User login
The sexually transmitted disease (STD) epidemic in the United States is intensifying, and it disproportionately impacts high-risk communities. In 2018, rates of reportable STDs, including syphilis and Neisseria gonorrhoeae and Chlamydia trachomatis infections, reached an all-time high.1 That year, there were 1.8 million cases of chlamydia (increased 19% since 2014), 583,405 cases of gonorrhea (increased 63% since 2014), and 35,063 cases of primary and secondary syphilis (71% increase from 2014).1
Cases of newborn syphilis have more than doubled in 4 years, with rates reaching a 20-year high.1
This surge has not received the attention it deserves given the broad-reaching impact of these infections on women’s health and maternal-child health.2 As ObGyns, we are on the front line, and we need to be engaged in evidence-based strategies and population-based health initiatives to expedite diagnoses and treatment and to reduce the ongoing spread of these infections.
Disparities exist and continue to fuel this epidemic
The STD burden is disproportionately high among reproductive-aged women, and half of all reported STDs occur in women aged 15 to 24 years. African American women have rates up to 12 times higher than white women.3,4 Substantial geographic variability also exists, with the South, Southeast, and West having some of the highest STD rates.
These disparities are fueled by inequalities in socioeconomic status (SES), including employment, insurance, education, incarceration, stress/trauma exposure, and discrimination.5-7 Those with lower SES often have trouble accessing and affording quality health care, including sexual health services. Access to quality health care, including STD prevention and treatment, that meets the needs of lower SES populations is key to reducing STD disparities in the United States; however, access likely will be insufficient unless the structural inequities that drive these disparities are addressed.
Clinical consequences for women, infants, and mothers
STDs are most prevalent among reproductive-aged women and can lead to pelvic inflammatory disease, infertility, ectopic pregnancy,4,8 and increased risk of acquiring human immunodeficiency virus (HIV). STDs during pregnancy present additional consequences. Congenital syphilis is perhaps the most salient, with neonates experiencing substantial disability or death.
In addition, STDs contribute to overall peripartum and long-term adverse health outcomes.4,9,10 Untreated chlamydia infection, for example, is associated with neonatal pneumonia, neonatal conjunctivitis, low birth weight, premature rupture of membranes, preterm labor, and postpartum endometritis.2,11 Untreated gonorrhea is linked to disseminated gonococcal infection in the newborn, neonatal conjunctivitis, low birth weight, miscarriage, premature rupture of membranes, preterm labor, and chorioamnionitis.2,12
As preterm birth is the leading cause of infant morbidity and mortality and disproportionately affects African American women and women in the southeastern United States,13 there is a critical public heath need to improve STD screening, treatment, and prevention of reinfection among high-risk pregnant women.
Quality clinical services for STDs: Areas for focus
More and more, STDs are being diagnosed in primary care settings. In January 2020, the Centers for Disease Control and Prevention (CDC) released a document, referred to as STD QCS (quality clinical services), that outlines recommendations for basic and specialty-level STD clinical services.14 ObGyns and other clinicians who provide primary care should meet the basic recommendations as a minimum.
The STD QCS outlines 8 recommendation areas: sexual history and physical examination, prevention, screening,
Continue to: Sexual history and physical examination...
Sexual history and physical examination
A complete sexual history and risk assessment should be performed at a complete initial or annual visit and as indicated. Routinely updating the sexual history and risk assessment is important to normalize these questions within the frame of the person’s overall health, and it may be valuable in reducing stigma. This routine approach may be important particularly for younger patients and others whose risk for STDs may change frequently and dramatically.
Creating a safe space that permits privacy and assurance of confidentiality may help build trust and set the stage for disclosure. The American College of Obstetricians and Gynecologists recommends that all young people have time alone without parents for confidential counseling and discussion.15 All states allow minors to consent for STD services themselves, although 11 states limit this to those beyond a certain age.16
The CDC recommends using the 5 P’s—partners, practices, protection, past history of STDs, and prevention of pregnancy—as a guide for discussion.14 ObGyns are more likely than other providers to perform this screening routinely. While a pelvic examination should be available for STD evaluation as needed, it is not required for routine screening.
Prevention
ObGyns should employ several recommendations for STD prevention. These include providing or referring patients for vaccination against hepatitis B and human papillomavirus and providing brief STD/HIV prevention counseling along with contraceptive counseling. ObGyns should be familiar with HIV pre-exposure prophylaxis (PrEP) and nonoccupational postexposure prophylaxis (nPEP) and provide risk assessment, education, and referral or link to HIV care. Providing these services would improve access to care and further remove barriers to care. ObGyns also could consider providing condoms in their offices.14
Screening
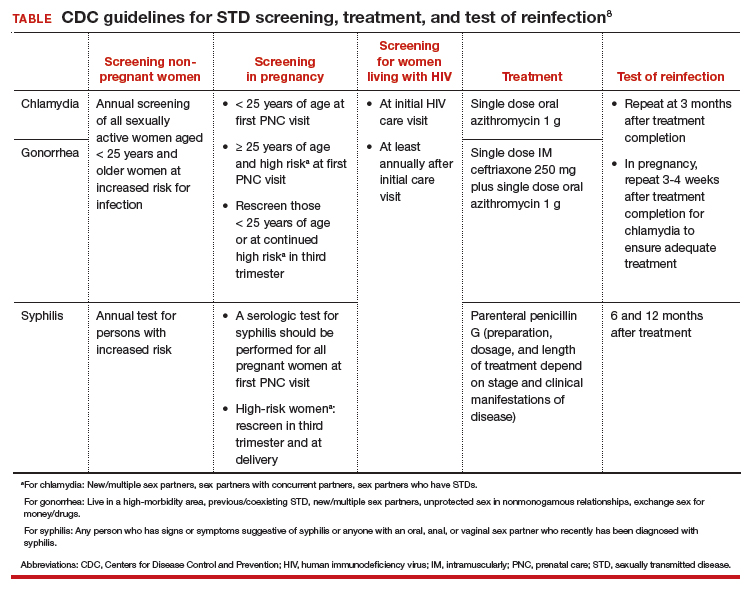
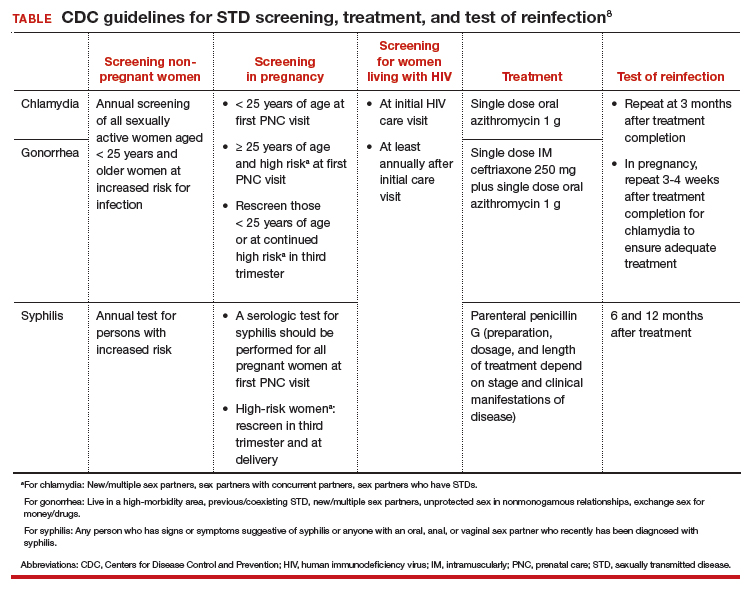
STD screening of women at risk is critical since more than 80% of infected women are asymptomatic.8 Because young people are disproportionately experiencing STDs, annual screening for chlamydia and gonorrhea is recommended for women younger than 25 years. For women older than 25, those at increased risk can be screened.
Risk factors for chlamydia infection include having new or multiple sex partners, sex partners with concurrent partners, or sex partners who have an STD. For gonorrhea, risk factors include living in a high-morbidity area, having a previous or coexisting STD, new or multiple sex partners, inconsistent condom use in people who are not in a mutually monogamous relationship, and exchanging sex for money or drugs. Screening for syphilis in nonpregnant women is recommended for those who have had any sexual activity with a person recently diagnosed with syphilis or those who personally display signs or symptoms of infection.17
STD screening is especially important for pregnant women, and treatment of infections may improve pregnancy outcomes. The CDC recommends screening at the first prenatal care visit for chlamydia and gonorrhea in pregnant women younger than 25 years of age and in older pregnant women at increased risk; women younger than 25 years or at continued high risk should be rescreened in their third trimester. The CDC recommends screening all women for syphilis at their first prenatal care visit and rescreening those at high risk in the third trimester and at delivery (TABLE).18
Continue to: Partner services...
Partner services
Clearly outlined partner management services is paramount for preventing STD reinfection.14 Reinfection rates for chlamydia and gonorrhea among young women are high and vary by study population.19 At a minimum, ObGyns should counsel patients with an STD that their partner(s) should be notified and encouraged to seek services.
For states in which it is legal, expedited partner therapy (EPT)—the clinician provides medication for the partner without seeing the partner—should be provided for chlamydia or gonorrhea if the partner is unlikely to access timely care. EPT is legal in most states. (To check the legal status of EPT in your state, visit https://www.cdc.gov/std/ept/legal/default.htm.) Research is needed to evaluate optimal strategies for effective implementation of EPT services in different clinical settings.
Laboratory tests
ObGyns should be able to provide a wide range of laboratory evaluations (for example, a nucleic acid amplification test [NAAT] for genital chlamydia and gonorrhea, quantitative nontreponemal serologic test for syphilis, treponemal serologic test for syphilis) that can be ordered for screening or diagnostic purposes. To improve rates of recommended screening, consider having clinic-level policies that support screening, such as standing orders, express or walk-in screening appointments, lab panels, and reflex testing.
Further, having rapid results or point-of-care testing available would help decrease lags in time to treatment. Delays in treatment are particularly important in lower-resource communities; thus, point-of-care testing may be especially valuable with immediate access to treatment on site.
Treatment
Adequate and timely treatment of STDs is critical to decrease sequelae and the likelihood of transmission to others. Treatment is evolving, particularly for gonorrhea. Over the past several years, gonorrhea has become resistant to 6 previously recommended treatment options.20 Since 2015, the CDC recommends dual therapy for gonorrhea with an injection of ceftriaxone and oral azithromycin.
The first-line recommended treatments for bacterial STDs are listed in the TABLE. When possible, it is preferred to offer directly observed therapy at the time of the visit. This decreases the time to treatment and ensures that therapy is completed.
A call to action for ObGyns
Clinicians have multiple opportunities to address and reduce the surge of STDs in the United States. We play a critical role in screening, diagnosing, and treating patients, and it is thus imperative to be up-to-date on the recommended guidelines. Further, clinicians can advocate for more rapid testing modalities, with the goal of obtaining point-of-care testing results when possible and implementing strategies to improve partner treatment.
While a positive STD result may be associated with significant patient distress, it also may be an opportunity for enhancing the patient-provider relationship, coupling education with motivational approaches to help patients increase protective health behaviors.
It is critical to approach clinical care in a nonjudgmental manner to improve patients’ comfort in their relationship with the health care system. ●
- Be aware of up-to-date screening, treatment, and follow-up recommendations for STDs
- Develop strategies to maximize partner treatment, including expedited partner therapy
- Identify high-risk individuals for whom counseling on HIV and unintended pregnancy prevention strategies can be reinforced, including PrEP and contraception
- Create a clinical environment that normalizes STD testing and destigmatizes infection
- Integrate client-centered counseling to improve protective health behaviors
Abbreviations: HIV, human immunodeficiency virus; PrEP, pre-exposure prophylaxis; STD, sexually transmitted disease.
- Centers for Disease Control and Prevention. 2018 STD surveillance report. https://www.cdc.gov/nchhstp /newsroom/2019/2018-STD-surveillance-report.html. Accessed March 19, 2020.
- Centers for Disease Control and Prevention. Sexually transmitted diseases (STDs): STDs during pregnancy—CDC fact sheet (detailed). www.cdc.gov/std/pregnancy/stdfact -sheet-pregnancy-detailed.htm. Accessed March 19, 2020.
- Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2017: STDs in racial and ethnic minorities 2017. https://www.cdc.gov/std/stats17 /minorities.htm. Accessed March 19, 2020.
- Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2017: STDs in women and infants. https://www.cdc.gov/std/stats17/womenandinf .htm. Accessed March 19, 2020.
- Semega JL, Fontenot KR, Kollar MA; US Census Bureau. Income and poverty in the United States: 2016. Washington, DC: US Government Printing Office; 2017. https://www.census.gov/content/dam/Census/library /publications/2017/demo/P60-259.pdf. Accessed March 19, 2020.
- Harling G, Subramanian S, Barnighausen T, et al. Socioeconomic disparities in sexually transmitted infections among young adults in the United States: examining the interaction between income and race/ethnicity. Sex Transm Dis. 2013;40:575-581.
- Meyer PA, Penman-Aguilar A, Campbell VA, et al; Centers for Disease Control and Prevention. Conclusion and future directions: CDC Health Disparities and Inequalities Report— United States, 2013. MMWR Suppl. 2013;62(3):184-186.
- Workowski KA, Bolan GA; Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64(RR-03): 1-137.
- Elliott B, Brunham RC, Laga M, et al. Maternal gonococcal infection as a preventable risk factor for low birth weight. J Infect Dis. 1990;161:531-536.
- Warr AJ, Pintye J, Kinuthia J, et al. Sexually transmitted infections during pregnancy and subsequent risk of stillbirth and infant mortality in Kenya: a prospective study. Sex Transm Infect. 2019;95:60-66.
- Andrews WW, Goldenberg RL, Mercer B, et al. The Preterm Prediction Study: association of second-trimester genitourinary chlamydia infection with subsequent spontaneous preterm birth. Am J Obstet Gynecol. 2000;183:662-668.
- Alger LS, Lovchik JC, Hebel JR, et al. The association of Chlamydia trachomatis, Neisseria gonorrhoeae, and group B streptococci with preterm rupture of the membranes and pregnancy outcome. Am J Obstet Gynecol. 1988;159:397-404.
- March of Dimes. Maternal, infant, and child health in the United States, 2016. https://www.marchofdimes.org /materials/March-of-Dimes-2016-Databook.pdf. Accessed March 19, 2020.
- Barrow RY, Ahmed F, Bolan GA, et al. Recommendations for providing quality sexually transmitted diseases clinical services, 2020. MMWR Recomm Rep. 2020;68(5):1-20.
- American College of Obstetricians and Gynecologists. ACOG committee opinion No. 598: The initial reproductive health visit. May 2014. https:// www.acog.org/-/media /project/acog/acogorg/clinical/files/committee-opinion /articles/2014/05/the-initial-reproductive-health-visit.pdf. Accessed March 31, 2020.
- Guttmacher Institute. An overview of consent to reproductive health services by young people. March 1, 2020. https://www .guttmacher.org/state-policy/explore/overview-minors -consent-law. Accessed March 19, 2020.
- Centers for Disease Control and Prevention. Pocket guide for providers: Syphilis: a provider’s guide to treatment and prevention. 2017. https://www.cdc.gov/std/syphilis /Syphilis-Pocket-Guide-FINAL-508.pdf. Accessed March 19, 2020.
- Centers for Disease Control and Prevention. 2015 Sexually transmitted diseases treatment guidelines: syphilis during pregnancy. https://www.cdc.gov/std/tg2015/syphilis -pregnancy.htm. Accessed March 19, 2020.
- Hosenfeld CB, Workowski KA, Berman S, et al. Repeat infection with chlamydia and gonorrhea among females: a systematic review of the literature. Sex Transm Dis. 2009;36:478-489.
- Bodie M, Gale-Rowe M, Alexandre S, et al. Addressing the rising rates of gonorrhea and drug-resistant gonorrhea: there is no time like the present. Can Commun Dis Rep. 2019;45:54-62.
The sexually transmitted disease (STD) epidemic in the United States is intensifying, and it disproportionately impacts high-risk communities. In 2018, rates of reportable STDs, including syphilis and Neisseria gonorrhoeae and Chlamydia trachomatis infections, reached an all-time high.1 That year, there were 1.8 million cases of chlamydia (increased 19% since 2014), 583,405 cases of gonorrhea (increased 63% since 2014), and 35,063 cases of primary and secondary syphilis (71% increase from 2014).1
Cases of newborn syphilis have more than doubled in 4 years, with rates reaching a 20-year high.1
This surge has not received the attention it deserves given the broad-reaching impact of these infections on women’s health and maternal-child health.2 As ObGyns, we are on the front line, and we need to be engaged in evidence-based strategies and population-based health initiatives to expedite diagnoses and treatment and to reduce the ongoing spread of these infections.
Disparities exist and continue to fuel this epidemic
The STD burden is disproportionately high among reproductive-aged women, and half of all reported STDs occur in women aged 15 to 24 years. African American women have rates up to 12 times higher than white women.3,4 Substantial geographic variability also exists, with the South, Southeast, and West having some of the highest STD rates.
These disparities are fueled by inequalities in socioeconomic status (SES), including employment, insurance, education, incarceration, stress/trauma exposure, and discrimination.5-7 Those with lower SES often have trouble accessing and affording quality health care, including sexual health services. Access to quality health care, including STD prevention and treatment, that meets the needs of lower SES populations is key to reducing STD disparities in the United States; however, access likely will be insufficient unless the structural inequities that drive these disparities are addressed.
Clinical consequences for women, infants, and mothers
STDs are most prevalent among reproductive-aged women and can lead to pelvic inflammatory disease, infertility, ectopic pregnancy,4,8 and increased risk of acquiring human immunodeficiency virus (HIV). STDs during pregnancy present additional consequences. Congenital syphilis is perhaps the most salient, with neonates experiencing substantial disability or death.
In addition, STDs contribute to overall peripartum and long-term adverse health outcomes.4,9,10 Untreated chlamydia infection, for example, is associated with neonatal pneumonia, neonatal conjunctivitis, low birth weight, premature rupture of membranes, preterm labor, and postpartum endometritis.2,11 Untreated gonorrhea is linked to disseminated gonococcal infection in the newborn, neonatal conjunctivitis, low birth weight, miscarriage, premature rupture of membranes, preterm labor, and chorioamnionitis.2,12
As preterm birth is the leading cause of infant morbidity and mortality and disproportionately affects African American women and women in the southeastern United States,13 there is a critical public heath need to improve STD screening, treatment, and prevention of reinfection among high-risk pregnant women.
Quality clinical services for STDs: Areas for focus
More and more, STDs are being diagnosed in primary care settings. In January 2020, the Centers for Disease Control and Prevention (CDC) released a document, referred to as STD QCS (quality clinical services), that outlines recommendations for basic and specialty-level STD clinical services.14 ObGyns and other clinicians who provide primary care should meet the basic recommendations as a minimum.
The STD QCS outlines 8 recommendation areas: sexual history and physical examination, prevention, screening,
Continue to: Sexual history and physical examination...
Sexual history and physical examination
A complete sexual history and risk assessment should be performed at a complete initial or annual visit and as indicated. Routinely updating the sexual history and risk assessment is important to normalize these questions within the frame of the person’s overall health, and it may be valuable in reducing stigma. This routine approach may be important particularly for younger patients and others whose risk for STDs may change frequently and dramatically.
Creating a safe space that permits privacy and assurance of confidentiality may help build trust and set the stage for disclosure. The American College of Obstetricians and Gynecologists recommends that all young people have time alone without parents for confidential counseling and discussion.15 All states allow minors to consent for STD services themselves, although 11 states limit this to those beyond a certain age.16
The CDC recommends using the 5 P’s—partners, practices, protection, past history of STDs, and prevention of pregnancy—as a guide for discussion.14 ObGyns are more likely than other providers to perform this screening routinely. While a pelvic examination should be available for STD evaluation as needed, it is not required for routine screening.
Prevention
ObGyns should employ several recommendations for STD prevention. These include providing or referring patients for vaccination against hepatitis B and human papillomavirus and providing brief STD/HIV prevention counseling along with contraceptive counseling. ObGyns should be familiar with HIV pre-exposure prophylaxis (PrEP) and nonoccupational postexposure prophylaxis (nPEP) and provide risk assessment, education, and referral or link to HIV care. Providing these services would improve access to care and further remove barriers to care. ObGyns also could consider providing condoms in their offices.14
Screening
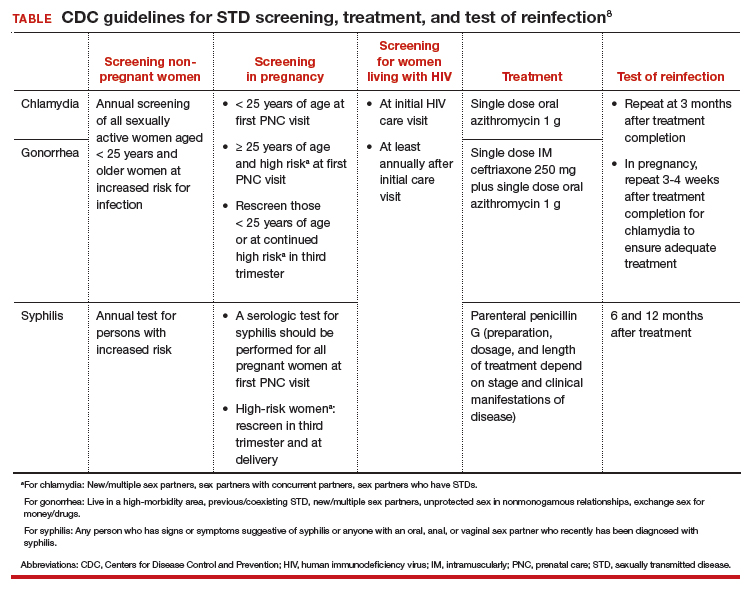
STD screening of women at risk is critical since more than 80% of infected women are asymptomatic.8 Because young people are disproportionately experiencing STDs, annual screening for chlamydia and gonorrhea is recommended for women younger than 25 years. For women older than 25, those at increased risk can be screened.
Risk factors for chlamydia infection include having new or multiple sex partners, sex partners with concurrent partners, or sex partners who have an STD. For gonorrhea, risk factors include living in a high-morbidity area, having a previous or coexisting STD, new or multiple sex partners, inconsistent condom use in people who are not in a mutually monogamous relationship, and exchanging sex for money or drugs. Screening for syphilis in nonpregnant women is recommended for those who have had any sexual activity with a person recently diagnosed with syphilis or those who personally display signs or symptoms of infection.17
STD screening is especially important for pregnant women, and treatment of infections may improve pregnancy outcomes. The CDC recommends screening at the first prenatal care visit for chlamydia and gonorrhea in pregnant women younger than 25 years of age and in older pregnant women at increased risk; women younger than 25 years or at continued high risk should be rescreened in their third trimester. The CDC recommends screening all women for syphilis at their first prenatal care visit and rescreening those at high risk in the third trimester and at delivery (TABLE).18
Continue to: Partner services...
Partner services
Clearly outlined partner management services is paramount for preventing STD reinfection.14 Reinfection rates for chlamydia and gonorrhea among young women are high and vary by study population.19 At a minimum, ObGyns should counsel patients with an STD that their partner(s) should be notified and encouraged to seek services.
For states in which it is legal, expedited partner therapy (EPT)—the clinician provides medication for the partner without seeing the partner—should be provided for chlamydia or gonorrhea if the partner is unlikely to access timely care. EPT is legal in most states. (To check the legal status of EPT in your state, visit https://www.cdc.gov/std/ept/legal/default.htm.) Research is needed to evaluate optimal strategies for effective implementation of EPT services in different clinical settings.
Laboratory tests
ObGyns should be able to provide a wide range of laboratory evaluations (for example, a nucleic acid amplification test [NAAT] for genital chlamydia and gonorrhea, quantitative nontreponemal serologic test for syphilis, treponemal serologic test for syphilis) that can be ordered for screening or diagnostic purposes. To improve rates of recommended screening, consider having clinic-level policies that support screening, such as standing orders, express or walk-in screening appointments, lab panels, and reflex testing.
Further, having rapid results or point-of-care testing available would help decrease lags in time to treatment. Delays in treatment are particularly important in lower-resource communities; thus, point-of-care testing may be especially valuable with immediate access to treatment on site.
Treatment
Adequate and timely treatment of STDs is critical to decrease sequelae and the likelihood of transmission to others. Treatment is evolving, particularly for gonorrhea. Over the past several years, gonorrhea has become resistant to 6 previously recommended treatment options.20 Since 2015, the CDC recommends dual therapy for gonorrhea with an injection of ceftriaxone and oral azithromycin.
The first-line recommended treatments for bacterial STDs are listed in the TABLE. When possible, it is preferred to offer directly observed therapy at the time of the visit. This decreases the time to treatment and ensures that therapy is completed.
A call to action for ObGyns
Clinicians have multiple opportunities to address and reduce the surge of STDs in the United States. We play a critical role in screening, diagnosing, and treating patients, and it is thus imperative to be up-to-date on the recommended guidelines. Further, clinicians can advocate for more rapid testing modalities, with the goal of obtaining point-of-care testing results when possible and implementing strategies to improve partner treatment.
While a positive STD result may be associated with significant patient distress, it also may be an opportunity for enhancing the patient-provider relationship, coupling education with motivational approaches to help patients increase protective health behaviors.
It is critical to approach clinical care in a nonjudgmental manner to improve patients’ comfort in their relationship with the health care system. ●
- Be aware of up-to-date screening, treatment, and follow-up recommendations for STDs
- Develop strategies to maximize partner treatment, including expedited partner therapy
- Identify high-risk individuals for whom counseling on HIV and unintended pregnancy prevention strategies can be reinforced, including PrEP and contraception
- Create a clinical environment that normalizes STD testing and destigmatizes infection
- Integrate client-centered counseling to improve protective health behaviors
Abbreviations: HIV, human immunodeficiency virus; PrEP, pre-exposure prophylaxis; STD, sexually transmitted disease.
The sexually transmitted disease (STD) epidemic in the United States is intensifying, and it disproportionately impacts high-risk communities. In 2018, rates of reportable STDs, including syphilis and Neisseria gonorrhoeae and Chlamydia trachomatis infections, reached an all-time high.1 That year, there were 1.8 million cases of chlamydia (increased 19% since 2014), 583,405 cases of gonorrhea (increased 63% since 2014), and 35,063 cases of primary and secondary syphilis (71% increase from 2014).1
Cases of newborn syphilis have more than doubled in 4 years, with rates reaching a 20-year high.1
This surge has not received the attention it deserves given the broad-reaching impact of these infections on women’s health and maternal-child health.2 As ObGyns, we are on the front line, and we need to be engaged in evidence-based strategies and population-based health initiatives to expedite diagnoses and treatment and to reduce the ongoing spread of these infections.
Disparities exist and continue to fuel this epidemic
The STD burden is disproportionately high among reproductive-aged women, and half of all reported STDs occur in women aged 15 to 24 years. African American women have rates up to 12 times higher than white women.3,4 Substantial geographic variability also exists, with the South, Southeast, and West having some of the highest STD rates.
These disparities are fueled by inequalities in socioeconomic status (SES), including employment, insurance, education, incarceration, stress/trauma exposure, and discrimination.5-7 Those with lower SES often have trouble accessing and affording quality health care, including sexual health services. Access to quality health care, including STD prevention and treatment, that meets the needs of lower SES populations is key to reducing STD disparities in the United States; however, access likely will be insufficient unless the structural inequities that drive these disparities are addressed.
Clinical consequences for women, infants, and mothers
STDs are most prevalent among reproductive-aged women and can lead to pelvic inflammatory disease, infertility, ectopic pregnancy,4,8 and increased risk of acquiring human immunodeficiency virus (HIV). STDs during pregnancy present additional consequences. Congenital syphilis is perhaps the most salient, with neonates experiencing substantial disability or death.
In addition, STDs contribute to overall peripartum and long-term adverse health outcomes.4,9,10 Untreated chlamydia infection, for example, is associated with neonatal pneumonia, neonatal conjunctivitis, low birth weight, premature rupture of membranes, preterm labor, and postpartum endometritis.2,11 Untreated gonorrhea is linked to disseminated gonococcal infection in the newborn, neonatal conjunctivitis, low birth weight, miscarriage, premature rupture of membranes, preterm labor, and chorioamnionitis.2,12
As preterm birth is the leading cause of infant morbidity and mortality and disproportionately affects African American women and women in the southeastern United States,13 there is a critical public heath need to improve STD screening, treatment, and prevention of reinfection among high-risk pregnant women.
Quality clinical services for STDs: Areas for focus
More and more, STDs are being diagnosed in primary care settings. In January 2020, the Centers for Disease Control and Prevention (CDC) released a document, referred to as STD QCS (quality clinical services), that outlines recommendations for basic and specialty-level STD clinical services.14 ObGyns and other clinicians who provide primary care should meet the basic recommendations as a minimum.
The STD QCS outlines 8 recommendation areas: sexual history and physical examination, prevention, screening,
Continue to: Sexual history and physical examination...
Sexual history and physical examination
A complete sexual history and risk assessment should be performed at a complete initial or annual visit and as indicated. Routinely updating the sexual history and risk assessment is important to normalize these questions within the frame of the person’s overall health, and it may be valuable in reducing stigma. This routine approach may be important particularly for younger patients and others whose risk for STDs may change frequently and dramatically.
Creating a safe space that permits privacy and assurance of confidentiality may help build trust and set the stage for disclosure. The American College of Obstetricians and Gynecologists recommends that all young people have time alone without parents for confidential counseling and discussion.15 All states allow minors to consent for STD services themselves, although 11 states limit this to those beyond a certain age.16
The CDC recommends using the 5 P’s—partners, practices, protection, past history of STDs, and prevention of pregnancy—as a guide for discussion.14 ObGyns are more likely than other providers to perform this screening routinely. While a pelvic examination should be available for STD evaluation as needed, it is not required for routine screening.
Prevention
ObGyns should employ several recommendations for STD prevention. These include providing or referring patients for vaccination against hepatitis B and human papillomavirus and providing brief STD/HIV prevention counseling along with contraceptive counseling. ObGyns should be familiar with HIV pre-exposure prophylaxis (PrEP) and nonoccupational postexposure prophylaxis (nPEP) and provide risk assessment, education, and referral or link to HIV care. Providing these services would improve access to care and further remove barriers to care. ObGyns also could consider providing condoms in their offices.14
Screening
STD screening of women at risk is critical since more than 80% of infected women are asymptomatic.8 Because young people are disproportionately experiencing STDs, annual screening for chlamydia and gonorrhea is recommended for women younger than 25 years. For women older than 25, those at increased risk can be screened.
Risk factors for chlamydia infection include having new or multiple sex partners, sex partners with concurrent partners, or sex partners who have an STD. For gonorrhea, risk factors include living in a high-morbidity area, having a previous or coexisting STD, new or multiple sex partners, inconsistent condom use in people who are not in a mutually monogamous relationship, and exchanging sex for money or drugs. Screening for syphilis in nonpregnant women is recommended for those who have had any sexual activity with a person recently diagnosed with syphilis or those who personally display signs or symptoms of infection.17
STD screening is especially important for pregnant women, and treatment of infections may improve pregnancy outcomes. The CDC recommends screening at the first prenatal care visit for chlamydia and gonorrhea in pregnant women younger than 25 years of age and in older pregnant women at increased risk; women younger than 25 years or at continued high risk should be rescreened in their third trimester. The CDC recommends screening all women for syphilis at their first prenatal care visit and rescreening those at high risk in the third trimester and at delivery (TABLE).18
Continue to: Partner services...
Partner services
Clearly outlined partner management services is paramount for preventing STD reinfection.14 Reinfection rates for chlamydia and gonorrhea among young women are high and vary by study population.19 At a minimum, ObGyns should counsel patients with an STD that their partner(s) should be notified and encouraged to seek services.
For states in which it is legal, expedited partner therapy (EPT)—the clinician provides medication for the partner without seeing the partner—should be provided for chlamydia or gonorrhea if the partner is unlikely to access timely care. EPT is legal in most states. (To check the legal status of EPT in your state, visit https://www.cdc.gov/std/ept/legal/default.htm.) Research is needed to evaluate optimal strategies for effective implementation of EPT services in different clinical settings.
Laboratory tests
ObGyns should be able to provide a wide range of laboratory evaluations (for example, a nucleic acid amplification test [NAAT] for genital chlamydia and gonorrhea, quantitative nontreponemal serologic test for syphilis, treponemal serologic test for syphilis) that can be ordered for screening or diagnostic purposes. To improve rates of recommended screening, consider having clinic-level policies that support screening, such as standing orders, express or walk-in screening appointments, lab panels, and reflex testing.
Further, having rapid results or point-of-care testing available would help decrease lags in time to treatment. Delays in treatment are particularly important in lower-resource communities; thus, point-of-care testing may be especially valuable with immediate access to treatment on site.
Treatment
Adequate and timely treatment of STDs is critical to decrease sequelae and the likelihood of transmission to others. Treatment is evolving, particularly for gonorrhea. Over the past several years, gonorrhea has become resistant to 6 previously recommended treatment options.20 Since 2015, the CDC recommends dual therapy for gonorrhea with an injection of ceftriaxone and oral azithromycin.
The first-line recommended treatments for bacterial STDs are listed in the TABLE. When possible, it is preferred to offer directly observed therapy at the time of the visit. This decreases the time to treatment and ensures that therapy is completed.
A call to action for ObGyns
Clinicians have multiple opportunities to address and reduce the surge of STDs in the United States. We play a critical role in screening, diagnosing, and treating patients, and it is thus imperative to be up-to-date on the recommended guidelines. Further, clinicians can advocate for more rapid testing modalities, with the goal of obtaining point-of-care testing results when possible and implementing strategies to improve partner treatment.
While a positive STD result may be associated with significant patient distress, it also may be an opportunity for enhancing the patient-provider relationship, coupling education with motivational approaches to help patients increase protective health behaviors.
It is critical to approach clinical care in a nonjudgmental manner to improve patients’ comfort in their relationship with the health care system. ●
- Be aware of up-to-date screening, treatment, and follow-up recommendations for STDs
- Develop strategies to maximize partner treatment, including expedited partner therapy
- Identify high-risk individuals for whom counseling on HIV and unintended pregnancy prevention strategies can be reinforced, including PrEP and contraception
- Create a clinical environment that normalizes STD testing and destigmatizes infection
- Integrate client-centered counseling to improve protective health behaviors
Abbreviations: HIV, human immunodeficiency virus; PrEP, pre-exposure prophylaxis; STD, sexually transmitted disease.
- Centers for Disease Control and Prevention. 2018 STD surveillance report. https://www.cdc.gov/nchhstp /newsroom/2019/2018-STD-surveillance-report.html. Accessed March 19, 2020.
- Centers for Disease Control and Prevention. Sexually transmitted diseases (STDs): STDs during pregnancy—CDC fact sheet (detailed). www.cdc.gov/std/pregnancy/stdfact -sheet-pregnancy-detailed.htm. Accessed March 19, 2020.
- Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2017: STDs in racial and ethnic minorities 2017. https://www.cdc.gov/std/stats17 /minorities.htm. Accessed March 19, 2020.
- Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2017: STDs in women and infants. https://www.cdc.gov/std/stats17/womenandinf .htm. Accessed March 19, 2020.
- Semega JL, Fontenot KR, Kollar MA; US Census Bureau. Income and poverty in the United States: 2016. Washington, DC: US Government Printing Office; 2017. https://www.census.gov/content/dam/Census/library /publications/2017/demo/P60-259.pdf. Accessed March 19, 2020.
- Harling G, Subramanian S, Barnighausen T, et al. Socioeconomic disparities in sexually transmitted infections among young adults in the United States: examining the interaction between income and race/ethnicity. Sex Transm Dis. 2013;40:575-581.
- Meyer PA, Penman-Aguilar A, Campbell VA, et al; Centers for Disease Control and Prevention. Conclusion and future directions: CDC Health Disparities and Inequalities Report— United States, 2013. MMWR Suppl. 2013;62(3):184-186.
- Workowski KA, Bolan GA; Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64(RR-03): 1-137.
- Elliott B, Brunham RC, Laga M, et al. Maternal gonococcal infection as a preventable risk factor for low birth weight. J Infect Dis. 1990;161:531-536.
- Warr AJ, Pintye J, Kinuthia J, et al. Sexually transmitted infections during pregnancy and subsequent risk of stillbirth and infant mortality in Kenya: a prospective study. Sex Transm Infect. 2019;95:60-66.
- Andrews WW, Goldenberg RL, Mercer B, et al. The Preterm Prediction Study: association of second-trimester genitourinary chlamydia infection with subsequent spontaneous preterm birth. Am J Obstet Gynecol. 2000;183:662-668.
- Alger LS, Lovchik JC, Hebel JR, et al. The association of Chlamydia trachomatis, Neisseria gonorrhoeae, and group B streptococci with preterm rupture of the membranes and pregnancy outcome. Am J Obstet Gynecol. 1988;159:397-404.
- March of Dimes. Maternal, infant, and child health in the United States, 2016. https://www.marchofdimes.org /materials/March-of-Dimes-2016-Databook.pdf. Accessed March 19, 2020.
- Barrow RY, Ahmed F, Bolan GA, et al. Recommendations for providing quality sexually transmitted diseases clinical services, 2020. MMWR Recomm Rep. 2020;68(5):1-20.
- American College of Obstetricians and Gynecologists. ACOG committee opinion No. 598: The initial reproductive health visit. May 2014. https:// www.acog.org/-/media /project/acog/acogorg/clinical/files/committee-opinion /articles/2014/05/the-initial-reproductive-health-visit.pdf. Accessed March 31, 2020.
- Guttmacher Institute. An overview of consent to reproductive health services by young people. March 1, 2020. https://www .guttmacher.org/state-policy/explore/overview-minors -consent-law. Accessed March 19, 2020.
- Centers for Disease Control and Prevention. Pocket guide for providers: Syphilis: a provider’s guide to treatment and prevention. 2017. https://www.cdc.gov/std/syphilis /Syphilis-Pocket-Guide-FINAL-508.pdf. Accessed March 19, 2020.
- Centers for Disease Control and Prevention. 2015 Sexually transmitted diseases treatment guidelines: syphilis during pregnancy. https://www.cdc.gov/std/tg2015/syphilis -pregnancy.htm. Accessed March 19, 2020.
- Hosenfeld CB, Workowski KA, Berman S, et al. Repeat infection with chlamydia and gonorrhea among females: a systematic review of the literature. Sex Transm Dis. 2009;36:478-489.
- Bodie M, Gale-Rowe M, Alexandre S, et al. Addressing the rising rates of gonorrhea and drug-resistant gonorrhea: there is no time like the present. Can Commun Dis Rep. 2019;45:54-62.
- Centers for Disease Control and Prevention. 2018 STD surveillance report. https://www.cdc.gov/nchhstp /newsroom/2019/2018-STD-surveillance-report.html. Accessed March 19, 2020.
- Centers for Disease Control and Prevention. Sexually transmitted diseases (STDs): STDs during pregnancy—CDC fact sheet (detailed). www.cdc.gov/std/pregnancy/stdfact -sheet-pregnancy-detailed.htm. Accessed March 19, 2020.
- Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2017: STDs in racial and ethnic minorities 2017. https://www.cdc.gov/std/stats17 /minorities.htm. Accessed March 19, 2020.
- Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2017: STDs in women and infants. https://www.cdc.gov/std/stats17/womenandinf .htm. Accessed March 19, 2020.
- Semega JL, Fontenot KR, Kollar MA; US Census Bureau. Income and poverty in the United States: 2016. Washington, DC: US Government Printing Office; 2017. https://www.census.gov/content/dam/Census/library /publications/2017/demo/P60-259.pdf. Accessed March 19, 2020.
- Harling G, Subramanian S, Barnighausen T, et al. Socioeconomic disparities in sexually transmitted infections among young adults in the United States: examining the interaction between income and race/ethnicity. Sex Transm Dis. 2013;40:575-581.
- Meyer PA, Penman-Aguilar A, Campbell VA, et al; Centers for Disease Control and Prevention. Conclusion and future directions: CDC Health Disparities and Inequalities Report— United States, 2013. MMWR Suppl. 2013;62(3):184-186.
- Workowski KA, Bolan GA; Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64(RR-03): 1-137.
- Elliott B, Brunham RC, Laga M, et al. Maternal gonococcal infection as a preventable risk factor for low birth weight. J Infect Dis. 1990;161:531-536.
- Warr AJ, Pintye J, Kinuthia J, et al. Sexually transmitted infections during pregnancy and subsequent risk of stillbirth and infant mortality in Kenya: a prospective study. Sex Transm Infect. 2019;95:60-66.
- Andrews WW, Goldenberg RL, Mercer B, et al. The Preterm Prediction Study: association of second-trimester genitourinary chlamydia infection with subsequent spontaneous preterm birth. Am J Obstet Gynecol. 2000;183:662-668.
- Alger LS, Lovchik JC, Hebel JR, et al. The association of Chlamydia trachomatis, Neisseria gonorrhoeae, and group B streptococci with preterm rupture of the membranes and pregnancy outcome. Am J Obstet Gynecol. 1988;159:397-404.
- March of Dimes. Maternal, infant, and child health in the United States, 2016. https://www.marchofdimes.org /materials/March-of-Dimes-2016-Databook.pdf. Accessed March 19, 2020.
- Barrow RY, Ahmed F, Bolan GA, et al. Recommendations for providing quality sexually transmitted diseases clinical services, 2020. MMWR Recomm Rep. 2020;68(5):1-20.
- American College of Obstetricians and Gynecologists. ACOG committee opinion No. 598: The initial reproductive health visit. May 2014. https:// www.acog.org/-/media /project/acog/acogorg/clinical/files/committee-opinion /articles/2014/05/the-initial-reproductive-health-visit.pdf. Accessed March 31, 2020.
- Guttmacher Institute. An overview of consent to reproductive health services by young people. March 1, 2020. https://www .guttmacher.org/state-policy/explore/overview-minors -consent-law. Accessed March 19, 2020.
- Centers for Disease Control and Prevention. Pocket guide for providers: Syphilis: a provider’s guide to treatment and prevention. 2017. https://www.cdc.gov/std/syphilis /Syphilis-Pocket-Guide-FINAL-508.pdf. Accessed March 19, 2020.
- Centers for Disease Control and Prevention. 2015 Sexually transmitted diseases treatment guidelines: syphilis during pregnancy. https://www.cdc.gov/std/tg2015/syphilis -pregnancy.htm. Accessed March 19, 2020.
- Hosenfeld CB, Workowski KA, Berman S, et al. Repeat infection with chlamydia and gonorrhea among females: a systematic review of the literature. Sex Transm Dis. 2009;36:478-489.
- Bodie M, Gale-Rowe M, Alexandre S, et al. Addressing the rising rates of gonorrhea and drug-resistant gonorrhea: there is no time like the present. Can Commun Dis Rep. 2019;45:54-62.


