User login
ANSWER
The least likely diagnosis is staph infection (choice “b”). By their very nature, staph infections are suppurative, often involving redness, swelling, pain, and purulent drainage. They can be chronic (eg, MRSA) but are more typically of acute onset. And they usually resolve on their own or with treatment; recall that this patient was treated for staph infection many times without any change.
She was also treated repeatedly for scabies (choice “a”), a condition that could certainly last 15 years. However, the lack of improvement with treatment, combined with the absence of suggestive signs, make this diagnosis improbable.
Mycosis fungoides (MF; choice “c”) is a type of T-cell lymphoma that often develops with itching and plaque formation over the course of years. It was ultimately ruled out by the biopsy results (as were scabies and staph infection).
What the biopsy did show was epidermal thickening—a characteristic sign of prurigo nodularis (choice “d”).
DISCUSSION
Prurigo nodularis is a localized form of neurodermatitis caused by picking and scratching. As with the classic form, the more the patient scratches, the more the lesions itch and multiply. In this case, biopsy of the larger plaque showed hypertrophic scarring.
The patient’s skin-picking habit likely developed during (and perhaps because of) her methamphetamine use. Long-term exposure to the itch-scratch-itch cycle can make treatment problematic. In this case, a class 4 topical steroid cream was prescribed, along with injection of several larger lesions with 10 mg/mL triamcinolone suspension.
It’s worth mentioning that for patients with this type of history, general lab testing (ie, complete blood count and complete metabolic panel) should be performed to rule out organic disease and other serious conditions (eg, renal or hepatic failure, leukemia). Fortunately, this patient’s results were reassuring on that front.
ANSWER
The least likely diagnosis is staph infection (choice “b”). By their very nature, staph infections are suppurative, often involving redness, swelling, pain, and purulent drainage. They can be chronic (eg, MRSA) but are more typically of acute onset. And they usually resolve on their own or with treatment; recall that this patient was treated for staph infection many times without any change.
She was also treated repeatedly for scabies (choice “a”), a condition that could certainly last 15 years. However, the lack of improvement with treatment, combined with the absence of suggestive signs, make this diagnosis improbable.
Mycosis fungoides (MF; choice “c”) is a type of T-cell lymphoma that often develops with itching and plaque formation over the course of years. It was ultimately ruled out by the biopsy results (as were scabies and staph infection).
What the biopsy did show was epidermal thickening—a characteristic sign of prurigo nodularis (choice “d”).
DISCUSSION
Prurigo nodularis is a localized form of neurodermatitis caused by picking and scratching. As with the classic form, the more the patient scratches, the more the lesions itch and multiply. In this case, biopsy of the larger plaque showed hypertrophic scarring.
The patient’s skin-picking habit likely developed during (and perhaps because of) her methamphetamine use. Long-term exposure to the itch-scratch-itch cycle can make treatment problematic. In this case, a class 4 topical steroid cream was prescribed, along with injection of several larger lesions with 10 mg/mL triamcinolone suspension.
It’s worth mentioning that for patients with this type of history, general lab testing (ie, complete blood count and complete metabolic panel) should be performed to rule out organic disease and other serious conditions (eg, renal or hepatic failure, leukemia). Fortunately, this patient’s results were reassuring on that front.
ANSWER
The least likely diagnosis is staph infection (choice “b”). By their very nature, staph infections are suppurative, often involving redness, swelling, pain, and purulent drainage. They can be chronic (eg, MRSA) but are more typically of acute onset. And they usually resolve on their own or with treatment; recall that this patient was treated for staph infection many times without any change.
She was also treated repeatedly for scabies (choice “a”), a condition that could certainly last 15 years. However, the lack of improvement with treatment, combined with the absence of suggestive signs, make this diagnosis improbable.
Mycosis fungoides (MF; choice “c”) is a type of T-cell lymphoma that often develops with itching and plaque formation over the course of years. It was ultimately ruled out by the biopsy results (as were scabies and staph infection).
What the biopsy did show was epidermal thickening—a characteristic sign of prurigo nodularis (choice “d”).
DISCUSSION
Prurigo nodularis is a localized form of neurodermatitis caused by picking and scratching. As with the classic form, the more the patient scratches, the more the lesions itch and multiply. In this case, biopsy of the larger plaque showed hypertrophic scarring.
The patient’s skin-picking habit likely developed during (and perhaps because of) her methamphetamine use. Long-term exposure to the itch-scratch-itch cycle can make treatment problematic. In this case, a class 4 topical steroid cream was prescribed, along with injection of several larger lesions with 10 mg/mL triamcinolone suspension.
It’s worth mentioning that for patients with this type of history, general lab testing (ie, complete blood count and complete metabolic panel) should be performed to rule out organic disease and other serious conditions (eg, renal or hepatic failure, leukemia). Fortunately, this patient’s results were reassuring on that front.
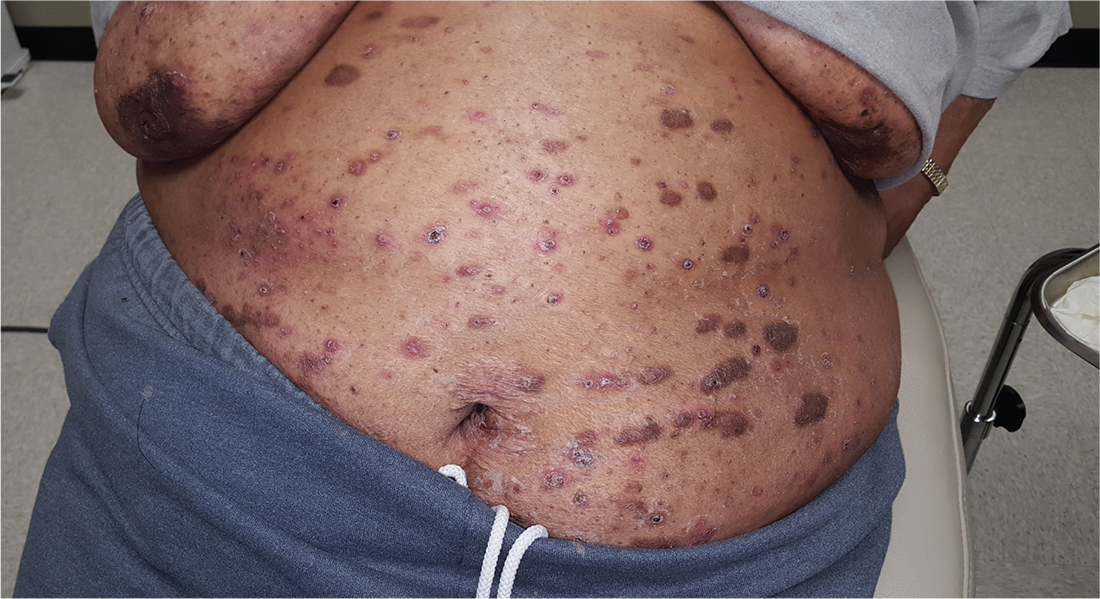
For at least 15 years, this 61-year-old African-American woman has had itchy lesions within arm’s reach. The patient says the problem manifested during a period in her life when she was addicted to several drugs, including methamphetamine. She complains bitterly about the itching and says it is difficult for her to leave the lesions alone.
No one else in her household is similarly affected. The patient has consulted a variety of health care providers, from primary care to dermatology and other specialties. She has received diagnoses of everything from scabies (for which she was treated, unsuccessfully) to pyoderma, bedbugs, and various forms of staph infection.
Examination reveals more than 100 lesions, mostly confined to her abdomen and lower chest, ranging from pinpoint to more than 3 cm. Many are excoriated, but most are purplish brown, oval plaques that somewhat match her type IV skin.
Her back, arms, and hands are spared. No lesions are seen between her fingers or on her volar wrists.
A biopsy is performed on two of the lesions—one small, the other larger.