User login
Pancreatic cancer incidence rates have been increasing among men and women since 2000. From 2006 to 2010, incidence rates increased by 1.3% per year, and the death rate for pancreatic cancer increased by 0.4% per year. An estimated 39,590 deaths are expected to occur in 2014, with similar numbers expected in women (19,420) and in men (20,170).1
Pancreatic cancer incidence and mortality rates vary across different racial/ethnic groups, with the highest rates in African Americans and the lowest rates in Asian Americans/Pacific Islanders. During 2005-2009, the incidence rate (per 100,000 persons) was 15.3 for African Americans, 11.6 for whites, and 8.8 for Asian Americans/Pacific Islanders. According to Surveillance, Epidemiology, and End Results (SEER) 18, for the period 2007-2011, the incidence rate was 17.2 for black men and 14 for white men; the incidence rate was 14.2 for black women and 10.7 for white women.2
Well-known risk factors for pancreatic cancer include tobacco use, chronic pancreatitis, obesity, diabetes, and alcohol use. Individuals with Lynch syndrome and certain other hereditary syndromes are at increased risk.3 Newer risk factors of interest include chronic infection with hepatitis B, hepatitis C, or Helicobacter pylori. These risk factors have in common a backdrop of inflammation, which may predispose the patient to developing pancreatic cancer.
Whether veterans as a group are at increased risk for developing pancreatic cancer is unclear. One study suggests there may be an increased risk in obese veterans.4 Certain high-risk groups among veterans have been identified, such as veterans with hepatitis C, diabetes, Gaucher disease, and women nurses from the Vietnam War era.5-8
Comorbidity, an area of increasing interest, was not a predictor of survival in a pilot study from one VA medical center.9
MANAGEMENT OF METASTATIC PANCREATIC CANCER
Management of metastatic pancreatic cancer has 2 components: systemic disease treatment and supportive care.
Systemic Disease Treatment
The standard of care at the VA for patients with metastatic pancreatic cancer follows the national guidelines, including the National Comprehensive Cancer Network (NCCN) guidelines.10
• For first-line therapy, currently recognized regimens include 5-fluorouracil (5-FU), with irinotecan, leucovorin, and oxaliplatin (FOLFIRINOX), gemcitabine with albumin-bound paclitaxel, and gemcitabine with erlotinib. Single- agent gemcitabine or supportive care is for patients with poor performance status.
• For second-line therapy, switching from a gemcitabine to a fluoropyrimidine-based regimen, and vice versa is a recognized option.
• When possible, participation in clinical trials is recommended.
Treatment for metastatic pancreatic cancer has not been satisfactory. In 1997, single-agent gemcitabine was approved by the FDA and became the standard of care when a randomized controlled trial of gemcitabine in symptomatic patients showed an increased survival compared with that of 5-FU.11 The median survival durations were 5.65 and 4.41 months for gemcitabine-treated and 5-FU-treated patients, respectively (P = .0025).
Many attempts to combine gemcitabine with other medications were unsuccessful until 2005 when gemcitabine in combination with erlotinib was approved by the FDA as a first-line therapy. A randomized trial showed a 2-week prolongation in survival with the addition of erlotinib. The median survivalwas 6.24 months in the combination group compared with 5.91 months in the gemcitabine group.12 Erlotinib is associatedwith increased skin toxicity anddiarrhea. Interestingly, trials with many other targeted agents, such as bevacizumab, have not demonstrated any survival improvement.13
In 2011, a French study showed that the multidrug combination of FOLFIRINOX in patients with good performance status (Eastern Cooperative Oncology Group Performance Status [ECOG PS] 0 or 1) increased overall mean survival to 11.1 months compared with 6.7 months in the gemcitabine group, but with more neutropenia, diarrhea, and sensory neuropathy.11
In 2013, a comparison of nab-paclitaxel plus gemcitabine and gemcitabine alone for patients with a Karnofsky performance-status score of 70 or more showed a median survival of 8.5 months vs 6.7 months, with more neutropenia, fatigue, and neurotoxicity in the combination group.14,15 This regimen was approved in September 2013 by the FDA as first-line treatment for patients with metastatic pancreatic cancer.
For second-line therapy, a recent phase 2 study of ruxolitinib and capecitabine demonstrated prolongation of overall survival in patients who had an elevated C-reactive protein (CRP). In the high CRP subgroup, 3- and 6-month survival was 48% and 42% with ruxolitinib, but was 29% and 11% with placebo.16 Further studies are planned.
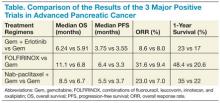
Although these developments, summarized in the Table, are exciting, determining how they will apply to clinical practice will require careful patient selection and shared decision making about anticipated toxicities.
List of New Agents
Erlotinib is an oral agent and a small molecule that inhibits the tyrosine kinase activity of the human epidermal growth factor receptor (EGFR or HER1) pathway.
Albumin-bound paclitaxel (nab-paclitaxel) is effective in tumors that overexpress the albumin-binding protein secreted protein, acidic and rich in cysteine (SPARC), such as breast cancer, and used in pancreatic cancer (as this cancer also overexpresses SPARC). It is hypothesized, but not yet proven, that blockage of SPARC proteins in pancreatic cancer patients can affect tumor growth. The strategy here is to attack inflammatory stromal tissue. Pegylated recombinant human hyaluronidase (PEGPH20) represents another way to target the tumor stroma.17
Ruxolitinib, a janus kinase (JAK) inhibitor, decreases the production of inflammatory cytokines.
Immunotherapy research is ongoing, using anti-cytotoxic-leukocyte associated antigens 4 (anti-CTLA-4) and cancer vaccines.18,19
Research is increasing along many different avenues, and many other research approaches beyond the scope of this article are also underway, funded by the NCCN, private foundations such as the Lustgarten Foundation, and other groups.
SUPPORTIVE CARE
Supportive care aspects relevant to pancreatic cancer are biliary drainage and pain control.
Biliary Drainage
It is often necessary to place stents to improve bilirubin levels to relieve jaundice as well as obtain tissue or cells for diagnosis.20
Pain Control
Recent studies have shown that an inflammatory perineural invasion by pancreatic cancer cells leads to increased arborization and hypertrophy of the sensory nerves, helping to explain in part the severe pain experienced by patients.21 In addition to opioids, other options include radiation therapy and an image-guided celiac plexus block.22 The timing of when to start radiation treatments or use a block is not settled, but there is a consensus to consider these interventions earlier rather than later.
IMPLEMENTATION IN THE VA
There are no major barriers for obtaining the newer agents or combinations at the VA when they are indicated. Most of the agents in the Table are on the VA National Formulary, with the exception of nab-paclitaxel and erlotinib. When the requested agents are not in the formulary, the case is reviewed, and the agents are usually approved for use if they are appropriate for treatment according to national guidelines. Patient education about the risks and benefits of chemotherapy is important because some patients may decide against chemotherapy based on past undesirable experiences of relatives or friends with cancer. The major barrier to using the newer regimens is the patient’s poor general condition at diagnosis. If the diagnosis can be made earlier, before their general condition deteriorates significantly, the patients will have more treatment options and an improved outcome. More research is needed to find better treatments for this deadly disease.
CONCLUSIONS
Systemic chemotherapy provides benefit to patients with advanced pancreatic cancer. For the patientswith good performance status (ECOG PS 0 or 1), FOLFIRINOX or gemcitabine plus nab-paclitaxel are reasonable choices for first-line treatment. Gemcitabine plus nab-paclitaxel is an option for the patients with modest performance status who cannot tolerate the FOLFIRINOX regimen. For patients with poor performance status, gemcitabine as a single-agent or as supportive care may be offered. Although the new combination regimens are more effective than single-agent gemcitabine, the median survival is still < 1 year. More effective therapy is needed. Participation in clinical trials is encouraged.
Acknowledgements
I want to thank my colleagues Dr. Victor Chang and Dr. Basil Kasimis for their comments.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014;64(1):9-29.
2. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63(1):11-30.
3. Solomon S, Das S, Brand R, Whitcomb DC. Inherited pancreatic cancer syndromes. Cancer J. 2012;18(6):485-491.
4. Samanic C, Gridley G, Chow WH, Lubin J, Hoover RN, Fraumeni JF Jr. Obesity and cancer risk among white and black United States veterans. Cancer Causes Control. 2004;15(1):35-43.
5. El-Serag HB, Engels EA, Landgren O, et al. Risk of hepatobiliary and pancreatic cancers after hepatitis C virus infection: A population-based study of U.S. veterans. Hepatology. 2009;49(1):116-123.
6. Atchison EA, Gridley G, Carreon JD, Leitzmann MF, McGlynn KA. Risk of cancer in a large cohort of U.S. veterans with diabetes. Int J Cancer. 2011;128(3):635-643.
7. Landgren O, Turesson I, Gridley G, Caporaso NE. Risk of malignant disease among 1525 adult male US Veterans with Gaucher disease. Arch Intern Med. 2007;167(11):1189-1194.
8. Kang HK, Cypel Y, Kilbourne AM, et al. HealthViEWS: Mortality study of female US Vietnam era veterans, 1965-2010. Am J Epidemiol. 2014;179(6):721-730.
9. Kim K, Zhong F, Chang VT, et al. Clinical characteristics and comorbidity of veterans with pancreatic cancer. J Clin Oncol. 2011;29(15)(suppl):Abstract e14549.
10. National Comprehensive Cancer Network. NCCN Guidelines in the treatment of pancreatic adenocarcinoma. http://www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf. Accessed June 15, 2014.
11. Burris HA III, Moore MJ, Andersen J, et al. Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: A randomized trial. J Clin Oncol. 1997;15(6):2403-2413.
12. Moore MJ, Goldstein D, Hamm J, et al. Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: A phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol. 2007;25(15):1960-1966.
13. Kindler HL, Niedzwiecki D, Hollis D, et al. Gemcitabine plus bevacizumab compared with gemcitabine plus placebo in patients with advanced pancreatic cancer: phase III trial of the Cancer and Leukemia Group B (CALGB 80303). J Clin Oncol. 2010;28(22):3617-3622.
14. Conroy T, Desseigne F, Ychou M. Groupe Tumeurs Digestives of Unicancer; PRODIGE Intergroup. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364(19):1817-1825.
15. Von Hoff DD, Ervin T, Arena FP, et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369(18):1691-1703.
16. Hurwitz H, Uppal N, Wagner SA, et al. A randomized double-blind phase 2 study of ruxolitinib (RUX) or placebo (PBO) with capecitabine (CAPE) as second-line therapy in patients (pts) with metastatic pancreatic cancer (mPC). Abstract 4000. J Clin Oncol. 2014;32(suppl):5s.
17. Provenzano PP, Cuevas C, Chang AE, Goel VK, Von Hoff DD, Hingorani SR. Enzymatic targeting of the stroma ablates physical barriers to treatment of pancreatic ductal adenocarcinoma. Cancer Cell. 2012;21(3):418-429.
18. Le DT, Lutz E, Uram JN, et al. Evaluation of ipilimumab in combination with allogeneic pancreatic tumor cells transfected with a GM-CSF gene in previously treated pancreatic cancer. J Immunother. 2013;36(7):382-389.
19. Plate JM. Advances in therapeutic vaccines for pancreatic cancer. Discov Med. 2012;14(75):89-94.
20. Sharaiha RZ, Widmer J, Kahaleh M. Palliation of pancreatic ductal obstruction in pancreatic cancer. Gastrointest Endosc Clin N Am. 2013;23(4):917-923.
21. Bapat AA, Hostetter G, Von Hoff DD, Han H. Perineural invasion and associated pain in pancreatic cancer. Nat Rev Cancer. 2011;11(10):695-707.
22. Erdek MA, King LM, Ellsworth SG. Pain management and palliative care in pancreatic cancer. Curr Probl Cancer. 2013;37(5):266-272.
Pancreatic cancer incidence rates have been increasing among men and women since 2000. From 2006 to 2010, incidence rates increased by 1.3% per year, and the death rate for pancreatic cancer increased by 0.4% per year. An estimated 39,590 deaths are expected to occur in 2014, with similar numbers expected in women (19,420) and in men (20,170).1
Pancreatic cancer incidence and mortality rates vary across different racial/ethnic groups, with the highest rates in African Americans and the lowest rates in Asian Americans/Pacific Islanders. During 2005-2009, the incidence rate (per 100,000 persons) was 15.3 for African Americans, 11.6 for whites, and 8.8 for Asian Americans/Pacific Islanders. According to Surveillance, Epidemiology, and End Results (SEER) 18, for the period 2007-2011, the incidence rate was 17.2 for black men and 14 for white men; the incidence rate was 14.2 for black women and 10.7 for white women.2
Well-known risk factors for pancreatic cancer include tobacco use, chronic pancreatitis, obesity, diabetes, and alcohol use. Individuals with Lynch syndrome and certain other hereditary syndromes are at increased risk.3 Newer risk factors of interest include chronic infection with hepatitis B, hepatitis C, or Helicobacter pylori. These risk factors have in common a backdrop of inflammation, which may predispose the patient to developing pancreatic cancer.
Whether veterans as a group are at increased risk for developing pancreatic cancer is unclear. One study suggests there may be an increased risk in obese veterans.4 Certain high-risk groups among veterans have been identified, such as veterans with hepatitis C, diabetes, Gaucher disease, and women nurses from the Vietnam War era.5-8
Comorbidity, an area of increasing interest, was not a predictor of survival in a pilot study from one VA medical center.9
MANAGEMENT OF METASTATIC PANCREATIC CANCER
Management of metastatic pancreatic cancer has 2 components: systemic disease treatment and supportive care.
Systemic Disease Treatment
The standard of care at the VA for patients with metastatic pancreatic cancer follows the national guidelines, including the National Comprehensive Cancer Network (NCCN) guidelines.10
• For first-line therapy, currently recognized regimens include 5-fluorouracil (5-FU), with irinotecan, leucovorin, and oxaliplatin (FOLFIRINOX), gemcitabine with albumin-bound paclitaxel, and gemcitabine with erlotinib. Single- agent gemcitabine or supportive care is for patients with poor performance status.
• For second-line therapy, switching from a gemcitabine to a fluoropyrimidine-based regimen, and vice versa is a recognized option.
• When possible, participation in clinical trials is recommended.
Treatment for metastatic pancreatic cancer has not been satisfactory. In 1997, single-agent gemcitabine was approved by the FDA and became the standard of care when a randomized controlled trial of gemcitabine in symptomatic patients showed an increased survival compared with that of 5-FU.11 The median survival durations were 5.65 and 4.41 months for gemcitabine-treated and 5-FU-treated patients, respectively (P = .0025).
Many attempts to combine gemcitabine with other medications were unsuccessful until 2005 when gemcitabine in combination with erlotinib was approved by the FDA as a first-line therapy. A randomized trial showed a 2-week prolongation in survival with the addition of erlotinib. The median survivalwas 6.24 months in the combination group compared with 5.91 months in the gemcitabine group.12 Erlotinib is associatedwith increased skin toxicity anddiarrhea. Interestingly, trials with many other targeted agents, such as bevacizumab, have not demonstrated any survival improvement.13
In 2011, a French study showed that the multidrug combination of FOLFIRINOX in patients with good performance status (Eastern Cooperative Oncology Group Performance Status [ECOG PS] 0 or 1) increased overall mean survival to 11.1 months compared with 6.7 months in the gemcitabine group, but with more neutropenia, diarrhea, and sensory neuropathy.11
In 2013, a comparison of nab-paclitaxel plus gemcitabine and gemcitabine alone for patients with a Karnofsky performance-status score of 70 or more showed a median survival of 8.5 months vs 6.7 months, with more neutropenia, fatigue, and neurotoxicity in the combination group.14,15 This regimen was approved in September 2013 by the FDA as first-line treatment for patients with metastatic pancreatic cancer.
For second-line therapy, a recent phase 2 study of ruxolitinib and capecitabine demonstrated prolongation of overall survival in patients who had an elevated C-reactive protein (CRP). In the high CRP subgroup, 3- and 6-month survival was 48% and 42% with ruxolitinib, but was 29% and 11% with placebo.16 Further studies are planned.
Although these developments, summarized in the Table, are exciting, determining how they will apply to clinical practice will require careful patient selection and shared decision making about anticipated toxicities.
List of New Agents
Erlotinib is an oral agent and a small molecule that inhibits the tyrosine kinase activity of the human epidermal growth factor receptor (EGFR or HER1) pathway.
Albumin-bound paclitaxel (nab-paclitaxel) is effective in tumors that overexpress the albumin-binding protein secreted protein, acidic and rich in cysteine (SPARC), such as breast cancer, and used in pancreatic cancer (as this cancer also overexpresses SPARC). It is hypothesized, but not yet proven, that blockage of SPARC proteins in pancreatic cancer patients can affect tumor growth. The strategy here is to attack inflammatory stromal tissue. Pegylated recombinant human hyaluronidase (PEGPH20) represents another way to target the tumor stroma.17
Ruxolitinib, a janus kinase (JAK) inhibitor, decreases the production of inflammatory cytokines.
Immunotherapy research is ongoing, using anti-cytotoxic-leukocyte associated antigens 4 (anti-CTLA-4) and cancer vaccines.18,19
Research is increasing along many different avenues, and many other research approaches beyond the scope of this article are also underway, funded by the NCCN, private foundations such as the Lustgarten Foundation, and other groups.
SUPPORTIVE CARE
Supportive care aspects relevant to pancreatic cancer are biliary drainage and pain control.
Biliary Drainage
It is often necessary to place stents to improve bilirubin levels to relieve jaundice as well as obtain tissue or cells for diagnosis.20
Pain Control
Recent studies have shown that an inflammatory perineural invasion by pancreatic cancer cells leads to increased arborization and hypertrophy of the sensory nerves, helping to explain in part the severe pain experienced by patients.21 In addition to opioids, other options include radiation therapy and an image-guided celiac plexus block.22 The timing of when to start radiation treatments or use a block is not settled, but there is a consensus to consider these interventions earlier rather than later.
IMPLEMENTATION IN THE VA
There are no major barriers for obtaining the newer agents or combinations at the VA when they are indicated. Most of the agents in the Table are on the VA National Formulary, with the exception of nab-paclitaxel and erlotinib. When the requested agents are not in the formulary, the case is reviewed, and the agents are usually approved for use if they are appropriate for treatment according to national guidelines. Patient education about the risks and benefits of chemotherapy is important because some patients may decide against chemotherapy based on past undesirable experiences of relatives or friends with cancer. The major barrier to using the newer regimens is the patient’s poor general condition at diagnosis. If the diagnosis can be made earlier, before their general condition deteriorates significantly, the patients will have more treatment options and an improved outcome. More research is needed to find better treatments for this deadly disease.
CONCLUSIONS
Systemic chemotherapy provides benefit to patients with advanced pancreatic cancer. For the patientswith good performance status (ECOG PS 0 or 1), FOLFIRINOX or gemcitabine plus nab-paclitaxel are reasonable choices for first-line treatment. Gemcitabine plus nab-paclitaxel is an option for the patients with modest performance status who cannot tolerate the FOLFIRINOX regimen. For patients with poor performance status, gemcitabine as a single-agent or as supportive care may be offered. Although the new combination regimens are more effective than single-agent gemcitabine, the median survival is still < 1 year. More effective therapy is needed. Participation in clinical trials is encouraged.
Acknowledgements
I want to thank my colleagues Dr. Victor Chang and Dr. Basil Kasimis for their comments.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Pancreatic cancer incidence rates have been increasing among men and women since 2000. From 2006 to 2010, incidence rates increased by 1.3% per year, and the death rate for pancreatic cancer increased by 0.4% per year. An estimated 39,590 deaths are expected to occur in 2014, with similar numbers expected in women (19,420) and in men (20,170).1
Pancreatic cancer incidence and mortality rates vary across different racial/ethnic groups, with the highest rates in African Americans and the lowest rates in Asian Americans/Pacific Islanders. During 2005-2009, the incidence rate (per 100,000 persons) was 15.3 for African Americans, 11.6 for whites, and 8.8 for Asian Americans/Pacific Islanders. According to Surveillance, Epidemiology, and End Results (SEER) 18, for the period 2007-2011, the incidence rate was 17.2 for black men and 14 for white men; the incidence rate was 14.2 for black women and 10.7 for white women.2
Well-known risk factors for pancreatic cancer include tobacco use, chronic pancreatitis, obesity, diabetes, and alcohol use. Individuals with Lynch syndrome and certain other hereditary syndromes are at increased risk.3 Newer risk factors of interest include chronic infection with hepatitis B, hepatitis C, or Helicobacter pylori. These risk factors have in common a backdrop of inflammation, which may predispose the patient to developing pancreatic cancer.
Whether veterans as a group are at increased risk for developing pancreatic cancer is unclear. One study suggests there may be an increased risk in obese veterans.4 Certain high-risk groups among veterans have been identified, such as veterans with hepatitis C, diabetes, Gaucher disease, and women nurses from the Vietnam War era.5-8
Comorbidity, an area of increasing interest, was not a predictor of survival in a pilot study from one VA medical center.9
MANAGEMENT OF METASTATIC PANCREATIC CANCER
Management of metastatic pancreatic cancer has 2 components: systemic disease treatment and supportive care.
Systemic Disease Treatment
The standard of care at the VA for patients with metastatic pancreatic cancer follows the national guidelines, including the National Comprehensive Cancer Network (NCCN) guidelines.10
• For first-line therapy, currently recognized regimens include 5-fluorouracil (5-FU), with irinotecan, leucovorin, and oxaliplatin (FOLFIRINOX), gemcitabine with albumin-bound paclitaxel, and gemcitabine with erlotinib. Single- agent gemcitabine or supportive care is for patients with poor performance status.
• For second-line therapy, switching from a gemcitabine to a fluoropyrimidine-based regimen, and vice versa is a recognized option.
• When possible, participation in clinical trials is recommended.
Treatment for metastatic pancreatic cancer has not been satisfactory. In 1997, single-agent gemcitabine was approved by the FDA and became the standard of care when a randomized controlled trial of gemcitabine in symptomatic patients showed an increased survival compared with that of 5-FU.11 The median survival durations were 5.65 and 4.41 months for gemcitabine-treated and 5-FU-treated patients, respectively (P = .0025).
Many attempts to combine gemcitabine with other medications were unsuccessful until 2005 when gemcitabine in combination with erlotinib was approved by the FDA as a first-line therapy. A randomized trial showed a 2-week prolongation in survival with the addition of erlotinib. The median survivalwas 6.24 months in the combination group compared with 5.91 months in the gemcitabine group.12 Erlotinib is associatedwith increased skin toxicity anddiarrhea. Interestingly, trials with many other targeted agents, such as bevacizumab, have not demonstrated any survival improvement.13
In 2011, a French study showed that the multidrug combination of FOLFIRINOX in patients with good performance status (Eastern Cooperative Oncology Group Performance Status [ECOG PS] 0 or 1) increased overall mean survival to 11.1 months compared with 6.7 months in the gemcitabine group, but with more neutropenia, diarrhea, and sensory neuropathy.11
In 2013, a comparison of nab-paclitaxel plus gemcitabine and gemcitabine alone for patients with a Karnofsky performance-status score of 70 or more showed a median survival of 8.5 months vs 6.7 months, with more neutropenia, fatigue, and neurotoxicity in the combination group.14,15 This regimen was approved in September 2013 by the FDA as first-line treatment for patients with metastatic pancreatic cancer.
For second-line therapy, a recent phase 2 study of ruxolitinib and capecitabine demonstrated prolongation of overall survival in patients who had an elevated C-reactive protein (CRP). In the high CRP subgroup, 3- and 6-month survival was 48% and 42% with ruxolitinib, but was 29% and 11% with placebo.16 Further studies are planned.
Although these developments, summarized in the Table, are exciting, determining how they will apply to clinical practice will require careful patient selection and shared decision making about anticipated toxicities.
List of New Agents
Erlotinib is an oral agent and a small molecule that inhibits the tyrosine kinase activity of the human epidermal growth factor receptor (EGFR or HER1) pathway.
Albumin-bound paclitaxel (nab-paclitaxel) is effective in tumors that overexpress the albumin-binding protein secreted protein, acidic and rich in cysteine (SPARC), such as breast cancer, and used in pancreatic cancer (as this cancer also overexpresses SPARC). It is hypothesized, but not yet proven, that blockage of SPARC proteins in pancreatic cancer patients can affect tumor growth. The strategy here is to attack inflammatory stromal tissue. Pegylated recombinant human hyaluronidase (PEGPH20) represents another way to target the tumor stroma.17
Ruxolitinib, a janus kinase (JAK) inhibitor, decreases the production of inflammatory cytokines.
Immunotherapy research is ongoing, using anti-cytotoxic-leukocyte associated antigens 4 (anti-CTLA-4) and cancer vaccines.18,19
Research is increasing along many different avenues, and many other research approaches beyond the scope of this article are also underway, funded by the NCCN, private foundations such as the Lustgarten Foundation, and other groups.
SUPPORTIVE CARE
Supportive care aspects relevant to pancreatic cancer are biliary drainage and pain control.
Biliary Drainage
It is often necessary to place stents to improve bilirubin levels to relieve jaundice as well as obtain tissue or cells for diagnosis.20
Pain Control
Recent studies have shown that an inflammatory perineural invasion by pancreatic cancer cells leads to increased arborization and hypertrophy of the sensory nerves, helping to explain in part the severe pain experienced by patients.21 In addition to opioids, other options include radiation therapy and an image-guided celiac plexus block.22 The timing of when to start radiation treatments or use a block is not settled, but there is a consensus to consider these interventions earlier rather than later.
IMPLEMENTATION IN THE VA
There are no major barriers for obtaining the newer agents or combinations at the VA when they are indicated. Most of the agents in the Table are on the VA National Formulary, with the exception of nab-paclitaxel and erlotinib. When the requested agents are not in the formulary, the case is reviewed, and the agents are usually approved for use if they are appropriate for treatment according to national guidelines. Patient education about the risks and benefits of chemotherapy is important because some patients may decide against chemotherapy based on past undesirable experiences of relatives or friends with cancer. The major barrier to using the newer regimens is the patient’s poor general condition at diagnosis. If the diagnosis can be made earlier, before their general condition deteriorates significantly, the patients will have more treatment options and an improved outcome. More research is needed to find better treatments for this deadly disease.
CONCLUSIONS
Systemic chemotherapy provides benefit to patients with advanced pancreatic cancer. For the patientswith good performance status (ECOG PS 0 or 1), FOLFIRINOX or gemcitabine plus nab-paclitaxel are reasonable choices for first-line treatment. Gemcitabine plus nab-paclitaxel is an option for the patients with modest performance status who cannot tolerate the FOLFIRINOX regimen. For patients with poor performance status, gemcitabine as a single-agent or as supportive care may be offered. Although the new combination regimens are more effective than single-agent gemcitabine, the median survival is still < 1 year. More effective therapy is needed. Participation in clinical trials is encouraged.
Acknowledgements
I want to thank my colleagues Dr. Victor Chang and Dr. Basil Kasimis for their comments.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014;64(1):9-29.
2. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63(1):11-30.
3. Solomon S, Das S, Brand R, Whitcomb DC. Inherited pancreatic cancer syndromes. Cancer J. 2012;18(6):485-491.
4. Samanic C, Gridley G, Chow WH, Lubin J, Hoover RN, Fraumeni JF Jr. Obesity and cancer risk among white and black United States veterans. Cancer Causes Control. 2004;15(1):35-43.
5. El-Serag HB, Engels EA, Landgren O, et al. Risk of hepatobiliary and pancreatic cancers after hepatitis C virus infection: A population-based study of U.S. veterans. Hepatology. 2009;49(1):116-123.
6. Atchison EA, Gridley G, Carreon JD, Leitzmann MF, McGlynn KA. Risk of cancer in a large cohort of U.S. veterans with diabetes. Int J Cancer. 2011;128(3):635-643.
7. Landgren O, Turesson I, Gridley G, Caporaso NE. Risk of malignant disease among 1525 adult male US Veterans with Gaucher disease. Arch Intern Med. 2007;167(11):1189-1194.
8. Kang HK, Cypel Y, Kilbourne AM, et al. HealthViEWS: Mortality study of female US Vietnam era veterans, 1965-2010. Am J Epidemiol. 2014;179(6):721-730.
9. Kim K, Zhong F, Chang VT, et al. Clinical characteristics and comorbidity of veterans with pancreatic cancer. J Clin Oncol. 2011;29(15)(suppl):Abstract e14549.
10. National Comprehensive Cancer Network. NCCN Guidelines in the treatment of pancreatic adenocarcinoma. http://www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf. Accessed June 15, 2014.
11. Burris HA III, Moore MJ, Andersen J, et al. Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: A randomized trial. J Clin Oncol. 1997;15(6):2403-2413.
12. Moore MJ, Goldstein D, Hamm J, et al. Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: A phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol. 2007;25(15):1960-1966.
13. Kindler HL, Niedzwiecki D, Hollis D, et al. Gemcitabine plus bevacizumab compared with gemcitabine plus placebo in patients with advanced pancreatic cancer: phase III trial of the Cancer and Leukemia Group B (CALGB 80303). J Clin Oncol. 2010;28(22):3617-3622.
14. Conroy T, Desseigne F, Ychou M. Groupe Tumeurs Digestives of Unicancer; PRODIGE Intergroup. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364(19):1817-1825.
15. Von Hoff DD, Ervin T, Arena FP, et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369(18):1691-1703.
16. Hurwitz H, Uppal N, Wagner SA, et al. A randomized double-blind phase 2 study of ruxolitinib (RUX) or placebo (PBO) with capecitabine (CAPE) as second-line therapy in patients (pts) with metastatic pancreatic cancer (mPC). Abstract 4000. J Clin Oncol. 2014;32(suppl):5s.
17. Provenzano PP, Cuevas C, Chang AE, Goel VK, Von Hoff DD, Hingorani SR. Enzymatic targeting of the stroma ablates physical barriers to treatment of pancreatic ductal adenocarcinoma. Cancer Cell. 2012;21(3):418-429.
18. Le DT, Lutz E, Uram JN, et al. Evaluation of ipilimumab in combination with allogeneic pancreatic tumor cells transfected with a GM-CSF gene in previously treated pancreatic cancer. J Immunother. 2013;36(7):382-389.
19. Plate JM. Advances in therapeutic vaccines for pancreatic cancer. Discov Med. 2012;14(75):89-94.
20. Sharaiha RZ, Widmer J, Kahaleh M. Palliation of pancreatic ductal obstruction in pancreatic cancer. Gastrointest Endosc Clin N Am. 2013;23(4):917-923.
21. Bapat AA, Hostetter G, Von Hoff DD, Han H. Perineural invasion and associated pain in pancreatic cancer. Nat Rev Cancer. 2011;11(10):695-707.
22. Erdek MA, King LM, Ellsworth SG. Pain management and palliative care in pancreatic cancer. Curr Probl Cancer. 2013;37(5):266-272.
1. Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014;64(1):9-29.
2. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63(1):11-30.
3. Solomon S, Das S, Brand R, Whitcomb DC. Inherited pancreatic cancer syndromes. Cancer J. 2012;18(6):485-491.
4. Samanic C, Gridley G, Chow WH, Lubin J, Hoover RN, Fraumeni JF Jr. Obesity and cancer risk among white and black United States veterans. Cancer Causes Control. 2004;15(1):35-43.
5. El-Serag HB, Engels EA, Landgren O, et al. Risk of hepatobiliary and pancreatic cancers after hepatitis C virus infection: A population-based study of U.S. veterans. Hepatology. 2009;49(1):116-123.
6. Atchison EA, Gridley G, Carreon JD, Leitzmann MF, McGlynn KA. Risk of cancer in a large cohort of U.S. veterans with diabetes. Int J Cancer. 2011;128(3):635-643.
7. Landgren O, Turesson I, Gridley G, Caporaso NE. Risk of malignant disease among 1525 adult male US Veterans with Gaucher disease. Arch Intern Med. 2007;167(11):1189-1194.
8. Kang HK, Cypel Y, Kilbourne AM, et al. HealthViEWS: Mortality study of female US Vietnam era veterans, 1965-2010. Am J Epidemiol. 2014;179(6):721-730.
9. Kim K, Zhong F, Chang VT, et al. Clinical characteristics and comorbidity of veterans with pancreatic cancer. J Clin Oncol. 2011;29(15)(suppl):Abstract e14549.
10. National Comprehensive Cancer Network. NCCN Guidelines in the treatment of pancreatic adenocarcinoma. http://www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf. Accessed June 15, 2014.
11. Burris HA III, Moore MJ, Andersen J, et al. Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: A randomized trial. J Clin Oncol. 1997;15(6):2403-2413.
12. Moore MJ, Goldstein D, Hamm J, et al. Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: A phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol. 2007;25(15):1960-1966.
13. Kindler HL, Niedzwiecki D, Hollis D, et al. Gemcitabine plus bevacizumab compared with gemcitabine plus placebo in patients with advanced pancreatic cancer: phase III trial of the Cancer and Leukemia Group B (CALGB 80303). J Clin Oncol. 2010;28(22):3617-3622.
14. Conroy T, Desseigne F, Ychou M. Groupe Tumeurs Digestives of Unicancer; PRODIGE Intergroup. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364(19):1817-1825.
15. Von Hoff DD, Ervin T, Arena FP, et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369(18):1691-1703.
16. Hurwitz H, Uppal N, Wagner SA, et al. A randomized double-blind phase 2 study of ruxolitinib (RUX) or placebo (PBO) with capecitabine (CAPE) as second-line therapy in patients (pts) with metastatic pancreatic cancer (mPC). Abstract 4000. J Clin Oncol. 2014;32(suppl):5s.
17. Provenzano PP, Cuevas C, Chang AE, Goel VK, Von Hoff DD, Hingorani SR. Enzymatic targeting of the stroma ablates physical barriers to treatment of pancreatic ductal adenocarcinoma. Cancer Cell. 2012;21(3):418-429.
18. Le DT, Lutz E, Uram JN, et al. Evaluation of ipilimumab in combination with allogeneic pancreatic tumor cells transfected with a GM-CSF gene in previously treated pancreatic cancer. J Immunother. 2013;36(7):382-389.
19. Plate JM. Advances in therapeutic vaccines for pancreatic cancer. Discov Med. 2012;14(75):89-94.
20. Sharaiha RZ, Widmer J, Kahaleh M. Palliation of pancreatic ductal obstruction in pancreatic cancer. Gastrointest Endosc Clin N Am. 2013;23(4):917-923.
21. Bapat AA, Hostetter G, Von Hoff DD, Han H. Perineural invasion and associated pain in pancreatic cancer. Nat Rev Cancer. 2011;11(10):695-707.
22. Erdek MA, King LM, Ellsworth SG. Pain management and palliative care in pancreatic cancer. Curr Probl Cancer. 2013;37(5):266-272.