.
However, total nonprescription medical costs decreased across the board, apparently driven by both less use of outpatient services and fewer inpatient hospital stays, with the greatest reduction seen for dimethyl fumarate.
Dr. Nicholas disclosed that she has received research funding from Genzyme, Novartis, Teva, Biogen, and Alexion, and has received consulting and speaking honoraria from Genzyme, Novartis, Teva, Biogen, and Medtronic. The study was supported by Biogen.
AT THE AAN 2016 ANNUAL MEETING
Key clinical point: In real-world care, dimethyl fumarate and fingolimod appear more effective than other disease-modifying therapies for MS.
Major finding: Dimethyl fumarate and fingolimod were associated 33% and 27% reductions, respectively, in the annualized relapse rate in the year after initiation of therapy.
Data source: A retrospective cohort study of 5,004 patients with MS treated with five oral or injectable disease-modifying therapies in routine clinical care.
Disclosures: Dr. Nicholas disclosed that she has received research funding from Genzyme; Novartis, the maker of fingolimod (Gilenya); Teva; Biogen, the maker of dimethyl fumarate (Tecfidera); and Alexion. She has received consulting and speaking honoraria from Genzyme, Novartis, Teva, Biogen, and Medtronic. The study was supported by Biogen.