User login
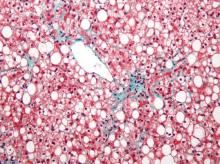
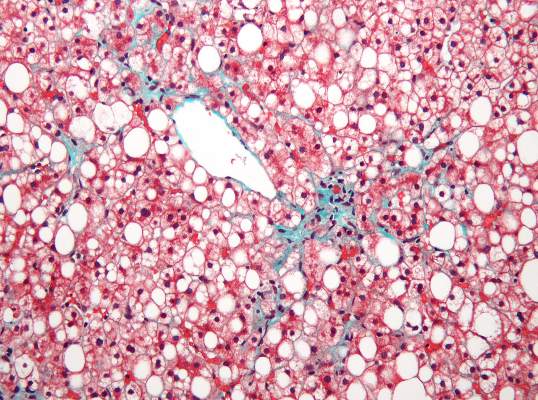
Researchers found an association between nonalcoholic fatty liver disease (NAFLD) and myocardial dysfunction and remodeling, according to a new study published in Hepatology.
“Both NAFLD and heart failure (particularly heart failure with preserved ejection fraction) are obesity-related conditions that have reached epidemic proportions. We know from epidemiologic studies that persons with NAFLD are more likely to die from cardiovascular disease than from liver-related death. This risk seems to be proportional to the amount of fat in the liver and is independent of the presence of nonalcoholic steatohepatitis (NASH). There have been numerous studies that have focused on the relationship between NAFLD and coronary artery disease, but very little work has been done to determine relationships with heart failure,” Dr. Lisa B. VanWagner of Northwestern University in Chicago noted. She continued, “There are several well-established major risk factors for the development of clinical heart failure, including coronary artery disease, diabetes, and hypertension, all of which are also closely associated with NAFLD. However, whether NAFLD is independently associated with subclinical myocardial remodeling or dysfunction that may lead to the development of clinical heart failure is unknown.”
NAFLD and heart failure are both associated with obesity. Likewise, there is evidence that NAFLD may also be related to endothelial dysfunction, coronary plaques, coronary artery calcifications, as well as being an independent risk factor for cardiovascular disease.
Dr. VanWagner and her colleagues conducted a cross-sectional study of 2,713 patients from the CARDIA (Coronary Artery Risk Development in Young Adults) study to understand any associations between NAFLD and abnormalities in left ventricular (LV) function and structure. Study participants completed CT quantification of liver fat and echocardiography with Doppler during the 25-year follow-up to the initial study (Hepatology 2015;62:773-83 [doi:10.1002/hep.27869]). Participants were excluded from analysis if they had missing or incomplete imaging, pregnancy, a history of MI or heart failure, cirrhosis, hepatitis, or chronic liver disease risk factors, or if they weighed more than 450 pounds,
Of the 2,713 subjects included in analysis, 48% were black and 58.8% were female. NAFLD was detected in 10% (n = 271) of participants. Those with NAFLD were more likely to be white males with metabolic syndrome and who were obese and had higher CT-measured levels of visceral adipose tissue, and an increased waist circumference and waist-to-hip ratio. Insulin resistance markers such as elevated fasting glucose, elevated C-reactive protein, and hypertriglyceridemia were more common in the participants with NAFLD.
Study participants with NAFLD had signs of myocardial remodeling such as more left ventricular wall thickness, LV end-diastolic volume, left aortic volume index, and LV mass index. Likewise, NAFLD was associated with more circumferential strain and global longitudinal strain but no differences in ejection fraction.
Subclinical systolic dysfunction (P less than .001 for the trend), subclinical diastolic dysfunction with impaired left ventricular relaxation (34.6% vs. 23.6%; P less than .0001), and elevated LV filling pressures (33.3% vs. 23.7%; P less than .001) was more common in NAFLD participants, compared with non-NAFLD subjects.
After researchers adjusted for health behaviors and demographic factors, evidence of NAFLD was associated with worse GLS (P less than .0001). Finally, NAFLD was associated with subclinical cardiac remodeling and dysfunction even after adjustment for body mass index and heart failure risk factors (P less than .01).
Dr. VanWagner summarized, “NAFLD may not necessarily be a ‘benign condition’ as previously thought. In our study, we determined liver fat by CT scan, which admittedly detects fat at a higher level (typically greater than 30%) than for example on MRI, which can detect fat as low as 5%. A fatty liver detected on CT or even on [ultrasound], which has similar sensitivity as CT for detecting liver fat should prompt evaluation for additional cardiovascular risk factors and treatment of identified abnormalities to reduce [atherosclerotic cardiovascular disease] and [heart failure] risk. Currently, our study only shows associations between liver fat and subclinical changes in the myocardium and causality cannot be determined. [On the basis] of our data, we cannot recommend screening for HF [heart failure] in this population, but future studies are needed to determine if NAFLD in fact lies in the casual pathway for the development of clinical HF.”
The investigators reported multiple supporting sources, including the National Institutes of Health, American Association for the Study of Liver Disease Foundation, and the American Heart Association. Dr. Lewis reported receiving grants from Novo Nordisk.
Researchers found an association between nonalcoholic fatty liver disease (NAFLD) and myocardial dysfunction and remodeling, according to a new study published in Hepatology.
“Both NAFLD and heart failure (particularly heart failure with preserved ejection fraction) are obesity-related conditions that have reached epidemic proportions. We know from epidemiologic studies that persons with NAFLD are more likely to die from cardiovascular disease than from liver-related death. This risk seems to be proportional to the amount of fat in the liver and is independent of the presence of nonalcoholic steatohepatitis (NASH). There have been numerous studies that have focused on the relationship between NAFLD and coronary artery disease, but very little work has been done to determine relationships with heart failure,” Dr. Lisa B. VanWagner of Northwestern University in Chicago noted. She continued, “There are several well-established major risk factors for the development of clinical heart failure, including coronary artery disease, diabetes, and hypertension, all of which are also closely associated with NAFLD. However, whether NAFLD is independently associated with subclinical myocardial remodeling or dysfunction that may lead to the development of clinical heart failure is unknown.”
NAFLD and heart failure are both associated with obesity. Likewise, there is evidence that NAFLD may also be related to endothelial dysfunction, coronary plaques, coronary artery calcifications, as well as being an independent risk factor for cardiovascular disease.
Dr. VanWagner and her colleagues conducted a cross-sectional study of 2,713 patients from the CARDIA (Coronary Artery Risk Development in Young Adults) study to understand any associations between NAFLD and abnormalities in left ventricular (LV) function and structure. Study participants completed CT quantification of liver fat and echocardiography with Doppler during the 25-year follow-up to the initial study (Hepatology 2015;62:773-83 [doi:10.1002/hep.27869]). Participants were excluded from analysis if they had missing or incomplete imaging, pregnancy, a history of MI or heart failure, cirrhosis, hepatitis, or chronic liver disease risk factors, or if they weighed more than 450 pounds,
Of the 2,713 subjects included in analysis, 48% were black and 58.8% were female. NAFLD was detected in 10% (n = 271) of participants. Those with NAFLD were more likely to be white males with metabolic syndrome and who were obese and had higher CT-measured levels of visceral adipose tissue, and an increased waist circumference and waist-to-hip ratio. Insulin resistance markers such as elevated fasting glucose, elevated C-reactive protein, and hypertriglyceridemia were more common in the participants with NAFLD.
Study participants with NAFLD had signs of myocardial remodeling such as more left ventricular wall thickness, LV end-diastolic volume, left aortic volume index, and LV mass index. Likewise, NAFLD was associated with more circumferential strain and global longitudinal strain but no differences in ejection fraction.
Subclinical systolic dysfunction (P less than .001 for the trend), subclinical diastolic dysfunction with impaired left ventricular relaxation (34.6% vs. 23.6%; P less than .0001), and elevated LV filling pressures (33.3% vs. 23.7%; P less than .001) was more common in NAFLD participants, compared with non-NAFLD subjects.
After researchers adjusted for health behaviors and demographic factors, evidence of NAFLD was associated with worse GLS (P less than .0001). Finally, NAFLD was associated with subclinical cardiac remodeling and dysfunction even after adjustment for body mass index and heart failure risk factors (P less than .01).
Dr. VanWagner summarized, “NAFLD may not necessarily be a ‘benign condition’ as previously thought. In our study, we determined liver fat by CT scan, which admittedly detects fat at a higher level (typically greater than 30%) than for example on MRI, which can detect fat as low as 5%. A fatty liver detected on CT or even on [ultrasound], which has similar sensitivity as CT for detecting liver fat should prompt evaluation for additional cardiovascular risk factors and treatment of identified abnormalities to reduce [atherosclerotic cardiovascular disease] and [heart failure] risk. Currently, our study only shows associations between liver fat and subclinical changes in the myocardium and causality cannot be determined. [On the basis] of our data, we cannot recommend screening for HF [heart failure] in this population, but future studies are needed to determine if NAFLD in fact lies in the casual pathway for the development of clinical HF.”
The investigators reported multiple supporting sources, including the National Institutes of Health, American Association for the Study of Liver Disease Foundation, and the American Heart Association. Dr. Lewis reported receiving grants from Novo Nordisk.
Researchers found an association between nonalcoholic fatty liver disease (NAFLD) and myocardial dysfunction and remodeling, according to a new study published in Hepatology.
“Both NAFLD and heart failure (particularly heart failure with preserved ejection fraction) are obesity-related conditions that have reached epidemic proportions. We know from epidemiologic studies that persons with NAFLD are more likely to die from cardiovascular disease than from liver-related death. This risk seems to be proportional to the amount of fat in the liver and is independent of the presence of nonalcoholic steatohepatitis (NASH). There have been numerous studies that have focused on the relationship between NAFLD and coronary artery disease, but very little work has been done to determine relationships with heart failure,” Dr. Lisa B. VanWagner of Northwestern University in Chicago noted. She continued, “There are several well-established major risk factors for the development of clinical heart failure, including coronary artery disease, diabetes, and hypertension, all of which are also closely associated with NAFLD. However, whether NAFLD is independently associated with subclinical myocardial remodeling or dysfunction that may lead to the development of clinical heart failure is unknown.”
NAFLD and heart failure are both associated with obesity. Likewise, there is evidence that NAFLD may also be related to endothelial dysfunction, coronary plaques, coronary artery calcifications, as well as being an independent risk factor for cardiovascular disease.
Dr. VanWagner and her colleagues conducted a cross-sectional study of 2,713 patients from the CARDIA (Coronary Artery Risk Development in Young Adults) study to understand any associations between NAFLD and abnormalities in left ventricular (LV) function and structure. Study participants completed CT quantification of liver fat and echocardiography with Doppler during the 25-year follow-up to the initial study (Hepatology 2015;62:773-83 [doi:10.1002/hep.27869]). Participants were excluded from analysis if they had missing or incomplete imaging, pregnancy, a history of MI or heart failure, cirrhosis, hepatitis, or chronic liver disease risk factors, or if they weighed more than 450 pounds,
Of the 2,713 subjects included in analysis, 48% were black and 58.8% were female. NAFLD was detected in 10% (n = 271) of participants. Those with NAFLD were more likely to be white males with metabolic syndrome and who were obese and had higher CT-measured levels of visceral adipose tissue, and an increased waist circumference and waist-to-hip ratio. Insulin resistance markers such as elevated fasting glucose, elevated C-reactive protein, and hypertriglyceridemia were more common in the participants with NAFLD.
Study participants with NAFLD had signs of myocardial remodeling such as more left ventricular wall thickness, LV end-diastolic volume, left aortic volume index, and LV mass index. Likewise, NAFLD was associated with more circumferential strain and global longitudinal strain but no differences in ejection fraction.
Subclinical systolic dysfunction (P less than .001 for the trend), subclinical diastolic dysfunction with impaired left ventricular relaxation (34.6% vs. 23.6%; P less than .0001), and elevated LV filling pressures (33.3% vs. 23.7%; P less than .001) was more common in NAFLD participants, compared with non-NAFLD subjects.
After researchers adjusted for health behaviors and demographic factors, evidence of NAFLD was associated with worse GLS (P less than .0001). Finally, NAFLD was associated with subclinical cardiac remodeling and dysfunction even after adjustment for body mass index and heart failure risk factors (P less than .01).
Dr. VanWagner summarized, “NAFLD may not necessarily be a ‘benign condition’ as previously thought. In our study, we determined liver fat by CT scan, which admittedly detects fat at a higher level (typically greater than 30%) than for example on MRI, which can detect fat as low as 5%. A fatty liver detected on CT or even on [ultrasound], which has similar sensitivity as CT for detecting liver fat should prompt evaluation for additional cardiovascular risk factors and treatment of identified abnormalities to reduce [atherosclerotic cardiovascular disease] and [heart failure] risk. Currently, our study only shows associations between liver fat and subclinical changes in the myocardium and causality cannot be determined. [On the basis] of our data, we cannot recommend screening for HF [heart failure] in this population, but future studies are needed to determine if NAFLD in fact lies in the casual pathway for the development of clinical HF.”
The investigators reported multiple supporting sources, including the National Institutes of Health, American Association for the Study of Liver Disease Foundation, and the American Heart Association. Dr. Lewis reported receiving grants from Novo Nordisk.
FROM HEPATOLOGY
Key clinical point: Researchers found an association between nonalcoholic fatty liver disease and myocardial dysfunction and remodeling.
Major finding: Subclinical systolic dysfunction (P less than .001 for the trend), subclinical diastolic dysfunction with impaired left ventricular relaxation (P less than .0001), and elevated LV filling pressures (P less than .001) was more common in participants with NAFLD than in those without.
Data source: A cross-sectional study of 2,713 patients from the CARDIA study using CT quantification of liver fat and echocardiography with Doppler during the 25-year follow-up to the initial study.
Disclosures: The investigators reported multiple supporting sources, including the National Institutes of Health, American Association for the Study of Liver Disease Foundation, and the American Heart Association. Dr. Lewis reported receiving grants from Novo Nordisk.