User login
PALM BEACH, FLA. – The number of U.S. patients with ruptured abdominal aortic aneurysms who were managed with endovascular aneurysm repair more than doubled during 2005-2009, suggesting that it’s time to develop a national triage system in order to perform emergency endovascular repairs around the clock, according to Dr. John J. Ricotta.
"A strategy that promotes development of EVAR [endovascular aneurysm repair] centers with triage of stable, EVAR-suitable patients may be the best approach," said Dr. Ricotta, a vascular surgeon and chairman of surgery at MedStar Washington (D.C.) Hospital Center.
"Regionalization of EVAR services may be practical, along with a triage system to rapidly diagnose and transfer patients with RAAA [ruptured abdominal aortic aneurysm]," Dr. Ricotta said at the annual meeting of the Southern Surgical Association.
Because the time from the onset of symptoms to the start of successful EVAR repair is often more than 10 hours, stable RAAA patients could be transferred.
"The focus should be on older patients, who are more likely to survive if you do EVAR, and stable patients. Patients who are hemodynamically stable and have good anatomy [for performing EVAR] should go to an EVAR center."
Dr. Ricotta and his associates analyzed data collected from the U.S. Nationwide Inpatient Sample for all patients aged 60 years or older treated for RAAA during 2005-2009. During the 5-year period, a total of 21,218 patients in the sample underwent treatment for RAAA; 60% of the patients underwent open surgical repair, 22% had no operative repair, and 18% had EVAR.
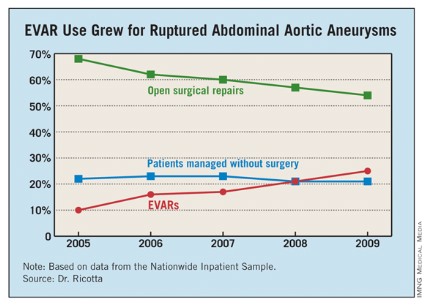
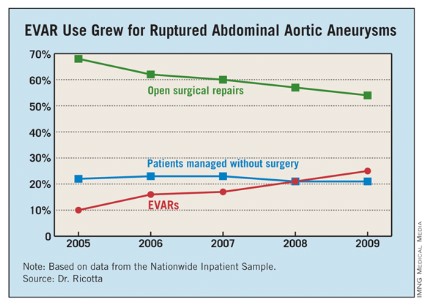
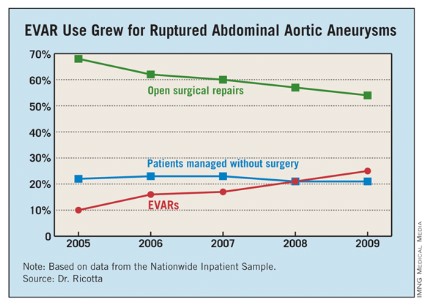
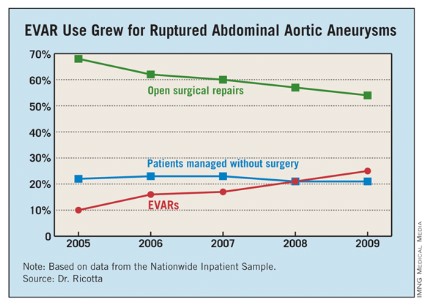
Use of EVAR rose from 10% of RAAA patients in 2005 to 25% in 2009 (see table). Among the subset of patients who had surgical management, EVAR use rose from 13% of patients in 2005 to 32% in 2009.
EVAR was performed primarily at urban teaching hospitals and in patients under 90. Throughout the 5-year period, EVAR use at urban teaching hospitals included 25% of RAAA patients, compared with 12% of these patients managed at urban nonteaching hospitals and 7% of RAAA patients managed at rural hospitals. About 19% of RAAA patients 60-89 years old underwent EVAR, compared with 12% of those aged 90 or older.
EVAR effectively reduced mortality. Throughout the period studied, the rate of in-hospital mortality was 41% in patients managed with open surgery and 28% in those managed with EVAR, a significant difference, Dr. Ricotta said.
Furthermore, EVAR produced a mortality benefit compared with open surgery across the spectrum of patients, regardless of age. For example, among patients who were at least 90 years old, in-hospital mortality following EVAR was 36%, compared with 77% among patients who had open repair. In a multivariate analysis, EVAR was the only demographic or clinical variable associated with a significant reduction in postoperative in-hospital death, cutting mortality by 47%.
Despite EVAR’s success, use of the technique is limited by the anatomic and physiologic presentation of RAAA patients. "With current technology, EVAR is generally thought to be applicable to 30%-50% of RAAA patients," Dr. Ricotta said. "Experienced centers report the use of EVAR for about 50% of RAAA patients."
Dr. Ricotta called for regionalization and a triage and transfer model, because "widespread adoption of EVAR for RAAA is not practical," he said. "It is an expensive and evolving technology that needs a dedicated staff and a high volume of procedures." An EVAR-first program requires ready CT access and suitable imaging facilities in the operating room, a suitable stock of endografts, and an EVAR team that’s available 24/7, he said.
"Patients who are transferred might do better than patients who are not transferred," agreed Dr. Spence M. Taylor, a vascular surgeon and professor of surgery at the University of South Carolina in Greenville. But he added that patient selection may also play a role. "EVAR does better than open surgical repair in patients who can be stabilized and have this intervention compared with patients who can’t."
Dr. Ricotta and Dr. Taylor had no disclosures.
PALM BEACH, FLA. – The number of U.S. patients with ruptured abdominal aortic aneurysms who were managed with endovascular aneurysm repair more than doubled during 2005-2009, suggesting that it’s time to develop a national triage system in order to perform emergency endovascular repairs around the clock, according to Dr. John J. Ricotta.
"A strategy that promotes development of EVAR [endovascular aneurysm repair] centers with triage of stable, EVAR-suitable patients may be the best approach," said Dr. Ricotta, a vascular surgeon and chairman of surgery at MedStar Washington (D.C.) Hospital Center.
"Regionalization of EVAR services may be practical, along with a triage system to rapidly diagnose and transfer patients with RAAA [ruptured abdominal aortic aneurysm]," Dr. Ricotta said at the annual meeting of the Southern Surgical Association.
Because the time from the onset of symptoms to the start of successful EVAR repair is often more than 10 hours, stable RAAA patients could be transferred.
"The focus should be on older patients, who are more likely to survive if you do EVAR, and stable patients. Patients who are hemodynamically stable and have good anatomy [for performing EVAR] should go to an EVAR center."
Dr. Ricotta and his associates analyzed data collected from the U.S. Nationwide Inpatient Sample for all patients aged 60 years or older treated for RAAA during 2005-2009. During the 5-year period, a total of 21,218 patients in the sample underwent treatment for RAAA; 60% of the patients underwent open surgical repair, 22% had no operative repair, and 18% had EVAR.
Use of EVAR rose from 10% of RAAA patients in 2005 to 25% in 2009 (see table). Among the subset of patients who had surgical management, EVAR use rose from 13% of patients in 2005 to 32% in 2009.
EVAR was performed primarily at urban teaching hospitals and in patients under 90. Throughout the 5-year period, EVAR use at urban teaching hospitals included 25% of RAAA patients, compared with 12% of these patients managed at urban nonteaching hospitals and 7% of RAAA patients managed at rural hospitals. About 19% of RAAA patients 60-89 years old underwent EVAR, compared with 12% of those aged 90 or older.
EVAR effectively reduced mortality. Throughout the period studied, the rate of in-hospital mortality was 41% in patients managed with open surgery and 28% in those managed with EVAR, a significant difference, Dr. Ricotta said.
Furthermore, EVAR produced a mortality benefit compared with open surgery across the spectrum of patients, regardless of age. For example, among patients who were at least 90 years old, in-hospital mortality following EVAR was 36%, compared with 77% among patients who had open repair. In a multivariate analysis, EVAR was the only demographic or clinical variable associated with a significant reduction in postoperative in-hospital death, cutting mortality by 47%.
Despite EVAR’s success, use of the technique is limited by the anatomic and physiologic presentation of RAAA patients. "With current technology, EVAR is generally thought to be applicable to 30%-50% of RAAA patients," Dr. Ricotta said. "Experienced centers report the use of EVAR for about 50% of RAAA patients."
Dr. Ricotta called for regionalization and a triage and transfer model, because "widespread adoption of EVAR for RAAA is not practical," he said. "It is an expensive and evolving technology that needs a dedicated staff and a high volume of procedures." An EVAR-first program requires ready CT access and suitable imaging facilities in the operating room, a suitable stock of endografts, and an EVAR team that’s available 24/7, he said.
"Patients who are transferred might do better than patients who are not transferred," agreed Dr. Spence M. Taylor, a vascular surgeon and professor of surgery at the University of South Carolina in Greenville. But he added that patient selection may also play a role. "EVAR does better than open surgical repair in patients who can be stabilized and have this intervention compared with patients who can’t."
Dr. Ricotta and Dr. Taylor had no disclosures.
PALM BEACH, FLA. – The number of U.S. patients with ruptured abdominal aortic aneurysms who were managed with endovascular aneurysm repair more than doubled during 2005-2009, suggesting that it’s time to develop a national triage system in order to perform emergency endovascular repairs around the clock, according to Dr. John J. Ricotta.
"A strategy that promotes development of EVAR [endovascular aneurysm repair] centers with triage of stable, EVAR-suitable patients may be the best approach," said Dr. Ricotta, a vascular surgeon and chairman of surgery at MedStar Washington (D.C.) Hospital Center.
"Regionalization of EVAR services may be practical, along with a triage system to rapidly diagnose and transfer patients with RAAA [ruptured abdominal aortic aneurysm]," Dr. Ricotta said at the annual meeting of the Southern Surgical Association.
Because the time from the onset of symptoms to the start of successful EVAR repair is often more than 10 hours, stable RAAA patients could be transferred.
"The focus should be on older patients, who are more likely to survive if you do EVAR, and stable patients. Patients who are hemodynamically stable and have good anatomy [for performing EVAR] should go to an EVAR center."
Dr. Ricotta and his associates analyzed data collected from the U.S. Nationwide Inpatient Sample for all patients aged 60 years or older treated for RAAA during 2005-2009. During the 5-year period, a total of 21,218 patients in the sample underwent treatment for RAAA; 60% of the patients underwent open surgical repair, 22% had no operative repair, and 18% had EVAR.
Use of EVAR rose from 10% of RAAA patients in 2005 to 25% in 2009 (see table). Among the subset of patients who had surgical management, EVAR use rose from 13% of patients in 2005 to 32% in 2009.
EVAR was performed primarily at urban teaching hospitals and in patients under 90. Throughout the 5-year period, EVAR use at urban teaching hospitals included 25% of RAAA patients, compared with 12% of these patients managed at urban nonteaching hospitals and 7% of RAAA patients managed at rural hospitals. About 19% of RAAA patients 60-89 years old underwent EVAR, compared with 12% of those aged 90 or older.
EVAR effectively reduced mortality. Throughout the period studied, the rate of in-hospital mortality was 41% in patients managed with open surgery and 28% in those managed with EVAR, a significant difference, Dr. Ricotta said.
Furthermore, EVAR produced a mortality benefit compared with open surgery across the spectrum of patients, regardless of age. For example, among patients who were at least 90 years old, in-hospital mortality following EVAR was 36%, compared with 77% among patients who had open repair. In a multivariate analysis, EVAR was the only demographic or clinical variable associated with a significant reduction in postoperative in-hospital death, cutting mortality by 47%.
Despite EVAR’s success, use of the technique is limited by the anatomic and physiologic presentation of RAAA patients. "With current technology, EVAR is generally thought to be applicable to 30%-50% of RAAA patients," Dr. Ricotta said. "Experienced centers report the use of EVAR for about 50% of RAAA patients."
Dr. Ricotta called for regionalization and a triage and transfer model, because "widespread adoption of EVAR for RAAA is not practical," he said. "It is an expensive and evolving technology that needs a dedicated staff and a high volume of procedures." An EVAR-first program requires ready CT access and suitable imaging facilities in the operating room, a suitable stock of endografts, and an EVAR team that’s available 24/7, he said.
"Patients who are transferred might do better than patients who are not transferred," agreed Dr. Spence M. Taylor, a vascular surgeon and professor of surgery at the University of South Carolina in Greenville. But he added that patient selection may also play a role. "EVAR does better than open surgical repair in patients who can be stabilized and have this intervention compared with patients who can’t."
Dr. Ricotta and Dr. Taylor had no disclosures.
AT THE ANNUAL MEETING OF THE SOUTHERN SURGICAL ASSOCIATION
Major Finding: From 2005 to 2009, the percentage of hospitalized U.S. patients with a ruptured AAA who underwent EVAR grew from 10% to 25%.
Data Source: The data came from an analysis of 21,218 U.S. patients hospitalized for a ruptured abdominal aortic aneurysm during 2005-2009 and included in the Nationwide Inpatient Sample.
Disclosures: Dr. Ricotta and Dr. Taylor had no disclosures.