User login
From the Cincinnati Children’s Hospital Medical Center, Cincinnati, OH.
This article is the third in our Hemoglobinopathy Learning Collaborative series. See the related editorial by Oyeku et al in the February 2014 issue of JCOM. (—Ed.)
ABSTRACT
• Objective: To develop and implement individualized home pain management plans that included pharmacologic as well as nonpharmacologic strategies for children with sickle cell disease (SCD).
• Methods: A multidisciplinary quality improvement team developed a questionnaire to assess the frequency, location, and severity of a patient’s pain during a routine comprehensive visit in order to help the patient and family develop an effective home pain management plan. Using plan-do-study-act cycles, the team was able to build this process into the daily workflow for all SCD patients age 5 years to 21 years of age. Patients with comprehensive visits scheduled from January 2012 to May 2013 were included (n = 188) in the intervention.
• Results: By May of 2013, 88% of eligible patients had an individualized home plan in place. There was a concomitant reduction in the percentage of SCD patients seen in the ED for uncomplicated SCD pain (6.9% vs. 1.1%).
• Conclusions: Using quality improvement methods, an individualized home pain management intervention was incorporated successfully into the daily workflow of a busy outpatient SCD clinic. This intervention has the potential to improve patient outcomes by decreasing avoidable ED visits as well as reducing overall health care costs.
Sickle cell disease (SCD) is one of the most common genetic disorders in the United States, affecting approximately 1 in 500 African-American infants each year [1]. The genetic mutation that causes SCD results in the production of an abnormal hemoglobin molecule (HbS) in the red blood cells (RBC). Under low oxygen conditions, the HbS polymerizes and causes the RBCs to elongate into a sickle form (crescent shape) and decreases the life span of the RBC. Additionally, RBCs with HbS are more “sticky,” adhering to vessel walls and limiting blood flow and oxygen delivery to many tissues and organs in the body. The resultant tissue ischemia causes progressive organ injury as well as episodes of pain (vaso-occlusive crisis).
Recurrent pain episodes are the hallmark of this disease, accounting for the majority of emergency department (ED) visits as well as hospitalizations. High-quality outpatient care can reduce acute care and ED visits as well as hospitalization rates in patients with SCD [2]. Additionally, ensuring that patients have a home pain management plan and understand how to assess and reassess their pain may improve outcomes [3]. Data from our population of children with SCD indicate that 40% to 50% of ED visits in 2011 were for uncomplicated pain episodes (no concomitant medical issues such as fever, increased respiratory rate, wheezing, worsening pallor). If these pain episodes had been effectively managed at home, the ED visits might have been avoided.
In an effort to reduce these potentially preventable ED visits and subsequent hospitalizations, the Comprehensive Sickle Cell Center at Cincinnati Children’s Hospital Medical Center assembled a quality improvement (QI) team to partner with patients and their families to develop individualized home pain management plans (HPMP) that incorporated both pharmacologic and nonpharmacologic pain management strategies. We also sought to identify and remove barriers to the successful use of a home pain management plan, such as not having enough analgesics at home or not allowing enough time for analgesics to work before presenting to the ED. We documented the plan in a standard location and format in the electronic medical record (EMR), making it available to all medical center providers. This paper describes the development, refinement, and testing of an individualized HPMP intervention and related outcomes.
METHODS
Setting
Cincinnati Children’s Hospital Medical Center is a nonprofit pediatric medical center with 587 inpatient beds in Ohio providing acute and chronic care for children in Southern Ohio, Northern Kentucky, and Southeastern Indiana. The center’s Comprehensive Sickle Cell Center provides comprehensive care to approximately 280 children with SCD in the region from birth to 21 years of age. The medical center is the only major pediatric inpatient facility in the tri-state area. Greater than 75% of the SCD patients at our center live within a 15-mile radius, therefore, essentially all ED visits and hospitalizations for our patients occur at our center.
Participants
Improvement Team
The core QI team consisted of multidisciplinary health care providers with experience caring for patients with SCD, including 3 SCD nurse care managers, 2 physicians, 2 PhD psychologists, 4 nurse practitioners, a QI consultant, and a data analyst. Additional support and suggestions were received from other SCD team members (eg, social workers, school interventionists). The core QI multidisciplinary team met weekly to design and test the intervention and implementation process.
Intervention
The intervention consisted of the following elements: (1) pre-visit review to identify eligible patients needing a new or updated home pain management plan; (2) family completion of a pain assessment tool; (3) review of pain assessment tool by SCD team; (4) development of collaborative home plan with family and the medical team; (4) integration of nonpharmacological strategies into the home plan (developed with the psychologist); (5) printed copy of the plan for family to take home; (6) documentation of HPMP in the EMR (Table 2); and, (7) a follow-up phone call for eligible patients with ED or urgent care visits for uncomplicated SCD pain by the nurse care manager.
Implementation
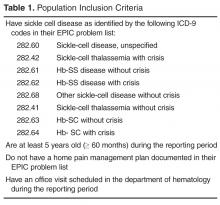
Each week the data analyst generated a list of eligible patients with ICD-9 diagnostic codes for SCD using SQL (structured query language) to extract the data from the EMR (Table 1). The SCD nurse care managers reviewed the list and notified the team of those patients needing a pain assessment and updated HPMP during the daily pre-clinic patient review rounds each morning.
The provider seeing the patient that day facilitated the patient and family’s completion of the pain assessment tool. The pain assessment tool consisted of 13 items and measured recent illnesses or transfusions, patient’s pain location, intensity, associated symptoms, potential triggers, and the impact of the pain on quality of life (missed days of school/work). In addition, the patient’s current pain management strategies, perceived effectiveness of those strategies, and analgesics available at home was recorded.
After discussing the results with the team, a medical provider reviewed the findings with the patient and family and developed a plan for pharmacologic pain management at home utilizing a stepwise approach based on the World Health Organization (WHO) analgesic ladder for selecting pain-relief drugs [4,5] and the American Pain Society guidelines for management of acute and chronic sickle cell pain [6]. The medication’s method of action, side effects, risks, and benefits were reviewed and prescriptions were provided as needed.
During the same visit, patients who reported acute or chronic pain within the last month met with the team psychology provider. The psychology provider educated the patient and family about pain, the mind-body connection, and nonpharmacologic approaches to pain management that could be incorporated in the home plan. Following the education, the psychology provider taught the patient at least one relaxation strategy (eg, diaphragmatic breathing, guided imagery, progressive muscle relaxation) and provided written materials to take home to encourage practice. At the time of discharge from the clinic, patients and families received a copy of the comprehensive home pain plan and any needed prescriptions for analgesics. Families were encouraged to access a copy of their plan at home by logging on to MyChart (Epic Systems), a limited version of the child’s EMR designed for patients and families.
After each ED or urgent care visit for uncomplicated SCD pain, the nurse care manager attempted to call the family within 3 business days to ask whether the home pain management plan had been used and determine if it needed to be revised. Medication refills were confirmed via phone follow-up by the nurse care manager at this time. Laminated pocket guides for the care managers facilitated and standardized the follow-up questions. A maximum of 3 attempts were made to contact the family. Information from the telephone encounter was documented in the patient’s EMR in a standard format and location. This information was then communicated to the SCD provider (nurse practitioner or physician) who modified the plan as needed. If the patient did not have any ED or acute care outpatient visits, the HPMP was reviewed every 6 months at a routinely scheduled comprehensive visit.
The team used multiple plan-do-study-act cycles (PDSAs) to refine the intervention and implementation process. One PDSA involved a focus group consisting of 3 young adult patients and 1 parent. Participants were asked if they knew what we were referring to when we used the term “home pain management plan,” what they remembered about their plan, and if they thought we should keep or change the name. All 4 participants reported that they were familiar with the term and were able to describe aspects of their or their child’s home pain management plan. Although 1 participant suggested shortening the name, the SCD team had worked to develop a high level of familiarity with the name, so it was retained. Another PDSA was conducted to assess whether the pediatric hematology fellows (post-graduate trainees) were aware of the HPMP and how to access it in the EMR. Eight of the 10 fellows responded, and the majority indicated that they were aware of the HPMP; however, only 1 fellow knew where to locate it in the EMR. This resulted in PDSAs to increase fellows’ awareness and use of the HPMP.
The QI team also completed a failure mode and effects analysis (FMEA) to identify potential failures in the clinic flow process. The FMEA helped to identify low-hanging fruit “quick fixes,” PDSAs, and develop process maps. Weekly data guided our PDSAs and allowed us to continuously improve our processes, and team members were accountable for specific weekly action items.
Measurement/Analysis
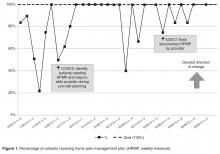
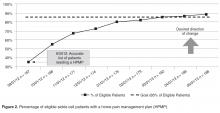
The home pain management implementation process was monitored and tracked using 2 weekly run charts: one that displayed the percentage of eligible SCD patients who needed a HPMP each week that actually received one and one that showed the overall number of eligible SCD patients with a HPMP (population metric). Run charts provide a graphic display of process performance over time and allowed the team to track and monitor process outcomes. The goal was that at least 85% of eligible patients would receive the HPMP intervention by November 2012.
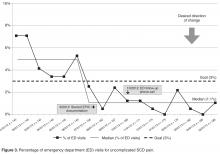
Outcomes were evaluated using a monthly p-chart showing the percentage of SCD patients seen in the ED for uncomplicated SCD pain. For the current project, a p-chart was used because ED visits were categorized (see below) and the sample size varied by month. We conducted a retrospective chart review of each ED visit to extract the initial complaint and the final assessment from the ED providers’ notes. ED visits were categorized as follows: (1) fever (with or without other symptoms such as pain), (2) uncomplicated SCD pain only, and (3) other (eg, trauma, asthma). The goal was to monitor ED visits for uncomplicated SCD pain only to determine if the rate of this type of ED visit decreased after the implementation of the HPMP. Based on the chart review of the 12 months prior to the implementation of the HPMP, the majority of SCD patients seen in the ED had 0–3 ED visits for uncomplicated SCD pain. Only 7 patients had more than 3 ED visits: two had 4 ED visits, two had 5 ED visits, one had 6 visits, one had 7 visits, and one had 13 visits to the ED. Because the patient with 13 visits has complex psychosocial issues that greatly impact the use of the ED and inpatient medical services, this data was excluded from our analyses.
The Children’s Hospital Medical Center Institutional Review Board exempted this study from review because it was deemed to be a QI project with the intent to improve care locally and not to develop generalizable
knowledge.
RESULTS
DISCUSSION
Using quality improvement methods, an individualized home pain management intervention was incorporated successfully into the daily workflow of a busy outpatient SCD clinic. The QI team provided critical guidance, organization, and resources for refining the HPMP intervention and implementing it into a very busy outpatient clinical setting. QI methods such as the PDSAs, FMEA, and process maps allowed us to continuously improve the intervention and develop an effective implementation process. As a result, we were able to reach our goal of ensuring that 100% of eligible patients received a HPMP during their clinic visit.
Several studies have shown cognitive-behavioral therapies, such as relaxation, imagery, and self-hypnosis, to improve outcomes in children and adults with SCD [7–10]. We believe that having psychology providers on our team who could train families in nonpharmacological strategies was critical to the project’s success. Most SCD patients are taught to increase fluid intake and use warm compresses, but few are trained in adjunctive nonpharmacologic strategies while awaiting the effects of oral analgesics. Thus, our multidisciplinary protocol is innovative; future studies may show it to to be more effective than interventions using pharmacologic or nonpharmacologic strategies alone.
Implementing a comprehensive home pain management intervention in a very busy clinical setting was challenging; it required a substantial coordination and communication among the clinical team. Although each member of the team had a well-defined role, we found that our nurse care managers were the drivers of the process during the clinic visit. They ensured the documentation of the HPMP and reconciliation of medications were completed in the EMR, that prescriptions for analgesics were written and educated families to execute the HPMP.
We were able to exceed our goal of ensuring that at least 85% of eligible patients in our population had a home plan in place. This is clinically significant as most SCD pain episodes occur at home [11]. Typically, the pain management strategies used by patients and families at home are inconsistent, and several studies indicate that parents may be reluctant to use analgesics for their children, use a dose that is too small, or do not give the medicine often enough [12–14]. Developing an home pain plan with a patient and family allowed for education about distinguishing different types of pain and the appropriate use of medications for specific types of pain.
Challenges to implementation of the home plan protocol included limited time during clinics visit to integrate the plan given competing clinical issues. Some families felt the visit lasted too long and were eager to leave the clinic without further delays. Additionally, the fixed design of the EMR posed some limitations related to documentation, medication reconciliation, and updating of the home plan because different team members could not simultaneously access some parts of the EMR. We also initially overlooked the need to educate other providers in our division about the home plan, such as fellows who take calls about patients after hours. This has subsequently been addressed via ongoing PDSAs to test processes for making fellows aware of the home pain plan and to ensure they use it consistently to coordinate care.
Following implementation of the protocol, the percentage of ED visits for SCD uncomplicated pain decreased by 84%. These results build on the previous literature which has focused primarily on standardized pain management protocols in the ED [15–17]. However, it makes a unique contribution in that the focus was on systematically teaching families strategies to use at home with the goal of minimizing the need for ED or urgent care intervention. We also learned more about the reasons for some ED visits: there were patients who presented to the ED with presumed acute SCD pain that actually had acute exacerbations of chronic back pain (8 patients), headaches (5 patients), or abdominal pain due to constipation (12 patients). Each of these is managed differently than acute SCD pain, and the HPMP was not designed for these conditions. In addition, we discovered that a few patients (3 patients) used opiate analgesics for difficulties with sleeping rather than pain, further supporting the need for ongoing patient/family education about pain management in pediatric SCD.
We conclude that the home pain plan intervention served to empower patients with SCD and their families by providing them with the tools to manage uncomplicated pain events at home thereby reduce utilization of the ED. Hence, the home plan intervention has the potential to improve patient outcomes by decreasing avoidable ED visits and reducing overall health care costs. It is hoped that other clinics or hospitals could use QI methods to implement home pain plans that would allow achievement of similar outcomes. Finally, this paper contributes to the limited literature on both QI and home management in pediatric SCD and addresses a critical gap in the literature: a clinical approach to reducing potentially preventable ED visits and subsequent hospitalizations for youth with SCD. It also serves as the basis for future innovative research examining the relationship between a home pain management, health care utilization, and health care costs.
Corresponding author: Kenya Simmons, MBA, Cincinnati Children’s Hospital Medical Center, 3333 Burnet Ave., Cincinnati, OH 45229.
Funding/support: This project was funded in part by HRSA grant #U38MC22218 and NIH grant #K07HL108720-03.
References
1. Armstrong FD. Acute and long-term neurodevelopmental outcomes in children following bone marrow transplantation. Front Biosc 2001;6:G6–G12.
2. Brousseau DC, Owens PL, Mosso AL, et al. Acute care utilization and rehospitalizations for sickle cell disease. JAMA 2010;303:1288–94.
3. Platt OS, Thorington BD, Brambilla DJ, et al. Pain in sickle cell disease: rates and risk factors. N Engl J Med 1991;325:11–16.
4. Vargas-Schaffer G. Is the WHO analgesic ladder still valid? Twenty-four years of experience. Can Fam Physician 2010;56:514–7.
5. Ventafridda V, Stjernsward J. Pain control and the World Health Organization analgesic ladder. JAMA 1996;275:835–6.
6. Rees DC, Olujohungbe AD, Parker NE, et al. Guidelines for the management of the acute painful crisis in sickle cell disease. Br J Haematol 2003:120:744–52.
7. Dampier C, Ely E, Eggleston B, et al. Physical and cognitive behavioral activities used in the home management of sickle pain: A daily diary study in children and adolescents. Ped Blood cancer 2004;43:674–8.
8. Dinges DF, Whitehouse WG, Orne EC, et al. Self-hypnosis training as an adjunctive treatment in the management of pain associated with sickle cell disease. Int J Clin Exp Hypnosis 1997;45:417–32.
9. Thomas VN, Wilson Barnett J, Goodhart F. The role of cognitive behavioural therapy in the management of pain in patients with sickle cell disease. J Adv Nurs 1998;27:1002–9.
10. Gil KM, Anthony KK, Carson JW, et al. Daily coping practice predicts treatment effects in children with sickle cell disease. J Ped Psychol 2001;26:163–73.
11. Dampier C, Ely E, Brodecki D, O’Neal P. Home management of pain in sickle cell disease: a daily diary study in children and adolescents. J Ped hematol oncol 2002;24:643–7.
12. Ferrell BR. Pain management: a moral imperative. Communique (Wash DC) 1996;5:4–5.
13. Finley GA, McGrath PJ, Forward SP, et al. Parents’ management of children’s pain following ‘minor’ surgery. Pain 1996;64:83–7.
14. Forward SP, Brown TL, McGrath PJ. Mothers’ attitudes and behavior toward medicating children’s pain. Pain 1996;67:469–74.
15. Givens M, Rutherford C, Joshi G, Delaney K. Impact of an emergency department pain management protocol on the pattern of visits by patients with sickle cell disease. J Emerg Med 2007;32:239–43.
16. Powers RD. Management protocol for sickle-cell disease patients with acute pain: impact on emergency department and narcotic use. Am J Emerg Med 1986;4:267–8.
17. Silbergleit R, Jancis MOS, McNamara RM. Management of sickle cell pain crisis in the emergency department at teaching hospitals. J Emerg Med 1999:17:625–30.
From the Cincinnati Children’s Hospital Medical Center, Cincinnati, OH.
This article is the third in our Hemoglobinopathy Learning Collaborative series. See the related editorial by Oyeku et al in the February 2014 issue of JCOM. (—Ed.)
ABSTRACT
• Objective: To develop and implement individualized home pain management plans that included pharmacologic as well as nonpharmacologic strategies for children with sickle cell disease (SCD).
• Methods: A multidisciplinary quality improvement team developed a questionnaire to assess the frequency, location, and severity of a patient’s pain during a routine comprehensive visit in order to help the patient and family develop an effective home pain management plan. Using plan-do-study-act cycles, the team was able to build this process into the daily workflow for all SCD patients age 5 years to 21 years of age. Patients with comprehensive visits scheduled from January 2012 to May 2013 were included (n = 188) in the intervention.
• Results: By May of 2013, 88% of eligible patients had an individualized home plan in place. There was a concomitant reduction in the percentage of SCD patients seen in the ED for uncomplicated SCD pain (6.9% vs. 1.1%).
• Conclusions: Using quality improvement methods, an individualized home pain management intervention was incorporated successfully into the daily workflow of a busy outpatient SCD clinic. This intervention has the potential to improve patient outcomes by decreasing avoidable ED visits as well as reducing overall health care costs.
Sickle cell disease (SCD) is one of the most common genetic disorders in the United States, affecting approximately 1 in 500 African-American infants each year [1]. The genetic mutation that causes SCD results in the production of an abnormal hemoglobin molecule (HbS) in the red blood cells (RBC). Under low oxygen conditions, the HbS polymerizes and causes the RBCs to elongate into a sickle form (crescent shape) and decreases the life span of the RBC. Additionally, RBCs with HbS are more “sticky,” adhering to vessel walls and limiting blood flow and oxygen delivery to many tissues and organs in the body. The resultant tissue ischemia causes progressive organ injury as well as episodes of pain (vaso-occlusive crisis).
Recurrent pain episodes are the hallmark of this disease, accounting for the majority of emergency department (ED) visits as well as hospitalizations. High-quality outpatient care can reduce acute care and ED visits as well as hospitalization rates in patients with SCD [2]. Additionally, ensuring that patients have a home pain management plan and understand how to assess and reassess their pain may improve outcomes [3]. Data from our population of children with SCD indicate that 40% to 50% of ED visits in 2011 were for uncomplicated pain episodes (no concomitant medical issues such as fever, increased respiratory rate, wheezing, worsening pallor). If these pain episodes had been effectively managed at home, the ED visits might have been avoided.
In an effort to reduce these potentially preventable ED visits and subsequent hospitalizations, the Comprehensive Sickle Cell Center at Cincinnati Children’s Hospital Medical Center assembled a quality improvement (QI) team to partner with patients and their families to develop individualized home pain management plans (HPMP) that incorporated both pharmacologic and nonpharmacologic pain management strategies. We also sought to identify and remove barriers to the successful use of a home pain management plan, such as not having enough analgesics at home or not allowing enough time for analgesics to work before presenting to the ED. We documented the plan in a standard location and format in the electronic medical record (EMR), making it available to all medical center providers. This paper describes the development, refinement, and testing of an individualized HPMP intervention and related outcomes.
METHODS
Setting
Cincinnati Children’s Hospital Medical Center is a nonprofit pediatric medical center with 587 inpatient beds in Ohio providing acute and chronic care for children in Southern Ohio, Northern Kentucky, and Southeastern Indiana. The center’s Comprehensive Sickle Cell Center provides comprehensive care to approximately 280 children with SCD in the region from birth to 21 years of age. The medical center is the only major pediatric inpatient facility in the tri-state area. Greater than 75% of the SCD patients at our center live within a 15-mile radius, therefore, essentially all ED visits and hospitalizations for our patients occur at our center.
Participants
Improvement Team
The core QI team consisted of multidisciplinary health care providers with experience caring for patients with SCD, including 3 SCD nurse care managers, 2 physicians, 2 PhD psychologists, 4 nurse practitioners, a QI consultant, and a data analyst. Additional support and suggestions were received from other SCD team members (eg, social workers, school interventionists). The core QI multidisciplinary team met weekly to design and test the intervention and implementation process.
Intervention
The intervention consisted of the following elements: (1) pre-visit review to identify eligible patients needing a new or updated home pain management plan; (2) family completion of a pain assessment tool; (3) review of pain assessment tool by SCD team; (4) development of collaborative home plan with family and the medical team; (4) integration of nonpharmacological strategies into the home plan (developed with the psychologist); (5) printed copy of the plan for family to take home; (6) documentation of HPMP in the EMR (Table 2); and, (7) a follow-up phone call for eligible patients with ED or urgent care visits for uncomplicated SCD pain by the nurse care manager.
Implementation
Each week the data analyst generated a list of eligible patients with ICD-9 diagnostic codes for SCD using SQL (structured query language) to extract the data from the EMR (Table 1). The SCD nurse care managers reviewed the list and notified the team of those patients needing a pain assessment and updated HPMP during the daily pre-clinic patient review rounds each morning.
The provider seeing the patient that day facilitated the patient and family’s completion of the pain assessment tool. The pain assessment tool consisted of 13 items and measured recent illnesses or transfusions, patient’s pain location, intensity, associated symptoms, potential triggers, and the impact of the pain on quality of life (missed days of school/work). In addition, the patient’s current pain management strategies, perceived effectiveness of those strategies, and analgesics available at home was recorded.
After discussing the results with the team, a medical provider reviewed the findings with the patient and family and developed a plan for pharmacologic pain management at home utilizing a stepwise approach based on the World Health Organization (WHO) analgesic ladder for selecting pain-relief drugs [4,5] and the American Pain Society guidelines for management of acute and chronic sickle cell pain [6]. The medication’s method of action, side effects, risks, and benefits were reviewed and prescriptions were provided as needed.
During the same visit, patients who reported acute or chronic pain within the last month met with the team psychology provider. The psychology provider educated the patient and family about pain, the mind-body connection, and nonpharmacologic approaches to pain management that could be incorporated in the home plan. Following the education, the psychology provider taught the patient at least one relaxation strategy (eg, diaphragmatic breathing, guided imagery, progressive muscle relaxation) and provided written materials to take home to encourage practice. At the time of discharge from the clinic, patients and families received a copy of the comprehensive home pain plan and any needed prescriptions for analgesics. Families were encouraged to access a copy of their plan at home by logging on to MyChart (Epic Systems), a limited version of the child’s EMR designed for patients and families.
After each ED or urgent care visit for uncomplicated SCD pain, the nurse care manager attempted to call the family within 3 business days to ask whether the home pain management plan had been used and determine if it needed to be revised. Medication refills were confirmed via phone follow-up by the nurse care manager at this time. Laminated pocket guides for the care managers facilitated and standardized the follow-up questions. A maximum of 3 attempts were made to contact the family. Information from the telephone encounter was documented in the patient’s EMR in a standard format and location. This information was then communicated to the SCD provider (nurse practitioner or physician) who modified the plan as needed. If the patient did not have any ED or acute care outpatient visits, the HPMP was reviewed every 6 months at a routinely scheduled comprehensive visit.
The team used multiple plan-do-study-act cycles (PDSAs) to refine the intervention and implementation process. One PDSA involved a focus group consisting of 3 young adult patients and 1 parent. Participants were asked if they knew what we were referring to when we used the term “home pain management plan,” what they remembered about their plan, and if they thought we should keep or change the name. All 4 participants reported that they were familiar with the term and were able to describe aspects of their or their child’s home pain management plan. Although 1 participant suggested shortening the name, the SCD team had worked to develop a high level of familiarity with the name, so it was retained. Another PDSA was conducted to assess whether the pediatric hematology fellows (post-graduate trainees) were aware of the HPMP and how to access it in the EMR. Eight of the 10 fellows responded, and the majority indicated that they were aware of the HPMP; however, only 1 fellow knew where to locate it in the EMR. This resulted in PDSAs to increase fellows’ awareness and use of the HPMP.
The QI team also completed a failure mode and effects analysis (FMEA) to identify potential failures in the clinic flow process. The FMEA helped to identify low-hanging fruit “quick fixes,” PDSAs, and develop process maps. Weekly data guided our PDSAs and allowed us to continuously improve our processes, and team members were accountable for specific weekly action items.
Measurement/Analysis
The home pain management implementation process was monitored and tracked using 2 weekly run charts: one that displayed the percentage of eligible SCD patients who needed a HPMP each week that actually received one and one that showed the overall number of eligible SCD patients with a HPMP (population metric). Run charts provide a graphic display of process performance over time and allowed the team to track and monitor process outcomes. The goal was that at least 85% of eligible patients would receive the HPMP intervention by November 2012.
Outcomes were evaluated using a monthly p-chart showing the percentage of SCD patients seen in the ED for uncomplicated SCD pain. For the current project, a p-chart was used because ED visits were categorized (see below) and the sample size varied by month. We conducted a retrospective chart review of each ED visit to extract the initial complaint and the final assessment from the ED providers’ notes. ED visits were categorized as follows: (1) fever (with or without other symptoms such as pain), (2) uncomplicated SCD pain only, and (3) other (eg, trauma, asthma). The goal was to monitor ED visits for uncomplicated SCD pain only to determine if the rate of this type of ED visit decreased after the implementation of the HPMP. Based on the chart review of the 12 months prior to the implementation of the HPMP, the majority of SCD patients seen in the ED had 0–3 ED visits for uncomplicated SCD pain. Only 7 patients had more than 3 ED visits: two had 4 ED visits, two had 5 ED visits, one had 6 visits, one had 7 visits, and one had 13 visits to the ED. Because the patient with 13 visits has complex psychosocial issues that greatly impact the use of the ED and inpatient medical services, this data was excluded from our analyses.
The Children’s Hospital Medical Center Institutional Review Board exempted this study from review because it was deemed to be a QI project with the intent to improve care locally and not to develop generalizable
knowledge.
RESULTS
DISCUSSION
Using quality improvement methods, an individualized home pain management intervention was incorporated successfully into the daily workflow of a busy outpatient SCD clinic. The QI team provided critical guidance, organization, and resources for refining the HPMP intervention and implementing it into a very busy outpatient clinical setting. QI methods such as the PDSAs, FMEA, and process maps allowed us to continuously improve the intervention and develop an effective implementation process. As a result, we were able to reach our goal of ensuring that 100% of eligible patients received a HPMP during their clinic visit.
Several studies have shown cognitive-behavioral therapies, such as relaxation, imagery, and self-hypnosis, to improve outcomes in children and adults with SCD [7–10]. We believe that having psychology providers on our team who could train families in nonpharmacological strategies was critical to the project’s success. Most SCD patients are taught to increase fluid intake and use warm compresses, but few are trained in adjunctive nonpharmacologic strategies while awaiting the effects of oral analgesics. Thus, our multidisciplinary protocol is innovative; future studies may show it to to be more effective than interventions using pharmacologic or nonpharmacologic strategies alone.
Implementing a comprehensive home pain management intervention in a very busy clinical setting was challenging; it required a substantial coordination and communication among the clinical team. Although each member of the team had a well-defined role, we found that our nurse care managers were the drivers of the process during the clinic visit. They ensured the documentation of the HPMP and reconciliation of medications were completed in the EMR, that prescriptions for analgesics were written and educated families to execute the HPMP.
We were able to exceed our goal of ensuring that at least 85% of eligible patients in our population had a home plan in place. This is clinically significant as most SCD pain episodes occur at home [11]. Typically, the pain management strategies used by patients and families at home are inconsistent, and several studies indicate that parents may be reluctant to use analgesics for their children, use a dose that is too small, or do not give the medicine often enough [12–14]. Developing an home pain plan with a patient and family allowed for education about distinguishing different types of pain and the appropriate use of medications for specific types of pain.
Challenges to implementation of the home plan protocol included limited time during clinics visit to integrate the plan given competing clinical issues. Some families felt the visit lasted too long and were eager to leave the clinic without further delays. Additionally, the fixed design of the EMR posed some limitations related to documentation, medication reconciliation, and updating of the home plan because different team members could not simultaneously access some parts of the EMR. We also initially overlooked the need to educate other providers in our division about the home plan, such as fellows who take calls about patients after hours. This has subsequently been addressed via ongoing PDSAs to test processes for making fellows aware of the home pain plan and to ensure they use it consistently to coordinate care.
Following implementation of the protocol, the percentage of ED visits for SCD uncomplicated pain decreased by 84%. These results build on the previous literature which has focused primarily on standardized pain management protocols in the ED [15–17]. However, it makes a unique contribution in that the focus was on systematically teaching families strategies to use at home with the goal of minimizing the need for ED or urgent care intervention. We also learned more about the reasons for some ED visits: there were patients who presented to the ED with presumed acute SCD pain that actually had acute exacerbations of chronic back pain (8 patients), headaches (5 patients), or abdominal pain due to constipation (12 patients). Each of these is managed differently than acute SCD pain, and the HPMP was not designed for these conditions. In addition, we discovered that a few patients (3 patients) used opiate analgesics for difficulties with sleeping rather than pain, further supporting the need for ongoing patient/family education about pain management in pediatric SCD.
We conclude that the home pain plan intervention served to empower patients with SCD and their families by providing them with the tools to manage uncomplicated pain events at home thereby reduce utilization of the ED. Hence, the home plan intervention has the potential to improve patient outcomes by decreasing avoidable ED visits and reducing overall health care costs. It is hoped that other clinics or hospitals could use QI methods to implement home pain plans that would allow achievement of similar outcomes. Finally, this paper contributes to the limited literature on both QI and home management in pediatric SCD and addresses a critical gap in the literature: a clinical approach to reducing potentially preventable ED visits and subsequent hospitalizations for youth with SCD. It also serves as the basis for future innovative research examining the relationship between a home pain management, health care utilization, and health care costs.
Corresponding author: Kenya Simmons, MBA, Cincinnati Children’s Hospital Medical Center, 3333 Burnet Ave., Cincinnati, OH 45229.
Funding/support: This project was funded in part by HRSA grant #U38MC22218 and NIH grant #K07HL108720-03.
References
1. Armstrong FD. Acute and long-term neurodevelopmental outcomes in children following bone marrow transplantation. Front Biosc 2001;6:G6–G12.
2. Brousseau DC, Owens PL, Mosso AL, et al. Acute care utilization and rehospitalizations for sickle cell disease. JAMA 2010;303:1288–94.
3. Platt OS, Thorington BD, Brambilla DJ, et al. Pain in sickle cell disease: rates and risk factors. N Engl J Med 1991;325:11–16.
4. Vargas-Schaffer G. Is the WHO analgesic ladder still valid? Twenty-four years of experience. Can Fam Physician 2010;56:514–7.
5. Ventafridda V, Stjernsward J. Pain control and the World Health Organization analgesic ladder. JAMA 1996;275:835–6.
6. Rees DC, Olujohungbe AD, Parker NE, et al. Guidelines for the management of the acute painful crisis in sickle cell disease. Br J Haematol 2003:120:744–52.
7. Dampier C, Ely E, Eggleston B, et al. Physical and cognitive behavioral activities used in the home management of sickle pain: A daily diary study in children and adolescents. Ped Blood cancer 2004;43:674–8.
8. Dinges DF, Whitehouse WG, Orne EC, et al. Self-hypnosis training as an adjunctive treatment in the management of pain associated with sickle cell disease. Int J Clin Exp Hypnosis 1997;45:417–32.
9. Thomas VN, Wilson Barnett J, Goodhart F. The role of cognitive behavioural therapy in the management of pain in patients with sickle cell disease. J Adv Nurs 1998;27:1002–9.
10. Gil KM, Anthony KK, Carson JW, et al. Daily coping practice predicts treatment effects in children with sickle cell disease. J Ped Psychol 2001;26:163–73.
11. Dampier C, Ely E, Brodecki D, O’Neal P. Home management of pain in sickle cell disease: a daily diary study in children and adolescents. J Ped hematol oncol 2002;24:643–7.
12. Ferrell BR. Pain management: a moral imperative. Communique (Wash DC) 1996;5:4–5.
13. Finley GA, McGrath PJ, Forward SP, et al. Parents’ management of children’s pain following ‘minor’ surgery. Pain 1996;64:83–7.
14. Forward SP, Brown TL, McGrath PJ. Mothers’ attitudes and behavior toward medicating children’s pain. Pain 1996;67:469–74.
15. Givens M, Rutherford C, Joshi G, Delaney K. Impact of an emergency department pain management protocol on the pattern of visits by patients with sickle cell disease. J Emerg Med 2007;32:239–43.
16. Powers RD. Management protocol for sickle-cell disease patients with acute pain: impact on emergency department and narcotic use. Am J Emerg Med 1986;4:267–8.
17. Silbergleit R, Jancis MOS, McNamara RM. Management of sickle cell pain crisis in the emergency department at teaching hospitals. J Emerg Med 1999:17:625–30.
From the Cincinnati Children’s Hospital Medical Center, Cincinnati, OH.
This article is the third in our Hemoglobinopathy Learning Collaborative series. See the related editorial by Oyeku et al in the February 2014 issue of JCOM. (—Ed.)
ABSTRACT
• Objective: To develop and implement individualized home pain management plans that included pharmacologic as well as nonpharmacologic strategies for children with sickle cell disease (SCD).
• Methods: A multidisciplinary quality improvement team developed a questionnaire to assess the frequency, location, and severity of a patient’s pain during a routine comprehensive visit in order to help the patient and family develop an effective home pain management plan. Using plan-do-study-act cycles, the team was able to build this process into the daily workflow for all SCD patients age 5 years to 21 years of age. Patients with comprehensive visits scheduled from January 2012 to May 2013 were included (n = 188) in the intervention.
• Results: By May of 2013, 88% of eligible patients had an individualized home plan in place. There was a concomitant reduction in the percentage of SCD patients seen in the ED for uncomplicated SCD pain (6.9% vs. 1.1%).
• Conclusions: Using quality improvement methods, an individualized home pain management intervention was incorporated successfully into the daily workflow of a busy outpatient SCD clinic. This intervention has the potential to improve patient outcomes by decreasing avoidable ED visits as well as reducing overall health care costs.
Sickle cell disease (SCD) is one of the most common genetic disorders in the United States, affecting approximately 1 in 500 African-American infants each year [1]. The genetic mutation that causes SCD results in the production of an abnormal hemoglobin molecule (HbS) in the red blood cells (RBC). Under low oxygen conditions, the HbS polymerizes and causes the RBCs to elongate into a sickle form (crescent shape) and decreases the life span of the RBC. Additionally, RBCs with HbS are more “sticky,” adhering to vessel walls and limiting blood flow and oxygen delivery to many tissues and organs in the body. The resultant tissue ischemia causes progressive organ injury as well as episodes of pain (vaso-occlusive crisis).
Recurrent pain episodes are the hallmark of this disease, accounting for the majority of emergency department (ED) visits as well as hospitalizations. High-quality outpatient care can reduce acute care and ED visits as well as hospitalization rates in patients with SCD [2]. Additionally, ensuring that patients have a home pain management plan and understand how to assess and reassess their pain may improve outcomes [3]. Data from our population of children with SCD indicate that 40% to 50% of ED visits in 2011 were for uncomplicated pain episodes (no concomitant medical issues such as fever, increased respiratory rate, wheezing, worsening pallor). If these pain episodes had been effectively managed at home, the ED visits might have been avoided.
In an effort to reduce these potentially preventable ED visits and subsequent hospitalizations, the Comprehensive Sickle Cell Center at Cincinnati Children’s Hospital Medical Center assembled a quality improvement (QI) team to partner with patients and their families to develop individualized home pain management plans (HPMP) that incorporated both pharmacologic and nonpharmacologic pain management strategies. We also sought to identify and remove barriers to the successful use of a home pain management plan, such as not having enough analgesics at home or not allowing enough time for analgesics to work before presenting to the ED. We documented the plan in a standard location and format in the electronic medical record (EMR), making it available to all medical center providers. This paper describes the development, refinement, and testing of an individualized HPMP intervention and related outcomes.
METHODS
Setting
Cincinnati Children’s Hospital Medical Center is a nonprofit pediatric medical center with 587 inpatient beds in Ohio providing acute and chronic care for children in Southern Ohio, Northern Kentucky, and Southeastern Indiana. The center’s Comprehensive Sickle Cell Center provides comprehensive care to approximately 280 children with SCD in the region from birth to 21 years of age. The medical center is the only major pediatric inpatient facility in the tri-state area. Greater than 75% of the SCD patients at our center live within a 15-mile radius, therefore, essentially all ED visits and hospitalizations for our patients occur at our center.
Participants
Improvement Team
The core QI team consisted of multidisciplinary health care providers with experience caring for patients with SCD, including 3 SCD nurse care managers, 2 physicians, 2 PhD psychologists, 4 nurse practitioners, a QI consultant, and a data analyst. Additional support and suggestions were received from other SCD team members (eg, social workers, school interventionists). The core QI multidisciplinary team met weekly to design and test the intervention and implementation process.
Intervention
The intervention consisted of the following elements: (1) pre-visit review to identify eligible patients needing a new or updated home pain management plan; (2) family completion of a pain assessment tool; (3) review of pain assessment tool by SCD team; (4) development of collaborative home plan with family and the medical team; (4) integration of nonpharmacological strategies into the home plan (developed with the psychologist); (5) printed copy of the plan for family to take home; (6) documentation of HPMP in the EMR (Table 2); and, (7) a follow-up phone call for eligible patients with ED or urgent care visits for uncomplicated SCD pain by the nurse care manager.
Implementation
Each week the data analyst generated a list of eligible patients with ICD-9 diagnostic codes for SCD using SQL (structured query language) to extract the data from the EMR (Table 1). The SCD nurse care managers reviewed the list and notified the team of those patients needing a pain assessment and updated HPMP during the daily pre-clinic patient review rounds each morning.
The provider seeing the patient that day facilitated the patient and family’s completion of the pain assessment tool. The pain assessment tool consisted of 13 items and measured recent illnesses or transfusions, patient’s pain location, intensity, associated symptoms, potential triggers, and the impact of the pain on quality of life (missed days of school/work). In addition, the patient’s current pain management strategies, perceived effectiveness of those strategies, and analgesics available at home was recorded.
After discussing the results with the team, a medical provider reviewed the findings with the patient and family and developed a plan for pharmacologic pain management at home utilizing a stepwise approach based on the World Health Organization (WHO) analgesic ladder for selecting pain-relief drugs [4,5] and the American Pain Society guidelines for management of acute and chronic sickle cell pain [6]. The medication’s method of action, side effects, risks, and benefits were reviewed and prescriptions were provided as needed.
During the same visit, patients who reported acute or chronic pain within the last month met with the team psychology provider. The psychology provider educated the patient and family about pain, the mind-body connection, and nonpharmacologic approaches to pain management that could be incorporated in the home plan. Following the education, the psychology provider taught the patient at least one relaxation strategy (eg, diaphragmatic breathing, guided imagery, progressive muscle relaxation) and provided written materials to take home to encourage practice. At the time of discharge from the clinic, patients and families received a copy of the comprehensive home pain plan and any needed prescriptions for analgesics. Families were encouraged to access a copy of their plan at home by logging on to MyChart (Epic Systems), a limited version of the child’s EMR designed for patients and families.
After each ED or urgent care visit for uncomplicated SCD pain, the nurse care manager attempted to call the family within 3 business days to ask whether the home pain management plan had been used and determine if it needed to be revised. Medication refills were confirmed via phone follow-up by the nurse care manager at this time. Laminated pocket guides for the care managers facilitated and standardized the follow-up questions. A maximum of 3 attempts were made to contact the family. Information from the telephone encounter was documented in the patient’s EMR in a standard format and location. This information was then communicated to the SCD provider (nurse practitioner or physician) who modified the plan as needed. If the patient did not have any ED or acute care outpatient visits, the HPMP was reviewed every 6 months at a routinely scheduled comprehensive visit.
The team used multiple plan-do-study-act cycles (PDSAs) to refine the intervention and implementation process. One PDSA involved a focus group consisting of 3 young adult patients and 1 parent. Participants were asked if they knew what we were referring to when we used the term “home pain management plan,” what they remembered about their plan, and if they thought we should keep or change the name. All 4 participants reported that they were familiar with the term and were able to describe aspects of their or their child’s home pain management plan. Although 1 participant suggested shortening the name, the SCD team had worked to develop a high level of familiarity with the name, so it was retained. Another PDSA was conducted to assess whether the pediatric hematology fellows (post-graduate trainees) were aware of the HPMP and how to access it in the EMR. Eight of the 10 fellows responded, and the majority indicated that they were aware of the HPMP; however, only 1 fellow knew where to locate it in the EMR. This resulted in PDSAs to increase fellows’ awareness and use of the HPMP.
The QI team also completed a failure mode and effects analysis (FMEA) to identify potential failures in the clinic flow process. The FMEA helped to identify low-hanging fruit “quick fixes,” PDSAs, and develop process maps. Weekly data guided our PDSAs and allowed us to continuously improve our processes, and team members were accountable for specific weekly action items.
Measurement/Analysis
The home pain management implementation process was monitored and tracked using 2 weekly run charts: one that displayed the percentage of eligible SCD patients who needed a HPMP each week that actually received one and one that showed the overall number of eligible SCD patients with a HPMP (population metric). Run charts provide a graphic display of process performance over time and allowed the team to track and monitor process outcomes. The goal was that at least 85% of eligible patients would receive the HPMP intervention by November 2012.
Outcomes were evaluated using a monthly p-chart showing the percentage of SCD patients seen in the ED for uncomplicated SCD pain. For the current project, a p-chart was used because ED visits were categorized (see below) and the sample size varied by month. We conducted a retrospective chart review of each ED visit to extract the initial complaint and the final assessment from the ED providers’ notes. ED visits were categorized as follows: (1) fever (with or without other symptoms such as pain), (2) uncomplicated SCD pain only, and (3) other (eg, trauma, asthma). The goal was to monitor ED visits for uncomplicated SCD pain only to determine if the rate of this type of ED visit decreased after the implementation of the HPMP. Based on the chart review of the 12 months prior to the implementation of the HPMP, the majority of SCD patients seen in the ED had 0–3 ED visits for uncomplicated SCD pain. Only 7 patients had more than 3 ED visits: two had 4 ED visits, two had 5 ED visits, one had 6 visits, one had 7 visits, and one had 13 visits to the ED. Because the patient with 13 visits has complex psychosocial issues that greatly impact the use of the ED and inpatient medical services, this data was excluded from our analyses.
The Children’s Hospital Medical Center Institutional Review Board exempted this study from review because it was deemed to be a QI project with the intent to improve care locally and not to develop generalizable
knowledge.
RESULTS
DISCUSSION
Using quality improvement methods, an individualized home pain management intervention was incorporated successfully into the daily workflow of a busy outpatient SCD clinic. The QI team provided critical guidance, organization, and resources for refining the HPMP intervention and implementing it into a very busy outpatient clinical setting. QI methods such as the PDSAs, FMEA, and process maps allowed us to continuously improve the intervention and develop an effective implementation process. As a result, we were able to reach our goal of ensuring that 100% of eligible patients received a HPMP during their clinic visit.
Several studies have shown cognitive-behavioral therapies, such as relaxation, imagery, and self-hypnosis, to improve outcomes in children and adults with SCD [7–10]. We believe that having psychology providers on our team who could train families in nonpharmacological strategies was critical to the project’s success. Most SCD patients are taught to increase fluid intake and use warm compresses, but few are trained in adjunctive nonpharmacologic strategies while awaiting the effects of oral analgesics. Thus, our multidisciplinary protocol is innovative; future studies may show it to to be more effective than interventions using pharmacologic or nonpharmacologic strategies alone.
Implementing a comprehensive home pain management intervention in a very busy clinical setting was challenging; it required a substantial coordination and communication among the clinical team. Although each member of the team had a well-defined role, we found that our nurse care managers were the drivers of the process during the clinic visit. They ensured the documentation of the HPMP and reconciliation of medications were completed in the EMR, that prescriptions for analgesics were written and educated families to execute the HPMP.
We were able to exceed our goal of ensuring that at least 85% of eligible patients in our population had a home plan in place. This is clinically significant as most SCD pain episodes occur at home [11]. Typically, the pain management strategies used by patients and families at home are inconsistent, and several studies indicate that parents may be reluctant to use analgesics for their children, use a dose that is too small, or do not give the medicine often enough [12–14]. Developing an home pain plan with a patient and family allowed for education about distinguishing different types of pain and the appropriate use of medications for specific types of pain.
Challenges to implementation of the home plan protocol included limited time during clinics visit to integrate the plan given competing clinical issues. Some families felt the visit lasted too long and were eager to leave the clinic without further delays. Additionally, the fixed design of the EMR posed some limitations related to documentation, medication reconciliation, and updating of the home plan because different team members could not simultaneously access some parts of the EMR. We also initially overlooked the need to educate other providers in our division about the home plan, such as fellows who take calls about patients after hours. This has subsequently been addressed via ongoing PDSAs to test processes for making fellows aware of the home pain plan and to ensure they use it consistently to coordinate care.
Following implementation of the protocol, the percentage of ED visits for SCD uncomplicated pain decreased by 84%. These results build on the previous literature which has focused primarily on standardized pain management protocols in the ED [15–17]. However, it makes a unique contribution in that the focus was on systematically teaching families strategies to use at home with the goal of minimizing the need for ED or urgent care intervention. We also learned more about the reasons for some ED visits: there were patients who presented to the ED with presumed acute SCD pain that actually had acute exacerbations of chronic back pain (8 patients), headaches (5 patients), or abdominal pain due to constipation (12 patients). Each of these is managed differently than acute SCD pain, and the HPMP was not designed for these conditions. In addition, we discovered that a few patients (3 patients) used opiate analgesics for difficulties with sleeping rather than pain, further supporting the need for ongoing patient/family education about pain management in pediatric SCD.
We conclude that the home pain plan intervention served to empower patients with SCD and their families by providing them with the tools to manage uncomplicated pain events at home thereby reduce utilization of the ED. Hence, the home plan intervention has the potential to improve patient outcomes by decreasing avoidable ED visits and reducing overall health care costs. It is hoped that other clinics or hospitals could use QI methods to implement home pain plans that would allow achievement of similar outcomes. Finally, this paper contributes to the limited literature on both QI and home management in pediatric SCD and addresses a critical gap in the literature: a clinical approach to reducing potentially preventable ED visits and subsequent hospitalizations for youth with SCD. It also serves as the basis for future innovative research examining the relationship between a home pain management, health care utilization, and health care costs.
Corresponding author: Kenya Simmons, MBA, Cincinnati Children’s Hospital Medical Center, 3333 Burnet Ave., Cincinnati, OH 45229.
Funding/support: This project was funded in part by HRSA grant #U38MC22218 and NIH grant #K07HL108720-03.
References
1. Armstrong FD. Acute and long-term neurodevelopmental outcomes in children following bone marrow transplantation. Front Biosc 2001;6:G6–G12.
2. Brousseau DC, Owens PL, Mosso AL, et al. Acute care utilization and rehospitalizations for sickle cell disease. JAMA 2010;303:1288–94.
3. Platt OS, Thorington BD, Brambilla DJ, et al. Pain in sickle cell disease: rates and risk factors. N Engl J Med 1991;325:11–16.
4. Vargas-Schaffer G. Is the WHO analgesic ladder still valid? Twenty-four years of experience. Can Fam Physician 2010;56:514–7.
5. Ventafridda V, Stjernsward J. Pain control and the World Health Organization analgesic ladder. JAMA 1996;275:835–6.
6. Rees DC, Olujohungbe AD, Parker NE, et al. Guidelines for the management of the acute painful crisis in sickle cell disease. Br J Haematol 2003:120:744–52.
7. Dampier C, Ely E, Eggleston B, et al. Physical and cognitive behavioral activities used in the home management of sickle pain: A daily diary study in children and adolescents. Ped Blood cancer 2004;43:674–8.
8. Dinges DF, Whitehouse WG, Orne EC, et al. Self-hypnosis training as an adjunctive treatment in the management of pain associated with sickle cell disease. Int J Clin Exp Hypnosis 1997;45:417–32.
9. Thomas VN, Wilson Barnett J, Goodhart F. The role of cognitive behavioural therapy in the management of pain in patients with sickle cell disease. J Adv Nurs 1998;27:1002–9.
10. Gil KM, Anthony KK, Carson JW, et al. Daily coping practice predicts treatment effects in children with sickle cell disease. J Ped Psychol 2001;26:163–73.
11. Dampier C, Ely E, Brodecki D, O’Neal P. Home management of pain in sickle cell disease: a daily diary study in children and adolescents. J Ped hematol oncol 2002;24:643–7.
12. Ferrell BR. Pain management: a moral imperative. Communique (Wash DC) 1996;5:4–5.
13. Finley GA, McGrath PJ, Forward SP, et al. Parents’ management of children’s pain following ‘minor’ surgery. Pain 1996;64:83–7.
14. Forward SP, Brown TL, McGrath PJ. Mothers’ attitudes and behavior toward medicating children’s pain. Pain 1996;67:469–74.
15. Givens M, Rutherford C, Joshi G, Delaney K. Impact of an emergency department pain management protocol on the pattern of visits by patients with sickle cell disease. J Emerg Med 2007;32:239–43.
16. Powers RD. Management protocol for sickle-cell disease patients with acute pain: impact on emergency department and narcotic use. Am J Emerg Med 1986;4:267–8.
17. Silbergleit R, Jancis MOS, McNamara RM. Management of sickle cell pain crisis in the emergency department at teaching hospitals. J Emerg Med 1999:17:625–30.