User login
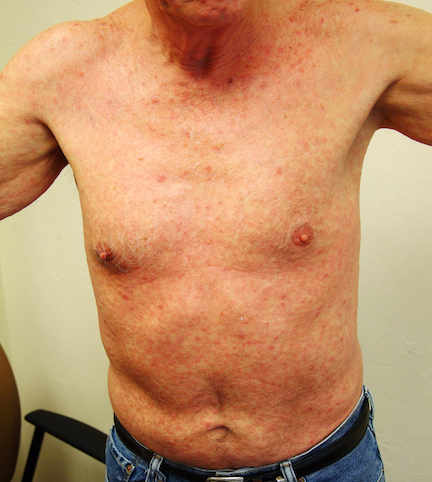
A 52-year-old man is referred to dermatology by his primary care provider for evaluation of an extensive rash. When it first appeared a month ago, the rash was confined to his abdomen. It has subsequently spread—slowly but steadily—to most of his body.
Although it is asymptomatic, the rash is nonetheless of considerable concern to the patient. He denies any history of atopy and has not experienced fever or malaise during the rash’s manifestation. A number of OTC products, including calamine lotion and hydrocortisone 1% cream, have been tried without success.
During history taking, the patient indicates that he is HIV-positive. He was diagnosed more than 10 years ago, and he reports that his disease is well controlled with medication. Homosexually active, he denies having any new contacts.
EXAMINATION
The patient is in no acute distress, although his complexion appears somewhat sallow. The rash is composed of blanchable, erythematous papules and nodules averaging a centimeter in diameter. It is fairly dense, uniformly covering most of his skin but sparing his face and soles. Two 7-mm scaly brown nodules are seen on his right palm. There are no palpable nodes in the usual locations.
Records from his primary care provider are examined. These confirm the patient’s report of his HIV-positive status.
A 4-mm punch biopsy is performed on one of his truncal lesions, with the sample submitted for routine handling.
HISTOPATHOLOGY
Superficial bandlike perivascular infiltrates composed of lymphocytes, macrophages, and plasma cells are noted, along with psoriasiform epidermal hyperplasia and hyperkeratosis. Stains for spirochetes are negative.
DISCUSSION
The differential for generalized red rashes is prodigious and includes granuloma annulare, lichen planus, lupus, and pityriasis rosea, just to name a few. However, this case presents a fairly typical clinical picture of secondary syphilis—a diagnosis that requires confirmation with syphilis serology: rapid plasma reagin (RPR) or Venereal Disease Research Laboratory (VDRL) testing. The latter measures antibodies to the lipids formed by the host against lipids formed on the treponemal cell surface.
In this case, the diagnosis had to be confirmed by more specific treponemal tests, usually conducted by the local health department, to which positive results must be reported. If further testing confirms the diagnosis (as expected), the patient will be treated by the health department. Investigators will question him, attempting to determine the source of the infection and thereby quell an outbreak.
Primary syphilis usually involves development of the characteristic asymptomatic ulcer with rolled edges, called a chancre, on the genitals, lips, or other area. This lesion is often overlooked or (as is often the case) no history of it can be obtained. Four to 10 weeks later, if left untreated, secondary syphilis develops, manifesting with the variable appearance of lesions on the palms and soles, generalized lymphadenopathy, patchy alopecia (termed a “moth-eaten” look), and generalized rash.
Left undiagnosed and treated, secondary syphilis can progress, over several years, to tertiary syphilis, which can manifest in a number of ways (eg, involvement of the heart or nervous system). It may play a role in the formation of “gummatous” lesions, foci of necrotic tissue that can develop in internal organs or in the mouth, where “punched out” defects can manifest.
The causative organism of syphilis is Treponema pallidum, a spirochete usually transmitted directly from the infected individual through breaks in genital or oral tissues. Though it is usually sexually transmitted, syphilis can be acquired congenitally, through direct contact with open lesions, or through exposure to blood products. Since T pallidum only lives for a very short time away from the body, acquiring it from exposure to fomites (eg, toilet seats or door knobs) is virtually impossible.
Huge spikes in rates of this infection occur periodically in the United States. For example, approximately one-tenth of all military draftees in WW1 tested positive for syphilis, a figure that so alarmed public health officials that it lead to the origins of the monitoring of syphilis by governmental agencies. Another spike was noted during WW2, reaching a rate of 66 cases per 100,000 population in 1947. But with the end of warfare and the introduction of penicillin, the rate fell rapidly and today stands at about 4 cases per 100,000 population, 80% of which occur in the South.
There is a high correlation between a history of men having sex with men (MSM) and infection with syphilis, with 64% of new cases currently coming from those ranks. As might be expected, the correlation between syphilis and HIV-positive status is high. The male to female ratio is approximately 6:1.
TREATMENT
Although this man’s treatment is pending as of this writing, he is likely to receive a single dose of benzathine penicillin G (2.4 million units given IM). Penicillin is so much more effective than alternative treatments that it is strongly recommended even when the patient is allergic to it. (In those cases, desensitization is advised if the allergy is confirmed.) Other treatment options include ceftriaxone and doxycycline.
TAKE-HOME LEARNING POINTS
• Secondary syphilis can present with a generalized rash, the appearance of which can vary greatly from one case to another.
• Persistent, unexplained generalized rashes require biopsy to attempt to explain their origin.
• The presence of plasma cells predominating in the inflammatory infiltrate of a rash is highly suggestive of secondary syphilis.
• Indiscriminate and unprotected sex, particularly among men who have sex with men, correlates with risk for a number of conditions, including syphilis and HIV; this information must be sought in the history-taking process.
• Secondary syphilis must be reported to the local health department for investigation and definitive treatment.
A 52-year-old man is referred to dermatology by his primary care provider for evaluation of an extensive rash. When it first appeared a month ago, the rash was confined to his abdomen. It has subsequently spread—slowly but steadily—to most of his body.
Although it is asymptomatic, the rash is nonetheless of considerable concern to the patient. He denies any history of atopy and has not experienced fever or malaise during the rash’s manifestation. A number of OTC products, including calamine lotion and hydrocortisone 1% cream, have been tried without success.
During history taking, the patient indicates that he is HIV-positive. He was diagnosed more than 10 years ago, and he reports that his disease is well controlled with medication. Homosexually active, he denies having any new contacts.
EXAMINATION
The patient is in no acute distress, although his complexion appears somewhat sallow. The rash is composed of blanchable, erythematous papules and nodules averaging a centimeter in diameter. It is fairly dense, uniformly covering most of his skin but sparing his face and soles. Two 7-mm scaly brown nodules are seen on his right palm. There are no palpable nodes in the usual locations.
Records from his primary care provider are examined. These confirm the patient’s report of his HIV-positive status.
A 4-mm punch biopsy is performed on one of his truncal lesions, with the sample submitted for routine handling.
HISTOPATHOLOGY
Superficial bandlike perivascular infiltrates composed of lymphocytes, macrophages, and plasma cells are noted, along with psoriasiform epidermal hyperplasia and hyperkeratosis. Stains for spirochetes are negative.
DISCUSSION
The differential for generalized red rashes is prodigious and includes granuloma annulare, lichen planus, lupus, and pityriasis rosea, just to name a few. However, this case presents a fairly typical clinical picture of secondary syphilis—a diagnosis that requires confirmation with syphilis serology: rapid plasma reagin (RPR) or Venereal Disease Research Laboratory (VDRL) testing. The latter measures antibodies to the lipids formed by the host against lipids formed on the treponemal cell surface.
In this case, the diagnosis had to be confirmed by more specific treponemal tests, usually conducted by the local health department, to which positive results must be reported. If further testing confirms the diagnosis (as expected), the patient will be treated by the health department. Investigators will question him, attempting to determine the source of the infection and thereby quell an outbreak.
Primary syphilis usually involves development of the characteristic asymptomatic ulcer with rolled edges, called a chancre, on the genitals, lips, or other area. This lesion is often overlooked or (as is often the case) no history of it can be obtained. Four to 10 weeks later, if left untreated, secondary syphilis develops, manifesting with the variable appearance of lesions on the palms and soles, generalized lymphadenopathy, patchy alopecia (termed a “moth-eaten” look), and generalized rash.
Left undiagnosed and treated, secondary syphilis can progress, over several years, to tertiary syphilis, which can manifest in a number of ways (eg, involvement of the heart or nervous system). It may play a role in the formation of “gummatous” lesions, foci of necrotic tissue that can develop in internal organs or in the mouth, where “punched out” defects can manifest.
The causative organism of syphilis is Treponema pallidum, a spirochete usually transmitted directly from the infected individual through breaks in genital or oral tissues. Though it is usually sexually transmitted, syphilis can be acquired congenitally, through direct contact with open lesions, or through exposure to blood products. Since T pallidum only lives for a very short time away from the body, acquiring it from exposure to fomites (eg, toilet seats or door knobs) is virtually impossible.
Huge spikes in rates of this infection occur periodically in the United States. For example, approximately one-tenth of all military draftees in WW1 tested positive for syphilis, a figure that so alarmed public health officials that it lead to the origins of the monitoring of syphilis by governmental agencies. Another spike was noted during WW2, reaching a rate of 66 cases per 100,000 population in 1947. But with the end of warfare and the introduction of penicillin, the rate fell rapidly and today stands at about 4 cases per 100,000 population, 80% of which occur in the South.
There is a high correlation between a history of men having sex with men (MSM) and infection with syphilis, with 64% of new cases currently coming from those ranks. As might be expected, the correlation between syphilis and HIV-positive status is high. The male to female ratio is approximately 6:1.
TREATMENT
Although this man’s treatment is pending as of this writing, he is likely to receive a single dose of benzathine penicillin G (2.4 million units given IM). Penicillin is so much more effective than alternative treatments that it is strongly recommended even when the patient is allergic to it. (In those cases, desensitization is advised if the allergy is confirmed.) Other treatment options include ceftriaxone and doxycycline.
TAKE-HOME LEARNING POINTS
• Secondary syphilis can present with a generalized rash, the appearance of which can vary greatly from one case to another.
• Persistent, unexplained generalized rashes require biopsy to attempt to explain their origin.
• The presence of plasma cells predominating in the inflammatory infiltrate of a rash is highly suggestive of secondary syphilis.
• Indiscriminate and unprotected sex, particularly among men who have sex with men, correlates with risk for a number of conditions, including syphilis and HIV; this information must be sought in the history-taking process.
• Secondary syphilis must be reported to the local health department for investigation and definitive treatment.
A 52-year-old man is referred to dermatology by his primary care provider for evaluation of an extensive rash. When it first appeared a month ago, the rash was confined to his abdomen. It has subsequently spread—slowly but steadily—to most of his body.
Although it is asymptomatic, the rash is nonetheless of considerable concern to the patient. He denies any history of atopy and has not experienced fever or malaise during the rash’s manifestation. A number of OTC products, including calamine lotion and hydrocortisone 1% cream, have been tried without success.
During history taking, the patient indicates that he is HIV-positive. He was diagnosed more than 10 years ago, and he reports that his disease is well controlled with medication. Homosexually active, he denies having any new contacts.
EXAMINATION
The patient is in no acute distress, although his complexion appears somewhat sallow. The rash is composed of blanchable, erythematous papules and nodules averaging a centimeter in diameter. It is fairly dense, uniformly covering most of his skin but sparing his face and soles. Two 7-mm scaly brown nodules are seen on his right palm. There are no palpable nodes in the usual locations.
Records from his primary care provider are examined. These confirm the patient’s report of his HIV-positive status.
A 4-mm punch biopsy is performed on one of his truncal lesions, with the sample submitted for routine handling.
HISTOPATHOLOGY
Superficial bandlike perivascular infiltrates composed of lymphocytes, macrophages, and plasma cells are noted, along with psoriasiform epidermal hyperplasia and hyperkeratosis. Stains for spirochetes are negative.
DISCUSSION
The differential for generalized red rashes is prodigious and includes granuloma annulare, lichen planus, lupus, and pityriasis rosea, just to name a few. However, this case presents a fairly typical clinical picture of secondary syphilis—a diagnosis that requires confirmation with syphilis serology: rapid plasma reagin (RPR) or Venereal Disease Research Laboratory (VDRL) testing. The latter measures antibodies to the lipids formed by the host against lipids formed on the treponemal cell surface.
In this case, the diagnosis had to be confirmed by more specific treponemal tests, usually conducted by the local health department, to which positive results must be reported. If further testing confirms the diagnosis (as expected), the patient will be treated by the health department. Investigators will question him, attempting to determine the source of the infection and thereby quell an outbreak.
Primary syphilis usually involves development of the characteristic asymptomatic ulcer with rolled edges, called a chancre, on the genitals, lips, or other area. This lesion is often overlooked or (as is often the case) no history of it can be obtained. Four to 10 weeks later, if left untreated, secondary syphilis develops, manifesting with the variable appearance of lesions on the palms and soles, generalized lymphadenopathy, patchy alopecia (termed a “moth-eaten” look), and generalized rash.
Left undiagnosed and treated, secondary syphilis can progress, over several years, to tertiary syphilis, which can manifest in a number of ways (eg, involvement of the heart or nervous system). It may play a role in the formation of “gummatous” lesions, foci of necrotic tissue that can develop in internal organs or in the mouth, where “punched out” defects can manifest.
The causative organism of syphilis is Treponema pallidum, a spirochete usually transmitted directly from the infected individual through breaks in genital or oral tissues. Though it is usually sexually transmitted, syphilis can be acquired congenitally, through direct contact with open lesions, or through exposure to blood products. Since T pallidum only lives for a very short time away from the body, acquiring it from exposure to fomites (eg, toilet seats or door knobs) is virtually impossible.
Huge spikes in rates of this infection occur periodically in the United States. For example, approximately one-tenth of all military draftees in WW1 tested positive for syphilis, a figure that so alarmed public health officials that it lead to the origins of the monitoring of syphilis by governmental agencies. Another spike was noted during WW2, reaching a rate of 66 cases per 100,000 population in 1947. But with the end of warfare and the introduction of penicillin, the rate fell rapidly and today stands at about 4 cases per 100,000 population, 80% of which occur in the South.
There is a high correlation between a history of men having sex with men (MSM) and infection with syphilis, with 64% of new cases currently coming from those ranks. As might be expected, the correlation between syphilis and HIV-positive status is high. The male to female ratio is approximately 6:1.
TREATMENT
Although this man’s treatment is pending as of this writing, he is likely to receive a single dose of benzathine penicillin G (2.4 million units given IM). Penicillin is so much more effective than alternative treatments that it is strongly recommended even when the patient is allergic to it. (In those cases, desensitization is advised if the allergy is confirmed.) Other treatment options include ceftriaxone and doxycycline.
TAKE-HOME LEARNING POINTS
• Secondary syphilis can present with a generalized rash, the appearance of which can vary greatly from one case to another.
• Persistent, unexplained generalized rashes require biopsy to attempt to explain their origin.
• The presence of plasma cells predominating in the inflammatory infiltrate of a rash is highly suggestive of secondary syphilis.
• Indiscriminate and unprotected sex, particularly among men who have sex with men, correlates with risk for a number of conditions, including syphilis and HIV; this information must be sought in the history-taking process.
• Secondary syphilis must be reported to the local health department for investigation and definitive treatment.