User login
CASE: In-office hysteroscopy spies previously missed polyp
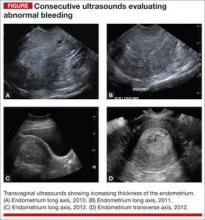
A 51-year-old woman with a history of breast cancer completed 5 years of tamoxifen. During her treatment she had a 3-year history of abnormal vaginal bleeding. Results from consecutive pelvic ultrasounds indicated that the patient had progressively thickening endometrium (from 1.4 cm to 2.5 cm to 4.7 cm). In-office biopsy was negative for endometrial pathology. An ultimate dilation and curettage (D&C) was performed with negative histologic diagnosis. The patient is seen in consultation, and the ultrasound images are reviewed (FIGURE).
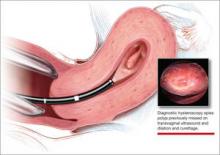
These images show an increasing thickness of the ednometrium with definitive intracavitary pathology that was missed with the prevous clinical evaluation with enodmetrial biopsy and D&C. An in-office hysteroscopy is performed, and a large 5 x 4 x 7 cm cystic and fibrous polyp is identified with normal endometrium (VIDEO 1).
Hysteroscopy reveals massive polyp extending into a dilated lower uterine segment
Abnormal uterine bleeding
The evaluation of abnormal uterine bleeding. (AUB), as described in this clinical scenario, is quite common. As a consequence, many patients have a missed or inaccurate diagnosis and undergo unnecessary invasive procedures under general anesthesia.
AUB is one of the primary indications for a gynecologic consultation, accounting for approximately 33% of all gynecology visits, and for 69% of visits among postmenopausal women.1 Confirming the etiology and planning appropriate intervention is important in the clinical management of AUB because accurate diagnosis may result in avoiding major gynecologic surgery in favor of minimally invasive hysteroscopic management.
Diagnostic hysteroscopy is proven in AUB evaluation
Drawbacks of other diagnostic tools. It is generally accepted that the initial evaluation of women with AUB is performed with noninvasive transvaginal ultrasound (TVUS).1-3 As illustrated by the opening case, however, the accuracy of TVUS is limited in the diagnosis of focal endometrial lesions, and further investigation of the uterine cavity is warranted.
Evaluation of the uterine cavity with sonohysterography (SH)—vaginal ultrasound with the instillation of saline into the uterine cavity—is more accurate than TVUS alone. Yet, diagnostic hysteroscopy (DH) has proven to be superior to either modality for the accurate evaluation of intracavitary pathology.1-3
Evidence of DH superiority. Farquhar and colleagues reported results of a systematic review of studies published from 1980 to July 2001 that examined TVUS versus SH and DH for the investigation of AUB in premenopausal women. The researchers found that TVUS had a higher rate of false negatives for detecting intrauterine pathology, compared with SH and DH. They also found that DH was superior to SH in diagnosing submucous myomas.2
In 2010, results of a prospective comparison of TVUS, SH, and DH for detecting endometrial pathology, showed that DH had a significantly better diagnostic performance than SH and TVUS and that hysteroscopy was significantly more precise in the diagnosis of intracavitary masses.3
Again, in 2012, a prospective comparison of TVUS, SH, and DH in the diagnosis of AUB revealed that hysteroscopy provided the most accurate diagnosis.1
In a systematic review and meta-analysis, van Dongen found the accuracy of DH to be estimated at 96.9%.4
Hysteroscopy is also considered to be more comfortable for patients than SH.2
blinded sampling missed intracavitary lesions such as polyps and myomas that accounted for bleeding abnormalities.5
A procedure performed “blind” limits its usefulness in AUB evaluation
This statement is not a new realization. As far back as 1989, Loffer showed that blind D&C was less accurate for diagnosing AUB than was hysteroscopy with visually directed biopsy. The sensitivity of diagnosing the etiology of AUB with D&C was 65%, compared to a sensitivity of 98% with hysteroscopy with directed biopsy. Hysteroscopy was shown to be better because blinded sampling missed intracavitary lesions such as polyps and myomas that accounted for bleeding abnormalities.5
The limitations of D&C are evident in the opening case, as the D&C performed in the operating room under general anesthesia, without visualization of the uterine cavity, failed to identify the patient’s intrauterine pathology. D&C is seldom necessary to evaluate AUB and has significant surgical risks beyond general anesthesia, including cervical or uterine trauma that can occur with cervical dilation and instrumentation of the uterus.
As with D&C, endometrial biopsy has limitations in diagnosing abnormalities within the uterine cavity. In a 2008 prospective comparative study of hysteroscopy versus blind biopsy with a suction biopsy curette, Angioni and colleagues showed a significant difference in the capability of these two procedures to accurately diagnose the etiology of bleeding for menopausal women. Blinded biopsy had a sensitivity for diagnosing polyps, myomas, and hyperplasia of 11%, 13%, and 25%, respectively. The sensitivity of hysteroscopy to diagnose the same intracavitary pathology was 89%, 100%, and 74%, respectively.6
This does not mean, however, that the endometrial biopsy is not beneficial in the evaluation of AUB. Several authors recommend that in a clinically relevant situation, endometrial biopsy with a small suction curette should be performed concomitantly with hysteroscopy to improve the sensitivity of the overall evaluation with histology.7,8 And, as Loffer showed, the hysteroscopic evaluation with a visually directed biopsy is extremely accurate (VIDEO 2, VIDEO 3).5
The bottom line for D&C use in AUB evaluation
Sometimes a D&C is needed. For instance, when more tissue is needed for histologic evaluation than can be obtained with small suction curette at endometrial biopsy. However, there are several shortcomings of D&C for the evaluation of AUB:
- Most clinicians perform D&C in the operating room under general anesthesia.
- It is often done without concomitant hysteroscopy.
- There is significant potential to miss pathology, such as polyps or myomas.
- There is risk of uterine perforation with cervical dilation and uterine instrumentation.
- Hysteroscopy with visually directed biopsy provides a method that offers a more accurate diagnosis, and the procedure can be performed in the office.
In-office AUB evaluation using hysteroscopy is possible and advantageous
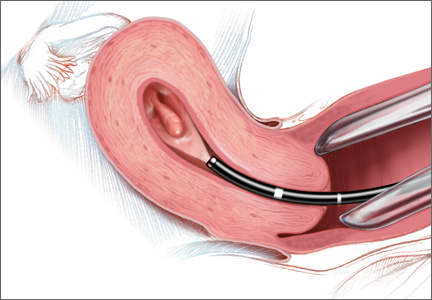
Hysteroscopy not only has increased accuracy for identifying the etiology of AUB, compared with D&C, but also offers the possibility of in-office use. Newer hysteroscopes with small diameters and decreasing costs of hysteroscopic equipment allow gynecologists to perform hysteroscopy economically and safely in the office.
Office evaluation of the uterine cavity and preoperative decision-making before a patient is taken to the operating room (OR) improve the likelihood that the appropriate procedure will be performed. They also provide an opportunity for the patient to see inside her own uterine cavity and for the surgeon to discuss management options with her (VIDEO 4: Diagnostic hysteroscopy with fundal myoma, VIDEO 5: Diagnostic hysteroscopy in a menopausal patient with atypical hyperplasia, VIDEO 6: Diagnostic hysteroscopy in a menopausal patient with polyps). If pathology is noted, there is a potential to treat abnormalities such as endometrial polyps at the same time, thus avoiding the OR altogether (VIDEO 7).
The small diameter of the hysteroscope allows evaluation in most menopausal and nulliparous patients comfortably without first having to dilate or soften the cervix. Paracervical placement of local anesthetic can be used as needed for patient comfort (VIDEO 8).9 A vaginoscopic approach will eliminate the discomfort of having to place a speculum (VIDEO 9).
It offers:
- a familiar and comfortable environment for the procedure
- saved time for patient and physician
- saved money for the patient with a large deductible or coinsurance
- no requirement for general anesthesia
- local anesthesia can be used but is not necessary
- immediate visual affirmation for the patient and physician
- a see and treat possibility
- possibility of preoperative decision-making
- saved trip to the OR if significant precancer or cancer is identified
- use in menopausal and nulliparous patients with no cervical preparation necessary when a small-diameter hysteroscope or flexible hysteroscope is used
- minimized discomfort from a speculum with the vaginoscopic approach for awake patients
- possibility of cervical access when needed (VIDEO 10).
My clinical recommendation
Use office hysteroscopy with endometrial biopsy as needed with the opportunity to perform a directed biopsy.
Coding for in-office hysteroscopy
Some procedures now can be performed in the office setting. Among these is operative hysteroscopy, for things such as abnormal uterine bleeding (AUB), foreign body removal, and tubal occlusion. When performing hysteroscopic evaluation of AUB, the Current Procedural Terminology (CPT) code 58558 (Hysteroscopy, surgical; with sampling (biopsy) of endometrium and/or polypectomy, with or without D&C) should be reported. This code is reported whether polyp(s) are removed or a sampling of the uterine lining or a full D&C is performed.
Under the Resource-Based Relative Value System (RBRVS), used by the majority of payers for reimbursement, there is a payment differential for site of service. In other words, when performed in the office setting, reimbursement will be higher than in the hospital setting to offset the increased practice expenses incurred. In the office setting, 58558 has 11.93 relative value units. In comparison, a D&C performed without hysteroscopy has 7.75 relative value units in the office setting. Keep in mind, however, that all supplies used in performing this procedure are included in the reimbursement amount.
Some payers will reimburse separately for administering a regional anesthetic, but a local anesthetic is considered integral to the procedure. Under CPT rules, you may bill separately for regional anesthesia. When performing office hysteroscopy, the most common regional anesthesia would be a paracervical nerve block (CPT code 66435—Injection, anesthetic agent; paracervical [uterine] nerve). Under CPT rules, coding should go in as 58558-47, 64435-51. The modifier -47 lets the payer know that the physician performed the regional block, and the modifier -51 identifies the regional block as a multiple procedure.
Medicare, however, will never reimburse separately for regional anesthesia performed by the operating physician, and because of this, Medicare’s Correct Coding Initiative (CCI) permanently bundles 64435 when billed with 58558. Medicare will not permit a modifier to be used to bypass this bundling edit, and separate payment is never allowed. If your payer has adopted this Medicare policy, separate payment will also not be made.
—Melanie Witt, RN, CPC, COBGC, MA
Ms. Witt is an independent coding and documentation consultant and former program manager, department of coding and nomenclature, American Congress of Obstetricians and Gynecologists
- Soguktas S, Cogendez E, Kayatas SE, Asoglu MR, Selcuk S, Ertekin A. Comparison of saline infusion sonohysterography and hysteroscopy in diagnosis of premenopausal women with abnormal uterine bleeding. Eur J Obstet Gynecol Repro Biol. 2012;161(1):66−70.
- Farquhar C, Ekeroma A, Furness S, Arroll B. A systematic review of transvaginal ultrasonography, sonohysterography and hysteroscopy for the investigation of abnormal uterine bleeding in premenopausal bleeding. Acta Obstet Gynecol Scand. 2003;82(6):493–504.
- Grimbizis GF, Tsolakidis D, Mikos T, et al. A prospective comparison of transvaginal ultrasound, saline infusion sonohysterography, and diagnostic hysteroscopy in the evaluation of endometrial pathology. Fertil Steril. 2010;94(7):2721−2725.
- van Dongen H, de Kroon CD, Jacobi CE, Trimbos JB, Jansen FW. Diagnostic hysteroscopy in abnormal uterine bleeding: a systematic review and meta-analysis. BJOG. 2007;114(6):664–75.
- Loffer FD. Hysteroscopy with selective endometrial sampling compared with D & C for abnormal uterine bleeding: the value of a negative hysteroscopic view. Obstet Gynecol. 1989;73(1):16–20.
- Angioni S, Loddo A, Milano F, Piras B, Minerba L, Melis GB. Detection of benign intracavitary lesions in postmenopausal women with abnormal uterine bleeding: a prospective comparative study on outpatient hysteroscopy and blind biopsy. J Minim Invasive Gynecol. 2008;15(1):87–91.
- Lo KY, Yuen PM. The role of outpatient diagnostic hysteroscopy in identifying anatomic pathology and histopathology in the endometrial cavity. J Am Assoc Gynecol Laparosc. 2000;7(3):381–385.
- Garuti G, Sambruni I, Colonneli M, Luerti M. Accuracy of hysteroscopy in predicting histopathology of endometrium in 1500 women. J Am Assoc Gynecol Laparosc. 2001;8(2):207–213.
- Munro MG, Brooks PG. Use of local anesthesia for office diagnostic and operative hysteroscopy. J Minim Invasive Gynecol. 2010;17(6):709–718.
CASE: In-office hysteroscopy spies previously missed polyp
A 51-year-old woman with a history of breast cancer completed 5 years of tamoxifen. During her treatment she had a 3-year history of abnormal vaginal bleeding. Results from consecutive pelvic ultrasounds indicated that the patient had progressively thickening endometrium (from 1.4 cm to 2.5 cm to 4.7 cm). In-office biopsy was negative for endometrial pathology. An ultimate dilation and curettage (D&C) was performed with negative histologic diagnosis. The patient is seen in consultation, and the ultrasound images are reviewed (FIGURE).
These images show an increasing thickness of the ednometrium with definitive intracavitary pathology that was missed with the prevous clinical evaluation with enodmetrial biopsy and D&C. An in-office hysteroscopy is performed, and a large 5 x 4 x 7 cm cystic and fibrous polyp is identified with normal endometrium (VIDEO 1).
Hysteroscopy reveals massive polyp extending into a dilated lower uterine segment
Abnormal uterine bleeding
The evaluation of abnormal uterine bleeding. (AUB), as described in this clinical scenario, is quite common. As a consequence, many patients have a missed or inaccurate diagnosis and undergo unnecessary invasive procedures under general anesthesia.
AUB is one of the primary indications for a gynecologic consultation, accounting for approximately 33% of all gynecology visits, and for 69% of visits among postmenopausal women.1 Confirming the etiology and planning appropriate intervention is important in the clinical management of AUB because accurate diagnosis may result in avoiding major gynecologic surgery in favor of minimally invasive hysteroscopic management.
Diagnostic hysteroscopy is proven in AUB evaluation
Drawbacks of other diagnostic tools. It is generally accepted that the initial evaluation of women with AUB is performed with noninvasive transvaginal ultrasound (TVUS).1-3 As illustrated by the opening case, however, the accuracy of TVUS is limited in the diagnosis of focal endometrial lesions, and further investigation of the uterine cavity is warranted.
Evaluation of the uterine cavity with sonohysterography (SH)—vaginal ultrasound with the instillation of saline into the uterine cavity—is more accurate than TVUS alone. Yet, diagnostic hysteroscopy (DH) has proven to be superior to either modality for the accurate evaluation of intracavitary pathology.1-3
Evidence of DH superiority. Farquhar and colleagues reported results of a systematic review of studies published from 1980 to July 2001 that examined TVUS versus SH and DH for the investigation of AUB in premenopausal women. The researchers found that TVUS had a higher rate of false negatives for detecting intrauterine pathology, compared with SH and DH. They also found that DH was superior to SH in diagnosing submucous myomas.2
In 2010, results of a prospective comparison of TVUS, SH, and DH for detecting endometrial pathology, showed that DH had a significantly better diagnostic performance than SH and TVUS and that hysteroscopy was significantly more precise in the diagnosis of intracavitary masses.3
Again, in 2012, a prospective comparison of TVUS, SH, and DH in the diagnosis of AUB revealed that hysteroscopy provided the most accurate diagnosis.1
In a systematic review and meta-analysis, van Dongen found the accuracy of DH to be estimated at 96.9%.4
Hysteroscopy is also considered to be more comfortable for patients than SH.2
blinded sampling missed intracavitary lesions such as polyps and myomas that accounted for bleeding abnormalities.5
A procedure performed “blind” limits its usefulness in AUB evaluation
This statement is not a new realization. As far back as 1989, Loffer showed that blind D&C was less accurate for diagnosing AUB than was hysteroscopy with visually directed biopsy. The sensitivity of diagnosing the etiology of AUB with D&C was 65%, compared to a sensitivity of 98% with hysteroscopy with directed biopsy. Hysteroscopy was shown to be better because blinded sampling missed intracavitary lesions such as polyps and myomas that accounted for bleeding abnormalities.5
The limitations of D&C are evident in the opening case, as the D&C performed in the operating room under general anesthesia, without visualization of the uterine cavity, failed to identify the patient’s intrauterine pathology. D&C is seldom necessary to evaluate AUB and has significant surgical risks beyond general anesthesia, including cervical or uterine trauma that can occur with cervical dilation and instrumentation of the uterus.
As with D&C, endometrial biopsy has limitations in diagnosing abnormalities within the uterine cavity. In a 2008 prospective comparative study of hysteroscopy versus blind biopsy with a suction biopsy curette, Angioni and colleagues showed a significant difference in the capability of these two procedures to accurately diagnose the etiology of bleeding for menopausal women. Blinded biopsy had a sensitivity for diagnosing polyps, myomas, and hyperplasia of 11%, 13%, and 25%, respectively. The sensitivity of hysteroscopy to diagnose the same intracavitary pathology was 89%, 100%, and 74%, respectively.6
This does not mean, however, that the endometrial biopsy is not beneficial in the evaluation of AUB. Several authors recommend that in a clinically relevant situation, endometrial biopsy with a small suction curette should be performed concomitantly with hysteroscopy to improve the sensitivity of the overall evaluation with histology.7,8 And, as Loffer showed, the hysteroscopic evaluation with a visually directed biopsy is extremely accurate (VIDEO 2, VIDEO 3).5
The bottom line for D&C use in AUB evaluation
Sometimes a D&C is needed. For instance, when more tissue is needed for histologic evaluation than can be obtained with small suction curette at endometrial biopsy. However, there are several shortcomings of D&C for the evaluation of AUB:
- Most clinicians perform D&C in the operating room under general anesthesia.
- It is often done without concomitant hysteroscopy.
- There is significant potential to miss pathology, such as polyps or myomas.
- There is risk of uterine perforation with cervical dilation and uterine instrumentation.
- Hysteroscopy with visually directed biopsy provides a method that offers a more accurate diagnosis, and the procedure can be performed in the office.
In-office AUB evaluation using hysteroscopy is possible and advantageous
Hysteroscopy not only has increased accuracy for identifying the etiology of AUB, compared with D&C, but also offers the possibility of in-office use. Newer hysteroscopes with small diameters and decreasing costs of hysteroscopic equipment allow gynecologists to perform hysteroscopy economically and safely in the office.
Office evaluation of the uterine cavity and preoperative decision-making before a patient is taken to the operating room (OR) improve the likelihood that the appropriate procedure will be performed. They also provide an opportunity for the patient to see inside her own uterine cavity and for the surgeon to discuss management options with her (VIDEO 4: Diagnostic hysteroscopy with fundal myoma, VIDEO 5: Diagnostic hysteroscopy in a menopausal patient with atypical hyperplasia, VIDEO 6: Diagnostic hysteroscopy in a menopausal patient with polyps). If pathology is noted, there is a potential to treat abnormalities such as endometrial polyps at the same time, thus avoiding the OR altogether (VIDEO 7).
The small diameter of the hysteroscope allows evaluation in most menopausal and nulliparous patients comfortably without first having to dilate or soften the cervix. Paracervical placement of local anesthetic can be used as needed for patient comfort (VIDEO 8).9 A vaginoscopic approach will eliminate the discomfort of having to place a speculum (VIDEO 9).
It offers:
- a familiar and comfortable environment for the procedure
- saved time for patient and physician
- saved money for the patient with a large deductible or coinsurance
- no requirement for general anesthesia
- local anesthesia can be used but is not necessary
- immediate visual affirmation for the patient and physician
- a see and treat possibility
- possibility of preoperative decision-making
- saved trip to the OR if significant precancer or cancer is identified
- use in menopausal and nulliparous patients with no cervical preparation necessary when a small-diameter hysteroscope or flexible hysteroscope is used
- minimized discomfort from a speculum with the vaginoscopic approach for awake patients
- possibility of cervical access when needed (VIDEO 10).
My clinical recommendation
Use office hysteroscopy with endometrial biopsy as needed with the opportunity to perform a directed biopsy.
Coding for in-office hysteroscopy
Some procedures now can be performed in the office setting. Among these is operative hysteroscopy, for things such as abnormal uterine bleeding (AUB), foreign body removal, and tubal occlusion. When performing hysteroscopic evaluation of AUB, the Current Procedural Terminology (CPT) code 58558 (Hysteroscopy, surgical; with sampling (biopsy) of endometrium and/or polypectomy, with or without D&C) should be reported. This code is reported whether polyp(s) are removed or a sampling of the uterine lining or a full D&C is performed.
Under the Resource-Based Relative Value System (RBRVS), used by the majority of payers for reimbursement, there is a payment differential for site of service. In other words, when performed in the office setting, reimbursement will be higher than in the hospital setting to offset the increased practice expenses incurred. In the office setting, 58558 has 11.93 relative value units. In comparison, a D&C performed without hysteroscopy has 7.75 relative value units in the office setting. Keep in mind, however, that all supplies used in performing this procedure are included in the reimbursement amount.
Some payers will reimburse separately for administering a regional anesthetic, but a local anesthetic is considered integral to the procedure. Under CPT rules, you may bill separately for regional anesthesia. When performing office hysteroscopy, the most common regional anesthesia would be a paracervical nerve block (CPT code 66435—Injection, anesthetic agent; paracervical [uterine] nerve). Under CPT rules, coding should go in as 58558-47, 64435-51. The modifier -47 lets the payer know that the physician performed the regional block, and the modifier -51 identifies the regional block as a multiple procedure.
Medicare, however, will never reimburse separately for regional anesthesia performed by the operating physician, and because of this, Medicare’s Correct Coding Initiative (CCI) permanently bundles 64435 when billed with 58558. Medicare will not permit a modifier to be used to bypass this bundling edit, and separate payment is never allowed. If your payer has adopted this Medicare policy, separate payment will also not be made.
—Melanie Witt, RN, CPC, COBGC, MA
Ms. Witt is an independent coding and documentation consultant and former program manager, department of coding and nomenclature, American Congress of Obstetricians and Gynecologists
CASE: In-office hysteroscopy spies previously missed polyp
A 51-year-old woman with a history of breast cancer completed 5 years of tamoxifen. During her treatment she had a 3-year history of abnormal vaginal bleeding. Results from consecutive pelvic ultrasounds indicated that the patient had progressively thickening endometrium (from 1.4 cm to 2.5 cm to 4.7 cm). In-office biopsy was negative for endometrial pathology. An ultimate dilation and curettage (D&C) was performed with negative histologic diagnosis. The patient is seen in consultation, and the ultrasound images are reviewed (FIGURE).
These images show an increasing thickness of the ednometrium with definitive intracavitary pathology that was missed with the prevous clinical evaluation with enodmetrial biopsy and D&C. An in-office hysteroscopy is performed, and a large 5 x 4 x 7 cm cystic and fibrous polyp is identified with normal endometrium (VIDEO 1).
Hysteroscopy reveals massive polyp extending into a dilated lower uterine segment
Abnormal uterine bleeding
The evaluation of abnormal uterine bleeding. (AUB), as described in this clinical scenario, is quite common. As a consequence, many patients have a missed or inaccurate diagnosis and undergo unnecessary invasive procedures under general anesthesia.
AUB is one of the primary indications for a gynecologic consultation, accounting for approximately 33% of all gynecology visits, and for 69% of visits among postmenopausal women.1 Confirming the etiology and planning appropriate intervention is important in the clinical management of AUB because accurate diagnosis may result in avoiding major gynecologic surgery in favor of minimally invasive hysteroscopic management.
Diagnostic hysteroscopy is proven in AUB evaluation
Drawbacks of other diagnostic tools. It is generally accepted that the initial evaluation of women with AUB is performed with noninvasive transvaginal ultrasound (TVUS).1-3 As illustrated by the opening case, however, the accuracy of TVUS is limited in the diagnosis of focal endometrial lesions, and further investigation of the uterine cavity is warranted.
Evaluation of the uterine cavity with sonohysterography (SH)—vaginal ultrasound with the instillation of saline into the uterine cavity—is more accurate than TVUS alone. Yet, diagnostic hysteroscopy (DH) has proven to be superior to either modality for the accurate evaluation of intracavitary pathology.1-3
Evidence of DH superiority. Farquhar and colleagues reported results of a systematic review of studies published from 1980 to July 2001 that examined TVUS versus SH and DH for the investigation of AUB in premenopausal women. The researchers found that TVUS had a higher rate of false negatives for detecting intrauterine pathology, compared with SH and DH. They also found that DH was superior to SH in diagnosing submucous myomas.2
In 2010, results of a prospective comparison of TVUS, SH, and DH for detecting endometrial pathology, showed that DH had a significantly better diagnostic performance than SH and TVUS and that hysteroscopy was significantly more precise in the diagnosis of intracavitary masses.3
Again, in 2012, a prospective comparison of TVUS, SH, and DH in the diagnosis of AUB revealed that hysteroscopy provided the most accurate diagnosis.1
In a systematic review and meta-analysis, van Dongen found the accuracy of DH to be estimated at 96.9%.4
Hysteroscopy is also considered to be more comfortable for patients than SH.2
blinded sampling missed intracavitary lesions such as polyps and myomas that accounted for bleeding abnormalities.5
A procedure performed “blind” limits its usefulness in AUB evaluation
This statement is not a new realization. As far back as 1989, Loffer showed that blind D&C was less accurate for diagnosing AUB than was hysteroscopy with visually directed biopsy. The sensitivity of diagnosing the etiology of AUB with D&C was 65%, compared to a sensitivity of 98% with hysteroscopy with directed biopsy. Hysteroscopy was shown to be better because blinded sampling missed intracavitary lesions such as polyps and myomas that accounted for bleeding abnormalities.5
The limitations of D&C are evident in the opening case, as the D&C performed in the operating room under general anesthesia, without visualization of the uterine cavity, failed to identify the patient’s intrauterine pathology. D&C is seldom necessary to evaluate AUB and has significant surgical risks beyond general anesthesia, including cervical or uterine trauma that can occur with cervical dilation and instrumentation of the uterus.
As with D&C, endometrial biopsy has limitations in diagnosing abnormalities within the uterine cavity. In a 2008 prospective comparative study of hysteroscopy versus blind biopsy with a suction biopsy curette, Angioni and colleagues showed a significant difference in the capability of these two procedures to accurately diagnose the etiology of bleeding for menopausal women. Blinded biopsy had a sensitivity for diagnosing polyps, myomas, and hyperplasia of 11%, 13%, and 25%, respectively. The sensitivity of hysteroscopy to diagnose the same intracavitary pathology was 89%, 100%, and 74%, respectively.6
This does not mean, however, that the endometrial biopsy is not beneficial in the evaluation of AUB. Several authors recommend that in a clinically relevant situation, endometrial biopsy with a small suction curette should be performed concomitantly with hysteroscopy to improve the sensitivity of the overall evaluation with histology.7,8 And, as Loffer showed, the hysteroscopic evaluation with a visually directed biopsy is extremely accurate (VIDEO 2, VIDEO 3).5
The bottom line for D&C use in AUB evaluation
Sometimes a D&C is needed. For instance, when more tissue is needed for histologic evaluation than can be obtained with small suction curette at endometrial biopsy. However, there are several shortcomings of D&C for the evaluation of AUB:
- Most clinicians perform D&C in the operating room under general anesthesia.
- It is often done without concomitant hysteroscopy.
- There is significant potential to miss pathology, such as polyps or myomas.
- There is risk of uterine perforation with cervical dilation and uterine instrumentation.
- Hysteroscopy with visually directed biopsy provides a method that offers a more accurate diagnosis, and the procedure can be performed in the office.
In-office AUB evaluation using hysteroscopy is possible and advantageous
Hysteroscopy not only has increased accuracy for identifying the etiology of AUB, compared with D&C, but also offers the possibility of in-office use. Newer hysteroscopes with small diameters and decreasing costs of hysteroscopic equipment allow gynecologists to perform hysteroscopy economically and safely in the office.
Office evaluation of the uterine cavity and preoperative decision-making before a patient is taken to the operating room (OR) improve the likelihood that the appropriate procedure will be performed. They also provide an opportunity for the patient to see inside her own uterine cavity and for the surgeon to discuss management options with her (VIDEO 4: Diagnostic hysteroscopy with fundal myoma, VIDEO 5: Diagnostic hysteroscopy in a menopausal patient with atypical hyperplasia, VIDEO 6: Diagnostic hysteroscopy in a menopausal patient with polyps). If pathology is noted, there is a potential to treat abnormalities such as endometrial polyps at the same time, thus avoiding the OR altogether (VIDEO 7).
The small diameter of the hysteroscope allows evaluation in most menopausal and nulliparous patients comfortably without first having to dilate or soften the cervix. Paracervical placement of local anesthetic can be used as needed for patient comfort (VIDEO 8).9 A vaginoscopic approach will eliminate the discomfort of having to place a speculum (VIDEO 9).
It offers:
- a familiar and comfortable environment for the procedure
- saved time for patient and physician
- saved money for the patient with a large deductible or coinsurance
- no requirement for general anesthesia
- local anesthesia can be used but is not necessary
- immediate visual affirmation for the patient and physician
- a see and treat possibility
- possibility of preoperative decision-making
- saved trip to the OR if significant precancer or cancer is identified
- use in menopausal and nulliparous patients with no cervical preparation necessary when a small-diameter hysteroscope or flexible hysteroscope is used
- minimized discomfort from a speculum with the vaginoscopic approach for awake patients
- possibility of cervical access when needed (VIDEO 10).
My clinical recommendation
Use office hysteroscopy with endometrial biopsy as needed with the opportunity to perform a directed biopsy.
Coding for in-office hysteroscopy
Some procedures now can be performed in the office setting. Among these is operative hysteroscopy, for things such as abnormal uterine bleeding (AUB), foreign body removal, and tubal occlusion. When performing hysteroscopic evaluation of AUB, the Current Procedural Terminology (CPT) code 58558 (Hysteroscopy, surgical; with sampling (biopsy) of endometrium and/or polypectomy, with or without D&C) should be reported. This code is reported whether polyp(s) are removed or a sampling of the uterine lining or a full D&C is performed.
Under the Resource-Based Relative Value System (RBRVS), used by the majority of payers for reimbursement, there is a payment differential for site of service. In other words, when performed in the office setting, reimbursement will be higher than in the hospital setting to offset the increased practice expenses incurred. In the office setting, 58558 has 11.93 relative value units. In comparison, a D&C performed without hysteroscopy has 7.75 relative value units in the office setting. Keep in mind, however, that all supplies used in performing this procedure are included in the reimbursement amount.
Some payers will reimburse separately for administering a regional anesthetic, but a local anesthetic is considered integral to the procedure. Under CPT rules, you may bill separately for regional anesthesia. When performing office hysteroscopy, the most common regional anesthesia would be a paracervical nerve block (CPT code 66435—Injection, anesthetic agent; paracervical [uterine] nerve). Under CPT rules, coding should go in as 58558-47, 64435-51. The modifier -47 lets the payer know that the physician performed the regional block, and the modifier -51 identifies the regional block as a multiple procedure.
Medicare, however, will never reimburse separately for regional anesthesia performed by the operating physician, and because of this, Medicare’s Correct Coding Initiative (CCI) permanently bundles 64435 when billed with 58558. Medicare will not permit a modifier to be used to bypass this bundling edit, and separate payment is never allowed. If your payer has adopted this Medicare policy, separate payment will also not be made.
—Melanie Witt, RN, CPC, COBGC, MA
Ms. Witt is an independent coding and documentation consultant and former program manager, department of coding and nomenclature, American Congress of Obstetricians and Gynecologists
- Soguktas S, Cogendez E, Kayatas SE, Asoglu MR, Selcuk S, Ertekin A. Comparison of saline infusion sonohysterography and hysteroscopy in diagnosis of premenopausal women with abnormal uterine bleeding. Eur J Obstet Gynecol Repro Biol. 2012;161(1):66−70.
- Farquhar C, Ekeroma A, Furness S, Arroll B. A systematic review of transvaginal ultrasonography, sonohysterography and hysteroscopy for the investigation of abnormal uterine bleeding in premenopausal bleeding. Acta Obstet Gynecol Scand. 2003;82(6):493–504.
- Grimbizis GF, Tsolakidis D, Mikos T, et al. A prospective comparison of transvaginal ultrasound, saline infusion sonohysterography, and diagnostic hysteroscopy in the evaluation of endometrial pathology. Fertil Steril. 2010;94(7):2721−2725.
- van Dongen H, de Kroon CD, Jacobi CE, Trimbos JB, Jansen FW. Diagnostic hysteroscopy in abnormal uterine bleeding: a systematic review and meta-analysis. BJOG. 2007;114(6):664–75.
- Loffer FD. Hysteroscopy with selective endometrial sampling compared with D & C for abnormal uterine bleeding: the value of a negative hysteroscopic view. Obstet Gynecol. 1989;73(1):16–20.
- Angioni S, Loddo A, Milano F, Piras B, Minerba L, Melis GB. Detection of benign intracavitary lesions in postmenopausal women with abnormal uterine bleeding: a prospective comparative study on outpatient hysteroscopy and blind biopsy. J Minim Invasive Gynecol. 2008;15(1):87–91.
- Lo KY, Yuen PM. The role of outpatient diagnostic hysteroscopy in identifying anatomic pathology and histopathology in the endometrial cavity. J Am Assoc Gynecol Laparosc. 2000;7(3):381–385.
- Garuti G, Sambruni I, Colonneli M, Luerti M. Accuracy of hysteroscopy in predicting histopathology of endometrium in 1500 women. J Am Assoc Gynecol Laparosc. 2001;8(2):207–213.
- Munro MG, Brooks PG. Use of local anesthesia for office diagnostic and operative hysteroscopy. J Minim Invasive Gynecol. 2010;17(6):709–718.
- Soguktas S, Cogendez E, Kayatas SE, Asoglu MR, Selcuk S, Ertekin A. Comparison of saline infusion sonohysterography and hysteroscopy in diagnosis of premenopausal women with abnormal uterine bleeding. Eur J Obstet Gynecol Repro Biol. 2012;161(1):66−70.
- Farquhar C, Ekeroma A, Furness S, Arroll B. A systematic review of transvaginal ultrasonography, sonohysterography and hysteroscopy for the investigation of abnormal uterine bleeding in premenopausal bleeding. Acta Obstet Gynecol Scand. 2003;82(6):493–504.
- Grimbizis GF, Tsolakidis D, Mikos T, et al. A prospective comparison of transvaginal ultrasound, saline infusion sonohysterography, and diagnostic hysteroscopy in the evaluation of endometrial pathology. Fertil Steril. 2010;94(7):2721−2725.
- van Dongen H, de Kroon CD, Jacobi CE, Trimbos JB, Jansen FW. Diagnostic hysteroscopy in abnormal uterine bleeding: a systematic review and meta-analysis. BJOG. 2007;114(6):664–75.
- Loffer FD. Hysteroscopy with selective endometrial sampling compared with D & C for abnormal uterine bleeding: the value of a negative hysteroscopic view. Obstet Gynecol. 1989;73(1):16–20.
- Angioni S, Loddo A, Milano F, Piras B, Minerba L, Melis GB. Detection of benign intracavitary lesions in postmenopausal women with abnormal uterine bleeding: a prospective comparative study on outpatient hysteroscopy and blind biopsy. J Minim Invasive Gynecol. 2008;15(1):87–91.
- Lo KY, Yuen PM. The role of outpatient diagnostic hysteroscopy in identifying anatomic pathology and histopathology in the endometrial cavity. J Am Assoc Gynecol Laparosc. 2000;7(3):381–385.
- Garuti G, Sambruni I, Colonneli M, Luerti M. Accuracy of hysteroscopy in predicting histopathology of endometrium in 1500 women. J Am Assoc Gynecol Laparosc. 2001;8(2):207–213.
- Munro MG, Brooks PG. Use of local anesthesia for office diagnostic and operative hysteroscopy. J Minim Invasive Gynecol. 2010;17(6):709–718.