User login
Much has changed in the management of menopausal women. The Women’s Health Initiative (WHI) and other trials shed light on the risk-benefit ratio of hormone therapy (HT) and significantly altered patterns of usage. A new fracture risk-assessment tool devised by the World Health Organization is now available for widespread use; it continues to be refined so that it can be applied to specific populations with greater accuracy. And the management of low bone mass and osteoporosis has evolved so that we can determine with greater precision exactly who merits our attention.
This year, the Update on Menopause describes:
- a reanalysis of WHI data, focusing on the relationship between hormone therapy and the risk of coronary artery disease (CAD)
- a study from Finland that explores the risk of endometrial cancer associated with various progestin regimens in women who are taking estrogen and who have an intact uterus
- guidance from the North American Menopause Society and the National Osteoporosis Foundation on who, how, and when to evaluate for a likelihood of fracture
- insight into the benefits of and need for vitamin D among menopausal women
- information on a new selective estrogen-receptor modulator under development.
Hormone therapy and CAD: Is the glass half full…or half empty?
Toh S, Hernández-Díaz S, Logan R, Rossouw JE, Hernán MA. Coronary heart disease in postmenopausal recipients of estrogen plus progestin therapy: Does the increased risk ever disappear? A randomized trial. Ann Intern Med. 2010;152(4):211–217.
North American Menopause Society. Position Statement: Estrogen and progestogens use in postmenopausal women: 2010 position statement of The North American Menopause Society. Menopause. 2010;17(2):242–255. DOI: 10.1097/gme.0b013e3181d0f6b9. http://www.menopause.org/PSht10.pdf. Accessed April 1, 2010.
When estrogen therapy is initiated within 10 years of menopause, it may reduce the risk of CAD, according to data from the WHI randomized trial and observational data.
The picture isn’t as clear in regard to estrogen-progestin HT. In a just-published study, Toh and colleagues reassessed data from the WHI trial of continuous oral conjugated equine estrogen plus medroxyprogesterone acetate versus placebo. They also compared the WHI findings with those of the large observational Nurses’ Health Study (NHS). Here are some of their findings:
- participants became less consistent in taking study medication over time—a finding of many long-term studies. This trend prompted Toh and colleagues to adjust their analysis for adherence
- among women who used HT within 10 years after the menopausal transition, the hazard ratio (HR) for CAD was 0.64 (95% confidence interval [CI], 0.21, 1.99) in the WHI and 0.68 (95% CI, 0.24, 1.91) in the NHS. Both hazard ratios suggest that the risk of CAD is lower in Ht users than in nonusers—although the difference is not significant
- when investigators pooled the WHI and NHS findings, the hazard ratio for CAD associated with combination HT was 0.66 (95% CI, 0.31, 1.42). Note that, as the number of participants increases, the confidence limits narrow.
Toh and colleagues concluded that their analysis demonstrated no diminished risk of CAD with HT use. My reading of these data is different: Combination HT does not increase the risk of CAD in women who have been postmenopausal for less than 10 years.
Focus on risk was unbalanced
The question of whether combination HT reduces the risk of CAD in younger women is somewhat moot. I am not aware of any ObGyn in the United States who uses HT to prevent CAD, and the great majority of symptomatic women who consider initiating HT have been menopausal for less than a decade. For these reasons, I find the conclusions drawn by Toh and colleagues a bit mystifying—and the title they chose for their study may be misleading:
Coronary heart disease in postmenopausal recipients of estrogen plus progestin therapy: Does the increased risk ever disappear?
Nevertheless, fear that HT might increase the risk of CAD is common among symptomatic menopausal women and their physicians. What this important analysis can offer is reassurance to symptomatic women who have been menopausal for less than 10 years: namely, that HT—estrogen alone or estrogen plus progestin—does not increase the risk of myocardial infarction or death from CAD.
You should counsel symptomatic women who have been menopausal less than 10 years that short-term use of estrogen therapy or estrogen-progestin therapy does not appear to increase their risk of CAD.
In women taking estrogen, sequential progestin therapy raises the risk of endometrial cancer
Jaakkola S, Lyytinen H, Pukkala E, Ylikorkala O. Endometrial cancer in postmenopausal women using estradiol-progestin therapy. Obstet Gynecol. 2009;114(6):1197–1204.
Because unopposed estrogen raises the risk of endometrial hyperplasia and adenocarcinoma, we prescribe progestational therapy when a menopausal woman who has an intact uterus decides to use estrogen.
Some ObGyns prescribe continuous progestin in this setting; others, sequential progestin (e.g., continuous estrogen along with 14 days of progestin each month). Still others prescribe “long-cycle” sequential regimens comprising continuous estrogen plus 2 weeks of progestin every 3 months. However, the long-term endometrial safety of these regimens has not been adequately explored.
In a national cohort study in Finland, Jaakkola and coworkers followed more than 200,000 menopausal women who used estrogen plus progestin (E+P) HT from 1994 to 2006. The incidence of endometrial cancer in these women was compared with that of all women in Finland. Overall, 1,400 newly diagnosed cases of endometrial cancer were identified.
Investigators found that, compared with the general population:
- E+P users overall had a 54% greater risk of endometrioid endometrial adenocarcinoma, the tumor most closely associated with use of unopposed estrogen
- monthly sequential E+P users had a 69% (5 years’ use) and 156% (10 years’ use) greater risk of this tumor
- at 5 and 10 years of use, long-cycle sequential HT was associated with a substantially higher risk of endometrial adenocarcinoma than was monthly sequential HT
- the endometrial safety profiles of transdermal and oral sequential HT were comparable; so were those of medroxyprogesterone acetate and norethindrone acetate
- in contrast to sequential HT regimens, continuous E+P was associated with a lower risk of endometrial cancer than that found in the overall population (76% risk reduction after 3 to 5 years of use).
These important findings clarify the safety profiles of long-term continuous E+P, which is protective, and sequential E+P, which substantially raises the risk of endometrial adenocarcinoma.
The authors estimate that, for every 1,000 women who use E+P for 10 years, eight additional cases of cancer will be diagnosed if that therapy is sequential and monthly; on the other hand, three or four fewer cases will be diagnosed if HT is continuous.
Women who use E+P hormone therapy should take the progestin continuously rather than sequentially.
Any woman who uses sequential progestin over the long term should undergo regular endometrial monitoring via transvaginal ultrasonography, endometrial biopsy, or both.
Guidance on who to assess for osteoporosis—and when to treat them
The North American Menopause Society. NAMS continuing medical education activity: Management of osteoporosis in postmenopausal women: 2010 position statement of The North American Menopause Society. Menopause. 2010;17(1):23–24.
National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Washington, D.C.: NOF: 2008. http://www.nof.org/professionals/NOF_Clinicians_Guide.pdf. Accessed April 1, 2010.
Kaunitz AM, McClung MR, Feldman RG, Wysocki S. Postmenopausal osteoporosis: fracture risk and prevention. OBG Management. 2009;21(10)(suppl):S1–6.
The North American Menopause Society (NAMS) has updated its position statement on the management of osteoporosis in postmenopausal women, incorporating many recommendations from guidelines issued in 2008 by the National Osteoporosis Foundation. You may find the recommendations on bone mineral density (BMD) assessment and use of medications to prevent fractures of particular interest.
BMD assessment should focus on women at high risk of fracture
In the United States, many women at low risk of fracture begin BMD assessment in their 50s via dual-energy x-ray absorptiometry (DXA) imaging of the lumbar spine and hip (FIGURE). As a result, many of these menopausal women are given a diagnosis of low bone mass (often termed “osteopenia” when in fact their DXA findings do not meet the criteria for osteoporosis) and are given a prescription for a bisphosphonate, often of indefinite duration.
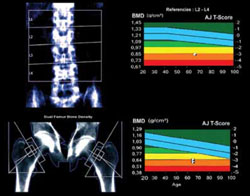
FIGURE When DXA imaging reveals low BMD
DXA scan of the lumbar spine and both hips showing osteoporosis in a 69-year-old woman. The colored graphs show the range of bone mineral density (BMD) across eight decades. The blue bars represent normal bone density; the white squares within the orange and red bars denote this patient’s low BMD. NAMS’s latest position statement clarifies exactly which women should be assessed, concluding that BMD measurement is appropriate in postmenopausal women who are not only at least 50 years old, but who also have one or more of the following risk factors for fracture:
- a history of fracture after menopause
- body mass index (BMI) <21 kg/m2 or weight <127 lb
- parental history of hip fracture
- current smoking, rheumatoid arthritis, or excessive alcohol intake (i.e., three or more drinks per day).
In the absence of these risk factors, BMD assessment should begin at 65 years of age.
Once initiated, treatment is usually long-term
The NAMS statement indicates that drug therapy—using bisphosphonates as first-line agents—is appropriate in postmenopausal women who have any of the following:
- a history of osteoporotic hip or vertebral fracture
- DXA-defined T-score lower than –2.5, indicating osteoporosis
- T-score from –1.0 to –2.5 (low bone mass) plus either a FRAX score that indicates a 10-year risk of hip fracture of at least 3% or a 10-year overall risk of osteoporotic fracture of at least 20%.
The World Health Organization (WHO) Fracture Risk Algorithm (FRAX) was developed to calculate the 10-year risk of hip fracture and the 10-year overall risk of osteoporotic fracture (online at http://www.shef.ac.uk/FRAX/). (For a description of two menopausal cases in which this Web site was used to determine appropriate clinical management, see the article by Kaunitz and colleagues cited above. Also, be aware that use of the FRAX Web site is inappropriate for making clinical decisions about women who are already using prescription antifracture therapy.)
NAMS points out that 1) treatment should usually span a period of years and 2) the risk of fracture after discontinuation of treatment has not been adequately studied.
Lasofoxifene seems unlikely to offer net benefits greater than what women obtain from existing therapies
Clinicians and menopausal women would welcome any agent that can prevent osteoporotic fracture with minimal adverse outcomes. Lasofoxifene appears to fulfill the first half of this equation, but its potential risks and questionable long-term effects cast doubt on its overall utility.
In a manufacturer-sponsored international trial, investigators randomized 8,556 women (mean age, 67 years) who met BMD criteria for osteoporosis to the selective estrogen-receptor modulator (SERM) lasofoxifene (0.25 mg daily or 0.5 mg daily) or placebo for 5 years. Women who received 0.5 mg daily of lasofoxifene had a substantially lower risk of vertebral (HR, 0.58) and nonvertebral (HR, 0.76) fracture than did women who received placebo.1
This dosage of lasofoxifene was also associated with a lower risk of estrogen-receptor–positive breast cancer (HR, 0.19), CAD events (HR, 0.68), and stroke (HR, 0.64), but a twofold higher risk of venous thromboembolic events overall and more than fourfold higher risk of pulmonary embolism. The incidence of endometrial cancer and endometrial hyperplasia was low (fewer than three women in each group), but endometrial polyps and hypertrophy were substantially more common among women who received either dosage of lasofoxifene.1
At 3 years, questionable benefit
Although these findings indicate that lasofoxifene lowers the risk of radiologically confirmed vertebral fracture, data submitted to the FDA reveal that the risk of clinical vertebral fracture was not reduced at 3 years.
Both raloxifene and lasofoxifene are associated with a heightened risk of venous thromboembolic events. Although lasofoxifene did not raise the risk of endometrial neoplasia or hyperplasia in the trial just described, the rates of other endometrial outcomes suggest that this agent has a proliferative effect on the endometrium.1
The reduced risk of estrogen-receptor–positive breast cancer and CAD events is intriguing. However, as an editorial writer points out, a clinician would need to treat 492 women for 1 year to prevent one major CAD event.2
Lasofoxifene does not seem to offer any clinically important benefit over existing SERMs. Moreover, alendronate, a generic bisphosphonate proven to prevent clinical vertebral and nonvertebral fracture, often fills the bill for the prevention of osteoporotic fracture in menopausal women.
References
1. Cummings SR, Ensrud K, Delmas PF, et al. Lasofoxifene in postmenopausal women with osteoporosis. N Engl J Med. 2010;362(8):686-696.
2. Becker C. Another selective estrogen-receptor modulator for osteoporosis. N Engl J Med. 2010;362(8):752-754.
BMD reassessment should be minimal
BMD assessment by means of DXA imaging to monitor the effects of therapy is appropriate after 1 or 2 years of treatment. Thereafter, repeat measurement is of little value in women whose BMD has stabilized or increased on therapy. A follow-up DXA scan is of limited use in predicting the effectiveness of antiresorptive therapy in lowering the risk of fracture. Moreover, changes in BMD can lag behind actual therapeutic benefits (i.e., fracture prevention).
In menopausal women who are not taking prescription antifracture therapy, the follow-up measurement of BMD is not useful until 2 to 5 years after initial testing. Although BMD may be lost rapidly in the initial years after menopause (or after discontinuation of HT), subsequently it plateaus or declines slowly.
If a woman is not using prescription antifracture therapy and is within 2 or 3 years of menopause (or if she has discontinued menopausal HT in the past 2 to 3 years), retesting in 2 years is prudent. However, if the same woman were 5 or more years post-menopausal and had not recently discontinued HT, follow-up BMD assessment can be deferred for 3 to 5 years.
This updated guidance from NAMS emphasizes that BMD need not be assessed in women younger than 65 years unless they have specific risk factors. FRAX evaluation also makes it possible to estimate the 10-year risk of fracture in women who have low bone mass but who do not meet criteria for osteoporosis. FRAX evaluation indicates that prescription therapy is rarely required for women in their 50s or 60s who have low bone mass (but not osteoporosis). For women in their 70s or 80s who have low bone mass (but not osteoporosis), however, FRAX evaluation often leads to a recommendation to initiate prescription antifracture treatment.
Many postmenopausal women who are in their 50s or 60s and who have T-scores of –1.0 to –2.5 are given bisphosphonates, despite being at low risk of fracture. Adherence to the NAMS guidelines will help prevent unnecessary assessment and treatment. In particular, the NAMS recommendations for follow-up BMD assessment—i.e., one-time evaluation 1 to 2 years after initiating therapy and no further assessment in women found to have stable BMD at the first follow-up DXA—should simplify clinical management in this setting.
Hold off on ordering DXA testing until women meet criteria for BMD assessment. In women who do not have osteoporosis, limit use of bisphosphonates to those who have an elevated 10-year risk of fracture, as assessed using the FRAX tool.
Our menopausal patients should be taking more vitamin D supplements
Bischoff-Ferrari H. Vitamin D: what is an adequate vitamin D level and how much supplementation is necessary? Best Pract Res Clin Rheumatol. 2009;23(6):789.
Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, et al. Fall prevention with supplemental and active forms of vitamin D: a meta-analysis of randomised controlled trials. BMJ. 2009;339:b3692.
Stewart JW, Alekel DL, Ritland LM, et al. Serum 25-hydroxyvitamin D is related to indicators of overall physical fitness in healthy postmenopausal women. Menopause. 2009;16(6):1093–1101.
Office of Dietary Supplements. Dietary Supplement Fact Sheet: Vitamin D. National Institutes of Health Web site. http://dietary-supplements.info.nih.gov/factsheets/vitamind.asp. Updated November 13, 2009. Accessed April 2, 2010.
We have long recognized the important role vitamin D plays in promoting calcium absorption from the gut and maintaining adequate serum calcium and phosphate concentrations to enable normal bone mineralization. Now, studies reveal that the vitamin also helps prevent falls and promotes overall fitness in menopausal women. It has also become clear that traditional targets for vitamin D supplementation are inadequate.
Two recent meta-analyses of double-blind, randomized trials concluded that vitamin D reduces the risk of falls in a dose-dependent manner. Dr. Heike Bischoff-Ferrari, a Swiss scientist and a leading vitamin D researcher, points out that 1) a minimum of 700 to 1,000 IU of vitamin D supplementation daily is appropriate in menopausal women and 2) a higher amount is indicated for those who are obese or deficient in vitamin D.
Compare the current recommended dietary allowance (RDA) for adults 51 to 70 years old: 400 IU daily. The federal Food and Nutrition Board is expected to update the vitamin D RDA this spring. The 2010 NAMS statement on osteoporosis recommends a daily vitamin D intake of 800 to 1,000 IU for menopausal women.
Ask your patient to add up the aggregate daily amount of vitamin D she ingests with her multivitamin and calcium and vitamin D supplements. If it is less than 800 IU, have her purchase over-the-counter vitamin D supplements (available in 400, 1,000, and 2,000 IU capsules). Obese patients and those known to be deficient may need to ingest higher daily amounts of vitamin D.
Much has changed in the management of menopausal women. The Women’s Health Initiative (WHI) and other trials shed light on the risk-benefit ratio of hormone therapy (HT) and significantly altered patterns of usage. A new fracture risk-assessment tool devised by the World Health Organization is now available for widespread use; it continues to be refined so that it can be applied to specific populations with greater accuracy. And the management of low bone mass and osteoporosis has evolved so that we can determine with greater precision exactly who merits our attention.
This year, the Update on Menopause describes:
- a reanalysis of WHI data, focusing on the relationship between hormone therapy and the risk of coronary artery disease (CAD)
- a study from Finland that explores the risk of endometrial cancer associated with various progestin regimens in women who are taking estrogen and who have an intact uterus
- guidance from the North American Menopause Society and the National Osteoporosis Foundation on who, how, and when to evaluate for a likelihood of fracture
- insight into the benefits of and need for vitamin D among menopausal women
- information on a new selective estrogen-receptor modulator under development.
Hormone therapy and CAD: Is the glass half full…or half empty?
Toh S, Hernández-Díaz S, Logan R, Rossouw JE, Hernán MA. Coronary heart disease in postmenopausal recipients of estrogen plus progestin therapy: Does the increased risk ever disappear? A randomized trial. Ann Intern Med. 2010;152(4):211–217.
North American Menopause Society. Position Statement: Estrogen and progestogens use in postmenopausal women: 2010 position statement of The North American Menopause Society. Menopause. 2010;17(2):242–255. DOI: 10.1097/gme.0b013e3181d0f6b9. http://www.menopause.org/PSht10.pdf. Accessed April 1, 2010.
When estrogen therapy is initiated within 10 years of menopause, it may reduce the risk of CAD, according to data from the WHI randomized trial and observational data.
The picture isn’t as clear in regard to estrogen-progestin HT. In a just-published study, Toh and colleagues reassessed data from the WHI trial of continuous oral conjugated equine estrogen plus medroxyprogesterone acetate versus placebo. They also compared the WHI findings with those of the large observational Nurses’ Health Study (NHS). Here are some of their findings:
- participants became less consistent in taking study medication over time—a finding of many long-term studies. This trend prompted Toh and colleagues to adjust their analysis for adherence
- among women who used HT within 10 years after the menopausal transition, the hazard ratio (HR) for CAD was 0.64 (95% confidence interval [CI], 0.21, 1.99) in the WHI and 0.68 (95% CI, 0.24, 1.91) in the NHS. Both hazard ratios suggest that the risk of CAD is lower in Ht users than in nonusers—although the difference is not significant
- when investigators pooled the WHI and NHS findings, the hazard ratio for CAD associated with combination HT was 0.66 (95% CI, 0.31, 1.42). Note that, as the number of participants increases, the confidence limits narrow.
Toh and colleagues concluded that their analysis demonstrated no diminished risk of CAD with HT use. My reading of these data is different: Combination HT does not increase the risk of CAD in women who have been postmenopausal for less than 10 years.
Focus on risk was unbalanced
The question of whether combination HT reduces the risk of CAD in younger women is somewhat moot. I am not aware of any ObGyn in the United States who uses HT to prevent CAD, and the great majority of symptomatic women who consider initiating HT have been menopausal for less than a decade. For these reasons, I find the conclusions drawn by Toh and colleagues a bit mystifying—and the title they chose for their study may be misleading:
Coronary heart disease in postmenopausal recipients of estrogen plus progestin therapy: Does the increased risk ever disappear?
Nevertheless, fear that HT might increase the risk of CAD is common among symptomatic menopausal women and their physicians. What this important analysis can offer is reassurance to symptomatic women who have been menopausal for less than 10 years: namely, that HT—estrogen alone or estrogen plus progestin—does not increase the risk of myocardial infarction or death from CAD.
You should counsel symptomatic women who have been menopausal less than 10 years that short-term use of estrogen therapy or estrogen-progestin therapy does not appear to increase their risk of CAD.
In women taking estrogen, sequential progestin therapy raises the risk of endometrial cancer
Jaakkola S, Lyytinen H, Pukkala E, Ylikorkala O. Endometrial cancer in postmenopausal women using estradiol-progestin therapy. Obstet Gynecol. 2009;114(6):1197–1204.
Because unopposed estrogen raises the risk of endometrial hyperplasia and adenocarcinoma, we prescribe progestational therapy when a menopausal woman who has an intact uterus decides to use estrogen.
Some ObGyns prescribe continuous progestin in this setting; others, sequential progestin (e.g., continuous estrogen along with 14 days of progestin each month). Still others prescribe “long-cycle” sequential regimens comprising continuous estrogen plus 2 weeks of progestin every 3 months. However, the long-term endometrial safety of these regimens has not been adequately explored.
In a national cohort study in Finland, Jaakkola and coworkers followed more than 200,000 menopausal women who used estrogen plus progestin (E+P) HT from 1994 to 2006. The incidence of endometrial cancer in these women was compared with that of all women in Finland. Overall, 1,400 newly diagnosed cases of endometrial cancer were identified.
Investigators found that, compared with the general population:
- E+P users overall had a 54% greater risk of endometrioid endometrial adenocarcinoma, the tumor most closely associated with use of unopposed estrogen
- monthly sequential E+P users had a 69% (5 years’ use) and 156% (10 years’ use) greater risk of this tumor
- at 5 and 10 years of use, long-cycle sequential HT was associated with a substantially higher risk of endometrial adenocarcinoma than was monthly sequential HT
- the endometrial safety profiles of transdermal and oral sequential HT were comparable; so were those of medroxyprogesterone acetate and norethindrone acetate
- in contrast to sequential HT regimens, continuous E+P was associated with a lower risk of endometrial cancer than that found in the overall population (76% risk reduction after 3 to 5 years of use).
These important findings clarify the safety profiles of long-term continuous E+P, which is protective, and sequential E+P, which substantially raises the risk of endometrial adenocarcinoma.
The authors estimate that, for every 1,000 women who use E+P for 10 years, eight additional cases of cancer will be diagnosed if that therapy is sequential and monthly; on the other hand, three or four fewer cases will be diagnosed if HT is continuous.
Women who use E+P hormone therapy should take the progestin continuously rather than sequentially.
Any woman who uses sequential progestin over the long term should undergo regular endometrial monitoring via transvaginal ultrasonography, endometrial biopsy, or both.
Guidance on who to assess for osteoporosis—and when to treat them
The North American Menopause Society. NAMS continuing medical education activity: Management of osteoporosis in postmenopausal women: 2010 position statement of The North American Menopause Society. Menopause. 2010;17(1):23–24.
National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Washington, D.C.: NOF: 2008. http://www.nof.org/professionals/NOF_Clinicians_Guide.pdf. Accessed April 1, 2010.
Kaunitz AM, McClung MR, Feldman RG, Wysocki S. Postmenopausal osteoporosis: fracture risk and prevention. OBG Management. 2009;21(10)(suppl):S1–6.
The North American Menopause Society (NAMS) has updated its position statement on the management of osteoporosis in postmenopausal women, incorporating many recommendations from guidelines issued in 2008 by the National Osteoporosis Foundation. You may find the recommendations on bone mineral density (BMD) assessment and use of medications to prevent fractures of particular interest.
BMD assessment should focus on women at high risk of fracture
In the United States, many women at low risk of fracture begin BMD assessment in their 50s via dual-energy x-ray absorptiometry (DXA) imaging of the lumbar spine and hip (FIGURE). As a result, many of these menopausal women are given a diagnosis of low bone mass (often termed “osteopenia” when in fact their DXA findings do not meet the criteria for osteoporosis) and are given a prescription for a bisphosphonate, often of indefinite duration.
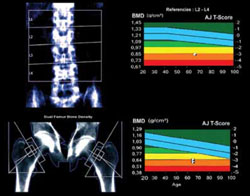
FIGURE When DXA imaging reveals low BMD
DXA scan of the lumbar spine and both hips showing osteoporosis in a 69-year-old woman. The colored graphs show the range of bone mineral density (BMD) across eight decades. The blue bars represent normal bone density; the white squares within the orange and red bars denote this patient’s low BMD. NAMS’s latest position statement clarifies exactly which women should be assessed, concluding that BMD measurement is appropriate in postmenopausal women who are not only at least 50 years old, but who also have one or more of the following risk factors for fracture:
- a history of fracture after menopause
- body mass index (BMI) <21 kg/m2 or weight <127 lb
- parental history of hip fracture
- current smoking, rheumatoid arthritis, or excessive alcohol intake (i.e., three or more drinks per day).
In the absence of these risk factors, BMD assessment should begin at 65 years of age.
Once initiated, treatment is usually long-term
The NAMS statement indicates that drug therapy—using bisphosphonates as first-line agents—is appropriate in postmenopausal women who have any of the following:
- a history of osteoporotic hip or vertebral fracture
- DXA-defined T-score lower than –2.5, indicating osteoporosis
- T-score from –1.0 to –2.5 (low bone mass) plus either a FRAX score that indicates a 10-year risk of hip fracture of at least 3% or a 10-year overall risk of osteoporotic fracture of at least 20%.
The World Health Organization (WHO) Fracture Risk Algorithm (FRAX) was developed to calculate the 10-year risk of hip fracture and the 10-year overall risk of osteoporotic fracture (online at http://www.shef.ac.uk/FRAX/). (For a description of two menopausal cases in which this Web site was used to determine appropriate clinical management, see the article by Kaunitz and colleagues cited above. Also, be aware that use of the FRAX Web site is inappropriate for making clinical decisions about women who are already using prescription antifracture therapy.)
NAMS points out that 1) treatment should usually span a period of years and 2) the risk of fracture after discontinuation of treatment has not been adequately studied.
Lasofoxifene seems unlikely to offer net benefits greater than what women obtain from existing therapies
Clinicians and menopausal women would welcome any agent that can prevent osteoporotic fracture with minimal adverse outcomes. Lasofoxifene appears to fulfill the first half of this equation, but its potential risks and questionable long-term effects cast doubt on its overall utility.
In a manufacturer-sponsored international trial, investigators randomized 8,556 women (mean age, 67 years) who met BMD criteria for osteoporosis to the selective estrogen-receptor modulator (SERM) lasofoxifene (0.25 mg daily or 0.5 mg daily) or placebo for 5 years. Women who received 0.5 mg daily of lasofoxifene had a substantially lower risk of vertebral (HR, 0.58) and nonvertebral (HR, 0.76) fracture than did women who received placebo.1
This dosage of lasofoxifene was also associated with a lower risk of estrogen-receptor–positive breast cancer (HR, 0.19), CAD events (HR, 0.68), and stroke (HR, 0.64), but a twofold higher risk of venous thromboembolic events overall and more than fourfold higher risk of pulmonary embolism. The incidence of endometrial cancer and endometrial hyperplasia was low (fewer than three women in each group), but endometrial polyps and hypertrophy were substantially more common among women who received either dosage of lasofoxifene.1
At 3 years, questionable benefit
Although these findings indicate that lasofoxifene lowers the risk of radiologically confirmed vertebral fracture, data submitted to the FDA reveal that the risk of clinical vertebral fracture was not reduced at 3 years.
Both raloxifene and lasofoxifene are associated with a heightened risk of venous thromboembolic events. Although lasofoxifene did not raise the risk of endometrial neoplasia or hyperplasia in the trial just described, the rates of other endometrial outcomes suggest that this agent has a proliferative effect on the endometrium.1
The reduced risk of estrogen-receptor–positive breast cancer and CAD events is intriguing. However, as an editorial writer points out, a clinician would need to treat 492 women for 1 year to prevent one major CAD event.2
Lasofoxifene does not seem to offer any clinically important benefit over existing SERMs. Moreover, alendronate, a generic bisphosphonate proven to prevent clinical vertebral and nonvertebral fracture, often fills the bill for the prevention of osteoporotic fracture in menopausal women.
References
1. Cummings SR, Ensrud K, Delmas PF, et al. Lasofoxifene in postmenopausal women with osteoporosis. N Engl J Med. 2010;362(8):686-696.
2. Becker C. Another selective estrogen-receptor modulator for osteoporosis. N Engl J Med. 2010;362(8):752-754.
BMD reassessment should be minimal
BMD assessment by means of DXA imaging to monitor the effects of therapy is appropriate after 1 or 2 years of treatment. Thereafter, repeat measurement is of little value in women whose BMD has stabilized or increased on therapy. A follow-up DXA scan is of limited use in predicting the effectiveness of antiresorptive therapy in lowering the risk of fracture. Moreover, changes in BMD can lag behind actual therapeutic benefits (i.e., fracture prevention).
In menopausal women who are not taking prescription antifracture therapy, the follow-up measurement of BMD is not useful until 2 to 5 years after initial testing. Although BMD may be lost rapidly in the initial years after menopause (or after discontinuation of HT), subsequently it plateaus or declines slowly.
If a woman is not using prescription antifracture therapy and is within 2 or 3 years of menopause (or if she has discontinued menopausal HT in the past 2 to 3 years), retesting in 2 years is prudent. However, if the same woman were 5 or more years post-menopausal and had not recently discontinued HT, follow-up BMD assessment can be deferred for 3 to 5 years.
This updated guidance from NAMS emphasizes that BMD need not be assessed in women younger than 65 years unless they have specific risk factors. FRAX evaluation also makes it possible to estimate the 10-year risk of fracture in women who have low bone mass but who do not meet criteria for osteoporosis. FRAX evaluation indicates that prescription therapy is rarely required for women in their 50s or 60s who have low bone mass (but not osteoporosis). For women in their 70s or 80s who have low bone mass (but not osteoporosis), however, FRAX evaluation often leads to a recommendation to initiate prescription antifracture treatment.
Many postmenopausal women who are in their 50s or 60s and who have T-scores of –1.0 to –2.5 are given bisphosphonates, despite being at low risk of fracture. Adherence to the NAMS guidelines will help prevent unnecessary assessment and treatment. In particular, the NAMS recommendations for follow-up BMD assessment—i.e., one-time evaluation 1 to 2 years after initiating therapy and no further assessment in women found to have stable BMD at the first follow-up DXA—should simplify clinical management in this setting.
Hold off on ordering DXA testing until women meet criteria for BMD assessment. In women who do not have osteoporosis, limit use of bisphosphonates to those who have an elevated 10-year risk of fracture, as assessed using the FRAX tool.
Our menopausal patients should be taking more vitamin D supplements
Bischoff-Ferrari H. Vitamin D: what is an adequate vitamin D level and how much supplementation is necessary? Best Pract Res Clin Rheumatol. 2009;23(6):789.
Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, et al. Fall prevention with supplemental and active forms of vitamin D: a meta-analysis of randomised controlled trials. BMJ. 2009;339:b3692.
Stewart JW, Alekel DL, Ritland LM, et al. Serum 25-hydroxyvitamin D is related to indicators of overall physical fitness in healthy postmenopausal women. Menopause. 2009;16(6):1093–1101.
Office of Dietary Supplements. Dietary Supplement Fact Sheet: Vitamin D. National Institutes of Health Web site. http://dietary-supplements.info.nih.gov/factsheets/vitamind.asp. Updated November 13, 2009. Accessed April 2, 2010.
We have long recognized the important role vitamin D plays in promoting calcium absorption from the gut and maintaining adequate serum calcium and phosphate concentrations to enable normal bone mineralization. Now, studies reveal that the vitamin also helps prevent falls and promotes overall fitness in menopausal women. It has also become clear that traditional targets for vitamin D supplementation are inadequate.
Two recent meta-analyses of double-blind, randomized trials concluded that vitamin D reduces the risk of falls in a dose-dependent manner. Dr. Heike Bischoff-Ferrari, a Swiss scientist and a leading vitamin D researcher, points out that 1) a minimum of 700 to 1,000 IU of vitamin D supplementation daily is appropriate in menopausal women and 2) a higher amount is indicated for those who are obese or deficient in vitamin D.
Compare the current recommended dietary allowance (RDA) for adults 51 to 70 years old: 400 IU daily. The federal Food and Nutrition Board is expected to update the vitamin D RDA this spring. The 2010 NAMS statement on osteoporosis recommends a daily vitamin D intake of 800 to 1,000 IU for menopausal women.
Ask your patient to add up the aggregate daily amount of vitamin D she ingests with her multivitamin and calcium and vitamin D supplements. If it is less than 800 IU, have her purchase over-the-counter vitamin D supplements (available in 400, 1,000, and 2,000 IU capsules). Obese patients and those known to be deficient may need to ingest higher daily amounts of vitamin D.
Much has changed in the management of menopausal women. The Women’s Health Initiative (WHI) and other trials shed light on the risk-benefit ratio of hormone therapy (HT) and significantly altered patterns of usage. A new fracture risk-assessment tool devised by the World Health Organization is now available for widespread use; it continues to be refined so that it can be applied to specific populations with greater accuracy. And the management of low bone mass and osteoporosis has evolved so that we can determine with greater precision exactly who merits our attention.
This year, the Update on Menopause describes:
- a reanalysis of WHI data, focusing on the relationship between hormone therapy and the risk of coronary artery disease (CAD)
- a study from Finland that explores the risk of endometrial cancer associated with various progestin regimens in women who are taking estrogen and who have an intact uterus
- guidance from the North American Menopause Society and the National Osteoporosis Foundation on who, how, and when to evaluate for a likelihood of fracture
- insight into the benefits of and need for vitamin D among menopausal women
- information on a new selective estrogen-receptor modulator under development.
Hormone therapy and CAD: Is the glass half full…or half empty?
Toh S, Hernández-Díaz S, Logan R, Rossouw JE, Hernán MA. Coronary heart disease in postmenopausal recipients of estrogen plus progestin therapy: Does the increased risk ever disappear? A randomized trial. Ann Intern Med. 2010;152(4):211–217.
North American Menopause Society. Position Statement: Estrogen and progestogens use in postmenopausal women: 2010 position statement of The North American Menopause Society. Menopause. 2010;17(2):242–255. DOI: 10.1097/gme.0b013e3181d0f6b9. http://www.menopause.org/PSht10.pdf. Accessed April 1, 2010.
When estrogen therapy is initiated within 10 years of menopause, it may reduce the risk of CAD, according to data from the WHI randomized trial and observational data.
The picture isn’t as clear in regard to estrogen-progestin HT. In a just-published study, Toh and colleagues reassessed data from the WHI trial of continuous oral conjugated equine estrogen plus medroxyprogesterone acetate versus placebo. They also compared the WHI findings with those of the large observational Nurses’ Health Study (NHS). Here are some of their findings:
- participants became less consistent in taking study medication over time—a finding of many long-term studies. This trend prompted Toh and colleagues to adjust their analysis for adherence
- among women who used HT within 10 years after the menopausal transition, the hazard ratio (HR) for CAD was 0.64 (95% confidence interval [CI], 0.21, 1.99) in the WHI and 0.68 (95% CI, 0.24, 1.91) in the NHS. Both hazard ratios suggest that the risk of CAD is lower in Ht users than in nonusers—although the difference is not significant
- when investigators pooled the WHI and NHS findings, the hazard ratio for CAD associated with combination HT was 0.66 (95% CI, 0.31, 1.42). Note that, as the number of participants increases, the confidence limits narrow.
Toh and colleagues concluded that their analysis demonstrated no diminished risk of CAD with HT use. My reading of these data is different: Combination HT does not increase the risk of CAD in women who have been postmenopausal for less than 10 years.
Focus on risk was unbalanced
The question of whether combination HT reduces the risk of CAD in younger women is somewhat moot. I am not aware of any ObGyn in the United States who uses HT to prevent CAD, and the great majority of symptomatic women who consider initiating HT have been menopausal for less than a decade. For these reasons, I find the conclusions drawn by Toh and colleagues a bit mystifying—and the title they chose for their study may be misleading:
Coronary heart disease in postmenopausal recipients of estrogen plus progestin therapy: Does the increased risk ever disappear?
Nevertheless, fear that HT might increase the risk of CAD is common among symptomatic menopausal women and their physicians. What this important analysis can offer is reassurance to symptomatic women who have been menopausal for less than 10 years: namely, that HT—estrogen alone or estrogen plus progestin—does not increase the risk of myocardial infarction or death from CAD.
You should counsel symptomatic women who have been menopausal less than 10 years that short-term use of estrogen therapy or estrogen-progestin therapy does not appear to increase their risk of CAD.
In women taking estrogen, sequential progestin therapy raises the risk of endometrial cancer
Jaakkola S, Lyytinen H, Pukkala E, Ylikorkala O. Endometrial cancer in postmenopausal women using estradiol-progestin therapy. Obstet Gynecol. 2009;114(6):1197–1204.
Because unopposed estrogen raises the risk of endometrial hyperplasia and adenocarcinoma, we prescribe progestational therapy when a menopausal woman who has an intact uterus decides to use estrogen.
Some ObGyns prescribe continuous progestin in this setting; others, sequential progestin (e.g., continuous estrogen along with 14 days of progestin each month). Still others prescribe “long-cycle” sequential regimens comprising continuous estrogen plus 2 weeks of progestin every 3 months. However, the long-term endometrial safety of these regimens has not been adequately explored.
In a national cohort study in Finland, Jaakkola and coworkers followed more than 200,000 menopausal women who used estrogen plus progestin (E+P) HT from 1994 to 2006. The incidence of endometrial cancer in these women was compared with that of all women in Finland. Overall, 1,400 newly diagnosed cases of endometrial cancer were identified.
Investigators found that, compared with the general population:
- E+P users overall had a 54% greater risk of endometrioid endometrial adenocarcinoma, the tumor most closely associated with use of unopposed estrogen
- monthly sequential E+P users had a 69% (5 years’ use) and 156% (10 years’ use) greater risk of this tumor
- at 5 and 10 years of use, long-cycle sequential HT was associated with a substantially higher risk of endometrial adenocarcinoma than was monthly sequential HT
- the endometrial safety profiles of transdermal and oral sequential HT were comparable; so were those of medroxyprogesterone acetate and norethindrone acetate
- in contrast to sequential HT regimens, continuous E+P was associated with a lower risk of endometrial cancer than that found in the overall population (76% risk reduction after 3 to 5 years of use).
These important findings clarify the safety profiles of long-term continuous E+P, which is protective, and sequential E+P, which substantially raises the risk of endometrial adenocarcinoma.
The authors estimate that, for every 1,000 women who use E+P for 10 years, eight additional cases of cancer will be diagnosed if that therapy is sequential and monthly; on the other hand, three or four fewer cases will be diagnosed if HT is continuous.
Women who use E+P hormone therapy should take the progestin continuously rather than sequentially.
Any woman who uses sequential progestin over the long term should undergo regular endometrial monitoring via transvaginal ultrasonography, endometrial biopsy, or both.
Guidance on who to assess for osteoporosis—and when to treat them
The North American Menopause Society. NAMS continuing medical education activity: Management of osteoporosis in postmenopausal women: 2010 position statement of The North American Menopause Society. Menopause. 2010;17(1):23–24.
National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Washington, D.C.: NOF: 2008. http://www.nof.org/professionals/NOF_Clinicians_Guide.pdf. Accessed April 1, 2010.
Kaunitz AM, McClung MR, Feldman RG, Wysocki S. Postmenopausal osteoporosis: fracture risk and prevention. OBG Management. 2009;21(10)(suppl):S1–6.
The North American Menopause Society (NAMS) has updated its position statement on the management of osteoporosis in postmenopausal women, incorporating many recommendations from guidelines issued in 2008 by the National Osteoporosis Foundation. You may find the recommendations on bone mineral density (BMD) assessment and use of medications to prevent fractures of particular interest.
BMD assessment should focus on women at high risk of fracture
In the United States, many women at low risk of fracture begin BMD assessment in their 50s via dual-energy x-ray absorptiometry (DXA) imaging of the lumbar spine and hip (FIGURE). As a result, many of these menopausal women are given a diagnosis of low bone mass (often termed “osteopenia” when in fact their DXA findings do not meet the criteria for osteoporosis) and are given a prescription for a bisphosphonate, often of indefinite duration.
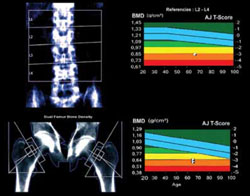
FIGURE When DXA imaging reveals low BMD
DXA scan of the lumbar spine and both hips showing osteoporosis in a 69-year-old woman. The colored graphs show the range of bone mineral density (BMD) across eight decades. The blue bars represent normal bone density; the white squares within the orange and red bars denote this patient’s low BMD. NAMS’s latest position statement clarifies exactly which women should be assessed, concluding that BMD measurement is appropriate in postmenopausal women who are not only at least 50 years old, but who also have one or more of the following risk factors for fracture:
- a history of fracture after menopause
- body mass index (BMI) <21 kg/m2 or weight <127 lb
- parental history of hip fracture
- current smoking, rheumatoid arthritis, or excessive alcohol intake (i.e., three or more drinks per day).
In the absence of these risk factors, BMD assessment should begin at 65 years of age.
Once initiated, treatment is usually long-term
The NAMS statement indicates that drug therapy—using bisphosphonates as first-line agents—is appropriate in postmenopausal women who have any of the following:
- a history of osteoporotic hip or vertebral fracture
- DXA-defined T-score lower than –2.5, indicating osteoporosis
- T-score from –1.0 to –2.5 (low bone mass) plus either a FRAX score that indicates a 10-year risk of hip fracture of at least 3% or a 10-year overall risk of osteoporotic fracture of at least 20%.
The World Health Organization (WHO) Fracture Risk Algorithm (FRAX) was developed to calculate the 10-year risk of hip fracture and the 10-year overall risk of osteoporotic fracture (online at http://www.shef.ac.uk/FRAX/). (For a description of two menopausal cases in which this Web site was used to determine appropriate clinical management, see the article by Kaunitz and colleagues cited above. Also, be aware that use of the FRAX Web site is inappropriate for making clinical decisions about women who are already using prescription antifracture therapy.)
NAMS points out that 1) treatment should usually span a period of years and 2) the risk of fracture after discontinuation of treatment has not been adequately studied.
Lasofoxifene seems unlikely to offer net benefits greater than what women obtain from existing therapies
Clinicians and menopausal women would welcome any agent that can prevent osteoporotic fracture with minimal adverse outcomes. Lasofoxifene appears to fulfill the first half of this equation, but its potential risks and questionable long-term effects cast doubt on its overall utility.
In a manufacturer-sponsored international trial, investigators randomized 8,556 women (mean age, 67 years) who met BMD criteria for osteoporosis to the selective estrogen-receptor modulator (SERM) lasofoxifene (0.25 mg daily or 0.5 mg daily) or placebo for 5 years. Women who received 0.5 mg daily of lasofoxifene had a substantially lower risk of vertebral (HR, 0.58) and nonvertebral (HR, 0.76) fracture than did women who received placebo.1
This dosage of lasofoxifene was also associated with a lower risk of estrogen-receptor–positive breast cancer (HR, 0.19), CAD events (HR, 0.68), and stroke (HR, 0.64), but a twofold higher risk of venous thromboembolic events overall and more than fourfold higher risk of pulmonary embolism. The incidence of endometrial cancer and endometrial hyperplasia was low (fewer than three women in each group), but endometrial polyps and hypertrophy were substantially more common among women who received either dosage of lasofoxifene.1
At 3 years, questionable benefit
Although these findings indicate that lasofoxifene lowers the risk of radiologically confirmed vertebral fracture, data submitted to the FDA reveal that the risk of clinical vertebral fracture was not reduced at 3 years.
Both raloxifene and lasofoxifene are associated with a heightened risk of venous thromboembolic events. Although lasofoxifene did not raise the risk of endometrial neoplasia or hyperplasia in the trial just described, the rates of other endometrial outcomes suggest that this agent has a proliferative effect on the endometrium.1
The reduced risk of estrogen-receptor–positive breast cancer and CAD events is intriguing. However, as an editorial writer points out, a clinician would need to treat 492 women for 1 year to prevent one major CAD event.2
Lasofoxifene does not seem to offer any clinically important benefit over existing SERMs. Moreover, alendronate, a generic bisphosphonate proven to prevent clinical vertebral and nonvertebral fracture, often fills the bill for the prevention of osteoporotic fracture in menopausal women.
References
1. Cummings SR, Ensrud K, Delmas PF, et al. Lasofoxifene in postmenopausal women with osteoporosis. N Engl J Med. 2010;362(8):686-696.
2. Becker C. Another selective estrogen-receptor modulator for osteoporosis. N Engl J Med. 2010;362(8):752-754.
BMD reassessment should be minimal
BMD assessment by means of DXA imaging to monitor the effects of therapy is appropriate after 1 or 2 years of treatment. Thereafter, repeat measurement is of little value in women whose BMD has stabilized or increased on therapy. A follow-up DXA scan is of limited use in predicting the effectiveness of antiresorptive therapy in lowering the risk of fracture. Moreover, changes in BMD can lag behind actual therapeutic benefits (i.e., fracture prevention).
In menopausal women who are not taking prescription antifracture therapy, the follow-up measurement of BMD is not useful until 2 to 5 years after initial testing. Although BMD may be lost rapidly in the initial years after menopause (or after discontinuation of HT), subsequently it plateaus or declines slowly.
If a woman is not using prescription antifracture therapy and is within 2 or 3 years of menopause (or if she has discontinued menopausal HT in the past 2 to 3 years), retesting in 2 years is prudent. However, if the same woman were 5 or more years post-menopausal and had not recently discontinued HT, follow-up BMD assessment can be deferred for 3 to 5 years.
This updated guidance from NAMS emphasizes that BMD need not be assessed in women younger than 65 years unless they have specific risk factors. FRAX evaluation also makes it possible to estimate the 10-year risk of fracture in women who have low bone mass but who do not meet criteria for osteoporosis. FRAX evaluation indicates that prescription therapy is rarely required for women in their 50s or 60s who have low bone mass (but not osteoporosis). For women in their 70s or 80s who have low bone mass (but not osteoporosis), however, FRAX evaluation often leads to a recommendation to initiate prescription antifracture treatment.
Many postmenopausal women who are in their 50s or 60s and who have T-scores of –1.0 to –2.5 are given bisphosphonates, despite being at low risk of fracture. Adherence to the NAMS guidelines will help prevent unnecessary assessment and treatment. In particular, the NAMS recommendations for follow-up BMD assessment—i.e., one-time evaluation 1 to 2 years after initiating therapy and no further assessment in women found to have stable BMD at the first follow-up DXA—should simplify clinical management in this setting.
Hold off on ordering DXA testing until women meet criteria for BMD assessment. In women who do not have osteoporosis, limit use of bisphosphonates to those who have an elevated 10-year risk of fracture, as assessed using the FRAX tool.
Our menopausal patients should be taking more vitamin D supplements
Bischoff-Ferrari H. Vitamin D: what is an adequate vitamin D level and how much supplementation is necessary? Best Pract Res Clin Rheumatol. 2009;23(6):789.
Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, et al. Fall prevention with supplemental and active forms of vitamin D: a meta-analysis of randomised controlled trials. BMJ. 2009;339:b3692.
Stewart JW, Alekel DL, Ritland LM, et al. Serum 25-hydroxyvitamin D is related to indicators of overall physical fitness in healthy postmenopausal women. Menopause. 2009;16(6):1093–1101.
Office of Dietary Supplements. Dietary Supplement Fact Sheet: Vitamin D. National Institutes of Health Web site. http://dietary-supplements.info.nih.gov/factsheets/vitamind.asp. Updated November 13, 2009. Accessed April 2, 2010.
We have long recognized the important role vitamin D plays in promoting calcium absorption from the gut and maintaining adequate serum calcium and phosphate concentrations to enable normal bone mineralization. Now, studies reveal that the vitamin also helps prevent falls and promotes overall fitness in menopausal women. It has also become clear that traditional targets for vitamin D supplementation are inadequate.
Two recent meta-analyses of double-blind, randomized trials concluded that vitamin D reduces the risk of falls in a dose-dependent manner. Dr. Heike Bischoff-Ferrari, a Swiss scientist and a leading vitamin D researcher, points out that 1) a minimum of 700 to 1,000 IU of vitamin D supplementation daily is appropriate in menopausal women and 2) a higher amount is indicated for those who are obese or deficient in vitamin D.
Compare the current recommended dietary allowance (RDA) for adults 51 to 70 years old: 400 IU daily. The federal Food and Nutrition Board is expected to update the vitamin D RDA this spring. The 2010 NAMS statement on osteoporosis recommends a daily vitamin D intake of 800 to 1,000 IU for menopausal women.
Ask your patient to add up the aggregate daily amount of vitamin D she ingests with her multivitamin and calcium and vitamin D supplements. If it is less than 800 IU, have her purchase over-the-counter vitamin D supplements (available in 400, 1,000, and 2,000 IU capsules). Obese patients and those known to be deficient may need to ingest higher daily amounts of vitamin D.
