User login
Dr. Adamson reports that he receives research grants from LabCorp and Auxogyn, and is the founder and CEO of Advanced Reproductive Care. Dr. Abusief reports no financial relationships relevant to this article.
The field of reproductive endocrinology has advanced at warp speed over the past few decades—and shows no sign of stopping any time soon. In this article, we outline noteworthy developments of the past year:
- publication of two important Committee Opinions from the American Society for Reproductive Medicine (ASRM)—one of them on the need to reduce the rate of multiple gestation among women undergoing treatment for infertility and the other focusing on a method of achieving this goal: elective single embryo transfer
- two studies of vitrification for cryopreservation of embryos and oocytes
- a trio of investigations into the utility of anti-Müllerian hormone as a means of assessing ovarian reserve and reproductive potential.
Goal of non-ART infertility therapy should be to produce a single child
Practice Committee of the American Society for Reproductive Medicine. Multiple gestation associated with infertility therapy: an American Society for Reproductive Medicine Practice Committee opinion [published online ahead of print December 20, 2011]. Fertil Steril. doi:10.1016/j.fertnstert.2011.11.048.
The goal of infertility treatment is for each patient to have one healthy child at a time, according to a new Practice Committee Opinion from the American Society for Reproductive Medicine (ASRM).
In women who experience oligo-ovulation or anovulation, ovulation induction is typically offered. For ovulatory women who have unexplained or age-related infertility, the treatment often is controlled ovarian stimulation. Either intervention can lead to ovulation from multiple follicles and, ultimately, increase the risk of multiple gestation.
Multiple gestation increases maternal morbidity and both fetal and neonatal morbidity and mortality. Most of the poor perinatal outcomes relate directly to preterm birth. Treatment of women who have infertility, therefore, requires achieving a balance between two competing needs:
- maximizing the probability of pregnancy
- minimizing the risk of multiple (two fetuses or more) or high-order multiple (more than two fetuses) gestation.
Many multiple births are iatrogenic
Approximately 60% of twin births result from natural conception, 30% from ovulation induction and controlled ovarian stimulation, and 10% from assisted reproductive technologies (ART). For high-order multiple gestation, the figures are 20% for natural conception, 50% for ovulation induction and controlled ovarian stimulation, and 30% for ART. These statistics reveal that a very large percentage of multiple births are iatrogenic, with fertility treatment increasing the risk of twins by a factor of approximately 20 and the risk of high-order multiples by a factor of more than 100. The risk of monozygotic twinning also increases by a factor of 2 or 3 after ovulation induction, compared with natural conception.
Triplets should be a rarity
Three-dimensional sonogram of triplets.
Multiple gestation is expensive
The economic costs associated with excess perinatal and maternal morbidity are substantial. They include the immediate costs associated with maternal hospitalization and neonatal intensive care and lifetime costs associated with care for chronic illness, rehabilitation, and special education. Although these costs might be offset by the productivity of individuals, the overall benefit to society is clearly greater when a singleton is born. Personal and familial nonfinancial costs of morbidity and mortality can also be significant.
A sense of urgency on the part of the patient may contribute to an increased risk of multiple gestation by prompting more aggressive treatment. Other contributors include limited health coverage, which creates a personal financial burden, and inadequate patient education about the risks of multiple gestation.
Strategies for limiting the risk of multiple gestation
Appropriate treatment goals are the foundation of risk-reducing strategies. For example, ovulation induction in women who have oligo-ovulation or anovulation should aim toward producing a single oocyte. These women tend to respond to lower dosages of ovarian-stimulation drugs than are typically given. Therefore, women undergoing ovulation induction should receive a lower dosage of gonadotropins and be monitored very carefully for the number of developing follicles and ovarian hyperstimulation syndrome.
In contrast, the goal of controlled ovarian stimulation in ovulatory women who have unexplained or age-related subfertility is to stimulate the development and ovulation of more than one mature follicle to increase cycle fecundity.
Regrettably, efforts have failed to identify estradiol levels and the specific size and number of follicles that prevent multiple gestation. The most likely reason is that follicular size cannot accurately predict the maturity of the oocyte within—follicles as small as 10 mm sometimes yield mature and fertilizable oocytes. Moreover, the population that undergoes ovulation induction or controlled ovarian stimulation is very heterogenous. Therefore, it is not possible to propose valid guidelines to reduce the rate of multiple gestation.
Nevertheless, multiple gestation is sufficiently problematic that we recommend some strategies to reduce its incidence:
- Use low-dosage gonadotropin stimulation with careful monitoring, and limit the number of follicles that are roughly 15 mm or larger to two in patients 37 years of age or younger; three in patient 38 to 40 years old; and more in patients older than 40
- Develop specific cancellation criteria, which should be explained to and accepted by patients undergoing controlled ovarian stimulation. Gonadotropin-releasing hormone (GnRH) antagonists may be of benefit.1
- When clomiphene citrate stimulates the development of two or more mature follicles, outcomes do not differ from those obtained with controlled ovarian stimulation using gonadotropins and intrauterine insemination (IUI).2 Therefore, a reasonable strategy in many patients is to consider initiating treatment with clomiphene citrate and IUI and to proceed directly to in vitro fertilization (IVF) when treatment fails, thereby avoiding controlled ovarian stimulation altogether.3
- Pre-ovulatory ultrasonography-guided aspiration of excess follicles to reduce the risk of multiple gestation has potential benefit but needs further study.
Overall, regardless of the medication or regimen employed, it may not be possible to entirely eliminate the risk of multiple gestation associated with ovulation induction or controlled ovarian stimulation.
When to consider gestation reduction
High-order multifetal gestation reduction has been utilized as a strategy to reduce complications associated with ovulation induction and controlled ovarian stimulation, but use of this technology must be regarded as an adverse outcome of infertility treatment. Overall, data suggest that multifetal gestation reduction is associated with a reduced risk of prematurity, although its true benefit is difficult to elucidate due to potential bias in the interpretation of data. A small percentage of patients lose the entire pregnancy, and the procedure can present patients with a profound ethical dilemma and psychological trauma. Thorough counseling is imperative.
Despite feelings of loss and guilt that persist for a year or longer, most patients report that they would make the decision to undergo gestation reduction again if a similar situation arose in the future.4
The procedure should be performed only in a specialized center by an experienced practitioner.
When performing ovulation induction and controlled ovarian stimulation, use the lowest dose of drug necessary to obtain a single mature follicle in anovulatory women, two follicles in young ovulatory women, and three follicles in women 38 to 40 years old. Because of the high risk of multiple gestation associated with controlled ovarian stimulation followed by IUI, consider moving directly to IVF after use of clomiphene citrate and IUI.
Practice Committee of the Society for Assisted Reproductive Technology and Practice Committee of the American Society for Reproductive Medicine. Elective single-embryo transfer [published online ahead of print December 22, 2011]. Fertil Steril. doi:10.1016/j.fertnstert.2011.11.050.
As IVF implantation rates have improved, the practice of transferring multiple embryos has resulted in a much-increased pregnancy rate but also a high percentage of multiple gestations. Elective single embryo transfer (eSET) has been advocated as the only effective means to avoid multiple pregnancy in IVF cycles, but there is significant concern that it might ultimately reduce the pregnancy rate.
ASRM recently published a Practice Committee Opinion that offers guidance for patient selection and describes barriers to eSET. Patient selection is critical.
Utilization of eSET in the United States has increased over the past decade but still lags behind other countries. Use of double embryo transfer (DET) has increased, significantly reducing the likelihood of high-order multiple pregnancies associated with ART but producing no change in the twin pregnancy rate (FIGURE). Randomized, controlled trials and other studies have demonstrated that the cumulative pregnancy rate per retrieval is no different for eSET followed by frozen embryo transfer than it is for DET in properly selected patients.
Most transfers involve two embryos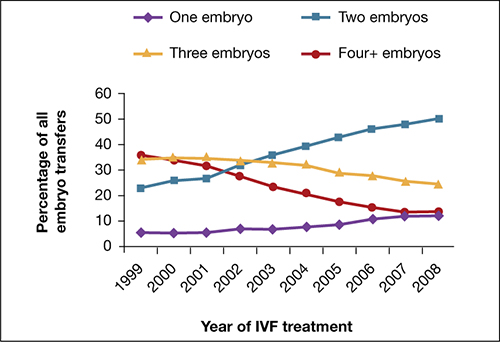
Percentage of transfer of one, two, three, or four or more embryos among all in vitro fertilization cycles performed in the United States, 1999–2008.
SOURCE: ASRM. Reproduced with permission.eSET is most appropriate for women who have a good prognosis:
- age younger than 35 years
- >1 top-quality embryo available for transfer
- first or second treatment cycle
- prior successful IVF
- recipients of embryos from donated eggs.
Women 35 to 40 years old can be considered for eSET if they have top-quality, blastocyst-stage embryos available for transfer.
Barriers to eSET include a lack of provider and patient education about it, financial considerations, embryo selection, and successful cryopreservation. When insurance coverage or refund guarantees are available, patient acceptance of eSET increases.
Elective single embryo transfer is the only ART embryo transfer strategy that will reduce the twin pregnancy rate. However, it is not a good approach for all patients and must be carefully utilized in selected patients who have a good prognosis.
Vitrification for cryopreservation of embryos appears to be superior to slow freezing
Leibo S, Pool T. The principal variables of cryopreservation: solutions, temperatures, and rate changes. Fertil Steril. 2011;96(2):269–276.
Cobo A, Diaz C. Clinical application of oocyte vitrification: a systematic review and meta-analysis of randomized controlled trials. Fertil Steril. 2011;96(2):277–285.
Cryopreservation is a method by which cells are suspended in a solution of salts and low-molecular-weight organic compound, cooled to subzero temperatures (approximately –196°C) in liquid nitrogen, stored, and then rewarmed. Cryopreservation has become a major component of the practice of assisted reproduction, with more than 37,000 pregnancies produced from cryopreserved embryos from 2005 through 2009 in the United States alone.5,6
Standard (slow) freezing methods for embryo cryopreservation involve suspension of the embryos in a 10% solution of propylene glycol supplemented with 3.4% sucrose, cooling them to –35°C at a rate of 0.3°C/min, submerging them in liquid nitrogen for storage, and rewarming the frozen embryos at a rate of approximately 300°C/min to thaw them.5
A major advance in the science of cryopreservation is the use of vitrification, a method of freezing in which the embryos are equilibrated with a 10% or 15% solution of cryoprotectant and then exposed briefly (30–60 seconds) to a 20% to 40% solution of cryoprotectant to achieve relative cellular dehydration. The embryos are then placed in a storage container and submerged in liquid nitrogen. During vitrification, embryos can be cooled at a rate exceeding 1,000°C/min. Vitrified embryos are stored at approximately –196°C and thawed in ultra-rapid fashion.
The development of vitrification methods has significantly advanced the technology of oocyte cryopreservation, which has been utilized for:
- preservation of fertility in cancer patients
- social reasons (e.g., lack of a partner)
- egg-donation programs
- minimization of the risk of ovarian hyperstimulation syndrome
- storage of surplus eggs when embryo cryopreservation is not feasible.
Cobo and Diaz recently conducted a systematic review and meta-analysis of randomized, controlled trials of oocyte vitrification. They found that the potential for fertilization, embryogenesis, and pregnancy from oocytes that had undergone vitrification and warming was not significantly different from the potential for fresh oocytes and was better than the potential for oocytes that had undergone freezing and thawing from standard freezing cycles.
Although the findings of the meta-analysis were limited by the small number of studies and possible selection bias, an increasing body of evidence supports the use of vitrification for cryopreservation of oocytes. Large-scale controlled trials are needed. Until they are performed, the findings of the meta-analysis should be interpreted with caution.
Newer ultra-rapid freezing of oocytes and embryos using vitrification appears to produce results that are superior to those obtained with traditional slow freezing. Large randomized, controlled trials are needed to confirm the improved efficacy of vitrification.
Anti-Müllerian hormone is an informative test of ovarian reserve—but lacks a nod from the FDA
Buyuk E, Seifer D, Younger J, Grazi R, Lieman H. Random anti-Mullerian hormone (AMH) is a predictor of ovarian response in women with elevated baseline early follicular follicle-stimulating hormone levels. Fertil Steril. 2011;95(7):2369–2372.
Li H, Yeung PW, Lau E, Ho PC, Ng EH. Evaluating the performance of serum anti-Müllerian hormone concentration in predicting the live birth rate of controlled ovarian stimulation and intrauterine insemination. Fertil Steril. 2010;94(6):2177–2181.
Lee J, Kim S, Jee B, Suh C, Kim KC, Moon SY. Anti-Müllerian hormone as a predictor of controlled ovarian hyperstimulation outcome: comparison of two commercial immunoassay kits. Fertil Steril. 2011;95(8):2602–2604.
Although it is well understood that both the quantity and quality of oocytes decline with age, the assessment of ovarian reserve continues to be a clinical challenge. Accurate evaluation can predict a woman’s response to infertility treatment, including IVF, and estimate her chance of conception. Noninvasive tests of ovarian reserve are a critical component of any evaluation of fertility. Although a woman’s age is the single most important historical factor in the assessment of reproductive capacity, there is significant variation in ovarian aging among women.
Historically, age, antral follicle count (AFC), and measurement of cycle day 3 follicle-stimulating hormone (FSH) and estradiol (E2) levels have been the most widely used measures of ovarian reserve, but mounting evidence suggests that assessment of the anti-Müllerian hormone (AMH) level may be even more informative.
AMH, also known as Müllerian-inhibiting substance, is a dimeric glycoprotein. A member of the transforming growth factor–ß family, AMH is closely related to inhibin and activin and is secreted by granulosa cells of preantral and small antral follicles in post-pubertal females.7 AMH aids in the coordination of ovarian follicular development by inhibiting recruitment of additional primordial follicles and decreasing the sensitivity of preantral and small antral follicles to FSH.8,9
AMH levels, measurable in serum, decline with age and are undetectable after menopause.10 Unlike FSH, which fluctuates during the menstrual cycle, AMH exhibits minimal intercycle and intracycle variation. The AMH level remains stable in women taking oral contraceptives and even in women who are pregnant.11
AMH is independently and significantly correlated with the ovarian response to gonadotropin therapy, with decreased levels of AMH associated with a poor response, and increased levels associated with a strong response.12 In the first cycle of IVF, an elevated AMH level has been associated with excessive response to gonadotropins and an increased risk of ovarian hyperstimulation syndrome (OHSS), independent of age and the presence of polycystic ovary syndrome.12
In a recent study of women who had an elevated FSH level and were undergoing IVF, the AMH level was strongly associated with the number of oocytes retrieved.13 Women who had an elevated FSH level but a serum AMH level of 0.6 ng/mL or above had a greater number of oocytes and day-3 embryos retrieved; they also had a lower cancellation rate than women who had a lower AMH level.13
Although no single test can predict the outcome of treatment for infertility, AMH concentrations are significantly higher in women who have a live birth (from the first cycle of stimulated IUI or after three cycles) than in women who do not.14
Two ELISA kits, one value?
Two types of enzyme-linked immunosorbent assay (ELISA) kits are commercially available for measurement of the AMH level: one from Immunotech Beckman Coulter and the other from Diagnostic Systems Laboratories. Neither kit has been approved for clinical use by the US Food and Drug Administration.
Studies comparing the values obtained using each kit have been inconsistent, generating controversy about the measurement of AMH. A recent study of women who were undergoing controlled ovarian stimulation found that the AMH levels obtained by the two kits were similar and significantly correlated with each other.15 In that study, the AMH level was measured on the day before gonadotropin administration or on the day of oocyte retrieval.15 In addition, the AMH concentrations measured by both kits were significantly associated with age, basal FSH levels, AFC, and the outcome of controlled ovarian stimulation.15 The authors concluded:
- The two commercially available kits provide reliable and similar results.
- The AMH level measured by either kit can predict the outcome of controlled ovarian stimulation, with similar reference values.15
Measurement of the AMH level can be an informative aspect of the evaluation of a patient’s fertility, as well as a valuable tool in the assessment of ovarian reserve. The AMH level can also help clinicians identify the appropriate dose of gonadotropins and predict which patients might be likely to over- or under-respond to stimulation—ultimately reducing the length and cost of treatment. Knowledge of the patient’s AMH level might inform pretreatment counseling and help women achieve reasonable expectations.
AMH is a useful test to help predict a patient’s response to ovarian stimulation and her chances of achieving pregnancy. However, AMH is only one measure of ovarian reserve and should not be used alone as a reason to exclude patients from treatment. In our practice, we use the AMH level along with cycle day 3 antral follicle count and FSH and estradiol levels.
We want to hear from you! Tell us what you think.
1. Ragni G, Caliari I, Nicolosi AE, Arnoldi M, Somigliana E, Crosignani PG. Preventing high-order multiple pregnancies during controlled ovarian hyperstimulation and intrauterine insemination: 3 years’ experience using low-dose recombinant follicle-stimulating hormone and gonadotropin-releasing hormone antagonists. Fertil Steril. 2006;85(3):619-624.
2. Ghesquiere SL, Castelain EG, Spiessens C, et al. Relationship between follicle number and (multiple) live birth rate after controlled ovarian hyperstimulation and intrauterine insemination. Am J Obstet Gynecol. 2007;197(6):589.e1-5.
3. Reindollar RH, Regan MM, Neumann PJ, et al. A randomized clinical trial to evaluate optimal treatment for unexplained infertility: the fast track and standard treatment (FASTT) trial. Fertil Steril. 2010;94(3):888-899.
4. Schreiner-Engel P, Walther VN, Mindes J, et al. First-trimester multifetal pregnancy reduction: acute and persistent psychologic reactions. Am J Obstet Gynecol. 1995;172(2 Pt 1):541.-
5. Leibo S, Pool T. The principal variables of cryopreservation: solutions temperatures, and rate changes. Fertil Steril. 2011;96(2):269-276.
6. Society for Assisted Reproductive Technology; American Society for Reproductive Medicine. Assisted reproductive technology in the United States: 2001 results generated from the American Society for Reproductive Medicine/Society for Assisted Reproductive Technology registry. Fertil Steril. 2007;87(6):1253-1266.
7. Vigier JA, Picard JY, Tran D, Legeai L, Josso N. Production of anti-Müllerian hormone: another homology between Sertoli and granulosa cells. Endocrinology. 1984;114(4):1315-1320.
8. Durlinger All, Gruijters MJG, Kramer P, et al. Anti-Müllerian hormone attenuates the effects of FSH on follicle development in the mouse ovary. Endocrinology. 2001;142(11):4891-4899.
9. Salmon NA, Handyside AH, Joyce IM. Oocyte regulation and anti-Müllerian hormone expression in granulosa cells during ovarian follicle development in mice. Dev Biol. 2004;266(1):201-208.
10. Shin SY, Lee JR, Noh GW, et al. Analysis of serum levels of anti-Müllerian hormone, inhibin B, insulin-like growth factor-I, insulin-like growth factor binding protein-3, and follicle-stimulating hormone with respect to age and menopausal status. J Korean Med Sci. 2008;23(1):104-110.
11. Streuli I, Fraisse T, Chapron C, Bijaoui G, Bischof P, de Ziegler D. Clinical uses of anti-Müllerian hormone assays: pitfalls and promises. Fertil Steril. 2009;91(1):226-230.
12. Nardo L, Gelbaya T, Wilkinson H, et al. Circulating basal anti-Müllerian hormone levels as predictor of ovarian response in women undergoing ovarian stimulation for in vitro fertilization. Fertil Steril. 2009;92(5):1586-1593.
13. Buyuk E, Seifer D, Younger J, Grazi R, Lieman H. Random anti-Müllerian hormone (AMH) is a predictor of ovarian response in women with elevated baseline early follicular follicle-stimulating hormone levels. Fertil Steril. 2011;95(7):2369-2372.
14. Li HW, Yeung PW, Lau E&, Ho PC, Ng EH. Evaluating the performance of serum anti-Müllerian hormone concentration in predicting the live birth rate of controlled ovarian stimulation and intrauterine insemination. Fertil Steril. 2010;94(6):2177-2181.
15. Lee J, Kim S, Jee B, Suh C, Kim KC, Moon SY. Anti- Müllerian hormone as a predictor of controlled ovarian hyperstimulation outcome: comparison of two commercial immunoassay kits. Fertil Steril. 2011;95(8):2602-2604.
Dr. Adamson reports that he receives research grants from LabCorp and Auxogyn, and is the founder and CEO of Advanced Reproductive Care. Dr. Abusief reports no financial relationships relevant to this article.
The field of reproductive endocrinology has advanced at warp speed over the past few decades—and shows no sign of stopping any time soon. In this article, we outline noteworthy developments of the past year:
- publication of two important Committee Opinions from the American Society for Reproductive Medicine (ASRM)—one of them on the need to reduce the rate of multiple gestation among women undergoing treatment for infertility and the other focusing on a method of achieving this goal: elective single embryo transfer
- two studies of vitrification for cryopreservation of embryos and oocytes
- a trio of investigations into the utility of anti-Müllerian hormone as a means of assessing ovarian reserve and reproductive potential.
Goal of non-ART infertility therapy should be to produce a single child
Practice Committee of the American Society for Reproductive Medicine. Multiple gestation associated with infertility therapy: an American Society for Reproductive Medicine Practice Committee opinion [published online ahead of print December 20, 2011]. Fertil Steril. doi:10.1016/j.fertnstert.2011.11.048.
The goal of infertility treatment is for each patient to have one healthy child at a time, according to a new Practice Committee Opinion from the American Society for Reproductive Medicine (ASRM).
In women who experience oligo-ovulation or anovulation, ovulation induction is typically offered. For ovulatory women who have unexplained or age-related infertility, the treatment often is controlled ovarian stimulation. Either intervention can lead to ovulation from multiple follicles and, ultimately, increase the risk of multiple gestation.
Multiple gestation increases maternal morbidity and both fetal and neonatal morbidity and mortality. Most of the poor perinatal outcomes relate directly to preterm birth. Treatment of women who have infertility, therefore, requires achieving a balance between two competing needs:
- maximizing the probability of pregnancy
- minimizing the risk of multiple (two fetuses or more) or high-order multiple (more than two fetuses) gestation.
Many multiple births are iatrogenic
Approximately 60% of twin births result from natural conception, 30% from ovulation induction and controlled ovarian stimulation, and 10% from assisted reproductive technologies (ART). For high-order multiple gestation, the figures are 20% for natural conception, 50% for ovulation induction and controlled ovarian stimulation, and 30% for ART. These statistics reveal that a very large percentage of multiple births are iatrogenic, with fertility treatment increasing the risk of twins by a factor of approximately 20 and the risk of high-order multiples by a factor of more than 100. The risk of monozygotic twinning also increases by a factor of 2 or 3 after ovulation induction, compared with natural conception.
Triplets should be a rarity
Three-dimensional sonogram of triplets.
Multiple gestation is expensive
The economic costs associated with excess perinatal and maternal morbidity are substantial. They include the immediate costs associated with maternal hospitalization and neonatal intensive care and lifetime costs associated with care for chronic illness, rehabilitation, and special education. Although these costs might be offset by the productivity of individuals, the overall benefit to society is clearly greater when a singleton is born. Personal and familial nonfinancial costs of morbidity and mortality can also be significant.
A sense of urgency on the part of the patient may contribute to an increased risk of multiple gestation by prompting more aggressive treatment. Other contributors include limited health coverage, which creates a personal financial burden, and inadequate patient education about the risks of multiple gestation.
Strategies for limiting the risk of multiple gestation
Appropriate treatment goals are the foundation of risk-reducing strategies. For example, ovulation induction in women who have oligo-ovulation or anovulation should aim toward producing a single oocyte. These women tend to respond to lower dosages of ovarian-stimulation drugs than are typically given. Therefore, women undergoing ovulation induction should receive a lower dosage of gonadotropins and be monitored very carefully for the number of developing follicles and ovarian hyperstimulation syndrome.
In contrast, the goal of controlled ovarian stimulation in ovulatory women who have unexplained or age-related subfertility is to stimulate the development and ovulation of more than one mature follicle to increase cycle fecundity.
Regrettably, efforts have failed to identify estradiol levels and the specific size and number of follicles that prevent multiple gestation. The most likely reason is that follicular size cannot accurately predict the maturity of the oocyte within—follicles as small as 10 mm sometimes yield mature and fertilizable oocytes. Moreover, the population that undergoes ovulation induction or controlled ovarian stimulation is very heterogenous. Therefore, it is not possible to propose valid guidelines to reduce the rate of multiple gestation.
Nevertheless, multiple gestation is sufficiently problematic that we recommend some strategies to reduce its incidence:
- Use low-dosage gonadotropin stimulation with careful monitoring, and limit the number of follicles that are roughly 15 mm or larger to two in patients 37 years of age or younger; three in patient 38 to 40 years old; and more in patients older than 40
- Develop specific cancellation criteria, which should be explained to and accepted by patients undergoing controlled ovarian stimulation. Gonadotropin-releasing hormone (GnRH) antagonists may be of benefit.1
- When clomiphene citrate stimulates the development of two or more mature follicles, outcomes do not differ from those obtained with controlled ovarian stimulation using gonadotropins and intrauterine insemination (IUI).2 Therefore, a reasonable strategy in many patients is to consider initiating treatment with clomiphene citrate and IUI and to proceed directly to in vitro fertilization (IVF) when treatment fails, thereby avoiding controlled ovarian stimulation altogether.3
- Pre-ovulatory ultrasonography-guided aspiration of excess follicles to reduce the risk of multiple gestation has potential benefit but needs further study.
Overall, regardless of the medication or regimen employed, it may not be possible to entirely eliminate the risk of multiple gestation associated with ovulation induction or controlled ovarian stimulation.
When to consider gestation reduction
High-order multifetal gestation reduction has been utilized as a strategy to reduce complications associated with ovulation induction and controlled ovarian stimulation, but use of this technology must be regarded as an adverse outcome of infertility treatment. Overall, data suggest that multifetal gestation reduction is associated with a reduced risk of prematurity, although its true benefit is difficult to elucidate due to potential bias in the interpretation of data. A small percentage of patients lose the entire pregnancy, and the procedure can present patients with a profound ethical dilemma and psychological trauma. Thorough counseling is imperative.
Despite feelings of loss and guilt that persist for a year or longer, most patients report that they would make the decision to undergo gestation reduction again if a similar situation arose in the future.4
The procedure should be performed only in a specialized center by an experienced practitioner.
When performing ovulation induction and controlled ovarian stimulation, use the lowest dose of drug necessary to obtain a single mature follicle in anovulatory women, two follicles in young ovulatory women, and three follicles in women 38 to 40 years old. Because of the high risk of multiple gestation associated with controlled ovarian stimulation followed by IUI, consider moving directly to IVF after use of clomiphene citrate and IUI.
Practice Committee of the Society for Assisted Reproductive Technology and Practice Committee of the American Society for Reproductive Medicine. Elective single-embryo transfer [published online ahead of print December 22, 2011]. Fertil Steril. doi:10.1016/j.fertnstert.2011.11.050.
As IVF implantation rates have improved, the practice of transferring multiple embryos has resulted in a much-increased pregnancy rate but also a high percentage of multiple gestations. Elective single embryo transfer (eSET) has been advocated as the only effective means to avoid multiple pregnancy in IVF cycles, but there is significant concern that it might ultimately reduce the pregnancy rate.
ASRM recently published a Practice Committee Opinion that offers guidance for patient selection and describes barriers to eSET. Patient selection is critical.
Utilization of eSET in the United States has increased over the past decade but still lags behind other countries. Use of double embryo transfer (DET) has increased, significantly reducing the likelihood of high-order multiple pregnancies associated with ART but producing no change in the twin pregnancy rate (FIGURE). Randomized, controlled trials and other studies have demonstrated that the cumulative pregnancy rate per retrieval is no different for eSET followed by frozen embryo transfer than it is for DET in properly selected patients.
Most transfers involve two embryos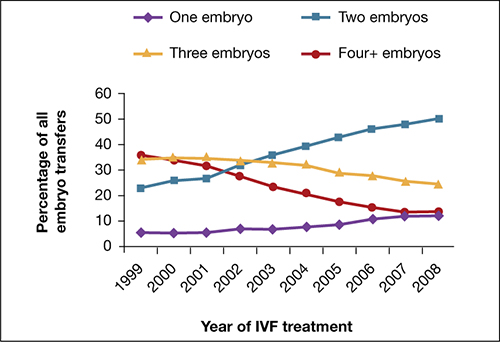
Percentage of transfer of one, two, three, or four or more embryos among all in vitro fertilization cycles performed in the United States, 1999–2008.
SOURCE: ASRM. Reproduced with permission.eSET is most appropriate for women who have a good prognosis:
- age younger than 35 years
- >1 top-quality embryo available for transfer
- first or second treatment cycle
- prior successful IVF
- recipients of embryos from donated eggs.
Women 35 to 40 years old can be considered for eSET if they have top-quality, blastocyst-stage embryos available for transfer.
Barriers to eSET include a lack of provider and patient education about it, financial considerations, embryo selection, and successful cryopreservation. When insurance coverage or refund guarantees are available, patient acceptance of eSET increases.
Elective single embryo transfer is the only ART embryo transfer strategy that will reduce the twin pregnancy rate. However, it is not a good approach for all patients and must be carefully utilized in selected patients who have a good prognosis.
Vitrification for cryopreservation of embryos appears to be superior to slow freezing
Leibo S, Pool T. The principal variables of cryopreservation: solutions, temperatures, and rate changes. Fertil Steril. 2011;96(2):269–276.
Cobo A, Diaz C. Clinical application of oocyte vitrification: a systematic review and meta-analysis of randomized controlled trials. Fertil Steril. 2011;96(2):277–285.
Cryopreservation is a method by which cells are suspended in a solution of salts and low-molecular-weight organic compound, cooled to subzero temperatures (approximately –196°C) in liquid nitrogen, stored, and then rewarmed. Cryopreservation has become a major component of the practice of assisted reproduction, with more than 37,000 pregnancies produced from cryopreserved embryos from 2005 through 2009 in the United States alone.5,6
Standard (slow) freezing methods for embryo cryopreservation involve suspension of the embryos in a 10% solution of propylene glycol supplemented with 3.4% sucrose, cooling them to –35°C at a rate of 0.3°C/min, submerging them in liquid nitrogen for storage, and rewarming the frozen embryos at a rate of approximately 300°C/min to thaw them.5
A major advance in the science of cryopreservation is the use of vitrification, a method of freezing in which the embryos are equilibrated with a 10% or 15% solution of cryoprotectant and then exposed briefly (30–60 seconds) to a 20% to 40% solution of cryoprotectant to achieve relative cellular dehydration. The embryos are then placed in a storage container and submerged in liquid nitrogen. During vitrification, embryos can be cooled at a rate exceeding 1,000°C/min. Vitrified embryos are stored at approximately –196°C and thawed in ultra-rapid fashion.
The development of vitrification methods has significantly advanced the technology of oocyte cryopreservation, which has been utilized for:
- preservation of fertility in cancer patients
- social reasons (e.g., lack of a partner)
- egg-donation programs
- minimization of the risk of ovarian hyperstimulation syndrome
- storage of surplus eggs when embryo cryopreservation is not feasible.
Cobo and Diaz recently conducted a systematic review and meta-analysis of randomized, controlled trials of oocyte vitrification. They found that the potential for fertilization, embryogenesis, and pregnancy from oocytes that had undergone vitrification and warming was not significantly different from the potential for fresh oocytes and was better than the potential for oocytes that had undergone freezing and thawing from standard freezing cycles.
Although the findings of the meta-analysis were limited by the small number of studies and possible selection bias, an increasing body of evidence supports the use of vitrification for cryopreservation of oocytes. Large-scale controlled trials are needed. Until they are performed, the findings of the meta-analysis should be interpreted with caution.
Newer ultra-rapid freezing of oocytes and embryos using vitrification appears to produce results that are superior to those obtained with traditional slow freezing. Large randomized, controlled trials are needed to confirm the improved efficacy of vitrification.
Anti-Müllerian hormone is an informative test of ovarian reserve—but lacks a nod from the FDA
Buyuk E, Seifer D, Younger J, Grazi R, Lieman H. Random anti-Mullerian hormone (AMH) is a predictor of ovarian response in women with elevated baseline early follicular follicle-stimulating hormone levels. Fertil Steril. 2011;95(7):2369–2372.
Li H, Yeung PW, Lau E, Ho PC, Ng EH. Evaluating the performance of serum anti-Müllerian hormone concentration in predicting the live birth rate of controlled ovarian stimulation and intrauterine insemination. Fertil Steril. 2010;94(6):2177–2181.
Lee J, Kim S, Jee B, Suh C, Kim KC, Moon SY. Anti-Müllerian hormone as a predictor of controlled ovarian hyperstimulation outcome: comparison of two commercial immunoassay kits. Fertil Steril. 2011;95(8):2602–2604.
Although it is well understood that both the quantity and quality of oocytes decline with age, the assessment of ovarian reserve continues to be a clinical challenge. Accurate evaluation can predict a woman’s response to infertility treatment, including IVF, and estimate her chance of conception. Noninvasive tests of ovarian reserve are a critical component of any evaluation of fertility. Although a woman’s age is the single most important historical factor in the assessment of reproductive capacity, there is significant variation in ovarian aging among women.
Historically, age, antral follicle count (AFC), and measurement of cycle day 3 follicle-stimulating hormone (FSH) and estradiol (E2) levels have been the most widely used measures of ovarian reserve, but mounting evidence suggests that assessment of the anti-Müllerian hormone (AMH) level may be even more informative.
AMH, also known as Müllerian-inhibiting substance, is a dimeric glycoprotein. A member of the transforming growth factor–ß family, AMH is closely related to inhibin and activin and is secreted by granulosa cells of preantral and small antral follicles in post-pubertal females.7 AMH aids in the coordination of ovarian follicular development by inhibiting recruitment of additional primordial follicles and decreasing the sensitivity of preantral and small antral follicles to FSH.8,9
AMH levels, measurable in serum, decline with age and are undetectable after menopause.10 Unlike FSH, which fluctuates during the menstrual cycle, AMH exhibits minimal intercycle and intracycle variation. The AMH level remains stable in women taking oral contraceptives and even in women who are pregnant.11
AMH is independently and significantly correlated with the ovarian response to gonadotropin therapy, with decreased levels of AMH associated with a poor response, and increased levels associated with a strong response.12 In the first cycle of IVF, an elevated AMH level has been associated with excessive response to gonadotropins and an increased risk of ovarian hyperstimulation syndrome (OHSS), independent of age and the presence of polycystic ovary syndrome.12
In a recent study of women who had an elevated FSH level and were undergoing IVF, the AMH level was strongly associated with the number of oocytes retrieved.13 Women who had an elevated FSH level but a serum AMH level of 0.6 ng/mL or above had a greater number of oocytes and day-3 embryos retrieved; they also had a lower cancellation rate than women who had a lower AMH level.13
Although no single test can predict the outcome of treatment for infertility, AMH concentrations are significantly higher in women who have a live birth (from the first cycle of stimulated IUI or after three cycles) than in women who do not.14
Two ELISA kits, one value?
Two types of enzyme-linked immunosorbent assay (ELISA) kits are commercially available for measurement of the AMH level: one from Immunotech Beckman Coulter and the other from Diagnostic Systems Laboratories. Neither kit has been approved for clinical use by the US Food and Drug Administration.
Studies comparing the values obtained using each kit have been inconsistent, generating controversy about the measurement of AMH. A recent study of women who were undergoing controlled ovarian stimulation found that the AMH levels obtained by the two kits were similar and significantly correlated with each other.15 In that study, the AMH level was measured on the day before gonadotropin administration or on the day of oocyte retrieval.15 In addition, the AMH concentrations measured by both kits were significantly associated with age, basal FSH levels, AFC, and the outcome of controlled ovarian stimulation.15 The authors concluded:
- The two commercially available kits provide reliable and similar results.
- The AMH level measured by either kit can predict the outcome of controlled ovarian stimulation, with similar reference values.15
Measurement of the AMH level can be an informative aspect of the evaluation of a patient’s fertility, as well as a valuable tool in the assessment of ovarian reserve. The AMH level can also help clinicians identify the appropriate dose of gonadotropins and predict which patients might be likely to over- or under-respond to stimulation—ultimately reducing the length and cost of treatment. Knowledge of the patient’s AMH level might inform pretreatment counseling and help women achieve reasonable expectations.
AMH is a useful test to help predict a patient’s response to ovarian stimulation and her chances of achieving pregnancy. However, AMH is only one measure of ovarian reserve and should not be used alone as a reason to exclude patients from treatment. In our practice, we use the AMH level along with cycle day 3 antral follicle count and FSH and estradiol levels.
We want to hear from you! Tell us what you think.
Dr. Adamson reports that he receives research grants from LabCorp and Auxogyn, and is the founder and CEO of Advanced Reproductive Care. Dr. Abusief reports no financial relationships relevant to this article.
The field of reproductive endocrinology has advanced at warp speed over the past few decades—and shows no sign of stopping any time soon. In this article, we outline noteworthy developments of the past year:
- publication of two important Committee Opinions from the American Society for Reproductive Medicine (ASRM)—one of them on the need to reduce the rate of multiple gestation among women undergoing treatment for infertility and the other focusing on a method of achieving this goal: elective single embryo transfer
- two studies of vitrification for cryopreservation of embryos and oocytes
- a trio of investigations into the utility of anti-Müllerian hormone as a means of assessing ovarian reserve and reproductive potential.
Goal of non-ART infertility therapy should be to produce a single child
Practice Committee of the American Society for Reproductive Medicine. Multiple gestation associated with infertility therapy: an American Society for Reproductive Medicine Practice Committee opinion [published online ahead of print December 20, 2011]. Fertil Steril. doi:10.1016/j.fertnstert.2011.11.048.
The goal of infertility treatment is for each patient to have one healthy child at a time, according to a new Practice Committee Opinion from the American Society for Reproductive Medicine (ASRM).
In women who experience oligo-ovulation or anovulation, ovulation induction is typically offered. For ovulatory women who have unexplained or age-related infertility, the treatment often is controlled ovarian stimulation. Either intervention can lead to ovulation from multiple follicles and, ultimately, increase the risk of multiple gestation.
Multiple gestation increases maternal morbidity and both fetal and neonatal morbidity and mortality. Most of the poor perinatal outcomes relate directly to preterm birth. Treatment of women who have infertility, therefore, requires achieving a balance between two competing needs:
- maximizing the probability of pregnancy
- minimizing the risk of multiple (two fetuses or more) or high-order multiple (more than two fetuses) gestation.
Many multiple births are iatrogenic
Approximately 60% of twin births result from natural conception, 30% from ovulation induction and controlled ovarian stimulation, and 10% from assisted reproductive technologies (ART). For high-order multiple gestation, the figures are 20% for natural conception, 50% for ovulation induction and controlled ovarian stimulation, and 30% for ART. These statistics reveal that a very large percentage of multiple births are iatrogenic, with fertility treatment increasing the risk of twins by a factor of approximately 20 and the risk of high-order multiples by a factor of more than 100. The risk of monozygotic twinning also increases by a factor of 2 or 3 after ovulation induction, compared with natural conception.
Triplets should be a rarity
Three-dimensional sonogram of triplets.
Multiple gestation is expensive
The economic costs associated with excess perinatal and maternal morbidity are substantial. They include the immediate costs associated with maternal hospitalization and neonatal intensive care and lifetime costs associated with care for chronic illness, rehabilitation, and special education. Although these costs might be offset by the productivity of individuals, the overall benefit to society is clearly greater when a singleton is born. Personal and familial nonfinancial costs of morbidity and mortality can also be significant.
A sense of urgency on the part of the patient may contribute to an increased risk of multiple gestation by prompting more aggressive treatment. Other contributors include limited health coverage, which creates a personal financial burden, and inadequate patient education about the risks of multiple gestation.
Strategies for limiting the risk of multiple gestation
Appropriate treatment goals are the foundation of risk-reducing strategies. For example, ovulation induction in women who have oligo-ovulation or anovulation should aim toward producing a single oocyte. These women tend to respond to lower dosages of ovarian-stimulation drugs than are typically given. Therefore, women undergoing ovulation induction should receive a lower dosage of gonadotropins and be monitored very carefully for the number of developing follicles and ovarian hyperstimulation syndrome.
In contrast, the goal of controlled ovarian stimulation in ovulatory women who have unexplained or age-related subfertility is to stimulate the development and ovulation of more than one mature follicle to increase cycle fecundity.
Regrettably, efforts have failed to identify estradiol levels and the specific size and number of follicles that prevent multiple gestation. The most likely reason is that follicular size cannot accurately predict the maturity of the oocyte within—follicles as small as 10 mm sometimes yield mature and fertilizable oocytes. Moreover, the population that undergoes ovulation induction or controlled ovarian stimulation is very heterogenous. Therefore, it is not possible to propose valid guidelines to reduce the rate of multiple gestation.
Nevertheless, multiple gestation is sufficiently problematic that we recommend some strategies to reduce its incidence:
- Use low-dosage gonadotropin stimulation with careful monitoring, and limit the number of follicles that are roughly 15 mm or larger to two in patients 37 years of age or younger; three in patient 38 to 40 years old; and more in patients older than 40
- Develop specific cancellation criteria, which should be explained to and accepted by patients undergoing controlled ovarian stimulation. Gonadotropin-releasing hormone (GnRH) antagonists may be of benefit.1
- When clomiphene citrate stimulates the development of two or more mature follicles, outcomes do not differ from those obtained with controlled ovarian stimulation using gonadotropins and intrauterine insemination (IUI).2 Therefore, a reasonable strategy in many patients is to consider initiating treatment with clomiphene citrate and IUI and to proceed directly to in vitro fertilization (IVF) when treatment fails, thereby avoiding controlled ovarian stimulation altogether.3
- Pre-ovulatory ultrasonography-guided aspiration of excess follicles to reduce the risk of multiple gestation has potential benefit but needs further study.
Overall, regardless of the medication or regimen employed, it may not be possible to entirely eliminate the risk of multiple gestation associated with ovulation induction or controlled ovarian stimulation.
When to consider gestation reduction
High-order multifetal gestation reduction has been utilized as a strategy to reduce complications associated with ovulation induction and controlled ovarian stimulation, but use of this technology must be regarded as an adverse outcome of infertility treatment. Overall, data suggest that multifetal gestation reduction is associated with a reduced risk of prematurity, although its true benefit is difficult to elucidate due to potential bias in the interpretation of data. A small percentage of patients lose the entire pregnancy, and the procedure can present patients with a profound ethical dilemma and psychological trauma. Thorough counseling is imperative.
Despite feelings of loss and guilt that persist for a year or longer, most patients report that they would make the decision to undergo gestation reduction again if a similar situation arose in the future.4
The procedure should be performed only in a specialized center by an experienced practitioner.
When performing ovulation induction and controlled ovarian stimulation, use the lowest dose of drug necessary to obtain a single mature follicle in anovulatory women, two follicles in young ovulatory women, and three follicles in women 38 to 40 years old. Because of the high risk of multiple gestation associated with controlled ovarian stimulation followed by IUI, consider moving directly to IVF after use of clomiphene citrate and IUI.
Practice Committee of the Society for Assisted Reproductive Technology and Practice Committee of the American Society for Reproductive Medicine. Elective single-embryo transfer [published online ahead of print December 22, 2011]. Fertil Steril. doi:10.1016/j.fertnstert.2011.11.050.
As IVF implantation rates have improved, the practice of transferring multiple embryos has resulted in a much-increased pregnancy rate but also a high percentage of multiple gestations. Elective single embryo transfer (eSET) has been advocated as the only effective means to avoid multiple pregnancy in IVF cycles, but there is significant concern that it might ultimately reduce the pregnancy rate.
ASRM recently published a Practice Committee Opinion that offers guidance for patient selection and describes barriers to eSET. Patient selection is critical.
Utilization of eSET in the United States has increased over the past decade but still lags behind other countries. Use of double embryo transfer (DET) has increased, significantly reducing the likelihood of high-order multiple pregnancies associated with ART but producing no change in the twin pregnancy rate (FIGURE). Randomized, controlled trials and other studies have demonstrated that the cumulative pregnancy rate per retrieval is no different for eSET followed by frozen embryo transfer than it is for DET in properly selected patients.
Most transfers involve two embryos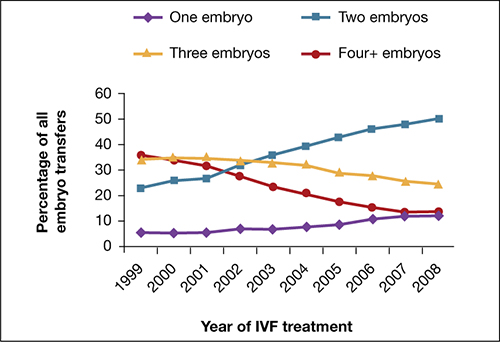
Percentage of transfer of one, two, three, or four or more embryos among all in vitro fertilization cycles performed in the United States, 1999–2008.
SOURCE: ASRM. Reproduced with permission.eSET is most appropriate for women who have a good prognosis:
- age younger than 35 years
- >1 top-quality embryo available for transfer
- first or second treatment cycle
- prior successful IVF
- recipients of embryos from donated eggs.
Women 35 to 40 years old can be considered for eSET if they have top-quality, blastocyst-stage embryos available for transfer.
Barriers to eSET include a lack of provider and patient education about it, financial considerations, embryo selection, and successful cryopreservation. When insurance coverage or refund guarantees are available, patient acceptance of eSET increases.
Elective single embryo transfer is the only ART embryo transfer strategy that will reduce the twin pregnancy rate. However, it is not a good approach for all patients and must be carefully utilized in selected patients who have a good prognosis.
Vitrification for cryopreservation of embryos appears to be superior to slow freezing
Leibo S, Pool T. The principal variables of cryopreservation: solutions, temperatures, and rate changes. Fertil Steril. 2011;96(2):269–276.
Cobo A, Diaz C. Clinical application of oocyte vitrification: a systematic review and meta-analysis of randomized controlled trials. Fertil Steril. 2011;96(2):277–285.
Cryopreservation is a method by which cells are suspended in a solution of salts and low-molecular-weight organic compound, cooled to subzero temperatures (approximately –196°C) in liquid nitrogen, stored, and then rewarmed. Cryopreservation has become a major component of the practice of assisted reproduction, with more than 37,000 pregnancies produced from cryopreserved embryos from 2005 through 2009 in the United States alone.5,6
Standard (slow) freezing methods for embryo cryopreservation involve suspension of the embryos in a 10% solution of propylene glycol supplemented with 3.4% sucrose, cooling them to –35°C at a rate of 0.3°C/min, submerging them in liquid nitrogen for storage, and rewarming the frozen embryos at a rate of approximately 300°C/min to thaw them.5
A major advance in the science of cryopreservation is the use of vitrification, a method of freezing in which the embryos are equilibrated with a 10% or 15% solution of cryoprotectant and then exposed briefly (30–60 seconds) to a 20% to 40% solution of cryoprotectant to achieve relative cellular dehydration. The embryos are then placed in a storage container and submerged in liquid nitrogen. During vitrification, embryos can be cooled at a rate exceeding 1,000°C/min. Vitrified embryos are stored at approximately –196°C and thawed in ultra-rapid fashion.
The development of vitrification methods has significantly advanced the technology of oocyte cryopreservation, which has been utilized for:
- preservation of fertility in cancer patients
- social reasons (e.g., lack of a partner)
- egg-donation programs
- minimization of the risk of ovarian hyperstimulation syndrome
- storage of surplus eggs when embryo cryopreservation is not feasible.
Cobo and Diaz recently conducted a systematic review and meta-analysis of randomized, controlled trials of oocyte vitrification. They found that the potential for fertilization, embryogenesis, and pregnancy from oocytes that had undergone vitrification and warming was not significantly different from the potential for fresh oocytes and was better than the potential for oocytes that had undergone freezing and thawing from standard freezing cycles.
Although the findings of the meta-analysis were limited by the small number of studies and possible selection bias, an increasing body of evidence supports the use of vitrification for cryopreservation of oocytes. Large-scale controlled trials are needed. Until they are performed, the findings of the meta-analysis should be interpreted with caution.
Newer ultra-rapid freezing of oocytes and embryos using vitrification appears to produce results that are superior to those obtained with traditional slow freezing. Large randomized, controlled trials are needed to confirm the improved efficacy of vitrification.
Anti-Müllerian hormone is an informative test of ovarian reserve—but lacks a nod from the FDA
Buyuk E, Seifer D, Younger J, Grazi R, Lieman H. Random anti-Mullerian hormone (AMH) is a predictor of ovarian response in women with elevated baseline early follicular follicle-stimulating hormone levels. Fertil Steril. 2011;95(7):2369–2372.
Li H, Yeung PW, Lau E, Ho PC, Ng EH. Evaluating the performance of serum anti-Müllerian hormone concentration in predicting the live birth rate of controlled ovarian stimulation and intrauterine insemination. Fertil Steril. 2010;94(6):2177–2181.
Lee J, Kim S, Jee B, Suh C, Kim KC, Moon SY. Anti-Müllerian hormone as a predictor of controlled ovarian hyperstimulation outcome: comparison of two commercial immunoassay kits. Fertil Steril. 2011;95(8):2602–2604.
Although it is well understood that both the quantity and quality of oocytes decline with age, the assessment of ovarian reserve continues to be a clinical challenge. Accurate evaluation can predict a woman’s response to infertility treatment, including IVF, and estimate her chance of conception. Noninvasive tests of ovarian reserve are a critical component of any evaluation of fertility. Although a woman’s age is the single most important historical factor in the assessment of reproductive capacity, there is significant variation in ovarian aging among women.
Historically, age, antral follicle count (AFC), and measurement of cycle day 3 follicle-stimulating hormone (FSH) and estradiol (E2) levels have been the most widely used measures of ovarian reserve, but mounting evidence suggests that assessment of the anti-Müllerian hormone (AMH) level may be even more informative.
AMH, also known as Müllerian-inhibiting substance, is a dimeric glycoprotein. A member of the transforming growth factor–ß family, AMH is closely related to inhibin and activin and is secreted by granulosa cells of preantral and small antral follicles in post-pubertal females.7 AMH aids in the coordination of ovarian follicular development by inhibiting recruitment of additional primordial follicles and decreasing the sensitivity of preantral and small antral follicles to FSH.8,9
AMH levels, measurable in serum, decline with age and are undetectable after menopause.10 Unlike FSH, which fluctuates during the menstrual cycle, AMH exhibits minimal intercycle and intracycle variation. The AMH level remains stable in women taking oral contraceptives and even in women who are pregnant.11
AMH is independently and significantly correlated with the ovarian response to gonadotropin therapy, with decreased levels of AMH associated with a poor response, and increased levels associated with a strong response.12 In the first cycle of IVF, an elevated AMH level has been associated with excessive response to gonadotropins and an increased risk of ovarian hyperstimulation syndrome (OHSS), independent of age and the presence of polycystic ovary syndrome.12
In a recent study of women who had an elevated FSH level and were undergoing IVF, the AMH level was strongly associated with the number of oocytes retrieved.13 Women who had an elevated FSH level but a serum AMH level of 0.6 ng/mL or above had a greater number of oocytes and day-3 embryos retrieved; they also had a lower cancellation rate than women who had a lower AMH level.13
Although no single test can predict the outcome of treatment for infertility, AMH concentrations are significantly higher in women who have a live birth (from the first cycle of stimulated IUI or after three cycles) than in women who do not.14
Two ELISA kits, one value?
Two types of enzyme-linked immunosorbent assay (ELISA) kits are commercially available for measurement of the AMH level: one from Immunotech Beckman Coulter and the other from Diagnostic Systems Laboratories. Neither kit has been approved for clinical use by the US Food and Drug Administration.
Studies comparing the values obtained using each kit have been inconsistent, generating controversy about the measurement of AMH. A recent study of women who were undergoing controlled ovarian stimulation found that the AMH levels obtained by the two kits were similar and significantly correlated with each other.15 In that study, the AMH level was measured on the day before gonadotropin administration or on the day of oocyte retrieval.15 In addition, the AMH concentrations measured by both kits were significantly associated with age, basal FSH levels, AFC, and the outcome of controlled ovarian stimulation.15 The authors concluded:
- The two commercially available kits provide reliable and similar results.
- The AMH level measured by either kit can predict the outcome of controlled ovarian stimulation, with similar reference values.15
Measurement of the AMH level can be an informative aspect of the evaluation of a patient’s fertility, as well as a valuable tool in the assessment of ovarian reserve. The AMH level can also help clinicians identify the appropriate dose of gonadotropins and predict which patients might be likely to over- or under-respond to stimulation—ultimately reducing the length and cost of treatment. Knowledge of the patient’s AMH level might inform pretreatment counseling and help women achieve reasonable expectations.
AMH is a useful test to help predict a patient’s response to ovarian stimulation and her chances of achieving pregnancy. However, AMH is only one measure of ovarian reserve and should not be used alone as a reason to exclude patients from treatment. In our practice, we use the AMH level along with cycle day 3 antral follicle count and FSH and estradiol levels.
We want to hear from you! Tell us what you think.
1. Ragni G, Caliari I, Nicolosi AE, Arnoldi M, Somigliana E, Crosignani PG. Preventing high-order multiple pregnancies during controlled ovarian hyperstimulation and intrauterine insemination: 3 years’ experience using low-dose recombinant follicle-stimulating hormone and gonadotropin-releasing hormone antagonists. Fertil Steril. 2006;85(3):619-624.
2. Ghesquiere SL, Castelain EG, Spiessens C, et al. Relationship between follicle number and (multiple) live birth rate after controlled ovarian hyperstimulation and intrauterine insemination. Am J Obstet Gynecol. 2007;197(6):589.e1-5.
3. Reindollar RH, Regan MM, Neumann PJ, et al. A randomized clinical trial to evaluate optimal treatment for unexplained infertility: the fast track and standard treatment (FASTT) trial. Fertil Steril. 2010;94(3):888-899.
4. Schreiner-Engel P, Walther VN, Mindes J, et al. First-trimester multifetal pregnancy reduction: acute and persistent psychologic reactions. Am J Obstet Gynecol. 1995;172(2 Pt 1):541.-
5. Leibo S, Pool T. The principal variables of cryopreservation: solutions temperatures, and rate changes. Fertil Steril. 2011;96(2):269-276.
6. Society for Assisted Reproductive Technology; American Society for Reproductive Medicine. Assisted reproductive technology in the United States: 2001 results generated from the American Society for Reproductive Medicine/Society for Assisted Reproductive Technology registry. Fertil Steril. 2007;87(6):1253-1266.
7. Vigier JA, Picard JY, Tran D, Legeai L, Josso N. Production of anti-Müllerian hormone: another homology between Sertoli and granulosa cells. Endocrinology. 1984;114(4):1315-1320.
8. Durlinger All, Gruijters MJG, Kramer P, et al. Anti-Müllerian hormone attenuates the effects of FSH on follicle development in the mouse ovary. Endocrinology. 2001;142(11):4891-4899.
9. Salmon NA, Handyside AH, Joyce IM. Oocyte regulation and anti-Müllerian hormone expression in granulosa cells during ovarian follicle development in mice. Dev Biol. 2004;266(1):201-208.
10. Shin SY, Lee JR, Noh GW, et al. Analysis of serum levels of anti-Müllerian hormone, inhibin B, insulin-like growth factor-I, insulin-like growth factor binding protein-3, and follicle-stimulating hormone with respect to age and menopausal status. J Korean Med Sci. 2008;23(1):104-110.
11. Streuli I, Fraisse T, Chapron C, Bijaoui G, Bischof P, de Ziegler D. Clinical uses of anti-Müllerian hormone assays: pitfalls and promises. Fertil Steril. 2009;91(1):226-230.
12. Nardo L, Gelbaya T, Wilkinson H, et al. Circulating basal anti-Müllerian hormone levels as predictor of ovarian response in women undergoing ovarian stimulation for in vitro fertilization. Fertil Steril. 2009;92(5):1586-1593.
13. Buyuk E, Seifer D, Younger J, Grazi R, Lieman H. Random anti-Müllerian hormone (AMH) is a predictor of ovarian response in women with elevated baseline early follicular follicle-stimulating hormone levels. Fertil Steril. 2011;95(7):2369-2372.
14. Li HW, Yeung PW, Lau E&, Ho PC, Ng EH. Evaluating the performance of serum anti-Müllerian hormone concentration in predicting the live birth rate of controlled ovarian stimulation and intrauterine insemination. Fertil Steril. 2010;94(6):2177-2181.
15. Lee J, Kim S, Jee B, Suh C, Kim KC, Moon SY. Anti- Müllerian hormone as a predictor of controlled ovarian hyperstimulation outcome: comparison of two commercial immunoassay kits. Fertil Steril. 2011;95(8):2602-2604.
1. Ragni G, Caliari I, Nicolosi AE, Arnoldi M, Somigliana E, Crosignani PG. Preventing high-order multiple pregnancies during controlled ovarian hyperstimulation and intrauterine insemination: 3 years’ experience using low-dose recombinant follicle-stimulating hormone and gonadotropin-releasing hormone antagonists. Fertil Steril. 2006;85(3):619-624.
2. Ghesquiere SL, Castelain EG, Spiessens C, et al. Relationship between follicle number and (multiple) live birth rate after controlled ovarian hyperstimulation and intrauterine insemination. Am J Obstet Gynecol. 2007;197(6):589.e1-5.
3. Reindollar RH, Regan MM, Neumann PJ, et al. A randomized clinical trial to evaluate optimal treatment for unexplained infertility: the fast track and standard treatment (FASTT) trial. Fertil Steril. 2010;94(3):888-899.
4. Schreiner-Engel P, Walther VN, Mindes J, et al. First-trimester multifetal pregnancy reduction: acute and persistent psychologic reactions. Am J Obstet Gynecol. 1995;172(2 Pt 1):541.-
5. Leibo S, Pool T. The principal variables of cryopreservation: solutions temperatures, and rate changes. Fertil Steril. 2011;96(2):269-276.
6. Society for Assisted Reproductive Technology; American Society for Reproductive Medicine. Assisted reproductive technology in the United States: 2001 results generated from the American Society for Reproductive Medicine/Society for Assisted Reproductive Technology registry. Fertil Steril. 2007;87(6):1253-1266.
7. Vigier JA, Picard JY, Tran D, Legeai L, Josso N. Production of anti-Müllerian hormone: another homology between Sertoli and granulosa cells. Endocrinology. 1984;114(4):1315-1320.
8. Durlinger All, Gruijters MJG, Kramer P, et al. Anti-Müllerian hormone attenuates the effects of FSH on follicle development in the mouse ovary. Endocrinology. 2001;142(11):4891-4899.
9. Salmon NA, Handyside AH, Joyce IM. Oocyte regulation and anti-Müllerian hormone expression in granulosa cells during ovarian follicle development in mice. Dev Biol. 2004;266(1):201-208.
10. Shin SY, Lee JR, Noh GW, et al. Analysis of serum levels of anti-Müllerian hormone, inhibin B, insulin-like growth factor-I, insulin-like growth factor binding protein-3, and follicle-stimulating hormone with respect to age and menopausal status. J Korean Med Sci. 2008;23(1):104-110.
11. Streuli I, Fraisse T, Chapron C, Bijaoui G, Bischof P, de Ziegler D. Clinical uses of anti-Müllerian hormone assays: pitfalls and promises. Fertil Steril. 2009;91(1):226-230.
12. Nardo L, Gelbaya T, Wilkinson H, et al. Circulating basal anti-Müllerian hormone levels as predictor of ovarian response in women undergoing ovarian stimulation for in vitro fertilization. Fertil Steril. 2009;92(5):1586-1593.
13. Buyuk E, Seifer D, Younger J, Grazi R, Lieman H. Random anti-Müllerian hormone (AMH) is a predictor of ovarian response in women with elevated baseline early follicular follicle-stimulating hormone levels. Fertil Steril. 2011;95(7):2369-2372.
14. Li HW, Yeung PW, Lau E&, Ho PC, Ng EH. Evaluating the performance of serum anti-Müllerian hormone concentration in predicting the live birth rate of controlled ovarian stimulation and intrauterine insemination. Fertil Steril. 2010;94(6):2177-2181.
15. Lee J, Kim S, Jee B, Suh C, Kim KC, Moon SY. Anti- Müllerian hormone as a predictor of controlled ovarian hyperstimulation outcome: comparison of two commercial immunoassay kits. Fertil Steril. 2011;95(8):2602-2604.

