User login
CASE Three hours of pushing
C.A., age 29 years, is 40 weeks’ pregnant with her first child. After an unremarkable pregnancy, she arrives at the hospital for cervical ripening and induction of labor. Oxytocin is given, and labor progresses uneventfully. When C.A.’s cervix is dilated 8 cm, however, labor stalls. The physician orders placement of a pressure catheter and increases the dosage of oxytocin, and the cervix dilates fully. Although C.A. pushes well, the vertex descends only from +1 to +2 station (of 5 stations) after 3 hours.
How would you manage this delivery?
One option in C.A.’s case is operative vaginal delivery using the vacuum extractor, which has replaced the forceps as the most commonly used approach for operative vaginal delivery. Like the forceps, the vacuum extractor has vociferous detractors as well as supporters. Liberal use of cesarean section and questions regarding the safety of operative vaginal delivery vis-à-vis cesarean section have fueled the debate over its role in obstetric practice.
Among the benefits of vacuum extraction are its cost-effectiveness and shorter hospital stay (TABLE 1). It also obviates the need for cesarean section, including repeat cesarean. Risks include an increased incidence of genital tract trauma and a greater risk of fetal subgaleal hemorrhage.
We review 4 critical spheres of concern in regard to vacuum extraction:
- Patient selection
- Informed consent
- Technique
- Documentation
Increased understanding of these aspects of vacuum extraction will improve outcomes for the patient and limit medicolegal risk.
In the case of C.A., the physician offered 3 options:
- Continue maternal expulsive efforts to allow descent
- Attempt delivery by vacuum extraction
- Proceed to cesarean section on the basis of protracted descent.
Risks and benefits were reviewed with the patient, who chose to deliver by cesarean section. A 3,780-g infant in occiput posterior position was delivered safely.
TABLE 1
Delicate balance: Risks and benefits of operative vaginal delivery
| WHO? | BENEFIT | RISK |
|---|---|---|
| Mother | Cost-effective Less blood loss Lower risk of febrile morbidity Maternal preference No need for cesarean section or repeat cesarean Shorter hospitalization and convalescence | Increased incidence of genital tract trauma Possible damage to pelvic floor, with urinary and anal incontinence |
| Fetus | Fewer respiratory difficulties at birth | Increased risk of subgaleal hemorrhage Association with shoulder dystocia |
1. Patient selection: Maternal and fetal indications
Vacuum extraction may be justified for maternal or fetal indications.1,2 Maternal indications include prolongation or arrest of the second stage of labor, or the need to shorten the second stage, for reasons such as maternal cardiac disease, complex congenital cardiovascular disorders, and maternal exhaustion.
No definitive time limit for the second stage of labor
There is more flexibility today than in the past about what constitutes a “safe” length of the second stage. Recommendations concerning when the mother should begin pushing—and for how long—have evolved from a strict time limit to a focus on progression. If the fetal heart rate (FHR) tracing is reassuring, the second stage no longer needs to be limited to 2 or 3 hours. On the contrary, if the patient is still able and willing to push, changes in positioning and further expectant management remain acceptable in contemporary practice.3 Otherwise, a trial of vacuum extraction may be appropriate.
Vacuum extraction is particularly useful when the mother has difficulty pushing because of exhaustion and the fetal head has descended enough that it distends the labia between contractions, as in outlet deliveries.
Fetal indications
Fetal indications for operative vaginal delivery include distress, jeopardy, or a “nonreassuring” FHR tracing. Such a tracing may include late and prolonged decelerations, baseline bradycardia or tachycardia with or without variable decelerations, or, occasionally, a normal baseline rate with diminished variability.
Use vacuum or forceps?
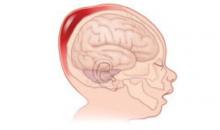
The choice depends on which device would achieve delivery in the safest manner with the lowest risk of fetal injury. With the vacuum, force is exerted directly on the fetal scalp and only secondarily on the fetal skull. This puts fetal vessels that traverse the subgaleal space at risk for injury (FIGURE). With forceps, force is exerted directly on the fetal skull and mitigated by the petrous bone. Little or no force is exerted on the fetal scalp, lessening the risk of traumatic injury such as potentially fatal subgaleal hemorrhage.
Indications and contraindications for vacuum extraction are similar, but not identical, to those for forceps delivery (TABLE 2).2,3 The most important determinant for either device is the experience of the operator. You must be familiar with the instrument and technique before making any attempt to assist delivery. An inability to accurately assess fetal position or station, fetopelvic proportion, adequacy of labor, engagement of the fetal head, or any degree of malpresentation (including minor degrees of deflexion) is a contraindication to a trial of operative vaginal delivery.
Vacuum extraction should be reserved for fetuses at more than 34 weeks’ gestation because of the increased risk of intracranial hemorrhage associated with prematurity.
All decisions involving vacuum extraction should be made with caution. The adequacy of the pelvis, estimated fetal size, and any suggestions of fetopelvic disproportion are of particular significance.3
FIGURE
Subgaleal hemorrhage, a deadly complication
Blood can accumulate in a large potential space between the galea aponeurotica and the periosteum of the cranial bones after vacuum extraction. An infant with subgaleal hemorrhage will exhibit a boggy scalp, with swelling that crosses the suture lines and expands head circumferenceTABLE 2
Factors that predict success—or failure—of vacuum extraction
| When a woman fits overlapping categories, the decision to use vacuum extraction—or not—may be a judgment call* |
| GOOD CANDIDACY |
| Multiparous |
| Term pregnancy |
| Occiput anterior position, well-flexed |
| Wide subpubic arch |
| Compliant |
| MARGINAL CANDIDACY |
| Primiparous |
| Post-term |
| Occiput posterior position |
| Average subpubic arch |
| Gestational diabetes |
| Arrest disorders in second stage |
| POOR CANDIDACY |
| Protraction disorders in second stage |
| Narrow subpubic arch |
| Uncertain position of fetal head |
| Deflexion or asynclitism |
| Anticipated large-for-gestational-age infant |
| Poor maternal compliance |
| * When faced with a good indication in a marginal candidate, we recommend delivery in a “double setup” situation in which preparations are made for both vacuum extraction and cesarean section. If the vacuum can be properly applied, the first application of traction is crucial. We will only proceed if significant descent is achieved. If the fetal head (not the scalp) can be advanced a full station, then we proceed cautiously. If not, ready access to cesarean section allows for completion of the delivery in a timely manner. |
2. Informed consent: Elicit the patient’s desires
Thorough discussion with the patient and her family—to explain the reasoning behind the clinical decision to use the vacuum extractor and delineate the alternatives—is paramount. Moreover, the patient should be encouraged to actively participate in this discussion.
Among the alternatives to vacuum extraction are expectant observation and expedited delivery by cesarean section. Because patients increasingly are requesting elective cesarean section in the absence of obvious obstetric indications, this option should receive extra attention.
Most women still consider vaginal delivery an important milestone of female adulthood. When safety concerns arise and the situation makes vaginal delivery unwise, many women experience disappointment and postpartum depression over their “failed” attempt at vaginal delivery. These perceptions need to be addressed in discussions with the patient.
The risk–benefit equation
Vacuum extraction lessens the risk of maternal lacerations, either of the lower genital tract in the case of obstetric forceps, or of the cervix and lower uterine segment in the case of cesarean section. In addition, vacuum extraction can be performed comfortably in the absence of regional anesthesia.
Avoiding cesarean section can produce multiple benefits
Another maternal benefit of vacuum extraction is the decreased need for cesarean section. A reduction in the primary cesarean rate also lowers the need for repeat cesarean section, which can be more technically challenging than primary C-section due to the presence of dense scar tissue and intra-abdominal adhesions. Cesarean section also increases the risk of placenta accreta, increta, or percreta in subsequent pregnancies. These complications increase the likelihood of emergency hysterectomy, massive blood loss, and serious maternal morbidity and mortality.
Even in the absence of placenta accreta, both primary and repeat cesarean sections raise the risk of hemorrhage and febrile morbidity, prolong convalescence, and increase cost, compared with vaginal delivery. For these reasons, avoiding primary cesarean section can obviate the need for multiple surgical procedures and their attendant risks. The degree to which these factors favor vaginal delivery over cesarean section is subject to debate.
Maternal risks include pelvic floor trauma
Both vacuum extraction and forceps delivery increase the risk of anal sphincter injury and can impair fecal continence.4 Both methods also appear to increase trauma to the genital tract in comparison with spontaneous delivery and may predispose the woman to pelvic floor dysfunction, including urinary and anal incontinence.5-10 However, anal sphincter trauma was less frequent after vacuum extraction than after forceps delivery.1
Other maternal injuries associated with vacuum extraction include perineal lacerations and injuries to the vulva, vagina, and cervix. Vacuum extraction also has been implicated as a significant risk factor for postpartum hemorrhage11 and genital-tract infection.1
Fewer neonatal respiratory problems with vaginal delivery
Compared with cesarean section, vaginal delivery is thought to diminish the risk of intrapartum aspiration and respiratory problems in the newborn. It also may facilitate the transition from fetal to neonatal circulation and reduce the need for immediate resuscitation at birth.
Neonatal risks include soft-tissue injury and potential hemorrhage
Infants delivered by vacuum extraction have a significantly higher rate of intracranial hemorrhage, brachial plexus injuries, convulsions, central nervous system depression, and the need for mechanical ventilation, compared with spontaneously delivered infants (TABLE 3).12,13
Although vacuum extraction is associated with a wide range of soft tissue injuries, they are often less serious than the fetal scalp injuries associated with obstetric forceps. Cup marks, bruising, and minor lacerations of the scalp and caput succedaneum are common fetal injuries, although the majority resolve without apparent sequelae.14
Subgaleal hemorrhage is the most serious neonatal complication of vacuum extraction, occurring in 1% to 3.8% of vacuum extractions (FIGURE).15 It coexists with neonatal coagulopathy in 19% to 29% of newborns16 and increases the risk of progression to hemorrhagic shock and death. Subgaleal hemorrhage has a mortality rate ranging from 2.7% to 22.8%.15-17
Cephalhematoma is another complication associated with vacuum extraction. It involves an accumulation of blood beneath the periosteum of a cranial bone (usually the parietal bone), and it almost always resolves spontaneously. The incidence of cephalhematoma varies. It is significantly more common in deliveries involving vacuum extraction (9.8%) than in forceps deliveries (4.1%).18 Its incidence increases with the length of time the vacuum cup is applied and with paramedian application.18
Intracranial hemorrhage occurs in 1 of 860 vacuum extractions, 1 of 664 forceps deliveries, 1 of 954 cesarean deliveries, and 1 of 1,900 spontaneous deliveries.12 Subdural hemorrhage is the most common form of intracranial hemorrhage and is almost invariably the result of birth trauma. However, asymptomatic subdural hematoma occurs in up to 6.1% of uncomplicated vaginal deliveries.19
Other, less common types of intracranial hemorrhage, such as subarachnoid, intraventricular, and intraparenchymal hemorrhage, have a more complex etiology, which includes birth asphyxia, hemorrhagic diathesis, infection, and vascular abnormalities.20
Retinal hemorrhage also may occur after vacuum extraction, with an incidence of 49% to 77.8%, compared with 30.3% after forceps delivery, 30.4% after normal vaginal delivery, and 8.3% after cesarean delivery.21 It generally resolves spontaneously without any permanent damage.22
TABLE 3
Vacuum extraction can injure the fetus
| DIRECT INJURY |
| Cephalhematoma |
| Intracranial hemorrhage (parenchymal, subdural, intraventricular, subarachnoid) |
| Nerve injury |
| Scalp laceration, abrasion, ecchymoses, necrosis |
| Skull fracture |
| Subgaleal hemorrhage |
| INDIRECT INJURY |
| Anemia, hyperbilirubinemia |
| Brachial plexus injury |
| Scalp infection or abscess |
| SOURCE: O’Grady et al31 |
Shoulder dystocia and brachial plexus palsy
Vacuum extraction also is associated with shoulder dystocia and brachial plexus palsy, although the primary risk factor for these complications is thought to be increased fetal size.23-25 The incidence of shoulder dystocia with vacuum extraction is 3.5%, compared with 1.5% for forceps delivery.25
The risk of brachial plexus palsy also increases with vacuum extraction, especially as the duration of the procedure increases.25
Less common complications associated with vacuum extraction are skull fractures, fetal hemorrhage from bleeding at the site of scalp electrodes, sepsis originating from infected scalp trauma, and corneal injury.
No long-term impairment
Long-term outcome studies of children delivered by vacuum extraction show no differences in physical or cognitive functioning or intelligence scores, compared with other modes of delivery.26
3. Technique: Create conditions that ensure success
Certain prerequisites to vacuum extraction can assure successful application and strict adherence to protocol. These prerequisites include having an appropriate indication, thorough informed consent, proper maternal positioning, adequate anesthesia, and knowledge of fetal position and station (TABLE 4).1 These objectives can be accomplished in the following steps:
- After an informed consent discussion, assess maternal positioning and repeat the pelvic exam. Also ascertain the adequacy of anesthesia. Insert a bladder catheter.
- Perform a “ghost” trial of vacuum extraction to visualize the procedure before the actual attempt.
- Test the function of the vacuum.
- Lubricate the vacuum cup with surgical soap or gel, insert it into the vagina, and maneuver it onto the fetal head. Place the vacuum extractor over the sagittal suture about 6 cm distal to the anterior fontanel and 2 cm proximal to the posterior fontanel. (The illustration on page 74 demonstrates positioning.) Apply a small degree of vacuum (approximately 20 mm Hg). Double-check application.
- Gradually apply full vacuum (550–600 mm Hg, depending on cup size), allowing the scalp to mold to the extractor cup.
- Apply 2-handed traction in concert with uterine contractions and supplemented by maternal pushing. Assuming there is no loss of vacuum (“pop-off” of the cup), the initial traction effort should produce a gain in station. If a “pop-off” occurs, a single additional attempt at delivery may be warranted.
- As the head crowns, perform episiotomy as needed and slowly deliver the fetal head. Remove the vacuum cup.
- After delivery of the placenta, inspect the vagina, cervix, and perineum closely.
- Dictate a full operative note and annotate the delivery in the chart. See the section on documentation, below.
Vacuum extraction may fail for a number of reasons (TABLE 5).
TABLE 4
Perform these predelivery checks before applying traction
| Is anesthesia adequate? Is maternal positioning correct? |
| Is the bladder empty? |
| Is the fetus in the proper attitude (flexion)? |
| Is fetal status reassuring? |
Is the vacuum properly applied?
|
| Has the patient been instructed on when and how long to push? |
| Are the proposed maneuvers appropriate? |
TABLE 5
Why might vacuum extraction fail?
| INSTRUMENT-RELATED |
| Pump failure |
| Vacuum leak |
| TECHNIQUE-RELATED |
| Failure to encourage maternal valsalva with traction efforts |
| Inappropriate intensity of traction |
| Incorrect axis of traction |
| Maternal tissue trapped beneath vacuum cup |
| Poor cup position |
| OBSTETRIC CONDITIONS |
Congenital anomaly
|
| Fetal macrosomia |
| Incomplete cervical dilation |
Position and attitude problems
|
| Unappreciated cephalopelvic disproportion |
| SOURCE: Modified from Plauche et al32 |
Most important variable: Cup placement
The single most critical step in vacuum extraction is placement of the cup. It should be applied at the point of maximum fetal cranial flexion, which is proximal to the leading edge of the posterior fontanel.
Once full vacuum is achieved, encourage the mother to push with the next contraction, and apply steady traction in concert with her efforts.
The initial application of traction should be directed to maintain proper flexion of the fetal head, and should bring about descent of the fetal head. If there is no descent with the first application of traction, and correct technique and cup placement have been applied, abandon operative vaginal delivery (TABLE 6).
Do not make a further attempt to deliver the child using forceps, as the risk of intracranial hemorrhage appears to be highest in infants delivered using a combination of vacuum extraction and forceps.
TABLE 6
Repeat traction efforts reap a diminishing return
| NUMBER OF TRACTION EFFORTS | SUCCESS RATE | |
|---|---|---|
| VACUUM EXTRACTION (N=433) | FORCEPS (N=555) | |
| 1 or 2 | 68.4% | 38.4% |
| 3 or 4 | 24.9% | 48.6% |
| 5 or more | 6.7% | 12.9% |
| Adapted from Sjostedt33 | ||
4. Documentation: The chart is the most important witness
The value of complete and contemporaneous notation cannot be overstated. The patient’s chart is the permanent repository of the record of delivery. It is without doubt the most important witness to the event and should be treated as such. Include a dictated operative note as well as notation in the chart itself. Notes should be legible and properly dated, with the time of day indicated.
When operative vaginal delivery is performed, record the following:
- indication for the procedure
- course of labor
- anesthesia
- personnel present
- instruments used
- position and station of the fetal head
- force and duration of traction
- complications, including how they were recognized and managed
- immediate condition of the newborn and all steps taken in resuscitation.
Operative vaginal delivery is no newcomer to obstetrics. Hindu writings from about 1000 BC, and Hippocrates’ own musings from the fifth century BC, describe instruments and techniques to combat arrested labor and salvage the lives of both mother and child.27 Crude forceps were described by the Muslim physician Albucasis in the 11th century.27
Before the advent of safe cesarean section, many maternal lives were no doubt saved by these instruments and techniques. Unfortunately, destruction of the fetus and maternal death were frequent outcomes of operative vaginal delivery by forceps before the 20th century.28
As for vacuum extraction in particular, the idea of attaching a device to the fetal head to aid in delivery is credited to Arnett, a 19th century surgeon and inventor, who envisioned the “pneumatic tractor.”29
In 1957, Malmstrom reintroduced the vacuum as an aid in delivery, designing a rigid cup that was connected by rubber tubing to a vacuum source.30 This allowed the separation of the pump mechanism from the cup and made for easier application.
Most recently, Kobayashi developed the soft-cup design, a low-cost flexible plastic alternative that allows for a disposable instrument.31
Minimizing medicolegal risk
The best way to prevent an accusation of medical malpractice is to develop strong clinical and interpersonal skills. These simple, intuitive suggestions may help:
- Understand the role of operative vaginal delivery in current practice.
- Develop a simple and interactive discussion model for use in labor and delivery with the patient and her family.
- Consider a woman’s preferences for delivery.
- Know the indications and contraindications for vacuum extraction.
- Use the checks and safeguards listed under 3. Technique: Create conditions that ensure success.
- Perform vacuum extraction in the cesarean section room. Stop the procedure at once if any problem arises, and proceed to cesarean delivery.
- Make all chart notations completely legible, and add dictated notes.
If you are a new physician or lack significant experience with vacuum extraction, ask for input, supervision, and education from more experienced clinicians. Also make it a point to ask about department guidelines and review the credentialing process. Once you become adept at vacuum extraction, mentor more junior colleagues.
Two critical concerns
When contemplating vacuum-assisted delivery, 2 risks are paramount:
- failure of the vacuum extractor to achieve delivery
- the potential for fetal and maternal injury.
Training must ensure appropriate case selection and technique. Vacuum extraction must be performed with the same precision and care used with forceps. If application of the device is incorrect, or if there is a wrong direction of traction, excessive traction, or traction in the presence of disproportion, the cup will slip or pop off, and vacuum delivery will fail, with the potential for traumatic fetal injury.
All risks must be discussed with the patient to fulfill informed consent, and the risks and benefits of alternative treatments should be part of the discussion. Active participation, in considering how best to approach delivery, is required of all parties concerned.
The vacuum extractor can be a useful adjunct in certain circumstances, and its use has become widespread in American delivery suites. As with the obstetric forceps, which largely antedated its use, the vacuum extractor can lessen the overall risks of childbirth for both mother and infant.
The authors report no financial relationships relevant to this article.
1. O’Grady JP, Gimovsky ML, McIlhargie CJ, eds. Operative Obstetrics. Pearl River, NY: Parthenon Publishing; 1995.
2. Johanson RB, Menon BKV. Vacuum extraction versus forceps for assisted vaginal delivery. Cochrane Database Syst Rev. 2000;(2):CD000224.-
3. Bloom SL, Casey BM, Schaffer JL, et al. Pushing in the second stage of labor. Am J Obstet Gynecol 2006;194:10-13.
4. Operative vaginal delivery. ACOG Practice Bulletin #17. Washington, DC: American College of Obstetricians and Gynecologists; June 2000.
5. Power D, Fitzpatrick M, O’Herlihy C. Obstetric anal sphincter injury: how to avoid, how to repair: a literature review. J Fam Pract 2006;55:193-200.
6. Chaliha C, Kalia V, Stanton S, et al. Antenatal prediction of postpartum urinary and fecal incontinence. Obstet Gynecol 1999;94:689-694.
7. Bofill JA, Rust OA, Schorr SJ, et al. A randomized prospective trial of the obstetric forceps versus the M-cup vacuum extractor. Am J Obstet Gynecol 1996;175:1325-1330.
8. Salamalekis E, Loghis C, Pyrgiotis E, et al. Soft cup vacuum extractor versus forceps delivery. J Obstet Gynecol. 1995;15:245-246.
9. Zetterstrom JP, Lopez A, Anzen B, et al. Anal incontinence after vaginal delivery: a prospective study in primiparous women. Br J Obstet Gynaecol. 1999;106:324-330.
10. Johanson RB, Heycock E, Carter J, et al. Maternal and child health after assisted vaginal delivery: five-year follow up of a randomized controlled study comparing forceps and ventouse. Br J Obstet Gynaecol. 1999;106:544-549
11. Faltin DL, Otero M, Petignat P, et al. Women’s health 18 years after rupture of the anal sphincter during childbirth: I. Fecal incontinence. Am J Obstet Gynecol. 2006;194:1255-1259.
12. Plauche WC. Fetal cranial injuries related to delivery with the Malmsträm vacuum extractor. Obstet Gynecol. 1979;53:750-757.
13. Towner D, Castro MA, Eby-Wilkens E, et al. Effect of mode of delivery in nulliparous women on neonatal intracranial injury. N Engl J Med. 1999;341:1709-1714.
14. Sheiner E, Sarid L, Levy A, et al. Obstetric risk factors and outcome of pregnancies complicated with early postpartum hemorrhage: a population-based study. J Matern Fetal Neonatal Med. 2005;18:149-154.
15. Johanson R. Choice of instrument for vaginal delivery. Curr Opin Obstet Gynecol. 1997;9:361-365.
16. Chadwick LM, Pemberton PJ, Kurinczuk JJ. Neonatal subgaleal hematoma: associated risk factors, complications, and outcome. J Pediatr Child Health. 1996;32:228-232.
17. Ng PC, Siu YK, Lewindon PJ. Subaponeurotic hemorrhage in the 1990s: a 3-year surveillance. Acta Pediatr. 1995;84:1065-1069
18. Bofill JA, Rust OA, Devidas M, et al. Neonatal cephalohematoma from vacuum extraction. J Reprod Med. 1997;42:565-569.
19. Doumouchtsis SK, Arulkumaran S. Head injuries after instrumental vaginal deliveries. Curr Opin Obstet Gynecol. 2006;18:129-134.
20. Govaert P. Cranial Hemorrhage in the Term Newborn Infant. London: Mac Keith Press; 1993.
21. Hughes LA, May K, Talbot JF, Parsons MA. Incidence, distribution, and duration of birth-related retinal hemorrhages: a prospective study. J AAPOS. 2006;10:102-106.
22. Sheiner E, Levy A, Hershkovitz R, et al. Determining factors associated with shoulder dystocia: a population-based study. Eur J Obstet Gynecol Reprod Biol. 2006;126:11-15.
23. Baskett TF, Allen AC. Perinatal implications of shoulder dystocia. Obstet Gynecol. 1995;86:15-18.
24. Mollberg M, Hagerg H, Bager B, et al. Risk factors for obstetric brachial plexus palsy among neonates delivered by vacuum extraction. Obstet Gynecol. 2005;106:913-918.
25. Caughey AB, Sandberg PL, Alantnik MG, et al. Forceps compared with vacuum: rates of neonatal and maternal morbidity. Obstet Gynecol. 2005;106:908-912.
26. Ngan HYS, Miu P, Ko L, et al. Long-term neurological sequelae following vacuum extractor delivery. Aust NZ J Obstet Gynecol. 1990;30:111-114.
27. Lyons AS, Petrucelli RJ. Medicine: An Illustrated History. New York: Harry N Abrams; 1978.
28. Speert H. Obstetric and Gynecologic Milestones Illustrated. Pearl River, NY: Parthenon Publishing; 1996.
29. Arnett N. Elements of Physics or Natural Philosophy, General and Medical, Explained Independently of Technical Mathematics and Containing New Disquisitions and Practical Suggestions. 2nd ed. Philadelphia: Carney and Lea; 1831.
30. Malmstrom T. The vacuum extractor, an obstetrical instrument. I. Acta Obstet Gynecol Scand. 1957;36(suppl 3):5-50.
31. O’Grady JP, Gimovsky ML, McIlhargie CJ. Vacuum Extraction in Modern Obstetric Practice. Pearl River, NY: Parthenon Publishing; 1995.
32. Plauche WC, Morrison JC, O’Sullivan MJ. Surgical Obstetrics. Philadelphia: WB Saunders; 1992.
33. Sjostedt JE. The vacuum extractor and forceps in obstetrics: a clinical study. Acta Obstet Gynecol Scand. 1967;48:638-639.
CASE Three hours of pushing
C.A., age 29 years, is 40 weeks’ pregnant with her first child. After an unremarkable pregnancy, she arrives at the hospital for cervical ripening and induction of labor. Oxytocin is given, and labor progresses uneventfully. When C.A.’s cervix is dilated 8 cm, however, labor stalls. The physician orders placement of a pressure catheter and increases the dosage of oxytocin, and the cervix dilates fully. Although C.A. pushes well, the vertex descends only from +1 to +2 station (of 5 stations) after 3 hours.
How would you manage this delivery?
One option in C.A.’s case is operative vaginal delivery using the vacuum extractor, which has replaced the forceps as the most commonly used approach for operative vaginal delivery. Like the forceps, the vacuum extractor has vociferous detractors as well as supporters. Liberal use of cesarean section and questions regarding the safety of operative vaginal delivery vis-à-vis cesarean section have fueled the debate over its role in obstetric practice.
Among the benefits of vacuum extraction are its cost-effectiveness and shorter hospital stay (TABLE 1). It also obviates the need for cesarean section, including repeat cesarean. Risks include an increased incidence of genital tract trauma and a greater risk of fetal subgaleal hemorrhage.
We review 4 critical spheres of concern in regard to vacuum extraction:
- Patient selection
- Informed consent
- Technique
- Documentation
Increased understanding of these aspects of vacuum extraction will improve outcomes for the patient and limit medicolegal risk.
In the case of C.A., the physician offered 3 options:
- Continue maternal expulsive efforts to allow descent
- Attempt delivery by vacuum extraction
- Proceed to cesarean section on the basis of protracted descent.
Risks and benefits were reviewed with the patient, who chose to deliver by cesarean section. A 3,780-g infant in occiput posterior position was delivered safely.
TABLE 1
Delicate balance: Risks and benefits of operative vaginal delivery
| WHO? | BENEFIT | RISK |
|---|---|---|
| Mother | Cost-effective Less blood loss Lower risk of febrile morbidity Maternal preference No need for cesarean section or repeat cesarean Shorter hospitalization and convalescence | Increased incidence of genital tract trauma Possible damage to pelvic floor, with urinary and anal incontinence |
| Fetus | Fewer respiratory difficulties at birth | Increased risk of subgaleal hemorrhage Association with shoulder dystocia |
1. Patient selection: Maternal and fetal indications
Vacuum extraction may be justified for maternal or fetal indications.1,2 Maternal indications include prolongation or arrest of the second stage of labor, or the need to shorten the second stage, for reasons such as maternal cardiac disease, complex congenital cardiovascular disorders, and maternal exhaustion.
No definitive time limit for the second stage of labor
There is more flexibility today than in the past about what constitutes a “safe” length of the second stage. Recommendations concerning when the mother should begin pushing—and for how long—have evolved from a strict time limit to a focus on progression. If the fetal heart rate (FHR) tracing is reassuring, the second stage no longer needs to be limited to 2 or 3 hours. On the contrary, if the patient is still able and willing to push, changes in positioning and further expectant management remain acceptable in contemporary practice.3 Otherwise, a trial of vacuum extraction may be appropriate.
Vacuum extraction is particularly useful when the mother has difficulty pushing because of exhaustion and the fetal head has descended enough that it distends the labia between contractions, as in outlet deliveries.
Fetal indications
Fetal indications for operative vaginal delivery include distress, jeopardy, or a “nonreassuring” FHR tracing. Such a tracing may include late and prolonged decelerations, baseline bradycardia or tachycardia with or without variable decelerations, or, occasionally, a normal baseline rate with diminished variability.
Use vacuum or forceps?
The choice depends on which device would achieve delivery in the safest manner with the lowest risk of fetal injury. With the vacuum, force is exerted directly on the fetal scalp and only secondarily on the fetal skull. This puts fetal vessels that traverse the subgaleal space at risk for injury (FIGURE). With forceps, force is exerted directly on the fetal skull and mitigated by the petrous bone. Little or no force is exerted on the fetal scalp, lessening the risk of traumatic injury such as potentially fatal subgaleal hemorrhage.
Indications and contraindications for vacuum extraction are similar, but not identical, to those for forceps delivery (TABLE 2).2,3 The most important determinant for either device is the experience of the operator. You must be familiar with the instrument and technique before making any attempt to assist delivery. An inability to accurately assess fetal position or station, fetopelvic proportion, adequacy of labor, engagement of the fetal head, or any degree of malpresentation (including minor degrees of deflexion) is a contraindication to a trial of operative vaginal delivery.
Vacuum extraction should be reserved for fetuses at more than 34 weeks’ gestation because of the increased risk of intracranial hemorrhage associated with prematurity.
All decisions involving vacuum extraction should be made with caution. The adequacy of the pelvis, estimated fetal size, and any suggestions of fetopelvic disproportion are of particular significance.3
FIGURE
Subgaleal hemorrhage, a deadly complication
Blood can accumulate in a large potential space between the galea aponeurotica and the periosteum of the cranial bones after vacuum extraction. An infant with subgaleal hemorrhage will exhibit a boggy scalp, with swelling that crosses the suture lines and expands head circumferenceTABLE 2
Factors that predict success—or failure—of vacuum extraction
| When a woman fits overlapping categories, the decision to use vacuum extraction—or not—may be a judgment call* |
| GOOD CANDIDACY |
| Multiparous |
| Term pregnancy |
| Occiput anterior position, well-flexed |
| Wide subpubic arch |
| Compliant |
| MARGINAL CANDIDACY |
| Primiparous |
| Post-term |
| Occiput posterior position |
| Average subpubic arch |
| Gestational diabetes |
| Arrest disorders in second stage |
| POOR CANDIDACY |
| Protraction disorders in second stage |
| Narrow subpubic arch |
| Uncertain position of fetal head |
| Deflexion or asynclitism |
| Anticipated large-for-gestational-age infant |
| Poor maternal compliance |
| * When faced with a good indication in a marginal candidate, we recommend delivery in a “double setup” situation in which preparations are made for both vacuum extraction and cesarean section. If the vacuum can be properly applied, the first application of traction is crucial. We will only proceed if significant descent is achieved. If the fetal head (not the scalp) can be advanced a full station, then we proceed cautiously. If not, ready access to cesarean section allows for completion of the delivery in a timely manner. |
2. Informed consent: Elicit the patient’s desires
Thorough discussion with the patient and her family—to explain the reasoning behind the clinical decision to use the vacuum extractor and delineate the alternatives—is paramount. Moreover, the patient should be encouraged to actively participate in this discussion.
Among the alternatives to vacuum extraction are expectant observation and expedited delivery by cesarean section. Because patients increasingly are requesting elective cesarean section in the absence of obvious obstetric indications, this option should receive extra attention.
Most women still consider vaginal delivery an important milestone of female adulthood. When safety concerns arise and the situation makes vaginal delivery unwise, many women experience disappointment and postpartum depression over their “failed” attempt at vaginal delivery. These perceptions need to be addressed in discussions with the patient.
The risk–benefit equation
Vacuum extraction lessens the risk of maternal lacerations, either of the lower genital tract in the case of obstetric forceps, or of the cervix and lower uterine segment in the case of cesarean section. In addition, vacuum extraction can be performed comfortably in the absence of regional anesthesia.
Avoiding cesarean section can produce multiple benefits
Another maternal benefit of vacuum extraction is the decreased need for cesarean section. A reduction in the primary cesarean rate also lowers the need for repeat cesarean section, which can be more technically challenging than primary C-section due to the presence of dense scar tissue and intra-abdominal adhesions. Cesarean section also increases the risk of placenta accreta, increta, or percreta in subsequent pregnancies. These complications increase the likelihood of emergency hysterectomy, massive blood loss, and serious maternal morbidity and mortality.
Even in the absence of placenta accreta, both primary and repeat cesarean sections raise the risk of hemorrhage and febrile morbidity, prolong convalescence, and increase cost, compared with vaginal delivery. For these reasons, avoiding primary cesarean section can obviate the need for multiple surgical procedures and their attendant risks. The degree to which these factors favor vaginal delivery over cesarean section is subject to debate.
Maternal risks include pelvic floor trauma
Both vacuum extraction and forceps delivery increase the risk of anal sphincter injury and can impair fecal continence.4 Both methods also appear to increase trauma to the genital tract in comparison with spontaneous delivery and may predispose the woman to pelvic floor dysfunction, including urinary and anal incontinence.5-10 However, anal sphincter trauma was less frequent after vacuum extraction than after forceps delivery.1
Other maternal injuries associated with vacuum extraction include perineal lacerations and injuries to the vulva, vagina, and cervix. Vacuum extraction also has been implicated as a significant risk factor for postpartum hemorrhage11 and genital-tract infection.1
Fewer neonatal respiratory problems with vaginal delivery
Compared with cesarean section, vaginal delivery is thought to diminish the risk of intrapartum aspiration and respiratory problems in the newborn. It also may facilitate the transition from fetal to neonatal circulation and reduce the need for immediate resuscitation at birth.
Neonatal risks include soft-tissue injury and potential hemorrhage
Infants delivered by vacuum extraction have a significantly higher rate of intracranial hemorrhage, brachial plexus injuries, convulsions, central nervous system depression, and the need for mechanical ventilation, compared with spontaneously delivered infants (TABLE 3).12,13
Although vacuum extraction is associated with a wide range of soft tissue injuries, they are often less serious than the fetal scalp injuries associated with obstetric forceps. Cup marks, bruising, and minor lacerations of the scalp and caput succedaneum are common fetal injuries, although the majority resolve without apparent sequelae.14
Subgaleal hemorrhage is the most serious neonatal complication of vacuum extraction, occurring in 1% to 3.8% of vacuum extractions (FIGURE).15 It coexists with neonatal coagulopathy in 19% to 29% of newborns16 and increases the risk of progression to hemorrhagic shock and death. Subgaleal hemorrhage has a mortality rate ranging from 2.7% to 22.8%.15-17
Cephalhematoma is another complication associated with vacuum extraction. It involves an accumulation of blood beneath the periosteum of a cranial bone (usually the parietal bone), and it almost always resolves spontaneously. The incidence of cephalhematoma varies. It is significantly more common in deliveries involving vacuum extraction (9.8%) than in forceps deliveries (4.1%).18 Its incidence increases with the length of time the vacuum cup is applied and with paramedian application.18
Intracranial hemorrhage occurs in 1 of 860 vacuum extractions, 1 of 664 forceps deliveries, 1 of 954 cesarean deliveries, and 1 of 1,900 spontaneous deliveries.12 Subdural hemorrhage is the most common form of intracranial hemorrhage and is almost invariably the result of birth trauma. However, asymptomatic subdural hematoma occurs in up to 6.1% of uncomplicated vaginal deliveries.19
Other, less common types of intracranial hemorrhage, such as subarachnoid, intraventricular, and intraparenchymal hemorrhage, have a more complex etiology, which includes birth asphyxia, hemorrhagic diathesis, infection, and vascular abnormalities.20
Retinal hemorrhage also may occur after vacuum extraction, with an incidence of 49% to 77.8%, compared with 30.3% after forceps delivery, 30.4% after normal vaginal delivery, and 8.3% after cesarean delivery.21 It generally resolves spontaneously without any permanent damage.22
TABLE 3
Vacuum extraction can injure the fetus
| DIRECT INJURY |
| Cephalhematoma |
| Intracranial hemorrhage (parenchymal, subdural, intraventricular, subarachnoid) |
| Nerve injury |
| Scalp laceration, abrasion, ecchymoses, necrosis |
| Skull fracture |
| Subgaleal hemorrhage |
| INDIRECT INJURY |
| Anemia, hyperbilirubinemia |
| Brachial plexus injury |
| Scalp infection or abscess |
| SOURCE: O’Grady et al31 |
Shoulder dystocia and brachial plexus palsy
Vacuum extraction also is associated with shoulder dystocia and brachial plexus palsy, although the primary risk factor for these complications is thought to be increased fetal size.23-25 The incidence of shoulder dystocia with vacuum extraction is 3.5%, compared with 1.5% for forceps delivery.25
The risk of brachial plexus palsy also increases with vacuum extraction, especially as the duration of the procedure increases.25
Less common complications associated with vacuum extraction are skull fractures, fetal hemorrhage from bleeding at the site of scalp electrodes, sepsis originating from infected scalp trauma, and corneal injury.
No long-term impairment
Long-term outcome studies of children delivered by vacuum extraction show no differences in physical or cognitive functioning or intelligence scores, compared with other modes of delivery.26
3. Technique: Create conditions that ensure success
Certain prerequisites to vacuum extraction can assure successful application and strict adherence to protocol. These prerequisites include having an appropriate indication, thorough informed consent, proper maternal positioning, adequate anesthesia, and knowledge of fetal position and station (TABLE 4).1 These objectives can be accomplished in the following steps:
- After an informed consent discussion, assess maternal positioning and repeat the pelvic exam. Also ascertain the adequacy of anesthesia. Insert a bladder catheter.
- Perform a “ghost” trial of vacuum extraction to visualize the procedure before the actual attempt.
- Test the function of the vacuum.
- Lubricate the vacuum cup with surgical soap or gel, insert it into the vagina, and maneuver it onto the fetal head. Place the vacuum extractor over the sagittal suture about 6 cm distal to the anterior fontanel and 2 cm proximal to the posterior fontanel. (The illustration on page 74 demonstrates positioning.) Apply a small degree of vacuum (approximately 20 mm Hg). Double-check application.
- Gradually apply full vacuum (550–600 mm Hg, depending on cup size), allowing the scalp to mold to the extractor cup.
- Apply 2-handed traction in concert with uterine contractions and supplemented by maternal pushing. Assuming there is no loss of vacuum (“pop-off” of the cup), the initial traction effort should produce a gain in station. If a “pop-off” occurs, a single additional attempt at delivery may be warranted.
- As the head crowns, perform episiotomy as needed and slowly deliver the fetal head. Remove the vacuum cup.
- After delivery of the placenta, inspect the vagina, cervix, and perineum closely.
- Dictate a full operative note and annotate the delivery in the chart. See the section on documentation, below.
Vacuum extraction may fail for a number of reasons (TABLE 5).
TABLE 4
Perform these predelivery checks before applying traction
| Is anesthesia adequate? Is maternal positioning correct? |
| Is the bladder empty? |
| Is the fetus in the proper attitude (flexion)? |
| Is fetal status reassuring? |
Is the vacuum properly applied?
|
| Has the patient been instructed on when and how long to push? |
| Are the proposed maneuvers appropriate? |
TABLE 5
Why might vacuum extraction fail?
| INSTRUMENT-RELATED |
| Pump failure |
| Vacuum leak |
| TECHNIQUE-RELATED |
| Failure to encourage maternal valsalva with traction efforts |
| Inappropriate intensity of traction |
| Incorrect axis of traction |
| Maternal tissue trapped beneath vacuum cup |
| Poor cup position |
| OBSTETRIC CONDITIONS |
Congenital anomaly
|
| Fetal macrosomia |
| Incomplete cervical dilation |
Position and attitude problems
|
| Unappreciated cephalopelvic disproportion |
| SOURCE: Modified from Plauche et al32 |
Most important variable: Cup placement
The single most critical step in vacuum extraction is placement of the cup. It should be applied at the point of maximum fetal cranial flexion, which is proximal to the leading edge of the posterior fontanel.
Once full vacuum is achieved, encourage the mother to push with the next contraction, and apply steady traction in concert with her efforts.
The initial application of traction should be directed to maintain proper flexion of the fetal head, and should bring about descent of the fetal head. If there is no descent with the first application of traction, and correct technique and cup placement have been applied, abandon operative vaginal delivery (TABLE 6).
Do not make a further attempt to deliver the child using forceps, as the risk of intracranial hemorrhage appears to be highest in infants delivered using a combination of vacuum extraction and forceps.
TABLE 6
Repeat traction efforts reap a diminishing return
| NUMBER OF TRACTION EFFORTS | SUCCESS RATE | |
|---|---|---|
| VACUUM EXTRACTION (N=433) | FORCEPS (N=555) | |
| 1 or 2 | 68.4% | 38.4% |
| 3 or 4 | 24.9% | 48.6% |
| 5 or more | 6.7% | 12.9% |
| Adapted from Sjostedt33 | ||
4. Documentation: The chart is the most important witness
The value of complete and contemporaneous notation cannot be overstated. The patient’s chart is the permanent repository of the record of delivery. It is without doubt the most important witness to the event and should be treated as such. Include a dictated operative note as well as notation in the chart itself. Notes should be legible and properly dated, with the time of day indicated.
When operative vaginal delivery is performed, record the following:
- indication for the procedure
- course of labor
- anesthesia
- personnel present
- instruments used
- position and station of the fetal head
- force and duration of traction
- complications, including how they were recognized and managed
- immediate condition of the newborn and all steps taken in resuscitation.
Operative vaginal delivery is no newcomer to obstetrics. Hindu writings from about 1000 BC, and Hippocrates’ own musings from the fifth century BC, describe instruments and techniques to combat arrested labor and salvage the lives of both mother and child.27 Crude forceps were described by the Muslim physician Albucasis in the 11th century.27
Before the advent of safe cesarean section, many maternal lives were no doubt saved by these instruments and techniques. Unfortunately, destruction of the fetus and maternal death were frequent outcomes of operative vaginal delivery by forceps before the 20th century.28
As for vacuum extraction in particular, the idea of attaching a device to the fetal head to aid in delivery is credited to Arnett, a 19th century surgeon and inventor, who envisioned the “pneumatic tractor.”29
In 1957, Malmstrom reintroduced the vacuum as an aid in delivery, designing a rigid cup that was connected by rubber tubing to a vacuum source.30 This allowed the separation of the pump mechanism from the cup and made for easier application.
Most recently, Kobayashi developed the soft-cup design, a low-cost flexible plastic alternative that allows for a disposable instrument.31
Minimizing medicolegal risk
The best way to prevent an accusation of medical malpractice is to develop strong clinical and interpersonal skills. These simple, intuitive suggestions may help:
- Understand the role of operative vaginal delivery in current practice.
- Develop a simple and interactive discussion model for use in labor and delivery with the patient and her family.
- Consider a woman’s preferences for delivery.
- Know the indications and contraindications for vacuum extraction.
- Use the checks and safeguards listed under 3. Technique: Create conditions that ensure success.
- Perform vacuum extraction in the cesarean section room. Stop the procedure at once if any problem arises, and proceed to cesarean delivery.
- Make all chart notations completely legible, and add dictated notes.
If you are a new physician or lack significant experience with vacuum extraction, ask for input, supervision, and education from more experienced clinicians. Also make it a point to ask about department guidelines and review the credentialing process. Once you become adept at vacuum extraction, mentor more junior colleagues.
Two critical concerns
When contemplating vacuum-assisted delivery, 2 risks are paramount:
- failure of the vacuum extractor to achieve delivery
- the potential for fetal and maternal injury.
Training must ensure appropriate case selection and technique. Vacuum extraction must be performed with the same precision and care used with forceps. If application of the device is incorrect, or if there is a wrong direction of traction, excessive traction, or traction in the presence of disproportion, the cup will slip or pop off, and vacuum delivery will fail, with the potential for traumatic fetal injury.
All risks must be discussed with the patient to fulfill informed consent, and the risks and benefits of alternative treatments should be part of the discussion. Active participation, in considering how best to approach delivery, is required of all parties concerned.
The vacuum extractor can be a useful adjunct in certain circumstances, and its use has become widespread in American delivery suites. As with the obstetric forceps, which largely antedated its use, the vacuum extractor can lessen the overall risks of childbirth for both mother and infant.
The authors report no financial relationships relevant to this article.
CASE Three hours of pushing
C.A., age 29 years, is 40 weeks’ pregnant with her first child. After an unremarkable pregnancy, she arrives at the hospital for cervical ripening and induction of labor. Oxytocin is given, and labor progresses uneventfully. When C.A.’s cervix is dilated 8 cm, however, labor stalls. The physician orders placement of a pressure catheter and increases the dosage of oxytocin, and the cervix dilates fully. Although C.A. pushes well, the vertex descends only from +1 to +2 station (of 5 stations) after 3 hours.
How would you manage this delivery?
One option in C.A.’s case is operative vaginal delivery using the vacuum extractor, which has replaced the forceps as the most commonly used approach for operative vaginal delivery. Like the forceps, the vacuum extractor has vociferous detractors as well as supporters. Liberal use of cesarean section and questions regarding the safety of operative vaginal delivery vis-à-vis cesarean section have fueled the debate over its role in obstetric practice.
Among the benefits of vacuum extraction are its cost-effectiveness and shorter hospital stay (TABLE 1). It also obviates the need for cesarean section, including repeat cesarean. Risks include an increased incidence of genital tract trauma and a greater risk of fetal subgaleal hemorrhage.
We review 4 critical spheres of concern in regard to vacuum extraction:
- Patient selection
- Informed consent
- Technique
- Documentation
Increased understanding of these aspects of vacuum extraction will improve outcomes for the patient and limit medicolegal risk.
In the case of C.A., the physician offered 3 options:
- Continue maternal expulsive efforts to allow descent
- Attempt delivery by vacuum extraction
- Proceed to cesarean section on the basis of protracted descent.
Risks and benefits were reviewed with the patient, who chose to deliver by cesarean section. A 3,780-g infant in occiput posterior position was delivered safely.
TABLE 1
Delicate balance: Risks and benefits of operative vaginal delivery
| WHO? | BENEFIT | RISK |
|---|---|---|
| Mother | Cost-effective Less blood loss Lower risk of febrile morbidity Maternal preference No need for cesarean section or repeat cesarean Shorter hospitalization and convalescence | Increased incidence of genital tract trauma Possible damage to pelvic floor, with urinary and anal incontinence |
| Fetus | Fewer respiratory difficulties at birth | Increased risk of subgaleal hemorrhage Association with shoulder dystocia |
1. Patient selection: Maternal and fetal indications
Vacuum extraction may be justified for maternal or fetal indications.1,2 Maternal indications include prolongation or arrest of the second stage of labor, or the need to shorten the second stage, for reasons such as maternal cardiac disease, complex congenital cardiovascular disorders, and maternal exhaustion.
No definitive time limit for the second stage of labor
There is more flexibility today than in the past about what constitutes a “safe” length of the second stage. Recommendations concerning when the mother should begin pushing—and for how long—have evolved from a strict time limit to a focus on progression. If the fetal heart rate (FHR) tracing is reassuring, the second stage no longer needs to be limited to 2 or 3 hours. On the contrary, if the patient is still able and willing to push, changes in positioning and further expectant management remain acceptable in contemporary practice.3 Otherwise, a trial of vacuum extraction may be appropriate.
Vacuum extraction is particularly useful when the mother has difficulty pushing because of exhaustion and the fetal head has descended enough that it distends the labia between contractions, as in outlet deliveries.
Fetal indications
Fetal indications for operative vaginal delivery include distress, jeopardy, or a “nonreassuring” FHR tracing. Such a tracing may include late and prolonged decelerations, baseline bradycardia or tachycardia with or without variable decelerations, or, occasionally, a normal baseline rate with diminished variability.
Use vacuum or forceps?
The choice depends on which device would achieve delivery in the safest manner with the lowest risk of fetal injury. With the vacuum, force is exerted directly on the fetal scalp and only secondarily on the fetal skull. This puts fetal vessels that traverse the subgaleal space at risk for injury (FIGURE). With forceps, force is exerted directly on the fetal skull and mitigated by the petrous bone. Little or no force is exerted on the fetal scalp, lessening the risk of traumatic injury such as potentially fatal subgaleal hemorrhage.
Indications and contraindications for vacuum extraction are similar, but not identical, to those for forceps delivery (TABLE 2).2,3 The most important determinant for either device is the experience of the operator. You must be familiar with the instrument and technique before making any attempt to assist delivery. An inability to accurately assess fetal position or station, fetopelvic proportion, adequacy of labor, engagement of the fetal head, or any degree of malpresentation (including minor degrees of deflexion) is a contraindication to a trial of operative vaginal delivery.
Vacuum extraction should be reserved for fetuses at more than 34 weeks’ gestation because of the increased risk of intracranial hemorrhage associated with prematurity.
All decisions involving vacuum extraction should be made with caution. The adequacy of the pelvis, estimated fetal size, and any suggestions of fetopelvic disproportion are of particular significance.3
FIGURE
Subgaleal hemorrhage, a deadly complication
Blood can accumulate in a large potential space between the galea aponeurotica and the periosteum of the cranial bones after vacuum extraction. An infant with subgaleal hemorrhage will exhibit a boggy scalp, with swelling that crosses the suture lines and expands head circumferenceTABLE 2
Factors that predict success—or failure—of vacuum extraction
| When a woman fits overlapping categories, the decision to use vacuum extraction—or not—may be a judgment call* |
| GOOD CANDIDACY |
| Multiparous |
| Term pregnancy |
| Occiput anterior position, well-flexed |
| Wide subpubic arch |
| Compliant |
| MARGINAL CANDIDACY |
| Primiparous |
| Post-term |
| Occiput posterior position |
| Average subpubic arch |
| Gestational diabetes |
| Arrest disorders in second stage |
| POOR CANDIDACY |
| Protraction disorders in second stage |
| Narrow subpubic arch |
| Uncertain position of fetal head |
| Deflexion or asynclitism |
| Anticipated large-for-gestational-age infant |
| Poor maternal compliance |
| * When faced with a good indication in a marginal candidate, we recommend delivery in a “double setup” situation in which preparations are made for both vacuum extraction and cesarean section. If the vacuum can be properly applied, the first application of traction is crucial. We will only proceed if significant descent is achieved. If the fetal head (not the scalp) can be advanced a full station, then we proceed cautiously. If not, ready access to cesarean section allows for completion of the delivery in a timely manner. |
2. Informed consent: Elicit the patient’s desires
Thorough discussion with the patient and her family—to explain the reasoning behind the clinical decision to use the vacuum extractor and delineate the alternatives—is paramount. Moreover, the patient should be encouraged to actively participate in this discussion.
Among the alternatives to vacuum extraction are expectant observation and expedited delivery by cesarean section. Because patients increasingly are requesting elective cesarean section in the absence of obvious obstetric indications, this option should receive extra attention.
Most women still consider vaginal delivery an important milestone of female adulthood. When safety concerns arise and the situation makes vaginal delivery unwise, many women experience disappointment and postpartum depression over their “failed” attempt at vaginal delivery. These perceptions need to be addressed in discussions with the patient.
The risk–benefit equation
Vacuum extraction lessens the risk of maternal lacerations, either of the lower genital tract in the case of obstetric forceps, or of the cervix and lower uterine segment in the case of cesarean section. In addition, vacuum extraction can be performed comfortably in the absence of regional anesthesia.
Avoiding cesarean section can produce multiple benefits
Another maternal benefit of vacuum extraction is the decreased need for cesarean section. A reduction in the primary cesarean rate also lowers the need for repeat cesarean section, which can be more technically challenging than primary C-section due to the presence of dense scar tissue and intra-abdominal adhesions. Cesarean section also increases the risk of placenta accreta, increta, or percreta in subsequent pregnancies. These complications increase the likelihood of emergency hysterectomy, massive blood loss, and serious maternal morbidity and mortality.
Even in the absence of placenta accreta, both primary and repeat cesarean sections raise the risk of hemorrhage and febrile morbidity, prolong convalescence, and increase cost, compared with vaginal delivery. For these reasons, avoiding primary cesarean section can obviate the need for multiple surgical procedures and their attendant risks. The degree to which these factors favor vaginal delivery over cesarean section is subject to debate.
Maternal risks include pelvic floor trauma
Both vacuum extraction and forceps delivery increase the risk of anal sphincter injury and can impair fecal continence.4 Both methods also appear to increase trauma to the genital tract in comparison with spontaneous delivery and may predispose the woman to pelvic floor dysfunction, including urinary and anal incontinence.5-10 However, anal sphincter trauma was less frequent after vacuum extraction than after forceps delivery.1
Other maternal injuries associated with vacuum extraction include perineal lacerations and injuries to the vulva, vagina, and cervix. Vacuum extraction also has been implicated as a significant risk factor for postpartum hemorrhage11 and genital-tract infection.1
Fewer neonatal respiratory problems with vaginal delivery
Compared with cesarean section, vaginal delivery is thought to diminish the risk of intrapartum aspiration and respiratory problems in the newborn. It also may facilitate the transition from fetal to neonatal circulation and reduce the need for immediate resuscitation at birth.
Neonatal risks include soft-tissue injury and potential hemorrhage
Infants delivered by vacuum extraction have a significantly higher rate of intracranial hemorrhage, brachial plexus injuries, convulsions, central nervous system depression, and the need for mechanical ventilation, compared with spontaneously delivered infants (TABLE 3).12,13
Although vacuum extraction is associated with a wide range of soft tissue injuries, they are often less serious than the fetal scalp injuries associated with obstetric forceps. Cup marks, bruising, and minor lacerations of the scalp and caput succedaneum are common fetal injuries, although the majority resolve without apparent sequelae.14
Subgaleal hemorrhage is the most serious neonatal complication of vacuum extraction, occurring in 1% to 3.8% of vacuum extractions (FIGURE).15 It coexists with neonatal coagulopathy in 19% to 29% of newborns16 and increases the risk of progression to hemorrhagic shock and death. Subgaleal hemorrhage has a mortality rate ranging from 2.7% to 22.8%.15-17
Cephalhematoma is another complication associated with vacuum extraction. It involves an accumulation of blood beneath the periosteum of a cranial bone (usually the parietal bone), and it almost always resolves spontaneously. The incidence of cephalhematoma varies. It is significantly more common in deliveries involving vacuum extraction (9.8%) than in forceps deliveries (4.1%).18 Its incidence increases with the length of time the vacuum cup is applied and with paramedian application.18
Intracranial hemorrhage occurs in 1 of 860 vacuum extractions, 1 of 664 forceps deliveries, 1 of 954 cesarean deliveries, and 1 of 1,900 spontaneous deliveries.12 Subdural hemorrhage is the most common form of intracranial hemorrhage and is almost invariably the result of birth trauma. However, asymptomatic subdural hematoma occurs in up to 6.1% of uncomplicated vaginal deliveries.19
Other, less common types of intracranial hemorrhage, such as subarachnoid, intraventricular, and intraparenchymal hemorrhage, have a more complex etiology, which includes birth asphyxia, hemorrhagic diathesis, infection, and vascular abnormalities.20
Retinal hemorrhage also may occur after vacuum extraction, with an incidence of 49% to 77.8%, compared with 30.3% after forceps delivery, 30.4% after normal vaginal delivery, and 8.3% after cesarean delivery.21 It generally resolves spontaneously without any permanent damage.22
TABLE 3
Vacuum extraction can injure the fetus
| DIRECT INJURY |
| Cephalhematoma |
| Intracranial hemorrhage (parenchymal, subdural, intraventricular, subarachnoid) |
| Nerve injury |
| Scalp laceration, abrasion, ecchymoses, necrosis |
| Skull fracture |
| Subgaleal hemorrhage |
| INDIRECT INJURY |
| Anemia, hyperbilirubinemia |
| Brachial plexus injury |
| Scalp infection or abscess |
| SOURCE: O’Grady et al31 |
Shoulder dystocia and brachial plexus palsy
Vacuum extraction also is associated with shoulder dystocia and brachial plexus palsy, although the primary risk factor for these complications is thought to be increased fetal size.23-25 The incidence of shoulder dystocia with vacuum extraction is 3.5%, compared with 1.5% for forceps delivery.25
The risk of brachial plexus palsy also increases with vacuum extraction, especially as the duration of the procedure increases.25
Less common complications associated with vacuum extraction are skull fractures, fetal hemorrhage from bleeding at the site of scalp electrodes, sepsis originating from infected scalp trauma, and corneal injury.
No long-term impairment
Long-term outcome studies of children delivered by vacuum extraction show no differences in physical or cognitive functioning or intelligence scores, compared with other modes of delivery.26
3. Technique: Create conditions that ensure success
Certain prerequisites to vacuum extraction can assure successful application and strict adherence to protocol. These prerequisites include having an appropriate indication, thorough informed consent, proper maternal positioning, adequate anesthesia, and knowledge of fetal position and station (TABLE 4).1 These objectives can be accomplished in the following steps:
- After an informed consent discussion, assess maternal positioning and repeat the pelvic exam. Also ascertain the adequacy of anesthesia. Insert a bladder catheter.
- Perform a “ghost” trial of vacuum extraction to visualize the procedure before the actual attempt.
- Test the function of the vacuum.
- Lubricate the vacuum cup with surgical soap or gel, insert it into the vagina, and maneuver it onto the fetal head. Place the vacuum extractor over the sagittal suture about 6 cm distal to the anterior fontanel and 2 cm proximal to the posterior fontanel. (The illustration on page 74 demonstrates positioning.) Apply a small degree of vacuum (approximately 20 mm Hg). Double-check application.
- Gradually apply full vacuum (550–600 mm Hg, depending on cup size), allowing the scalp to mold to the extractor cup.
- Apply 2-handed traction in concert with uterine contractions and supplemented by maternal pushing. Assuming there is no loss of vacuum (“pop-off” of the cup), the initial traction effort should produce a gain in station. If a “pop-off” occurs, a single additional attempt at delivery may be warranted.
- As the head crowns, perform episiotomy as needed and slowly deliver the fetal head. Remove the vacuum cup.
- After delivery of the placenta, inspect the vagina, cervix, and perineum closely.
- Dictate a full operative note and annotate the delivery in the chart. See the section on documentation, below.
Vacuum extraction may fail for a number of reasons (TABLE 5).
TABLE 4
Perform these predelivery checks before applying traction
| Is anesthesia adequate? Is maternal positioning correct? |
| Is the bladder empty? |
| Is the fetus in the proper attitude (flexion)? |
| Is fetal status reassuring? |
Is the vacuum properly applied?
|
| Has the patient been instructed on when and how long to push? |
| Are the proposed maneuvers appropriate? |
TABLE 5
Why might vacuum extraction fail?
| INSTRUMENT-RELATED |
| Pump failure |
| Vacuum leak |
| TECHNIQUE-RELATED |
| Failure to encourage maternal valsalva with traction efforts |
| Inappropriate intensity of traction |
| Incorrect axis of traction |
| Maternal tissue trapped beneath vacuum cup |
| Poor cup position |
| OBSTETRIC CONDITIONS |
Congenital anomaly
|
| Fetal macrosomia |
| Incomplete cervical dilation |
Position and attitude problems
|
| Unappreciated cephalopelvic disproportion |
| SOURCE: Modified from Plauche et al32 |
Most important variable: Cup placement
The single most critical step in vacuum extraction is placement of the cup. It should be applied at the point of maximum fetal cranial flexion, which is proximal to the leading edge of the posterior fontanel.
Once full vacuum is achieved, encourage the mother to push with the next contraction, and apply steady traction in concert with her efforts.
The initial application of traction should be directed to maintain proper flexion of the fetal head, and should bring about descent of the fetal head. If there is no descent with the first application of traction, and correct technique and cup placement have been applied, abandon operative vaginal delivery (TABLE 6).
Do not make a further attempt to deliver the child using forceps, as the risk of intracranial hemorrhage appears to be highest in infants delivered using a combination of vacuum extraction and forceps.
TABLE 6
Repeat traction efforts reap a diminishing return
| NUMBER OF TRACTION EFFORTS | SUCCESS RATE | |
|---|---|---|
| VACUUM EXTRACTION (N=433) | FORCEPS (N=555) | |
| 1 or 2 | 68.4% | 38.4% |
| 3 or 4 | 24.9% | 48.6% |
| 5 or more | 6.7% | 12.9% |
| Adapted from Sjostedt33 | ||
4. Documentation: The chart is the most important witness
The value of complete and contemporaneous notation cannot be overstated. The patient’s chart is the permanent repository of the record of delivery. It is without doubt the most important witness to the event and should be treated as such. Include a dictated operative note as well as notation in the chart itself. Notes should be legible and properly dated, with the time of day indicated.
When operative vaginal delivery is performed, record the following:
- indication for the procedure
- course of labor
- anesthesia
- personnel present
- instruments used
- position and station of the fetal head
- force and duration of traction
- complications, including how they were recognized and managed
- immediate condition of the newborn and all steps taken in resuscitation.
Operative vaginal delivery is no newcomer to obstetrics. Hindu writings from about 1000 BC, and Hippocrates’ own musings from the fifth century BC, describe instruments and techniques to combat arrested labor and salvage the lives of both mother and child.27 Crude forceps were described by the Muslim physician Albucasis in the 11th century.27
Before the advent of safe cesarean section, many maternal lives were no doubt saved by these instruments and techniques. Unfortunately, destruction of the fetus and maternal death were frequent outcomes of operative vaginal delivery by forceps before the 20th century.28
As for vacuum extraction in particular, the idea of attaching a device to the fetal head to aid in delivery is credited to Arnett, a 19th century surgeon and inventor, who envisioned the “pneumatic tractor.”29
In 1957, Malmstrom reintroduced the vacuum as an aid in delivery, designing a rigid cup that was connected by rubber tubing to a vacuum source.30 This allowed the separation of the pump mechanism from the cup and made for easier application.
Most recently, Kobayashi developed the soft-cup design, a low-cost flexible plastic alternative that allows for a disposable instrument.31
Minimizing medicolegal risk
The best way to prevent an accusation of medical malpractice is to develop strong clinical and interpersonal skills. These simple, intuitive suggestions may help:
- Understand the role of operative vaginal delivery in current practice.
- Develop a simple and interactive discussion model for use in labor and delivery with the patient and her family.
- Consider a woman’s preferences for delivery.
- Know the indications and contraindications for vacuum extraction.
- Use the checks and safeguards listed under 3. Technique: Create conditions that ensure success.
- Perform vacuum extraction in the cesarean section room. Stop the procedure at once if any problem arises, and proceed to cesarean delivery.
- Make all chart notations completely legible, and add dictated notes.
If you are a new physician or lack significant experience with vacuum extraction, ask for input, supervision, and education from more experienced clinicians. Also make it a point to ask about department guidelines and review the credentialing process. Once you become adept at vacuum extraction, mentor more junior colleagues.
Two critical concerns
When contemplating vacuum-assisted delivery, 2 risks are paramount:
- failure of the vacuum extractor to achieve delivery
- the potential for fetal and maternal injury.
Training must ensure appropriate case selection and technique. Vacuum extraction must be performed with the same precision and care used with forceps. If application of the device is incorrect, or if there is a wrong direction of traction, excessive traction, or traction in the presence of disproportion, the cup will slip or pop off, and vacuum delivery will fail, with the potential for traumatic fetal injury.
All risks must be discussed with the patient to fulfill informed consent, and the risks and benefits of alternative treatments should be part of the discussion. Active participation, in considering how best to approach delivery, is required of all parties concerned.
The vacuum extractor can be a useful adjunct in certain circumstances, and its use has become widespread in American delivery suites. As with the obstetric forceps, which largely antedated its use, the vacuum extractor can lessen the overall risks of childbirth for both mother and infant.
The authors report no financial relationships relevant to this article.
1. O’Grady JP, Gimovsky ML, McIlhargie CJ, eds. Operative Obstetrics. Pearl River, NY: Parthenon Publishing; 1995.
2. Johanson RB, Menon BKV. Vacuum extraction versus forceps for assisted vaginal delivery. Cochrane Database Syst Rev. 2000;(2):CD000224.-
3. Bloom SL, Casey BM, Schaffer JL, et al. Pushing in the second stage of labor. Am J Obstet Gynecol 2006;194:10-13.
4. Operative vaginal delivery. ACOG Practice Bulletin #17. Washington, DC: American College of Obstetricians and Gynecologists; June 2000.
5. Power D, Fitzpatrick M, O’Herlihy C. Obstetric anal sphincter injury: how to avoid, how to repair: a literature review. J Fam Pract 2006;55:193-200.
6. Chaliha C, Kalia V, Stanton S, et al. Antenatal prediction of postpartum urinary and fecal incontinence. Obstet Gynecol 1999;94:689-694.
7. Bofill JA, Rust OA, Schorr SJ, et al. A randomized prospective trial of the obstetric forceps versus the M-cup vacuum extractor. Am J Obstet Gynecol 1996;175:1325-1330.
8. Salamalekis E, Loghis C, Pyrgiotis E, et al. Soft cup vacuum extractor versus forceps delivery. J Obstet Gynecol. 1995;15:245-246.
9. Zetterstrom JP, Lopez A, Anzen B, et al. Anal incontinence after vaginal delivery: a prospective study in primiparous women. Br J Obstet Gynaecol. 1999;106:324-330.
10. Johanson RB, Heycock E, Carter J, et al. Maternal and child health after assisted vaginal delivery: five-year follow up of a randomized controlled study comparing forceps and ventouse. Br J Obstet Gynaecol. 1999;106:544-549
11. Faltin DL, Otero M, Petignat P, et al. Women’s health 18 years after rupture of the anal sphincter during childbirth: I. Fecal incontinence. Am J Obstet Gynecol. 2006;194:1255-1259.
12. Plauche WC. Fetal cranial injuries related to delivery with the Malmsträm vacuum extractor. Obstet Gynecol. 1979;53:750-757.
13. Towner D, Castro MA, Eby-Wilkens E, et al. Effect of mode of delivery in nulliparous women on neonatal intracranial injury. N Engl J Med. 1999;341:1709-1714.
14. Sheiner E, Sarid L, Levy A, et al. Obstetric risk factors and outcome of pregnancies complicated with early postpartum hemorrhage: a population-based study. J Matern Fetal Neonatal Med. 2005;18:149-154.
15. Johanson R. Choice of instrument for vaginal delivery. Curr Opin Obstet Gynecol. 1997;9:361-365.
16. Chadwick LM, Pemberton PJ, Kurinczuk JJ. Neonatal subgaleal hematoma: associated risk factors, complications, and outcome. J Pediatr Child Health. 1996;32:228-232.
17. Ng PC, Siu YK, Lewindon PJ. Subaponeurotic hemorrhage in the 1990s: a 3-year surveillance. Acta Pediatr. 1995;84:1065-1069
18. Bofill JA, Rust OA, Devidas M, et al. Neonatal cephalohematoma from vacuum extraction. J Reprod Med. 1997;42:565-569.
19. Doumouchtsis SK, Arulkumaran S. Head injuries after instrumental vaginal deliveries. Curr Opin Obstet Gynecol. 2006;18:129-134.
20. Govaert P. Cranial Hemorrhage in the Term Newborn Infant. London: Mac Keith Press; 1993.
21. Hughes LA, May K, Talbot JF, Parsons MA. Incidence, distribution, and duration of birth-related retinal hemorrhages: a prospective study. J AAPOS. 2006;10:102-106.
22. Sheiner E, Levy A, Hershkovitz R, et al. Determining factors associated with shoulder dystocia: a population-based study. Eur J Obstet Gynecol Reprod Biol. 2006;126:11-15.
23. Baskett TF, Allen AC. Perinatal implications of shoulder dystocia. Obstet Gynecol. 1995;86:15-18.
24. Mollberg M, Hagerg H, Bager B, et al. Risk factors for obstetric brachial plexus palsy among neonates delivered by vacuum extraction. Obstet Gynecol. 2005;106:913-918.
25. Caughey AB, Sandberg PL, Alantnik MG, et al. Forceps compared with vacuum: rates of neonatal and maternal morbidity. Obstet Gynecol. 2005;106:908-912.
26. Ngan HYS, Miu P, Ko L, et al. Long-term neurological sequelae following vacuum extractor delivery. Aust NZ J Obstet Gynecol. 1990;30:111-114.
27. Lyons AS, Petrucelli RJ. Medicine: An Illustrated History. New York: Harry N Abrams; 1978.
28. Speert H. Obstetric and Gynecologic Milestones Illustrated. Pearl River, NY: Parthenon Publishing; 1996.
29. Arnett N. Elements of Physics or Natural Philosophy, General and Medical, Explained Independently of Technical Mathematics and Containing New Disquisitions and Practical Suggestions. 2nd ed. Philadelphia: Carney and Lea; 1831.
30. Malmstrom T. The vacuum extractor, an obstetrical instrument. I. Acta Obstet Gynecol Scand. 1957;36(suppl 3):5-50.
31. O’Grady JP, Gimovsky ML, McIlhargie CJ. Vacuum Extraction in Modern Obstetric Practice. Pearl River, NY: Parthenon Publishing; 1995.
32. Plauche WC, Morrison JC, O’Sullivan MJ. Surgical Obstetrics. Philadelphia: WB Saunders; 1992.
33. Sjostedt JE. The vacuum extractor and forceps in obstetrics: a clinical study. Acta Obstet Gynecol Scand. 1967;48:638-639.
1. O’Grady JP, Gimovsky ML, McIlhargie CJ, eds. Operative Obstetrics. Pearl River, NY: Parthenon Publishing; 1995.
2. Johanson RB, Menon BKV. Vacuum extraction versus forceps for assisted vaginal delivery. Cochrane Database Syst Rev. 2000;(2):CD000224.-
3. Bloom SL, Casey BM, Schaffer JL, et al. Pushing in the second stage of labor. Am J Obstet Gynecol 2006;194:10-13.
4. Operative vaginal delivery. ACOG Practice Bulletin #17. Washington, DC: American College of Obstetricians and Gynecologists; June 2000.
5. Power D, Fitzpatrick M, O’Herlihy C. Obstetric anal sphincter injury: how to avoid, how to repair: a literature review. J Fam Pract 2006;55:193-200.
6. Chaliha C, Kalia V, Stanton S, et al. Antenatal prediction of postpartum urinary and fecal incontinence. Obstet Gynecol 1999;94:689-694.
7. Bofill JA, Rust OA, Schorr SJ, et al. A randomized prospective trial of the obstetric forceps versus the M-cup vacuum extractor. Am J Obstet Gynecol 1996;175:1325-1330.
8. Salamalekis E, Loghis C, Pyrgiotis E, et al. Soft cup vacuum extractor versus forceps delivery. J Obstet Gynecol. 1995;15:245-246.
9. Zetterstrom JP, Lopez A, Anzen B, et al. Anal incontinence after vaginal delivery: a prospective study in primiparous women. Br J Obstet Gynaecol. 1999;106:324-330.
10. Johanson RB, Heycock E, Carter J, et al. Maternal and child health after assisted vaginal delivery: five-year follow up of a randomized controlled study comparing forceps and ventouse. Br J Obstet Gynaecol. 1999;106:544-549
11. Faltin DL, Otero M, Petignat P, et al. Women’s health 18 years after rupture of the anal sphincter during childbirth: I. Fecal incontinence. Am J Obstet Gynecol. 2006;194:1255-1259.
12. Plauche WC. Fetal cranial injuries related to delivery with the Malmsträm vacuum extractor. Obstet Gynecol. 1979;53:750-757.
13. Towner D, Castro MA, Eby-Wilkens E, et al. Effect of mode of delivery in nulliparous women on neonatal intracranial injury. N Engl J Med. 1999;341:1709-1714.
14. Sheiner E, Sarid L, Levy A, et al. Obstetric risk factors and outcome of pregnancies complicated with early postpartum hemorrhage: a population-based study. J Matern Fetal Neonatal Med. 2005;18:149-154.
15. Johanson R. Choice of instrument for vaginal delivery. Curr Opin Obstet Gynecol. 1997;9:361-365.
16. Chadwick LM, Pemberton PJ, Kurinczuk JJ. Neonatal subgaleal hematoma: associated risk factors, complications, and outcome. J Pediatr Child Health. 1996;32:228-232.
17. Ng PC, Siu YK, Lewindon PJ. Subaponeurotic hemorrhage in the 1990s: a 3-year surveillance. Acta Pediatr. 1995;84:1065-1069
18. Bofill JA, Rust OA, Devidas M, et al. Neonatal cephalohematoma from vacuum extraction. J Reprod Med. 1997;42:565-569.
19. Doumouchtsis SK, Arulkumaran S. Head injuries after instrumental vaginal deliveries. Curr Opin Obstet Gynecol. 2006;18:129-134.
20. Govaert P. Cranial Hemorrhage in the Term Newborn Infant. London: Mac Keith Press; 1993.
21. Hughes LA, May K, Talbot JF, Parsons MA. Incidence, distribution, and duration of birth-related retinal hemorrhages: a prospective study. J AAPOS. 2006;10:102-106.
22. Sheiner E, Levy A, Hershkovitz R, et al. Determining factors associated with shoulder dystocia: a population-based study. Eur J Obstet Gynecol Reprod Biol. 2006;126:11-15.
23. Baskett TF, Allen AC. Perinatal implications of shoulder dystocia. Obstet Gynecol. 1995;86:15-18.
24. Mollberg M, Hagerg H, Bager B, et al. Risk factors for obstetric brachial plexus palsy among neonates delivered by vacuum extraction. Obstet Gynecol. 2005;106:913-918.
25. Caughey AB, Sandberg PL, Alantnik MG, et al. Forceps compared with vacuum: rates of neonatal and maternal morbidity. Obstet Gynecol. 2005;106:908-912.
26. Ngan HYS, Miu P, Ko L, et al. Long-term neurological sequelae following vacuum extractor delivery. Aust NZ J Obstet Gynecol. 1990;30:111-114.
27. Lyons AS, Petrucelli RJ. Medicine: An Illustrated History. New York: Harry N Abrams; 1978.
28. Speert H. Obstetric and Gynecologic Milestones Illustrated. Pearl River, NY: Parthenon Publishing; 1996.
29. Arnett N. Elements of Physics or Natural Philosophy, General and Medical, Explained Independently of Technical Mathematics and Containing New Disquisitions and Practical Suggestions. 2nd ed. Philadelphia: Carney and Lea; 1831.
30. Malmstrom T. The vacuum extractor, an obstetrical instrument. I. Acta Obstet Gynecol Scand. 1957;36(suppl 3):5-50.
31. O’Grady JP, Gimovsky ML, McIlhargie CJ. Vacuum Extraction in Modern Obstetric Practice. Pearl River, NY: Parthenon Publishing; 1995.
32. Plauche WC, Morrison JC, O’Sullivan MJ. Surgical Obstetrics. Philadelphia: WB Saunders; 1992.
33. Sjostedt JE. The vacuum extractor and forceps in obstetrics: a clinical study. Acta Obstet Gynecol Scand. 1967;48:638-639.