User login
Several years ago, I adopted a single-incision approach to virtually all benign gynecologic laparoscopic procedures as the next logical step in the practice of minimally invasive surgery. In this time, my partner and I have performed more than 450 single-incision hysterectomies using a simple, reproducible technique that differs from other approaches to single-incision laparoscopy, or laparoendoscopic single-site surgery (LESS), as it is most commonly called.
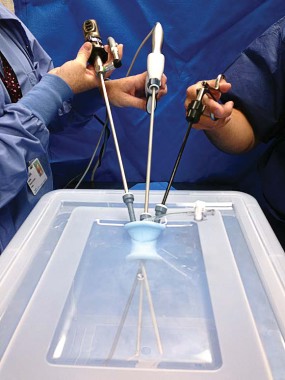
Rather than using articulating instruments, we use a 30-degree 5-mm bariatric-length laparoscope and straight, extra-long instruments. With sequential placement of one instrument at a time and attention to the direction of extra-abdominal hand movements, we create a work space with unimpeded access to the uterus and prevent the clashing of instruments, or "sword fighting," that can come with inserting several instruments through a single port.
Morcellation of the uterine fundus is accomplished extraperitoneally with specimen removal through the umbilicus. Use of a wider port with the LESS technique allows for morcellation by hand under direct vision with a #15 scalpel. This makes morcellation easier, safer, and more efficient than using an automated morcellator placed through a smaller port as in traditional multiport laparoscopic hysterectomy. We have successfully removed multiple uteri in excess of 1,000 grams – including a 3,000-gram uterus – using this technique.
Overall surgical principles/technique
We routinely use either the SILS port (Covidien), which has a predetermined setup of channels as depicted in the illustrations, or the GelPoint (Applied Medical), which allows for various trocar arrangements. Other single-incision ports can be used, though; the key to the procedure lies not in the port used, but in the placement of the instruments. A right-angled light connector also is essential, as it deviates the light cord out of the surgical field.
Regardless of the single-incision port used, the camera and a laparoscopic single-tooth tenaculum are placed in the lateral trocars, in the same horizontal plane. The active, working instrument – either Kleppinger bipolar forceps or a 45-cm Harmonic ACE Shears (Ethicon Endo-Surgery) – is then placed in the middle trocar.
While the use of angled instruments may seem helpful for creating appropriate triangulation in LESS, we have found that such instrumentation is actually counterproductive. Angled instrumentation creates new angles, in essence, which complicates instrument placement and makes it more difficult to achieve enough intra-abdominal working space and avoid sword fighting.
One exception is the laparoscope. We have found that a 30-degree 5-mm bariatric-length laparoscope works best. When exposing the right side of the uterus, the laparoscope is first inserted into the far left trocar and directed toward the right lower quadrant of the abdomen. The camera is then angled to visualize the uterus from a slightly elevated position. In this position, the operator’s external hand – holding the camera – is now deviated inferiorly and to the left side of the patient.
A 5-mm single-tooth tenaculum is then inserted into the other lateral trocar and used to manipulate the uterus anteriorly and to the left. In a simple supracervical hysterectomy, once the uterus is properly positioned, the utero-ovarian ligament and fallopian tube are exposed. In surgeries involving oophorectomy, the ovary rather than the uterus is first grasped and deviated medially and elevated, exposing the infundibulopelvic ligament. In this position, the assistant’s external hand is now deviated slightly inferiorly and to the right side of the patient.
When properly placed, the camera and the tenaculum are crossed intra-abdominally and held in slightly elevated positions. This allows for insertion of the active instrument underneath both the camera and grasper and directly toward the tissue to be incised. The slight elevation and intra-abdominal crossing of the instruments, while at first confusing, serves to create the angles that give the surgeon good external work space as well as excellent internal range of motion. We apply a significant amount of tension on the uterus to create this working space. The greater the deviation of the uterus (and the longer the instruments), the more work space there is.
With correct instrument placement, the active trocar has direct access to the uterus, so insertion of an instrument is simple, ergonomic, and intuitive. With this positioning, the active instrument (bipolar forceps, harmonic scalpel, suction, or probe) also has complete freedom of movement internally and externally. The operator’s hand can move superiorly, inferiorly, or laterally as needed to access the uterus.
We utilize the Kleppinger forceps and the 45-cm Harmonic Ace Shears for all of our dissection. Because the uterus is held on some tension, we first coagulate all vascular pedicles with the Kleppinger forceps before cutting. For safety, the uterine arteries are transected fairly high, just cephalad to the internal os. This gives us plenty of room to safely grasp and recoagulate a bleeding pedicle without fear of injuring the ureter.
Sequential instrument placement is key to this technique. If sword fighting occurs, one must reexamine the sequence of instrument placement and pay greater attention to the direction of extra-abdominal hand movements and subsequent angles. Again, the laparoscope and grasper must be inserted, positioned, and frozen in place before the active instrument is introduced.
Once one side of the uterus has been dissected free and the uterine artery transected, then all instruments are removed and replaced in a mirror-image manner to access the opposite side. Essentially, the camera and grasper switch trocars, and the active instrument remains in the middle.
Abdominal entry is performed with the traditional open laparoscopy technique described by Dr. Harrith Hasson of Chicago (Am. J. Obstet. Gynecol. 1971;110:886-7). While single-channel trocars generally require a 5- to 10-mm incision, LESS multichannel ports require a slightly larger incision. We recommend a straight vertical incision of about 2 cm through the center of the umbilicus.
The position of the surgeon also differs from multipart laparoscopy. With LESS, the surgeon stands in line with the port and the pathology, usually between the patient’s head and shoulder, and holds either the grasper or camera while operating the active blade. To prevent sliding in a steep Trendelenburg position, the patient is placed on an egg-crate mattress, and both the patient and the mattress are taped to the table. The arms also are tucked to the sides in a manner more resembling robotic positioning than the positioning traditionally associated with laparoscopic surgery. For morcellation, the patient is brought to the standard supine position and then returned to steep Trendelenburg afterward.
Other surgical tips
• Uterine manipulation. In most of our cases of LESS hysterectomy, placement of a traditional uterine manipulator has been unnecessary and, in fact, detracts from the simplicity of our approach, which utilizes the single-tooth tenaculum to manipulate and expose the uterus. We quickly learned that even lightweight manipulators compromise uterine mobility and interfere with the creation of necessary angles. The manipulator becomes like a ball and chain on the cervix.
For total laparoscopic hysterectomy, however, a uterine manipulator can be helpful for the colpotomy. Late placement of the manipulator in these cases – after the lateral attachments are dissected and before colpotomy is performed – works perfectly.
• Control of the uterine vessels. Access to the uterine vessels can be difficult with LESS. It requires severely angulating the uterus to expose the uterine artery and vein, allowing a more direct approach from the umbilicus. With the uterus on significant tension, initial cauterization with the bipolar forceps is performed before ligating the vessels with the harmonic scalpel.
• Cervical amputation. We use a monopolar loop (LiNA Loop or Storz SupraLoop) for amputation of the uterine fundus in supracervical hysterectomies. We place the loop after we’ve carried our dissection down to the middle of the cardinal ligament. The loop is placed at the level of the internal os.
Placement of the LiNA Loop device was more challenging than we expected, as the camera and grasper must be removed and reinserted on opposite sides in order to visualize the entire loop, a process during which the loop can potentially loosen and trap small bowel or other tissue on the nonvisualized side.
Our solution has been to tighten the loop on the cervix and place a Kelly clamp on the shaft of the loop before switching our instruments from side to side. The clamp keeps the loop snug against the cervix. This technique allows us to visualize one side, remove the instruments, and then visualize the other side without worrying that the loop may loosen and cause damage.
• Vaginal cuff closure. When the vaginal apex is easily accessible, transvaginal closure is the simplest method. The vaginal cuff can be closed intracorporeally with a conventional straight needle driver and a curved grasper; however, intra-abdominal closure of the cuff can be technically challenging in LESS. Historically, I used the angulating 5-mm Endo Grasp and a 0-Vicryl suture on a CT-2 needle and secured the stitch on both ends with absorbable Lapra Ty anchors (Ethicon Endo-Surgery). Increasingly, however, I use the EndoStitch (Covidien, Mansfield, Mass.), a 10 mm suturing device, to place interrupted stitches, and I secure each one with the TK Ti-Knot Device (LSI Solutions), an automated knot-tying device.*
• Umbilical suturing. We close the umbilicus with one running 3-4-bite suture through the fascia and peritoneum of 0-Vicryl or 0-PDS (polydioxanone). The skin is closed with three to five sutures – one that reattaches the center of the umbilicus to the fascial plate and one or two inverted sutures on either side that reapproximate the lower and upper poles of the umbilicus.
• Postoperative care. Patients are discharged either the evening of the procedure or, if they choose, the following morning. We use 0.25% Marcaine with epinephrine in the umbilicus for preemptive analgesia. Xeroform gauze is placed in the umbilicus. The wound is then covered with an eye patch and Tegaderm for 3 days. The umbilicus has a poor nerve supply, which helps minimize pain, but it also has a poor blood supply, which slows the healing process. We have found that a 1-week course of broad-spectrum antibiotics promotes and speeds healing.
Outcomes/experience
In 2009, at a set point in time, I transitioned to LESS as the primary approach for all laparoscopic hysterectomies. As a result, I have been able to compare the LESS approach to traditional multiport laparoscopic hysterectomy using my own cases as retrospective controls, free of selection bias. Allowing for a short learning curve of about 20 cases, analysis of our data revealed no significant difference in operative times, blood loss, conversion to laparotomy, or complication rates.
Our patients have had significantly lower pain levels with LESS, which is consistent with the literature. The cosmetic advantages of LESS have also been significant. In addition, the lack of accessory ports in LESS eliminates any potential for port-site complications such as hematoma or hernia. Umbilical hernias have been rare in our patients, occurring in only one or two patients.
Interestingly, we found that as uterine weight increased, operating times with the LESS procedure increased at a lower rate than did operating times with traditional laparoscopy. Clearly, large uteri are more easily removed with a single-port technique using extraperitoneal morcellation than with a traditional four-port technique using an automated morcellator through an accessory port. Extracorporeal morcellation with LESS is also safer and less expensive.
Dr. Wagner has been in private practice in East Northport, N.Y., since 1991. He practices at Huntington (N.Y.) Hospital, where he is the codirector of minimally invasive surgery. He was instrumental in developing the gynecologic residency program at the institution. Dr. Wagner reported that he has no financial disclosures relevant to this Master Class.
*Correction 7/30/2013: This article was updated to reflect new information from the author.
Several years ago, I adopted a single-incision approach to virtually all benign gynecologic laparoscopic procedures as the next logical step in the practice of minimally invasive surgery. In this time, my partner and I have performed more than 450 single-incision hysterectomies using a simple, reproducible technique that differs from other approaches to single-incision laparoscopy, or laparoendoscopic single-site surgery (LESS), as it is most commonly called.
Rather than using articulating instruments, we use a 30-degree 5-mm bariatric-length laparoscope and straight, extra-long instruments. With sequential placement of one instrument at a time and attention to the direction of extra-abdominal hand movements, we create a work space with unimpeded access to the uterus and prevent the clashing of instruments, or "sword fighting," that can come with inserting several instruments through a single port.
Morcellation of the uterine fundus is accomplished extraperitoneally with specimen removal through the umbilicus. Use of a wider port with the LESS technique allows for morcellation by hand under direct vision with a #15 scalpel. This makes morcellation easier, safer, and more efficient than using an automated morcellator placed through a smaller port as in traditional multiport laparoscopic hysterectomy. We have successfully removed multiple uteri in excess of 1,000 grams – including a 3,000-gram uterus – using this technique.
Overall surgical principles/technique
We routinely use either the SILS port (Covidien), which has a predetermined setup of channels as depicted in the illustrations, or the GelPoint (Applied Medical), which allows for various trocar arrangements. Other single-incision ports can be used, though; the key to the procedure lies not in the port used, but in the placement of the instruments. A right-angled light connector also is essential, as it deviates the light cord out of the surgical field.
Regardless of the single-incision port used, the camera and a laparoscopic single-tooth tenaculum are placed in the lateral trocars, in the same horizontal plane. The active, working instrument – either Kleppinger bipolar forceps or a 45-cm Harmonic ACE Shears (Ethicon Endo-Surgery) – is then placed in the middle trocar.
While the use of angled instruments may seem helpful for creating appropriate triangulation in LESS, we have found that such instrumentation is actually counterproductive. Angled instrumentation creates new angles, in essence, which complicates instrument placement and makes it more difficult to achieve enough intra-abdominal working space and avoid sword fighting.
One exception is the laparoscope. We have found that a 30-degree 5-mm bariatric-length laparoscope works best. When exposing the right side of the uterus, the laparoscope is first inserted into the far left trocar and directed toward the right lower quadrant of the abdomen. The camera is then angled to visualize the uterus from a slightly elevated position. In this position, the operator’s external hand – holding the camera – is now deviated inferiorly and to the left side of the patient.
A 5-mm single-tooth tenaculum is then inserted into the other lateral trocar and used to manipulate the uterus anteriorly and to the left. In a simple supracervical hysterectomy, once the uterus is properly positioned, the utero-ovarian ligament and fallopian tube are exposed. In surgeries involving oophorectomy, the ovary rather than the uterus is first grasped and deviated medially and elevated, exposing the infundibulopelvic ligament. In this position, the assistant’s external hand is now deviated slightly inferiorly and to the right side of the patient.
When properly placed, the camera and the tenaculum are crossed intra-abdominally and held in slightly elevated positions. This allows for insertion of the active instrument underneath both the camera and grasper and directly toward the tissue to be incised. The slight elevation and intra-abdominal crossing of the instruments, while at first confusing, serves to create the angles that give the surgeon good external work space as well as excellent internal range of motion. We apply a significant amount of tension on the uterus to create this working space. The greater the deviation of the uterus (and the longer the instruments), the more work space there is.
With correct instrument placement, the active trocar has direct access to the uterus, so insertion of an instrument is simple, ergonomic, and intuitive. With this positioning, the active instrument (bipolar forceps, harmonic scalpel, suction, or probe) also has complete freedom of movement internally and externally. The operator’s hand can move superiorly, inferiorly, or laterally as needed to access the uterus.
We utilize the Kleppinger forceps and the 45-cm Harmonic Ace Shears for all of our dissection. Because the uterus is held on some tension, we first coagulate all vascular pedicles with the Kleppinger forceps before cutting. For safety, the uterine arteries are transected fairly high, just cephalad to the internal os. This gives us plenty of room to safely grasp and recoagulate a bleeding pedicle without fear of injuring the ureter.
Sequential instrument placement is key to this technique. If sword fighting occurs, one must reexamine the sequence of instrument placement and pay greater attention to the direction of extra-abdominal hand movements and subsequent angles. Again, the laparoscope and grasper must be inserted, positioned, and frozen in place before the active instrument is introduced.
Once one side of the uterus has been dissected free and the uterine artery transected, then all instruments are removed and replaced in a mirror-image manner to access the opposite side. Essentially, the camera and grasper switch trocars, and the active instrument remains in the middle.
Abdominal entry is performed with the traditional open laparoscopy technique described by Dr. Harrith Hasson of Chicago (Am. J. Obstet. Gynecol. 1971;110:886-7). While single-channel trocars generally require a 5- to 10-mm incision, LESS multichannel ports require a slightly larger incision. We recommend a straight vertical incision of about 2 cm through the center of the umbilicus.
The position of the surgeon also differs from multipart laparoscopy. With LESS, the surgeon stands in line with the port and the pathology, usually between the patient’s head and shoulder, and holds either the grasper or camera while operating the active blade. To prevent sliding in a steep Trendelenburg position, the patient is placed on an egg-crate mattress, and both the patient and the mattress are taped to the table. The arms also are tucked to the sides in a manner more resembling robotic positioning than the positioning traditionally associated with laparoscopic surgery. For morcellation, the patient is brought to the standard supine position and then returned to steep Trendelenburg afterward.
Other surgical tips
• Uterine manipulation. In most of our cases of LESS hysterectomy, placement of a traditional uterine manipulator has been unnecessary and, in fact, detracts from the simplicity of our approach, which utilizes the single-tooth tenaculum to manipulate and expose the uterus. We quickly learned that even lightweight manipulators compromise uterine mobility and interfere with the creation of necessary angles. The manipulator becomes like a ball and chain on the cervix.
For total laparoscopic hysterectomy, however, a uterine manipulator can be helpful for the colpotomy. Late placement of the manipulator in these cases – after the lateral attachments are dissected and before colpotomy is performed – works perfectly.
• Control of the uterine vessels. Access to the uterine vessels can be difficult with LESS. It requires severely angulating the uterus to expose the uterine artery and vein, allowing a more direct approach from the umbilicus. With the uterus on significant tension, initial cauterization with the bipolar forceps is performed before ligating the vessels with the harmonic scalpel.
• Cervical amputation. We use a monopolar loop (LiNA Loop or Storz SupraLoop) for amputation of the uterine fundus in supracervical hysterectomies. We place the loop after we’ve carried our dissection down to the middle of the cardinal ligament. The loop is placed at the level of the internal os.
Placement of the LiNA Loop device was more challenging than we expected, as the camera and grasper must be removed and reinserted on opposite sides in order to visualize the entire loop, a process during which the loop can potentially loosen and trap small bowel or other tissue on the nonvisualized side.
Our solution has been to tighten the loop on the cervix and place a Kelly clamp on the shaft of the loop before switching our instruments from side to side. The clamp keeps the loop snug against the cervix. This technique allows us to visualize one side, remove the instruments, and then visualize the other side without worrying that the loop may loosen and cause damage.
• Vaginal cuff closure. When the vaginal apex is easily accessible, transvaginal closure is the simplest method. The vaginal cuff can be closed intracorporeally with a conventional straight needle driver and a curved grasper; however, intra-abdominal closure of the cuff can be technically challenging in LESS. Historically, I used the angulating 5-mm Endo Grasp and a 0-Vicryl suture on a CT-2 needle and secured the stitch on both ends with absorbable Lapra Ty anchors (Ethicon Endo-Surgery). Increasingly, however, I use the EndoStitch (Covidien, Mansfield, Mass.), a 10 mm suturing device, to place interrupted stitches, and I secure each one with the TK Ti-Knot Device (LSI Solutions), an automated knot-tying device.*
• Umbilical suturing. We close the umbilicus with one running 3-4-bite suture through the fascia and peritoneum of 0-Vicryl or 0-PDS (polydioxanone). The skin is closed with three to five sutures – one that reattaches the center of the umbilicus to the fascial plate and one or two inverted sutures on either side that reapproximate the lower and upper poles of the umbilicus.
• Postoperative care. Patients are discharged either the evening of the procedure or, if they choose, the following morning. We use 0.25% Marcaine with epinephrine in the umbilicus for preemptive analgesia. Xeroform gauze is placed in the umbilicus. The wound is then covered with an eye patch and Tegaderm for 3 days. The umbilicus has a poor nerve supply, which helps minimize pain, but it also has a poor blood supply, which slows the healing process. We have found that a 1-week course of broad-spectrum antibiotics promotes and speeds healing.
Outcomes/experience
In 2009, at a set point in time, I transitioned to LESS as the primary approach for all laparoscopic hysterectomies. As a result, I have been able to compare the LESS approach to traditional multiport laparoscopic hysterectomy using my own cases as retrospective controls, free of selection bias. Allowing for a short learning curve of about 20 cases, analysis of our data revealed no significant difference in operative times, blood loss, conversion to laparotomy, or complication rates.
Our patients have had significantly lower pain levels with LESS, which is consistent with the literature. The cosmetic advantages of LESS have also been significant. In addition, the lack of accessory ports in LESS eliminates any potential for port-site complications such as hematoma or hernia. Umbilical hernias have been rare in our patients, occurring in only one or two patients.
Interestingly, we found that as uterine weight increased, operating times with the LESS procedure increased at a lower rate than did operating times with traditional laparoscopy. Clearly, large uteri are more easily removed with a single-port technique using extraperitoneal morcellation than with a traditional four-port technique using an automated morcellator through an accessory port. Extracorporeal morcellation with LESS is also safer and less expensive.
Dr. Wagner has been in private practice in East Northport, N.Y., since 1991. He practices at Huntington (N.Y.) Hospital, where he is the codirector of minimally invasive surgery. He was instrumental in developing the gynecologic residency program at the institution. Dr. Wagner reported that he has no financial disclosures relevant to this Master Class.
*Correction 7/30/2013: This article was updated to reflect new information from the author.
Several years ago, I adopted a single-incision approach to virtually all benign gynecologic laparoscopic procedures as the next logical step in the practice of minimally invasive surgery. In this time, my partner and I have performed more than 450 single-incision hysterectomies using a simple, reproducible technique that differs from other approaches to single-incision laparoscopy, or laparoendoscopic single-site surgery (LESS), as it is most commonly called.
Rather than using articulating instruments, we use a 30-degree 5-mm bariatric-length laparoscope and straight, extra-long instruments. With sequential placement of one instrument at a time and attention to the direction of extra-abdominal hand movements, we create a work space with unimpeded access to the uterus and prevent the clashing of instruments, or "sword fighting," that can come with inserting several instruments through a single port.
Morcellation of the uterine fundus is accomplished extraperitoneally with specimen removal through the umbilicus. Use of a wider port with the LESS technique allows for morcellation by hand under direct vision with a #15 scalpel. This makes morcellation easier, safer, and more efficient than using an automated morcellator placed through a smaller port as in traditional multiport laparoscopic hysterectomy. We have successfully removed multiple uteri in excess of 1,000 grams – including a 3,000-gram uterus – using this technique.
Overall surgical principles/technique
We routinely use either the SILS port (Covidien), which has a predetermined setup of channels as depicted in the illustrations, or the GelPoint (Applied Medical), which allows for various trocar arrangements. Other single-incision ports can be used, though; the key to the procedure lies not in the port used, but in the placement of the instruments. A right-angled light connector also is essential, as it deviates the light cord out of the surgical field.
Regardless of the single-incision port used, the camera and a laparoscopic single-tooth tenaculum are placed in the lateral trocars, in the same horizontal plane. The active, working instrument – either Kleppinger bipolar forceps or a 45-cm Harmonic ACE Shears (Ethicon Endo-Surgery) – is then placed in the middle trocar.
While the use of angled instruments may seem helpful for creating appropriate triangulation in LESS, we have found that such instrumentation is actually counterproductive. Angled instrumentation creates new angles, in essence, which complicates instrument placement and makes it more difficult to achieve enough intra-abdominal working space and avoid sword fighting.
One exception is the laparoscope. We have found that a 30-degree 5-mm bariatric-length laparoscope works best. When exposing the right side of the uterus, the laparoscope is first inserted into the far left trocar and directed toward the right lower quadrant of the abdomen. The camera is then angled to visualize the uterus from a slightly elevated position. In this position, the operator’s external hand – holding the camera – is now deviated inferiorly and to the left side of the patient.
A 5-mm single-tooth tenaculum is then inserted into the other lateral trocar and used to manipulate the uterus anteriorly and to the left. In a simple supracervical hysterectomy, once the uterus is properly positioned, the utero-ovarian ligament and fallopian tube are exposed. In surgeries involving oophorectomy, the ovary rather than the uterus is first grasped and deviated medially and elevated, exposing the infundibulopelvic ligament. In this position, the assistant’s external hand is now deviated slightly inferiorly and to the right side of the patient.
When properly placed, the camera and the tenaculum are crossed intra-abdominally and held in slightly elevated positions. This allows for insertion of the active instrument underneath both the camera and grasper and directly toward the tissue to be incised. The slight elevation and intra-abdominal crossing of the instruments, while at first confusing, serves to create the angles that give the surgeon good external work space as well as excellent internal range of motion. We apply a significant amount of tension on the uterus to create this working space. The greater the deviation of the uterus (and the longer the instruments), the more work space there is.
With correct instrument placement, the active trocar has direct access to the uterus, so insertion of an instrument is simple, ergonomic, and intuitive. With this positioning, the active instrument (bipolar forceps, harmonic scalpel, suction, or probe) also has complete freedom of movement internally and externally. The operator’s hand can move superiorly, inferiorly, or laterally as needed to access the uterus.
We utilize the Kleppinger forceps and the 45-cm Harmonic Ace Shears for all of our dissection. Because the uterus is held on some tension, we first coagulate all vascular pedicles with the Kleppinger forceps before cutting. For safety, the uterine arteries are transected fairly high, just cephalad to the internal os. This gives us plenty of room to safely grasp and recoagulate a bleeding pedicle without fear of injuring the ureter.
Sequential instrument placement is key to this technique. If sword fighting occurs, one must reexamine the sequence of instrument placement and pay greater attention to the direction of extra-abdominal hand movements and subsequent angles. Again, the laparoscope and grasper must be inserted, positioned, and frozen in place before the active instrument is introduced.
Once one side of the uterus has been dissected free and the uterine artery transected, then all instruments are removed and replaced in a mirror-image manner to access the opposite side. Essentially, the camera and grasper switch trocars, and the active instrument remains in the middle.
Abdominal entry is performed with the traditional open laparoscopy technique described by Dr. Harrith Hasson of Chicago (Am. J. Obstet. Gynecol. 1971;110:886-7). While single-channel trocars generally require a 5- to 10-mm incision, LESS multichannel ports require a slightly larger incision. We recommend a straight vertical incision of about 2 cm through the center of the umbilicus.
The position of the surgeon also differs from multipart laparoscopy. With LESS, the surgeon stands in line with the port and the pathology, usually between the patient’s head and shoulder, and holds either the grasper or camera while operating the active blade. To prevent sliding in a steep Trendelenburg position, the patient is placed on an egg-crate mattress, and both the patient and the mattress are taped to the table. The arms also are tucked to the sides in a manner more resembling robotic positioning than the positioning traditionally associated with laparoscopic surgery. For morcellation, the patient is brought to the standard supine position and then returned to steep Trendelenburg afterward.
Other surgical tips
• Uterine manipulation. In most of our cases of LESS hysterectomy, placement of a traditional uterine manipulator has been unnecessary and, in fact, detracts from the simplicity of our approach, which utilizes the single-tooth tenaculum to manipulate and expose the uterus. We quickly learned that even lightweight manipulators compromise uterine mobility and interfere with the creation of necessary angles. The manipulator becomes like a ball and chain on the cervix.
For total laparoscopic hysterectomy, however, a uterine manipulator can be helpful for the colpotomy. Late placement of the manipulator in these cases – after the lateral attachments are dissected and before colpotomy is performed – works perfectly.
• Control of the uterine vessels. Access to the uterine vessels can be difficult with LESS. It requires severely angulating the uterus to expose the uterine artery and vein, allowing a more direct approach from the umbilicus. With the uterus on significant tension, initial cauterization with the bipolar forceps is performed before ligating the vessels with the harmonic scalpel.
• Cervical amputation. We use a monopolar loop (LiNA Loop or Storz SupraLoop) for amputation of the uterine fundus in supracervical hysterectomies. We place the loop after we’ve carried our dissection down to the middle of the cardinal ligament. The loop is placed at the level of the internal os.
Placement of the LiNA Loop device was more challenging than we expected, as the camera and grasper must be removed and reinserted on opposite sides in order to visualize the entire loop, a process during which the loop can potentially loosen and trap small bowel or other tissue on the nonvisualized side.
Our solution has been to tighten the loop on the cervix and place a Kelly clamp on the shaft of the loop before switching our instruments from side to side. The clamp keeps the loop snug against the cervix. This technique allows us to visualize one side, remove the instruments, and then visualize the other side without worrying that the loop may loosen and cause damage.
• Vaginal cuff closure. When the vaginal apex is easily accessible, transvaginal closure is the simplest method. The vaginal cuff can be closed intracorporeally with a conventional straight needle driver and a curved grasper; however, intra-abdominal closure of the cuff can be technically challenging in LESS. Historically, I used the angulating 5-mm Endo Grasp and a 0-Vicryl suture on a CT-2 needle and secured the stitch on both ends with absorbable Lapra Ty anchors (Ethicon Endo-Surgery). Increasingly, however, I use the EndoStitch (Covidien, Mansfield, Mass.), a 10 mm suturing device, to place interrupted stitches, and I secure each one with the TK Ti-Knot Device (LSI Solutions), an automated knot-tying device.*
• Umbilical suturing. We close the umbilicus with one running 3-4-bite suture through the fascia and peritoneum of 0-Vicryl or 0-PDS (polydioxanone). The skin is closed with three to five sutures – one that reattaches the center of the umbilicus to the fascial plate and one or two inverted sutures on either side that reapproximate the lower and upper poles of the umbilicus.
• Postoperative care. Patients are discharged either the evening of the procedure or, if they choose, the following morning. We use 0.25% Marcaine with epinephrine in the umbilicus for preemptive analgesia. Xeroform gauze is placed in the umbilicus. The wound is then covered with an eye patch and Tegaderm for 3 days. The umbilicus has a poor nerve supply, which helps minimize pain, but it also has a poor blood supply, which slows the healing process. We have found that a 1-week course of broad-spectrum antibiotics promotes and speeds healing.
Outcomes/experience
In 2009, at a set point in time, I transitioned to LESS as the primary approach for all laparoscopic hysterectomies. As a result, I have been able to compare the LESS approach to traditional multiport laparoscopic hysterectomy using my own cases as retrospective controls, free of selection bias. Allowing for a short learning curve of about 20 cases, analysis of our data revealed no significant difference in operative times, blood loss, conversion to laparotomy, or complication rates.
Our patients have had significantly lower pain levels with LESS, which is consistent with the literature. The cosmetic advantages of LESS have also been significant. In addition, the lack of accessory ports in LESS eliminates any potential for port-site complications such as hematoma or hernia. Umbilical hernias have been rare in our patients, occurring in only one or two patients.
Interestingly, we found that as uterine weight increased, operating times with the LESS procedure increased at a lower rate than did operating times with traditional laparoscopy. Clearly, large uteri are more easily removed with a single-port technique using extraperitoneal morcellation than with a traditional four-port technique using an automated morcellator through an accessory port. Extracorporeal morcellation with LESS is also safer and less expensive.
Dr. Wagner has been in private practice in East Northport, N.Y., since 1991. He practices at Huntington (N.Y.) Hospital, where he is the codirector of minimally invasive surgery. He was instrumental in developing the gynecologic residency program at the institution. Dr. Wagner reported that he has no financial disclosures relevant to this Master Class.
*Correction 7/30/2013: This article was updated to reflect new information from the author.